Newborn no urine in first 24 hours
Baby's First Days: Bowel Movements & Urination
Many new parents wonder what's normal and what's not when it comes to diapering their newborn. Here's what you can expect during your baby's first few days.
Urination
Your baby may urinate as often as every one to three hours or as infrequently as four to six times a day. If they're ill or feverish, or when the weather is extremely hot, their usual output of urine may drop by half and still be normal.
Urination should never be painful. If you notice any signs of distress while your infant is urinating, notify your pediatrician. This could be a sign of infection or some other problem in the urinary tract.
In a healthy child, urine is light to dark yellow in color. (The darker the color, the more concentrated the urine; the urine will be more concentrated when your child is not drinking a lot of liquid.) In the first week after birth, you may see a pink or brick-red stain on the
diaper, often mistaken for blood. In fact, this stain is usually a sign of highly concentrated urine, which has a pinkish color. As long as the baby is wetting at least four diapers a day, there probably is no cause for concern. If the pinkish staining persists, consult your pediatrician.
Newborn girls may have a small spot of blood in the diaper, also usually in the first week after birth; this blood is caused by her mother's hormones affecting the baby's uterus. After that time, however, the presence of actual blood in the urine or a bloody spot on the diaper is never normal, and your pediatrician should be notified. It may be due to nothing more serious than a small diaper rash sore, but it also could be a more serious problem. If this bleeding is accompanied by other symptoms, such as abdominal pain, poor feeding, vomiting, fever, or bleeding in other areas, seek medical attention immediately.
Bowel movements
For the first few days after birth, your baby's first
bowel movements will be a substance known as meconium. This thick black or dark green substance filled their intestines before birth, and once passed, the stools turn
yellow-green.
This thick black or dark green substance filled their intestines before birth, and once passed, the stools turn
yellow-green.
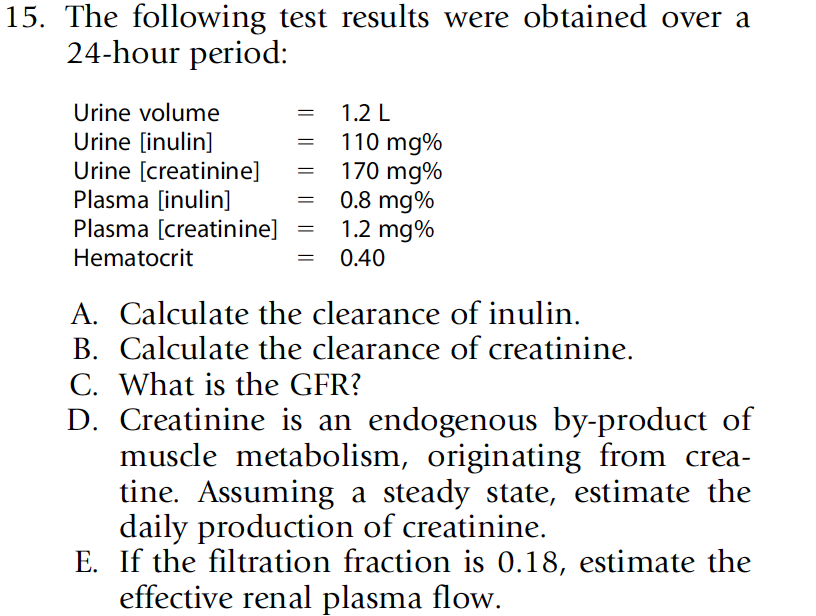
Baby stools vary in color and consistency due to their immature digestive system. If your baby is breastfed, their stools soon should be yellow liquid mixed with some particles. Until they start to eat solid foods, the consistency of the stools may range from very soft to loose and runny. If they're formula-fed, their stools usually will be tan or yellow in color. They will be firmer than a breastfed baby's, but should be no firmer than soft clay. Green stools are not unusual, either, and they should not cause you alarm.
Whether your baby is breastfed or bottle-fed, hard or very dry stools may be a sign that she is not getting enough
fluid or that she is losing too much fluid due to illness, fever, or heat. Once solids are introduced, hard stools might indicate that she's eating too many
constipating foods, such as cereal or cow's milk, before her system can handle them. (Whole
cow's milk is not recommended for babies under twelve months.)
(Whole
cow's milk is not recommended for babies under twelve months.)
Here are some other important points to keep in mind about bowel movements:
Occasional variations in color and consistency of the stools are normal. For example, if the digestive process slows down because of foods requiring more effort to digest (such as large amounts of cereal), the stools may become green; or if the baby is given supplemental iron, the stools may turn dark brown. If there is a minor irritation of the anus, streaks of blood may appear on the outside of the stools. However, if there are large amounts of blood, mucus, or water in the stool, call your pediatrician immediately. These symptoms may warrant attention from your doctor.
