Mumps with pregnancy
Mumps | For Healthcare Providers
The Virus
Mumps is a viral illness caused by a paramyxovirus, a member of the Rubulavirus family. The average incubation period for mumps is 16 to 18 days, with a range of 12 to 25 days.
Clinical Features
Mumps usually involves pain, tenderness, and swelling in one or both parotid salivary glands (cheek and jaw area). Swelling usually peaks in 1 to 3 days and then subsides during the next week. The swollen tissue pushes the angle of the ear up and out. As swelling worsens, the angle of the jawbone below the ear is no longer visible. Often, the jawbone cannot be felt because of swelling of the parotid. One parotid may swell before the other, and in 25% of patients, only one side swells. Other salivary glands (submandibular and sublingual) under the floor of the mouth also may swell but do so less frequently (10%).
Nonspecific prodromal symptoms may precede parotitis by several days, including low-grade fever which may last 3 to 4 days, myalgia, anorexia, malaise, and headache. Parotitis usually lasts on average 5 days and most cases resolve after 10 days. Mumps infection may also present only with nonspecific or primarily respiratory symptoms, or may be asymptomatic. Reinfection after natural infection and recurrent parotitis, when parotitis on one side resolves but is followed weeks to months later by parotitis on the other side, can also occur in mumps patients.
Mumps can occur in a person who is fully vaccinated, but vaccinated patients are less likely to present severe symptoms or complications than under- or unvaccinated cases. Mumps should be suspected in all patients with parotitis or mumps complications, regardless of age, vaccination status, and travel history.
Mumps infection is most often confused with swelling of the lymph nodes of the neck. Lymph node swelling can be differentiated by the well-defined borders of the lymph nodes, their location behind the angle of the jawbone, and lack of the ear protrusion or obscuring of the angle of the jaw, which are characteristics of mumps.
Background
Before the U.S. mumps vaccination program started in 1967, about 186,000 cases were reported each year, and many more unreported cases occurred. The disease caused complications, such as permanent deafness in children, and occasionally, encephalitis, which could rarely result in death. Following the implementation of the routine two dose MMR vaccination policy, there was a 99% decrease in mumps cases in the United States, with just a few hundred cases reported each year by the early 2000s. However, starting in 2006 there has been an increase in mumps cases with several peak years. From year to year, the number of mumps cases can range from roughly a couple hundred to a several thousand, with majority of cases and outbreaks occurring among people who are fully vaccinated and in close-contact or congregate settings.
Transmission
The mumps virus replicates in the upper respiratory tract and is transmitted person to person through direct contact with saliva or respiratory droplets of a person infected with mumps. The risk of spreading the virus increases the longer and the closer the contact a person has with someone who has mumps. The infectious period is considered from 2 days before to 5 days after parotitis onset, although virus has been isolated from saliva as early as 7 days prior to and up to 9 days after parotitis onset. Mumps virus has also been isolated up to 14 days in urine and semen.
The risk of spreading the virus increases the longer and the closer the contact a person has with someone who has mumps. The infectious period is considered from 2 days before to 5 days after parotitis onset, although virus has been isolated from saliva as early as 7 days prior to and up to 9 days after parotitis onset. Mumps virus has also been isolated up to 14 days in urine and semen.
When a person is ill with mumps, they should avoid contact with others from the time of diagnosis until 5 days after the onset of parotitis by staying home from work or school and staying in a separate room if possible.
Complications
Mumps complications include orchitis, oophoritis, mastitis, meningitis, encephalitis, pancreatitis, and hearing loss. Complications can occur in the absence of parotitis and occur less frequently in vaccinated patients. Some complications of mumps are known to occur more frequently among adults than children.
