Calf cramp when walking
Claudication (Cramp when walking) - Vascular Society
Leg pain walking due to poor circulation
Claudication is a common condition where pain occurs in the legs with exercise due to a reduction in the circulation. The cause is hardening of the arteries otherwise known as atherosclerosis. The common symptom is of a cramp like pain developing in the calf muscles on walking. The thigh and buttock muscles may also be involved. After a brief rest the pain resolves and it is possible to walk on again. The distance walked along the flat (not up hills) before the pain starts is used as a rough guide to the severity of the condition. During walking the leg muscles use more oxygen which is supplied by the circulating blood. If the supply is reduced the oxygen is used up and the muscles become painful. After a rest the oxygen levels return to normal and it is possible to walk again.
With the above symptoms and an examination of the pulses in the leg (weak or absent) it is often possible to diagnose claudication without any tests. The blood pressure in the legs can be measured with doppler, at rest and after walking on a treadmill, to confirm the diagnosis.
TREATMENT.
The most important part of the treatment is to make sure your arteries do not get any worse. Atherosclerosis not only affects the arteries in your leg, but also those to your heart causing heart attacks, and your brain causing strokes. If you smoke it is vital that you stop altogether. You will be tested for diabetes, high blood pressure and raised cholesterol. These may require you to go on a diet or start some medication if you are not already on treatment. If you are overweight, losing weight will help your arteries and enable you to walk further. Lastly, it has been shown that taking a small dose of aspirin (75 mgs) once a day also helps the arteries.
If you are overweight, losing weight will help your arteries and enable you to walk further. Lastly, it has been shown that taking a small dose of aspirin (75 mgs) once a day also helps the arteries.
Regular exercise is good for the legs. Although walking can be frustrating because of the frequent stops when the legs are painful, it is important to persist and try to walk each day, increasing the distance as the legs improve. Do not try to “walk through the pain”. Over a period of 3 - 6 months the muscles in the legs will become more efficient enabling you to walk further on the limited blood supply. In addition the blood flow in the leg will increase as smaller undiseased arteries increase in size. It is uncommon for the legs to get worse. Many patients are worried they may lose their leg but with the above treatment this is extremely unlikely and not a cause for concern.
If the claudication remains troublesome then you will need an ultrasound scan of the leg or an angiogram to see exactly where the narrowings or blockages in the arteries are.
ANGIOGRAM: this can be performed with a CT or MRI scan with some dye injected into the bloodstream, which allows the scan to highlight the arteries. If you are allergic to the dye or have reduced kidney function then this investigation may not be appropriate for you or special precautions may need to be taken.
Some narrowings and blockages in your arteries can be treated by using a balloon to stretch the artery open again. This is called an angioplasty . In some arteries the results of angioplasty can be improved by also putting a stent inside the artery. This is like an internal sophisticated “scaffold” that holds the artery open. Medication can be attached to the stent to reduce the risk of the stent being narrowed by growth of new tissue into the artery.
If there is a long or very hard blockage in the artery, it may not be possible to get through an perform an angioplasty. In these circumstances, if the claudication is bad, a bypass operation will be considered and discussed with you. In some cases the risks of surgery are to high and a longer period spent exercising, losing weight etc.. is needed.
In these circumstances, if the claudication is bad, a bypass operation will be considered and discussed with you. In some cases the risks of surgery are to high and a longer period spent exercising, losing weight etc.. is needed.
Calf Pain When Walking: Causes, Symptoms, Treatment, Prevention
Your calves are located at the back of your lower legs. The muscles in your calves are vital for activities like walking, running, and jumping. They’re also responsible for helping you bend your foot downward or stand on your tiptoes.
Sometimes, you may feel calf pain when you walk. This can be due to a variety of causes. In this article, we’ll take a closer look at the most common causes of calf pain when walking, the treatment options, and when to call your doctor.
There are a variety of reasons why you may feel calf pain when you walk. Some causes are due to common muscle conditions, while others may be due to an underlying health condition.
Below, we’ll explore what can cause this type of pain, the symptoms you may feel, and any preventive steps you can take.
Muscle cramps happen when your muscles contract involuntarily. They most commonly affect your legs, including your calves. These cramps often happen when you’re walking, running, or engaging in some type of physical activity.
Muscle cramps can have many causes, though sometimes the cause is unknown. Some of the most common causes include:
- not stretching properly before physical activity
- overuse of your muscles
- dehydration
- low electrolyte levels
- low blood supply to the muscles
The main symptom of muscle cramping is pain, which can range in intensity from mild to severe. The affected muscle may also feel hard to the touch.
A cramp can last anywhere from a few seconds to several minutes.
There are steps you can take to help reduce the likelihood of having a cramp in your calf muscles. These include staying hydrated and stretching before starting any type of physical activity.
These include staying hydrated and stretching before starting any type of physical activity.
An injury to your calf muscle can also lead to pain when walking. The most common injuries that can cause pain in your lower legs include bruises and strains.
- A bruise happens when a blow to the body damages the underlying muscle and other tissues without breaking the skin.
- A strain occurs when a muscle is overused or overstretched, causing damage to the muscle fibers.
Common symptoms of a calf muscle injury include:
- pain in the affected area, which often occurs with movement
- a visible bruise
- swelling
- tenderness
Many bruises or strains can be treated at home. However, more serious injuries may need to be evaluated by a doctor.
You can help prevent calf muscle injuries by:
- stretching and warming up before physical activity
- maintaining a healthy weight
- practicing good posture
Peripheral artery disease (PAD) is a condition where plaque builds up in the arteries that carry blood to areas like your legs, arms, and internal organs.
PAD is caused by damage to your arteries, which can be a result of:
- diabetes
- high blood pressure
- high cholesterol
- smoking
If you have PAD, you may experience intermittent claudication, or pain when you walk or climb stairs that goes away with rest. This is because your muscles aren’t getting enough blood. This is due to blood vessels that have become narrowed or blocked.
Other symptoms of PAD include:
- skin that’s pale or blue
- a weak pulse in your legs or feet
- slow wound healing
The management of PAD is lifelong and is aimed at slowing the progression of the condition. To prevent PAD from progressing, it’s important to:
- take steps to manage and monitor your glucose levels, cholesterol levels, and blood pressure
- not smoke
- get regular exercise
- focus on a heart-healthy diet
- maintain a healthy weight
Chronic venous insufficiency (CVI) is when your blood has trouble flowing back to your heart from your legs.
Valves in your veins typically help keep blood flowing. But with CVI, these valves are less functional. This can lead to backflow or pooling of blood in your legs.
With CVI, you may feel pain in your legs when walking that eases when you rest or elevate your legs. Additional symptoms can include:
- calves that feel tight
- varicose veins
- swelling in your legs or ankles
- cramping or muscle spasms
- discolored skin
- ulcers on your legs
CVI needs to be treated to prevent complications like leg ulcers or deep vein thrombosis. The recommended treatment will depend on the severity of the condition.
Lumbar spinal stenosis is when pressure is placed on the nerves in your lower back due to the narrowing of your spinal canal. It’s often caused by issues like degenerative disc disease or the formation of bone spurs.
Lumbar spinal stenosis can cause pain or cramping in your calves or thighs when walking. The pain may ease when you bend forward, sit, or lie down.
In addition to pain, you may also feel weakness or numbness in your legs.
Generally, lumbar spinal stenosis is managed through conservative measures, such as physical therapy and pain management. Severe cases may require surgery.
Chronic exertional compartment syndrome (CECS) is when a specific group of muscles, called a compartment, swells during exertion. This leads to an increase in pressure within the compartment, which decreases blood flow and leads to pain.
CECS most often affects people who do activities with repetitive leg motions, like fast walking, running, or swimming.
If you have CECS, you may experience pain in your calves during physical activity. The pain typically goes away when the activity stops. Other symptoms may include:
- numbness
- muscle bulging
- trouble moving your foot
CECS usually isn’t serious, and the pain goes away when you rest. You can help prevent CECS by avoiding the types of activities that cause pain.
Make an appointment with your doctor if you have calf pain when walking that:
- doesn’t improve or gets worse with a few days of at-home care
- makes moving around or performing daily activities difficult
- affects your range of movement
Seek prompt medical attention if you notice:
- swelling in one or both legs
- a leg that’s unusually pale or cool to the touch
- calf pain that occurs after a long period of sitting, such as after a long plane trip or car ride
- signs of infection, including fever, redness, and tenderness
- any leg symptoms that develop suddenly and can’t be explained by a specific event or condition
The Healthline FindCare tool can provide options in your area if you don’t already have a doctor.