Because an infant's stools are normally soft and a little runny, it's not always easy to tell when a young baby has mild diarrhea. The telltale signs are a sudden increase in frequency (to more than one bowel movement per feeding) and unusually high liquid content in the stool.
 Diarrhea may be a sign of
intestinal infection, or it may be caused by a change in the baby's diet. If the baby is breastfeeding, they can even develop diarrhea because of a change in the
mother's diet.
Diarrhea may be a sign of
intestinal infection, or it may be caused by a change in the baby's diet. If the baby is breastfeeding, they can even develop diarrhea because of a change in the
mother's diet.The main concern with diarrhea is the possibility of dehydration. If fever is also present and your infant is less than three months old, call your pediatrician. If your baby is over three months and the fever lasts more than a day, check her urine output and rectal temperature; then report your findings to your doctor for consideration. Make sure your baby continues to feed frequently. As much as anything else, if they simply looks sick, let your doctor know.
The frequency of bowel movements varies widely among babies. Many pass a stool soon after each feeding. This is a result of the gastrocolic reflex, which causes the digestive system to become active whenever the stomach is filled with food.
By three to six weeks of age, some breastfed babies have only one bowel movement a week and still are normal. Breast milk leaves very little solid waste to be eliminated from the child's digestive system. Thus, infrequent stools are not a sign of constipation and should not be considered a problem as long as the stools are soft, and your infant is otherwise normal, gaining weight steadily, and nursing regularly. Babies with this breastfed stool variant usually have a large volume of stool if it has been a few days (so you should be prepared with lots of wipes to clean up).
Breast milk leaves very little solid waste to be eliminated from the child's digestive system. Thus, infrequent stools are not a sign of constipation and should not be considered a problem as long as the stools are soft, and your infant is otherwise normal, gaining weight steadily, and nursing regularly. Babies with this breastfed stool variant usually have a large volume of stool if it has been a few days (so you should be prepared with lots of wipes to clean up).
If your baby is formula-fed, they should have at least one bowel movement a day. If they have fewer than this and appear to be straining, they may be constipated. Check with your pediatrician for advice on how to handle this problem.
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Baby's first 24 hours | Pregnancy Birth and Baby
Baby's first 24 hours | Pregnancy Birth and Baby beginning of content5-minute read
Listen
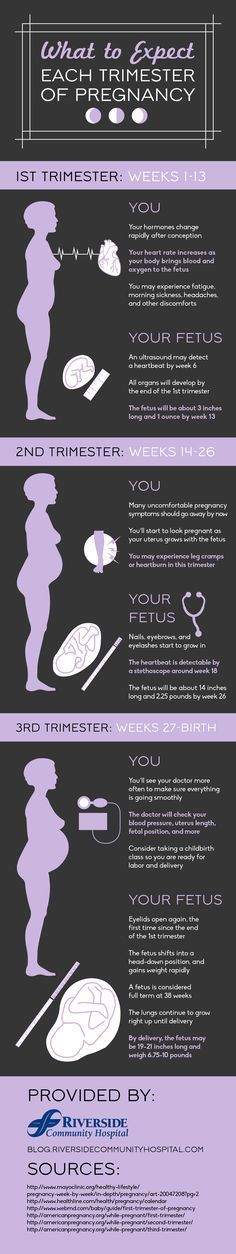
The first day of your new baby’s life is thrilling and exhausting for both of you. This page explains what your newborn baby can sense, and how the umbilical cord and placenta can be managed. It has general information for you if you have had a healthy, full-term pregnancy – 37 to 42 weeks’ gestation.
What will my newborn baby look like?
When your baby is born, their skin might be blue and mottled. They are likely to be covered in amniotic fluid, blood and vernix, which is a cheesy white substance. This is normal.
Their skin will start to become pink as they start to breathe — which is about a minute after birth. Your baby’s hands and feet may still appear blueish for several hours.
Your baby’s hands and feet may still appear blueish for several hours.
The amniotic fluid and the vernix are there because they were there in the womb. They are important for your baby to be able to smell and taste after birth. These familiar things help your baby to feel secure outside the womb.
Birth of the placenta and cutting the umbilical cord
After you have given birth to your baby, you will have more contractions that will help you deliver the placenta. Once this happens, the umbilical cord, which is connected to the placenta, will be clamped in two places and cut. Your support person might be invited to cut the cord.
Skin-to-skin contact
After a normal vaginal birth, your newborn baby will be put on your chest for skin-to-skin contact. Your baby needs sleep and food, and they need to feel secure and warm, so they need to feel your skin.
