Meningitis rash infant
Kids Health Information : Meningitis
Meningitis happens when the membrane covering the brain and the spinal cord, called the meninges, becomes infected and swollen or inflamed. Meningitis is usually caused by either bacterial or viral infections.
Meningitis is not common, but it can be very serious and requires urgent medical treatment. There are many viral and bacterial infections that can cause meningitis, and sometimes meningitis happens because of a complication from another illness such as measles or chickenpox.
Bacterial meningitis can get worse very quickly. One in five children infected is left with permanent disabilities, such as deafness or cerebral palsy. In a small number of cases, bacterial meningitis can cause death. Viral meningitis is more common, but it is less serious than bacterial meningitis.
Most children will make a full recovery after meningitis, but it can take time.
Signs and symptoms of meningitis
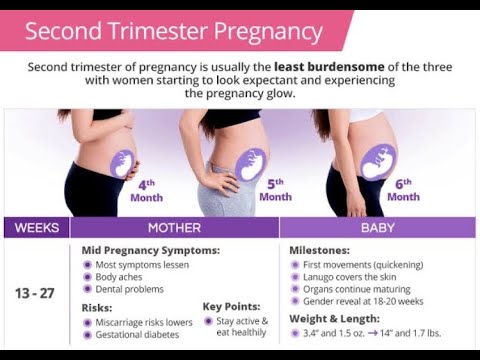
The signs and symptoms of meningitis can be different depending on the age of your child, and whether the disease is caused by a virus or bacteria. Signs and symptoms may include:
- fever
- vomiting
- seizures (fits)
- headache
- irritability and high-pitched cry (especially in babies)
- the soft spot on the top of a baby’s head (the fontanelle) may bulge and look very full
- tiredness, drowsiness (lethargy) or hard to wake
- a stiff neck
- dislike of bright lights (photophobia)
- babies may hold their head back or arch their back.
When to see a doctor
If your child has a skin rash of small bright red spots or purple spots or bruises that do not turn white (blanch) when you press on them, this may be a sign of meningitis caused by the meningococcal bacteria. See our fact sheet Meningococcal infection.
If your child is showing signs of meningitis or meningococcal infection, take them to the nearest doctor or hospital emergency department immediately.
To diagnose meningitis, your child will need a lumbar puncture (see our fact sheet Lumbar puncture).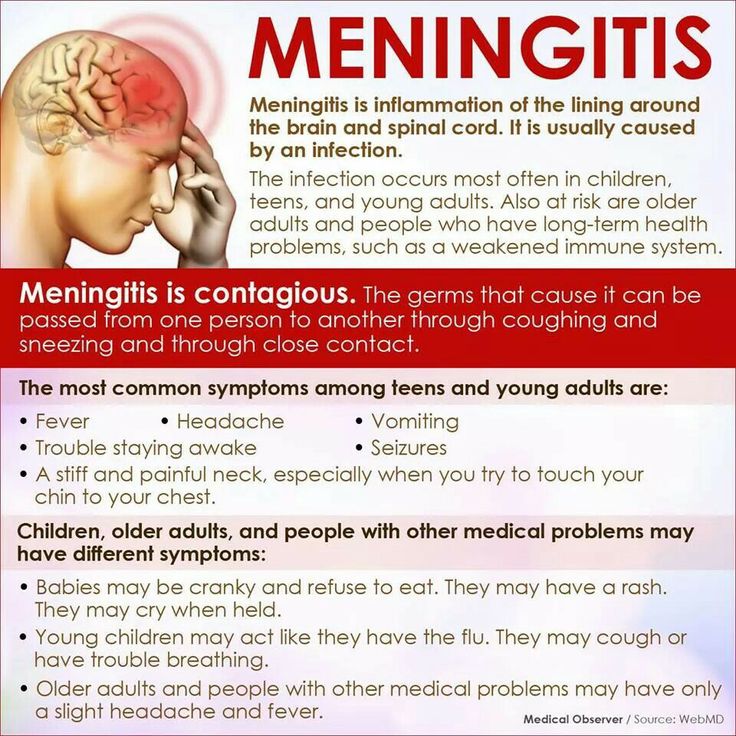 This is a safe test performed by an experienced doctor, to take a sample of the fluid around the spine. A diagnosis of meningitis is made by examining this fluid and doing blood tests.
This is a safe test performed by an experienced doctor, to take a sample of the fluid around the spine. A diagnosis of meningitis is made by examining this fluid and doing blood tests.