To diagnose the cause of your calf pain, your doctor will first take your medical history and perform a physical examination. They may also use additional tests to help diagnose your condition. These tests may include:
These tests may include:
- Imaging. Using imaging technology like X-ray, CT scan, or ultrasound can help your doctor better visualize the structures in the affected area.
- Ankle-brachial index. An ankle-brachial index compares the blood pressure in your ankle with the blood pressure in your arm. It can help determine how well blood is flowing in your limbs.
- Treadmill test. While monitoring you on a treadmill, your doctor can get an idea of how severe your symptoms are and what level of physical activity brings them on.
- Blood tests. Blood tests can check for high cholesterol, diabetes, and other underlying conditions.
- Electromyography (EMG). EMG is used to record the electrical activity of your muscles. Your doctor may use this if they suspect a problem with nerve signaling.
The treatment of calf pain will depend on the condition or issue that’s causing the pain. Potential treatment may include:
Potential treatment may include:
- Medications. If you have an underlying condition that’s contributing to your calf pain, your doctor may prescribe medication to treat it. One example is medication to lower blood pressure or cholesterol in PAD.
- Physical therapy. Physical therapy can help improve flexibility, strength, and movement. Your doctor may recommend this type of therapy to help with conditions like:
- muscle injuries
- lumbar spinal stenosis
- CECS
- Surgery. In severe cases, surgery may be recommended. Examples include:
- surgery to repair severe muscle injuries
- angioplasty to open arteries in PAD
- laminectomy to relieve pressure on nerves due to lumbar spinal stenosis
- Lifestyle changes. Your doctor may recommend that you make some lifestyle changes to help manage your condition or prevent it from worsening. Recommended lifestyle changes may include:
- exercising regularly
- eating a balanced diet
- maintaining a healthy weight
If your calf pain isn’t too severe, there are self-care measures you can try at home to manage the pain. Some options you can try include:
Some options you can try include:
- Rest. If you’ve injured your calf, try to rest it for a couple of days. Avoid long periods of not moving it at all, as this can reduce blood flow to the muscles and prolong healing.
- Cold. Consider applying a cold compress to calf muscles that are sore or tender.
- Over-the-counter (OTC) medications. Medications like ibuprofen (Motrin, Advil) and acetaminophen (Tylenol) may help with pain and swelling.
- Compression. In cases of a calf injury, wrapping your calf with a soft bandage may help. Using compression stockings can also work to promote blood flow in CVI.
- Elevation. Elevating an injured calf above the level of your hips can ease pain and swelling. Leg elevation may also help relieve symptoms of CVI.
Sometimes, you may experience calf pain that happens when you’re walking. Many times, this pain eases or goes away completely when you rest.
There are several common causes for this type of pain, such as muscle cramps, bruises, or strains.
However, calf pain when walking can be also caused by underlying conditions that affect your blood vessels or nerves. Examples of these conditions include peripheral artery disease (PAD), chronic venous insufficiency (CVI), and lumbar spinal stenosis.
You may be able to ease mild calf pain at home by resting, applying ice, and using OTC medications. See your doctor if your pain doesn’t improve with at-home care, gets worse, or affects your daily activities.
Muscle cramps - treatment, symptoms, causes, diagnosis
- Muscle cramps are involuntary and intense muscle contractions without a period of relaxation.
- Almost everyone has experienced a seizure episode at least once in their life.
- There are different types of seizures and different causes.
- Many different medications can cause muscle cramps.
- In most cases, muscle cramps can be stopped by relaxing (stretching) the muscle.

- Muscle cramps can often be prevented by measures such as good nutrition with sufficient micronutrients and adequate fluid intake.
Muscle cramps is an involuntary and violent contraction of a muscle without a period of relaxation. When muscles that can be controlled voluntarily, such as the muscles of the arms or legs, are used, they alternately contract and relax as certain movements are made in the limbs. The muscles that support the head, neck and torso work in synchrony and maintain the position of the body. A muscle (or even a few muscle fibers) can be involuntarily in a state of spasm. If the spasm is strong and persistent, then this leads to the appearance of convulsions. Muscle cramps are often visualized or palpated in the region of the muscle involved.
Muscle cramps can last from a few seconds to a quarter of an hour, and sometimes longer. It is also not uncommon for the seizures to recur until the muscle relaxes. The spasmodic contractions may involve part of a muscle, the entire muscle, or several muscles that usually contract at the same time when performing movements, such as flexing several fingers. In some cases, cramps can be simultaneously in the antagonist muscles responsible for movements in opposite directions. Muscle cramps are widespread. Almost all people (according to some studies about 95% of people) have experienced seizures at some point in their lives. Muscle cramps are common in adults and become more common with age, but cramps can still occur in children. In any muscle (skeletal) in which voluntary movements are performed, there may be cramps. Cramps of the limbs, legs and feet, and especially the calf muscle, are very common.
The spasmodic contractions may involve part of a muscle, the entire muscle, or several muscles that usually contract at the same time when performing movements, such as flexing several fingers. In some cases, cramps can be simultaneously in the antagonist muscles responsible for movements in opposite directions. Muscle cramps are widespread. Almost all people (according to some studies about 95% of people) have experienced seizures at some point in their lives. Muscle cramps are common in adults and become more common with age, but cramps can still occur in children. In any muscle (skeletal) in which voluntary movements are performed, there may be cramps. Cramps of the limbs, legs and feet, and especially the calf muscle, are very common.
Types and causes of muscle cramps
Skeletal muscle cramps can be divided into four main types. These include "true" seizures, tetanic seizures, contractures, and dystonic seizures. Seizures are classified according to the causes of the seizures and the muscle groups they affect.
Types of muscle cramps
True cramps . True cramps involve part or all of a muscle or group of muscles that normally function together, such as the muscles involved in flexing several adjacent fingers. Most researchers agree that true cramps are caused by increased excitability of nerves that stimulate muscle contractions. They are overwhelmingly the most common type of skeletal muscle cramps. True seizures can occur in a variety of circumstances.
Injuries : Persistent muscle spasms may occur as a defense mechanism after an injury such as a broken bone. In this case, as a rule, spasm allows you to minimize movement and stabilize the area of injury. Injury to just the muscle can also lead to muscle spasm.
Vigorous activity: true cramps are usually associated with active muscle loading and muscle fatigue (during sports or unusual activities). Such convulsions can occur both during the activity and after, sometimes many hours later. In addition, muscle fatigue from sitting or lying down for a long period of time in an awkward position or any repetitive movement can also cause cramps. Older people are more at risk of seizures during vigorous or strenuous physical activity.
In addition, muscle fatigue from sitting or lying down for a long period of time in an awkward position or any repetitive movement can also cause cramps. Older people are more at risk of seizures during vigorous or strenuous physical activity.
Rest seizures : Rest seizures are very common, especially in the elderly, but can occur at any age, including childhood. Rest spasms often occur at night. Night cramps, while not life threatening, can be painful, disrupt sleep, and may recur frequently (i.e., many times a night and/or many nights a week). The actual cause of nighttime cramps is unknown. Sometimes these cramps are initiated by a movement that contracts the muscles. An example would be stretching the foot in bed, which shortens the calf muscle, where cramps are most common.
Dehydration : Sports and other strenuous exercise may cause excessive fluid loss through sweat. With this type of dehydration, the likelihood of true seizures increases. These cramps most often occur in warm weather and may be an early sign of heat stroke. Chronic dehydration due to diuretics and poor fluid intake can similarly lead to seizures, especially in the elderly. Seizures can also be associated with a lack of sodium.
Redistribution of fluids in the body: true convulsions can also be noted in conditions where there is an unusual distribution of fluid in the body. An example is cirrhosis of the liver, in which there is an accumulation of fluid in the abdominal cavity (ascites). Similarly, seizures are a relatively common complication of the rapid changes in body fluids that occur during dialysis for kidney failure.
Low levels of electrolytes in the blood (calcium, magnesium): low blood levels of calcium or magnesium directly increase the excitability of the nerve endings innervating the muscles. This may be a predisposing factor for the spontaneous true seizures that many older people experience, and these seizures are also common in pregnant women. Low levels of calcium and magnesium are common in pregnant women, especially if these minerals are not getting enough from the diet. Seizures occur in any circumstance that reduces the availability of calcium or magnesium in body fluids, such as diuretics, hyperventilation, excessive vomiting, lack of calcium and/or magnesium in the diet, insufficient absorption of calcium due to vitamin D deficiency, reduced parathyroid function.
Low levels of calcium and magnesium are common in pregnant women, especially if these minerals are not getting enough from the diet. Seizures occur in any circumstance that reduces the availability of calcium or magnesium in body fluids, such as diuretics, hyperventilation, excessive vomiting, lack of calcium and/or magnesium in the diet, insufficient absorption of calcium due to vitamin D deficiency, reduced parathyroid function.
