Blood loss miscarriage
Miscarriage - Atlanta Gynecology and Obstetrics
Loss of pregnancy before 20 weeks is called a miscarriage. Spontaneous miscarriage is the most common complication of early pregnancy and the rate decreases as the pregnancy progresses.
Miscarriages occur in 8-20% of clinically-recognized pregnancies:
- 80% of these happen in the first 12 weeks of pregnancy
- The rate of loss for unrecognized or “chemical pregnancies” is 13-26%
- The overall risk of loss after 15 weeks is relatively low
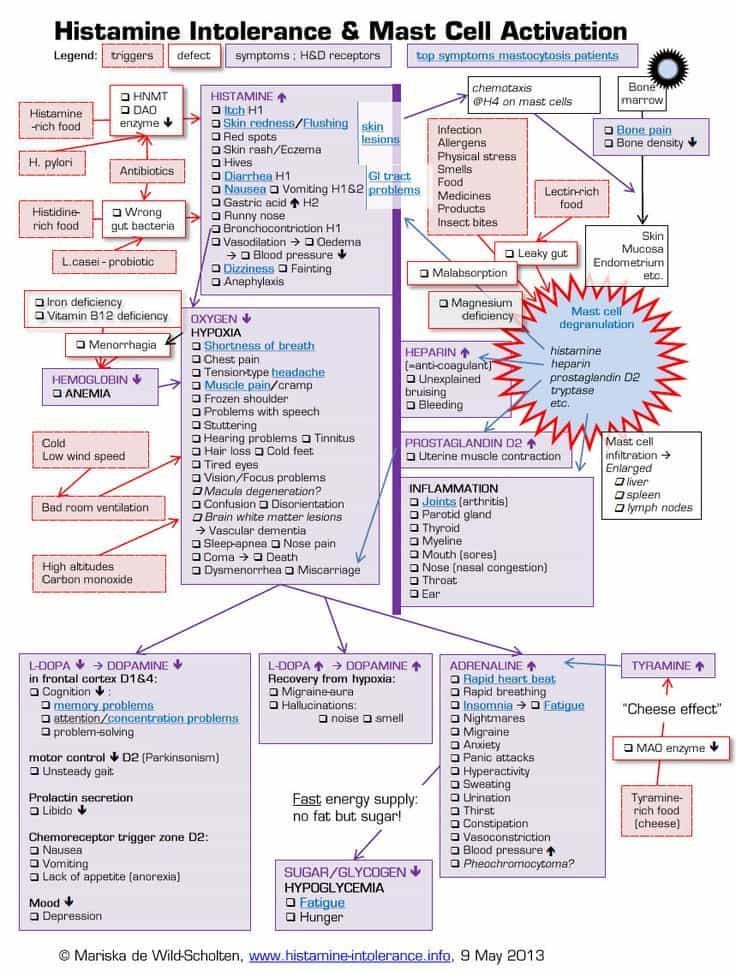
Causes of miscarriage
Though it is difficult to identify what causes all miscarriages, most pregnancy losses are thought to be due to chromosomal defects.
- Chromosomal Abnormalities > 60%
- Maternal: Structural Abnormalities
- Uterine Fibroids, Septums, and Adhesions
- Trauma
- Acute Infections
- Blood Disorders (Thrombophilia)
- Unexplained
Loss of viability of the pregnancy usually occurs between 6-12 weeks. Recognition may not occur until weeks later. The course of treatment that you take will depend on your current condition, your desires, the size of your pregnancy, and your provider recommendations.
Factors associated with miscarriage
There can be many factors that affect the probability of having a miscarriage. In many cases, there is more than one factor that comes into play. If you know what these factors are, you can be more cautious.
- Age: Miscarriage risk increases with age. The risk can be as high as 40% at 40 years old and 80% after 45 years old
- Previous miscarriage: The rate of miscarriage increases with the number of previous miscarriages: 20% after one, 28% after two consecutive, and 43% after three or more consecutive losses
- Smoking: Increases the risk of loss
- Alcohol use: Studies have been inconsistent in proving that alcohol can cause an increased rate of pregnancy loss.
 One study indicated that there was an increase in miscarriages among women who drank more than 3 drinks a day
One study indicated that there was an increase in miscarriages among women who drank more than 3 drinks a day - Cocaine use
- Non-steroid anti-inflammatories (NSAIDs: Ibuprofen, Advil, Motrin): May be associated with an increased risk of miscarriage if used around the time of conception. The prostaglandin in NSAIDs may interfere with proper implantation
- Caffeine: The risks of miscarriage increase with high levels of consumption (>300mg /day)
Miscarriage at home
You may first note mild vaginal spotting and/or cramping. This bleeding and cramping will increase, at which point you may expel the tissue of the pregnancy. During the miscarriage, you may bleed heavily with large clots, soaking a pad every 10-20 minutes. The cramping may be significant. Tylenol and a heating pad are okay to use at this time. You should call the office or the on-call doctor if the heavy bleeding does not improve after two hours.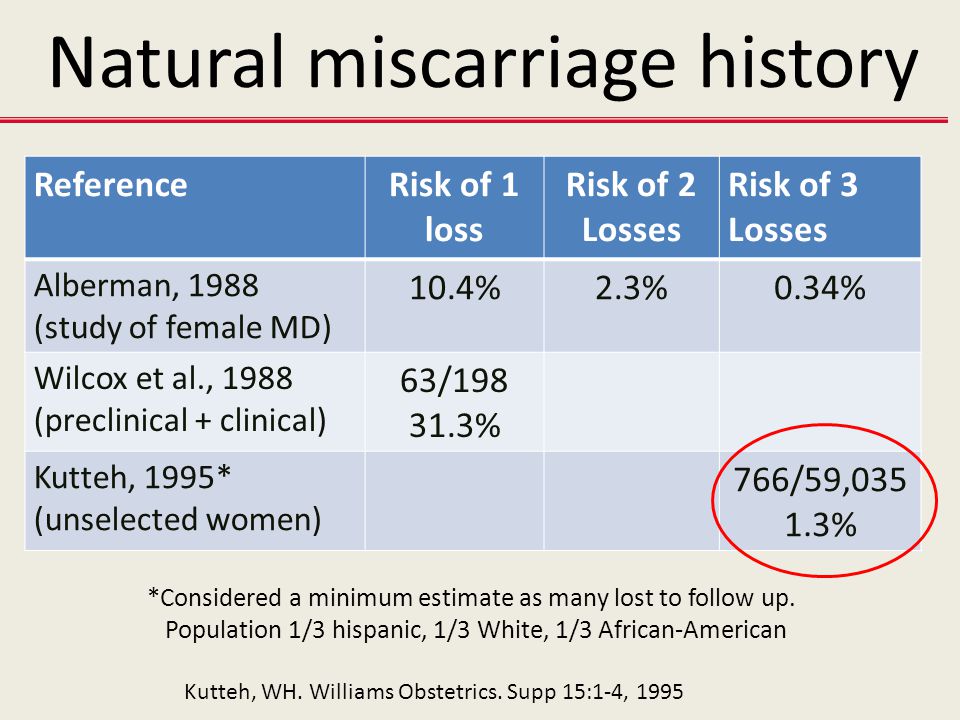
Once you have passed the pregnancy tissue, you will notice a decrease in bleeding and cramping. You may collect the passed tissue and store it in a clean and dry container and bring it to the office so that it may be sent out for pathological identification. You may call the office or the on-call doctor at any time for direction and advice.
