Stomach black spots
Black Spot, a Novel Gastric Finding Potentially Induced by Proton Pump Inhibitors
1. el-Zimaity HM, Jackson FW, Graham DY. Fundic gland polyps developing during omeprazole therapy. Am J Gastroenterol 92: 1858-1860, 1997. [PubMed] [Google Scholar]
2. Jalving M, Koornstra JJ, Wesseling J, Boezen HM, DE Jong S, Kleibeuker JH. Increased risk of fundic gland polyps during long-term proton pump inhibitor therapy. Aliment Pharmacol Ther 24: 1341-1348, 2006. [PubMed] [Google Scholar]
3. Hongo M, Fujimoto K. Incidence and risk factor of fundic gland polyp and hyperplastic polyp in long-term proton pump inhibitor therapy: a prospective study in Japan. J Gastroenterol 45: 618-624, 2010. [PubMed] [Google Scholar]
4. Graham JR. Gastric polyposis: onset during long-term therapy with omeprazole. Med J Aust 157: 287-288, 1992. [PubMed] [Google Scholar]
5. Choudhry U, Boyce HW Jr, Coppola D. Proton pump inhibitor-associated gastric polyps: a retrospective analysis of their frequency, and endoscopic, histologic, and ultrastructural characteristics. Am J Clin Pathol 110: 615-621, 1998. [PubMed] [Google Scholar]
6. Cats A, Schenk BE, Bloemena E, et al.. Parietal cell protrusions and fundic gland cysts during omeprazole maintenance treatment. Hum Pathol 31: 684-690, 2000. [PubMed] [Google Scholar]
7. Stolte M, Bethke B, Rühl G, Ritter M. Omeprazole-induced pseudohypertrophy of gastric parietal cells. Z Gastroenterol 30: 134-138, 1992. [PubMed] [Google Scholar]
8. Driman DK, Wright C, Tougas G, Riddell RH. Omeprazole produces parietal cell hypertrophy and hyperplasia in humans. Dig Dis Sci 41: 2039-2047, 1996. [PubMed] [Google Scholar]
9. Parfitt JR, Driman DK. Pathological effects of drugs on the gastrointestinal tract: a review. Hum Pathol 38: 527-536, 2007. [PubMed] [Google Scholar]
10. Krishnamurthy S, Dayal Y. Parietal cell protrusions in gastric ulcer disease. Hum Pathol 28: 1126-1130, 1997. [PubMed] [Google Scholar]
11. Benzo J, Matos M, Milanes C, Arminio A, Stempel CA. Endoscopic findings in the upper digestive tract in patients with terminal chronic kidney failure.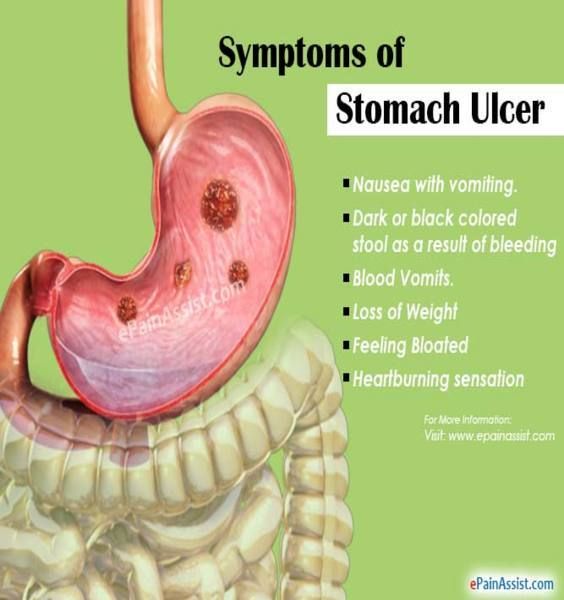 G E N 48: 34-38, 1994. (in Spanish, Abstract in English). [PubMed] [Google Scholar]
G E N 48: 34-38, 1994. (in Spanish, Abstract in English). [PubMed] [Google Scholar]
12. Sotoudehmanesh R, Ali Asgari A, Ansari R, Nouraie M. Endoscopic findings in end-stage renal disease. Endoscopy 35: 502-505, 2003. [PubMed] [Google Scholar]
13. McCormack TT, Sims J, Eyre-Brook I, et al.. Gastric lesions in portal hypertension: inflammatory gastritis or congestive gastropathy? Gut 26: 1226-1232, 1985. [PMC free article] [PubMed] [Google Scholar]
14. Toyonaga A, Iwao T, Shimotsuura Y, Tanikawa K. Endoscopic, histologic and haemodynamic studies on portal hypertensive gastric mucosa. J Gastroenterol Hepatol 4 (Suppl 1): 132-135, 1989. [PubMed] [Google Scholar]
