Dna test for down syndrome
FAQ: Cell-Free DNA Screening | Patient Education
- What is cell-free DNA screening?
- Does the test detect all pregnancies with Down syndrome and trisomies 18 and 13?
- What if cell-free DNA screening indicates a high risk?
- Who should consider cell-free DNA screening?
- Is cell-free DNA screening covered by insurance?
- Where can I find more information?
What is cell-free DNA screening?
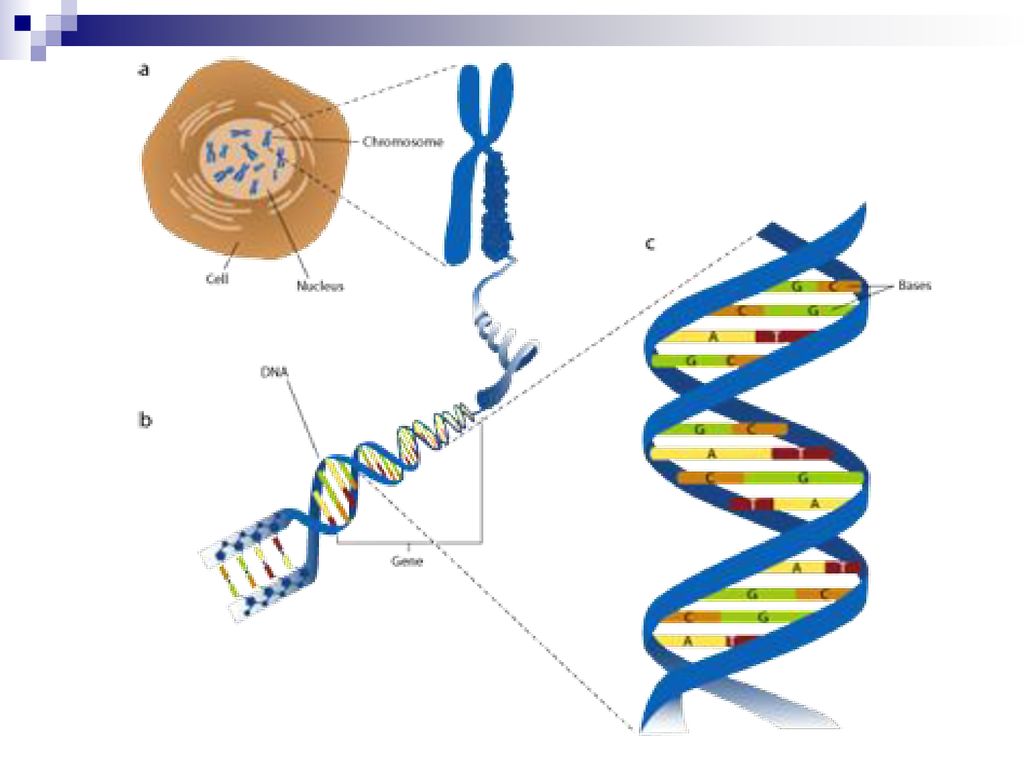
Cell-free DNA screening is a test that can determine if a woman has a higher chance of having a fetus with Down syndrome (trisomy 21), trisomy 18, trisomy 13 or an abnormality in the sex chromosomes (X and Y chromosomes).
With this test, a sample of the woman's blood is taken after 10 weeks of pregnancy. The test measures the small fragments of fetal DNA in the mother's blood, and can determine the chance of a chromosome problem based on the relative amount of DNA from chromosomes 21, 18, 13 and the sex chromosomes. The results are usually available within two weeks of the blood draw.
Does the test detect all pregnancies with Down syndrome and trisomies 18 and 13?
No. Cell-free DNA screening can detect more than 99 percent of Down syndrome pregnancies and 97 percent of trisomy 18 pregnancies. It detects about 87 percent of trisomy 13 pregnancies.
What if cell-free DNA screening indicates a high risk?
Women who are found to be at increased risk can have definitive testing with chorionic villus sampling (CVS) or amniocentesis to find out for sure. Whether or not to have diagnostic testing is a personal choice for each woman.
Who should consider cell-free DNA screening?
