Sleeping pregnant first trimester
Sleeping While Pregnant 1st Trimester
1.
Ku, C. W., Allen, J. C., Jr, Lek, S. M., Chia, M. L., Tan, N. S., & Tan, T. C. (2018). Serum progesterone distribution in normal pregnancies compared to pregnancies complicated by threatened miscarriage from 5 to 13 weeks gestation: a prospective cohort study. BMC pregnancy and childbirth, 18(1), 360. https://doi.org/10.1186/s12884-018-2002-z
2.
Won C. H. (2015). Sleeping for Two: The Great Paradox of Sleep in Pregnancy. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 11(6), 593–594. https://doi.org/10.5664/jcsm.4760
3.
Martin-Fairey, C. A., Zhao, P., Wan, L., Roenneberg, T., Fay, J., Ma, X., McCarthy, R., Jungheim, E. S., England, S. K., & Herzog, E. D. (2019). Pregnancy Induces an Earlier Chronotype in Both Mice and Women. Journal of biological rhythms, 34(3), 323–331. https://doi.org/10.1177/0748730419844650
4.
Baumgartel, K. L., Terhorst, L., Conley, Y. P., & Roberts, J. M. (2013). Psychometric evaluation of the Epworth sleepiness scale in an obstetric population. Sleep medicine, 14(1), 116–121. https://doi.org/10.1016/j.sleep.2012.10.007
5.
Lee, K. A., Zaffke, M. E., & McEnany, G. (2000). Parity and sleep patterns during and after pregnancy. Obstetrics and gynecology, 95(1), 14–18. https://doi.org/10.1016/s0029-7844(99)00486-x
6.
Neau, J. P., Texier, B., & Ingrand, P. (2009). Sleep and vigilance disorders in pregnancy. European neurology, 62(1), 23–29. https://doi.org/10.1159/000215877
7.
Okun, M. L., Buysse, D. J., & Hall, M. H. (2015). Identifying Insomnia in Early Pregnancy: Validation of the Insomnia Symptoms Questionnaire (ISQ) in Pregnant Women. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 11(6), 645–654. https://doi.org/10. 5664/jcsm.4776
5664/jcsm.4776
8.
Bai, G., Korfage, I. J., Groen, E. H., Jaddoe, V. W., Mautner, E., & Raat, H. (2016). Associations between Nausea, Vomiting, Fatigue and Health-Related Quality of Life of Women in Early Pregnancy: The Generation R Study. PloS one, 11(11), e0166133. https://doi.org/10.1371/journal.pone.0166133
9.
Oyiengo, D., Louis, M., Hott, B., & Bourjeily, G. (2014). Sleep disorders in pregnancy. Clinics in chest medicine, 35(3), 571–587. https://doi.org/10.1016/j.ccm.2014.06.012
10.
Gartland, D., Brown, S., Donath, S., & Perlen, S. (2010). Women's health in early pregnancy: findings from an Australian nulliparous cohort study. The Australian & New Zealand journal of obstetrics & gynaecology, 50(5), 413–418. https://doi.org/10.1111/j.1479-828X.2010.01204.x
11.
Nazik, E., & Eryilmaz, G. (2014). Incidence of pregnancy-related discomforts and management approaches to relieve them among pregnant women. Journal of clinical nursing, 23(11-12), 1736–1750. https://doi.org/10.1111/jocn.12323
Journal of clinical nursing, 23(11-12), 1736–1750. https://doi.org/10.1111/jocn.12323
12.
Bradley, C. S., Kennedy, C. M., Turcea, A. M., Rao, S. S., & Nygaard, I. E. (2007). Constipation in pregnancy: prevalence, symptoms, and risk factors. Obstetrics and gynecology, 110(6), 1351–1357. https://doi.org/10.1097/01.AOG.0000295723.94624.b1
13.
Gomes, C. F., Sousa, M., Lourenço, I., Martins, D., & Torres, J. (2018). Gastrointestinal diseases during pregnancy: what does the gastroenterologist need to know?. Annals of gastroenterology, 31(4), 385–394. https://doi.org/10.20524/aog.2018.0264
14.
Malfertheiner, S. F., Malfertheiner, M. V., Kropf, S., Costa, S. D., & Malfertheiner, P. (2012). A prospective longitudinal cohort study: evolution of GERD symptoms during the course of pregnancy. BMC gastroenterology, 12, 131. https://doi.org/10.1186/1471-230X-12-131
15.
Bourjeily, G., Chambers, A. , Salameh, M., Bublitz, M. H., Kaur, A., Coppa, A., Risica, P., & Lambert-Messerlian, G. (2019). Anthropometric Measures and Prediction of Maternal Sleep-Disordered Breathing. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 15(6), 849–856. https://doi.org/10.5664/jcsm.7834
, Salameh, M., Bublitz, M. H., Kaur, A., Coppa, A., Risica, P., & Lambert-Messerlian, G. (2019). Anthropometric Measures and Prediction of Maternal Sleep-Disordered Breathing. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 15(6), 849–856. https://doi.org/10.5664/jcsm.7834
16.
Sweet, L., Arjyal, S., Kuller, J. A., & Dotters-Katz, S. (2020). A Review of Sleep Architecture and Sleep Changes During Pregnancy. Obstetrical & gynecological survey, 75(4), 253–262. https://doi.org/10.1097/OGX.0000000000000770
17.
Doyon, M., Pelland-St-Pierre, L., Allard, C., Bouchard, L., Perron, P., & Hivert, M. F. (2020). Associations of sleep duration, sedentary behaviours and energy expenditure with maternal glycemia in pregnancy. Sleep medicine, 65, 54–61. https://doi.org/10.1016/j.sleep.2019.07.008
18.
Okada, K., Saito, I., Katada, C., & Tsujino, T. (2019). Influence of quality of sleep in the first trimester on blood pressure in the third trimester in primipara women. Blood pressure, 28(5), 345–355. https://doi.org/10.1080/08037051.2019.1637246
Influence of quality of sleep in the first trimester on blood pressure in the third trimester in primipara women. Blood pressure, 28(5), 345–355. https://doi.org/10.1080/08037051.2019.1637246
19.
Okun, M. L., Kline, C. E., Roberts, J. M., Wettlaufer, B., Glover, K., & Hall, M. (2013). Prevalence of sleep deficiency in early gestation and its associations with stress and depressive symptoms. Journal of women's health (2002), 22(12), 1028–1037. https://doi.org/10.1089/jwh.2013.4331
20.
Lee, E. K., Gutcher, S. T., & Douglass, A. B. (2014). Is sleep-disordered breathing associated with miscarriages? An emerging hypothesis. Medical hypotheses, 82(4), 481–485. https://doi.org/10.1016/j.mehy.2014.01.031
21.
Medical Encyclopedia: A.D.A.M Medical Encyclopedia. (2018, April 19). Problems sleeping during pregnancy. Retrieved August 27, 2020. https://medlineplus.gov/ency/patientinstructions/000559.htm
22.
Miller, M. A., Mehta, N., Clark-Bilodeau, C., & Bourjeily, G. (2020). Sleep Pharmacotherapy for Common Sleep Disorders in Pregnancy and Lactation. Chest, 157(1), 184–197. https://doi.org/10.1016/j.chest.2019.09.026
23.
Lee, K. A., Zaffke, M. E., & Baratte-Beebe, K. (2001). Restless legs syndrome and sleep disturbance during pregnancy: the role of folate and iron. Journal of women's health & gender-based medicine, 10(4), 335–341. https://doi.org/10.1089/152460901750269652
24.
McParlin, C., O'Donnell, A., Robson, S. C., Beyer, F., Moloney, E., Bryant, A., Bradley, J., Muirhead, C. R., Nelson-Piercy, C., Newbury-Birch, D., Norman, J., Shaw, C., Simpson, E., Swallow, B., Yates, L., & Vale, L. (2016). Treatments for Hyperemesis Gravidarum and Nausea and Vomiting in Pregnancy: A Systematic Review. JAMA, 316(13), 1392–1401. https://doi.org/10.1001/jama.2016.14337
25.
