Newborns after birth
Baby's first 24 hours | Pregnancy Birth and Baby
Baby's first 24 hours | Pregnancy Birth and Baby beginning of content5-minute read
Listen
The first day of your new baby’s life is thrilling and exhausting for both of you. This page explains what your newborn baby can sense, and how the umbilical cord and placenta can be managed. It has general information for you if you have had a healthy, full-term pregnancy – 37 to 42 weeks’ gestation.
What will my newborn baby look like?
When your baby is born, their skin might be blue and mottled. They are likely to be covered in amniotic fluid, blood and vernix, which is a cheesy white substance. This is normal.
Their skin will start to become pink as they start to breathe — which is about a minute after birth. Your baby’s hands and feet may still appear blueish for several hours.
The amniotic fluid and the vernix are there because they were there in the womb. They are important for your baby to be able to smell and taste after birth. These familiar things help your baby to feel secure outside the womb.
Birth of the placenta and cutting the umbilical cord
After you have given birth to your baby, you will have more contractions that will help you deliver the placenta. Once this happens, the umbilical cord, which is connected to the placenta, will be clamped in two places and cut. Your support person might be invited to cut the cord.
Skin-to-skin contact
After a normal vaginal birth, your newborn baby will be put on your chest for skin-to-skin contact. Your baby needs sleep and food, and they need to feel secure and warm, so they need to feel your skin.
Doing this simple thing:
- reduces newborn crying
- helps start and sustain breastfeeding
- helps maintain your baby’s body temperature
After this first contact, they will be weighed, measured and observed to make sure they are healthy.
If you have a caesarean section, ask your midwife to make sure your baby has skin-to-skin contact with you as early as possible. It may be possible for you or your partner to hold your baby-skin-to skin in theatre and in recovery.
Feeding
Babies start to show signs of wanting to feed soon after birth and usually attach and suck at the breast about 50 minutes after birth. They may then breastfeed for an hour or more. Put your baby against your chest, and they will probably find your breast and start feeding. If that doesn’t happen, you can ask your midwife or a lactation consultant for help.
The first milk you make is called 'colostrum'. It’s thick and often yellowish, rather than pure white. It’s the ideal milk for your baby. Normally a small amount is produced — your baby’s tummy is just the size of a marble.
If they haven’t fed an hour or so after birth, try again a couple of hours later. You can also express some colostrum to feed to your baby on a spoon.
Weighing and measuring
After skin-to-skin contact and the first breastfeed, your midwife might offer to weigh your baby, and measure your baby’s length and head circumference. Your baby doesn’t need to be washed for at least 24 hours.
Vitamin K
At the time of weighing, your midwife will also offer to give your baby a vitamin K injection to prevent bleeding from vitamin K deficiency.
Cord blood collection if you are Rh negative
If your blood group is Rh negative, some blood will be taken from the umbilical cord to determine whether your baby’s blood group is compatible.
Sleeping
Your baby will stay with you so you can bond and respond easily to their needs. They’ll probably sleep soon after their first feed, and that might last 6 hours or so. They will probably sleep for more than half of their first day in the world.
Apgar scores
One of the main observations made after birth is called an Apgar score. It assesses your baby’s adjustment to life outside the womb. The Apgar score is measured at 1 minute and 5 minutes after birth while the baby is on your chest. Sometimes it is measured again at 10 minutes after birth.
The Apgar score is measured at 1 minute and 5 minutes after birth while the baby is on your chest. Sometimes it is measured again at 10 minutes after birth.
It records your baby’s heart rate, breathing, colour, muscle tone and reflexes. The maximum score is 10. A score of 7 or above usually means your baby is doing well. It is not an ability or intelligence test, and it doesn’t predict your baby’s health later in life.
What will my newborn baby see, hear, smell, taste and feel?
Your baby has been listening to your voice for the last half of your pregnancy and will recognise it when you speak to them after birth. Your partner or support person’s voice may also be familiar if they have also been talking near your baby. Your baby will feel secure when they hear your voices and may respond by turning their head towards you. Your baby will also be able to hear your heart beating as they did in the womb.