Office Number: 404-299-9724 | After Hours Number: 404-487-2450
D&C at the hospital
A D&C is a surgical procedure performed under anesthesia to remove tissue from the uterus that has not started to or that has not entirely come out.
A D&C is an outpatient procedure that lasts for about 15-20 minutes. You usually go home about 1-2 hours after the procedure is completed. Most women return to light duties and activity the next day. Cramping and bleeding are common after a D&C. You may have bleeding for up to 2 weeks after your procedure.
Alternatively, we offer appropriate candidates a procedure called a Mechanical Vacuum Aspiration (MVA).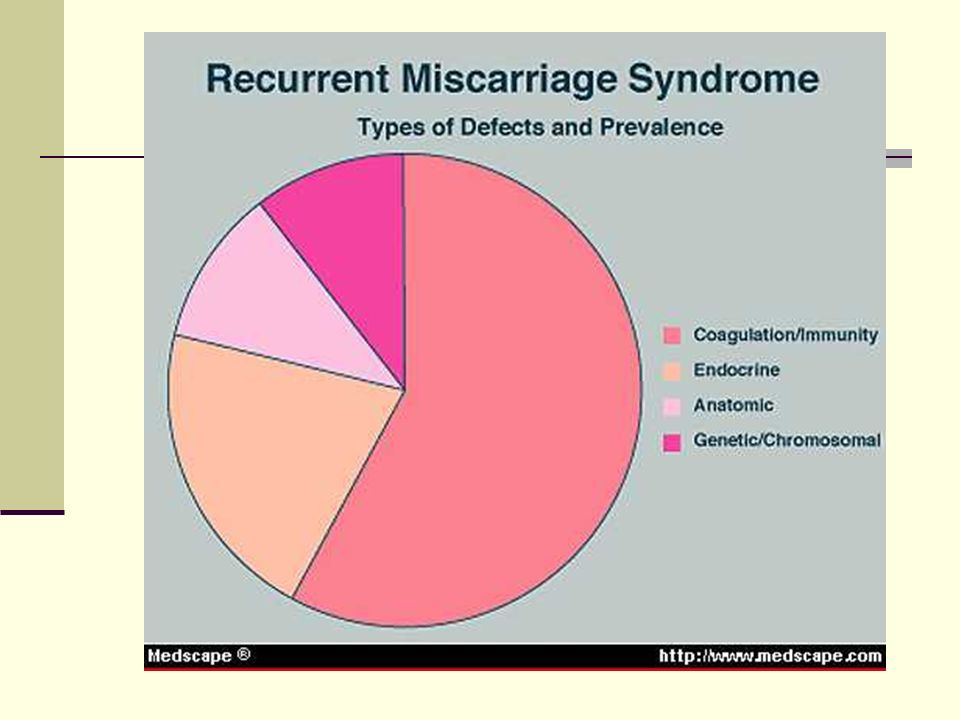 This procedure is similar to the D&C, but it can be done in the office under local anesthesia. Recovery and warning signs are similar to those of the D&C procedure.
This procedure is similar to the D&C, but it can be done in the office under local anesthesia. Recovery and warning signs are similar to those of the D&C procedure.
With either of these procedures, we recommend that you do not put anything in the vagina (no tampons, douching, or intercourse) until you are seen again in the office.
Warning signs after a miscarriage or D&C
Call the office if you have:
- Temperature > 100.4
- Nausea and vomiting for > 12 hours
- Increasing pain or bleeding
- Foul-smelling vaginal discharge
Coping with the loss of pregnancy
Emotional healing can take longer than physical healing. Grief after a pregnancy loss is a normal response. In the days and weeks after your pregnancy loss, you may experience a loss of appetite, emotional changes, irritability, sleep disturbances, and inability to focus on daily tasks. This is all normal and should resolve in a few weeks or months. If you find that these symptoms are severe or that you are unable to cope with these feelings, please call and make an appointment to talk to a provider in our practice. We will be able to help you and make any other referrals you may need.
If you find that these symptoms are severe or that you are unable to cope with these feelings, please call and make an appointment to talk to a provider in our practice. We will be able to help you and make any other referrals you may need.
The next pregnancy
Your next period should come within 4-6 weeks after your miscarriage. We recommend that you use contraception until after you have had a normal period. You may continue prenatal vitamins during and after this time. You may also discuss birth control at your post-miscarriage visit if you do not desire to become pregnant again.
What Does a Miscarriage Look Like? Bleeding, Duration, and More
A miscarriage is a spontaneous pregnancy loss before 20 weeks of gestation. Some 8 to 20 percent known pregnancies end in miscarriage, with the majority happening before the 12th week.
The signs and symptoms of miscarriage vary from person to person. Symptoms may also vary depending on how far along you are. For example, a fetus at 14 weeks will be much larger than a fetus at 5 weeks of gestation, so there may be more bleeding and tissue loss with a later miscarriage.
For example, a fetus at 14 weeks will be much larger than a fetus at 5 weeks of gestation, so there may be more bleeding and tissue loss with a later miscarriage.
Miscarriage symptoms may include:
- spotting or bleeding from the vagina
- abdominal cramping or pain in the lower back
- passage of tissue, fluid, or other products from the vagina
Read on to learn more about identifying a miscarriage and what to do if you suspect you’re experiencing one.
Bleeding may start as light spotting, or it could be heavier and appear as a gush of blood. As the cervix dilates to empty, the bleeding becomes heavier.
The heaviest bleeding is generally over within three to five hours from the time heavy bleeding begins. Lighter bleeding may stop and start over one to two weeks before it completely ends.