Doing this simple thing:
- reduces newborn crying
- helps start and sustain breastfeeding
- helps maintain your baby’s body temperature
After this first contact, they will be weighed, measured and observed to make sure they are healthy.
If you have a caesarean section, ask your midwife to make sure your baby has skin-to-skin contact with you as early as possible. It may be possible for you or your partner to hold your baby-skin-to skin in theatre and in recovery.
Feeding
Babies start to show signs of wanting to feed soon after birth and usually attach and suck at the breast about 50 minutes after birth. They may then breastfeed for an hour or more. Put your baby against your chest, and they will probably find your breast and start feeding. If that doesn’t happen, you can ask your midwife or a lactation consultant for help.
The first milk you make is called 'colostrum'. It’s thick and often yellowish, rather than pure white. It’s the ideal milk for your baby. Normally a small amount is produced — your baby’s tummy is just the size of a marble.
If they haven’t fed an hour or so after birth, try again a couple of hours later. You can also express some colostrum to feed to your baby on a spoon.
Weighing and measuring
After skin-to-skin contact and the first breastfeed, your midwife might offer to weigh your baby, and measure your baby’s length and head circumference. Your baby doesn’t need to be washed for at least 24 hours.
Vitamin K
At the time of weighing, your midwife will also offer to give your baby a vitamin K injection to prevent bleeding from vitamin K deficiency.
Cord blood collection if you are Rh negative
If your blood group is Rh negative, some blood will be taken from the umbilical cord to determine whether your baby’s blood group is compatible.
Sleeping
Your baby will stay with you so you can bond and respond easily to their needs. They’ll probably sleep soon after their first feed, and that might last 6 hours or so. They will probably sleep for more than half of their first day in the world.
Apgar scores
One of the main observations made after birth is called an Apgar score. It assesses your baby’s adjustment to life outside the womb. The Apgar score is measured at 1 minute and 5 minutes after birth while the baby is on your chest. Sometimes it is measured again at 10 minutes after birth.
The Apgar score is measured at 1 minute and 5 minutes after birth while the baby is on your chest. Sometimes it is measured again at 10 minutes after birth.
It records your baby’s heart rate, breathing, colour, muscle tone and reflexes. The maximum score is 10. A score of 7 or above usually means your baby is doing well. It is not an ability or intelligence test, and it doesn’t predict your baby’s health later in life.
What will my newborn baby see, hear, smell, taste and feel?
Your baby has been listening to your voice for the last half of your pregnancy and will recognise it when you speak to them after birth. Your partner or support person’s voice may also be familiar if they have also been talking near your baby. Your baby will feel secure when they hear your voices and may respond by turning their head towards you. Your baby will also be able to hear your heart beating as they did in the womb.
Your baby’s vision is blurred at birth but they will be able to focus on your face from about 30 centimetres away.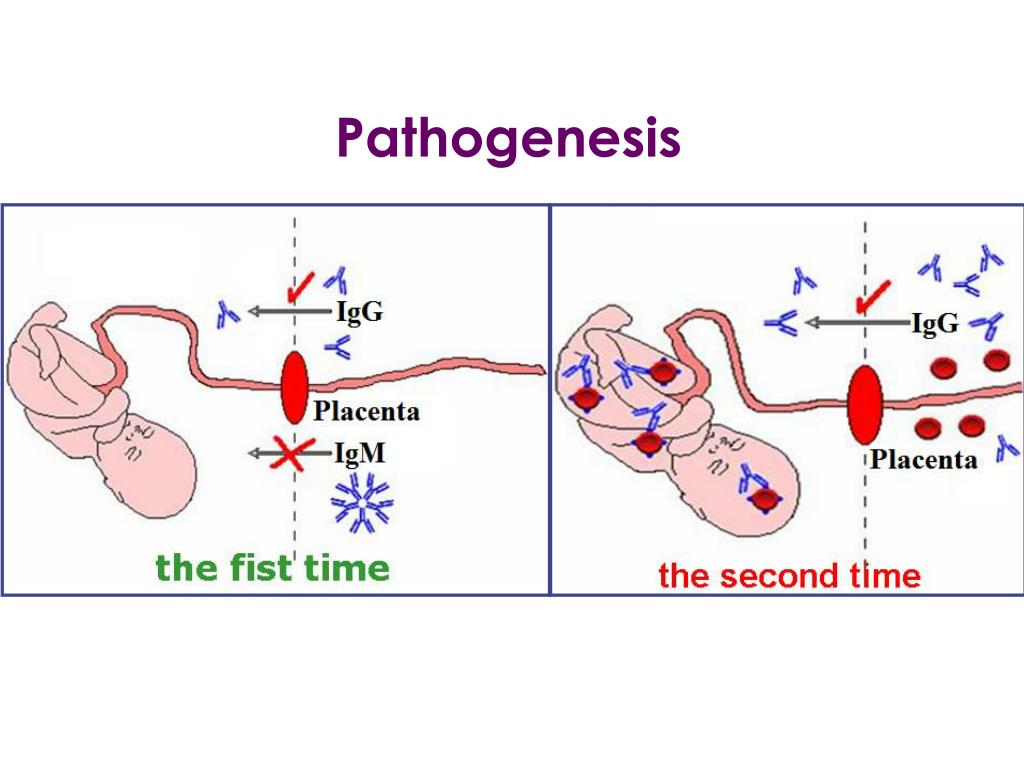 This is called the ‘cuddle distance’. It is roughly the distance from your breast to your face. Your baby will make the connection between what they hear and what they see.