At the UCSF Prenatal Diagnostic Center, we offer cell-free DNA screening to women who have a higher than average chance of having a fetus with Down syndrome. This includes women who will be at least 35 years old at the time of their due date, those who are found to be at increased risk for Down syndrome or trisomy 18 with standard screening tests, and those who have had a previous pregnancy or baby with Down syndrome or trisomy 13 or 18.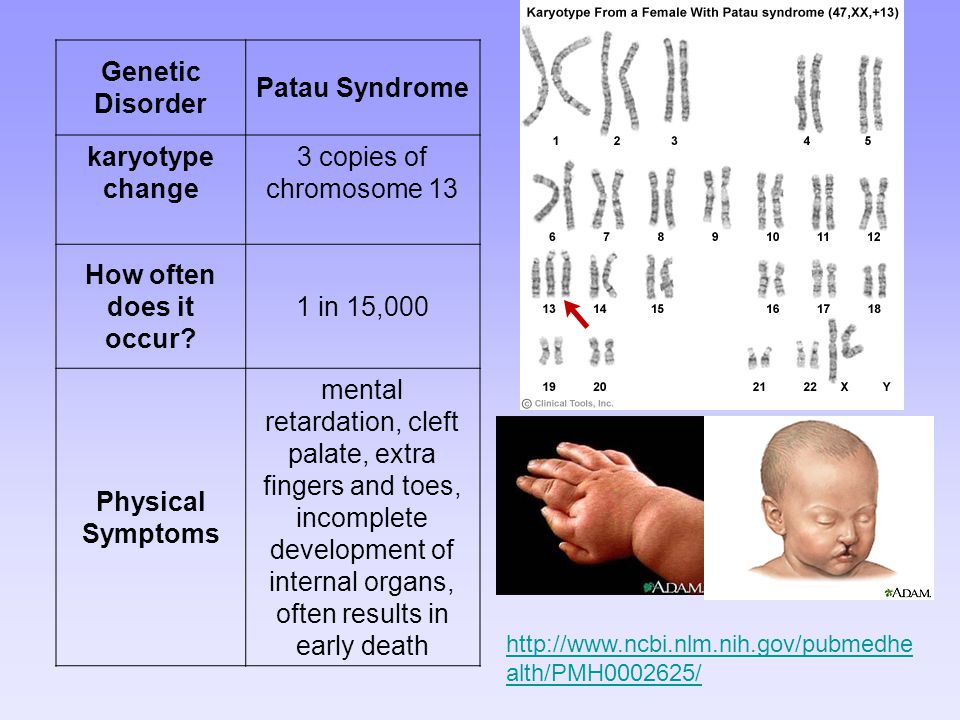
Women with a lower probability of Down syndrome can also have cell-free DNA screening, but we ask that they meet with a genetic counselor or other provider to discuss all of their testing options. The American College of Obstetricians and Gynecologists has suggested that traditional screening tests, which test for more disorders, remain the most appropriate choice for first-line screening for most women in the general population.
Cell-free DNA screening is not as accurate in women with twins, and cannot be used in women with triplets.
Is cell-free DNA screening covered by insurance?
Insurance coverage for this test varies based on individual plans, and not all insurance companies cover the testing for all patients. You should check with your insurer if you are interested in having this test.
Where can I find more information?
If you have additional questions about cell-free fetal DNA testing, please contact one of our genetic counselors at the UCSF Prenatal Diagnostic Center.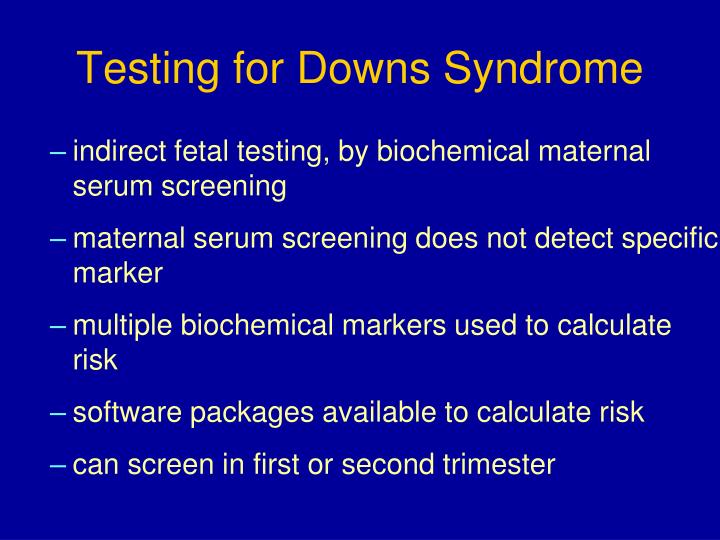 To talk with a genetic counselor or to schedule an appointment, call (415) 476-4080.