Low potassium levels: Low blood potassium levels sometimes cause muscle cramps, although muscle weakness is more common in hypokalemia.
Tetany
Tetany activates all nerve cells in the body, which then stimulate muscle contraction. In this type, convulsive contractions occur throughout the body. The name tetany comes from the spasms that occur when tetanus toxin affects the nerves. However, this name for this type of cramp is now widely used to refer to muscle cramps in other conditions, such as low blood levels of calcium and magnesium.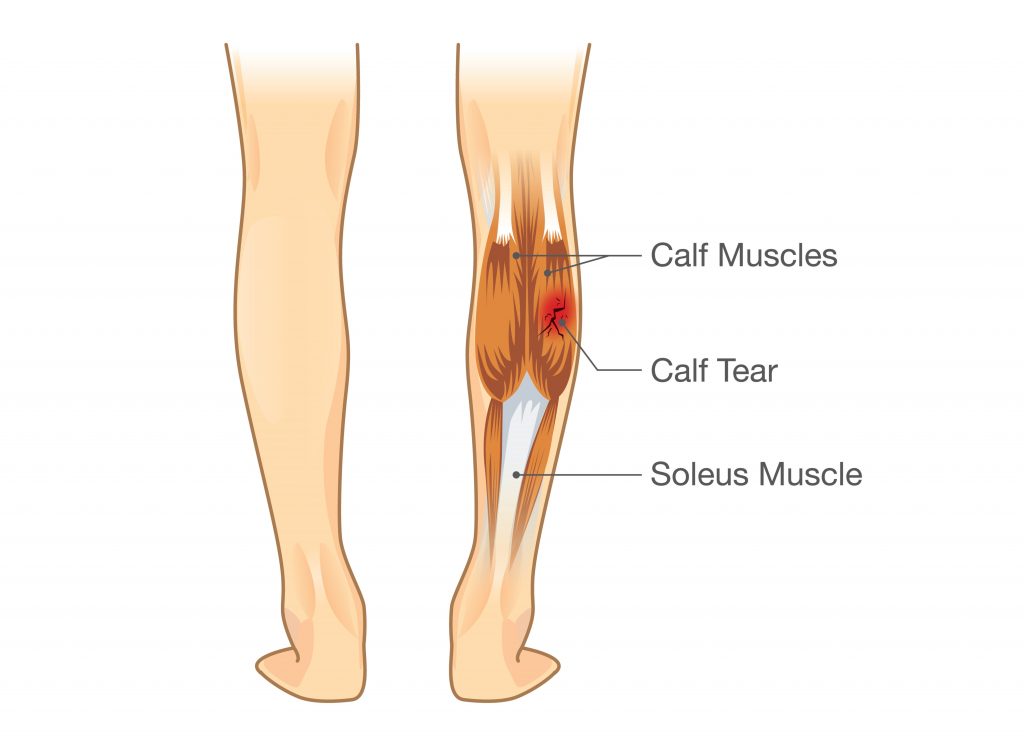 Low levels of calcium and magnesium increase the activity of the nervous tissue non-specifically, which can lead to the appearance of tetanic seizures. Often these seizures are accompanied by signs of hyperactivity of other nerve functions in addition to muscle hyperstimulation. For example, low blood calcium not only causes muscle spasm in the hands and wrists, but it can also cause numbness and tingling sensations around the mouth and other areas of the body.
Low levels of calcium and magnesium increase the activity of the nervous tissue non-specifically, which can lead to the appearance of tetanic seizures. Often these seizures are accompanied by signs of hyperactivity of other nerve functions in addition to muscle hyperstimulation. For example, low blood calcium not only causes muscle spasm in the hands and wrists, but it can also cause numbness and tingling sensations around the mouth and other areas of the body.
Occasionally, tetanic seizures are indistinguishable from true seizures. Additional changes in sensation or other nerve function may not be noticeable, as the pain of a cramp may mask other symptoms.
Contractures
Contractures occur when the muscles cannot relax for an even longer period than in the main types of muscle cramps. Constant spasms are caused by the depletion of adenosine triphosphate (ATP) - the energy intracellular substrate of the cell. This prevents relaxation of the muscle fibers. The nerves are inactive in this type of muscle cramp.
The nerves are inactive in this type of muscle cramp.
Contracture may be the result of genetic inheritance (eg, McArdle disease, which is a defect in the breakdown of glycogen to sugar in muscle cells) or acquired conditions (eg, hyperthyroid myopathy, which is a muscle disease associated with an overactive thyroid gland) . Convulsions of the type of contractures are rare.
Dystonic seizures
The last category of seizures are dystonic seizures, in which muscles not involved in the intended movement are affected and contracted. Muscles that are involved in this type of cramp include antagonistic muscles that usually work in the opposite direction of the intended movement and/or others that enhance the movement. Some dystonic spasms usually affect small muscle groups (eyelids, cheeks, neck, larynx, etc.). The arms and hands may be affected during repetitive movements such as writing (writer's cramp), playing a musical instrument. These activities can also lead to true cramps due to muscle fatigue.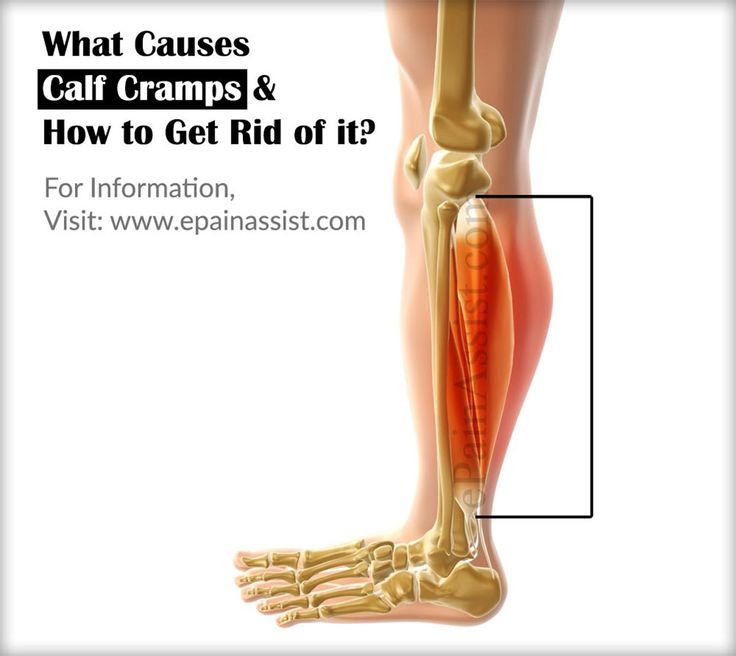 Dystonic seizures are not as common as true seizures.
Dystonic seizures are not as common as true seizures.
Other types of seizures
Some seizures are caused by a number of nerve and muscle disorders. For example, these are diseases such as amyotrophic lateral sclerosis (Lou Gehrig's disease), accompanied by muscle weakness and atrophy; radiculopathy in degenerative diseases of the spine (hernia, disc protrusion, osteophytes), when root compression is accompanied by pain, impaired sensitivity and sometimes convulsions. Seizures can also occur with peripheral nerve damage, such as diabetic neuropathy.
Crumpy . This type of cramps, as a rule, describes cramps in the calf muscle, and associate their appearance with muscle overstrain and the presence of degenerative changes in the spine (osteochondrosis of the lumbar spine, lumbar ischialgia). In addition, cramps are possible with disorders of the vascular circulation in the lower extremities (with obliterating endarteritis or post-thrombophlebitic syndrome). Also, various biochemical disorders in the triceps muscle of the leg can be the cause of cramps.
Also, various biochemical disorders in the triceps muscle of the leg can be the cause of cramps.
Many medicines can cause seizures. Strong diuretics such as furosemide or vigorous fluid removal from the body, even with less potent diuretics, can induce seizures as dehydration and sodium loss occur. At the same time, diuretics often cause loss of potassium, calcium and magnesium, which can also cause seizures.
Medicines such as donepezil (Aricept, which is used to treat Alzheimer's disease) and neostigmine (Prostigmine, used for myasthenia gravis), asraloxifene (Evista) is used to prevent osteoporosis in postmenopausal women - may cause seizures. Tolcapone (Tasmar), which is used to treat Parkinson's disease, has been shown to cause muscle cramps in at least 10% of patients. True seizures have been reported with nifedipine and the drugs Terbutaline (Brethine) and albuterol (Proventil, Ventolin). Some medicines used to lower cholesterol, such as lovastatin (Mevacor), can also cause seizures.