Orchitis occurs in approximately 30% of unvaccinated and 6% of vaccinated post-pubertal male mumps patients. In 60% to 83% of males with mumps orchitis, only one testis is affected. Mumps orchitis has not been linked to infertility, but may result in testicular atrophy and hypofertility. Among adolescent and adult female mumps patients in the United States in the post-vaccine era, rates of oophoritis and mastitis have been ≤1%. However, these complications may be more difficult to recognize and are likely underreported. Pancreatitis, deafness, meningitis, and encephalitis have been reported in less than 1% of cases in recent U.S. outbreaks. Cases of nephritis and myocarditis and other sequelae, including paralysis, seizures, cranial nerve palsies, and hydrocephalus, in mumps patients have been reported but are very rare. Death from mumps is exceedingly rare. There have been no mumps-related deaths reported in the United States during recent mumps outbreaks.
In 60% to 83% of males with mumps orchitis, only one testis is affected. Mumps orchitis has not been linked to infertility, but may result in testicular atrophy and hypofertility. Among adolescent and adult female mumps patients in the United States in the post-vaccine era, rates of oophoritis and mastitis have been ≤1%. However, these complications may be more difficult to recognize and are likely underreported. Pancreatitis, deafness, meningitis, and encephalitis have been reported in less than 1% of cases in recent U.S. outbreaks. Cases of nephritis and myocarditis and other sequelae, including paralysis, seizures, cranial nerve palsies, and hydrocephalus, in mumps patients have been reported but are very rare. Death from mumps is exceedingly rare. There have been no mumps-related deaths reported in the United States during recent mumps outbreaks.
Mumps during Pregnancy
Mumps that occurs in pregnant women is generally benign and not more severe than in women who are not pregnant. Like other infections, there is a theoretical risk that mumps during the early months of pregnancy may cause complications. Most studies on the effects of gestational mumps on the fetus were conducted in the 1950s–60s when the disease was more common before mumps vaccine was available. One study from 1966 reported an association between mumps infection during the first trimester of pregnancy and an increase in the rate of spontaneous abortion or intrauterine fetal death1, but this result has not been observed in other studies2. One study of low birth weight in relation to mumps during pregnancy found no significant association1. While there are case reports of congenital malformations in infants born to mothers who had mumps during pregnancy, the only prospective, controlled study found rates of malformations were similar between mothers who had mumps and those who did not have mumps during pregnancy3.
Like other infections, there is a theoretical risk that mumps during the early months of pregnancy may cause complications. Most studies on the effects of gestational mumps on the fetus were conducted in the 1950s–60s when the disease was more common before mumps vaccine was available. One study from 1966 reported an association between mumps infection during the first trimester of pregnancy and an increase in the rate of spontaneous abortion or intrauterine fetal death1, but this result has not been observed in other studies2. One study of low birth weight in relation to mumps during pregnancy found no significant association1. While there are case reports of congenital malformations in infants born to mothers who had mumps during pregnancy, the only prospective, controlled study found rates of malformations were similar between mothers who had mumps and those who did not have mumps during pregnancy3.
Learn more about preventing infections during pregnancy.
Mumps in Vaccinated People
People who previously had one or two doses of MMR vaccine can still get mumps and transmit the disease. During mumps outbreaks in highly vaccinated communities, the proportion of cases that occur among people who have been vaccinated may be high. This does not mean that the vaccine is ineffective. The effectiveness of the vaccine is assessed by comparing the attack rate in people who are vaccinated with the attack rate in those who have not been vaccinated. In outbreaks of highly vaccinated populations, people who have not been vaccinated against mumps usually have a much greater mumps attack rate than those who have been fully vaccinated. Disease symptoms are generally milder and complications are less frequent in vaccinated people.
Vaccination
Vaccination is the best way to prevent mumps and mumps complications. This vaccine is included in the combination measles-mumps-rubella (MMR) and measles-mumps-rubella-varicella (MMRV) vaccines. Two doses of mumps vaccine are 88% (range 32% to 95%) effective at preventing the disease; one dose is 78% (range 49% to 91%) effective.