Lindblad, A. J., & Koppula, S. (2016). Ginger for nausea and vomiting of pregnancy. Canadian family physician Medecin de famille canadien, 62(2), 145. https://pubmed.ncbi.nlm.nih.gov/26884528/
(2016). Ginger for nausea and vomiting of pregnancy. Canadian family physician Medecin de famille canadien, 62(2), 145. https://pubmed.ncbi.nlm.nih.gov/26884528/
26.
Quach, D. T., Le, Y. T., Mai, L. H., Hoang, A. T., & Nguyen, T. T. (2020). Short Meal-to-Bed Time Is a Predominant Risk Factor of Gastroesophageal Reflux Disease in Pregnancy. Journal of clinical gastroenterology, 10.1097/MCG.0000000000001399. Advance online publication. https://doi.org/10.1097/MCG.0000000000001399
27.
Izci Balserak, B., Jackson, N., Ratcliffe, S. A., Pack, A. I., & Pien, G. W. (2013). Sleep-disordered breathing and daytime napping are associated with maternal hyperglycemia. Sleep & breathing = Schlaf & Atmung, 17(3), 1093–1102. https://doi.org/10.1007/s11325-013-0809-4
28.
Gaston, A., & Prapavessis, H. (2013). Tired, moody and pregnant? Exercise may be the answer. Psychology & health, 28(12), 1353–1369. https://doi. org/10.1080/08870446.2013.809084
org/10.1080/08870446.2013.809084
29.
Kusaka, M., Matsuzaki, M., Shiraishi, M., & Haruna, M. (2016). Immediate stress reduction effects of yoga during pregnancy: One group pre-post test. Women and birth : journal of the Australian College of Midwives, 29(5), e82–e88. https://doi.org/10.1016/j.wombi.2016.04.003
30.
Rodriguez-Blanque, R., Sánchez-García, J. C., Sánchez-López, A. M., Mur-Villar, N., & Aguilar-Cordero, M. J. (2018). The influence of physical activity in water on sleep quality in pregnant women: A randomised trial. Women and birth : journal of the Australian College of Midwives, 31(1), e51–e58. https://doi.org/10.1016/j.wombi.2017.06.018
Sleeping During Pregnancy (for Parents)
Reviewed by: Larissa Hirsch, MD
en español El sueño durante el embarazo
Why Does Pregnancy Sometimes Make Sleeping Difficult?
When you're pregnant, it can be hard to get a good night’s sleep. As you get bigger, it gets tougher to find a comfortable sleeping position. You may need to pee in the middle of the night. And heartburn can wake you up.
You may need to pee in the middle of the night. And heartburn can wake you up.
Some women have leg cramps and backaches, especially as they begin carrying more and more weight. Many pregnant women report that their dreams become more vivid than usual, and some even have nightmares.
Stress can interfere with sleep too. Maybe you're worried about your baby's health, anxious about your abilities as a parent, or feeling nervous about the delivery itself. All these feelings are normal, but they might keep you (and your partner) up at night.
How Can I Get a Better Night’s Sleep?
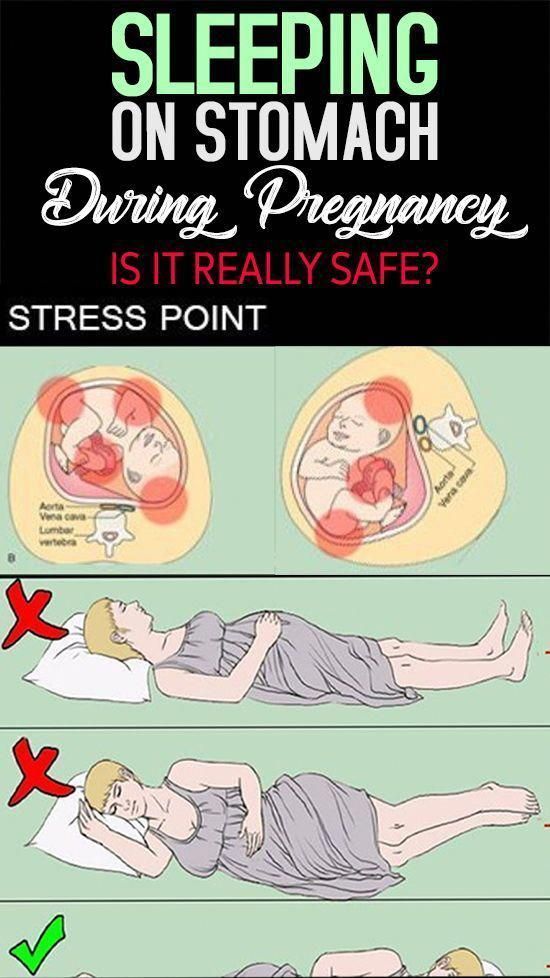
Early in your pregnancy, try to get into the habit of sleeping on your side. Lying on your side with your knees bent is likely to be the most comfortable position as your pregnancy progresses. It also makes your heart's job easier because it keeps the baby's weight from applying pressure to the large vein (called the inferior vena cava) that carries blood back to the heart from your feet and legs.
But don't drive yourself crazy worrying that you might roll over onto your back during the night. Shifting positions is a natural part of sleeping that you can't control.
Try experimenting with pillows to find a comfortable sleeping position. Some women place a pillow under their abdomen or between their legs. Also, using a bunched-up pillow or rolled-up blanket at the small of your back may help to relieve some pressure. In fact, you'll see many "pregnancy pillows" on the market. If you're thinking about buying one, talk with your doctor first about which might work for you.
Over-the-counter sleep aids, including herbal remedies, are not recommended for pregnant women.
Instead, these tips may safely improve your chances of getting a good night's sleep:
- Cut out caffeinated drinks like soda, coffee, and tea from your diet as much as possible. Restrict any intake of them to the morning or early afternoon.
- Avoid drinking a lot of fluids or eating a full meal within a few hours of going to bed.
 (But make sure that you also get plenty of nutrients and liquids throughout the day.) Some women find it helpful to eat more at breakfast and lunch and then have a smaller dinner. If nausea keeps you up, try eating a few crackers before you go to bed.
(But make sure that you also get plenty of nutrients and liquids throughout the day.) Some women find it helpful to eat more at breakfast and lunch and then have a smaller dinner. If nausea keeps you up, try eating a few crackers before you go to bed. - Get into a routine of going to bed and waking up at the same time each day.
- Avoid rigorous exercise right before you go to bed. Instead, do something relaxing, like reading a book or having a warm, caffeine-free drink, such as milk with honey or a cup of herbal tea.
- If a leg cramp awakens you, it may help to press your feet hard against the wall or to stand on the leg. Some women find that stretching their calf muscles before bed helps. Also, make sure that you're getting enough calcium and magnesium in your diet, which can help reduce leg cramps. But don't take any supplements without checking with your doctor.
- Take a yoga class or learn other relaxation techniques to help you unwind after a busy day.
 (Be sure to discuss any new activity or fitness regimen with your doctor first.)
(Be sure to discuss any new activity or fitness regimen with your doctor first.) - If fear and anxiety are keeping you awake, consider enrolling in a childbirth class or parenting class. More knowledge and the company of other pregnant women may help to ease the fears that keep you awake at night.
What If I Still Can't Sleep?
Of course, there will be times when you just can't sleep. Instead of tossing and turning, worrying that you're not asleep, and counting the hours until your alarm clock will go off, get up and do something calm: read a book, listen to music, or look at a magazine. Eventually, you'll probably feel tired enough to get back to sleep.
And if possible, take short naps (30–60 minutes) during the day. Naps can help you have energy to get through the day and give your body the rest it needs.
