Can early pregnancy cause acid reflux
Indigestion and heartburn in pregnancy
Indigestion, also called heartburn or acid reflux, is common in pregnancy. It can be caused by hormonal changes and the growing baby pressing against your stomach.
You can help ease indigestion and heartburn by making changes to your diet and lifestyle, and there are medicines that are safe to take in pregnancy.
Symptoms of indigestion and heartburn
Symptoms of indigestion and heartburn include:
- a burning sensation or pain in the chest
- feeling full, heavy or bloated
- burping or belching
- feeling or being sick
- bringing up food
Symptoms usually come on soon after eating or drinking, but there can sometimes be a delay between eating and developing indigestion.
You can get symptoms at any point during your pregnancy, but they are more common from 27 weeks onwards.
Things you can do to help with indigestion and heartburn
Changes to your diet and lifestyle may be enough to control your symptoms, particularly if they are mild.
Eat healthily
You're more likely to get indigestion if you're very full.
If you're pregnant, it may be tempting to eat more than you would normally, but this may not be good for you or your baby.
Find out more about a healthy diet in pregnancy and foods to avoid.
Change your eating and drinking habits
You may be able to control your indigestion with changes to your eating habits.
It can help to eat small meals often, rather than larger meals 3 times a day, and to not eat within 3 hours of going to bed at night.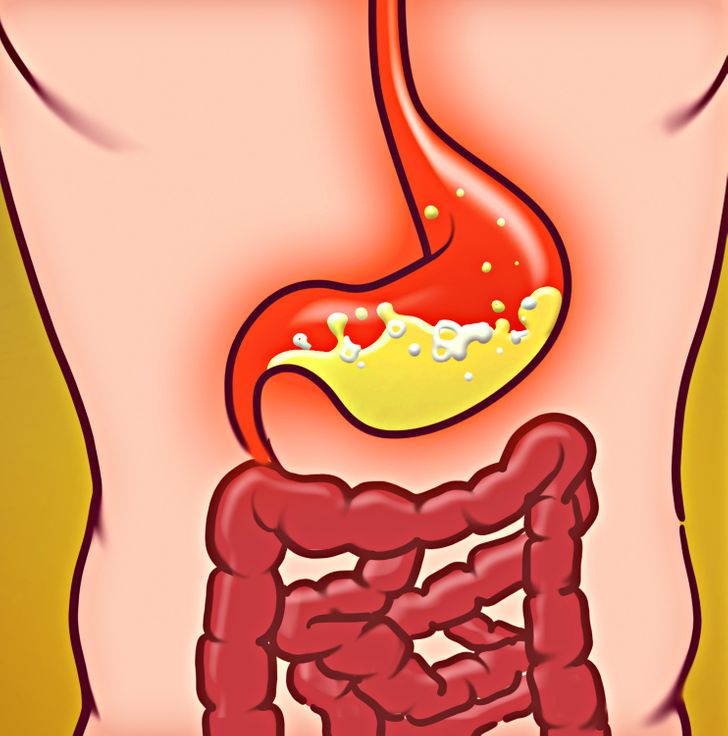
Cutting down on drinks containing caffeine, and foods that are rich, spicy or fatty, can also ease symptoms.
Keep upright
Sit up straight when you eat. This will take the pressure off your stomach. Propping your head and shoulders up when you go to bed can stop stomach acid coming up while you sleep.
Stop smoking
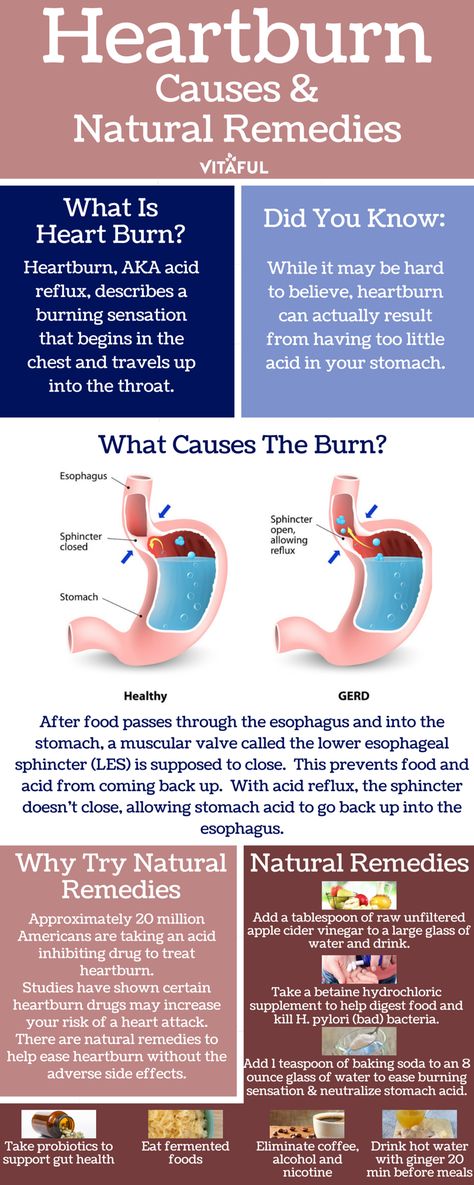
Smoking when pregnant can cause indigestion, and can seriously affect the health of you and your unborn baby.
When you smoke, the chemicals you inhale can contribute to your indigestion. These chemicals can cause the ring of muscle at the lower end of your gullet to relax, which allows stomach acid to come back up more easily. This is known as acid reflux.
Smoking also increases the risk of:
- your baby being born prematurely (before week 37 of your pregnancy)
- your baby being born with a low birthweight
- sudden infant death syndrome (SIDS), or "cot death"
There's lots of help available to stop smoking. Talk to your midwife or call the NHS Smokefree helpline on 0300 123 1044. Find out more about stopping smoking in pregnancy.
Talk to your midwife or call the NHS Smokefree helpline on 0300 123 1044. Find out more about stopping smoking in pregnancy.
Avoid alcohol
Drinking alcohol can cause indigestion. During pregnancy, it can also lead to long-term harm to the baby. It's safest to not drink alcohol at all in pregnancy.
Find out more about alcohol and pregnancy
When to get medical help
See your midwife or GP if you need help managing your symptoms or if changes to your diet and lifestyle do not work. They may recommend medicine to ease your symptoms.
You should also see your midwife or GP if you have any of the following:
- difficulty eating or keeping food down
- weight loss
- stomach pains
Your midwife or GP may ask about your symptoms and examine you by pressing gently on different areas of your chest and stomach to see whether it's painful.
