Blood clots in early pregnancy 4 weeks
Blood Clots During Pregnancy | American Pregnancy Association
Blood clots are serious concerns and even more so while you are pregnant. Developing a blood clot while pregnant has additional risks or concerns because of your developing baby, thankfully they are rare and there is little need for concern.
However, there are steps you can take to further minimize your risk of experiencing them while you are pregnant.
What is a Blood Clot?
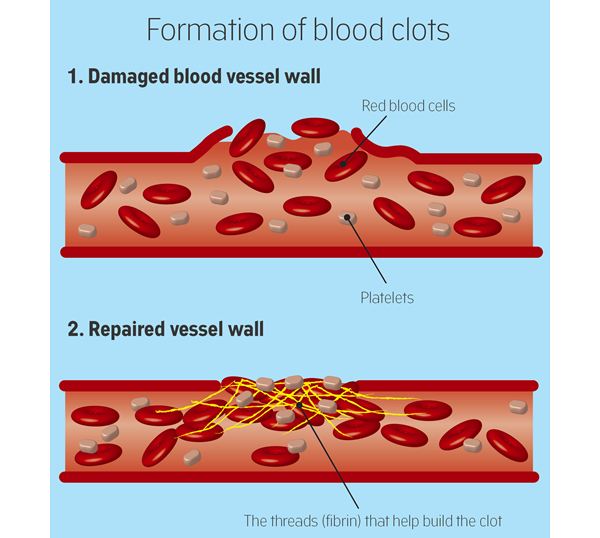
A blood clot occurs when your body sends cells, called platelets, to block the flow of blood. Normally, this occurs when you have a cut, to keep the injury from bleeding continuously. During pregnancy, your blood is more likely to clot as a safeguard against losing too much blood during labor.
However, a condition known as deep-vein thrombosis (DVT), which happens when blood clots form in the legs and pelvic region, can occur and is linked with a number of serious health concerns. The good news is there are ways to both prevent DVT and to treat it after it occurs.
Also, blood clots affect only 1 or 2 pregnant women out of every 1,000, so there is no need for alarm unless you feel you may be at risk.
What are the Causes of Blood Clots during Pregnancy?
Research has shown a number of possible causes of DVT, and it is important to note whether you fall into any of these categories. Women are most likely to experience a blood clot in their first three months of pregnancy or in the first six weeks after giving birth. If you believe you may be at risk for DVT, be sure to talk to your healthcare provider.
You could be at risk if:
- You or a close relative have experienced DVT before
- You smoke or are exposed to secondhand smoke frequently
- You are over 35 years old
- You are overweight
- You travel long distances while pregnant
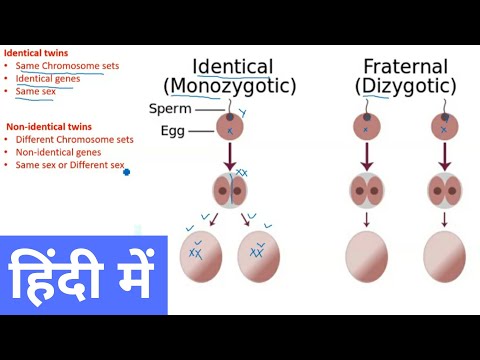
- You are expecting multiples
- You are sedentary for long periods of time
- You have a Cesarean section
Women tend to be more sensitive and aware of potential complications while they are pregnant.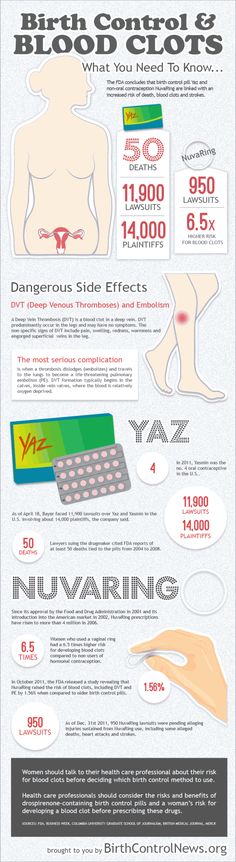 Although blood clots are unlikely, there are a few signs that can indicate the possibility of a blood clot.