Two doses of mumps vaccine are 88% (range 32% to 95%) effective at preventing the disease; one dose is 78% (range 49% to 91%) effective.
In October 2017, the Advisory Committee on Immunization Practices (ACIP) recommended that people identified by public health authorities as being part of a group at increased risk for acquiring mumps because of a mumps outbreak should receive a third dose of MMR vaccine. The purpose of the recommendation is to improve protection of people in outbreak settings against mumps disease and mumps-related complications.
- Your health department will provide information on groups at increased risk who should receive a dose. If you suspect an outbreak, or are unsure if your patient belongs to a group at increased risk, contact your local health department for more information.
- You should not give a third dose unless your patient is part of a group at increased risk as determined by your local public health authorities.
- MMR vaccine has not been shown to prevent illness in persons already infected with mumps and should not be used as post-exposure prophylaxis in immediate close contacts.
 However, close contacts should still be offered a dose to help protect them against future exposures in the event their prior exposures did not result in infection.
However, close contacts should still be offered a dose to help protect them against future exposures in the event their prior exposures did not result in infection.
See Mumps Vaccination for vaccination recommendations.
Case Classification
For information about how to classify mumps cases, visit the Laboratory Testing Section of the Manual for the Surveillance of Vaccine-Preventable Diseases (2018), Chapter 9: Mumps.
Laboratory Tests to Diagnose Mumps
RT-PCR and viral culture are used to confirm mumps infection. Buccal swabs are most commonly used for RT-PCR testing, but urine and CSF may also be used in specific situations. IgM serology can also be used to aid in diagnosing mumps infection. A patient’s vaccination status and timing of specimen collection are important for interpreting laboratory results. A negative test result does not rule out mumps infection.
Reporting Mumps Cases
Mumps is a nationally notifiable disease, and all cases should be reported to the state or local health department. Contact your state health department for more information on how to report mumps in your state.
Contact your state health department for more information on how to report mumps in your state.
Mumps Prevention and Control in Healthcare Settings
Mumps transmission in healthcare settings, while not common, has occurred in past outbreaks, involving hospitals and long-term care facilities housing adolescents and adults. Information about what measures to take to prevent and control mumps in healthcare settings can be found under the Healthcare Setting section of the Manual for the Surveillance of Vaccine-Preventable Diseases (2018), Chapter 9: Mumps
Footnotes
- Siegel M, Fuerst HT, Peress NS. Comparative fetal mortality in maternal virus diseases. A prospective study on rubella, measles, mumps, chicken pox and hepatitis. N Engl J Med 1966;274(14):768-71.
- Wilson CB, Nizet V, Maldonado YA, Remington JS, Klein JO. Remington and Klein’s infectious diseases of the fetus and newborn infant. 8th Edition, Elsevier Health Sciences, 2016.

- Siegel M. Congenital malformations following chickenpox, measles, mumps, and hepatitis. Results of a cohort study. JAMA 1973;226(13):1521-4.
Mumps and pregnancy | Pregnancy Birth and Baby
Mumps and pregnancy | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What is mumps?
Mumps is a contagious viral illness that is not commonly seen in Australia due to widespread participation in the National Immunisation Program.
Most people with mumps have only mild symptoms, but occasionally the virus can cause serious complications that affect the brain, nerves and other body organs. Around 1 in every 3 people who are infected with the mumps virus won’t have any signs and don’t feel sick at all.
What are the symptoms of mumps?
The most recognisable sign of mumps is large swollen glands — especially the parotid gland, which is in front of the ears.
If you have mumps, you may also experience some of the following symptoms:
- fever
- headache
- muscle aches
- tiredness
- loss of appetite
How can mumps affect my pregnancy? Are there risks to my unborn baby?
Being infected with mumps in the first trimester (12 weeks) of pregnancy increases the risk of miscarriage. However, having mumps in pregnancy is not associated with an increased risk of birth defects for your baby.
How is mumps spread?