Reviewed by: Larissa Hirsch, MD
Date reviewed: May 2022
Miscarriage - causes timing signs of miscarriage
According to statistics, it is observed in one of 176 women. At the same time, it is difficult to guess which woman will have a fading pregnancy - age, social status and other factors are of secondary importance.
At the same time, it is difficult to guess which woman will have a fading pregnancy - age, social status and other factors are of secondary importance.
The concept of a missed pregnancy
A missed pregnancy means intrauterine death of the fetus, which occurs due to the development of irreversible processes. Thus, the development of the embryo stops, and its gradual decomposition occurs.
Missed pregnancy does not have severe symptoms that are characteristic of a miscarriage, but it is dangerous in its own way and needs to be diagnosed in a timely manner.
Missed pregnancy should be distinguished from another pathology - an empty fetal egg. This is a fertilized egg attached to the tissues of the uterus, but there is no embryo in it.
Causes
The most common factor in the fading of pregnancy are gene mutations, when the death of the embryo occurs for up to 8 weeks. In addition to chronic and hereditary diseases of future parents, the pathology can be provoked by the consumption of drugs and alcohol in large quantities, potent drugs. The risk of pathology increases when a woman continues to eat, smoke and drink alcoholic beverages.
The risk of pathology increases when a woman continues to eat, smoke and drink alcoholic beverages.
Sometimes the intake of potent medications that is not coordinated with the doctor becomes a factor in the fading of pregnancy. In this regard, in the first weeks of pregnancy, drug therapy is prescribed with extreme caution and in exceptional situations. After the 10th week, when the placenta is finally formed, the embryo is better protected from destructive external factors. Therefore, in the second trimester, taking the necessary medications can be resumed.
The risk of pregnancy failure is also increased in the following cases :
- Rh conflict between mother and child: this primarily concerns women with multiple miscarriages and a history of abortions. With each termination of pregnancy, the body is more willing to reject the fetus, which gradually reduces the chances of successfully bearing a child.
- Viral and infectious processes: in complicated forms, there is a high risk of infection of the unborn child and its abnormal development, as well as death.
 When infected with rubella, measles or chickenpox, pregnant women are advised to have an abortion. Otherwise, it will remain to raise a child with developmental disabilities, which doctors must warn about.
When infected with rubella, measles or chickenpox, pregnant women are advised to have an abortion. Otherwise, it will remain to raise a child with developmental disabilities, which doctors must warn about. - Hormonal disorders: with a deficiency of prolactin or an excess of testosterone, which is often manifested by irregular menstruation, the risk of miscarriage increases.
Multiple abortions, past cases of ectopic pregnancy and anomalies in the structure of the uterus are a reason for the special control of a pregnant woman. Close attention of a doctor is also required by women over 35 years old.
There is a high probability of pathology in women who neglect the management of pregnancy by a doctor. Therefore, for a successful delivery, registration with a specialist is required no later than 7-8 weeks of pregnancy.
It is also very important to undergo tests prescribed by narrow specialists - this is necessary for the early detection of genetic abnormalities and the prevention of serious complications.
Terms of increased risk
Cases of miscarriage are recorded at different terms, including when there are only a few days left before delivery. But, according to statistics, the greatest risks occur at certain times:
- 3-4 weeks after conception;
- 7-11 weeks;
- 16-18 weeks.
The highest percentage of missed pregnancies is determined by doctors before the 14th week, after the 20th week the embryo is already less vulnerable. In the first weeks, the fetus ceases to function due to hormonal surges and due to hereditary causes, after the first trimester, its development is interrupted by infectious and viral diseases.
Symptoms
In the early stages of pregnancy
Miscarriage is not expressed by acute clinical symptoms, so women often notice the pathology too late. However, it is deadly because the decomposition of the fetus causes intoxication of the mother's body. In the future, this has a bad effect on reproductive health and complicates attempts to bear a child in the future.
It is important to pay close attention to your condition in order to notice possible symptoms of a fading pregnancy in time:
- Vaginal discharge: first, about 48 hours, white discharge is noted, then mucus appears with bloody patches, bleeding gradually increases. So the body tries to expel the foreign body.
- Features of toxicosis: attachment of the fetus to the endometrium provokes the production of the hormone hCG, which causes vomiting. With a frozen pregnancy, the production of hCG stops, the feeling of nausea goes away. However, early diagnosis is not made. It happens that a decrease in the intensity of toxicosis is simply an adaptation of a woman's body to the presence of a fetus.
- Jumps in basal temperature: in the normal state, this figure does not exceed 37 ° C. After the death of the embryo, it decreases to 36.7 ° C, and when it decomposes, it rises sharply to 37.5 ° C.
- Feeling unwell: observed with a long decomposition of the fetus, when the pathology has not yet been identified - a woman regards a woman as feeling unwell as a cold, a general breakdown.
 Then there are other serious signs: dizziness, fever, abdominal cramps, anxiety.
Then there are other serious signs: dizziness, fever, abdominal cramps, anxiety.
In late pregnancy
In the second and third trimesters, the fetus gains weight well and grows to a large size. Therefore, in addition to the symptoms characteristic of pathology in the early stages, other manifestations are also observed:
- The fetus does not move for more than 24 hours.
- Stomach hurts and pulls.
- Leaking amniotic fluid with a characteristic putrid odor.
If the fetus does not move for more than 24 hours, another pathology is possible. Similar symptoms are characteristic of a lack of oxygen, which is caused by the umbilical cord wrapping around the neck and torso of the child. But it is also a reason for emergency medical attention, since a child wrapped around the umbilical cord can still be saved.
Regular breast assessments are recommended. With a frozen pregnancy for up to 25 weeks, after a few days, the mammary glands acquire their normal size. In the later stages, colostrum sometimes begins to stand out from the chest after the death of the fetus.
In the later stages, colostrum sometimes begins to stand out from the chest after the death of the fetus.
It is also possible to reduce the abdomen, which is caused by leakage of amniotic fluid. These are attempts by the body to expel the fetus, which has become a foreign body. Symptoms usually start within 2-3 days after the embryo has lost viability.
Diagnosis
Any of the above symptoms is a serious reason to visit a doctor and undergo the following diagnostic measures:
- visual examination in the gynecologist's office;
- hCG blood test;
- ultrasound;
- measurement of basal temperature.
Medical examination and ultrasound are the main research methods, blood sample and basal temperature measurement are auxiliary.
On ultrasound for up to 7 weeks, the fetus may not yet show signs of vital activity read by the device. Also, the reason for the lack of signs of life often becomes an incorrectly established gestational age. Therefore, abortion is sometimes delayed until a second ultrasound.
Therefore, abortion is sometimes delayed until a second ultrasound.
The fetus is delayed in development up to 4 weeks in case of stress loads or failures of the hormonal system. If, after a second ultrasound performed after 2 weeks, the fetus remains unchanged in size, this is a sign of its death.
Ultrasound is usually enough to make a diagnosis. In the first weeks, this is evidenced by the incorrect location and ruptures of the fetal egg. In the later stages, there is no heartbeat, the dimensions do not correspond to the deadline.
Treatment
If the diagnosis is confirmed, the woman is scheduled for an abortion. Each patient has their own method.
First trimester
Medical abortion is usually prescribed to terminate a missed pregnancy up to 9 weeks in Russia and up to 12 weeks in the West. The active ingredients are mifepristone and misoprostol. With high efficiency, this method has the following contraindications:
- ectopic pregnancy;
- severe anemia;
- renal and hepatic insufficiency;
- poor blood clotting.

Curettage is a traditional way of terminating a pregnancy, which is prescribed only for low effectiveness of medications and for cleaning the uterus from embryo fragments. Curettage is indicated until the 12th week of pregnancy. Whenever possible, doctors try to avoid this procedure, since irreversible consequences are possible as a result of trauma to the tissues of the reproductive organs.