Your baby’s vision is blurred at birth but they will be able to focus on your face from about 30 centimetres away. This is called the ‘cuddle distance’. It is roughly the distance from your breast to your face. Your baby will make the connection between what they hear and what they see.
This is called the ‘cuddle distance’. It is roughly the distance from your breast to your face. Your baby will make the connection between what they hear and what they see.
Your baby will smell and taste the amniotic fluid and your colostrum, which has a similar flavour.
Urine and meconium
Within the first 24 hours your baby will probably pass urine and meconium (newborn faeces) at least once. Meconium is black and sticky. Your baby’s poo will change colour and consistency over the next few days.
More information
You can call Pregnancy, Birth and Baby, 7 days a week on 1800 882 436 to speak with a maternal child health nurse to find out more.
Sources:
Cochrane (Early skin-to-skin contact for mothers and their healthy newborn infants), National Institute for Health and Care Excellence (NICE) (NICE Guideline CG37: Postnatal care up to 8 weeks after birth), World Health Organization (WHO) (Recommendations on newborn health), Raising Children Network (After baby is born: what to expect in the first few hours), Australian Breastfeeding Association (Breastfeeding timeline)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Mum's first few days after giving birth
- Mum's first 24 hours after birth
- Your baby in the first few days
- Birth injury (to the baby)
- What is kangaroo care?
Need more information?
Newborn clothes & dressing a newborn | Raising Children Network
How many clothes does a newborn need? And what newborn clothes are best? Get answers to these questions and more in our guide to dressing a newborn.
Read more on raisingchildren.net.au website
Newborns behaviour | Raising Children Network
Newborn behaviour baffling you? Here's all you need on newborns behaviour with articles, videos and resources on crying, colic and more.
Read more on raisingchildren.net.au website
Newborn bloodspot screening - MyDr.com.au
Newborn screening tests can detect rare but serious genetic or metabolic disorders in newborn babies.
Read more on myDr website
Dressing a newborn
When dressing your newborn, here are a few things to consider, like which clothes to use, how to dress them and making sure the change table is safe.
Read more on Pregnancy, Birth & Baby website
Newborn essentials
Here is a newborn's essentials checklist including vaccinations and immunisations, health checks, nappy changing and breastfeeding and bottle feeding.
Read more on Pregnancy, Birth & Baby website
Wind, burping & newborn babies in pictures | Raising Children Network
Newborns might have wind from swallowing air when crying or feeding. Burping can help newborns get rid of wind. See how to burp your newborn – in pictures
Burping can help newborns get rid of wind. See how to burp your newborn – in pictures
Read more on raisingchildren.net.au website
Newborns development | Raising Children Network
Want to track newborns development? Here's all you need on newborn development with articles, videos and resources on growth, relationships and more.
Read more on raisingchildren.net.au website
Is my newborn safe? - MyDr.com.au
Dr Norman Swan explains the risks of COVID-19 to your newborn.
Read more on myDr website
Newborns sleep | Raising Children Network
Need help understanding newborn sleep? Here’s all you need on newborn sleep with articles, videos and resources on safe sleep, sleep habits, tiredness and more.
Read more on raisingchildren.net.au website
Newborns safety | Raising Children Network
Newborn safety stressing you? Here’s all you need on newborns safety with articles, videos and resources on first aid, CPR, equipment, car seats and more.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
After the Baby Arrives | CDC
- Health
- Safety
- Development
- Medical Conditions
After your baby arrives, there’s a lot to think about. Click on the following links to learn more about how to help keep you and your baby healthy and safe, as well as learn about certain birth defects and medical conditions.
Health
Breastfeeding: You and your baby gain many benefits from breastfeeding. Breast milk is easy to digest and has antibodies that can protect your baby from bacterial and viral infections.
Proper Handling and Storage of Breast Milk: Safely prepare and store your expressed breast milk to maintain its high quality and keep your baby healthy. Make sure your baby’s caregivers know how to safely prepare and store the breast milk, too.