Mumps is spread by droplets that travel through the air when an infected person coughs or sneezes. The virus can also spread through contact with items that an infected person has touched — such as surfaces and tissues — or from sharing food or drink.
Mumps may also spread through contact with urine, so if anyone in your household has mumps, it is particularly important to wash your hands frequently, and especially after using the toilet, helping someone in the toilet or changing a nappy.
It can take 12 to 25 days after being exposed to someone with mumps before you see signs of illness. A person with mumps is contagious from about 7 days before the illness to around 9 days after they first notice the symptoms. It’s important to remember that not everyone with mumps has symptoms, and even people without them can spread mumps.
If you have been diagnosed with mumps, you need to keep away from any place where you could infect others. It is best to stay home from work and avoid picking children up from school or day care. Standard hygiene practices like hand washing, not sharing food and drink, coughing and sneezing into your elbows and throwing used tissues directly into the bin can also help prevent spread of the disease.
How can I manage mumps at home?
Most cases resolve by themselves, and there is no specific treatment for mumps. Paracetamol can relieve the pain of swollen glands and help with fever. You can also apply a cold compress to your glands if they are sore and this may provide some relief from the discomfort. It may be uncomfortable to eat when you have swollen glands, but try to keep drinking water. Purees and soft foods may be easier for you to swallow than solid foods.
It may be uncomfortable to eat when you have swollen glands, but try to keep drinking water. Purees and soft foods may be easier for you to swallow than solid foods.
Paracetamol can be taken during pregnancy within the dosage guidelines specified on the pack. It is important to note that other pain medications may need to be avoided in pregnancy, and some pain medicines should not be taken together with paracetamol. Talk to your doctor or pharmacist before taking any medicine during pregnancy.
What complications can occur?
Long-term complications due to mumps are not common. Infection of the brain and brain lining is a serious complication although it is rare and unlikely to cause a permanent problem. Rarely, you could experience pain and swelling of the pancreas, ovaries, liver, heart, thyroid or breasts. Deafness can also occur also but this is usually temporary.
If you have pain other than in your face and the front of your neck around your glands, or if you have a high fever or seem to be feeling sicker over time, seek advice from a doctor.
Check your symptoms with the healthdirect symptom checker tool.
I’m planning a pregnancy — what can I do to avoid mumps?
Mumps can be prevented by vaccination, but vaccination during pregnancy is not recommended. If you are planning a pregnancy, speak to your doctor or contact the National Immunisation Information Line for more information on when and how to get vaccinated against mumps.
Even if you were vaccinated as a child, you may need a booster dose of vaccine to make sure you are still immune.
The mumps vaccine is provided as a combined vaccination. It is given in the same injection as the measles and rubella vaccines. It's known as the ‘measles, mumps, rubella’ or MMR vaccine.
Read more
Vaccinations and pregnancy
Some vaccinations are recommended before pregnancy, while others you can safely have during pregnancy.
If you get vaccinated with the MMR vaccine, you should use contraception and not get pregnant for at least 28 days after the injection. It’s safe to have the MMR vaccine after your baby is born, even if you are breastfeeding.
It’s safe to have the MMR vaccine after your baby is born, even if you are breastfeeding.
Mumps in babies and children
Find out how babies and children can catch measles, how to treat your child at home, and when to have them vaccinated.
Sources:
Australian Institute of Health and Welfare (Mumps in Australia), Australian Government Department of Health (Health Topics – mumps), Tasmanian Government Department of Health (Mumps), Australian Immunisation Handbook (Mumps), BetterHealth Channel (Mumps), Queensland Government (Pregnant and breastfeeding women)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: April 2021
Back To Top
Related pages
- Medicines during pregnancy
- Vaccinations and pregnancy
- Mumps in babies and children
Need more information?
Mumps in Australia | Australian Institute of Health and Welfare
Mumps is a contagious infection of the salivary glands, caused by the mumps virus.