This is called the ‘cuddle distance’. It is roughly the distance from your breast to your face. Your baby will make the connection between what they hear and what they see.
Your baby will smell and taste the amniotic fluid and your colostrum, which has a similar flavour.
Urine and meconium
Within the first 24 hours your baby will probably pass urine and meconium (newborn faeces) at least once. Meconium is black and sticky. Your baby’s poo will change colour and consistency over the next few days.
More information
You can call Pregnancy, Birth and Baby, 7 days a week on 1800 882 436 to speak with a maternal child health nurse to find out more.
Sources:
Cochrane (Early skin-to-skin contact for mothers and their healthy newborn infants), National Institute for Health and Care Excellence (NICE) (NICE Guideline CG37: Postnatal care up to 8 weeks after birth), World Health Organization (WHO) (Recommendations on newborn health), Raising Children Network (After baby is born: what to expect in the first few hours), Australian Breastfeeding Association (Breastfeeding timeline)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Mum's first few days after giving birth
- Mum's first 24 hours after birth
- Your baby in the first few days
- Birth injury (to the baby)
- What is kangaroo care?
Need more information?
Newborn clothes & dressing a newborn | Raising Children Network
How many clothes does a newborn need? And what newborn clothes are best? Get answers to these questions and more in our guide to dressing a newborn.
Read more on raisingchildren.net.au website
Newborns behaviour | Raising Children Network
Newborn behaviour baffling you? Here's all you need on newborns behaviour with articles, videos and resources on crying, colic and more.
Read more on raisingchildren.net.au website
Dressing a newborn
When dressing your newborn, here are a few things to consider, like which clothes to use, how to dress them and making sure the change table is safe.
Read more on Pregnancy, Birth & Baby website
Newborn bloodspot screening - MyDr.com.au
Newborn screening tests can detect rare but serious genetic or metabolic disorders in newborn babies.
Read more on myDr website
Newborn essentials
Here is a newborn's essentials checklist including vaccinations and immunisations, health checks, nappy changing and breastfeeding and bottle feeding.
Read more on Pregnancy, Birth & Baby website
Newborns development | Raising Children Network
Want to track newborns development? Here's all you need on newborn development with articles, videos and resources on growth, relationships and more.
Read more on raisingchildren.net.au website
Is my newborn safe? - MyDr.com.au
Dr Norman Swan explains the risks of COVID-19 to your newborn.
Read more on myDr website
Newborns sleep | Raising Children Network
Need help understanding newborn sleep? Here’s all you need on newborn sleep with articles, videos and resources on safe sleep, sleep habits, tiredness and more.