15. D'Amico G, Montalbano L, Traina M, et al.. Natural history of congestive gastropathy in cirrhosis. The Liver Study Group of V. Cervello Hospital. Gastroenterology 99: 1558-1564, 1990. [PubMed] [Google Scholar]
16. Toyonaga A, Iwao T. Portal-hypertensive gastropathy. J Gastroenterol Hepatol 13: 865-877, 1998.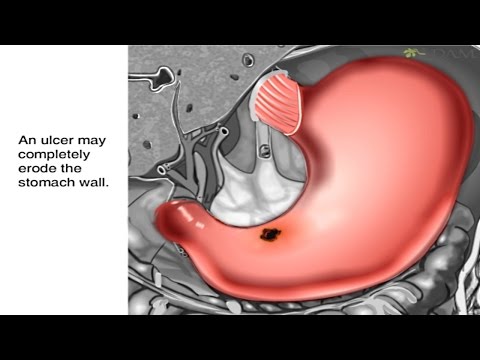 [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
17. Jabbari M, Cherry R, Lough JO, Daly DS, Kinnear DG, Goresky CA. Gastric antral vascular ectasia: the watermelon stomach. Gastroenterology 87: 1165-1170, 1984. [PubMed] [Google Scholar]
18. Ward EM, Raimondo M, Rosser BG, Wallace MB, Dickson RD. Prevalence and natural history of gastric antral vascular ectasia in patients undergoing orthotopic liver transplantation. J Clin Gastroenterol 38: 898-900, 2004. [PubMed] [Google Scholar]
19. Lagoudianakis EE, Genetzakis M, Tsekouras DK, et al.. Primary gastric melanoma: a case report. World J Gastroenterol 12: 4425-4427, 2006. [PMC free article] [PubMed] [Google Scholar]
20. Yamamura K, Kondo K, Moritani S. Primary malignant melanoma of the stomach: report of a case. Surg Today 42: 195-199, 2012. [PMC free article] [PubMed] [Google Scholar]
21. Jelincic Z, Jakic-Razumovic J, Petrovic I, Cavcic I, Unusic J, Trotic R. Primary malignant melanoma of the stomach. Tumori 91: 201-203, 2005. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
22. Antaki F, Irwin BC, Levi E. Rare occurrence of gastric pseudomelanosis. Gastrointest Endosc 69: 599; Author reply 599-600, 2009. [PubMed] [Google Scholar]
23. Weinstock LB, Katzman D, Wang HL. Pseudomelanosis of stomach, duodenum, and jejunum. Gastrointest Endosc 58: 578, 2003. [PubMed] [Google Scholar]
24. Matsuo S, Imai E, Horio M, et al.. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53: 982-992, 2009. [PubMed] [Google Scholar]
25. Kimura K, Takemoto T. An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy 1: 87-97, 1969. [Google Scholar]
26. Haruma K, Kato M, Inoue K, Murakami K, Kamada T In: Ien no Kyoto Bunrui. Nihon Medical Center, 2014: 91-93 (in Japanese). [Google Scholar]
27. Miyamoto M, Haruma K, Okamoto T, Higashi Y, Hidaka T, Manabe N. Continuous proton pump inhibitor treatment decreases upper gastrointestinal bleeding and related death in rural area in Japan. J Gastroenterol Hepatol 27: 372-377, 2012. [PubMed] [Google Scholar]
J Gastroenterol Hepatol 27: 372-377, 2012. [PubMed] [Google Scholar]
28. Synnerstad I, Holm L. Omeprazole induces high intraglandular pressure in the rat gastric mucosa. Gastroenterology 112: 1221-1230, 1997. [PubMed] [Google Scholar]
29. Kes P. Serum gastrin concentration in chronic renal failure. Acta Med Croatica 46: 47-58, 1992. [PubMed] [Google Scholar]
30. Okahata H, Nishi Y, Muraki K, et al.. In vitro study of antral gastrin biosynthesis in response to weaning and corticosteron acetate in rats. Acta Endocrinol (Copenh) 111: 539-545, 1986. [PubMed] [Google Scholar]