Read more on AIHW – Australian Institute of Health and Welfare website
Mumps
Mumps is an infection of the salivary glands caused by the mumps virus.
Read more on Queensland Health website
Mumps in babies and children
Find out about the symptoms of mumps, how babies and children catch mumps, how to treat your child at home, and when to have them vaccinated against mumps.
Read more on Pregnancy, Birth & Baby website
Mumps fact sheet - Fact sheets
Mumps is a contagious viral infection that occurs mainly in school-aged children. Immunisation with mumps containing vaccine prevents the disease.
Read more on NSW Health website
Mumps - MyDr.
 com.au
com.au Find out about the symptoms, treatment, and complications of mumps, as well as how to prevent this disease.
Read more on myDr website
Mumps - Better Health Channel
Mumps is a viral illness that causes fever and swollen salivary glands, and a swollen face.
Read more on Better Health Channel website
Measles and Mumps tests - Pathology Tests Explained
Why and how tests for measles and mumps are carried out
Read more on Pathology Tests Explained website
Mumps in children and teenagers | Raising Children Network
Mumps is a viral illness that spreads through saliva from coughing and sneezing. Mumps is rare in Australia because most children are immunised against it.
Mumps is rare in Australia because most children are immunised against it.
Read more on raisingchildren.net.au website
Measles, Mumps And Rubella (MMR) Vaccine | SA Health
Measles, mumps and rubella (MMR) vaccine recommendations, possible side effects and how to reduce the side effects
Read more on SA Health website
Mumps | Australian Government Department of Health and Aged Care
Find out how we define and monitor cases of mumps, how you can get vaccinated, and where you can learn more about this disease.
Read more on Department of Health and Aged Care website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Mumps during pregnancy - maternity hospital "Leleka"
Mumps, or viral parotitis, is quite common in pregnant women. Together with measles and chickenpox, this is one of the childhood diseases that can overtake the expectant mother during the gestation period. But unlike other diseases, mumps is almost harmless, with the exception of the disease in the first third of pregnancy.
The mumps virus infects the salivary glands, primarily the parotid glands. The glands swell and slightly deform the oval of the patient's face, the auricle moves back. The face acquires a characteristic pear-shaped shape. As a result, the popular name for this disease appeared - mumps. In severe cases of the disease, the lesion extends to other glands, including the testicles in boys.
As a result, the popular name for this disease appeared - mumps. In severe cases of the disease, the lesion extends to other glands, including the testicles in boys.
The incubation period for mumps is about two weeks. The acute period lasts up to 9 days, and the contact period, during which the patient remains a carrier of the infection, lasts 21 days.
Symptoms of mumps:
- Sudden increase in body temperature, fever;
- Pain in and around the ears, especially when chewing and talking;
- Hearing loss;
- Edema of the face and neck;
- Muscle aches, weakness.
Sometimes, with an atypical course of the disease, characteristic symptoms do not appear, and the existing symptoms are more similar to SARS. Women who have not been vaccinated against mumps should be aware of this and report this to their doctor if similar symptoms appear.