Although blood clots are unlikely, there are a few signs that can indicate the possibility of a blood clot.
These include:
- Swelling or pain in one leg
- Pain that worsens when you walk
- Veins that look larger than normal
What are the Risks during Pregnancy?
DVT can seriously affect your pregnancy in a number of ways:
- Blood clots in the placenta
- Heart attack
- Stroke
- Pulmonary embolism, which is when blood clots break off and are lodged in the lungs
- Miscarriage
How can you Prevent and Treat Blood Clots?
Prevention of DVT is important and can be achieved by a healthy lifestyle. Staying active is a crucial component in combating DVT, so check with your healthcare provider to see which activities and types of exercises you can do. Regular exercise improves circulation and can keep clots from forming. It is also important to eat healthily, and if you are currently smoking, you should stop immediately. It is important to notify your healthcare provider if you feel you may be at risk of DVT.
It is important to notify your healthcare provider if you feel you may be at risk of DVT.
If you have been diagnosed with DVT, you will most likely be treated with an anticoagulant, which hinders the blood from clotting as easily.
Want to Know More?
- Pregnancy Exercise Guidelines
- Exercise Warning Signs
Compiled from the following Resources:
Blood Clotting and Pregnancy. (n.d.). Retrieved August 8, 2014, from https://www.hematology.org/Patients/Clots/Pregnancy.aspx
Preidt, R. (2014, April 2). Some Women at Risk for Blood Clots From Pregnancy. Retrieved August 8, 2014, from https://www.webmd.com/baby/news/20130402/study-pinpoints-women-at-risk-for-blood-clots-from-pregnancy
Blood Clots and Pregnancy. (2014, January 1). Retrieved August 8, 2014, from https://www.marchofdimes.org
Vaginal Bleeding and Blood Clots During Pregnancy
Written by Stephanie Watson
In this Article
- Bleeding in the First Trimester
- Bleeding in the Second and Third Trimesters
- What to Do If You Have Abnormal Bleeding During Pregnancy
Bleeding during pregnancy is common, especially during the first trimester, and usually it's no cause for alarm. But because bleeding can sometimes be a sign of something serious, it's important to know the possible causes, and get checked out by your doctor to make sure you and your baby are healthy.
But because bleeding can sometimes be a sign of something serious, it's important to know the possible causes, and get checked out by your doctor to make sure you and your baby are healthy.
Bleeding in the First Trimester
About 20% of women have some bleeding during the first 12 weeks of pregnancy. Possible causes of first trimester bleeding include:
Implantation bleeding. You may experience some normal spotting within the first six to 12 days after you conceive as the fertilized egg implants itself in the lining of the uterus. Some women don't realize they are pregnant because they mistake this bleeding for a light period. Usually the bleeding is very light and lasts from a few hours to a few days.
Miscarriage. Because miscarriage is most common during the first 12 weeks of pregnancy, it tends to be one of the biggest concerns with first trimester bleeding. However, first trimester bleeding does not necessarily mean that you’ve miscarried or will miscarry. In fact, if a heartbeat is seen on ultrasound, over 90% of women who experience first trimester vaginal bleeding will not miscarry.
In fact, if a heartbeat is seen on ultrasound, over 90% of women who experience first trimester vaginal bleeding will not miscarry.
Other symptoms of miscarriage are strong cramps in the lower abdomen and tissue passing through the vagina.