Read more on raisingchildren.net.au website
Newborns safety | Raising Children Network
Newborn safety stressing you? Here’s all you need on newborns safety with articles, videos and resources on first aid, CPR, equipment, car seats and more.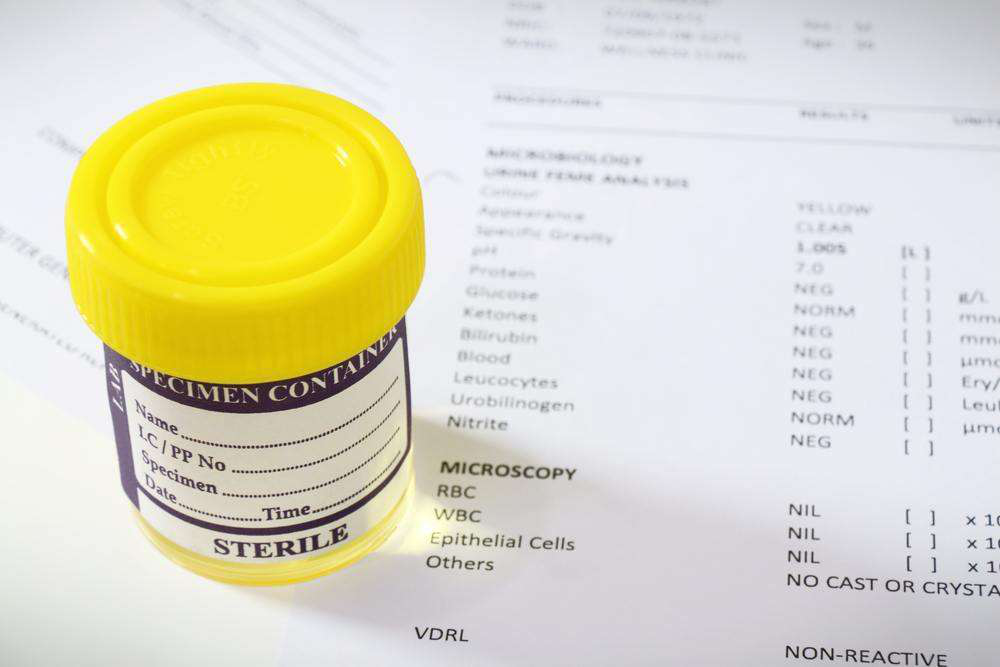
Read more on raisingchildren.net.au website
Bathing your newborn
Step-by-step infographic on how to give your newborn a bath.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.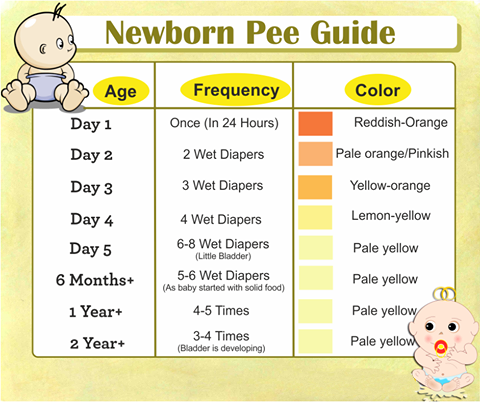
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Urination in newborns - how it should be | Mamovediya
For the first time, a child urinates sometimes during childbirth, and sometimes immediately after them. In general, the first urination in newborns occurs in the first 12 hours of life. However, in every 10th child, it can occur only on the 2nd and even on the 3rd day.
Therefore, if you gave birth at home and it so happened that the baby does not pee, wait 2-3 days after giving birth. If the situation has not changed during this time, invite a doctor.
Newborns produce little urine in the first 3 days of life, although their urinary system is well formed. What is the matter here has not been definitively established. But, of course, a certain role is played by the fact that the child outside the womb excretes water with the entire surface of the body, and so far receives little liquid.
Reduced urine output in newborns in the 1st week of life is called transient oliguria (Greek oligos - few, insignificant).
In the same week, all newborns develop another transitional state - uric acid infarction, which externally manifests itself as an unusual yellow-brick color of urine. It is cloudy and leaves a correspondingly colored stain on the diaper. By the end of the week, urine acquires its natural color and transparency.
The frequency of urination in full-term newborns in the 1st week of life is 4–5, and in preterm infants 8–13 times a day.
Usually, in healthy children, by the end of the 1st week, the daily urine output reaches an average of 209±26 ml. If by this time it is significantly less than the age norm (for example, it is only a third of it), you should observe the baby.
Reduced urine output is not always associated with kidney, bladder or ureter disease.
A child may develop a high temperature (38-39°C) if they are dressed too warmly, lying next to a radiator, or the room is very hot, all of which can lead to decreased urine output.
The same result occurs with a disorder of the stool - diarrhea, which is accompanied by large losses of fluid.
However, if the child is not overheated and his stools are normal, you should see a doctor.
The unusual color of urine should also alert you. It can be concentrated - very yellow. At the same time, diapers are also painted yellow, and the skin of the child in the place where the urine has got turns pink. An increased concentration of urine can be caused by the fact that the baby is not getting enough liquid. In this case, he needs to give more to drink.
If he drinks a lot and his urine is still concentrated, you should consult your doctor.
Newborns rarely experience acute urinary retention in the first days. At the same time, the bladder is full of it, stretched and clearly visible above the womb. Sometimes it even reaches the level of the navel.
The reasons for this may vary, but in any case, the baby will need urgent medical attention.
A combination of two symptoms may serve as a reason for an urgent visit to a doctor: 1) the child has not urinated for 2-3 days and 2) his bladder is empty.
Anuria, a severe disease characterized by such a combination of symptoms, can soon lead to a sharp deterioration in the child's condition. He will turn pale, become drowsy and lethargic, and will refuse to eat. Further, convulsions, coma are possible. Anuria is treated exclusively in a hospital.