Methods of transmission of the mumps virus
This infection is transmitted by airborne droplets.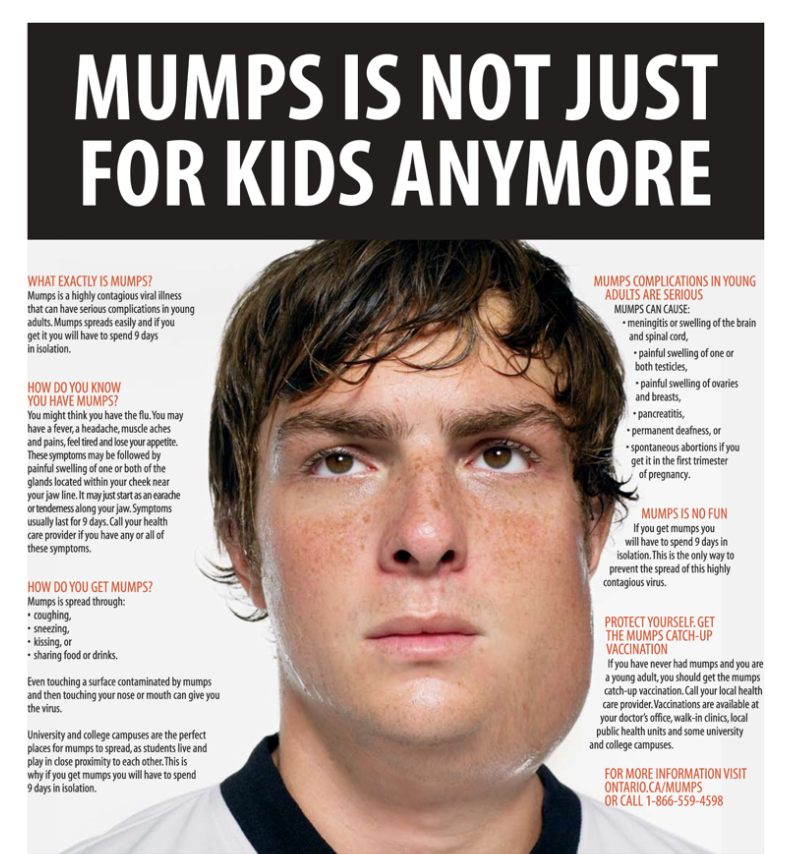 With direct and close contact with the carrier of the infection, the risk is quite high. Since the virus can exist outside the human body for a long time, it is also transmitted through objects. For example, cases of infection through toys in kindergarten are not uncommon. But at the same time, even with direct contact with a carrier, infection may not occur.
With direct and close contact with the carrier of the infection, the risk is quite high. Since the virus can exist outside the human body for a long time, it is also transmitted through objects. For example, cases of infection through toys in kindergarten are not uncommon. But at the same time, even with direct contact with a carrier, infection may not occur.
Pre-pregnancy vaccinations
If you are planning a child, it is recommended that you make a number of preparations, including vaccinations, before conception. The mumps vaccine is included in the list of mandatory vaccinations before pregnancy. But if pregnancy has already occurred, it is better to refuse vaccination.
Mumps in the first trimester of pregnancy
Parotitis is not the most dangerous disease, and it is easily treated. But if a pregnant woman falls ill with mumps, the risk of fading or spontaneous abortion increases in the first trimester. In some cases, the virus infects the breasts, ovaries, and pancreas, and interferes with hormone production. Therefore, if there are cases of mumps in the area (check with your doctor), it is better for a pregnant woman to reduce the number of casual contact with people.
Therefore, if there are cases of mumps in the area (check with your doctor), it is better for a pregnant woman to reduce the number of casual contact with people.
If a pregnant woman has had mumps and kept her pregnancy, there is no need to worry: the virus is not a pathogen. There are no identified cases of the development of fetal pathologies after this disease. This will not affect the health of the baby.
Treatment of mumps
Treatment is carried out on an outpatient or inpatient basis, under the supervision of the attending physician. The patient is prescribed bed rest, a minimum of contact with others, liquid or semi-purified food. Antibiotics and antivirals are not recommended. At high temperatures, paracetamol-based antipyretics are prescribed, aspirin and other salicylic acid preparations are contraindicated. In severe cases, antihistamines are prescribed to reduce swelling, injections of glucose and saline solutions to replenish fluid reserves.
Particular attention should be paid to oral hygiene. Since the salivary glands do not function properly in parotitis, patients often complain of dry mouth. Drying of the mucous membranes of the oral cavity leads to the appearance of microcracks and the development of a secondary infection. Therefore, it is recommended to moisten and rinse your mouth with antiseptic solutions, as well as thoroughly brush your teeth twice a day.