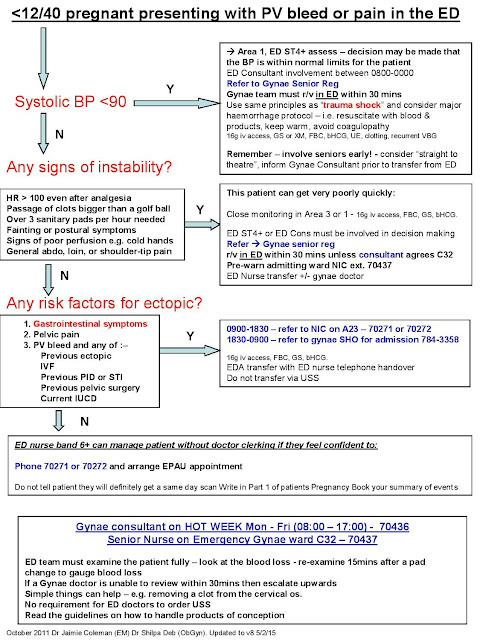
Ectopic pregnancy. In an ectopic pregnancy, the fertilized embryo implants outside of the uterus, usually in the fallopian tube. If the embryo keeps growing, it can cause the fallopian tube to burst, which can be life-threatening to the mother. Although ectopic pregnancy is potentially dangerous, it only occurs in about 2% of pregnancies.
Other symptoms of ectopic pregnancy are strong cramps or pain in the lower abdomen, and lightheadedness.
Molar pregnancy (also called gestational trophoblastic disease). This is a very rare condition in which abnormal tissue grows inside the uterus instead of a baby. In rare cases, the tissue is cancerous and can spread to other parts of the body.
Other symptoms of molar pregnancy are severe nausea and vomiting, and rapid enlargement of the uterus.
Additional causes of bleeding in early pregnancy include:
- Cervical changes. During pregnancy, extra blood flows to the cervix. Intercourse or a Pap test, which cause contact with the cervix, can trigger bleeding. This type of bleeding isn't cause for concern.
- Infection. Any infection of the cervix, vagina, or a sexually transmitted infection (such as chlamydia, gonorrhea, or herpes) can cause bleeding in the first trimester.
Bleeding in the Second and Third Trimesters
Abnormal bleeding in late pregnancy may be more serious because it can signal a problem with the mother or baby. Call your doctor as soon as possible if you experience any bleeding in your second or third trimester.
Possible causes of bleeding in late pregnancy include:
Placenta previa. This condition occurs when the placenta sits low in the uterus and partially or completely covers the opening of the birth canal. Placenta previa is very rare in the late third trimester, occurring in only one in 200 pregnancies. A bleeding placenta previa, which can be painless, is an emergency requiring immediate medical attention.
A bleeding placenta previa, which can be painless, is an emergency requiring immediate medical attention.
Placental abruption. In about 1% of pregnancies, the placenta detaches from the wall of the uterus before or during labor and blood pools between the placenta and uterus. Placental abruption can be very dangerous to both the mother and baby.
Other signs and symptoms of placental abruption are abdominal pain, clots from the vagina, tender uterus, and back pain.
Uterine rupture. In rare cases, a scar from a previous C-section can tear open during pregnancy. Uterine rupture can be life-threatening, and requires an emergency C-section.
Other symptoms of uterine rupture are pain and tenderness in the abdomen.