In some pathologies of the urinary system, blood is found in the urine of a newborn. This symptom may also be associated with other diseases, such as hemorrhagic disease of the newborn.
However, the urine may turn reddish after taking certain drugs. Therefore, after consulting a doctor, you can not give the child medicine for some time to find out if it is to blame.
Quite rarely, in children in the first days of life, signs of hereditary metabolic pathologies may appear. At birth, the baby looks quite healthy, but after a few days (and more often months) he becomes drowsy and lethargic, he has vomiting, convulsions. And at the same time, an unusual smell of urine and body appears. It is associated with the smell of mice, sweaty feet, mustiness, maple syrup, rotting fish
You should consult a doctor without delay, because the treatment of hereditary fermentopathies, in order to be effective, must be started in the neonatal period, and the sooner the better.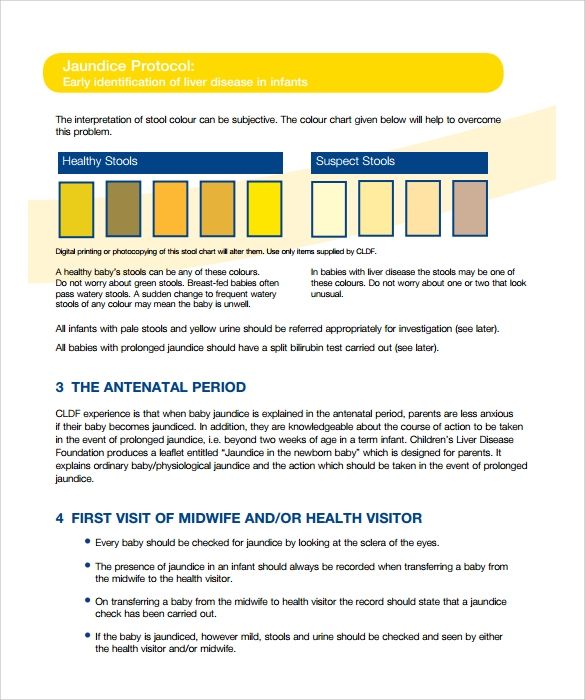 Otherwise, as a rule, the mental development of the baby suffers. And often the course of the disease acquires a life-threatening character.
Otherwise, as a rule, the mental development of the baby suffers. And often the course of the disease acquires a life-threatening character.
Sometimes it happens that the diaper on which the child urinates, when dry, turns black as pitch. Urine acquires the same color when standing. This is a sign of another hereditary fermentopathy - alkaptonuria. Often the disease does not give other symptoms. However, over time, alkapton (black pigment) can accumulate in the cartilage of the nose and ears, and then in the joints, the mobility of which will decrease because of this.
The disease is treatable if treated early.
Congenital diabetes mellitus, which is extremely rare in newborns, is characterized by characteristic signs. The child sucks a lot and greedily, urinates often and profusely, the diaper, having dried, becomes hard, as if starched.
The child may quickly develop a diabetic coma. Therefore, with such symptoms, you need to urgently consult a doctor.
It is important to pay attention to the color, consistency and turbidity of the baby's urine. It should be fairly clear and light, not cloudy, not orange or red.
The first days in the hospital - articles from the specialists of the clinic "Mother and Child"
Bogomolova Marina Vadimovna
Embryologist
Clinic "Mother and Child" St. Petersburg
Immediately after childbirth
Immediately after the birth of the baby is placed on the mother's stomach , then the umbilical cord is cut and the baby is applied to the mother's breast. Then the skin of the newborn is cleaned, its length and weight, head and chest circumference are measured. The doctor examines the birth canal, if necessary, sews up tears in the soft tissues of the birth canal, assesses the tone of the postpartum uterus, and helps the woman empty her bladder. But even after all these standard manipulations, the mother is not transferred to the postpartum ward, another for two to three hours, the puerperal stays in the maternity block . Why? In the first two hours after childbirth, some complications are possible, primarily uterine bleeding or an increase in blood pressure. Therefore, during these two hours, the mother lies on a stretcher or a bed in the maternity ward, since doctors and midwives are constantly there, and the operating room, in which case, is also located nearby. The child at this time is usually taken to the children's department, where he most often sleeps. And only two hours later, if everything is fine, the mother is transferred to the postpartum ward.
Why? In the first two hours after childbirth, some complications are possible, primarily uterine bleeding or an increase in blood pressure. Therefore, during these two hours, the mother lies on a stretcher or a bed in the maternity ward, since doctors and midwives are constantly there, and the operating room, in which case, is also located nearby. The child at this time is usually taken to the children's department, where he most often sleeps. And only two hours later, if everything is fine, the mother is transferred to the postpartum ward.