Treatment for meningitis
If your child has meningitis, they will be admitted to hospital. Their treatment and care will depend on the type of meningitis they have and how unwell they are.
The results from the lumbar puncture can take two to three days to come back. In the meantime, your child will be given antibiotics directly into a vein through a drip (intravenous or IV therapy), in case they have bacterial meningitis.
Viral meningitis
Generally, viral meningitis is not as severe as bacterial meningitis. The treatment does not include antibiotics because antibiotics do not work on viruses. Children with viral meningitis will continue to be watched closely during their hospital stay.
Bacterial meningitis
Bacterial meningitis can be more severe, and your child will need ongoing antibiotics. Your child will be watched closely throughout their hospital stay for any changes in their condition. The regular checks made on your child during their stay in hospital may include checking your child's
vital signs (such as heart rate, temperature and blood pressure) and the state of their neurological system (brain and nerves).
Your child will be watched closely throughout their hospital stay for any changes in their condition. The regular checks made on your child during their stay in hospital may include checking your child's
vital signs (such as heart rate, temperature and blood pressure) and the state of their neurological system (brain and nerves).
Your child may also receive:
- fluids and medicines through a drip
- additional blood tests
- steroid medicines to reduce the swelling in their brain.
If meningococcal meningitis is suspected, it may be necessary for people who have had close contact with your child to receive antibiotics – your child’s doctor will advise you if this is needed.
Depending on the age of your child, the type of bacteria and other factors, intravenous (through a drip) antibiotic treatment may be required for up to three weeks. In some cases, some children may be able to finish their antibiotic therapy at home, under the supervision of a nurse.
Follow-up
Most children will make a full recovery after meningitis, but it can take time. There are some possible after-effects of meningitis, which may include:
- general tiredness
- frequent headaches
- difficulty in concentration and short-term memory lapses
- clumsiness or problems with balance
- hearing problems
- mood swings.
After your child goes home from hospital, they may need check-ups to monitor their recovery. They may need a hearing test, as a small number of children who have had meningitis develop problems with their hearing.
Some children may be left with permanent damage and disability following meningitis. Your doctor will be able to give you more information about your child's long-term outlook.
How is meningitis spread?
Many people carry the bacteria that causes bacterial meningitis in their noses and throats without getting sick. These people are called healthy carriers.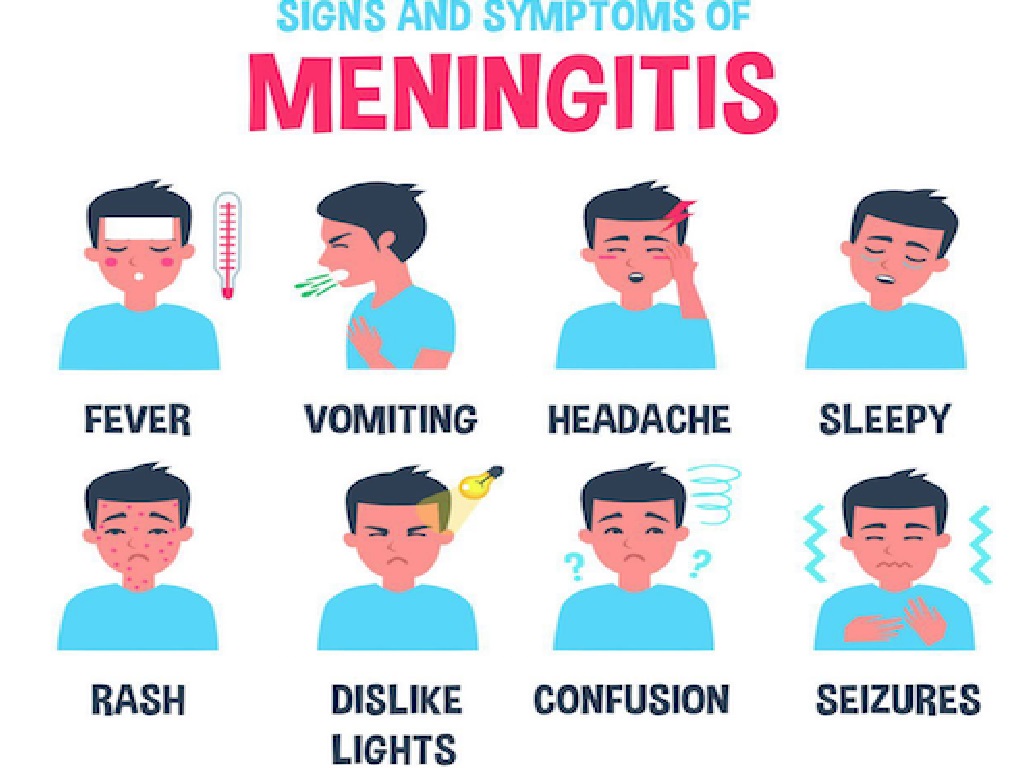 Healthy carriers can spread the bacteria to other people, who may become sick.