Before the curettage procedure, a woman must undergo ultrasound, ECG, donate blood, consult an anesthesiologist. The scraping procedure consists of the following steps:
- Intravenous anesthesia (using a fast-acting agent).
- Treatment of the genitals with antiseptics.
- Fixation of the cervix with forceps and dilation of the cervical canal.
- Curettage of the mucous membranes of the uterus and cervical canal with a curette - a gynecological instrument with a loop at the end.
- Treatment of the uterus with drugs to stimulate contractions and a disinfectant iodine solution.

After the procedure is completed, the doctor removes the fixation instruments and applies a cold compress to the woman's abdomen. This helps to tone the uterus due to vasoconstriction. After 6-7 weeks, the menstrual cycle is restored.
Second trimester
At 13-22 weeks of pregnancy, other methods are used that cause artificial induction of labor:
- Intramial: 20% sodium chloride solution is injected into the water bladder with a special thin needle.
- Isolated: Mifepristone or misoprostol is injected into the genital tract, and one of these drugs is given by mouth.
In case of contraindications or low effectiveness of the above methods, a weight is applied to the pre- posed section of the amniotic sac.
Third trimester
In the third trimester, the only sure way is artificial labor, which is carried out urgently and without anesthesia. Cesarean section is excluded due to the high risk of infection of the woman.
Rehabilitation
In order for the results of treatment to give a positive effect, the woman must strictly follow the doctor's recommendations and continue rehabilitation therapy:
- Hormone therapy for the regeneration of uterine endometrial cells.
- Antibacterial therapy including macrolides or cephalosporins to prevent infection of the endometrium.
- Physiotherapy necessary for the healing of uterine tissues.
- Taking immunostimulating drugs.
Consequences
Termination of pregnancy, even for medical reasons, in any way, is a blow to the reproductive system of a woman. Therefore, a complete rehabilitation of the body is possible no earlier than six months later. All this time, hormone therapy is necessary in accordance with the doctor's recommendations.
If not properly treated, a missed pregnancy has a devastating effect on women's health and causes the following complications:
- Mental disorder: after an abortion, a woman has doubts about the next attempts to become pregnant and bear a child, fear of failure grows.
 Therefore, treatment must be accompanied by competent psychotherapy.
Therefore, treatment must be accompanied by competent psychotherapy. - Inflammatory processes in the uterus: this common complication occurs after curettage, because during the procedure the mucous membranes are stopped and the tissues of the uterus remain defenseless against bacteria.
- Adhesive processes: adhesion and adhesion of the inner surfaces of the uterus to each other is usually the result of inflammation. This provokes deformation of the uterus, which, if not properly treated, most likely leads to infertility.
Infertility, the most serious complication of a miscarriage, results from non-compliance with medical recommendations and improper treatment. Therefore, it is not enough to terminate a frozen pregnancy. Throughout the rehabilitation period and until a new pregnancy, a woman should be regularly observed by a gynecologist.
Prevention
In order for the pathology not to recur, competent preparation for pregnancy should not be neglected. Future parents must undergo a comprehensive medical examination, including blood samples, genetic tests, ultrasound screening and other procedures. The doctor may prescribe additional diagnostic procedures. You should not conceive a child if one of the spouses had rubella, chickenpox or severe flu less than six months ago. Pregnancy planning also includes the treatment of chronic diseases even before the first attempts at conception.
Future parents must undergo a comprehensive medical examination, including blood samples, genetic tests, ultrasound screening and other procedures. The doctor may prescribe additional diagnostic procedures. You should not conceive a child if one of the spouses had rubella, chickenpox or severe flu less than six months ago. Pregnancy planning also includes the treatment of chronic diseases even before the first attempts at conception.
Other preventive measures are also recommended:
- healthy lifestyle;
- timely vaccination;
- monitoring the state of the hormonal system;
- genetic counseling;
- refusal of air travel in the first weeks of pregnancy.
High-quality preparation is a proven factor for successful pregnancy and pregnancy. Even if a woman has previously experienced unsuccessful pregnancy attempts with miscarriages and missed pregnancy, competent planning gives a chance to endure and give birth to a healthy child at 90% of cases. After a diagnosed fading, it is necessary to plan a pregnancy with the support of multidisciplinary specialists and quality control over the woman's health.
After a diagnosed fading, it is necessary to plan a pregnancy with the support of multidisciplinary specialists and quality control over the woman's health.
“The fetus froze”, “The heart of the fetus stopped” - these phrases are heard by about 20% of Russian women during a routine routine examination or after an extended ultrasound. And then - the cruel "You will give birth again."
It seems that it is impossible to realize and accept: just yesterday you thought up a name for the baby you carried under your heart and managed to fall in love with, but today you have to come to terms with the loss of an unborn child.
“Twice in my life, doctors said the most important words —“ you are pregnant ”— and the most terrible —“ the pregnancy is frozen, we are preparing for hospitalization, ”writes our reader Elena. - The first time it happened during an ultrasound. I looked at the monitor, on which a little man with miniature arms and legs was already looming, the doctor moved the device over my stomach and noted something in the medical record. Everything happened as usual. And suddenly, for some reason, they began to call another gynecologist by phone. After a long deliberation, the doctors came up with a terrible verdict: “We are very sorry, but your fetus is dead.” It is the fetus, not the child. This happened at 24 weeks. Three years later, I managed to get pregnant again, but I stayed in an interesting position for only 7 weeks. My friends don't understand my grief. Everyone repeats like parrots: you will give birth again. I look at the only ultrasound of my first baby and I don't believe I can carry a baby. I am tormented by guilt in front of the baby, which doctors call the embryo.
Everything happened as usual. And suddenly, for some reason, they began to call another gynecologist by phone. After a long deliberation, the doctors came up with a terrible verdict: “We are very sorry, but your fetus is dead.” It is the fetus, not the child. This happened at 24 weeks. Three years later, I managed to get pregnant again, but I stayed in an interesting position for only 7 weeks. My friends don't understand my grief. Everyone repeats like parrots: you will give birth again. I look at the only ultrasound of my first baby and I don't believe I can carry a baby. I am tormented by guilt in front of the baby, which doctors call the embryo.
Elena Remez
ELENA REMEZ
Obstetrician-gynecologist, Candidate of Medical Sciences, leading specialist of the SM-Clinic holding
The first signs of missed pregnancy
term, - explains Elena Anatolyevna. - From the moment of conception to 8 weeks - the most important and decisive period in the development of the embryo.
 It is at this time that genetic mutations can occur, leading to severe malformations of the fetus and its death.
It is at this time that genetic mutations can occur, leading to severe malformations of the fetus and its death. A woman may independently suspect a missed pregnancy by indirect signs, for example, a sudden cessation of toxicosis, the appearance of pulling pains in the lower abdomen and spotting from the genital tract, the absence of pain in the chest (women may notice that their mammary glands have ceased to "pour" and abruptly decreased in size).
“If you notice something like this, you should immediately contact a gynecologist to clarify the situation and take timely measures. The doctor will prescribe an ultrasound scan and blood tests to confirm the diagnosis or refute suspicions, ”emphasizes Elena Anatolyevna.
Why does miscarriage occur?