How does a woman feel at this time? Chills may occur, abdominal pain may occur, especially in multiparas.
What should a woman do at this time? Relax and unwind. Take shelter so as not to freeze, especially if chills appear. Place an ice pack on the uterus. If possible, ask the midwife to bring hot tea.
1st day after birth
Shortly after the woman is transferred to the postpartum ward, she will come to postnatal midwife . She will tell you about the arrangement of the department (where the shower, toilet, dining room are), about the daily routine (the time for visiting doctors, eating) and will help the young mother, if necessary, to empty the bladder using a catheter. If a woman lies together with the baby, then immediately after the transfer to the postpartum ward, the child will be brought to her. The midwife will help the mother to properly attach the baby to the breast and start breastfeeding. Then baby nurse will come and show you how to swaddle your baby and explain how to take care of him. Do not be afraid that after childbirth there will not be enough strength for the child: most newborns sleep most of the day and wake up only for feeding. In addition, in the maternity hospital, the child is usually washed and dressed by nurses, so that the woman will have enough time to relax. If there is no joint stay of mother and child in the maternity hospital, then every three hours they will bring him to the ward for feeding, and then take him back to the children's department.
She will tell you about the arrangement of the department (where the shower, toilet, dining room are), about the daily routine (the time for visiting doctors, eating) and will help the young mother, if necessary, to empty the bladder using a catheter. If a woman lies together with the baby, then immediately after the transfer to the postpartum ward, the child will be brought to her. The midwife will help the mother to properly attach the baby to the breast and start breastfeeding. Then baby nurse will come and show you how to swaddle your baby and explain how to take care of him. Do not be afraid that after childbirth there will not be enough strength for the child: most newborns sleep most of the day and wake up only for feeding. In addition, in the maternity hospital, the child is usually washed and dressed by nurses, so that the woman will have enough time to relax. If there is no joint stay of mother and child in the maternity hospital, then every three hours they will bring him to the ward for feeding, and then take him back to the children's department.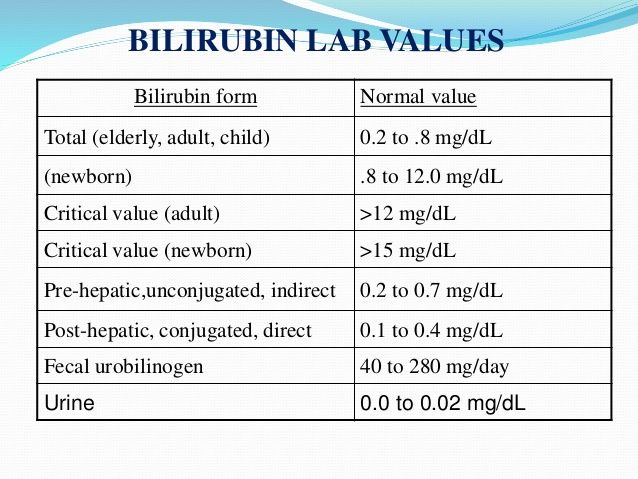 Over time, the woman herself will pick up and carry the child.
Over time, the woman herself will pick up and carry the child.
How does a woman feel at this time? On the first day after giving birth, women feel differently. Some experience an incredible elation (this is due to the release of endorphins into the blood - the hormones of pleasure), while others, on the contrary, feel very tired. Some want to call all their friends and announce the birth of a child, they are inspired, full of energy and ready to take care of the baby on their own. Other mothers want to be alone and come to their senses, they still do not have the strength to constantly be with the child.
What should a woman do at this time? In any case, immediately after childbirth, as after any heavy load, you need to restore strength: first eat, and then go to bed or just relax. By the way, the following situation is possible: the birth occurred in the evening or at night, and dinner time has already expired; therefore, in order not to starve, you need to bring something light for a snack (cookies, bread rolls) with you to the hospital in advance.
6 hours after birth, the mother can usually get out of bed.
In general, if the childbirth went without complications, then you should start getting up as early as possible, first with the help of a midwife, and then on your own.
It helps to improve blood circulation, normalize the functioning of the urinary system and intestines, and accelerate healing processes. In addition, very soon the baby will require more attention.
Important point: After childbirth, the tone of the bladder decreases, so the urge to urinate may be absent or it may become painful and frequent. However, you should go to the toilet at least four times a day. Urination can be caused reflexively by opening a tap with water, this helps many people a lot. In the absence of the desired effect, urine is removed by a catheter. Most often there is no stool on the first day after birth.