Healthy carriers can spread the bacteria to other people, who may become sick.
The bacteria or virus causing meningitis can be spread from person to person by coughing, sneezing, kissing or sharing cups, drink bottles or cutlery.
Prevention of meningitis
- Several of the bacteria that cause meningitis can be largely prevented by the routine childhood immunisations. Making sure your child is fully up to date with these immunisations is the best way to prevent meningitis.
- Children who are exposed to cigarette smoke are at a greater risk of getting meningitis. Do not allow anyone to smoke in your home or around your child.
Good hygiene reduces the chance of getting viruses or bacterial infections, or passing them onto others. Good hygiene includes:
- regularly washing hands thoroughly
- not sharing drink bottles, cups or cutlery
- encouraging children to cough or sneeze into their elbow
- teaching your child to throw tissues into the bin as soon as they have used them and to wash their hands afterwards.

Key points to remember
- Meningitis is an inflammation of the meninges (the membrane covering the brain and spinal cord).
- Meningitis is caused by either a bacterial infection or a viral infection. Bacterial meningitis can get worse very quickly.
- If your child is showing signs of meningitis, seek immediate medical attention.
- Most people recover from meningitis, although it may take a long time.
- Keeping your child's immunisations up to date is the best way to prevent meningitis.
For more information
- Kids Health Info factsheet: Lumbar puncture
- Kids Health Info factsheet: Meningococcal infection
- Kids Health Info fact sheet: Stopping the spread of germs
- The Meningitis Research Foundation (UK)
Common questions our doctors are asked
When will someone with meningitis stop being contagious?
As long as a person with meningitis is coughing or sneezing
droplets into the air, they will be contagious.
If tests show my child has viral meningitis, will the antibiotics cause any problems?
There are risks associated with all medicines, including antibiotics.
But the risk of leaving bacterial meningitis untreated is far greater than the
risk of a reaction to one of the antibiotics. The safest option is to
administer antibiotics immediately, before losing valuable time while we wait
for test results.
Developed by The Royal Children's Hospital General Medicine department. We acknowledge the input of RCH consumers and carers.
Reviewed April 2018.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit www.rchfoundation.org.au.
Meningitis Symptoms in Babies & Toddlers
Meningitis and septicaemia can happen together. Be aware of all the signs and symptoms of them in babies and toddlers. It is especially important to keep an eye on babies since they are unable to communicate when they are not feeling well
DO NOT wait for a rash. If your baby or toddler is ill and getting worse, get medical help immediately.
If your baby or toddler is ill and getting worse, get medical help immediately.
Symptoms can appear in any order. Some may not appear at all.
Common signs & symptoms of meningitis and septicaemia in babies and toddlers.
-
Fever, cold hands and feet
-
Refusing food and vomiting
-
Fretful, dislike being handled
-
Drowsy, floppy, unresponsive
-
Rapid breathing or grunting
-
Pale, blotchy skin. Spots/rash.
See the Glass Test -
Unusual cry, moaning
-
Tense, bulging fontanelle (soft spot)
-
Stiff neck, dislike bright lights
-
Convulsions/seizures
Early symptoms can include:
Fever, headache, vomiting, muscle pain and fever with cold hands and feet.
Someone with meningitis or septicaemia can get a lot worse very quickly. Keep checking them.
Trust your instincts – Get medical help immediately
Get medical help immediately
Why are the under-5s at risk?
Babies and young children are particularly vulnerable to meningitis as they cannot easily fight infection because their immune system is not yet fully developed. The most common causes of meningitis are bacteria and viruses.
Viral meningitis is rarely life-threatening, but can still make babies and young children very unwell. Most children will make a good recovery, but recovery can be slow.
Bacterial meningitis can be fatal and needs rapid admission to hospital and urgent medical treatment. Whilst most children will make a good recovery, around 10% will die and some will be left with lifelong disabilities.