Seizures are sometimes observed in addicts during the cessation of sedatives.
A lack of certain vitamins can also lead directly or indirectly to muscle cramps. These include deficiencies in thiamine (B1), pantothenic acid (B5), and pyridoxine (B6). The exact role of deficiency of these vitamins in causing seizures is unknown.
Poor circulation in the legs leads to a lack of oxygen in the muscle tissue and can cause severe muscle pain (intermittent claudication) that occurs when walking. It usually occurs in the calf muscles. But the pain in vascular disorders in such cases is not caused by the muscle cramp itself. This pain may be more related to the buildup of lactic acid and other chemicals in muscle tissue. Cramps in the calf muscles can also be associated with a violation of the outflow of blood in varicose veins and, as a rule, cramps in the calf muscles occur at night.
Symptoms and diagnosis of muscle cramps
Characteristically, a cramp is often quite painful. As a rule, the patient has to stop activities and urgently take measures to relieve seizures; the person is unable to use the affected muscle during the seizure. Severe cramps may be accompanied by soreness and swelling, which can sometimes persist for up to several days after the cramp has subsided. At the time of the cramp, the affected muscles will bulge, feel hard and tender to the touch.
As a rule, the patient has to stop activities and urgently take measures to relieve seizures; the person is unable to use the affected muscle during the seizure. Severe cramps may be accompanied by soreness and swelling, which can sometimes persist for up to several days after the cramp has subsided. At the time of the cramp, the affected muscles will bulge, feel hard and tender to the touch.
Diagnosis of seizures is usually not difficult, but finding out the causes may require both a thorough medical history and instrumental and laboratory examinations.
Treatment
Most seizures can be interrupted by stretching the muscle. For many leg and foot cramps, this stretch can often be achieved by standing up and walking. With cramps in the calf muscles, it is possible to bend the ankle with the help of the hand, while lying in bed with the leg extended straight. In writing spasm, pressing the hand against the wall with the fingers down will stretch the flexors of the fingers.
A gentle muscle massage can also be performed to relax a spasmodic muscle. If the cramp is associated with fluid loss, as is often the case with strenuous exercise, rehydration and restoration of electrolyte levels is necessary.
Muscle relaxants may be used in the short term in certain situations to allow muscles to relax during injury or other conditions (eg, radiculopathy). These drugs include cyclobenzaprine (Flexeril), orphenadrine (NORFLEX), and baclofen (Lioresal).
In recent years, injections of therapeutic doses of botulinum toxin (Botox) have been successfully used for certain dystonic muscle disorders that are localized in a limited group of muscles. A good response may last several months or more, and injections may be repeated.
Treatment of seizures that are associated with specific diseases, usually focuses on the treatment of the underlying disease.
In cases where seizures are severe, frequent, prolonged, difficult to treat, or not associated with an obvious cause, both additional investigation and more intensive treatment are required.
Prevention of seizures
Adequate nutrition with sufficient fluids and electrolytes is essential to prevent possible seizures, especially during strenuous exercise or during pregnancy.
Night cramps and other rest cramps can often be prevented with regular stretching exercises, especially if done before bed.
Magnesium and calcium supplements are also good for preventing seizures, but caution is required when prescribing them in the presence of renal insufficiency. In the presence of hypovitaminosis, it is necessary to take vitamins of group B, vitamin D, E.
If the patient is taking diuretics, it is necessary to take potassium supplements.
Recently, the only drug that is widely used for the prevention, and sometimes for the treatment of seizures, is quinine. Quinine has been used for many years in the treatment of malaria. The action of quinine is due to a decrease in muscle excitability. However, quinine has a number of serious side effects that limit its use to all groups of patients (nausea, vomiting, headaches, heart rhythm disturbances, hearing impairment, etc. ).
).
Muscle cramps - City Hospital No. 12, Barnaul: articles
Muscle spasms are involuntary muscle contractions that do not have time to relax. When using voluntary muscles, such as the muscles of the arms and legs, when the limbs are forced to move in a fixed way, they alternately contract and relax. Muscles that simultaneously support the head, neck and torso and maintain posture. Muscles (or some muscle fibers) may contract involuntarily. If the spasms are strong and persistent, they lead to seizures. Muscle spasms are often identified by visualization or palpation of the affected part of the muscle.
Muscle spasms last from a few seconds to 25 minutes, sometimes longer. Attacks are often repeated until muscle relaxation occurs. Spasmodic contractions may involve part of a muscle, the entire muscle, or several muscles, usually contracting together during movement, such as flexing several fingers of the hand. In some cases, spasms occur simultaneously in competing muscles responsible for opposing movements. Muscle soreness predominates. Most people (about 95% in some studies) say they have had spasms at some point in their lives. Muscle spasms are a classic symptom in adults and become more frequent as they get older, but can also occur in children. There may be spasms in muscles (skeletal) that move voluntarily. Cramps in the limbs, especially in the calf muscles, are very common.
Muscle soreness predominates. Most people (about 95% in some studies) say they have had spasms at some point in their lives. Muscle spasms are a classic symptom in adults and become more frequent as they get older, but can also occur in children. There may be spasms in muscles (skeletal) that move voluntarily. Cramps in the limbs, especially in the calf muscles, are very common.
Types and causes of muscle cramps
Skeletal muscle spasms can be roughly divided into four types. These include "true" seizures, tetanic seizures, contractions, and dystonic seizures. Spasms are classified according to the cause of the attack and the affected muscle groups.
seizure type
True seizure. True spasm covers part or all of the muscle. Or a group of muscles that usually work together, such as the muscles involved in flexing several adjacent fingers. Many researchers agree that true convulsions are caused by increased excitability of nerves that stimulate muscle contraction. Extremely common in skeletal muscle attacks. A true seizure can occur in many different situations.
Extremely common in skeletal muscle attacks. A true seizure can occur in many different situations.
Some injured. Sustained muscle spasms may occur as a defense mechanism after an injury such as a fracture. In this case, as a rule, spasms allow you to minimize movement and stabilize the injured area. Muscle damage itself can also cause muscle spasms.
I am active. True cramps are usually associated with active muscle tension or muscle fatigue (during sports or unusual movements). Such spasms can occur during activity, after activity, or even hours later. In addition, muscle fatigue caused by prolonged sitting or lying in an unreasonable position or repetitive movements can also cause cramps. Older adults are at increased risk of seizures during vigorous or strenuous exercise.
Destroy the world. Seizures are common during rest, especially in the elderly, but can occur at any age, including children. At rest, seizures often occur at night. At night, there is no difference in life at night, but it can be painful enough to sleep, and this often works out (i. e. several times a night or several times a week). The actual cause of nighttime cramps is unknown. An attack can also occur due to movement towards muscle contraction. For example, stretching the legs in bed will reduce the calf muscles that may develop.
e. several times a night or several times a week). The actual cause of nighttime cramps is unknown. An attack can also occur due to movement towards muscle contraction. For example, stretching the legs in bed will reduce the calf muscles that may develop.
Energy exercises such as Idur sport can lead to excessive loss of body fluids later on. This dehydration increases the chances of having a true seizure. This seizure often occurs when it is hot and may be the initial symptoms of heat stroke. Chronic dehydration due to diuretics and consumption of weak water can also cause seizures, especially in the elderly. In addition, seizures can also occur due to sodium deficiency.
Re-distribution of body fluids: even if there is an abnormality in the distribution of body fluids, true capture can be resolved. For example, water accumulates in abdominal cirrhosis (ascites). Similarly, on dialysis with kidney failure, it is relatively common to have seizures due to rapid changes in bioel.
Blood drops electrolytes (calcium, magnesium): low blood concentrations of calcium and magnesium will directly increase the excitement of the nerve end of the a-o scenes. This may be the underlying cause of the naturally occurring seizures experienced by many older people and is common in pregnant women. Calcium and magnesium are more common in pregnant women, especially when these minerals are not enough to eat. After receiving diuretic hyperventilation, excessive vomiting, lack of calcium and magnesium from food intake, calcium absorption and due to vitamin D deficiency, decreased subthyroid function, convulsions, subject to a decrease in calcium and magnesium in body fluids. You will see.
Potassium value is low. Hypokalemia has weaker muscle strength, but it sometimes causes muscle pain when blood potassium is low.