The color of the blood can range from pink to red to brown. Red blood is fresh blood that leaves the body quickly. Brown blood, on the other hand, is blood that’s been in the uterus a while.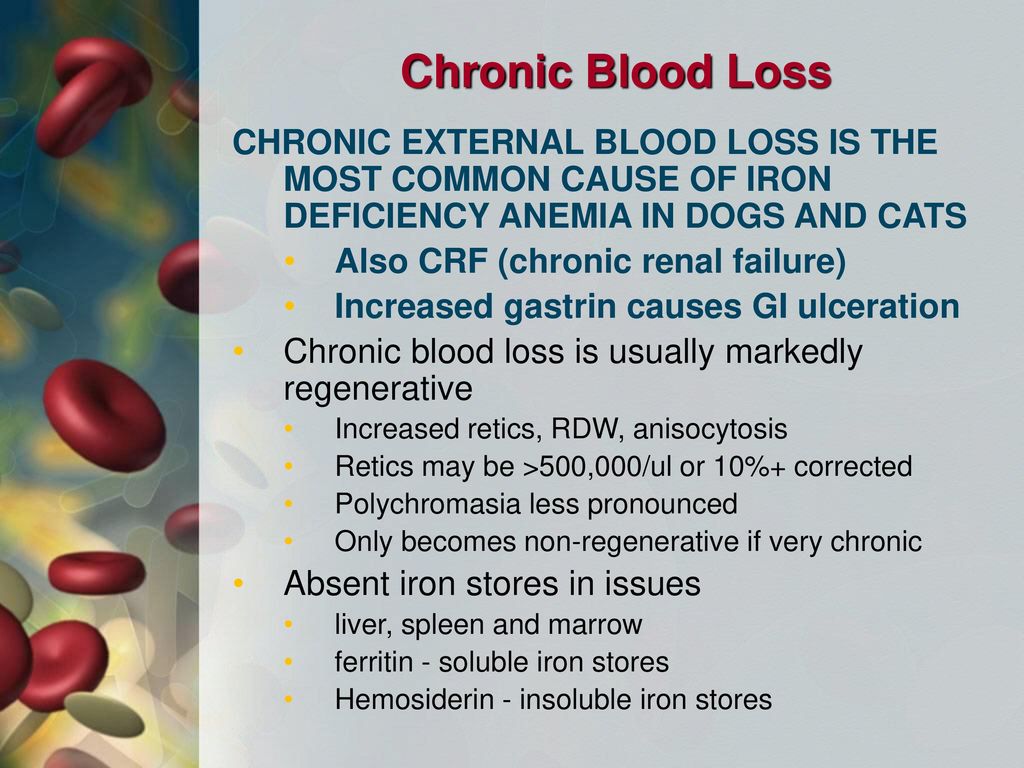 You may see discharge the color of coffee grounds, or near black, during a miscarriage.
You may see discharge the color of coffee grounds, or near black, during a miscarriage.
Exactly how much bleeding you’ll experience depends on a variety of circumstances, including how far along you are and whether or not your miscarriage is progressing naturally.
While you may see a lot of blood, let your doctor know if you fill more than two sanitary pads an hour for two or more hours in a row.
What does a missed miscarriage look like?
You may not experience bleeding or other symptoms with a miscarriage, at least at first.
A missed miscarriage, also referred to as a missed abortion, happens when the fetus has died but the products of conception remain in the uterus. This type of miscarriage is usually diagnosed via ultrasound.
Just as with the amount of blood you’ll see, the duration of a miscarriage will vary from person to person and even from pregnancy to pregnancy.
In many cases, a miscarriage will take around two weeks to pass naturally.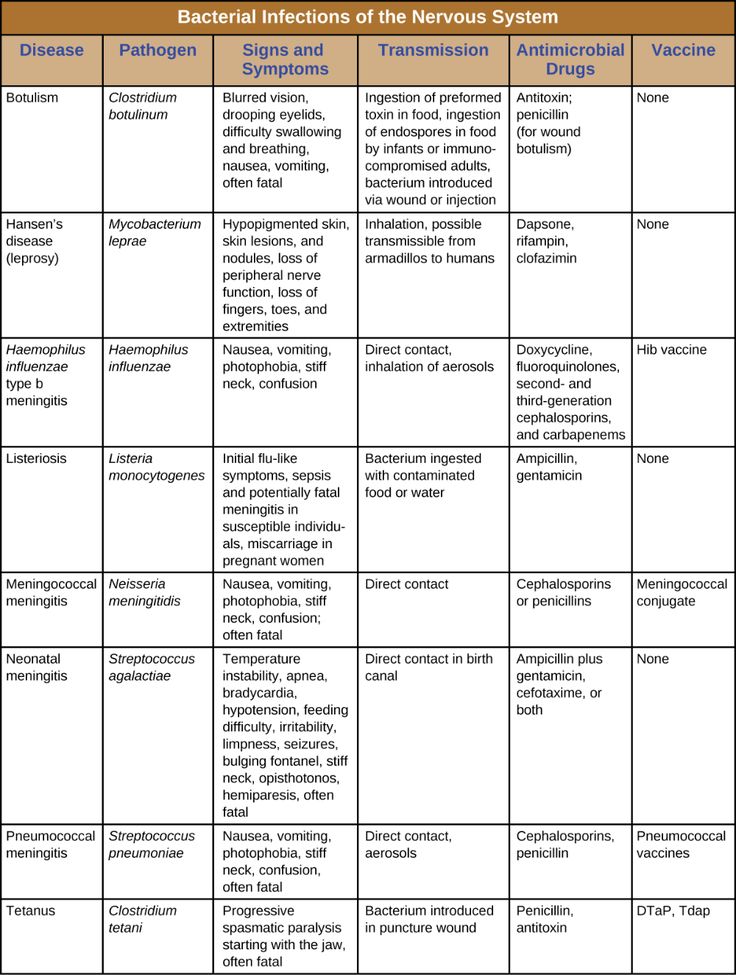 Your doctor may prescribe the medication misoprostol (Cytotec) to help a miscarriage pass more quickly. Bleeding may start within two days of beginning the medication. For others, it may take up to two weeks.
Your doctor may prescribe the medication misoprostol (Cytotec) to help a miscarriage pass more quickly. Bleeding may start within two days of beginning the medication. For others, it may take up to two weeks.
Once the miscarriage has started, the tissue and heaviest bleeding should be passed in about three to five hours. After the fetus has passed, you may still experience spotting and mild tissue loss for one to two weeks.
It may be difficult to tell a very early miscarriage from a late period. In fact, many miscarriages happen before a person even knows they’re pregnant.