To talk with a genetic counselor or to schedule an appointment, call (415) 476-4080.
Prenatal Testing for Down Syndrome | Patient Education
Down syndrome is a genetic condition caused by extra genes from the 21st chromosome. It results in certain characteristics, including some degree of cognitive disability and other developmental delays. Common physical traits include an upward slant of the eyes; flattened bridge of the nose; single, deep crease on the palm of the hand; and decreased muscle tone. A child with Down syndrome, however, may not have all these traits.
The incidence of Down syndrome in the United States is about 1 in 1,000 births. There is no association between Down syndrome and culture, ethnic group, socioeconomic status or geographic region.
Age-Related Risks
Generally, the chance of having a Down syndrome birth is related to the mother's age. Under age 25, the odds of having a child with Down syndrome are about 1 in 1,400. At age 35, the odds are about 1 in 350.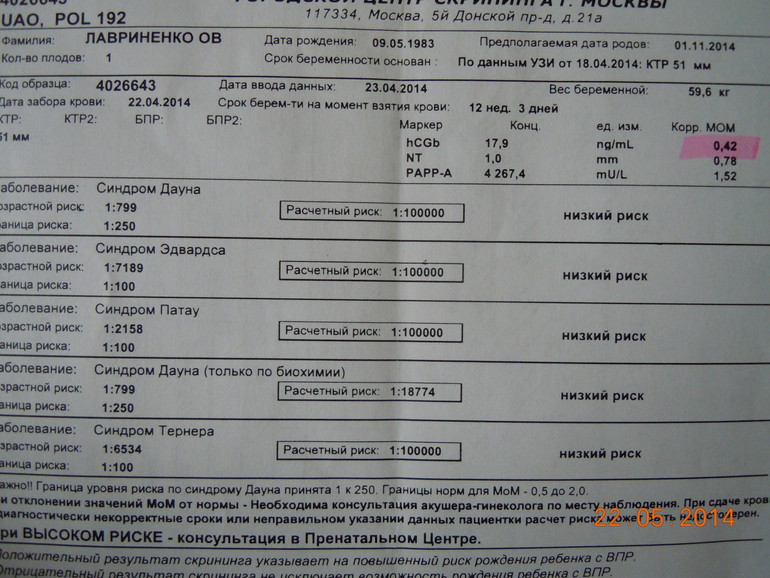 At age 40, the odds are about 1 in 100.
At age 40, the odds are about 1 in 100.
Causes of Down Syndrome
There are three causes of Down syndrome:
Trisomy 21
An estimated 95 percent of people with Down syndrome have trisomy 21, meaning they have three number 21 chromosomes instead of two. We normally have 23 pairs of chromosomes, each made up of genes. During the formation of the egg and the sperm, a woman's or a man's pair of chromosomes normally split so that only one chromosome is in each egg or sperm. In trisomy 21, the 21st chromosome pair does not split and a double dose goes to the egg or sperm. An estimated 95 to 97 percent of the extra chromosome is of maternal origin.
Translocation
Translocation occurs in about 3 to 4 percent of people with Down syndrome. In this type, an extra part of the 21st chromosome gets stuck onto another chromosome. In about half of these situations, one parent carries the extra 21st chromosome material in a "balanced" or hidden form.