If you're taking prescription medicines
Speak to your GP if you're taking medicine for another condition, such as antidepressants, and you think it may be making your indigestion worse. They may be able to prescribe an alternative medicine.
Never stop taking a prescribed medicine unless you're advised to do so by your GP or another qualified healthcare professional who's responsible for your care.
Medicines for indigestion and heartburn
Medicines for indigestion and heartburn during pregnancy include:
- antacids – to neutralise the acid in your stomach (some are available over the counter from a pharmacist)
- alginates – to relieve indigestion caused by acid reflux by stopping the acid in your stomach coming back up your gullet
You may only need to take antacids and alginates when you start getting symptoms. However, your GP may recommend taking them before symptoms come on – for example, before a meal or before bed.
However, your GP may recommend taking them before symptoms come on – for example, before a meal or before bed.
If you're taking iron supplements as well as antacids, do not take them at the same time. Antacids can stop iron from being absorbed by your body.
If antacids and alginates do not improve your symptoms, your GP may prescribe a medicine to reduce the amount of acid in your stomach. 2 that are widely used in pregnancy and not known to be harmful to an unborn baby are:
- ranitidine – a tablet you take twice a day
- omeprazole – a tablet you take once a day
Causes of indigestion in pregnancy
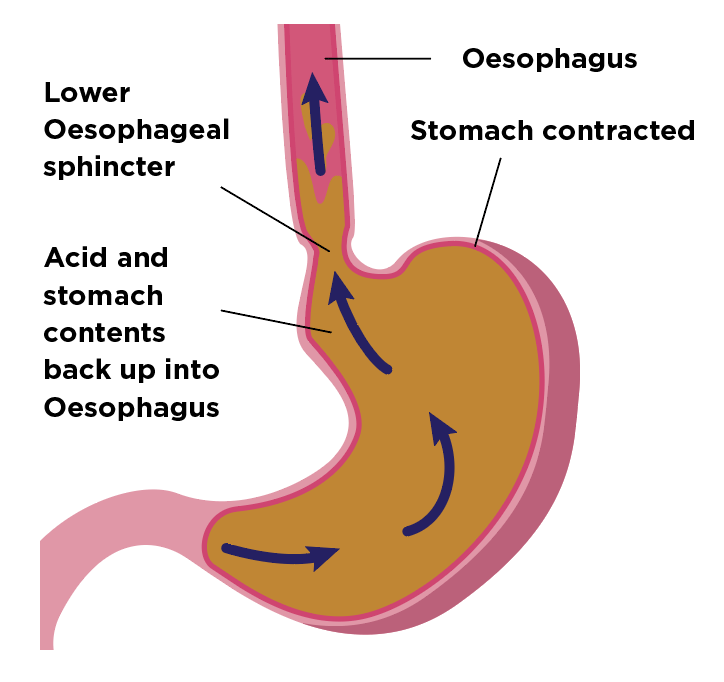
Symptoms of indigestion come when the acid in your stomach irritates your stomach lining or your gullet. This causes pain and a burning feeling.
When you're pregnant, you're more likely to have indigestion because of:
- hormonal changes
- the growing baby pressing on your stomach
- the muscles between your stomach and gullet relaxing, allowing stomach acid to come back up
You may be more likely to get indigestion in pregnancy if:
- you had indigestion before you were pregnant
- you've been pregnant before
- you're in the later stages of pregnancy
Video: Eating well on a budget
In this video, a dietitian gives advice on how to eat healthily on a budget.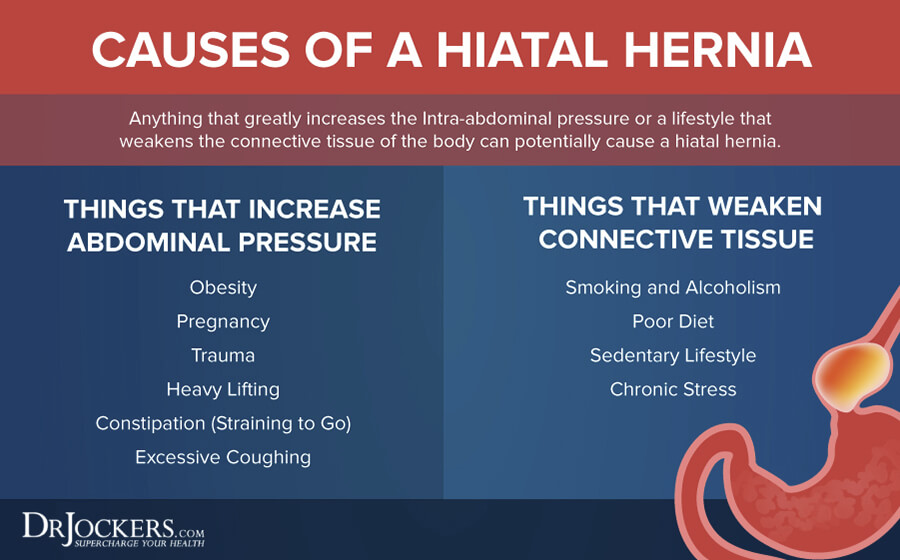
Media last reviewed: 13 January 2021
Media review due: 13 January 2024
Heartburn, Acid Reflux, and GERD During Pregnancy
It’s called heartburn, although that burning feeling in your chest has nothing to do with the heart. Uncomfortable and frustrating, it bothers many women, particularly during pregnancy.
The first question you may have is how to make it stop. You may also wonder if treatments are safe for your baby. Learn what causes heartburn during pregnancy and what you can do about it.
During normal digestion, food travels down the esophagus (the tube between your mouth and stomach), through a muscular valve called the lower esophageal sphincter (LES), and into the stomach.
The LES is part of the doorway between your esophagus and your stomach. It opens to allow food through and closes to stop stomach acids from coming back up.
When you have heartburn, or acid reflux, the LES relaxes enough to allow stomach acid to rise up into the esophagus. This can cause pain and burning in the chest area.
This can cause pain and burning in the chest area.
During pregnancy, hormone changes can allow the muscles in the esophagus, including the LES, to relax more frequently. The result is that more acids may seep back up, particularly when you’re lying down or after you’ve eaten a large meal.