In the first trimester, the main cause of miscarriage is genetic mutations, unfortunately, we cannot influence this. Also during this period, the embryo is more susceptible to the influence of negative external factors, so it is important to plan pregnancy and strictly adhere to a healthy lifestyle: exclude alcohol, do not take medications without consulting a doctor, postpone studies using x-rays, do not come into contact with chemicals.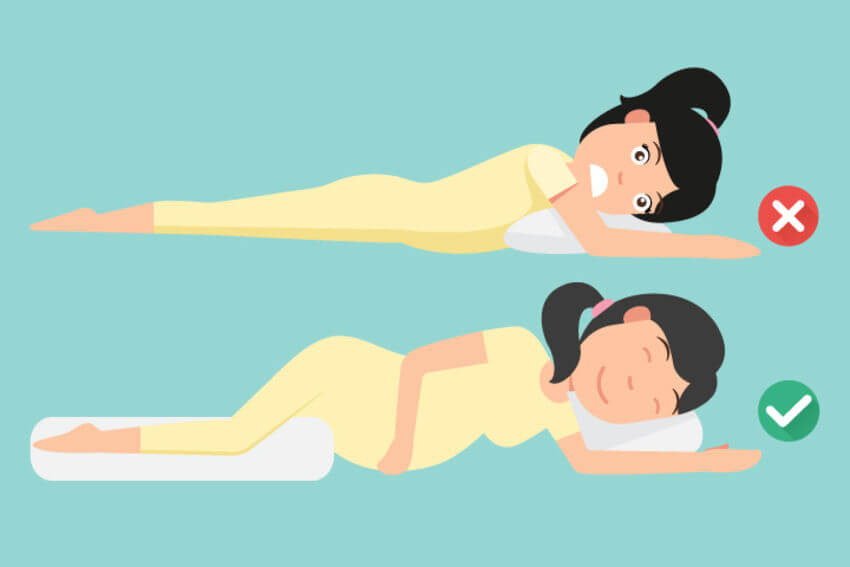
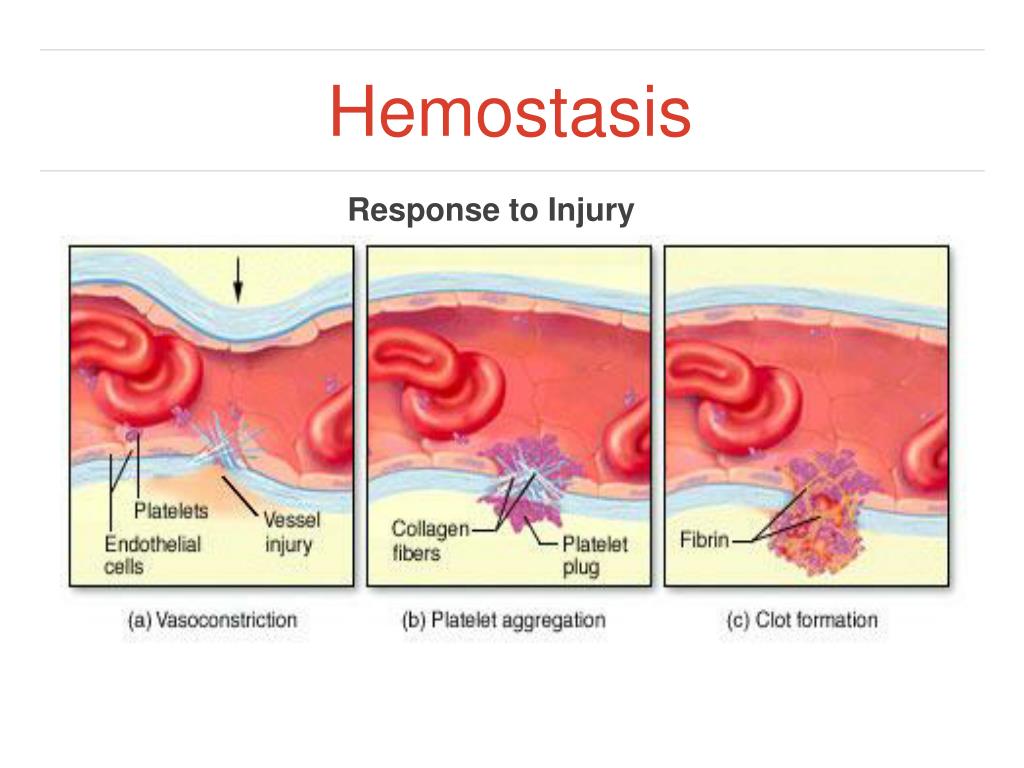
At the beginning of pregnancy, the expectant mother should try to avoid viral diseases. Even SARS can lead to sad consequences. The presence of problems associated with hormonal imbalance and hemostasis can also cause the death of the embryo, so it is important to find out all the risk factors before pregnancy.
Immune, hormonal and hemostatic system failures; acute and chronic processes in the uterus and appendages, pathological processes in the cervical canal, infections of the genital tract, as well as stress, work overload, an overly active lifestyle can cause fetal loss not only in the early stages, but also in the second and third trimesters .
Miscarriages may be due to past abortions, miscarriages or pelvic surgeries. To avoid this, doctors recommend conducting a pre-gravid examination - a medical examination of the state of the female body, during which various pathologies are detected before conception. History taking, blood tests, genetics consultation, screening for hereditary diseases.
When can I try to get pregnant again?
The period of rehabilitation depends on how long the pregnancy loss occurred. If this happened in the first trimester (the period from the 3rd to the 8th week is especially dangerous, when the internal organs of the child are being formed), then it will take six months to restore the body.
“During the first month, excessive physical activity, visits to baths, saunas, sexual intercourse are prohibited,” the doctor notes. “It is also recommended to undergo a full examination during this period, consult a psychologist and a geneticist.”
Treatment is individual for every woman. The doctor may prescribe hormone therapy, genetic studies, examinations for sexually transmitted infections, MRI of the pelvic organs, etc. In some cases, laparoscopy or hysteroscopy is necessary.
A missed pregnancy is not a sentence
“If a woman has already had a missed pregnancy in her anamnesis, what should be done to prevent this from happening again?”. This question often worries patients, says the doctor. - I want to immediately reassure expectant mothers: a missed pregnancy is not a sentence, but a serious reason to undergo a full examination, which will help identify the cause of the loss of a child, if possible, eliminate it or correct it with medications. This will allow you to plan a future pregnancy as safely as possible.
This question often worries patients, says the doctor. - I want to immediately reassure expectant mothers: a missed pregnancy is not a sentence, but a serious reason to undergo a full examination, which will help identify the cause of the loss of a child, if possible, eliminate it or correct it with medications. This will allow you to plan a future pregnancy as safely as possible.
There is a chance to carry and give birth to a healthy child even after two or more missed pregnancies. There are many happy examples in medical practice when women already despaired of becoming mothers, but fate gave them such an opportunity.
Unfortunately, the loss of a child at an early stage of pregnancy is quite common. After the first miscarriage, a woman lives in constant fear and is afraid that the second attempt to become a mother will turn into a tragedy.
“A miscarriage is a spontaneous termination of pregnancy before the fetus reaches a viable term. A fetus weighing up to 500 g is considered viable, which corresponds to a period of less than 22 weeks of pregnancy. Many women face this diagnosis. About 80 percent of miscarriages occur before 12 weeks of pregnancy.”
Many women face this diagnosis. About 80 percent of miscarriages occur before 12 weeks of pregnancy.”
Causes of miscarriage
Approximately half of early miscarriages occur due to genetic pathologies in the development of the fetus, that is, defects in the number and composition of chromosomes. It is in the first weeks that the formation of the baby's organs begins, which requires 23 normal chromosomes from each of the future parents. When at least one abnormal changes occur, there is a risk of losing a child.
At 8-11 weeks the rate of such miscarriages is 41-50%, at 16-19weeks of pregnancy, the frequency of miscarriages caused by chromosomal defects drops to 10 to 20 percent.
There are other causes of miscarriage. Among them:
- Congenital and acquired disorders of the anatomy of the genital organs If there are fibroids, polyps in the uterus, this can cause abnormal development of the embryo. The threat of miscarriage may be in women with an abnormal development of the uterus.

- Infectious causes Numerous studies have shown that the risk of miscarriage increases with sexually transmitted infections. Dangerous for a pregnant woman are measles, rubella, cytomegalovirus, as well as diseases that occur with an increase in body temperature. Intoxication of the body often leads to the loss of a child.