Mosaicism
In mosaicism, the person with Down syndrome has an extra 21st chromosome in some of the cells but not all of them.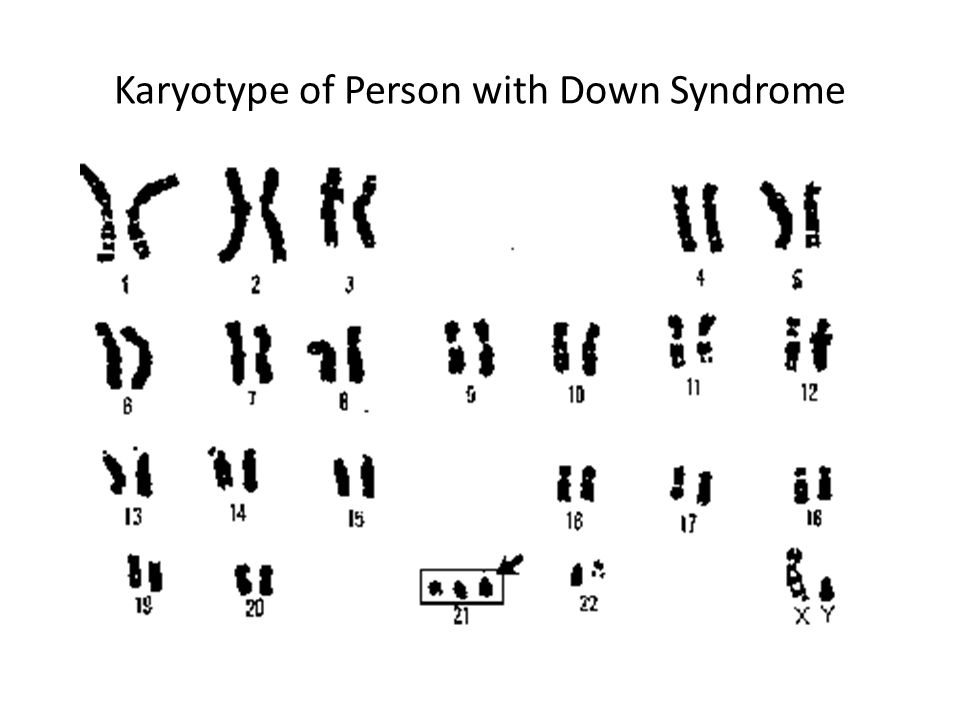 The other cells have the usual pair of 21st chromosomes. About 1 to 2 percent of people with Down syndrome have this type.
The other cells have the usual pair of 21st chromosomes. About 1 to 2 percent of people with Down syndrome have this type.
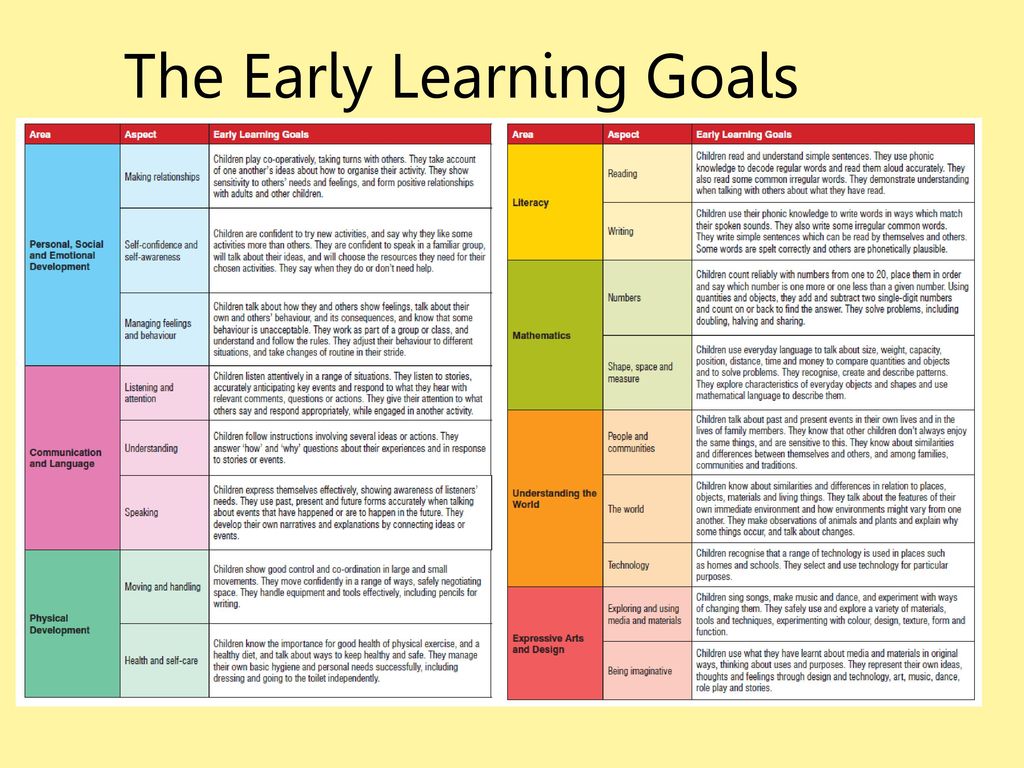
Prenatal Testing
Screening tests can identify women at increased risk of having a baby with Down syndrome. These tests have no risks of miscarriage, but can't determine with certainty whether a fetus is affected. Diagnostic tests, on the other hand, are extremely accurate at identifying certain abnormalities in the fetus, but carry a small — generally less than 1 percent — risk of miscarriage. We offer options for both screening and diagnostic testing.