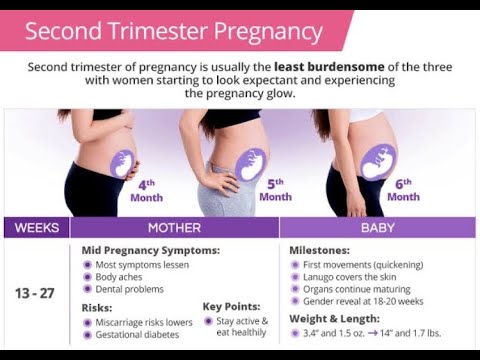
In addition, as your fetus grows during the second and third trimesters and your uterus expands to accommodate that growth, your stomach is under more pressure. This can also result in food and acid being pushed back up into your esophagus.
Heartburn is a common occurrence for most people at one time or another, but it doesn’t necessarily mean you’re pregnant. However, if you also experience other symptoms, such as a missed period or nausea, these could be signs that you need to take a pregnancy test.
Pregnancy increases your risk of heartburn or acid reflux. During the first trimester, muscles in your esophagus push food more slowly into the stomach and your stomach takes longer to empty.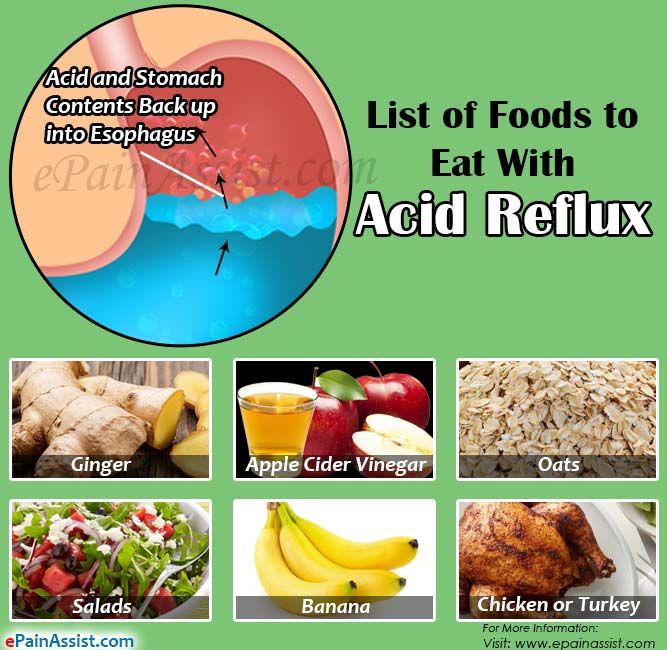
This gives your body more time to absorb nutrients for the fetus, but it can also result in heartburn.
During the third trimester, the growth of your baby can push your stomach out of its normal position, which can lead to heartburn.
However, each woman is different. Being pregnant doesn’t necessarily mean you’ll have heartburn. It depends on many factors, including your physiology, diet, daily habits, and your pregnancy.
Relieving heartburn during pregnancy typically involves some trial and error. Lifestyle habits that can reduce heartburn are often the safest methods for mother and baby. The following tips may help relieve your heartburn:
- Eat smaller meals more frequently and avoid drinking while eating. Drink water in between meals instead.
- Eat slowly and chew every bite thoroughly.
- Avoid eating a few hours before bed.
- Avoid foods and beverages that trigger your heartburn. Typical culprits include chocolate, fatty foods, spicy foods, acidic foods like citrus fruits and tomato-based items, carbonated beverages, and caffeine.
- Stay upright for at least one hour after a meal. A leisurely walk may also encourage digestion.
- Wear comfortable rather than tight-fitting clothing.
- Maintain a healthy weight.
- Use pillows or wedges to elevate your upper body while sleeping.
- Sleep on your left side. Lying on your right side will position your stomach higher than your esophagus, which may lead to heartburn.
- Chew a piece of sugarless gum after meals. The increased saliva may neutralize any acid coming back up into the esophagus.
- Eat yogurt or drink a glass of milk to quell symptoms once they start.
Alternative medicine options include acupuncture and relaxation techniques, such as progressive muscle relaxation, yoga, or guided imagery. Always check with your doctor before trying new treatments.
Over-the-counter antacids such as Tums, Rolaids, and Maalox may help you cope with occasional heartburn symptoms. Those made of calcium carbonate or magnesium are good options.
However, it may be best to avoid magnesium during the last trimester of pregnancy. Magnesium could interfere with contractions during labor.
Most doctors recommend avoiding antacids that contain high levels of sodium. These antacids can lead to a buildup of fluid in the tissues.
You should also avoid any antacids that list aluminum on the label, as in “aluminum hydroxide” or “aluminum carbonate”. These antacids can lead to constipation.
Finally, stay away from medications like Alka-Seltzer that may contain aspirin.
Ask your doctor for the best option. If you find yourself downing bottles of antacids, your heartburn may have progressed to gastroesophageal acid reflux disease (GERD). In that case, you may need a stronger treatment.
If you have heartburn that often wakes you up at night, returns as soon as your antacid wears off, or creates other symptoms (such as difficulty swallowing, coughing, weight loss, or black stools), you may have a more serious problem that requires attention.
Your doctor may diagnose you with GERD. This means that your heartburn needs to be controlled to protect you from complications such as damage to the esophagus.
Your doctor may prescribe certain acid-reducing medications to reduce your symptoms. Research indicates that medications called h3 blockers, which help block the production of acid, appear to be safe.
Another type of medication, called proton pump inhibitors, is used for people with heartburn that doesn’t respond to other treatments.
If you’re concerned about the effects of medications, be sure to talk to your doctor. Doctors can help you control your symptoms while keeping your unborn child safe.