Find out more about the after-effects of meningitis and septicaemia.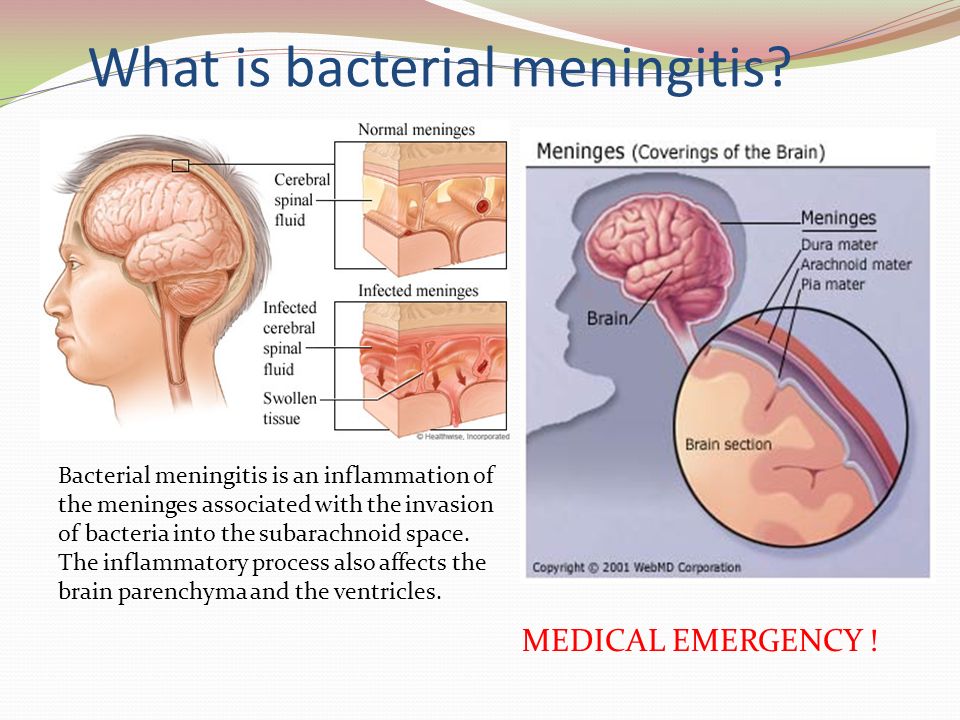
Some bacteria that cause meningitis can also cause septicaemia (blood poisoning). The rash associated with meningitis is actually caused by septicaemia. You should never wait for a rash, it can be a late sign or may not appear at all. Learn more about the rash and glass test.
Download more information about meningitis in babies and children under 5.
-
Glass test
A rash that does not fade under pressure is a sign of meningococcal septicaemia, do the glass test
-
Signs and symptoms
By learning the signs and symptoms of the disease now, you could be saving a life in the future
-
Meningitis symptoms in adults
A visual list of meningitis symptoms in adults
Meningococcal infection and its prevention
Meningococcal infection occupies an important place in infectious pathology and continues to be relevant for the Republic of Belarus
Meningococcal infection affects only people.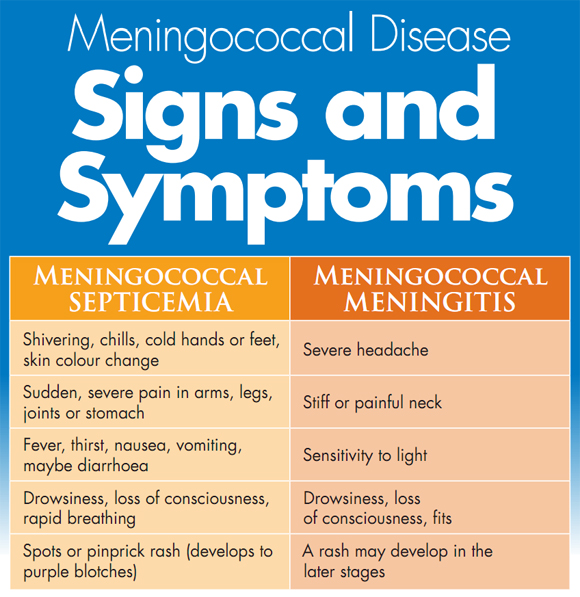 The causative agent - meningococcus - is transmitted by airborne droplets, as well as, for example, with the flu. This microbe lives in the nasal cavity and can be transmitted from person to person by sneezing, coughing and even talking. This is a very serious disease that can develop among full health in a matter of hours and minutes. Children are more often ill, and generalized forms of the disease in 80% of cases occur in children under 2 years of age. Sometimes it is not possible to save a sick child.