Tetanus
Aunt activates nerve cells throughout the body, which promotes muscle contraction. This type of convulsions occurs throughout the body. The origin of the car's name comes from the seizure that occurs when tetanus toxin sticks to the nerves. However, the name for this type of seizure is now widely used to refer to seizures in other conditions, such as low blood levels of calcium and magnesium. Low calcium and magnesium will lead to the activity of active nervous tissue, which will lead to tetany seizures. Such cramps are often accompanied by an increase in other nerve functions, in addition to an increase in muscle metabolism. For example, low blood calcium can not only cause cramps in the muscles of the hand and wrist, but also cause numbness around the mouth or tingling.
The origin of the car's name comes from the seizure that occurs when tetanus toxin sticks to the nerves. However, the name for this type of seizure is now widely used to refer to seizures in other conditions, such as low blood levels of calcium and magnesium. Low calcium and magnesium will lead to the activity of active nervous tissue, which will lead to tetany seizures. Such cramps are often accompanied by an increase in other nerve functions, in addition to an increase in muscle metabolism. For example, low blood calcium can not only cause cramps in the muscles of the hand and wrist, but also cause numbness around the mouth or tingling.
Tetanic greens may be indistinguishable from true seizures. Because the pain of seizures hides other symptoms, additional changes in sensation and other nerve functions may not be noticed.
Agreement
The contribution occurs when the muscles cannot be relaxed for a longer time than the main types of cramps. Seizures are caused by depletion of the triple phosphoric acid adenosine (ATP), which is the energy substrate of cells. This prevents the muscle fibers from relaxing. In this type of seizure, the nerves are inactive.
This prevents the muscle fibers from relaxing. In this type of seizure, the nerves are inactive.
Shrinkage is inherited (for example, McArdle's disease, this is a defect in the decomposition of fungal glycogen in muscle cells) or acquired diseases (for example, hypertriodesis. This is due to). Controllers are rare.
Zstonic Spasm
The last category is the dyskeyny spasm, which contracts and contracts muscles that are not involved in the expected movement. The muscles involved in this type of attack include the antagonists, which usually work in the opposite direction to the intended exercise, and other muscles that are reinforced/exercised. Some spasms in dyskeynae usually affect small muscle groups (eyelids, cheeks, throat, larynx, etc.). Arms and hands may be affected by repeated activities such as writing (growing hands) and musical instruments. In addition, these activities can lead to actual cramps and muscle fatigue. Zystonic Kaizen is not as common as true seizures.
Other types of seizures
There are also seizures caused by nerve and muscle disorders. For example, it is a disease that is accompanied by muscle strength and muscle atrophy, such as sclerosis by muscle atrophy (Ludholig's disease). Radiculopathy with degeneration of the spine (hernias, hernias, discs and osteopathy) causes pain, decreased sensation, and sometimes convulsions and due to compression of the spine. In addition, seizures can also occur due to damage to the peripheral nerves, such as diabetic neuropathy.
Crabs This type of cramps, in principle, explains the calf suppressors and is associated with the existence of excessive ACI and a degenerate spine (cubin lumbar spine, lumbar spine spine). Crampi is also possible for disorders of the vascular circulation in the lower extremity (for example, destruction of the intestine or semi-regulatory consequences). In addition, various biochemical disorders can occur in three muscles in the lower extremities.
Many medicines can cause seizures. With the help of basic diuretic drugs such as floasem, or less powerful diuretics, actively removing water from the body can cause dehydration and sodium loss, causing seizures. At the same time, diuretics often lose potassium, calcium, and magnesium, which can also cause seizures.
Drugs such as anti-arsenics, used to treat Alzheimer's disease), neostigmine (prostagmin), used for muscle health, and Aslocksfen (ebisuta), which are used to prevent osteoporosis in postmenopausal women, are caused by the center. possibility. TASMAR, which is used as a treatment for Parkinson's disease, has shown that at least 10% of patients have muscle cramps. True cleansing has been documented with Nifegipin, Brethine, and Albentilin (Proventil, Ventolin). Specific drugs used to lower cholesterol, such as lobastatin (Mebacol), can also cause seizures.
When the sedative effect is cancelled, the addict may have convulsions.
In addition, certain vitamin deficiencies may cause seizure directly or indirectly.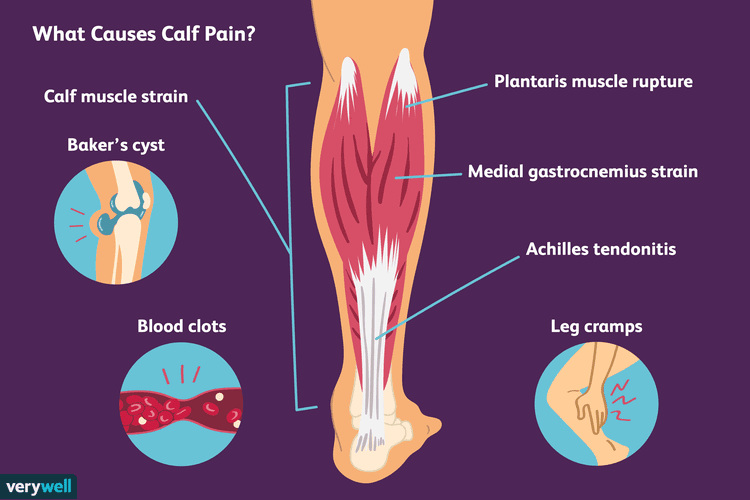 This is a deficiency of chiamine (B1), pantothenic acid (B5) and pyridoxine (B6). The exact role of this vitamin deficiency in causing seizures is unknown.
This is a deficiency of chiamine (B1), pantothenic acid (B5) and pyridoxine (B6). The exact role of this vitamin deficiency in causing seizures is unknown.
Poor circulation in the legs leads to a lack of oxygen in the muscle tissue, causing severe muscle pain (intermittent hunger) that occurs while walking. It usually occurs in the calf muscles. However, the pain of the vascular disorder in such cases is not related to the muscle CRENES itself. This pain appears to be more related to chemicals such as lactic acids accumulated in muscle tissue. Muscle cramps can occur at night, as this is due to poor blood flow in varicose veins.
Symptoms and diagnosis of muscle cramps
Convulsions are typical in that they often cause pain. In principle, urgent measures must be taken to stop activities and relieve convulsions. During seizures, people cannot use the restricted muscles. In the case of severe attacks, it may be painful and swollen, and this may last for several days after the attack has subsided.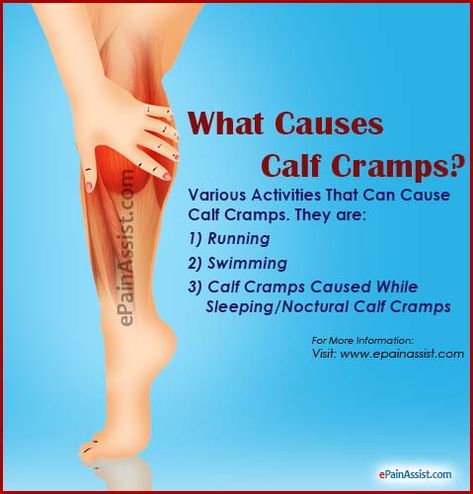 When the cramps, the muscle settings become noticeable, and when the convulsions become stiff and the sensation becomes painful.
When the cramps, the muscle settings become noticeable, and when the convulsions become stiff and the sensation becomes painful.
Diagnosis of seizures is usually not difficult, but to clarify the cause, the method of hearing medical history, equipment test and clinical test is required.
Treatment
Most attacks can be interrupted by stretching the muscles. In the case of many legs, this stretch seems to be possible while standing and walking. In your calf muscles, you can flex your ankle with one hand, sleep in bed, and line your legs up. In spouses, pressing the wall with your fingers down will increase your flexible finger muscles.
In addition, you can relax crampy muscles by properly performing muscle massage. If the seizure is accompanied by loss of body fluid, it is necessary to withdraw the electrolyte level and recover, as is often observed during vigorous exercise.
Muscle relaxants can be used in a specific situation in a specific situation to relax muscles in trauma or other conditions (eg neurosis). These drugs include cyclobenzaprine (Flexellil), Orphenadrine (Nolflex), and Baclofenac.
These drugs include cyclobenzaprine (Flexellil), Orphenadrine (Nolflex), and Baclofenac.
In recent years, Botox toxin treatment dosage has begun to be well used in certain muscle disorders of dyskinesia that are limited to limited muscle groups. Good reactions may last for more than a few months, so you may want to repeat the injections.
The treatment of disease-specific epileptic seizures focuses in principle on the treatment of underlying diseases.
If seizures are severe, frequent, long-term, undertreated, or if they have nothing to do with obvious causes, both additional tests and more intensive treatment are required.
Seizure prevention
To prevent convulsions, high quality meals, including adequate water and electrolytes, are essential, especially during intense exercise or during pregnancy.