- Endocrine causes Problems with childbearing occur with diabetes, thyroid disease, and adrenal disorders.
- Unfavorable ecology, exposure
- Blood clotting disorders (thrombosis, antiphospholipid syndrome) APS (antiphospholipid syndrome) is a disease in which the human body produces a lot of antibodies to phospholipids - the chemical structures that make up parts of cells. The body mistakenly perceives its own phospholipids as foreign and begins to defend itself against them: it produces antibodies to them that damage blood components. Blood clotting increases, microthrombi appear in small vessels that feed the fetal egg and placenta.
 Blood circulation in the fetal egg is disturbed. As a result, the pregnancy stops or the growth of the fetus slows down. Both of these lead to miscarriage. All this is due to the hormonal background that has changed during pregnancy.
Blood circulation in the fetal egg is disturbed. As a result, the pregnancy stops or the growth of the fetus slows down. Both of these lead to miscarriage. All this is due to the hormonal background that has changed during pregnancy. - Lifestyle and bad habits Nicotine addiction, alcohol use, obesity.
Is it possible to miss a miscarriage
Sometimes women mistake a miscarriage for normal menstruation. This occurs during the so-called biochemical pregnancy, when there is a violation of the implantation of the embryo at a very early stage and menstruation begins. But before the appearance of spotting, the test will show two strips.
The classic variant is when a miscarriage is manifested by bleeding against the background of a long delay in menstruation, which rarely stops on its own. Therefore, even if a woman does not follow the menstrual cycle, the signs of an interrupted pregnancy will be immediately noticed by the doctor during examination and ultrasound.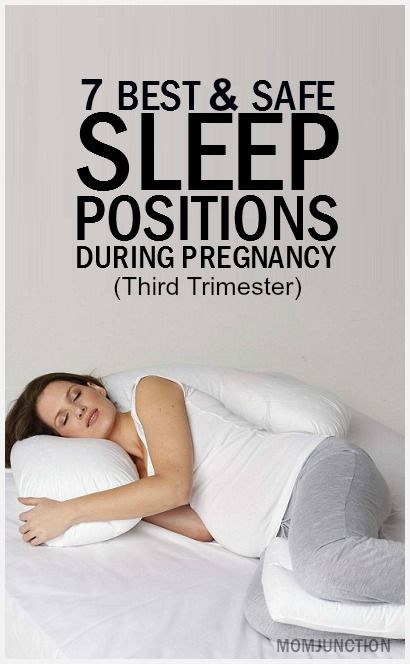
Alarm
Symptoms of a miscarriage can be completely different, and depending on them, as a rule, you can predict the likelihood of maintaining and successfully continuing this pregnancy.
For the threat of miscarriage is characterized by pulling pains in the lower abdomen and lumbar region, scanty bloody discharge from the genital tract. Ultrasound signs: the tone of the uterus is increased, the cervix is not shortened and closed, the body of the uterus corresponds to the gestational age, the fetal heartbeat is recorded.
Started miscarriage - pain and discharge from the genital tract are more pronounced, the cervix is ajar.
Miscarriage in progress - cramping pains in the lower abdomen, copious bloody discharge from the genital tract. On examination, as a rule, the uterus does not correspond to the gestational age, the cervix is open, the elements of the fetal egg are in the cervix or in the vagina.
Incomplete miscarriage - the pregnancy was interrupted, but there are delayed elements of the fetal egg in the uterine cavity. This is manifested by ongoing bleeding due to the lack of a full contraction of the uterus.
This is manifested by ongoing bleeding due to the lack of a full contraction of the uterus.
Non-progressive pregnancy - the death of an embryo (up to 9 weeks) or a fetus up to 22 weeks of gestation in the absence of any signs of termination of pregnancy.
Important!
Severe pain in the abdomen and bloody discharge at any stage of pregnancy is a reason for an urgent appeal to an obstetrician-gynecologist with a solution to the issue of hospitalization in a gynecological hospital.
Is it possible to avoid miscarriage
“Today, there are no methods to prevent miscarriages,” says the doctor. “Therefore, it is very important to comprehensively prepare for pregnancy before it occurs by visiting an obstetrician-gynecologist and following all the necessary recommendations for examination and taking the necessary drugs.”
But if, nevertheless, the pregnancy could not be maintained, then the birth of a child can be planned again no earlier than 3-6 months after the miscarriage. This time is needed to figure out, together with the attending physician, what are the causes of miscarriage and whether it is possible to avoid them in the future.
This time is needed to figure out, together with the attending physician, what are the causes of miscarriage and whether it is possible to avoid them in the future.
By the way, a common misconception for both women and men is that only the woman is to blame for the loss of pregnancy, but this is far from being the case.
“A man is also responsible, which is why future dads are required to perform a study - a spermogram and be screened for genital infections, since with a pathology of spermatozoa, the likelihood of miscarriage due to genetic abnormalities increases many times,” emphasizes our expert.
There is always a chance
Most women whose first pregnancy ends in miscarriage have a high chance of a successful next pregnancy (about 85 per cent) if they are examined before pregnancy and the causes are eliminated. “A woman who has lost a child needs the support of her family and friends. Sometimes words are unnecessary, just be there. Duty phrases from the series “You will definitely give birth”, “It was just an embryo” hurt very much. The best consolation is to advise you to see a doctor,” says Natalia Kalinina.
The best consolation is to advise you to see a doctor,” says Natalia Kalinina.
In a non-developing pregnancy, which is also called a "missed pregnancy", the death of the embryo/fetus occurs, but there are no clinical signs of spontaneous miscarriage.
Causes of miscarriage
The causes of miscarriage are very diverse, for example, stopping the development of the embryo/fetus may be due to an inflammatory process as a result of the action of various microorganisms. Most often, the causative agents of inflammation are: streptococci, staphylococci, E. coli, Klebsiella, rubella virus, cytomegalovirus, herpes simplex virus, Coxsackie virus, mycoplasmas, chlamydia, treponema, mycobacteria, toxoplasma, plasmodia, fungi (thrush).
Chronic infectious diseases in a woman most often do not directly lead directly to intrauterine death of the fetus, but cause certain disturbances in its development, which contribute to intrauterine death under the influence of other factors. For example, as a result of direct exposure to an infectious factor, a heart defect is formed in the fetus, which prevents its further normal development. However, not always and not every infection leads to the death of the embryo/fetus. In this case, the influence of the infection depends on the route of its penetration, the involvement of the fetus and amniotic membranes in the infection, the type and activity of the pathogen, the number of penetrating microorganisms, the duration of the mother's disease, the activity of the body's defenses, and other factors.
For example, as a result of direct exposure to an infectious factor, a heart defect is formed in the fetus, which prevents its further normal development. However, not always and not every infection leads to the death of the embryo/fetus. In this case, the influence of the infection depends on the route of its penetration, the involvement of the fetus and amniotic membranes in the infection, the type and activity of the pathogen, the number of penetrating microorganisms, the duration of the mother's disease, the activity of the body's defenses, and other factors.
Microorganisms can enter the uterus from the lower parts of the reproductive system, infecting the amniotic fluid, which is then swallowed by the fetus. The infection can spread through the amniotic membranes, and further to the fetus, causing damage to its internal organs, which, in turn, is the cause of its death. The infection can also get to the fetus from chronic foci of inflammation in the fallopian tubes and ovaries.