Vasa previa. In this very rare condition, the developing baby's blood vessels in the umbilical cord or placenta cross the opening to the birth canal. Vasa previa can be very dangerous to the baby because the blood vessels can tear open, causing the baby to bleed severely and lose oxygen.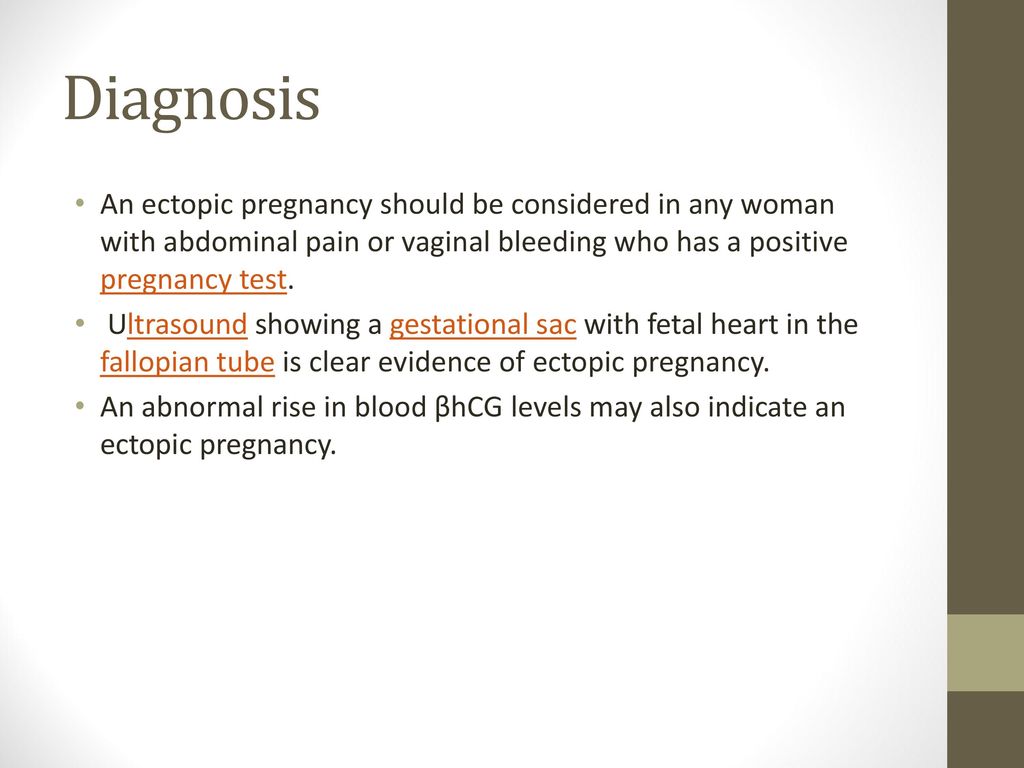
Other signs of vasa previa include abnormal fetal heart rate and excessive bleeding.
Premature labor. Vaginal bleeding late in pregnancy may just be a sign that your body is getting ready to deliver. A few days or weeks before labor begins, the mucus plug that covers the opening of the uterus will pass out of the vagina, and it will usually have small amounts of blood in it (this is known as "bloody show"). If bleeding and symptoms of labor begin before the 37th week of pregnancy, contact your doctor right away because you might be in preterm labor.
Other symptoms of preterm labor include contractions, vaginal discharge, abdominal pressure, and ache in the lower back.
Additional causes of bleeding in late pregnancy are:
- Injury to the cervix or vagina
- Polyps
- Cancer
What to Do If You Have Abnormal Bleeding During Pregnancy
Because vaginal bleeding in any trimester can be a sign of a problem, call your doctor. Wear a pad so that you can keep track of how much you're bleeding, and record the type of blood (for example, pink, brown, or red; smooth or full of clots). Bring any tissue that passes through the vagina to your doctor for testing. Don't use a tampon or have sex while you are still bleeding.
Bring any tissue that passes through the vagina to your doctor for testing. Don't use a tampon or have sex while you are still bleeding.
Your doctor might recommend that you rest as much as you can and avoid exercise and travel.
You should expect to receive an ultrasound to identify what the underlying cause of your bleeding may be. Vaginal and abdominal ultrasounds are often performed together as part of a full evaluation.
Go to the emergency room or call 911 right away if you have any of the following symptoms, which could be signs of a miscarriage or other serious problem:
- Severe pain or intense cramps low in the abdomen
- Severe bleeding, with or without pain
- Discharge from the vagina that contains tissue
- Dizziness or fainting
- A fever of more than 100.4 or more degrees Fahrenheit and/or chills
Health & Pregnancy Guide
- Getting Pregnant
- First Trimester
- Second Trimester
- Third Trimester
- Labor and Delivery
- Pregnancy Complications
- All Guide Topics
Risk of thrombosis during pregnancy
Deep vein thrombosis is the formation of a clot (thrombus) in the lumen of a vessel (in this case, deep veins located in the thickness of the muscles of the lower extremities), which causes a violation of blood circulation. The disease is manifested by arching pain, redness and swelling at the site of thrombosis. The disease can be asymptomatic or lead to a life-threatening complication - pulmonary embolism 1 .