Stolis, such as nocturnal convulsions, can often be avoided by regular exercise, especially at bedtime.
In addition, taking a magnesium or calcium formulation is also effective in preventing seizures, but if you have kidney failure, you must be careful with the prescription.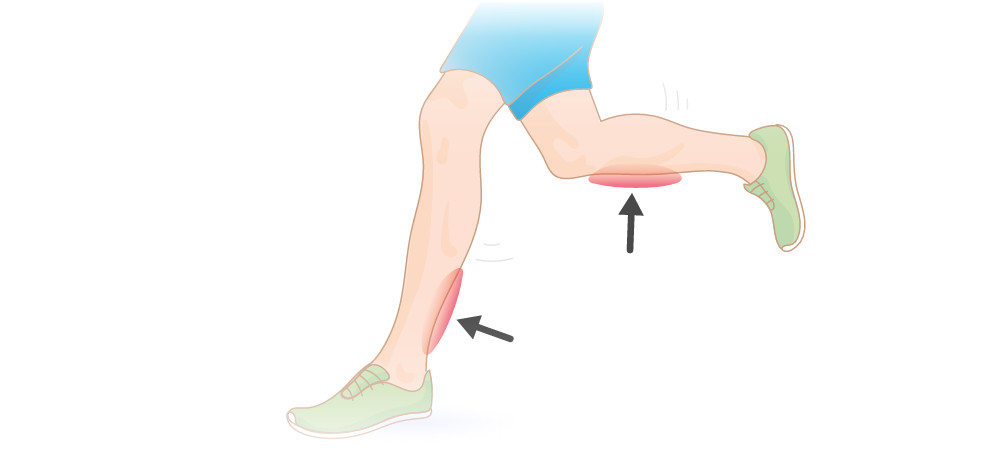 In case of low o-vinilization, vitamin B, vitamin D, etc. must be consumed.
In case of low o-vinilization, vitamin B, vitamin D, etc. must be consumed.
If you are taking diuretics, you must take potassium supplements.
Only Kinin has recently been widely used for the prevention of seizures, and sometimes for treatment. Kinin has been used for many years to treat malaria. The Kinna effect is due to a decrease in muscle excitement. However, Kinin has serious side effects and the purpose of use in all patients is limited (nausea, vomiting, headache, heart rate, hearing, etc.).
When showing active hyperlinks on the permanent page of the article, the use of material is allowed.
Muscle pain is contraction of two muscles on the instep of human legs. It is located on the muscles and is connected to the heel through the Achilles tendon. Therefore, it is natural at the same time as the muscles.
Muscles of the calf are represented by a pair of strong thick heads (outer head and intermediate head) generated from below the pyrifying protrusion. Close around the middle of the lower leg, then move into the common tendon. The muscles of the calf are bolstered by branches extending from the lower leg, and the base is at S1 and S2.
Close around the middle of the lower leg, then move into the common tendon. The muscles of the calf are bolstered by branches extending from the lower leg, and the base is at S1 and S2.
The calf muscles are important muscles for humans that can control leg movements and stabilize the body when walking or running.
When muscles are overworked, muscle spasms occur. Also, if the blood supply system in the artery and vein is abnormal, if the body is deficient, or if the nerve is not working well, muscle spasms will occur.
The strength of the seizures varies. It is weak and barely noticed, but people can hurt and cry. Muscle cramps last from a few seconds to minutes. Conventions can happen to anyone, regardless of gender or age. I often suffer at night. At present, because the body is relaxed, the convulsions are said to be particularly violent.
Seizures never come on their own. There is always some pre-existing precipitating factor, from normal hypothermia to severe neurological and circulatory disturbances. Thus, the body tells people that something is wrong. It is necessary to recognize this signal as soon as possible. Therefore, if convulsions occur frequently, it is necessary to find out the cause and carry out appropriate treatment.
Thus, the body tells people that something is wrong. It is necessary to recognize this signal as soon as possible. Therefore, if convulsions occur frequently, it is necessary to find out the cause and carry out appropriate treatment.
Calf cramps can also be dangerous in their own right. You can easily imagine the horror of losing control of your legs while driving a car, in the deep sea or in the mountains.
Mechanism of development of calf cramp
To understand the mechanism of calf pain, it is necessary to understand its structural characteristics to some extent. Thus, this muscle is represented by many myofibrils. Myofibrils are strips of muscle cells arranged in hundreds of rows. They are called muscle cells (myocytes).
Each muscle cell (myocyte) has a contractile apparatus consisting of many proteins. Typical examples are actin, accessory troponin, myosin, and tropomyosin. Myosin and actin are connected like filaments. Under the influence of ATP, calcium ions, troponin and trophomyosin, they approach each other and muscle contraction occurs.
It is processed in several layers through several stages.
The impulse is generated in the brain and sent along the nerve to the calf muscles.
Acetylcholine transmits electrical signals from the nerves to the surface of the muscles.
Then this impulse spreads throughout the muscle fiber and through the T-shaped channels penetrates into deep structures.
From the channel, the impulse passes to cysteine cells (cells containing calcium ions). Calcium channels open and calcium leaves the cell.
Calcium activates tropin and tropomyosin, bringing together actin and myosin filaments. ATP is involved in this process.
Muscle contraction occurs when myosin and actin filaments approach each other.
Failure anywhere in this complex process can lead to spasms.
Video: A neurologist explains the causes and treatment of seizures during sleep.
Causes of calf cramps
There are five main factors contributing to the development of pain in the calf muscles.
There are five main causes of muscle pain.
Excessive presence of acetylcholine in the synaptic cleft.
Low ATP.
Insufficient excitability of cardiomyocytes.
Defects in contractile proteins that occur at the genetic level.
All of them seem to be difficult conditions for ordinary people to understand, but in fact there are hidden diseases and disorders known to everyone. I must read more carefully.
brain injury
The cerebellum is responsible for maintaining the tone of the calf muscles. Even when we sleep, we continue to send impulses to this part of the brain and other muscles, but not as much as when we are awake.
A disease that can increase the impulses sent from the cerebellum.
Received a traumatic brain injury.
Intracranial bleeding.
Intracerebral thromboembolism.
Eclampsia only affects pregnant women. This condition is dangerous for her life and the life of her child. Eclampsia does not appear immediately, but becomes more noticeable at lightning speed. First, the pregnant woman's blood pressure rises, her legs swell, her general well-being begins to deteriorate. At the same time, it can cause spasms of the calf muscles. In the future, this can affect the uterus, causing placental abruption and serious health problems. Therefore, it can also be said that convulsions in pregnant women are a frightening signal.
Eclampsia does not appear immediately, but becomes more noticeable at lightning speed. First, the pregnant woman's blood pressure rises, her legs swell, her general well-being begins to deteriorate. At the same time, it can cause spasms of the calf muscles. In the future, this can affect the uterus, causing placental abruption and serious health problems. Therefore, it can also be said that convulsions in pregnant women are a frightening signal.
Excess acetylcholine in the synaptic cleft
Acetylcholine is involved in the process of impulse transmission from nerves to muscle cells. When present in large amounts in the synaptic cleft, it causes spasmodic muscle contractions.
Causes of increased acetylcholine
Lack of magnesium in the body. Magnesium is an essential electrolyte that performs many functions in the body. In particular, it controls the opening of channels containing acetylcholine. If you don't have enough magnesium, this channel will close and your calf muscles will contract.
The body lacks magnesium for the following reasons:
Dieting, unreasonable nutrition.
Malabsorption syndrome, intestinal inflammation, bowel resection. All these conditions lead to poor absorption of magnesium by the body.
Excessive dietary intake of calcium and foods high in fat and protein interfere with intestinal absorption of magnesium.
In some situations, the body consumes more magnesium than it receives. This happens during times of stress, during intense sports training, during pregnancy and lactation, during periods of active physical growth, during periods of physical recovery after illness, and so on. Each of these situations contributes to the development of spasms of the calf muscles.
Vomiting, diarrhea and taking laxatives can cause large amounts of magnesium to be excreted from the body. Magnesium deficiency is observed in lovers of coffee and strong tea, alcoholics. In this regard, kidney disease, diabetes, inhalants, and cancer treatment are dangerous.
Magnesium deficiency and leg cramps can often plague people with endocrine disorders such as hyperthyroidism, hyperparathyroidism, and aldosteronism.
Magnesium deficiency has been found to be the most common cause of leg pain in people of all ages. In addition to spasmodic muscle contractions, hearing loss, migraine headaches, skin diseases and hair loss, back and abdominal pain, and stool disorders are of concern.
Magnesium deficiency in childhood is said to cause serious problems such as heart disease, vascular spasms and a weakened immune system.