The causative agent - meningococcus - is transmitted by airborne droplets, as well as, for example, with the flu. This microbe lives in the nasal cavity and can be transmitted from person to person by sneezing, coughing and even talking. This is a very serious disease that can develop among full health in a matter of hours and minutes. Children are more often ill, and generalized forms of the disease in 80% of cases occur in children under 2 years of age. Sometimes it is not possible to save a sick child.
The incubation period (the period from the moment meningococcus enters the body until the first signs of the disease appear) can last from several hours to 10 days. It all depends on the age and immune status of the patient.
The microbe itself is relatively unstable in the external environment. Outside of a person, he dies within 30 minutes. Fresh air, direct sunlight, ultraviolet radiation and disinfectants are especially detrimental to meningococcus.
This disease is characterized by a very acute onset, one might say in the midst of full health or after a slight runny nose. The temperature rises sharply to very high numbers, the child complains of a severe headache, at first a single, and then indomitable vomiting appears. Young children, who cannot yet complain, may have regurgitation, lethargy, refusal of the breast.
The temperature rises sharply to very high numbers, the child complains of a severe headache, at first a single, and then indomitable vomiting appears. Young children, who cannot yet complain, may have regurgitation, lethargy, refusal of the breast.
The main symptom of the fulminant form and the appearance of an infectious agent in the blood (meningococcemia) is a rash on the child's skin. Rash with meningitis in children is one of the most characteristic symptoms. Initially, it may be morbilliform in nature - in the form of small red spots and papules. After some time, such a rash disappears and a hemorrhagic rash characteristic of meningococcal infection appears. Pinpoint hemorrhages appear first in the feet and legs of the child, and then spread higher to the trunk and other parts of the body. On pale skin, they resemble a picture of a starry sky.
- Note that meningococcal rash does not go away with pressure. If a rash appears on the face, eyelids, oral mucosa, auricles, or at the very beginning of the disease, this is an unfavorable factor and is typical for severe forms of the disease.
 The rash will increase. And it is precisely in the presence of it that it is necessary to re-call the doctor, since the primary diagnosis before the rash can be set as an acute respiratory disease.
The rash will increase. And it is precisely in the presence of it that it is necessary to re-call the doctor, since the primary diagnosis before the rash can be set as an acute respiratory disease.
This form of meningitis is dangerous because toxic-septic shock can develop due to hemorrhage in vital organs and, above all, in the adrenal glands. This shock causes death in 5-10 percent of patients. Therefore, the sooner parents seek medical help, and the sooner an appropriate diagnosis is made, the greater the chance of saving the patient. But in any case, hospitalization will be required and parents do not need to refuse it.
- What are the preventive measures for meningococcal disease?
You just need to carefully monitor the child's condition and, if warning signs appear, immediately seek medical help.
Oddly enough, the best prevention of meningitis is to strengthen the immune system - walks in the fresh air, rational nutrition and hardening. Equally important is personal hygiene. Thorough hand washing is very important to avoid infection. Teach your children to wash their hands frequently, especially before eating, after being in a public place, and after they have touched animals.
Equally important is personal hygiene. Thorough hand washing is very important to avoid infection. Teach your children to wash their hands frequently, especially before eating, after being in a public place, and after they have touched animals.
And most importantly, do not try to treat the baby yourself. In many ways, the results of the treatment of meningitis depend on the time that has passed since the onset of the first symptoms and the start of therapy. Only a specialist is able to correctly assess the situation and select treatment tactics.
Prevention of meningitis in children is primarily the prevention of airborne infection of the child. For children aged 1 to 3 years, the main danger is adults, and first of all, relatives. The most dangerous age for meningitis is up to 5 years, and in many respects the health of the child depends on his parents. If one of the older family members has a cough, runny nose, nasal congestion, think about the child - do not approach him, or put on a four-layer gauze bandage, covering both the nose and mouth.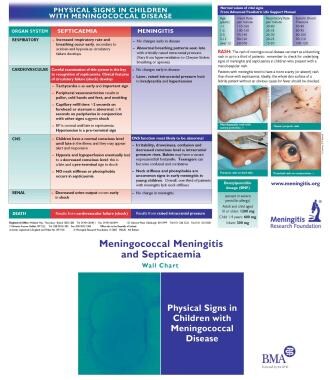
- Meningococcus is one of the weakest microbes, it dies very quickly outside the human body, especially from the action of ultraviolet rays of sunlight. Regular ventilation of the premises and sufficient sunlight can quickly get rid of these microbes in the air. Thus, you need to take care of good lighting in your child's room. The nursery should always be ventilated and washed clean.