Pseudomelanosis of the stomach | QJM: An International Journal of Medicine
Journal Article
M.C. Alraies,
M.C. Alraies
Search for other works by this author on:
Oxford Academic
PubMed
Google Scholar
A. H. Alraiyes,
H. Alraiyes,
A.H. Alraiyes
Search for other works by this author on:
Oxford Academic
PubMed
Google Scholar
M. Baibars,
M. Baibars
Search for other works by this author on:
Oxford Academic
PubMed
Google Scholar
K. Shaheen
K. Shaheen
Search for other works by this author on:
Oxford Academic
PubMed
Google Scholar
QJM: An International Journal of Medicine, Volume 107, Issue 1, January 2014, Pages 83–84, https://doi.org/10.1093/qjmed/hct015
Published:
24 January 2013
Navbar Search Filter QJM: An International Journal of MedicineThis issueMedicine and HealthBooksJournalsOxford Academic Mobile Microsite Search Term
Close
Navbar Search Filter QJM: An International Journal of MedicineThis issueMedicine and HealthBooksJournalsOxford Academic Microsite Search Term
Advanced Search
A 83-year-old woman presented with 1-day epigastric abdominal pain with black stool. She denied any chest pain, dyspnea, hematemesis, hematochezia, dizziness or fever. The patient’s medical history included diabetes mellitus, hypertension, coronary artery disease status after coronary artery bypass surgery, hypothyroidism and chronic renal failure. Current medications included hydrochlorothiazide, turesamide, isosorbide mononitrate, levothyroxine, esomeprazole, atorvastatin, Humulin N insulin, metoprolol, hydralazine, diltiazem and aspirin. In addition, the patient had a history of normocytic anemia and had taken ferrous sulfate for about 2 years. On examination, vital signs were stable with unremarkable physical findings. On presentation, hemoglobin was 8.0 g/dl and hematocrit 26%.
She denied any chest pain, dyspnea, hematemesis, hematochezia, dizziness or fever. The patient’s medical history included diabetes mellitus, hypertension, coronary artery disease status after coronary artery bypass surgery, hypothyroidism and chronic renal failure. Current medications included hydrochlorothiazide, turesamide, isosorbide mononitrate, levothyroxine, esomeprazole, atorvastatin, Humulin N insulin, metoprolol, hydralazine, diltiazem and aspirin. In addition, the patient had a history of normocytic anemia and had taken ferrous sulfate for about 2 years. On examination, vital signs were stable with unremarkable physical findings. On presentation, hemoglobin was 8.0 g/dl and hematocrit 26%.
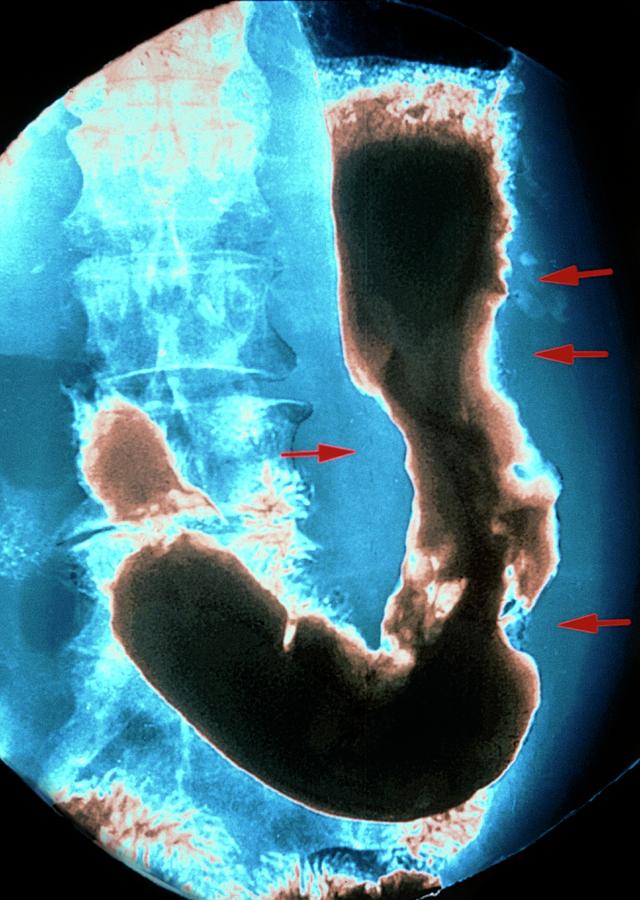
Upper endoscopy revealed a speckled pattern of black pigmentation seen throughout the stomach and duodenum (Figure 1a). Biopsy specimens confirmed pigment of pseudomelanosis gastri and duodeni located in stromal macrophages of the villous tips (Figure 1b). Iron staining (Perl’s staining) was negative for presence of iron sulfide granules in the lamina propria. These findings were consistent with pseudomelanosis.