Acid related diseases in pregnancy | Rassvet Clinic
Heartburn during pregnancy is a very common complaint. It is known that up to 80% of pregnant women experience symptoms characteristic of gastroesophageal reflux disease (GERD) (heartburn, dysphagia, belching, and others), and the frequency of heartburn in the first trimester is 7.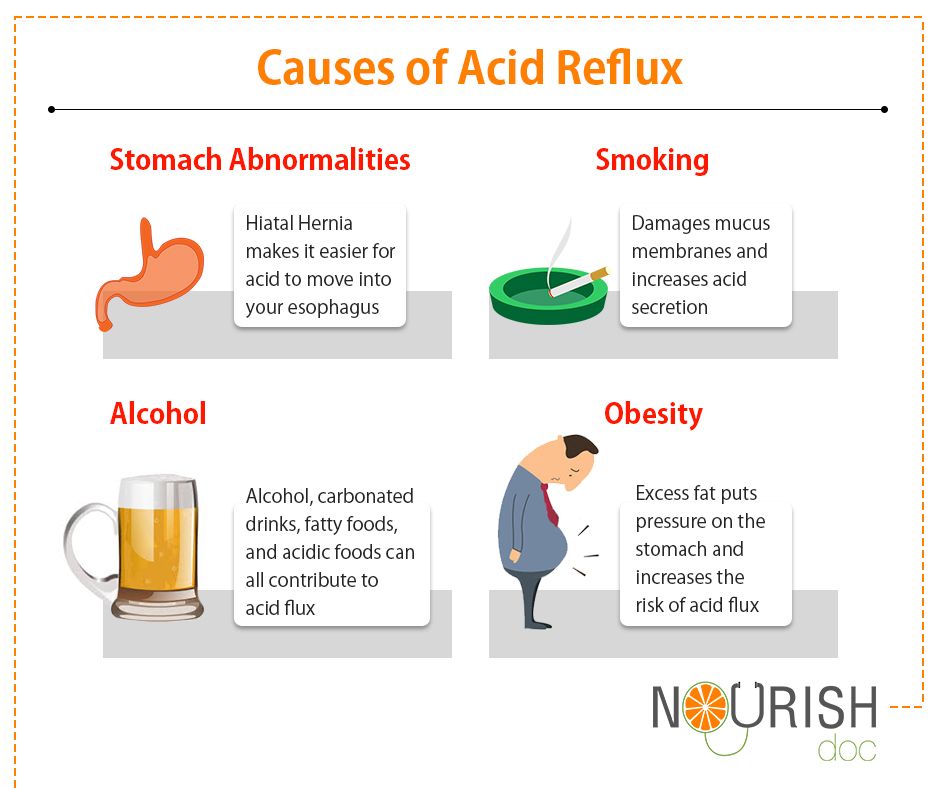 2%, in the second - 18.2%, in the third - 40%.
2%, in the second - 18.2%, in the third - 40%.
The main factors behind this high prevalence of GERD in pregnancy include hormonal changes such as hyperprogesteronemia (increased levels of the hormone progesterone) and hyperestrogenemia (increased levels of estrogen hormones), as well as increased intra-abdominal pressure due to uterine and fetal growth.
The action of gestational hormones in the first trimester of pregnancy is due to the fact that they, without affecting the basal tone of the lower esophageal sphincter (LES), reduce the increase in pressure of this sphincter in response to a variety of physiological stimuli, including food intake. In the second and third trimesters of pregnancy, progesterone and estrogen reduce the basal tone of the LES to 50% of the initial level, the maximum decrease occurs at 36 weeks of gestation. After a successful delivery, the tone of the LES in women who did not suffer from GERD before pregnancy, as a rule, returns to normal - in connection with this, this condition is called "pregnancy heartburn.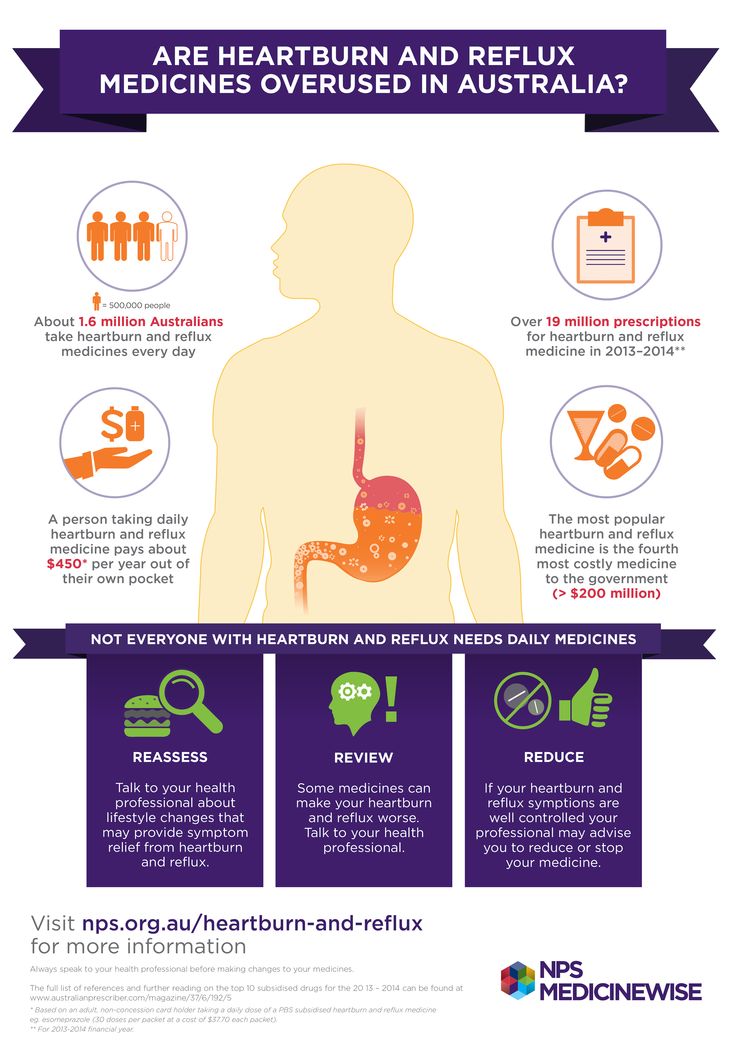 "
"
Pregnancy heartburn usually does not lead to the development of esophagitis, complications of GERD (strictures, ulcers, bleeding) and does not require serious medical treatment.
If a woman had GERD before pregnancy, the complaints may worsen during pregnancy and require examination and medication.
The diagnosis of GERD during pregnancy is established primarily on the basis of complaints, anamnesis data and objective examination. X-ray examination in pregnant women - due to possible damaging effects on the fetus - is not used, pH-metry and manometry can be used, but the need for its use is doubtful.
Esophagogastroduodenoscopy (EGD) is the method of choice for diagnosing GERD in pregnant women, but it should only be used for strict indications, such as a history of complications of GERD and the ineffectiveness of ongoing drug therapy.