Next days
Every day, the mother will be examined by an obstetrician-gynecologist : he will evaluate the contraction of the uterus, the condition of the sutures and the amount of discharge, see if colostrum is secreted. The midwife will regularly measure the temperature, pulse, blood pressure and treat the external stitches with disinfectant solutions several times a day. Also, every day the baby will be watched by a pediatrician, after which he will tell his mother about the condition of the child. After a normal birth, a woman, as a rule, is discharged on the 3rd-4th day (after a caesarean section - on the 5th-6th).
The midwife will regularly measure the temperature, pulse, blood pressure and treat the external stitches with disinfectant solutions several times a day. Also, every day the baby will be watched by a pediatrician, after which he will tell his mother about the condition of the child. After a normal birth, a woman, as a rule, is discharged on the 3rd-4th day (after a caesarean section - on the 5th-6th).
How does a woman feel at this time?
After childbirth, a woman may experience pain in the abdomen due to uterine contractions, as well as slight muscle pain in different parts of the body. On the face and on the whites of the eyes, a “rash” may appear - pinpoint hemorrhages that appear due to the fact that small capillaries burst during attempts from tension. Blood pressure can be lowered, so dizziness is possible (to avoid it, you should get up smoothly, without sudden movements). There may be pain in the perineum, even if there were no tears and its incision (pain appears because the perineum was severely stretched during childbirth).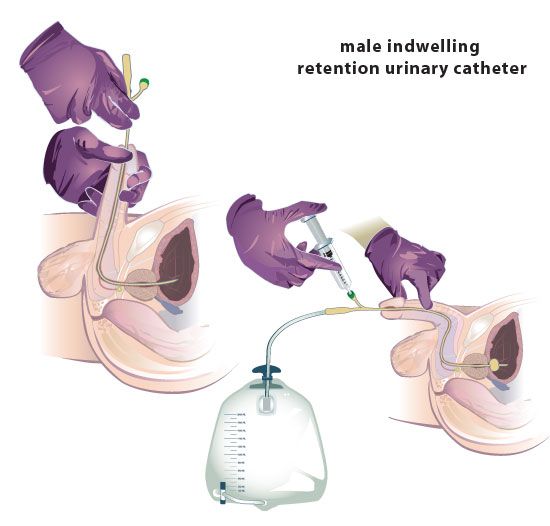 If the perineum is sutured, then it will not be possible to sit for at least the first two weeks. Sometimes after childbirth, varicose veins appear in the anus (hemorrhoids), which means discomfort in this place.
If the perineum is sutured, then it will not be possible to sit for at least the first two weeks. Sometimes after childbirth, varicose veins appear in the anus (hemorrhoids), which means discomfort in this place.
What should a woman do at this time? Mom needs to continue to rest and gain strength. And you should also follow the rules of personal hygiene: often change postpartum pads, do air baths for seams (if any), take a shower daily, wash yourself every time after a bowel movement. Well, the most important thing is to establish breastfeeding and learn how to take care of the baby in practice.
Time in the maternity hospital flies very quickly. Try to spend it usefully - restore your strength and acquire useful skills: at home, all this will be very useful to you!
REMINDER
Things to do at the maternity hospital
- Have a good rest: sleep all your free time and eat well.
- Get complete information about your child's condition: so ask your pediatrician all your questions.

- Establish contact with the child: therefore, spend as much time with the baby as possible, ideally - be with him all the time. Take the baby in your arms, unfold the diapers, carefully examine the baby without clothes.
- Learn how to care for your baby: so ask your baby nurse to show you how to wash your baby, how to change clothes, swaddle, change diapers, clean ears and nose, cut nails.
- Establish breastfeeding: To do this, feed your baby on demand. Ask the midwife to show you how to properly hold the baby at the breast, how to give and take away the breast.
Make an appointment
to the doctor - Bogomolova Marina Vadimovna
Clinic "Mother and Child" St. Petersburg
Cryopreservation of embryos, eggs, spermJoint consultation of a reproductive specialist and embryologistEmbryology
By clicking on the send button, I consent to the processing of personal data
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
To clarify the current cost, select a clinic
Clinical Hospital MD GROUP LAHTAK Clinic "Mother and Child" St. Petersburg
All directionsSpecialist consultations (adults)Specialist consultations (children's)Laboratory of molecular geneticsGeneral clinical examinationsProcedural roomOther gynecological operationsTelemedicine for adultsTherapeutic examinationsUltrasound examinations for adults
01.
Specialist consultations (adults)
02.
Consultations of specialists (children)
03.
Laboratory of molecular genetics
04.
General studies
05.
Procedure cabinet
06.
06.
other gynecological operations
07. 9000. 9000.
Adult Telemedicine
08.
Therapeutic Research
09.