These findings were consistent with pseudomelanosis.
Figure 1.
Open in new tabDownload slide
(a) Upper endoscopy showing speckled pattern of black pigmentation throughout the stomach due pseudomelanosis. (b) Duodenal biopsy showing villi with brownish-black pigment located within the apical portion of the villi using hematoxylin-eosin (H&E) stain at 100× (A) and 200× (B). Gastric antrum biopsy showed again brownish-black pigment using H&E stain (C). However, Perl’s iron stain did not show blue staining which reflects absence of iron deposition (D).
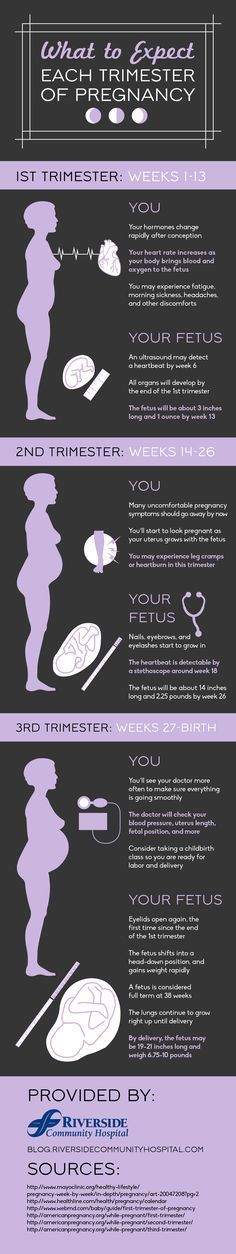
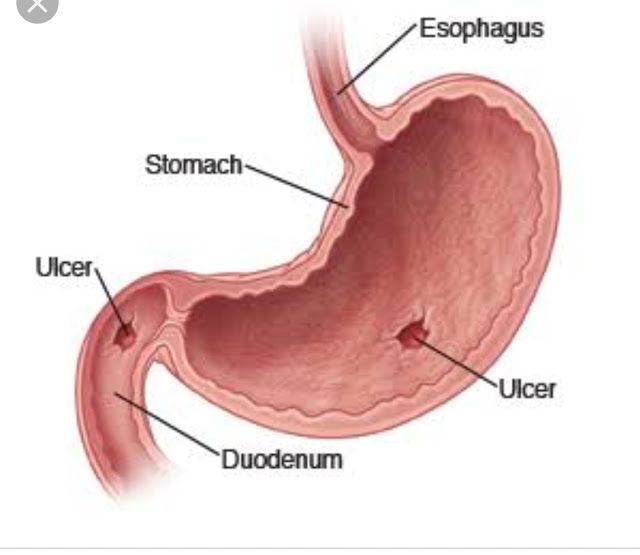
Pseudomelanosis of the gastrointestinal tract manifests itself on endoscopy as discrete, flat, small, black spots in a speckled pattern on a flat mucosa and is associated with melanin, iron or lipofuscin uptake by macrophages in the subepithelial lamina propria often at the tips of villi. Chronic renal disease, hypertension, diabetes mellitus, oral iron supplementation, antihypertensive medications (especially with hydralazine, thiazide diuretics, furosemide and beta-blockers) and gastric hemorrhage have been most frequently described in association with this entity. Although no definite etiology or mechanism has been traced, it is thought that the large size of the particles that cause pigmentation is one explanation for the difficulty in absorption of and subsequent pigmentation by melanin, iron and lipofuscin.1,2 In our case, the extensive, intense pigmentation was likely caused by the large number of factors present that are known to be associated with pseudomelanosis, including chronic renal insufficiency, diabetes mellitus and treatment with antihypertensive medications (primarily hydralazine and turosemide), as well as therapy with iron supplements, despite the fact that 20% of cases do not stain for iron. Finally, pseudomelanosis is not premalignant and has no clinical significance.3
Although no definite etiology or mechanism has been traced, it is thought that the large size of the particles that cause pigmentation is one explanation for the difficulty in absorption of and subsequent pigmentation by melanin, iron and lipofuscin.1,2 In our case, the extensive, intense pigmentation was likely caused by the large number of factors present that are known to be associated with pseudomelanosis, including chronic renal insufficiency, diabetes mellitus and treatment with antihypertensive medications (primarily hydralazine and turosemide), as well as therapy with iron supplements, despite the fact that 20% of cases do not stain for iron. Finally, pseudomelanosis is not premalignant and has no clinical significance.3
Our patients received two units of blood during hospitalization. A few days later, she was discharged in a stable condition. She reported no recurrent bleeding on her subsequent follow-ups.