Mumps before childbirth
If a pregnant woman falls ill with mumps shortly before childbirth, it can also infect her baby. The disease can be transmitted by airborne droplets, as well as through breast milk. Nevertheless, you should not be afraid: both in adults and in infants, mumps is easy and quickly cured.
Mumps (mumps) during pregnancy
Mumps (mumps) during pregnancy Mumps is a viral childhood infection, but adults also sometimes get it. Therefore, there is some risk of getting mumps during pregnancy, although it is much lower compared to the risk of getting rubella or measles.
How you can get mumps
For people who do not have immunity to mumps, exposure to the pathogen will almost certainly lead to mumps . Infection occurs by airborne droplets or through toys and utensils contaminated with the patient's saliva (for example, in kindergarten or at home in the family). The virus is shed as early as a week before obvious signs of illness, and a person remains contagious for 17 days (up to day 9 of the disease from the onset of the first symptoms). Therefore, if a future mother has a focus of infection at home or at work, then it is worth remembering if she had mumps in her childhood. And at the same time, check in your medical record the presence of all age-related vaccinations against mumps. These data will influence the decision on the need for additional examination and administration of immunoglobulin.
How is mumps in pregnant women
From infection to the onset of the first symptoms can take from 11 to 23 days , but more often the incubation period lasts 15-20 days. A typical form of parotitis begins acutely - with a high temperature (up to 40 °), chills, headaches and muscle pain, severe weakness. There is pain in the ear (one-sided or near both ears), aggravated by chewing movements and opening the mouth, painful salivation, stuffy ears and hearing loss.
A typical form of parotitis begins acutely - with a high temperature (up to 40 °), chills, headaches and muscle pain, severe weakness. There is pain in the ear (one-sided or near both ears), aggravated by chewing movements and opening the mouth, painful salivation, stuffy ears and hearing loss.
On the first day, severe edema develops in the area of the affected salivary glands (more often parotid, but submandibular and sublingual glands may be involved). Puffiness increases rapidly, with a bilateral lesion, asynchronous development of the symptom is possible. The site of inflammation is painful. The skin over the salivary gland is strongly stretched, shiny, but the color of the skin is not changed. Due to edema and an enlarged salivary gland, the earlobe shifts up and forward, the face acquires a characteristic pear-shaped shape, for which the disease got its common name "mumps" or "mumps" . The edema increases in the first five days, all this time the temperature remains at high numbers, then decreases slightly (to about 38 °) and lasts until the end of the peak period (about 2 weeks). Then the swelling decreases, the pain in the gland gradually disappears, and recovery occurs.
Then the swelling decreases, the pain in the gland gradually disappears, and recovery occurs.
Atypical forms of mumps
In some cases, mumps proceeds in an atypical form, in which there is no pronounced edema above the parotid salivary gland. The main signs of the disease with erased forms of parotitis, symptoms of general intoxication (high temperature, weakness) and respiratory symptoms similar to the signs of SARS remain - a runny nose, sore throat, dry cough. Sometimes the disease can be completely asymptomatic. Therefore, if for a pregnant woman there is a risk of infection with the mumps virus (there was contact with a sick mumps, but there were no vaccinations, and she had not previously had this disease), then it is worth donating blood to determine the titer of specific antibodies or to detect the mumps virus itself.
What is the danger of mumps during pregnancy
Adults are often more difficult to tolerate diseases from the group of childhood infections, and mumps is no exception. Therefore, the first danger that awaits the future mother, if she falls ill with mumps, is a serious general condition. Sometimes severe forms of mumps are recorded with involvement in the process of other glands, except for salivary glands - ovaries, mammary gland, pancreas. In this case, they talk about the complication of parotitis with mastitis, oophoritis or pancreatitis. The most severe complications include meningitis and encephalitis.
Therefore, the first danger that awaits the future mother, if she falls ill with mumps, is a serious general condition. Sometimes severe forms of mumps are recorded with involvement in the process of other glands, except for salivary glands - ovaries, mammary gland, pancreas. In this case, they talk about the complication of parotitis with mastitis, oophoritis or pancreatitis. The most severe complications include meningitis and encephalitis.