If left untreated, this condition can cause spasms not only of the calf muscles, but also of the arms, back, occipital muscles, and facial muscles.
Drug overdose In this regard, it is dangerous to take drugs that inhibit the enzyme cholinesterase and destroy acetylcholine. Without cholinesterase, acetylcholine accumulates in the synaptic cleft, causing muscle contraction in the form of spasms. These drugs include Axamon, Alzepil, Ipiglix, Nivarin, Exelon, etc.
Reduced excitability of muscle cells
If it is a stimulus of muscle cells representing muscles. Such disturbances lose the balance of electrolytes in the body and cause vitamins.
The main electrolytes found in the human body are sodium, potassium, calcium and magnesium. Increased momentum, lack of oxygen, weakness, lack of water in the body and due to various diseases, excessive salty food, and if you cannot get drunk, you may be unbalanced under various conditions.
Excess water flow in the body is still dangerous. In addition, the balance between water and electrolytes may be lost and seizures may occur.
Muscle capacity is reduced, affects vitamin deficiency. If vitamin D, E and B are not enough, cramps can occur in the calf muscles.
ATP concentration decreases
As the concentration of ATP, which is the main energy transport of the human body, decreases, calf muscles can cause cramps due to the following diseases and conditions.
Anemia (regardless of cause), heart failure, vascular disorder, lung disease, influenza, adenoid flame, disease elevation. All of these diseases are common in the sense that they cause a state of hypoxia in muscle tissue, that is, seizures.
Hypoglycemia, which develops hypoglycemia, as well as diabetes.
Many people worry about leg cramps at night. This condition cannot be called an independent disease, but it still interferes with human happiness.
The convention is muscle spasm, and in this case the lower extremities. In addition, these convulsions mostly occur at night. You won't last long at night, but you will wake up with short-term information about your calf muscles. When an attack occurs, it can sometimes be severe. The average capture duration is 10 seconds.
Nocturnal attacks on the legs occur, regardless of age, but in many cases, older attractiveness.
It's usually at night when your legs hang and many people worry why they don't get smaller during the day. In fact, the muscles during sleep are small and the air is easy to fill. In this state, lactic acid begins to accumulate in the cells and causes painful cramps. In addition, those with blood vessels have ideal vein leakage and insufficient arterial blood flow. As a result, the tissue of the lower limb causes oxygen deficiency and causes seizures.
In fact, the muscles during sleep are small and the air is easy to fill. In this state, lactic acid begins to accumulate in the cells and causes painful cramps. In addition, those with blood vessels have ideal vein leakage and insufficient arterial blood flow. As a result, the tissue of the lower limb causes oxygen deficiency and causes seizures.
Causes of leg cramps at night
Each of them is a discharged carrier, because the inside of the wall is covered with potassium ions, and the outside is covered with sodium ions. Cells have special pumps to maintain this ionized balance. Cells can be contracted by the charge of ions.
When a neural impulse acts on cells, the charge is weakened by calcium and sodium ions inside, and potassium is released. When cells contain calcium ions, convulsions occur. It is in this state that people consider seizures. To remove cramps, cells send potassium and run a special pump to remove calcium and sodium.
Seizures may be caused by irregular electrolyte balance, nervous breakdown, and abnormalities in the circulatory system. In addition, each reason may be single or compound for the development of conventions. You need to follow more details.
In addition, each reason may be single or compound for the development of conventions. You need to follow more details.
Water / electrolytic imbalance
When the balance between Incellus ions and ions outside the cells is lost, people get cramps.
Break the balance between potassium, calcium, sodium, magnesium and chlorine. The following pathological causes.
Body dehydration. With dehydration, the electrolyte balance is lost, the blood is deeper, the sodium concentration in the blood is reduced, and muscle convulsions are common. In addition, an attack develops even with massive bleeding, where the amount of circulating blood in the body decreases rapidly.
I take diuretics. If you don't follow your doctor's instructions about self-assessment or take a diuretic, you may have a seizure. In particular, it is dangerous not to maintain the dose of diuretics with a loop, such as flosemide, Lasix, Carbanil MUNEA inhibitor (diacarb). These drugs remove sodium and magnesium from the body, causing agitation and muscle spasms and by removing the nerve. This problem is especially important for the elderly. Appeals for muscle cramps and contractions that occur at night. Also, changing your position can cause cramps.
This problem is especially important for the elderly. Appeals for muscle cramps and contractions that occur at night. Also, changing your position can cause cramps.
During pregnancy. While you are pregnant with your child, women have plenty of vitamins and minerals. It is used to grow the fruit. Therefore, pregnant women often have leg cramps at night.
Living defeat. In cirrhosis, the balance between globulin and albumin is lost. As a result, seizures may occur.
Chronic renal failure. Patients who are forced to undergo regular dialysis often have leg cramps. (Read more: chronic renal failure)
Chronic renal failure
If the body tissue becomes oxygen deficient, the body will accumulate metabolites that are not oxidized enough. Hypoxic muscles begin to contract and cause visible pain.
Lower varicose veins. People who suffer from varicose veins often experience leg attacks. At the same time, the load on the legs is wonderful all day, and if you are a well entertained person, your muscles are sore at night. In this regard, the placement of the vein is not only dynamic, but static overflow is dangerous. In addition to leg cramps, the patient is swollen and in the evening feels rigor. The legs are covered with veins and small capillaries that expand and glow in the skin. Frequent urination is a phenomenon often seen by barbershops, teachers, and salespeople who work who constrict their legs at night. Also, it seems that varicose veins often get worse in pregnant women.
In this regard, the placement of the vein is not only dynamic, but static overflow is dangerous. In addition to leg cramps, the patient is swollen and in the evening feels rigor. The legs are covered with veins and small capillaries that expand and glow in the skin. Frequent urination is a phenomenon often seen by barbershops, teachers, and salespeople who work who constrict their legs at night. Also, it seems that varicose veins often get worse in pregnant women.
The capillaries won. Firstly, the small artery suffers from diabetics, smokers and intermittent chromium patients. The tissue of the lower limb is not fed because arterial blood flow is disrupted. In addition to cramps at night, people who worry about leg pain while walking, limb deterioration, and reduced body temperature regulation function.
If flat leg development is abnormal, the load on the muscles and ligaments will be displaced. This is the main cause of cramps in the lower extremities. In flat legs, both blood and nerves hurt at the same time.
Raynow's disease. This disease is characterized by impaired blood flow in the capillaries and hypoxic tissue. As a result, symptoms such as frozen feet, frozen limbs turn blue when exposed to cold, and cramps.
Disease of the nervous system
Sitting in the middle of the night suffers from the following diseases:
High body temperature, which causes heat.
Spasmodic paralysis may cause intense direct convulsions.
Infectious diseases such as meningitis infections.
Poisoning with alcoholic products.
It is slaughtered by poisonous insects and poisonous snakes.
Sea urchin and wounds
Excessive intake of vitamin D
Other causes
Diseases such as subcorn hydraulic symptoms seem to be agreements of the legs. However, when the inferior thyroid gland has a disorder and its function is reduced, it looks like musical music.
In this case, the cramps begin to affect the face and hands. Characteristic symptoms also appear due to hormones in the body, such as hair removal, weakness and fatigue.
Characteristic symptoms also appear due to hormones in the body, such as hair removal, weakness and fatigue.
Taking contraceptives can cause women's legs.
Magnesium deficiency, calcium deficiency and vitamin B deficiency can lead to legs. Lack of magnesium can cause symptoms such as insomnia, fatigue, and frustration.
If calcium is not enough, the condition of the hair and nails will deteriorate.
If vitamin B is not enough, you will feel numbness in the fingers, weakness of the whole body and loss of effectiveness in addition to cramps.
Alcohol addiction is one of the causes of legs in the middle of the night. If alcoholic beverages are always taken for a long time, vitamin B leaks out of the body and affects the condition of the muscles.
Prolonged stress can cause legs.
How do you feel about the legs you see in the video, Dr. Evdokimenko?
Why do seizures occur in healthy people?
Hanging in the middle of the night can happen to a perfectly healthy person. In many cases, this is caused by excessive muscle tension. Occupation, people spend a lot of time in one place. In the evening, when the muscles are weakened, they begin to cause cramps.
In many cases, this is caused by excessive muscle tension. Occupation, people spend a lot of time in one place. In the evening, when the muscles are weakened, they begin to cause cramps.
For example, circus members and a ballerina often have more feet than others. The same applies to professional athletes, track and field athletes, skiers and ice skaters. Thus, depending on the characteristics of the professional activity, you can put your feet up in the middle of the night, even if you are not sick.