The disease is manifested by arching pain, redness and swelling at the site of thrombosis. The disease can be asymptomatic or lead to a life-threatening complication - pulmonary embolism 1 .
Women are less at risk of developing venous thrombosis, however, during pregnancy, the likelihood of its occurrence increases significantly. This is due to changes in hormonal levels, compression of the pelvic veins by an enlarged uterus, imbalance in the blood coagulation system, which can lead to pathological thrombosis in the veins 2 .
From the first days of pregnancy, the body of the expectant mother undergoes serious changes: hormonal changes occur, hemoglobin, ferritin, vitamin B12 levels may decrease, cholesterol, insulin, alkaline phosphatase levels increase, the volume of circulating blood changes (in this way the body adapts to the development of the fetus and subsequent childbirth), the circulatory system is rebuilt, and the organs begin to work “for two”.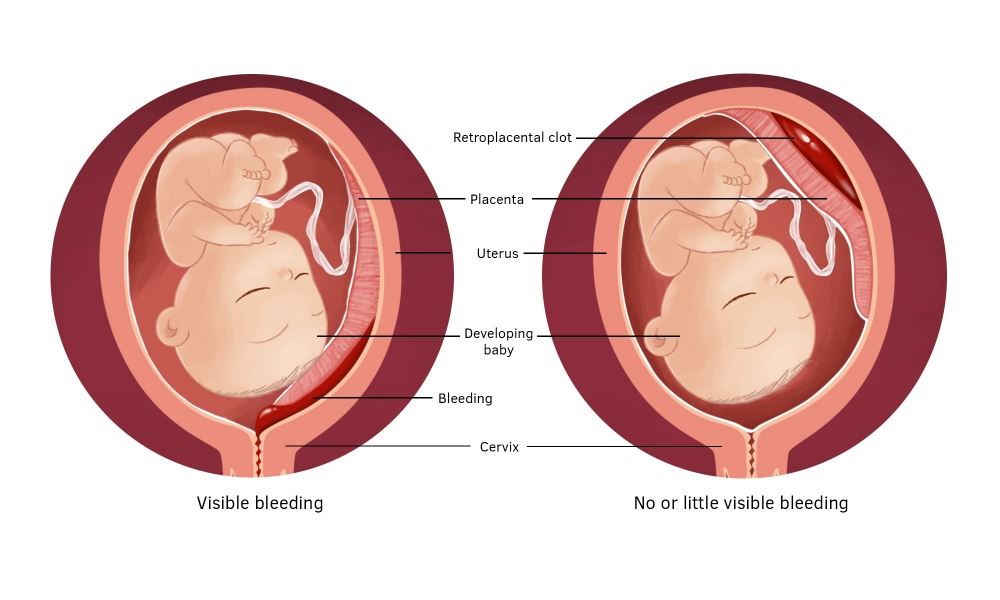
Thrombotic complications are the main direct cause of maternal death during pregnancy and the postpartum period: 12.8% of all maternal deaths 3.6 . Therefore, it is necessary to closely monitor the health of a woman during pregnancy.
Major risk factors for thrombosis in pregnant women
Congenital vessels of blood vessels and blood coagulation systems
The use of oral contraceptives and hormonal therapy
Oncological diseases
Varicose veins
Pressure of the veins of the pelvis
Chronic diseases of the cardiovascular system
Pregnancy and the postpartum period
years of more years
Sedentary lifestyle
Major risk factors for thrombosis in pregnant women
Main risk factors for thrombosis in pregnant women
Key symptoms of thrombosis 4
Almost always, the disease in the early stages is asymptomatic. However, some common signs of thrombosis can be identified:
How to protect yourself?
Avoid oral contraceptives and other drugs that affect blood clotting 6 months before the planned pregnancy to reduce the risk of blood clots.
During the planning and course of pregnancy, regularly consult a doctor, carefully following all his recommendations aimed at improving the health of mother and baby 4 .