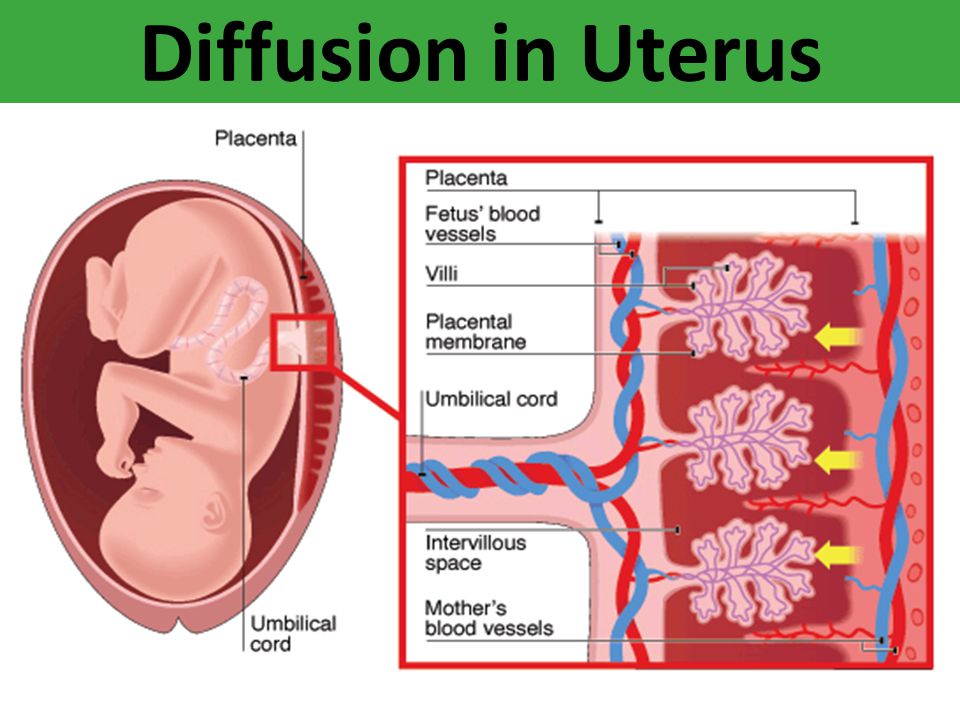
The mumps virus is not dangerous for the fetus in terms of the development of severe malformations, since it does not cross the placenta. But mumps disease in the early stages sometimes leads to spontaneous miscarriages, due to severe intoxication of the pregnant woman's body.
Treatment of mumps during pregnancy
Treatment of mumps in pregnant women should be strictly under medical supervision . In severe and complicated cases, hospitalization is indicated; in milder cases, the pregnant woman can stay at home, observing bed rest. Since there are no specific drugs for the treatment of mumps, the main therapy is aimed at eliminating intoxication and reducing inflammation in the affected organs.
Since there are no specific drugs for the treatment of mumps, the main therapy is aimed at eliminating intoxication and reducing inflammation in the affected organs.
Detoxification of the organism is carried out by several methods . In addition to drinking plenty of water (tea, compotes, juices), if necessary, intravenous infusions of solutions (glucose, reopoliglyukin, gemodez) are prescribed. During a fever, antipyretic drugs should be used - paracetamol, Nurofen. To reduce inflammation, non-steroidal anti-inflammatory drugs (ortofen, indomethacin) are used. In severe cases, prescribe hormonal drugs (prednisolone, dexamethasone). Antihistamines (diphenhydramine, suprastin, tavegil) will also help to cope with edema. Temporary relief will bring cold compresses to the area of the affected gland.
Antibiotics are not prescribed for the treatment of mumps, as this is a viral disease . It is also inappropriate to prescribe immunoglobulins for prevention and treatment.