Treatment of GERD in pregnant women should be based on changes in lifestyle and nutrition: exclusion of a horizontal position of the body immediately after meals, sleeping with the head end of the bed elevated (by 15 cm), exclusion of physical activity that increases intra-abdominal pressure (including wearing corsets, tight belts, bandages).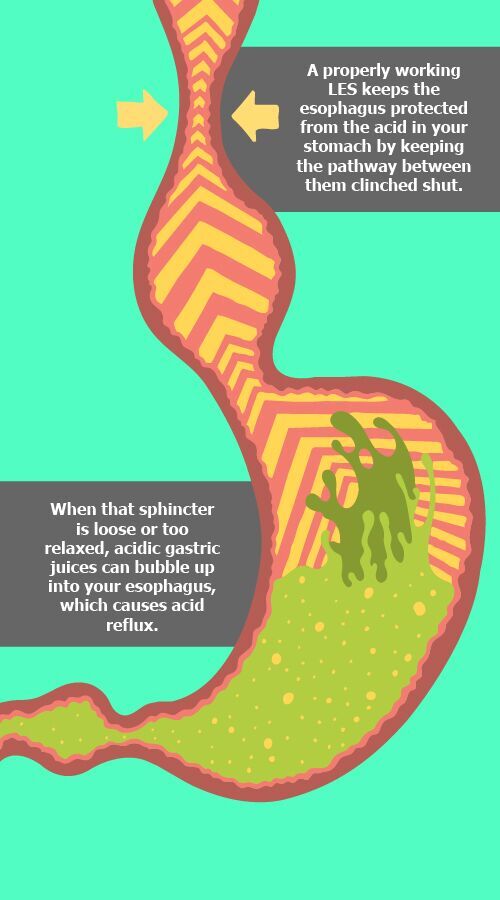 The last meal should take place no later than 3 hours before bedtime, you need to eat in small portions, pay special attention to the normalization of the stool.
The last meal should take place no later than 3 hours before bedtime, you need to eat in small portions, pay special attention to the normalization of the stool.
First-line drugs for the treatment of GERD in pregnant women include antacids and alginates. With the ineffectiveness of these drugs, it is permissible to prescribe prokinetics (metoclopramide), blockers of histamine h3 receptors and (according to strict indications) proton pump inhibitors (PPIs).
H2-histamine blockers are the most commonly prescribed group of drugs for pregnant women. They are classified as risk category B by the US Food and Drug Administration (FDA) ( "drugs taken by a limited number of pregnant women without evidence of their effect on the incidence of congenital anomalies or damaging effects on the fetus") . In Russian instructions, only cimetidine and ranitidine are allowed with a caveat: use during pregnancy is possible only if the expected effect of therapy outweighs the potential risk to the fetus. Famotidine and nizatidine in the Russian Federation are contraindicated for pregnant women.
Famotidine and nizatidine in the Russian Federation are contraindicated for pregnant women.
Although most PPIs are also classified by the FDA as risk category B, in Russia there are more stringent restrictions on the use of this group of drugs in pregnant women. So, lansoprazole is contraindicated in the first trimester, in the second and third trimesters it can be used only if the expected benefit of therapy outweighs the potential risk to the fetus. The use of pantoprazole and esomeprazole is possible only under strict indications, when the benefit to the mother outweighs the potential risk to the fetus. Rabeprazole during pregnancy is contraindicated.
Pregnancy has a beneficial effect on the course of peptic ulcer disease: 75-80% of women experience remission of the disease, and it does not have a noticeable effect on its outcome. However, some patients may experience an exacerbation. This is most often observed in the first trimester of pregnancy (14.8%) and the third trimester (10.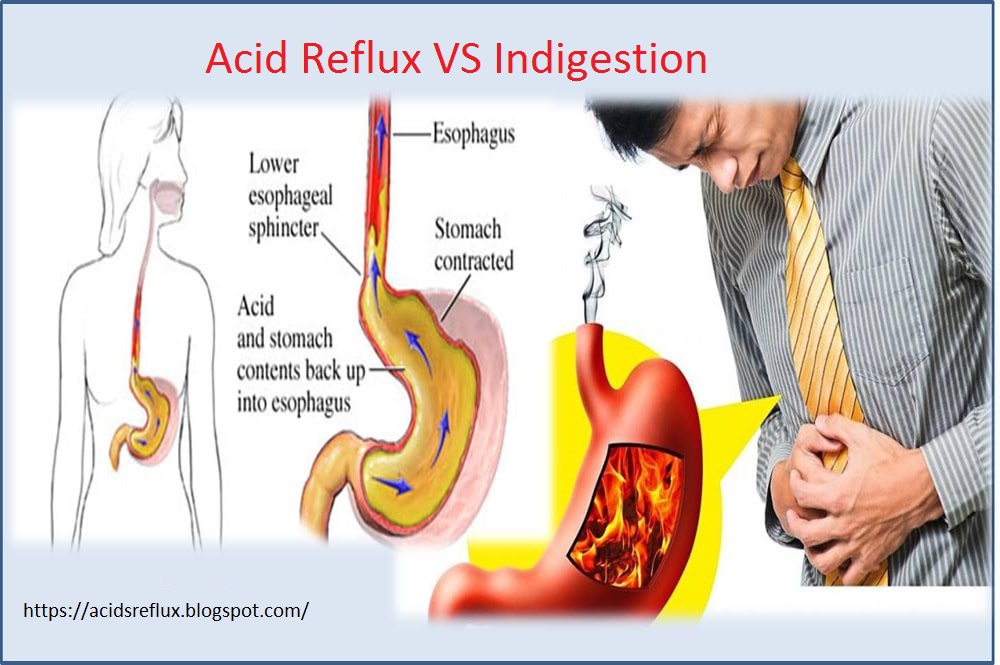 2%), as well as 2-4 weeks before the due date or in the early postpartum period. Uncomplicated peptic ulcer does not adversely affect the development of the fetus.
2%), as well as 2-4 weeks before the due date or in the early postpartum period. Uncomplicated peptic ulcer does not adversely affect the development of the fetus.
Treatment of peptic ulcer in pregnant women includes adherence to generally accepted "regime" measures and diet; taking in the usual therapeutic doses of non-absorbable antacids (1 sachet 3 times a day 1 hour after meals and adsorbents 1 sachet 3 times a day 1 hour after meals). If there is no effect, h3-blockers are prescribed (ranitidine 150/300 mg once a night), in case of their insufficient effectiveness, as well as with the development of complications, we can take PPIs (omeprazole 20-40 mg, lansoprazole 30-60 mg, pantoprazole 40 mg). mg in the morning before the first meal). Bismuth preparations are contraindicated for pregnant women. Eradication therapy for H. pylori infection in pregnant women is not carried out.
Author:
Kaibysheva Valeria Olegovna
Gastroenterologist Ph. D.
D.