Conflict of interest: None declared.
1
Weinstock
LB
,
Katzman
D
,
Wang
HL
.
Pseudomelanosis of stomach, duodenum, and jejunum
,
Gastrointest Endosc
,
2003
, vol.
58
pg.
578
2
Cheng
CL
,
Chen
PC
,
Chen
TC
.
Pseudomelanosis duodeni: case report
,
Chang Gung Med J
,
2000
, vol.
23
(pg.
372
-
6
)
3
,
Jersild
RA
Jr.
.
Further characterization of the pigment in pseudomelanosis duodeni in three patients
,
Gastroenterology
,
1988
, vol.
95
(pg.
177
-
82
)
© The Author 2013. Published by Oxford University Press on behalf of the Association of Physicians. All rights reserved. For Permissions, please email: [email protected]
© The Author 2013. Published by Oxford University Press on behalf of the Association of Physicians. All rights reserved. For Permissions, please email: journals. [email protected]
[email protected]
Issue Section:
Clinical pictures
Download all slides
Advertisement
Citations
Altmetric
More metrics information
Email alerts
Article activity alert
Advance article alerts
New issue alert
Receive exclusive offers and updates from Oxford Academic
Citing articles via
-
Latest
-
Most Read
-
Most Cited
MIF is a Common Genetic Determinant of COVID-19 Symptomatic Infection and Severity
Clostridium perfringens bacteremia and intravascular hemolysis
Primary amyloidosis presenting as unusual cutaneous nodules diagnosed by 18F-FDG PET/CT aided biopsy: a case report
Synovial Chondromatosis
Hoffman Myopathy & Hypothyroidism
Advertisement
ᐉ Black dots on the human stomach - CLICK HERE
Black dots on the human body appear in the same way as on the face. Active production of sebum and non-exfoliated skin particles clog pores and turn black upon contact with oxygen.
Active production of sebum and non-exfoliated skin particles clog pores and turn black upon contact with oxygen.
Contents:
- Causes of black spots on the abdomen
- Puberty
- Menopause
- Hereditary factor
- Poor hygiene
- Wrong cosmetics
- Prevention of black spots on the stomach
Black spots on the human stomach is a rather unpleasant problem, but it can be dealt with.
Causes of black spots on the stomach
0003
Most often, during adolescence, the hormonal background changes in adolescents and, at the same time, the sebaceous glands begin to become active.
They and excess dead skin cells close the pores and form black dots on the human abdomen.
Menopausal period
Back to contents
The same as in transitional age. When menopause comes, a woman's hormones are rearranged, the balance is disturbed.
Hence the increased oiliness of the skin and the appearance of black spots.

During puberty, you just need to cleanse the skin, do not abuse harmful products, do not squeeze problem areas. Then the black dots will go away by themselves.