Among other preventive measures, it is recommended to have fewer contacts during the period of the seasonal rise in the incidence of influenza and ARVI, to attend social events less frequently. All festive events (christenings) associated with the birth of a child must be carried out outside the apartment where he is.
And most importantly, don't try to treat yourself. The results of treatment of meningococcal infection largely depend on the time interval between the onset of the first symptoms and the start of therapy. Only a specialist can correctly assess the situation and choose the tactics of treatment.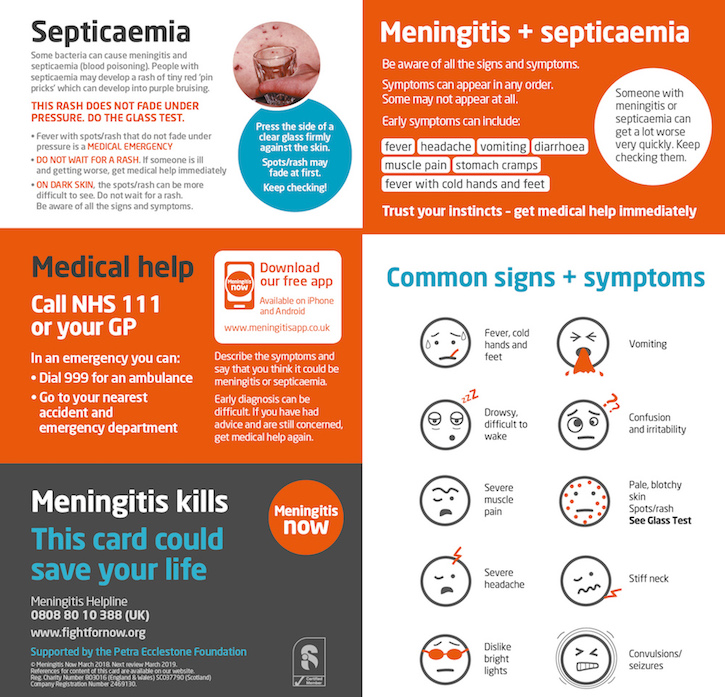
If hospitalization is suggested by a health worker, do not refuse it, your child's life may depend on it.
A complete and balanced diet enriched with vitamins and microelements, playing sports, hardening the body also contribute to the body's resistance to infection. 9Nedved N.V.
How to recognize one of the most dangerous infections for a child
Irina Stanislavovna, why are we talking about meningococcal infection right now? After all, doctors encountered this disease less and less often ...
Irina Koroleva: Indeed, from 2003 to 2017, the incidence has seriously decreased. But then the increase began again - and immediately by 10 percent per year: both in 2017 and in 2018. Today, the average figure for Russia is 0.52 per 100,000 people. That's not a lot. But there are regions where people get meningitis two to three times more often. In the Orel, Novgorod, Penza, Ulyanovsk, Omsk regions, Khabarovsk Territory, the Republic of Buryatia and Moscow.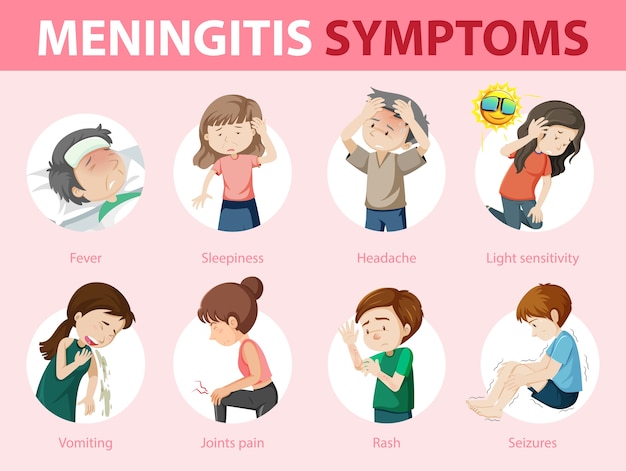 In the capital, the situation is especially alarming - the incidence is more than one per 100,000 people. The prognosis is not the most favorable.