Pregnancy doctor visit schedule 3.5
Preparing for the visit 3
When planning a pregnancy, in addition to your doctor, you can also consult a hematologist or any other specialist who deals with the problem of thrombosis and hemostasis during pregnancy. It is worth remembering which of the tests you have taken in the last couple of months: this will help the doctor track the dynamics of your condition.
Laboratory study of the hemostasis system
To prevent thrombotic complications during pregnancy, in some cases, doctors may recommend that some pregnant patients undergo a laboratory study with an assessment of the blood coagulation system - Coagulogram with indicators of coagulation factors such as 2-4 :
- Fibrinogen - a blood coagulation factor, turns into fibrin, the latter subsequently forms a blood clot.

- The number of platelets - cells directly involved in the process of blood coagulation.
- Activated partial thromboplastin time (APTT) - the time it takes for a blood clot to form after adding special activators of this process to it.
- INR (international normalized ratio) - used for a comprehensive assessment of the patient's circulatory system, shows how “liquid” the blood is.
Show your doctor a list of all the drugs you have taken regularly over the past two months. This information is very important!
It is necessary to find out in advance whether your relatives had any diseases associated with increased blood clotting and the formation of blood clots in the venous system, as well as diseases of the kidneys and the cardiovascular system.
If you track fitness activity, you can provide this data to your healthcare provider.
Tips for pregnant women
During pregnancy, in the absence of contraindications, if possible, it is worth maintaining a fairly active lifestyle. Small physical activities, such as swimming and long walks, will only help you and your unborn baby to be healthy.
Small physical activities, such as swimming and long walks, will only help you and your unborn baby to be healthy.
As a diet, it is recommended to eat foods low in cholesterol, for example: bran, fish, vegetables, fruits, and animal fats should also be present in the food.
A thorough gynecological history is required: history of previous births, IVF procedures or abortions.
However, these data are almost always recorded in your outpatient records and are worthy of a separate clarification only if your medical data has somehow been lost
The most important thing is to regularly visit doctors and medical centers, take all the necessary tests, follow all the prescribed recommendations. Remember that serious complications can be prevented in the early stages.
By all means, you should give up all bad habits.
You can get a consultation from a specialized specialist
And you can get a specialized examination of the hemostasis system at the medical centers shown on the map
Find a clinic
Thrombogenic risk factors in pregnant women.

220045, Minsk, st. Semashko, 10
This email address is being protected from spambots. You must have JavaScript enabled to view.
Site version for the visually visible
Healthcare Institution
Minsk Clinical Consultative Diagnostic Center
Call-Center (Registration)
| +375 17 311 10 19 (10 lines) | |
| +375 17 355 94 50 (7 lines) | |
| +375 29 238 00 90 (mobile MTS 4 lines) | |
| +375 44 550 00 90 (mobile A1 4 lines) |
Apply online
Minsk Clinical Consultative and Diagnostic Center Book online If a woman has a history of recurrent miscarriage or fetal loss in late pregnancy, second toxicosis half pregnancy, intrauterine growth retardation, placental abruption or placental infarction, she should be tested for thrombophilia. Hyperhomocysteinemia, which sometimes develops under the influence of hereditary genetic polymorphism, is associated with late toxicosis and is involved in the development of infarcts and placental abruption. Inflammation of the endothelial lining of blood vessels associated with elevated levels of homocysteine causes an increased risk of both venous and arterial thrombosis. Hyperhomocysteinemia can be caused by the presence in the body of altered forms of the enzyme methylenetetrahydrofolate reductase (MTHFR), which is normally involved in the conversion of homocysteine to methionine. Hereditary polymorphism of factor Leiden (V), which has a strong predisposition to thrombosis, occurs with an increased frequency in women with recurrent miscarriage. Among patients with recurrent miscarriage, abnormal forms of factor V Leiden are most common in women who have miscarriages in the second trimester of pregnancy. Hyperhomocysteinemia itself does not have a significant association with early fetal loss, suggesting that folic acid deficiency and MTHFR polymorphism may act through additional as yet unknown factors. Elevated levels of homocysteine are also detected during pregnancies complicated by preeclampsia, and this increase persists after childbirth. Other causes of placental thrombosis. Pregnancy may contribute to the manifestation of a genetic