In general, a miscarriage will cause more intense symptoms than a menstrual period. For example:
- Your menstrual flow may be relatively similar from month to month with heavy days and light days. A miscarriage can also have heavy and light days, but bleeding may be especially heavy at times and last longer than you’re used to.
- Bleeding from a miscarriage may also contain large clots and tissue you don’t normally see during your period.
- Cramps can be a part of your normal monthly cycle, but with a miscarriage, they may be particularly painful as the cervix dilates.
- The color of blood during your period can range from pink to red to brown. If you see a color you’re not used to seeing, it may be a sign of miscarriage.
Always contact your doctor if you’re pregnant and experience bleeding. While a miscarriage can’t be stopped once it starts, you doctor can run tests to help determine if you’re experiencing the loss of your pregnancy or something else.
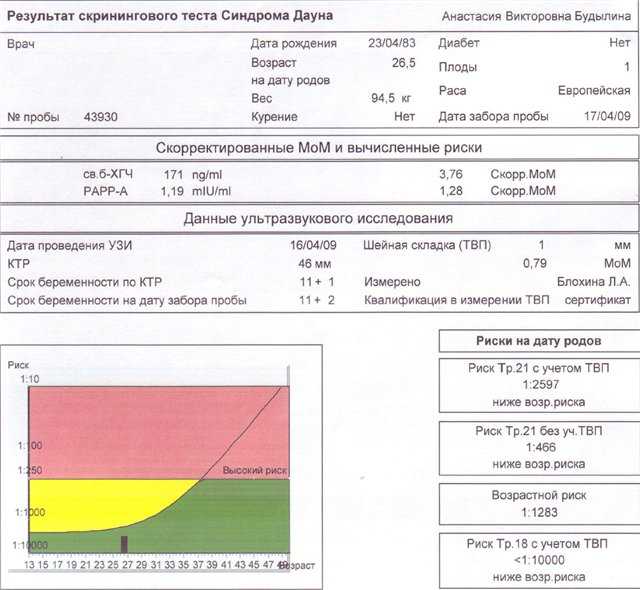
To diagnose a miscarriage, your doctor will likely perform an ultrasound to look for the baby’s heartbeat, if you’re far enough along to see a heartbeat. Your doctor may also order a blood test to check human chorionic gonadotropin (hcG) levels to see if they’re rising or falling.
If a miscarriage is confirmed, your doctor may suggest “expectant management” or waiting for the miscarriage to pass naturally. This generally happens within two weeks.
Incomplete miscarriage
The miscarriage may be incomplete if:
- your bleeding is particularly heavy
- you have a fever
- an ultrasound reveals there’s still tissue in your uterus
If this is the case, your doctor may suggest a dilation and curettage (D and C), which is a surgical procedure done to remove remaining tissue. The procedure is done under general or regional anesthesia, and is considered safe. D and C doesn’t usually lead to long-term complications.
Threatened miscarriage
It’s important to report any bleeding or pain you experience in your pregnancy to your doctor. In some cases, you may have what’s called a threatened miscarriage, and there may be certain treatments that can help. These include:
- hormone supplements if the bleeding is caused by low progesterone
- a cerclage (stitch in the cervix) if the issue is with the cervix opening prematurely
Speak with your healthcare provider if you’re looking to get pregnant again after a miscarriage.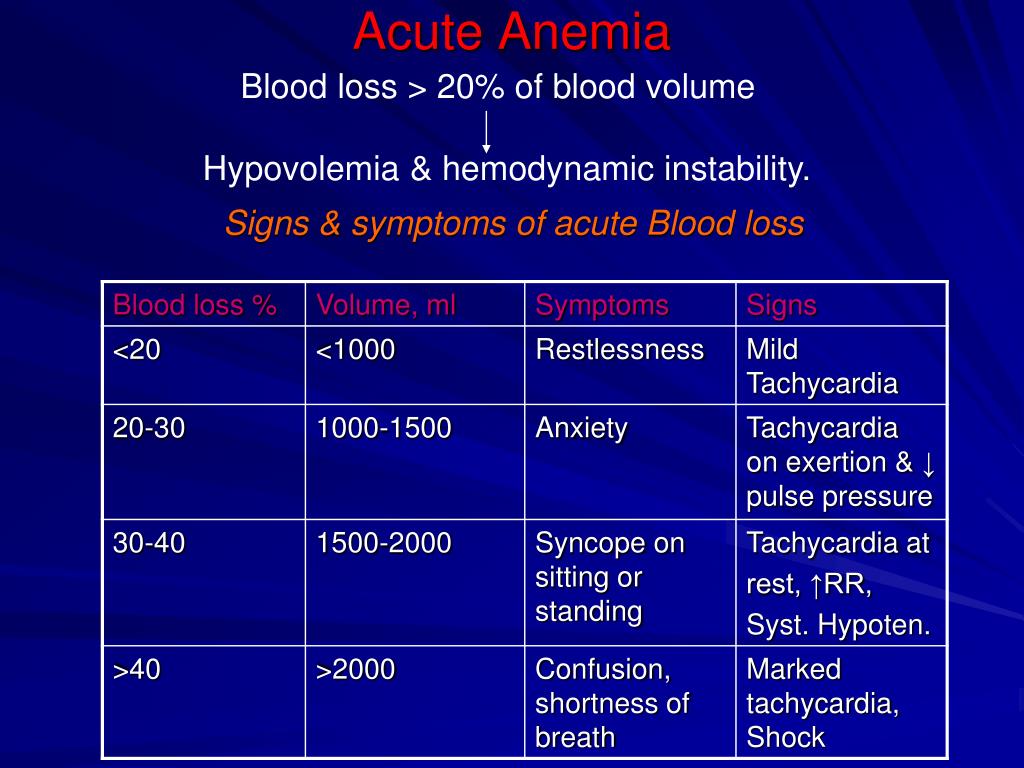 While it may be safe to start trying after your first normal period, you may want to schedule a checkup depending on the cause or the number of miscarriages you’ve had.
While it may be safe to start trying after your first normal period, you may want to schedule a checkup depending on the cause or the number of miscarriages you’ve had.
The reason for loss isn’t always known, but around half of miscarriages are caused by issues with the baby’s chromosomes.