In the capital, the situation is especially alarming - the incidence is more than one per 100,000 people. The prognosis is not the most favorable.
Who is at risk?
Irina Koroleva: Meningitis is considered the most dangerous infection for children: about every fifth case ends in tragedy. Moreover, 70 percent of the sick are children under 14 years old. And in the most "acute" risk zone - babies up to a year. The disease affects the soft membranes of the brain: 20 percent have severe cognitive impairment, very often deafness occurs. That's why we're so active in vaccinating. The goal is to prevent the first case of the disease, save as many lives as possible.
How can a mother suspect an illness in a child?
Irina Koroleva: Perhaps there is no more insidious and unpredictable disease than meningococcal infection. The most important thing that should alert parents is a high temperature of 39-40 degrees, which is difficult to bring down.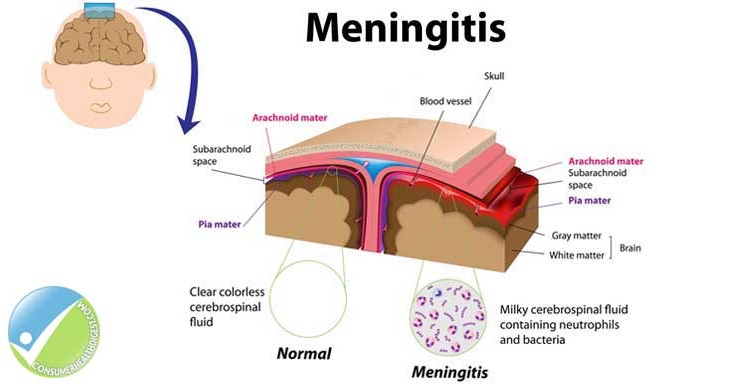 Even the flu, as a rule, does not give such a stable temperature. Unusual behavior of the child, a rash, an unbearable headache (even if the baby cannot tell, this can be suspected by his behavior) - these are the main signs. In principle, there may be other symptoms: photophobia, pale hands and feet. Or maybe not - the disease develops individually. There are acute forms of meningitis, in which the infectious process cascades, at lightning speed. And the bill is not for a day, but literally for hours. Therefore, at the first suspicions, it is urgent to call an ambulance and in no case refuse hospitalization. And in a hospital - not to refuse a lumbar puncture. This procedure is fundamentally important for the treatment of the child.
Even the flu, as a rule, does not give such a stable temperature. Unusual behavior of the child, a rash, an unbearable headache (even if the baby cannot tell, this can be suspected by his behavior) - these are the main signs. In principle, there may be other symptoms: photophobia, pale hands and feet. Or maybe not - the disease develops individually. There are acute forms of meningitis, in which the infectious process cascades, at lightning speed. And the bill is not for a day, but literally for hours. Therefore, at the first suspicions, it is urgent to call an ambulance and in no case refuse hospitalization. And in a hospital - not to refuse a lumbar puncture. This procedure is fundamentally important for the treatment of the child.
Why?
Irina Koroleva: An analysis of the cerebrospinal fluid will allow you to find out if there are purulent inflammations and accurately determine the pathogen itself. Pick the right antibiotic. Indeed, besides meningococcus, there are other bacteria: pneumococci, Haemophilus influenzae.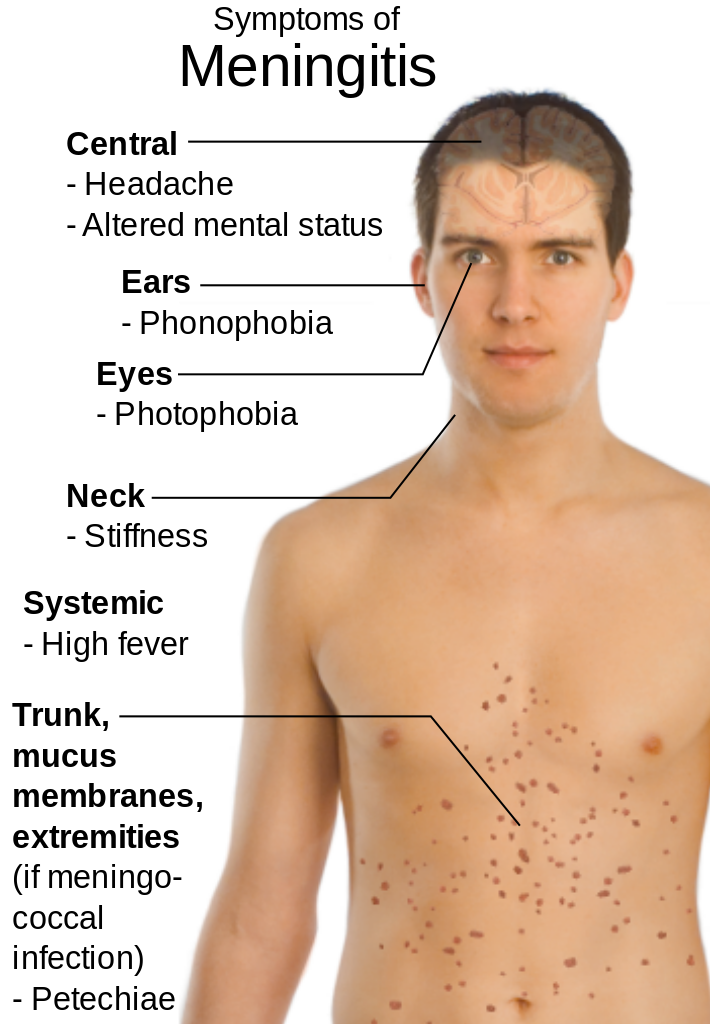 ..