defect, as it develops the following features: The risk of thrombosis in inherited forms of thrombophilia can be reduced by using small doses of aspirin, heparin, folic acid, intravenous immunoglobulin G, or hematogenous factor concentrates. For carriers of inherited thrombophilia with recurrent adverse pregnancy outcomes, two prophylactic treatment options deserve attention: administration of low molecular weight heparin (enoxaparin) to women with recurrent late fetal loss and folic acid treatment for severe toxicosis of the 2nd half of pregnancy. In all pregnant and non-pregnant individuals, folic acid intake significantly reduces homocysteine levels. Efficiency is high in cases where pre-treatment homocysteine levels were highest and lowest if homocysteine levels were relatively low. A decrease in homocysteine levels has been observed with the use of folic acid at a dose of 0.5 mg to 5 mg per day in combination with vitamin B6. There is a high probability of thromboembolic complications and in the presence of cardiovascular diseases, overweight, anemia, late toxicosis. The risk of thrombosis also increases in women in the age group after 40 years, in the presence of malignant tumors, a sedentary lifestyle. Prolonged, prolonged labor, caesarean section also predispose to complications. The group of very high risk for the development of thrombosis, including in the postpartum period, includes women with varicose veins of the lower extremities. Causes of thrombosis First of all, the development of postpartum thrombosis is associated with changes in the blood coagulation system. To reduce the risk of venous thromboembolic complications during pregnancy, the use of low molecular weight heparins (LMWH) in prophylactic and intermediate doses in the form of subcutaneous injections is recommended. However, at present, the decision to prescribe LMWH to pregnant women is made only on the basis of a thrombotic history or if a particular thrombophilia is detected (factor V Leiden mutations, prothrombin mutations, antithrombin deficiency, carriage of antiphospholipid antibodies, etc. Congenital thrombophilia (a condition of increased blood clotting), caesarean section, advanced age of the woman in labor and overweight increase the likelihood of blood clots during pregnancy. If a woman has previously given birth three or more times or has multiple pregnancies (twins or more), the risk of thrombosis also increases. Additional risk factors for blood clots are: hypertension, cardiovascular disease and diabetes; use of oral contraceptives before pregnancy; dehydration. It is important to note that the risk of blood clots persists for up to two months after delivery. The treatment of thrombosis is a complex process that must necessarily take place under the supervision of a physician. Antiphospholipid syndrome (APS) is the cause of many obstetric complications such as fetal loss syndrome, HELLP syndrome, preterm birth. The high risk of adverse obstetric outcomes in APS necessitates pregnancy planning and the selection of adequate therapy for a pregnant woman with this pathology. Today, APS is one of the urgent problems in obstetric practice. Clinical manifestations of APS in obstetrics are fetal loss syndrome, intrauterine growth retardation, HELLP syndrome, oligohydramnios, fetoplacental insufficiency, preterm birth, preeclampsia (preeclampsia and eclampsia). The high risk of adverse obstetric outcomes in APS dictates the need for pregnancy planning in these patients, careful selection of drug therapy and constant monitoring of the mother and fetus. At the stage of planning pregnancy in a patient with APS, it is necessary to exclude concomitant risk factors for thrombosis. The range of preventive measures includes correction of excess weight, treatment of concomitant arterial hypertension, correction of lipid disorders, smoking cessation, as well as the use of compression stockings for post-thrombophlebitic syndrome. Pregnant women with APS from the moment of conception are prescribed low doses of ASA (50-100 mg per day, but not more than 150 mg per day) and low molecular weight heparins until the moment of delivery. +375 17 355 94 50 (Hor.) +375 29 238 00 90 (mobile MTS) +375 44 550 00 90 (mobile A1) You are here:



 During natural childbirth or caesarean section, blood is lost. The volume of blood loss can be different - from minimal (physiological) to significant (pathological), which depends on the specific situation. In any case, the body seeks to stop further blood flow, producing a large number of factors that increase blood coagulation by forming clots-plugs in the lumen of blood vessels. And the more blood loss, the more active these processes. In addition, when the placenta passes or due to mechanical tissue damage during the operation, the vessel wall is also damaged, special proteins and enzymes of the endothelium (the inner lining of the vessel) are released into the blood, which is also important for shifting processes towards increased blood coagulation.