Continue reading
Screening Tests
Sequential Integrated Screening — Sequential integrated screening is offered to all pregnant women by the state of California. This non-invasive screening is performed in two steps.
In the first step, which is performed between 10 and 14 weeks of pregnancy, a blood sample is taken from the mother and a nuchal translucency ultrasound is performed to measure the amount of fluid at the back of the baby's neck. If the blood test is scheduled prior to the ultrasound, we can provide the results at the end of the ultrasound appointment. The results of the blood test, the nuchal translucency measurement and the mother's age are used to estimate the risk for Down syndrome and trisomy 18.
If the blood test is scheduled prior to the ultrasound, we can provide the results at the end of the ultrasound appointment. The results of the blood test, the nuchal translucency measurement and the mother's age are used to estimate the risk for Down syndrome and trisomy 18.
The second step is a maternal blood test between 15 to 20 weeks of pregnancy. When the results of this blood test are combined with the results from the first trimester blood test and nuchal translucency ultrasound, the detection rate for Down syndrome increases. This test also provides a personal risk assessment for having a fetus with trisomy 18, Smith-Lemli-Opitz syndrome, an open neural tube defect or an abdominal wall defect.
Diagnostic Tests
Amniocentesis, chorionic villus sampling (CVS) and ultrasound are the three primary procedures for diagnostic testing.
Amniocentesis — Amniocentesis is used most commonly to identify chromosomal problems such as Down syndrome. When the fetus is known to be at risk, it can detect other genetic diseases like cystic fibrosis, Tay-Sachs disease and sickle cell disease.
An amniocentesis procedure for genetic testing is typically performed between 15 and 20 weeks of pregnancy. Under ultrasound guidance, a needle is inserted through the abdomen to remove a small amount of amniotic fluid. The cells from the fluid are then cultured and a karyotype analysis — an analysis of the chromosomal make-up of the cells — is performed. It takes about two weeks to receive the results of the test.
Amniocentesis detects most chromosomal disorders, such as Down syndrome, with a high degree of accuracy. Testing for other genetic diseases, such as Tay-Sachs disease, is not routinely performed but can be detected through specialized testing if your fetus is known to be at risk. Testing for neural tube defects, such as spina bifida, also can be performed.
There is a small risk of miscarriage as a result of amniocentesis — about 1 in 100 or less. Miscarriage rates for procedures performed at UCSF Medical Center are less than 1 in 350.
Chorionic Villus Sampling (CVS) — Like amniocentesis, chorionic villus sampling is used most commonly to identify chromosomal problems such as Down syndrome. It can detect other genetic diseases like cystic fibrosis, Tay-Sachs disease and sickle cell disease in at-risk fetuses. The main advantage of CVS over amniocentesis is that it is done much earlier in pregnancy, at 10 to 12 weeks rather than 15 to 20 weeks.
It can detect other genetic diseases like cystic fibrosis, Tay-Sachs disease and sickle cell disease in at-risk fetuses. The main advantage of CVS over amniocentesis is that it is done much earlier in pregnancy, at 10 to 12 weeks rather than 15 to 20 weeks.