The death of the embryo/fetus may be due to a violation of the immune relationship, given that the fetal egg is half foreign to the mother's body. At the same time, rejection reactions are activated, aimed at defeating the fetal egg and removing it from the uterus. Non-developing pregnancy can be caused by various chromosomal disorders in the first 6-7 weeks of pregnancy, chromosomal changes are present in 60-75% of cases of spontaneous abortion, at 12-17 weeks. - in 20-25%, at 17-28 weeks. at 2-7%. With age, the likelihood of chromosomal abnormalities increases. The causes of the development of chromosomal disorders are also unfavorable external factors. The thrombotic complications caused by genetic defects in the blood coagulation system in a pregnant woman can cause an arrest in the growth and development of the embryo/fetus. The most common among them are: factor V Leiden mutation, prothrombin G202110A mutation, methyltetrahydrofolate reductase mutation, plasminogen activator gene polymorphism, platelet receptor polymorphism.
Disorders of the blood coagulation system caused by antiphospholipid syndrome also determine the unfavorable development of the embryo/fetus. In the early stages of pregnancy, the role of the direct damaging effect of antiphospholipid antibodies on the structures of the fetal egg, followed by spontaneous abortion, is not excluded. With this pathology, the process of implantation of the fetal egg is disrupted. In addition, with antiphospholipid syndrome, a decrease in the formation of placental vessels and a decrease in its function, which may be the cause of an undeveloped pregnancy. Another cause of impaired development of the embryo / fetus and placenta in antiphospholipid syndrome is thrombosis and damage to the uteroplacental vessels.
Hormonal changes are also distinguished among the causes of miscarriage. Violation of the formation and decrease in the function of the corpus luteum in the ovary leads to a decrease in progesterone and inadequate preparation of the uterus for implantation of the fetal egg. In this regard, the formation of uteroplacental circulation is disrupted, which entails a decrease in the blood supply to the embryo/fetus, and its death. Often, such disorders occur with excessive accumulation in the body of a woman of male sex hormones (Stein-Leventhal syndrome, adrenogenital syndrome), with reduced or increased thyroid function.
In this regard, the formation of uteroplacental circulation is disrupted, which entails a decrease in the blood supply to the embryo/fetus, and its death. Often, such disorders occur with excessive accumulation in the body of a woman of male sex hormones (Stein-Leventhal syndrome, adrenogenital syndrome), with reduced or increased thyroid function.
The shorter the gestational age, the higher the sensitivity of the embryo/fetus to the action of damaging factors. However, it decreases unevenly throughout fetal development. There are critical periods during pregnancy, in which the ovum, embryo, fetus are especially vulnerable to adverse effects: the implantation period (7-12 days), the embryogenesis period (3-8 weeks), the placenta formation period (up to 12 weeks), the formation period the most important functional systems of the fetus (20-24 weeks).
Clinical signs - symptoms of missed pregnancy
There are a number of consecutive disorders, characteristic of missed pregnancy : decrease and cessation of uteroplacental circulation against the background of damage to the structures of the placenta; cessation of uteroplacental circulation; violation of the structure of the inner layer of the uterus (endometrium), caused by the presence of dead elements of the fetal egg in the uterine cavity.
Clinical signs of miscarriage may be extremely poor against the background of the cessation of the increase in the size of the uterus and their inconsistency with the gestational age. However, the uterus can be of normal size, can be reduced, and can even be enlarged if it is filled with blood during detachment of the fetal egg.
For some time after the death of the embryo/fetus, the patient may feel pregnant. However, over time, the subjective signs of pregnancy gradually disappear. Smearing spotting from the genital tract and spastic pains in the abdomen are periodically noted. Chorionic gonadotropin in the blood of a woman, as a rule, is at an extremely low level or even completely absent.
Diagnosis of non-developing pregnancy
0290 ultrasound in the absence of a fetal heartbeat. One of the most common options for non-developing pregnancy is anembryony, i.e. the absence of an embryo in the cavity of the fetal egg after 5-6 weeks of pregnancy. In this case, the fetal egg is smaller than expected, and the embryo is not visualized.
In other cases of non-developing pregnancy, according to ultrasound, the fetal egg matches or lags in size in its development, the embryo can be visualized, but without a heartbeat. Often, a retrochorial hematoma can be detected, which is an accumulation of blood at the site of detachment of the fetal egg from the uterine wall.
With a longer stay of the dead embryo in the uterus, visualization of the embryo is impossible, there are no signs of its vital activity. The size of the uterus lags behind the gestational age, there is a deformation of the fetal egg with fuzzy contours.
Removal of the dead ovum
The death of the embryo/fetus is not always accompanied by its spontaneous expulsion from the uterus. Often there are cases when a dead fetal egg lingers in the uterus for an indefinitely long time. The reason for such a delay may be: primary tight attachment of the fetal egg to the uterine wall during implantation, inferiority of immune rejection reactions of the dead fetal egg, and a decrease in the contractile activity of the uterus.
If a dead embryo is in the uterus for 2-4 weeks or more, the elements of the decay of the dead fetal egg enter the maternal bloodstream, which leads to a violation of the blood coagulation system and can cause massive bleeding when trying to terminate the pregnancy. In this regard, before curettage of the uterus in order to remove the dead fetal egg, it is necessary to perform studies of the state of the blood coagulation system and, if necessary, conduct appropriate treatment.
After a thorough examination and appropriate preparation of the woman (carrying out therapeutic and preventive measures aimed at reducing the risk of possible complications), it is necessary to terminate the miscarriage. For this purpose, instrumental or drug-induced dilation of the cervix and instrumental removal of the contents of the uterus are performed. It is also possible to use special medications for non-operative removal of the ovum from the uterus. An ultrasound scan should be performed immediately during the abortion or immediately after it is completed to ensure that parts of the fetus and placenta have been completely removed. After removal of the fetal egg in non-developing pregnancy, regardless of the method of termination, it is advisable to conduct anti-inflammatory treatment.
After removal of the fetal egg in non-developing pregnancy, regardless of the method of termination, it is advisable to conduct anti-inflammatory treatment.
In each case of a non-developing pregnancy, an in-depth examination is required to identify possible causes of abortion with their subsequent elimination or weakening of the effect.
How to reduce the risk of embryo death?
To reduce the likelihood of possible damaging factors in the course of pregnancy, it is necessary to conduct screening examinations of patients planning pregnancy, as well as women in the early stages of pregnancy for urogenital infection. It is also important to conduct medical genetic counseling in order to identify high-risk groups for congenital and hereditary pathologies. In the presence of endocrine causes of miscarriage, appropriate corrective hormonal therapy should be selected.
It is also important to identify various autoimmune disorders and their correction. Re-pregnancy is possible when the identified causes of embryo/fetal death are eliminated, and after the necessary treatment has been carried out. In case of a new pregnancy, an ultrasound examination is performed, markers of possible fetal developmental disorders are determined in the blood, including: α - fetoprotein, chorionic gonadotropin, PAPP-A test in the most informative terms. According to indications, invasive prenatal diagnostics is also carried out, including chorion biopsy, amniocentesis or cordocentesis to determine chromosomal and a number of monogenic diseases of the fetus. In addition, they carry out therapeutic and preventive measures aimed at eliminating the infectious process, conduct specific anti-inflammatory therapy in combination with immunocorrectors, correct violations of the blood coagulation system and prevent placental insufficiency from 14-16 weeks of pregnancy.
Re-pregnancy is possible when the identified causes of embryo/fetal death are eliminated, and after the necessary treatment has been carried out. In case of a new pregnancy, an ultrasound examination is performed, markers of possible fetal developmental disorders are determined in the blood, including: α - fetoprotein, chorionic gonadotropin, PAPP-A test in the most informative terms. According to indications, invasive prenatal diagnostics is also carried out, including chorion biopsy, amniocentesis or cordocentesis to determine chromosomal and a number of monogenic diseases of the fetus. In addition, they carry out therapeutic and preventive measures aimed at eliminating the infectious process, conduct specific anti-inflammatory therapy in combination with immunocorrectors, correct violations of the blood coagulation system and prevent placental insufficiency from 14-16 weeks of pregnancy.