Other possible causes include:
- uterine issues
- hormonal imbalances
- other health conditions, such as diabetes, autoimmune disorders, or polycystic ovary syndrome
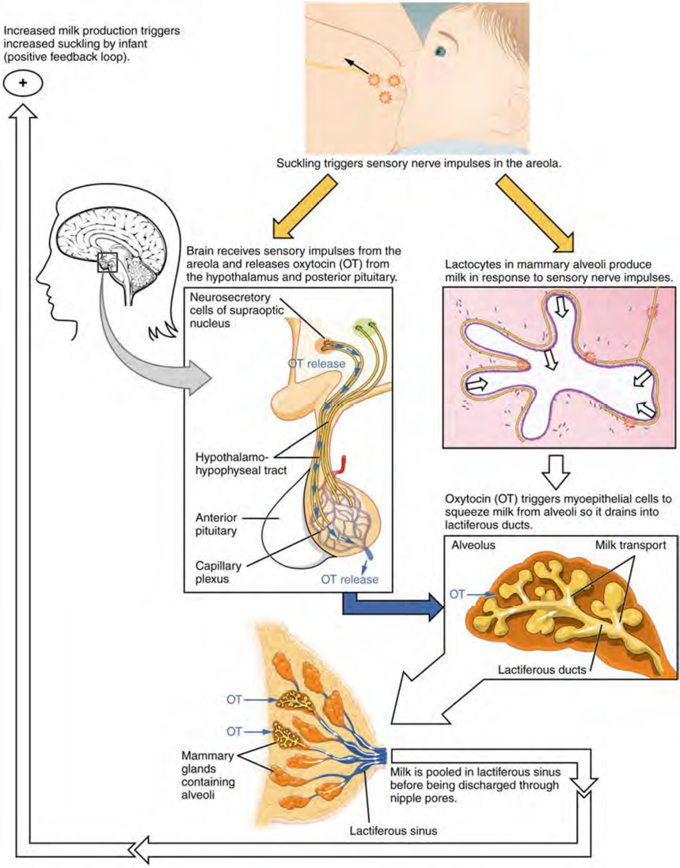
After a miscarriage, you may have hcG in your blood for one to two months, which could lead to a false positive pregnancy test. In most cases, your period will return within four to six weeks, though you may start ovulating almost immediately following a miscarriage.
Speak with your doctor about birth control options if you don’t wish to become pregnant after a miscarriage.
Will I miscarry again?
Having one miscarriage doesn’t necessarily increases your chances of having another. The risk remains around 20 percent.
The risk remains around 20 percent.
Two or more miscarriages is referred to as recurrent pregnancy loss (RPL). The risk of miscarriage after two losses is 28 percent. After three consecutive losses, it increases to 43 percent.
Only 1 percent of people experience three or more miscarriages. About 65 percent of those with unexplained RPL go on to have successful pregnancies.
Activities like exercise, work, morning sickness, and sex don’t cause miscarriages. Even things like smoking or drinking alcohol or caffeine, which can lead to other complications, are also unlikely to lead to early pregnancy loss.
A miscarriage can be physically painful, and it may also cause a variety of emotions. While your body may recover in a few weeks, be sure to take time to process your feelings, grieve, and reach out for help when you need it.
Spontaneous abortion (miscarriage)
If the pregnancy is terminated naturally before the fetus reaches gestational age, this is called a spontaneous abortion or miscarriage.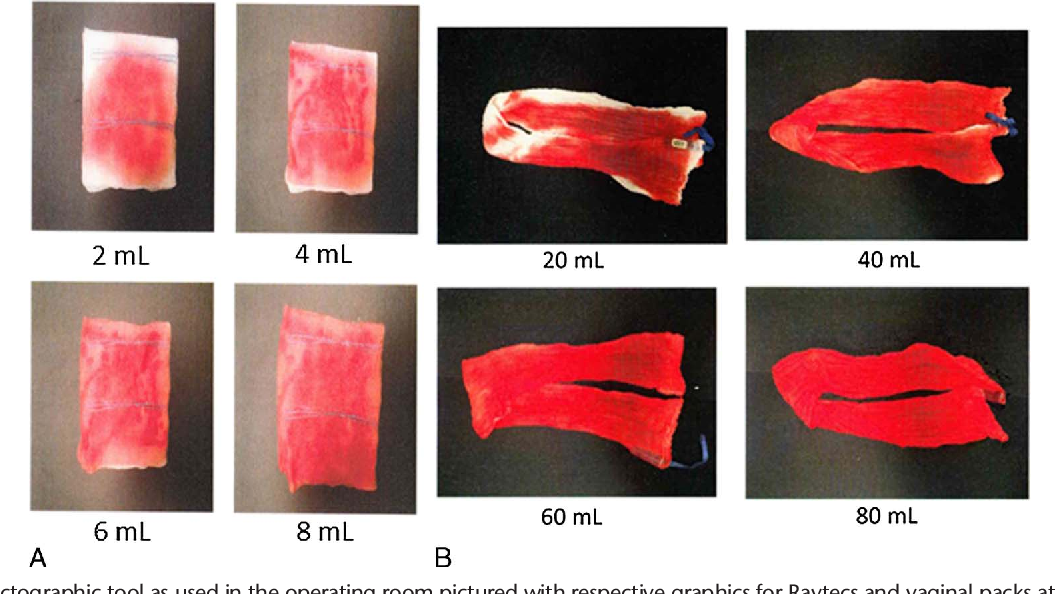 More than half of miscarriages occur no later than 12 weeks of gestation due to fetal abnormalities. The rest falls on the period up to 20 weeks and is associated with pathologies of pregnancy. If the pregnancy is terminated in the second half, it is called preterm labor.
More than half of miscarriages occur no later than 12 weeks of gestation due to fetal abnormalities. The rest falls on the period up to 20 weeks and is associated with pathologies of pregnancy. If the pregnancy is terminated in the second half, it is called preterm labor.
Spontaneous abortion, otherwise known as miscarriage, is one of the most common complications during pregnancy, accounting for 10-20% of diagnosed pregnancies, and is the rejection of a fetus weighing no more than 500 grams. and less than 22 weeks. Unfortunately, with such indicators, the fetus is not viable. Usually 80% of the total number of spontaneous abortions occurs before the 12th week of pregnancy.
Types of spontaneous abortion
1. Threat of miscarriage - characterized by mild uterine cramps, pulling pain in the lower abdomen and sometimes mild bloody discharge from the vagina.