Toxemia, Intestinal Problems & Heartburn
Find out how pregnancy affects the digestive tract, which trimesters are more likely to cause bowel symptoms and nausea, and what to do to manage them.
During pregnancy, the burden on the mother's body increases. The body needs more nutrients, the body produces additional hormones. And the growing fetus puts pressure on neighboring organs, including the stomach and intestines. We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn.
Contents:
- 2. Toxicosis and pregnancy
- 3. Causes, risks and treatment of diarrhea during pregnancy
- 4. Heartburn and stomach pain during pregnancy
- 5. Bloating, constipation and microbiota during pregnancy
- 6. Note
Changes in the work of the gastrointestinal tract by trimesters of pregnancy
The average duration of pregnancy is 40 weeks, which are usually divided into trimesters in accordance with the stages of intrauterine development of the child.
Each trimester is accompanied by a number of changes in the body, including in the gastrointestinal tract:
| The first trimester 26 weeks | Third trimester of pregnancy 27–40 weeks |
| Morning sickness Morning sickness Zapor Intestinal disorder increased appetite TREAM to certain products Acid Reflux | Zapor Acid Office 9000 95 900. Flatulence Constipation Heartburn Violation of the outflow of bile Hemorrhoids |
The Atlas genetic test will help you find out how your genes affect the level of female sex hormones necessary for fertility and pregnancy.
Causes of gastrointestinal problems during pregnancy
Every pregnancy is accompanied by inevitable changes in the functioning of the digestive system. They are more often caused by hormonal changes and increased stress on the organs, but they can also be associated with lifestyle and health conditions, for example:
- Sedentary lifestyle and unbalanced diet;
- Certain drugs, including calcium or aluminum antacids;
- Viral and bacterial infections;
- Intolerance to certain nutrients and allergic reactions;
- Stress;
- Diseases of the thyroid gland.
If you have chronic diseases of the gastrointestinal tract and you are planning a pregnancy, try to consult your doctor in advance. Symptoms of conditions such as irritable bowel syndrome (IBS) or acid reflux are more likely to get worse during pregnancy. Your doctor will help prepare your body and create a prevention plan to help relieve symptoms during this time.
Irritable bowel syndrome, or IBS, is a functional bowel disease that causes frequent abdominal pain, impaired peristalsis, bloating, constipation, or diarrhea.
Morning sickness, vomiting and general malaise during pregnancy
Morning sickness and morning sickness during early pregnancy are common, because the body undergoes important changes necessary for the development of the child.
up to 90%
women experience nausea during pregnancy
Doctors find it difficult to say with certainty why pregnant women feel sick in the morning. The main theory is hormonal changes. But there are some patterns associated with an increased risk of morning sickness:
- Multiple pregnancy;
- Toxicosis during previous pregnancy;
- History of morning sickness during pregnancy in close relatives;
- Tendency to motion sickness in transport;
- Use of oral contraceptives containing estrogen before pregnancy;
- Frequent migraines;
- BMI 30 and above;
- Increased levels of stress hormones
Risks of severe morning sickness and how to reduce nausea
Nausea and vomiting are usually not associated with a risk for mother and child and will pass by 16-20 weeks of pregnancy, but it is not necessary to wait so long - there are ways that can help reduce nausea and enjoy the process of waiting for a new person:
- Get plenty of rest - fatigue increases toxicosis;
- Avoid smells and foods that cause nausea;
- Eat something right after waking up.
 A toast or a slice of bread will help reduce nausea;
A toast or a slice of bread will help reduce nausea; - Avoid hunger - empty stomach increases nausea. Eat small meals often, prefer low-fat, high-carbohydrate foods;
- Try ginger - studies show it helps with nausea;
- Sip as often as possible and prefer still water.
In rare cases, pregnant women may develop hyperemesis gestationis or excessive vomiting. This is a serious condition that can lead to dehydration, kidney damage, seizures, abnormal heart rhythms, and even death.
Signs of dehydration include: dry mouth, dizziness, dark urine, infrequent urination and/or dizziness.
Symptoms of excessive pregnancy vomiting:
- frequent nausea for a long time and regular vomiting after meals;
- dry skin and lips;
- sudden weight loss;
- low blood pressure (below 90/60).
If symptoms of excessive pregnancy vomiting occur, do not wait until the condition resolves on its own.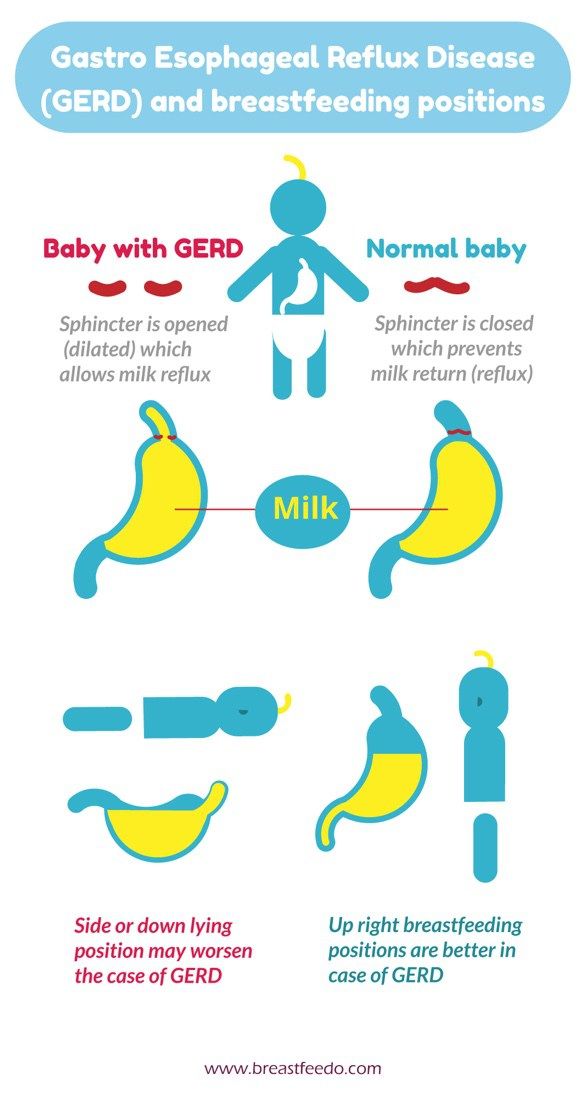 It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
0.5–2%
pregnant women experience excessive vomiting
Diarrhea in pregnancy
The word "diarrhea" comes from the Greek language and literally means "to flow through". This is a condition during which bowel movements or bowel movements occur three times a day or more often. This phenomenon is especially typical for the third trimester of pregnancy, but it can also occur earlier.