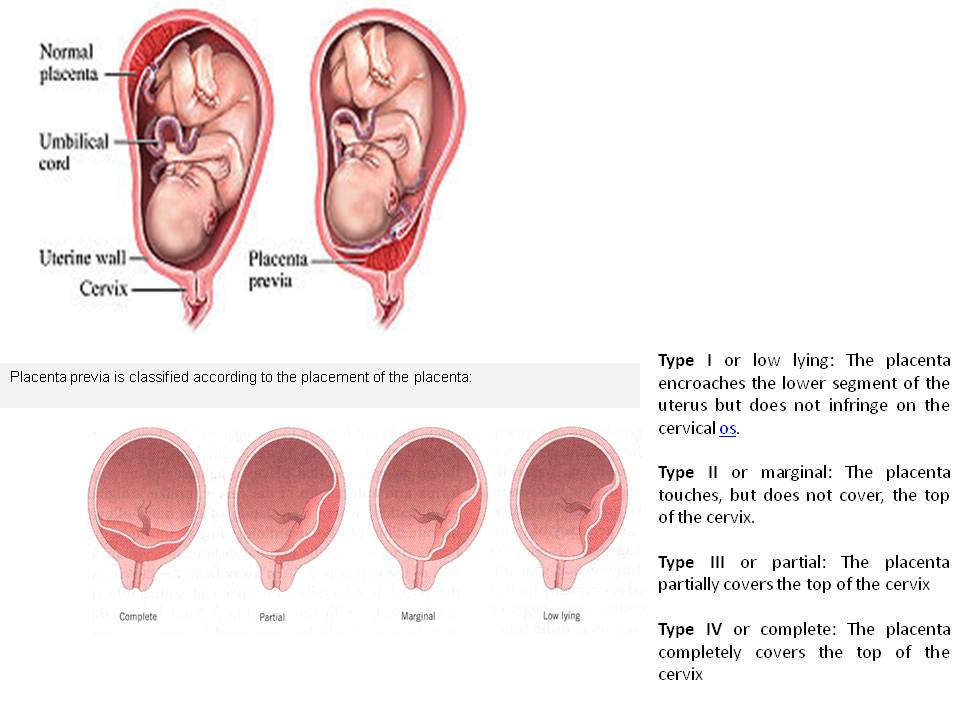
CVS involves removing a tiny piece of tissue from the placenta. Under ultrasound guidance, the tissue is obtained either with a needle inserted through the abdomen or a catheter inserted through the cervix. The tissue is then cultured and a karyotype analysis of the chromosomal make-up of the cells is performed. It takes about two weeks to receive the results.
The advantage of CVS over amniocentesis is that the test is performed much earlier in pregnancy, so results are typically available by the end of the third month. A disadvantage is that spinal cord defects cannot be detected. Expanded alpha fetoprotein (AFP) blood testing or ultrasound can be performed later in the pregnancy to screen for spinal cord defects.
There is a small risk of miscarriage as a result of CVS — 1 in 100 or less.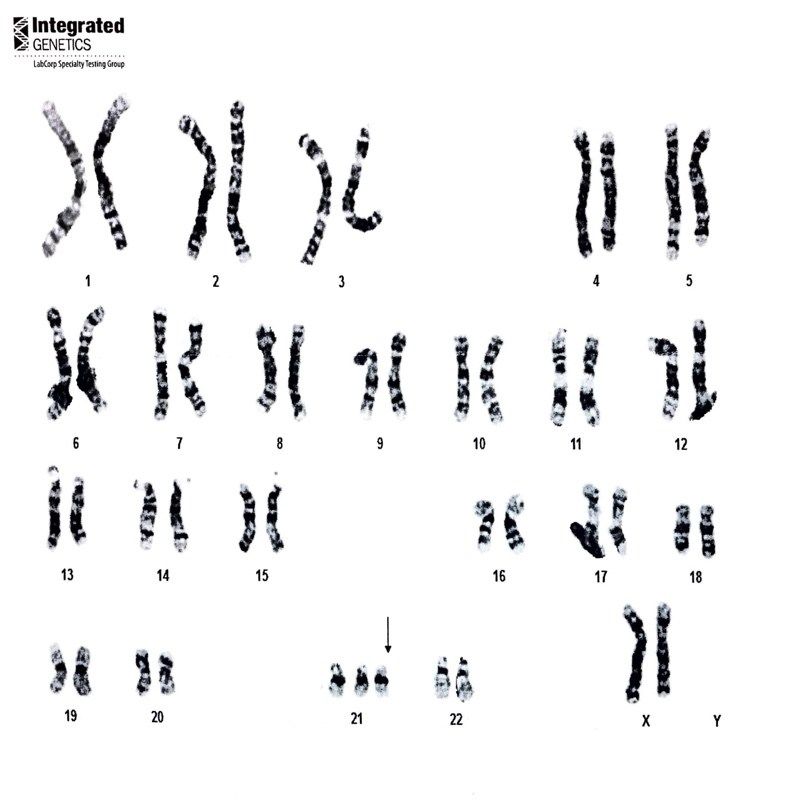 Miscarriage rates for procedures performed at UCSF Medical Center are less than 1 in 350.