2. A miscarriage that has begun - is characterized by more severe pain and profuse bleeding. At the same time, the tone of the uterus is slightly increased, and the internal os is closed.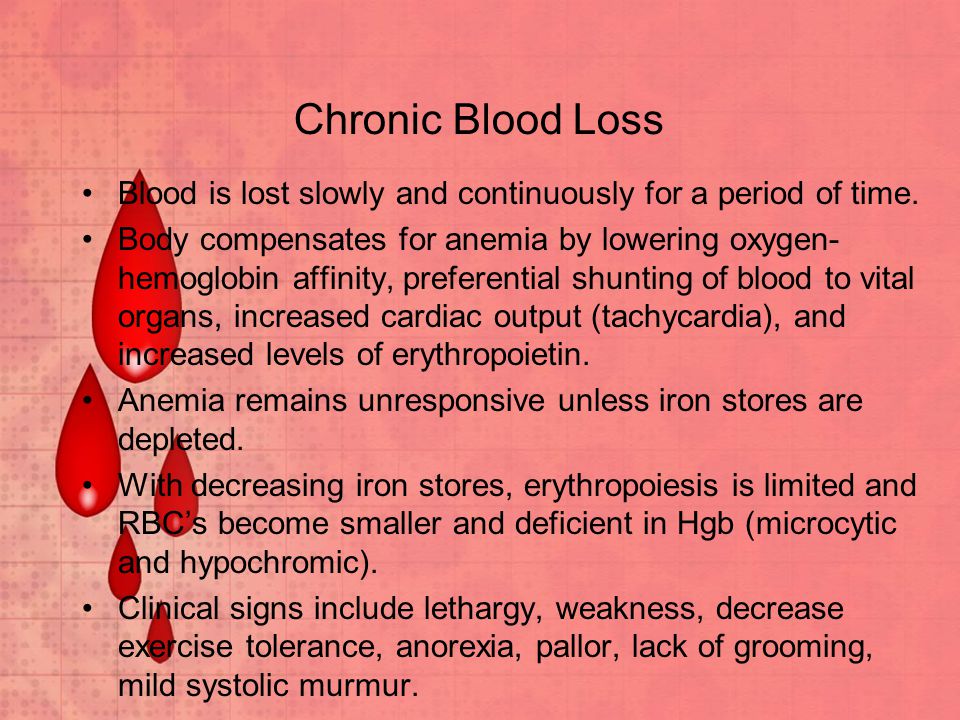
3. Inevitable miscarriage - accompanied by dilatation of the cervix - a fetal egg can be distinguished - with profuse bleeding and severe cramps in the lower abdomen.
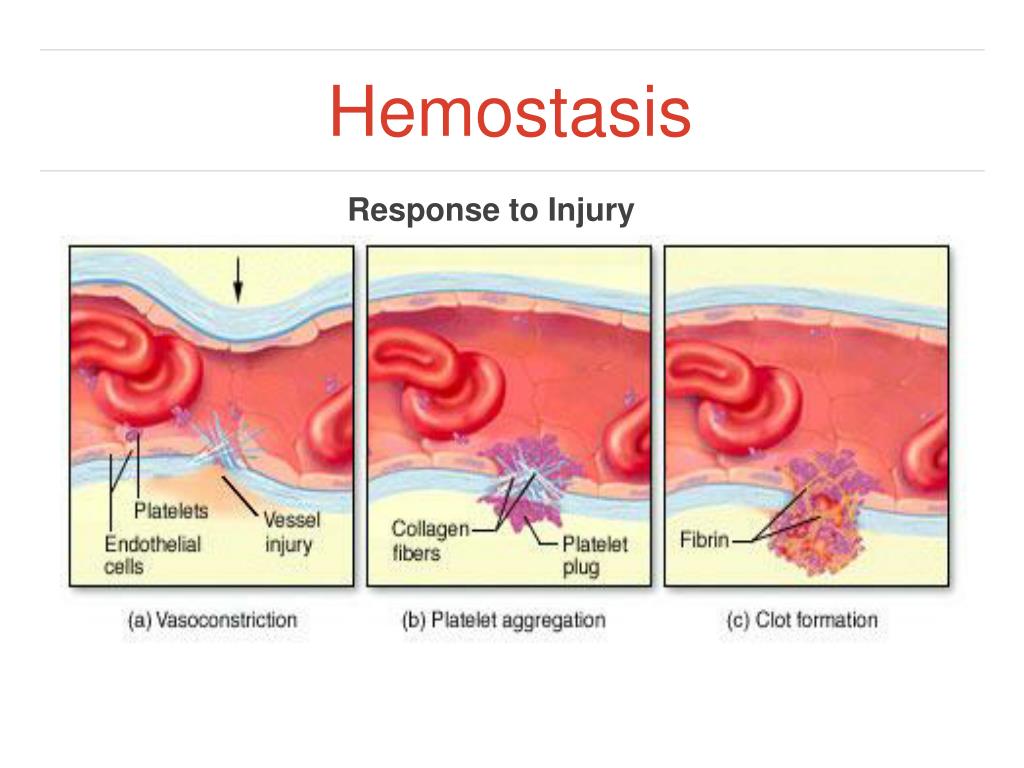
4. Incomplete miscarriage - part of the fetus comes out. The bleeding is so profuse that it can lead to the death of a woman.
5. Completed miscarriage - the fetal egg and the fetus itself are completely out. After that, the bleeding and spasms stop.
The etiology of miscarriage is due to many factors. Among them:
- genetic disorders;
- previous induced abortions;
- too little time has passed since the previous pregnancy;
- inflammatory infections in the mother, endocrine disorders;
- blood conflict between mother and fetus;
- taking hormonal contraceptives and certain medications;
- smoking during pregnancy and drinking alcohol;
- unknown causes.