..
There is no more insidious and unpredictable disease than meningitis
The most common cause of meningitis in Russia for a long time was the bacterium Neisseria meningitidis serogroup B. In second place - serogroup C, on the third - A, on the fourth - W. And it is the last W that worries us the most today. Why? If in the first three groups the incidence even decreases from year to year, then W-meningococcus (which has practically never been seen in Russia before) is steadily "taking positions". In Moscow, for example, last year it was he who caused half of all cases. The most dangerous thing here is that it is much more difficult to recognize even compared to a common infection - the symptoms can be completely atypical for meningitis.
So the disease is "disguised"?
Irina Koroleva: Exactly. If with ordinary meningitis the hospitalization period is 1-2 days, then with W - three to four. In the usual case, the rash appears on the first or second day, and with W - on the third or fourth.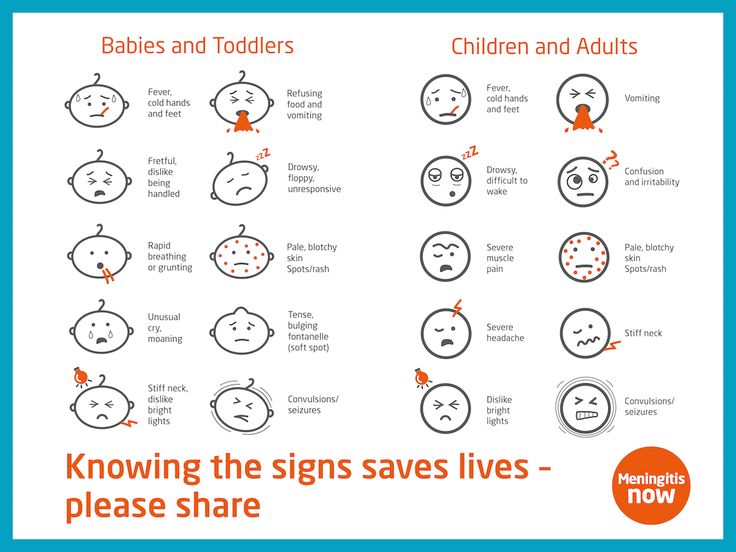 W-meningitis is more severe than usual, can give a picture of "acute abdomen". As a result, an incorrect diagnosis is made, the patient ends up in a non-core hospital and does not receive the necessary assistance on time. Because of this, the number of deaths is increasing.
W-meningitis is more severe than usual, can give a picture of "acute abdomen". As a result, an incorrect diagnosis is made, the patient ends up in a non-core hospital and does not receive the necessary assistance on time. Because of this, the number of deaths is increasing.
A big positive is that serogroup W meningococcus is included in the modern quadrivalent vaccine, which is registered and used in Russia. It creates a stable immunity and can be shown from 9 months to 55 years.
Is meningitis prevention included in the national immunization schedule?
Irina Koroleva: Planned - no. Vaccination is indicated for people who are in the focus of infection. In addition, all conscripts are vaccinated. But we have already proposed to make changes to the national calendar and expand prevention according to epidemic indications. Include vaccination of children under five years of age at risk, include health workers. In Moscow, this problem has already been attended to - in city clinics, mothers are offered to vaccinate small children against meningitis.