Symptoms of diarrhea:
- Three or more bowel movements per day
- Urgent urge to have a bowel movement
- Abdominal pain and cramps
- Bloating
Causes of diarrhea during pregnancy poisoning, dysbacteriosis, bacterial and viral infections:
| Gastroenteritis | Use of lactose and gluten in case of intolerance to these nutrients |
| Bacterial infections: listeriosis or salmonella | Chronic gastrointestinal diseases: Crohn's disease, IBS, ulcerative colitis |
| Certain antibiotics and antacids to reduce acidity | Laxatives |
| Sugar substitutes such as sorbitol | Overconsumption of certain foods |
Tip: If you have recently returned from a vacation in an exotic country with nausea and diarrhea and find out you are pregnant, see your doctor as soon as possible.
Gastroenteritis
One common cause of diarrhea during pregnancy is gastroenteritis, or stomach flu. It is caused by bacterial or viral infections: norovirus, rotavirus, E. coli, salmonella, which enter the body through contact with contaminated surfaces, dishes, food and water.
Gastroenteritis usually lasts about three days. However, severe illness is a health hazard, especially during pregnancy, as it can cause dehydration, electrolyte imbalance, and lead to preterm labor.
The main symptoms of gastroenteritis are diarrhea without blood, nausea and vomiting, stomach cramps and pain, slight fever, headache and muscle pain.
Take extra precautions to reduce your risk of getting sick: frequent handwashing and surface disinfection. If the expectant mother has small children, they are not recommended to use the same cutlery.
Risks of diarrhea during pregnancy
Usually diarrhea during pregnancy is not a cause for concern. However, you should consult a doctor if the following symptoms occur during this period:
However, you should consult a doctor if the following symptoms occur during this period:
- Diarrhea for more than two days;
- Stools with blood or mucus;
- Sudden weight loss;
- Abdominal pain;
- Dehydration.
How to treat diarrhea during pregnancy
If you have diarrhea during pregnancy, drink plenty of fluids, avoid foods high in fat and sugar, avoid dairy products, and caffeinated drinks.
Dehydration is a serious risk, especially during pregnancy, so electrolyte balance should be restored first with fluids and simple foods:
| Moderate fruit juices | Drinks without alcohol and caffeine |
| Bananas | Potatoes |
| Rice | Toast |
| Rusks | Light soups and broths |
| Pasta | Applesauce |
Find out about your body's ability to break down lactose and gluten with the Atlas Microbiota Test.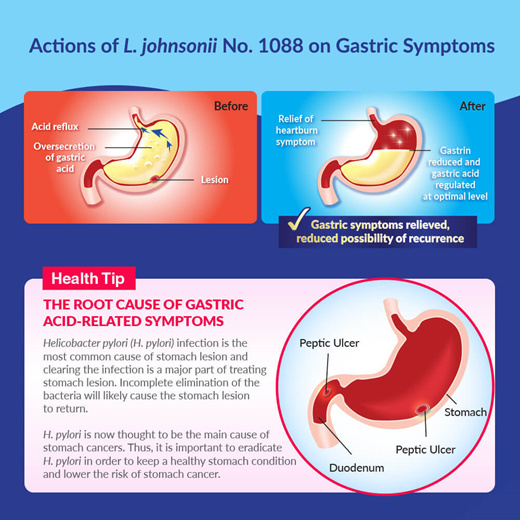
Stomach pain and heartburn during pregnancy
Many women experience stomach pain during pregnancy, especially the upper part of the stomach, as well as heartburn - a burning sensation in the chest and esophagus.
This is more common in the third trimester, after about 27 weeks. This is an unpleasant but natural phenomenon during pregnancy: the baby grows inside the uterus and presses on other organs, including the stomach. And hormones cause the muscles to relax, which causes acid from the stomach to enter the esophagus and irritate it. In addition, pain can be caused by problems with certain organs such as the gallbladder, or inflammation of the pancreas.
Symptoms of heartburn during pregnancy:
- Burning in chest and esophagus;
- Feeling of overeating, heaviness or bloating;
- Belching, including with acid and/or food particles;
- Nausea.
It is unlikely that you will be able to avoid cramps and heartburn during pregnancy.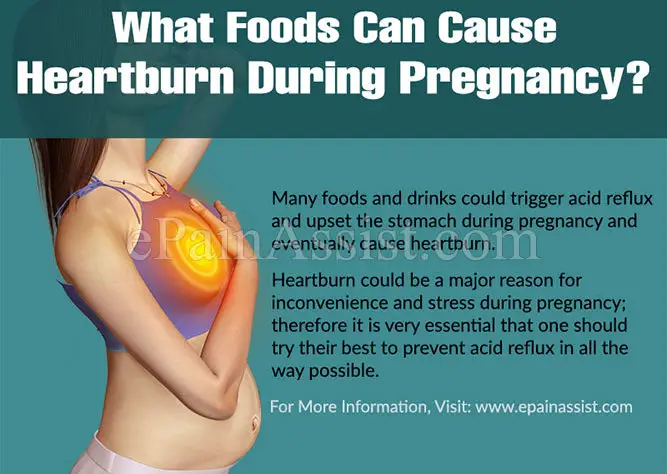 However, some tips can help reduce their frequency:
However, some tips can help reduce their frequency:
Nutrition : try to avoid overeating - eat easily digestible food in small portions; do not eat three hours before bedtime; watch your posture while eating - so the pressure on your stomach will be less.
Smoking and alcohol: In addition to known harms to mothers and babies, tobacco smoke also relaxes the muscles in the lower esophagus, allowing acid to enter the esophagus. And alcohol provokes heartburn and acid reflux.
Although stomach pain and heartburn often accompany pregnancy, abdominal pain, especially in the third trimester, should be taken seriously. It can be a sign of preterm labor or placental abruption, and puts mother and baby at risk.