To prevent miscarriage, it is necessary to give up bad habits, not to have abortions and to be regularly examined by a doctor.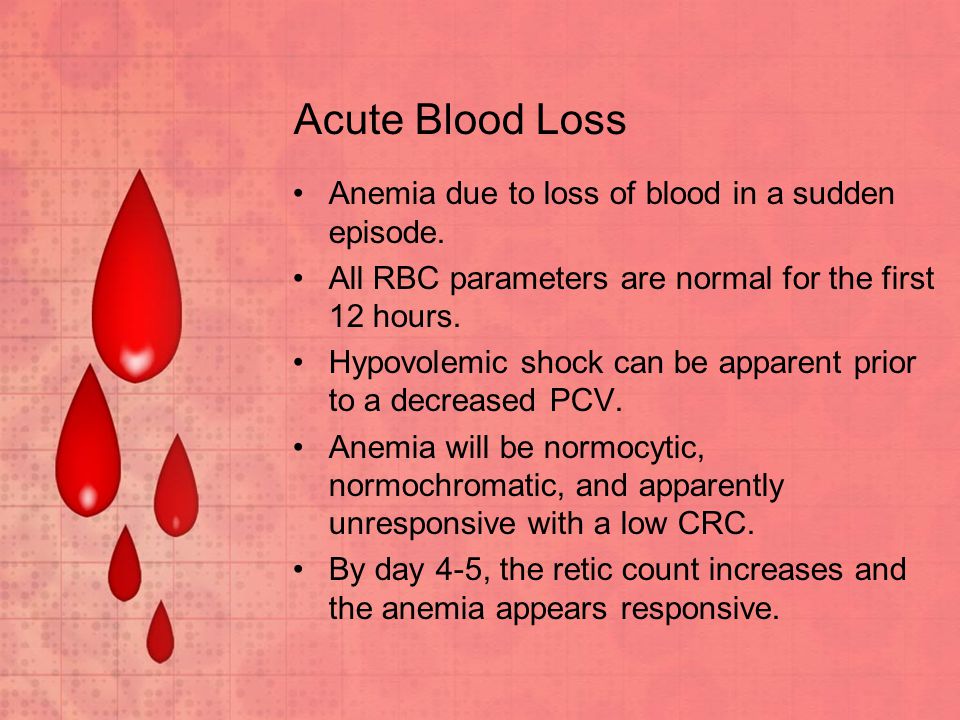
Spontaneous abortion begins with the appearance of cramping, drawing pains, similar to pain during menstruation. Then bleeding from the uterus begins. At first, the discharge is slight or moderate, and then, after detachment of the fetal egg, abundant discharge with bloody clots begins. The appearance of these symptoms requires urgent hospitalization.
After examining a woman in a hospital, having determined the degree of detachment of the embryo, one of the following diagnoses will be made:
- the threat of pregnancy - detachment is only outlined or is completely insignificant. In this case, the pregnancy can be saved;
- a miscarriage that has begun - detachment is already quite decent with a pronounced pain syndrome. And in this case, the fetus can be saved;
- abortion in progress - detachment with displacement progresses, labor-like contractions begin. Pregnancy cannot be saved, cleaning is required;
- incomplete miscarriage - independent exit of a part of the fetus and membranes, curettage is necessary for the final curettage of the uterus;
- late abortion - premature delivery of an unviable baby.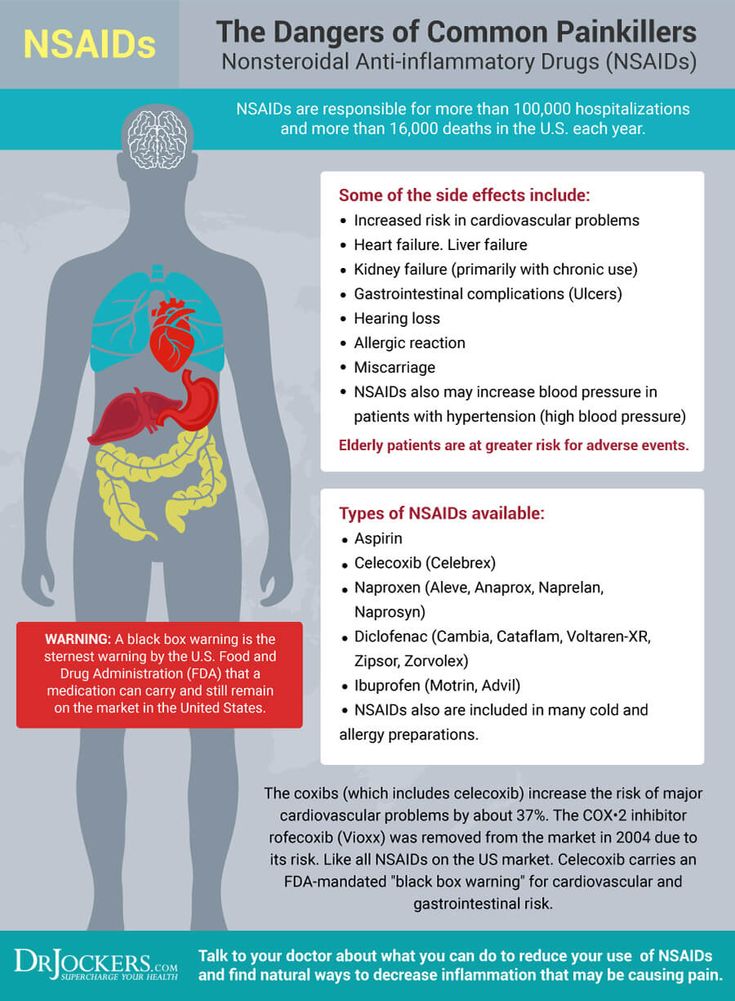
After a spontaneous abortion, it is recommended to take a short break in planning and take preventive measures to avoid recurrence.
In case of repeated miscarriage, a thorough comprehensive examination is necessary to determine the causes of miscarriage and eliminate them.
A miscarriage is a severe psychological trauma, especially during the first pregnancy. But do not give up, with a competent approach to planning and bearing, the next pregnancy will certainly end with the appearance of a long-awaited baby.
Causes of spontaneous abortion
1. Doctors call various chromosomal pathologies one of the main reasons: monosomy, autosomal trisomies, polyploidy. They account for 82-88% of spontaneous miscarriages.
2. The second most common cause is disorders in the female genital area: endometritis - inflammation of the uterine mucosa - preventing the implantation of the fetal egg and its development and polycystic ovaries.
3. Hormonal disorders, namely progesterone deficiency.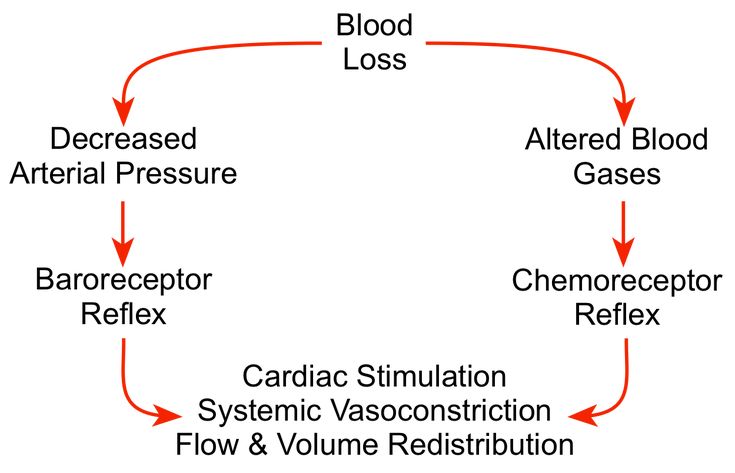
4. Chronic diseases - uncontrolled diabetes mellitus, high blood pressure.
5. Viral infections rubella, chlamydia and others.
Treatment
In case of severe blood loss, ultrasound is performed to determine the viability of the fetus and rule out an ectopic pregnancy. A woman is prescribed bed rest and is treated with antispasmodic drugs to relax the uterine myometrium and stop bleeding.