Breastfeeding and Travel: Travel need not be a reason to stop breastfeeding. A mother traveling with a nursing infant may find breastfeeding makes travel easier than it would be if traveling with a bottle-fed infant. Find helpful tips for traveling while breastfeeding, and learn about vaccinations for international travel.
Postpartum Depression: Postpartum depression is depression that occurs after having a baby. If you think you have postpartum depression, seek treatment from your health care provider as soon as possible.
Jaundice and Kernicterus: Jaundice can sometimes lead to brain damage in newborns. Before leaving the hospital, ask your doctor or nurse about a jaundice bilirubin test. If you think your baby has jaundice, call and visit your baby’s doctor right away.
Before leaving the hospital, ask your doctor or nurse about a jaundice bilirubin test. If you think your baby has jaundice, call and visit your baby’s doctor right away.
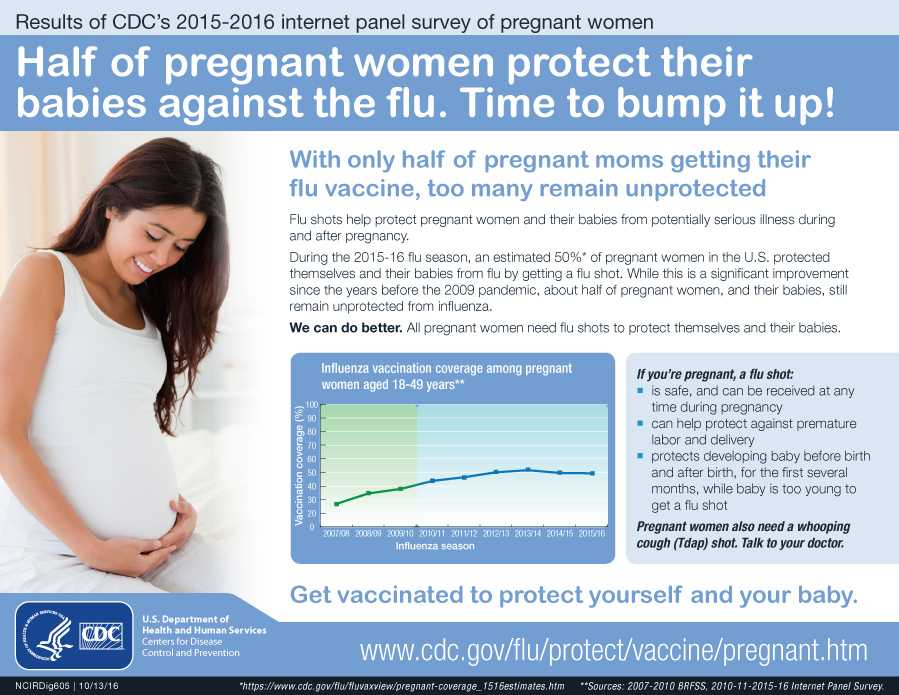
Vaccinations: Vaccines are very important to your baby’s health. When you get vaccinated against whooping cough and the flu during your pregnancy, you will pass some immunity (protection) to your baby. However, that protection will begin to decrease over time, leaving your infant vulnerable to disease. Make sure he or she gets vaccinated according to CDC’s childhood immunization schedule for safe, proven disease protection.
Immunization Schedules: Follow the schedule found at this link to be sure your baby gets his or her shots on time. If you miss any, check with your doctor about getting back on track.
Vaccination After Pregnancy: It is safe for a woman to receive vaccines right after giving birth, even while she is breastfeeding. Vaccination after pregnancy is especially important if you did not receive certain vaccines before or during your pregnancy.
Newborn Screening: Within 48 hours of your baby’s birth, a sample of blood is taken from a “heel stick,” and the blood is tested for treatable diseases. More than 98% of all children born in the United States are tested for these disorders.