Hereditary factor
Back to contents
Skin problems are often inherited. The genes that carry information in our body are passed on to children.
If you have problematic skin, you may be deficient in vitamins A and B.
Since such information is in the genes, it can be easily passed on to offspring.
Hereditary blackheads are more difficult to deal with. And sometimes it takes most of life. But such people live well and take care of their skin.
If you see pimples or blackheads that persist for a long time, see your doctor. Perhaps it is hereditary.
Poor Hygiene
Back to Contents
If you sweat a lot and don't shower often, then blackheads on your belly are a small problem that could be.
To get rid of black spots on the body, you need to follow some rules:
- Wash your body at least twice a day
- Change sweaty clothes
- Do not walk in a wet swimsuit
- Use non-comedogenic shower gels
- Shower Gel
- Body Scrubs
- Body Cream
- Choose cosmetics according to your skin type.
- Use2 clean towels
In addition to all of the above, experts advise visiting a bath or sauna at least 2 times a week.
Visit Vsebani.com.ua right now and choose the best bath or sauna in your city. Without neglecting these rules, you will protect your skin from various types of rashes. And your skin will be healthy.
Wrong cosmetics
Back to content
Incorrectly selected body care cosmetics can cause irritation and blackheads.
To avoid such precedents, try to choose products suitable for your skin type.
Belly Black Spot Treatments:
Using body scrubs, you can effectively remove black spots in a bath or sauna. The effect will be maximum. Go to the site Vsebani.com.ua, and you will get the best bath or sauna.
The effect will be maximum. Go to the site Vsebani.com.ua, and you will get the best bath or sauna.
Prevention of black spots on the stomach
Back to content Even oily skin needs moisture.
Take care of your skin and be healthy!
Back to content
What causes black dots on a dog's skin?
The owner of the animal can be very excited that black marks of various shapes and sizes have appeared on the skin of the dog. These can be small black dots resembling human comedones, located on the face, abdomen or body, dark spots all over the body, scaly marks on the skin under the coat, and much more.
Causes of dark marks
The appearance of various marks and marks on the skin of a dog can be caused by the following conditions and diseases:
- Lentigo. Traces of this disease are found on the abdomen and paws of the animal, less common on other parts of the body.
 Lentigo is a cosmetic skin defect, there is no effective treatment.
Lentigo is a cosmetic skin defect, there is no effective treatment. - Dermatophytoses. These are fungal infections that appear on the dog's body with spots of various shapes and sizes. Most often they form dark spots on the skin of a dog, located on the muzzle, neck, paws and in the anal area. They are mainly characterized by the appearance of scaly, inflamed, crusted or weeping marks, characterized by severe itching. The dog actively scratches the painful areas, spreading the infection throughout the body and introducing additional various bacteria, which further aggravates the situation.
- Acute weeping dermatitis. It appears with strong combing of the skin by dogs and the introduction of bacterial microflora into the wounds. Traces of scratching cause severe itching, the dog itches and spreads the infection even more. Because of this, dark spots appear in the groin and in other areas, covered with a crust due to constant injury. Also, pus accumulates on the combs and ichor can flow.
- Dark spots on a dog's abdomen can be comedones. These are enlarged and clogged with sebaceous plugs of the mouth of the sebaceous glands or inflamed hair follicles. An outwardly harmless skin condition is the result of serious endocrine problems of the body or a secondary symptom of demodicosis. In miniature schnauzers, primary comedones - black dots on the back - are a cosmetic defect that does not need treatment, which is genetically characteristic of this breed.
- Black spots on the skin of a pet can be a manifestation of an allergy - to food, cosmetics, medications and much more.
- Demodicosis covers the paws of the animal with a reddish rash similar to scabies. This microscopic mite can provoke severe itching and scratching, in place of which dark spots appear, covered with a dry, flaky crust.
- seborrhea. With this disease, dark marks appear on the skin, the coat deteriorates, fades, falls off, breaks and falls out. Scales, dandruff are formed on the skin, accompanied by skin irritation and itching.

- Hormonal disorders. They are usually accompanied by increased greasiness of the skin, the appearance of an unpleasant odor from the animal, spots on the skin and itching, as well as baldness.