If doctors still diagnose a spontaneous abortion that has begun, then the actions are reduced either to expectant tactics (within 2-6 weeks the fetal egg should come out by itself), or to prescribing drugs that accelerate the delivery of the fetus, or to vacuum aspiration (medical abortion ).
Lost liters of blood. In Voronezh, a doctor is on trial for the death of a woman after a miscarriage
- News Voronezh
- News
- Lost liters of blood. In Voronezh, a doctor is on trial for the death of a woman after a miscarriage0080
Oksana Gribkova Vesti Voronezh 32119
Sovetsky District Court on Monday, February 18, began considering the case of the death of 39-year-old Ekaterina Tarakanova. The woman died in emergency hospital No. 1 from blood loss. Catherine left four children, the youngest of whom was then 2.5 years old. For the death of the patient, the doctor Tatyana Chesnokova turned out to be in the dock.
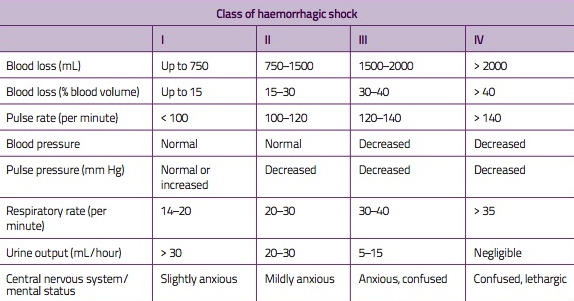
At the first meeting, the prosecutor announced that she was accused of negligently causing the patient's death. According to the version of the investigation, the doctor on duty underestimated the severity of the patient's condition, did not perform the operation on time, and did not replenish the blood loss. Ekaterina lost 2.5 liters of blood and died due to DIC, a bleeding disorder. As experts have established, the woman's life could have been saved if time had not been lost.
As experts have established, the woman's life could have been saved if time had not been lost.
A resident of Voronezh, Ekaterina Tarakanova, was taken to Emergency Hospital No. 1 at the 15th week of pregnancy with the threat of losing her baby on November 7, 2017. The doctors of the gynecology department found that the baby had died, and the next day, on November 8, at about 4 pm, the attending doctor gave the patient a drug for artificial termination of pregnancy.
On that day, from 8 am November 8 to 8 am November 9, 2017, obstetrician-gynecologist Tatyana Chesnokova was on duty at the department. According to the indictment, after the patient's miscarriage at 11 p.m., the doctor performed an operation on her. From that moment - from 23:30 on November 8 to 1:45 on November 9, the patient was under the supervision of Chesnokova, the state prosecutor read out. At this time, the woman's condition worsened due to severe blood loss. The fact that Tarakanova could die became clear at about 2 am, and she was urgently taken to the operating room, where the uterus was removed.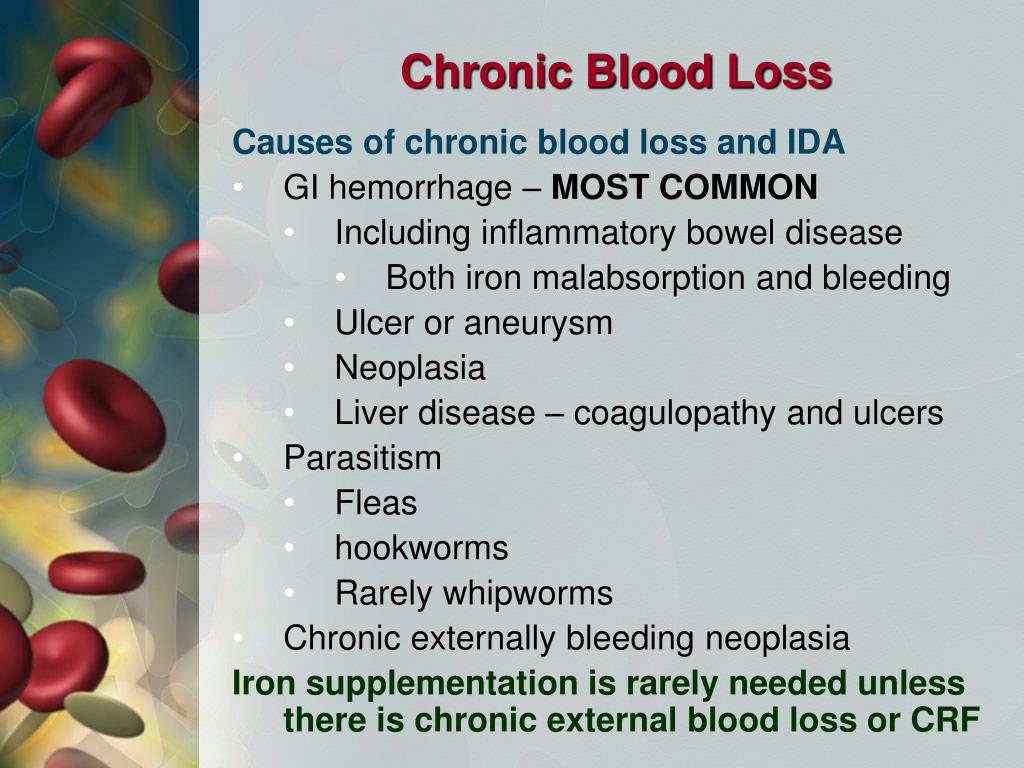
After the operation on November 9 at 4:55 the patient was sent to the intensive care unit. But Catherine's bleeding did not end. Her blood has lost its ability to clot. At 10:30 the woman began to die. Doctors gave her a heart massage, used all the possibilities of resuscitation, but at 11:10 they were forced to announce the time of death.
Reading out the conclusions of the forensic examination, the prosecutor focused on the erroneous assessment of blood loss. So at 1:30 it was about 500 ml of blood, while the clinical picture and the patient's condition spoke of a blood loss of 1-1.5 liters. By 1:55 this estimate was 650 ml, but in fact the patient had already lost 2 liters of blood.
- There were shortcomings in the provision of medical care - lack of monitoring of the patient and her hemodynamic parameters, untimely measures to surgically stop bleeding. It was decided to do the operation with a significant delay of 1 hour 30 minutes, - the state prosecutor read out.