During natural childbirth or caesarean section, blood is lost. The volume of blood loss can be different - from minimal (physiological) to significant (pathological), which depends on the specific situation. In any case, the body seeks to stop further blood flow, producing a large number of factors that increase blood coagulation by forming clots-plugs in the lumen of blood vessels. And the more blood loss, the more active these processes. In addition, when the placenta passes or due to mechanical tissue damage during the operation, the vessel wall is also damaged, special proteins and enzymes of the endothelium (the inner lining of the vessel) are released into the blood, which is also important for shifting processes towards increased blood coagulation. 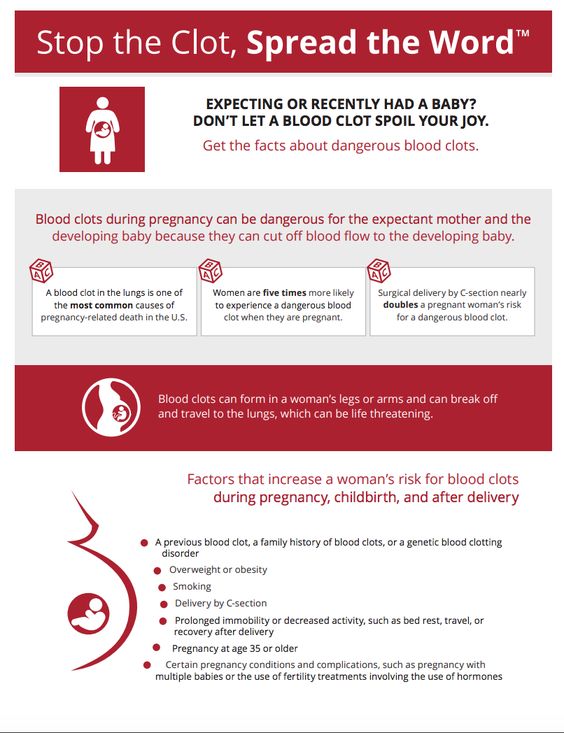 ). These indications for the appointment of LMWH are subjective, since they are not based on accurate laboratory data measuring excessive (thrombotic) activation of blood coagulation at different stages of pregnancy. Accordingly, the use of these indications leads to unreasonably widespread use of heparins during pregnancy.
). These indications for the appointment of LMWH are subjective, since they are not based on accurate laboratory data measuring excessive (thrombotic) activation of blood coagulation at different stages of pregnancy. Accordingly, the use of these indications leads to unreasonably widespread use of heparins during pregnancy.  Therefore, in the presence of risk factors, thrombosis prophylaxis is recommended. Prevention can be non-drug and drug. The doctor determines the degree of risk for each patient - low, moderate, high. After that, a method of prevention is selected. As a rule, one non-drug prophylaxis is not enough for people with an increased risk of developing thrombosis, therefore, drug prophylaxis is carried out along with it. In this case, special drugs are used that prevent the formation of blood clots.
Therefore, in the presence of risk factors, thrombosis prophylaxis is recommended. Prevention can be non-drug and drug. The doctor determines the degree of risk for each patient - low, moderate, high. After that, a method of prevention is selected. As a rule, one non-drug prophylaxis is not enough for people with an increased risk of developing thrombosis, therefore, drug prophylaxis is carried out along with it. In this case, special drugs are used that prevent the formation of blood clots.  Fetal loss syndrome is currently considered as a specific marker of APS. Termination of pregnancy in APS can occur at any stage of pregnancy, and very often spontaneous miscarriage is the only symptom to suspect APS in a patient.
Fetal loss syndrome is currently considered as a specific marker of APS. Termination of pregnancy in APS can occur at any stage of pregnancy, and very often spontaneous miscarriage is the only symptom to suspect APS in a patient.