Appointment to specialists by phone of a single call center: +7 (495) 636-29-46 (m. "Shchukinskaya" and "Street of 1905 Goda"). You can also make an appointment with a doctor on our website, we will call you back!
"Shchukinskaya" and "Street of 1905 Goda"). You can also make an appointment with a doctor on our website, we will call you back!
Do you feel like sleeping all the time during pregnancy? 13 Ways to Cope
Headings : Pregnancy, Main Tags : first trimester, fatigue
Fatigue, weakness, drowsiness - this is what almost every woman faces at some point in her pregnancy. Most often this occurs during the first trimester, and sometimes returns towards the end of pregnancy. You will be surprised how much such fatigue can affect your life. This is not just ordinary fatigue, and you may find yourself sleeping at the most unexpected moments. Have you bought tickets for the premiere of a promising performance? Before leaving, I overcame a dream. Important meeting at work? You can fall asleep even during the lunch break before it. Want to have amazing, pregnancy hormone-boosted sex with your husband? They wanted to, but a minute later they were in the arms of Morpheus. To make sure you miss fewer important events, try these tips to deal with the weakness that makes you fall asleep at every possible moment.
To make sure you miss fewer important events, try these tips to deal with the weakness that makes you fall asleep at every possible moment.
Advice #1: Sleep whenever possible
Short naps during the day will be your friend, as will rising late and going to bed early. You are growing a whole new person inside, give yourself a break and increase the amount of time you spend sleeping. A growing baby takes all your energy, so give yourself a chance to recover. Even a short 20 minutes of sleep during the day can revitalize you for the rest of the day.Tip #2: Find some time to rest
You don't need to sleep to re-energize, even just resting can refresh you. At the end of pregnancy, a baby jumping on your bladder, combined with a large belly and an inability to find a comfortable position, can keep you awake. Instead of getting up and going to wash the stove, try to just relax. Soak in the bath, read a book, listen to soothing music, or meditate—do things that help you feel calm and relaxed.
Tip #3: Listen to your body
From the moment your pregnancy test came back positive, you must have felt that your body is amazing. And it is also very wise, so you should listen to its tips. If you feel weak, rest. Pregnancy takes a lot of energy, so you need to take better care of yourself than before.Tip #4: Drink Enough Fluid
People are often surprised to discover how much they are affected by enough or not enough fluids. During pregnancy, you should drink about eight glasses of water a day. Dehydration feels like a lack of energy and focus, so try increasing your water intake and see if you feel better. If you don't like the taste of water, you can add a slice of lemon or cucumber.Tip #5: Eat well
Your baby will take everything it needs to grow from your body - so you'll have to make sure you get all the nutrients you need to function well - from a healthy, balanced diet rich in fresh vegetables, protein, and healthy fats (especially omega 3s). , 6 and 9) - such as almonds, salmon or avocado, coconut oil and chia seeds. Nuts and seeds are a great snack during the day and can give you extra energy. Legumes, whole grains, berries and green leafy vegetables. What you don't eat is just as important as what you eat. If you often eat sweets, processed foods, or junk food, this can affect your level of fatigue. These foods are often high in sugar, and you will have to suffer a sharp drop in blood sugar after two hours. Such food is harder to digest, which means that your energy will be wasted on assimilating this food. Try eliminating, or at least reducing, these foods for a couple of weeks and see if you notice an increase in your energy levels.
, 6 and 9) - such as almonds, salmon or avocado, coconut oil and chia seeds. Nuts and seeds are a great snack during the day and can give you extra energy. Legumes, whole grains, berries and green leafy vegetables. What you don't eat is just as important as what you eat. If you often eat sweets, processed foods, or junk food, this can affect your level of fatigue. These foods are often high in sugar, and you will have to suffer a sharp drop in blood sugar after two hours. Such food is harder to digest, which means that your energy will be wasted on assimilating this food. Try eliminating, or at least reducing, these foods for a couple of weeks and see if you notice an increase in your energy levels. Tip #6: Eat little and often
Many people only eat three meals a day, but you need to eat 5-6 times and less. Smaller, more frequent meals can help keep blood sugar levels more even, preventing energy drops. Try incorporating healthy snacks into your daily routine so you can eat more often.
Tip #7: Get regular exercise
When you suffer from weakness, exercise is the last thing you want to do. But it is likely that this will help to cope with weakness and increase energy levels. The more you move, the more your cells move - wake them up and you will feel energized. Even a 20-minute walk can give you the energy boost you need. It may seem like a huge effort, but think about it - you just have to go out and walk for 10 minutes and then come back home! Start small, and gradually increase the load until you have been exercising for half an hour every day. Yoga, Pilates, swimming and walking are popular activities for pregnant women, but you can also find something else to your taste - dancing or even special exercises with equipment. It's best to schedule your workouts at times during the day when you have a lot of energy.Tip #8: Talk to your boss
If your boss knows you're pregnant, you may be able to arrange flexible hours. For example, arriving late and leaving late if that allows you to get more sleep. Or schedule meetings or important meetings with clients for your peak performance. Think about how you can organize your workflow in the most efficient way and try to offer this to your bosses, they are often ready to meet you.
Or schedule meetings or important meetings with clients for your peak performance. Think about how you can organize your workflow in the most efficient way and try to offer this to your bosses, they are often ready to meet you. Tip #9: Be realistic
If you try to live the way you did before pregnancy, this can contribute to a constant feeling of tiredness. Just because you used to stay up late with your girlfriends in the middle of the work week doesn't mean you need it now. Replace evening meetings with joint dinners, calls or weekend meetings and give yourself the opportunity to go to bed early. Don't take on additional commitments at work and shorten your schedule where possible, give yourself a couple of weeks to recover before moving on to something new. Most often, the energy returns in the second trimester, and you will be able to catch up.Tip #10: Accept all offers of help
It's time to ask for help. Reach out to friends and family who might be involved in your life.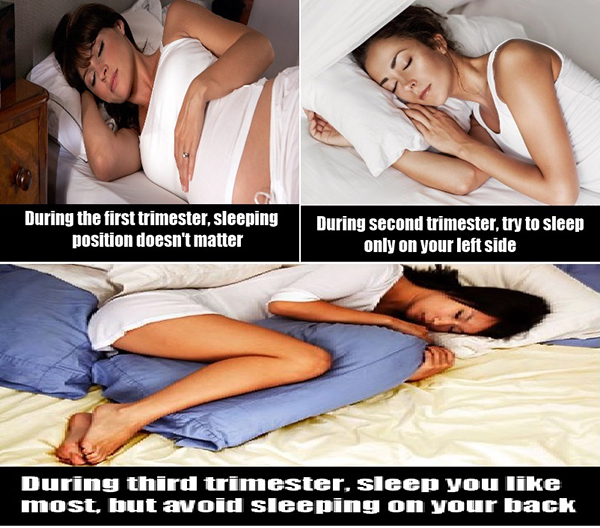 If you already have a child, ask someone you trust to take him to the playground for a couple of hours while you sleep. Ask your husband to take on more chores around the house so you can save energy to raise his child.
If you already have a child, ask someone you trust to take him to the playground for a couple of hours while you sleep. Ask your husband to take on more chores around the house so you can save energy to raise his child. Tip #11: Organize your to-do list
Sometimes, despite being tired, you will find yourself lying awake in bed at night, thinking about everything that is not yet done. Make a list and organize your to-dos to be more manageable—you don't have to redecorate your nursery in week eight, there's still plenty of time for that sort of thing. Focus on what needs to be done right now and make a schedule so you know when you need to get it done. Organizing your worries will give you a sense of control and allow you to sleep better at night.Tip #12: Make your bed beautiful
Your bed should be an oasis of calm, a haven of sleep that calls you to it. All distractions - phones, computers, TV, it is better to remove. The bed should be comfortable, clean, and there should be a lot of different pillows on it - during pregnancy, without them, it can be uncomfortable.