If you experience severe abdominal pain during pregnancy that is accompanied by the following symptoms, seek medical attention as soon as possible:
| Abdominal pain and fever | Bleeding |
| Regular convulsions | Unusual vaginal discharge/ spotting |
| Vomiting | Low back pain |
| Pain or burning when urinating | Severe pain that lasts 30-60 minutes |
Bloating, constipation and microbiota during pregnancy
Excessive gas and constipation during pregnancy can be caused by hormonal changes, such as increased production of progesterone.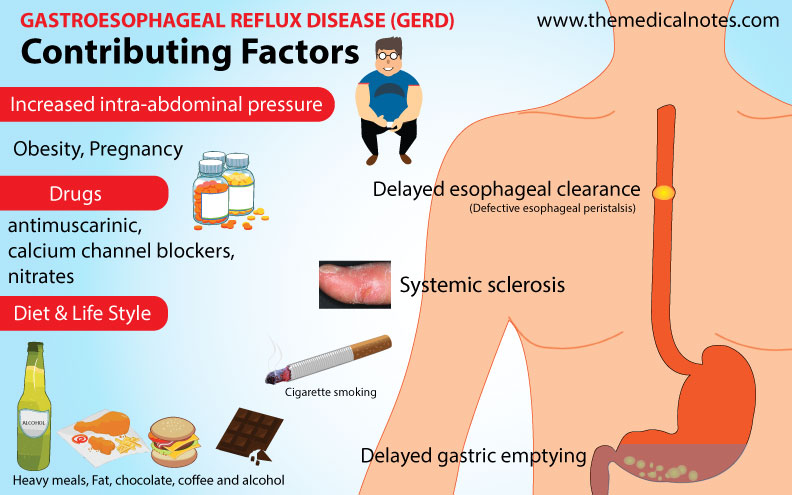 This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
Flatulence - bloating of the abdomen due to the accumulation of gases.
Here are a few simple rules that will help improve intestinal motility and avoid constipation and bloating:
- If you do not usually eat a lot of fiber and indigestible foods like legumes, try to gradually introduce them into your diet;
- Avoid carbonated drinks and fatty foods;
- Move more;
- Drink plenty of fluids.
If bloating and constipation are accompanied by severe pain that lasts more than 30 minutes, or if you have been constipated for two or more weeks, see your doctor.
Gut microbiota and bacteria during pregnancy
A woman's body goes through many changes during pregnancy, and this can affect the microbiota, the bacterial ecosystem that lives in the gut.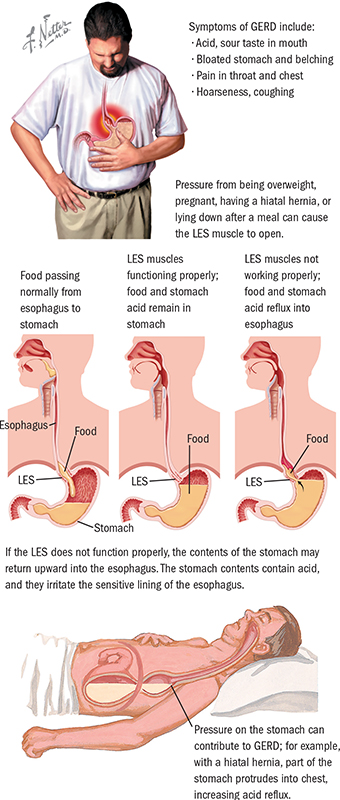 Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
The additional influx of female hormones that accompanies pregnancy alters gut function and affects the microbiota. This is good, because the bacterial community is constantly adjusting to external and internal conditions in order to keep up with the needs of the body.
To keep your gut bacteria running smoothly, they need your help. Provide them with healthy foods and plant fibers. Fruits, vegetables, whole grains, nuts, and seeds contain prebiotics, special substances that beneficial bacteria feed on. When properly balanced, the bacteria even increase your body's defenses against harmful microorganisms that can cause gastroenteritis during pregnancy.
The Atlas Microbiota Test helps you understand how to prepare your gut for future pregnancies and reduce the risk of digestive problems.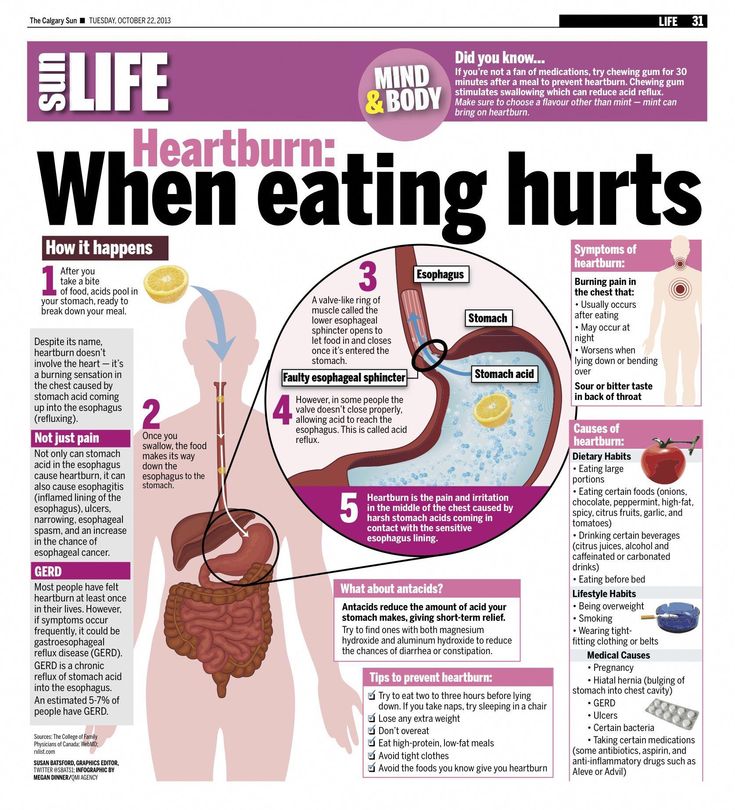
☝️ Take note
Now you have all the necessary knowledge and tools to help you deal with digestive problems during pregnancy. They are quite varied and quite natural, but in some cases it is necessary to immediately seek medical help:
- Vomiting blood;
- Blood in stool;
- Diarrhea for more than two days;
- Constipation for more than two weeks;
- Sudden weight loss;
- Severe pain interfering with daily activities;
- Difficulty breathing;
- Pain when swallowing or difficulty swallowing;
- Excessive fatigue.
More articles on the causes of digestive problems on the blog:
- 7 foods that cause gas and bloating
- Lindsey J Wegrzyniak, Treatment of Hyperemesis Gravidarum, 2012
- Edwards A. et al., The Maternal Gut Microbiome During Pregnancy, 2018
- National Health and Safety (NHS), Vomiting and morning sickness in pregnancy
- Kudzai Kanhutu, Travel and pregnancy: an infectious diseases perspective, 2011
- CDC, Pregnant travelers
- U.