Miscarriage rates for procedures performed at UCSF Medical Center are less than 1 in 350.
Ultrasound — The primary purpose of ultrasound is to determine the status of a pregnancy — the due date, size of the fetus and if the mother is carrying multiples. Ultrasound also can provide some information about possible birth defects in a fetus. All patients at UCSF Medical Center undergo a comprehensive ultrasound examination before any invasive tests are performed. Results of the ultrasound are explained at the time of the visit.
In some patients, an ultrasound raises concern of a possible abnormality in the fetus. We have extensive experience in performing and interpreting ultrasounds in pregnancy.
If You Receive a Positive Result
If you receive positive results on a screening test, we recommend that you discuss this with your doctor and a genetic counselor. Options for further diagnostic testing will be explained. The decision as to whether to have invasive genetic testing is up to you.
If a diagnostic test finds a genetic abnormality, the significance of such results should be discussed with experts familiar with the condition, including a medical geneticist and a genetic counselor, as well as your own doctor.
Panorama test, Down syndrome, Edwards syndrome and Patau syndrome
The Panorama test is a non-invasive prenatal, safe and accurate screening test for chromosomal disorders based on the study of extracellular DNA of the fetus in the mother's blood, which can be performed starting from the ninth week of pregnancy.
Panorama recognizes 99% of fetuses with Down syndrome, Edwards syndrome and Patau syndrome and 92% of fetuses with Turner syndrome.
Although the test is very accurate, Panorama is not a diagnostic test, so in the case of a positive Panorama test, an invasive examination is necessary to clarify the diagnosis (chorionic biopsy or amniotic fluid test). Loote Ultraheliskriining is collaborating with the Tallinn Genetics Center on invasive research.
Loote Ultraheliskriining is collaborating with the Tallinn Genetics Center on invasive research.
The Panorama test is completely safe for both you and your fetus, and the test does not endanger the pregnancy in any way. The screening test is performed from your venous blood.
Panorama test is indicated for women at risk *:
- Pregnant age 35 years at the time of delivery
- Increased risk of chromosomal pathology on fetal ultrasound
- Screening test of the first or second semester of a pregnant woman found an increased risk of chromosomal diseases
- Down syndrome during a previous pregnancy
- Balanced Robertsonian translocation in parents due to increased risk of Down syndrome or Patau syndrome.