Muscles in the lower extremities may twitch at night, causing vegetarianism. This trend is especially noticeable, especially when the food is extremely limited in protein, or when foods containing calcium or magnesium are limited.
Although unsurprisingly well known, those who enjoy green tea may have epileptic seizures in their legs. If you continue to drink in large quantities for many years, this will lead to an elite withdrawal of beneficial trace elements in the body. In fact, this drink has a diuretic effect, and many do not doubt it.
In fact, this drink has a diuretic effect, and many do not doubt it.
How to treat leg cramps at night?
Feet in feet never happen on their own. To prevent the onset, it is necessary to influence the causes of convulsive attacks.
The facts are as follows.
To prevent dehydration, you need to drink enough water. This is very important for the muscles to work properly. This rule is especially important for those involved in active sports, not only in the hot season. It's a good idea to prioritize mineral water, which contains abundant trace elements.
To lose moisture during vomiting or diarrhea, you need to drink enough water. If the situation has not improved after a few hours, consult your healthcare provider.
Thus, seizures do not lead to medication, which should clearly be in accordance with the recommendations of doctors. However, if the muscle pain continues to be increased, treatment should be considered.
To prevent leg pain during pregnancy, you need to take vitamins and minerals.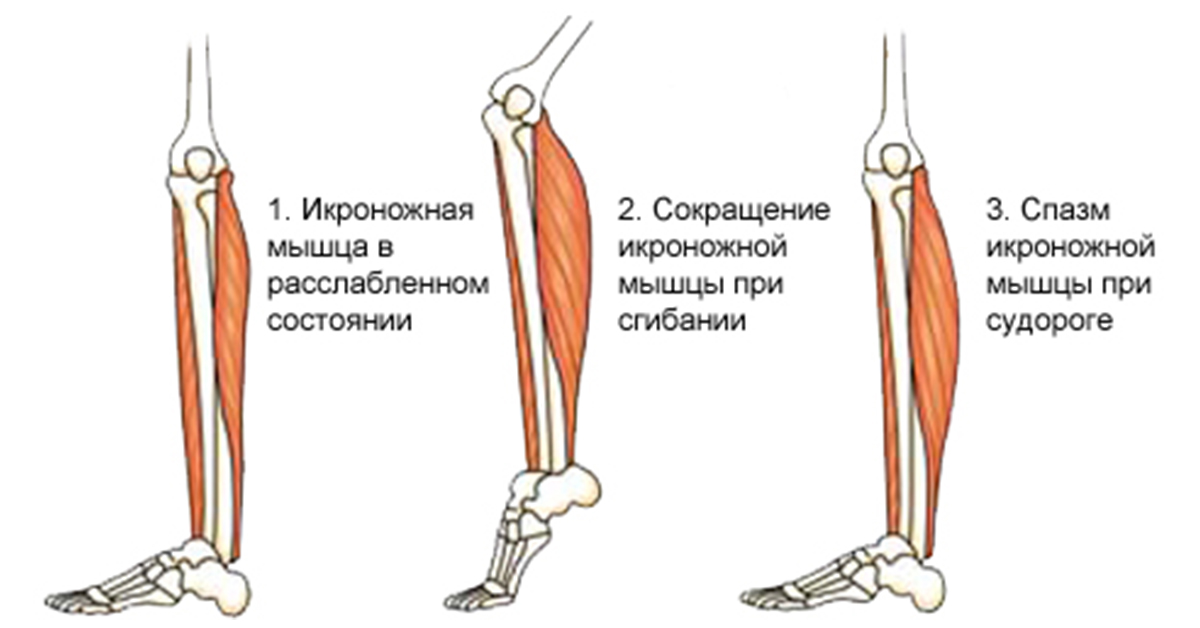
Patients with cirrhosis should receive adequate treatment, take liver protection, advocate dietary therapy, and abstain from alcohol. When fluid accumulates in the abdomen, it is necessary to suck with a pump.
If the veins of the lower varicose veins of varicose use are the causes of seizures, you must diet to lose weight. Be sure to quit smoking. When varicose veins begin to form, the use of compression sheets is effective. When you begin to relate to the venots, you will not be bothered by cramps. Surgery is required if conservative treatment fails to resolve existing problems.
Patients with diabetes should make every effort to control their blood sugar levels. This suppresses the progress of the disease and does not develop serious complications. In the early stages of diabetes, it is recommended to adjust the menu, maintain strict dietary restrictions, and increase your exercise. If this still has no effect, supplement treatment with carbohydrate, restricted or insulin injections.
To eliminate endometritis and relieve blood vessels, a dosing agent is needed, which causes the legs of the legs. He says he takes vitamins and anticoagulants. If there is an ulcer, it is necessary to repair the veins and improve the function of the blood vessels.
If your feet are caused by flat feet, you need to start treatment as soon as possible. Conservative therapy is valid only at the initial stage of onset. Installations should reduce weight loss, dietary restrictions and burden on the legs. If the condition progresses late, you will have surgery.
Vitamin D must be strictly given in the amount prescribed by the physician.
It is necessary to warm the extremities in order not to cause the legs of the legs at night with Raynow's syndrome. At the same time, the treatment of the underlying diseases that cause the development of Raynow's syndrome will also be performed. Physical therapy, reflexology, high pressure oxygen therapy, etc. are often demonstrated.
Regular consultations with endocrine scientists are required to prevent hyperthyroidism seizures. Menus such as vegetables, fruits and milk drinks are required. Calcium and magnesium are abundant, but lack of phosphorus. At the same time, calcium preparations and vitamin D preparations containing ammonium chloride are also prescribed.
If you are subject to thermal agreements, you need to administer an anti-ifritic in time to prevent a high body temperature.
If you have convulsions due to a magnesium deficiency, be sure to take it with vitamin B6. As a rule, the total amount is about 8 weeks. After that, cramps will not be a concern. At the same time, you need to eat foods rich in magnesium: parsley, onion, dill, dry apricot, prunes, bran, beans, beans, seaweed, etc.
Maintaining a healthy lifestyle and avoiding smoking and drinking is a great prevention method for your feet.
[Video] Dr. Berg's seizures.
How to quickly get rid of cramps after waking up?
There are simple tips to quickly stop the legs and restore sensation.
Stretching the lower legs and feet can relieve the cramps that caused the awakening. To do this, get out of bed and walk around with your toes for a bit.
If you do not want to get out of bed, you can simply stretch your legs while lying down.
You can also gently massage your feet on the bed or knead.
If it is possible to enter the refrigerator, cut a slice of a lemon and apply lemon juice to the pig. Results will be received within 30 seconds.
It is a good idea to apply a thermal ointment to the skin of the lower limb or rub it in with alcohol.
Just by moving your feet, your brain can get a signal that "the body is unusual."
By following these recommendations, you can not only stop cramps, but also prevent recurrence.
[Video] Super way to eliminate leg cramps, the fastest proven.
Cramps Prevention Exercises
To keep your legs from hanging in the middle of the night, you should do the following exercise before bed.
Place your heel and hold for 20 seconds.
Spread the heel to the side and match the toes. 20 seconds in this state.
Pull your heels together to spread your socks in the other direction. Please wait about 20 minutes in this pose.
Sit in a chair, bend over quickly and bend your toes.
Get up and go outside and at your feet.
Sit in a chair and write the numbers from 1 to 10 with your feet in the air.
Sit on the floor with your knees bent and your toes pointed towards you. You should be able to feel your calf muscles grow as you exercise. You have to walk three times for 10 seconds each.
Be a finger, stretch out your arms and drop your heels. Exercise for 10 seconds 5 times.
Stand up and tilt your trunk forward, touching your toes but keeping your heels on the floor. Repeat the 10-second exercise six times.
Simple tips to prevent leg cramps
Preventive measures to prevent beriberi.
Drinking clean water should be a habit for people.
Avoid alcohol and caffeine.
It is recommended to stretch the muscles of the legs before going to bed.
Choose a spacious width so you don't interfere with normal blood flow.
You have to eat it right. Food should not only eat vegetables, but also the animal. The balance of both should be well balanced.
Choose shoes that are as comfortable and physiologically correct as possible.
Do not sit or stand in one place for a long time. The person is moving. So you need a break for any work. It is recommended to raise your legs on your back and raise your legs on the slope whenever you have the opportunity. In this position, you need to spend at least 5 minutes.
It is recommended to have a contrasting woman with legs before going to bed. You can add sea salt or herbal tea.
These precautions are only suitable for perfectly healthy people. If your legs are caused by diseases such as veins, you need to consult a doctor and get the appropriate treatment.