Since there are many reasons for the appearance of black marks on the skin of a dog, and they are all different, the most important action of the owner of the animal is to visit the veterinary clinic to establish the correct diagnosis.
Treatment of diseases
In order to know what to do if various spots appear on the skin of a dog, it is necessary to undergo a full examination by a veterinarian. Only an accurate diagnosis can be the basis for treatment, as various diseases require specialized therapy.
The appearance of lichen and other forms of dermatophytosis will require the use of complex measures. The dog will need to be bathed using special shampoos that cleanse the skin of flaking and relieve inflammation, as well as use antifungal drugs prescribed by a doctor.
Dark spots in the groin, or comedones, indicate disruption of the endocrine system, therefore, to get rid of them, it is necessary to cure the underlying disease. Hairless dog breeds are particularly susceptible to this condition, as are miniature schnauzers, dachshunds, poodles, Samoyeds, and the adorable Japanese Akita Inu.
If the dark spots on the dog's stomach are not associated with the disease, but are only a cosmetic defect, it is not necessary to treat them. However, black dots on the back or on other areas can be removed with the help of special shampoos for animals containing the active ingredient - benzoyl peroxide. They perfectly cleanse the skin, eliminate blockage of the sebaceous glands and increased oiliness of the skin.
Infected skin areas are treated with antibiotics. Only a doctor should prescribe such funds, since drugs for people are not always allowed to be used for animals, and the dosage is selected individually according to the weight and age of the dog.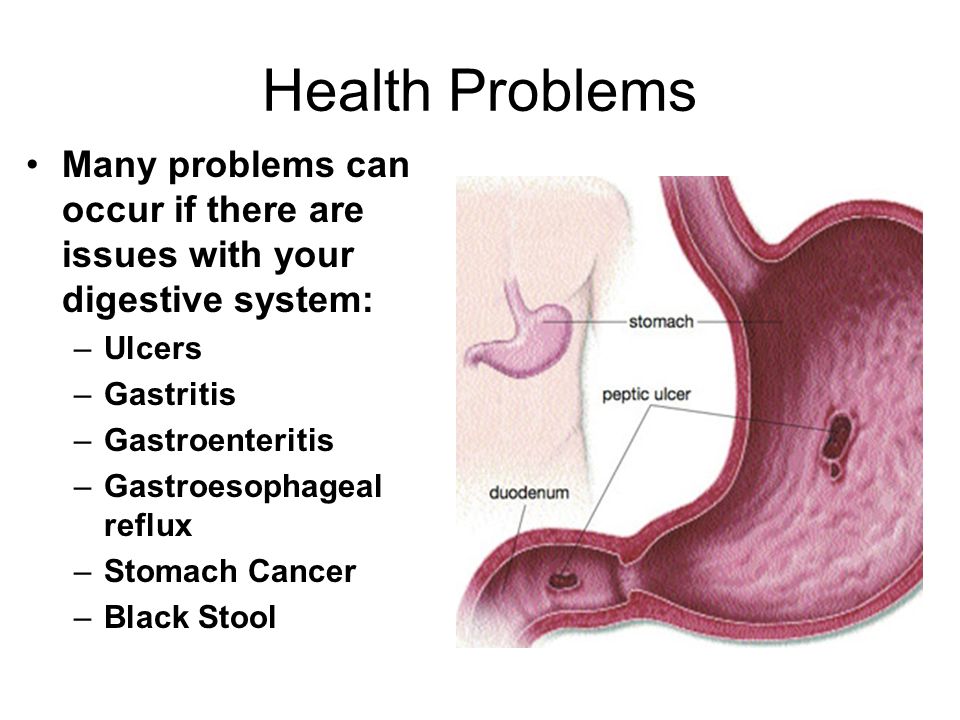
 C. Alraies, A.H. Alraiyes, M. Baibars, K. Shaheen, Pseudomelanosis of the stomach, QJM: An International Journal of Medicine, Volume 107, Issue 1, January 2014, Pages 83–84, https://doi.org/10.1093/qjmed/hct015
C. Alraies, A.H. Alraiyes, M. Baibars, K. Shaheen, Pseudomelanosis of the stomach, QJM: An International Journal of Medicine, Volume 107, Issue 1, January 2014, Pages 83–84, https://doi.org/10.1093/qjmed/hct015