This test is also used:
- Hereditary X-linked diseases in the family (to determine the sex of the fetus).
- Test sensitivity >99%.
Benefits of Panorama over other non-invasive screening tests:
- High disease detection
- Low false positive rate
- Shows also the risk of Patau syndrome and Turner syndrome
- Gives an opportunity to estimate the sex of the fetus
Panorama test not performed:
- If the child's NT (occipital translucency) is greater than 3.0 mm
- In case of multiple pregnancy
- In case of twin pregnancy, if one of the fetuses died
- In case of IVF pregnancy with donor egg
- If the pregnant woman had a bone marrow transplant before pregnancy
If the body mass index (BMI) of the pregnant woman is above 30 kg/m 2 , there is a danger that the blood test contains so little fetal extracellular DNA that a scraping from the father's mucosa will be needed to ensure an accurate diagnosis.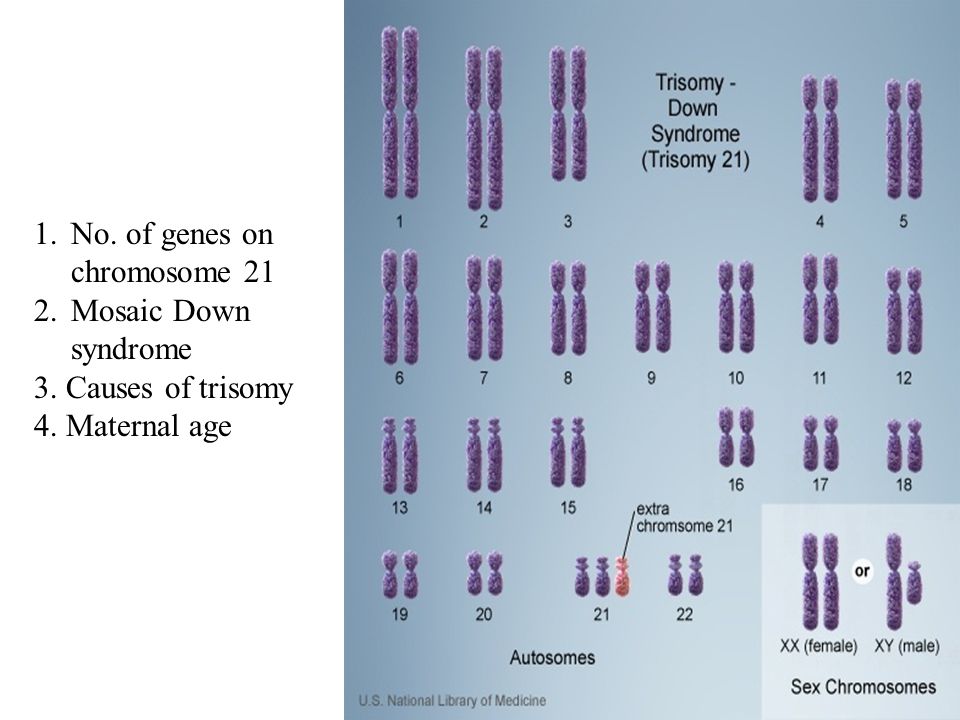 There is also a small chance that no result will come from your initial sample. In this case, we advise you to take a second venous blood test, in which case no additional fee is required.
There is also a small chance that no result will come from your initial sample. In this case, we advise you to take a second venous blood test, in which case no additional fee is required.
Since the Panorama test cannot evaluate fetal anatomy, neural tube pathology, risk of congenital heart disease, preeclampsia in pregnancy, fetal growth retardation and preterm birth, Loote Ultraheliskriining offers the OSCAR test as one part of the Panorama test, where the analysis maternal blood is done preferably at 10 weeks of gestation and ultrasound at 12 weeks of gestation. The results of the combined study, together with a detailed explanation of the test, will be received by the family immediately after the ultrasound examination.
In case of elevated NT ( nuchal translucency ) > 3.5 mm and euploid chromosome set, Loote Ultraheliskriining cooperates with the Tallinn Genetics Center in carrying out a genetic test based on the APEX method ( adrenogenital primer extension 901 syndrome, Noonan syndrome, Smith-Lemli-Opitz syndrome, spinal muscular atrophy) and in performing FISH (fluorescence in situ hybridization) analysis to detect 22q11.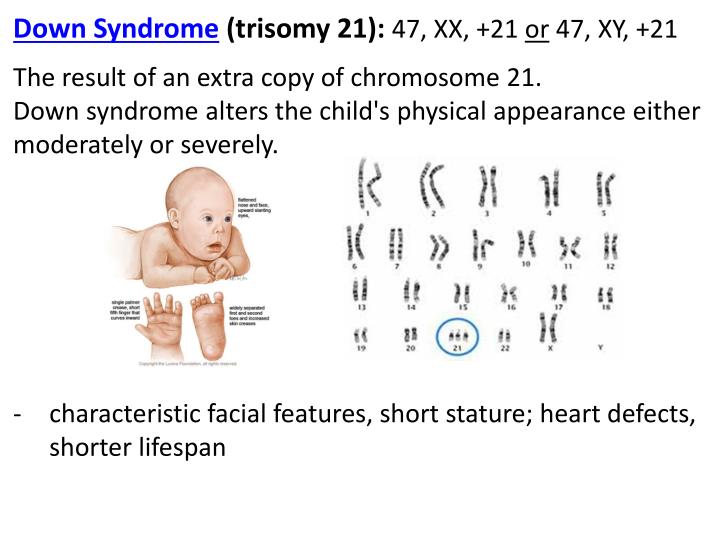 2 microdeletion syndrome (DiGeorge syndrome).
2 microdeletion syndrome (DiGeorge syndrome).
Read more:
- How does the Panorama test work?
- What will I learn by doing the Panorama test?
- Importance of identifying chromosomal abnormalities
- Administering the Panorama test to women at risk for the OSCAR test
- Patient Information Sheet
Not Found (#404)
Not Found (#404)
|