Some babies with a critical congenital heart defect (CHD) appear healthy at first and may be sent home before their critical CHD is detected. Newborn screening for critical CHDs is a tool that works with prenatal diagnosis and physical exams after birth to improve detection of critical CHDs.
Your baby should be screened for hearing loss before 1 month of age, preferably before leaving the birth hospital. Learn more about newborn hearing screening and what happens if your baby doesn’t pass the screening test.
Once your baby is born, you can learn more about ATSDR’s Choose Safe Places for Early Care and Education program, which protects the health of children where they learn and play to reduce your child’s risk of being exposed to dangerous chemicals during their care.
Top of Page
Visit CDC’s Hear Her campaign website to learn the warning signs to watch for during pregnancy.
Safety
Child Medication Safety: Every year, one out of every 150 two-year-olds is treated in an emergency department for an accidental medication overdose. Find tips for keeping all medications up and away and out of sight of young children.
Sudden Infant Death Syndrome (SIDS): Learn what parents and caregivers can do to help babies sleep safely and reduce the risk of sleep-related infant deaths, including SIDS.
Child Safety Seats: Motor vehicle injuries are a leading cause of death among children in the United States. But many of these deaths can be prevented. Always buckling children in age- and size-appropriate car seats, booster seats, and seat belts reduces serious and fatal injuries by up to 80%.
Travel: An estimated 2.4 million children from the United States travel internationally each year. Learn how to travel safely with your baby within the country and internationally.
Fire Safety: Find tips to help prevent injury or death from a fire in your home.
Child Maltreatment: Maltreatment is a serious problem that can have lasting harmful effects on a child’s life. Find some strategies to help prevent child maltreatment.
Disaster Safety for Expecting and New Parents Learn general tips to get prepared before a disaster and what to do in case of a disaster to help keep you and your family safe and healthy.
Top of Page
Development
Child Development: The early years of a child’s life are crucial for learning, social, and emotional development. Learn what you can do to ensure that your child grows up in an environment that meets his or her needs.
Positive Parenting Tips for Babies: Learn how to give your baby a healthy and safe start in the first year of life.
Learn the Signs. Act Early. Measuring your baby’s growth involves more than tracking height and weight. Learn about milestones to watch for in how your baby plays, learns, speaks, and acts.
Top of Page
Medical Conditions
Birth Defects: Birth defects are structural changes present at birth that can affect almost any part or parts of the body (e.g., heart, brain, foot). They may affect how the body looks, works, or both. About one in every 33 babies is born with a birth defect.
Developmental Disabilities: Developmental disabilities are a group of conditions due to an impairment in physical, learning, language, or behavior areas. About one in six children in the U.S. have one or more developmental disabilities or other developmental delays.
Genetics: If your baby was born with a genetic condition, you may want to work with a genetic counselor in your area to help with information, resources, and support.
Blood Disorders: CDC works to prevent and reduce complications among people with certain blood disorders (bleeding disorders, hemophilia, von Willebrand disease, thrombophilia, and thalassemia).
How a newborn baby changes - articles from the specialists of the clinic "Mother and Child"
Babin Evgeny Alexandrovich
Pediatric surgeon, Orthopedic traumatologist, Pediatric orthopedic surgeon
Mother and Child Clinic South-West, Mother and Child Clinic Kuntsevo,
The baby was born, and we expect him to look like beautiful and pink babies from advertising pictures. And he is some kind of red, then suddenly turned yellow, on the skin or a rash, or peeling. In addition, the weight is still unstable, the chair is incomprehensible - is the child healthy? Healthy, and all these changes are the so-called transient (transitional) states. Where do they come from, what do they look like and what to do with it all?
And he is some kind of red, then suddenly turned yellow, on the skin or a rash, or peeling. In addition, the weight is still unstable, the chair is incomprehensible - is the child healthy? Healthy, and all these changes are the so-called transient (transitional) states. Where do they come from, what do they look like and what to do with it all?
The child sat in the mother's stomach for nine months, swam in the water and received oxygen through the placenta. As soon as the baby was born, his world immediately became different: instead of water around him, air, the ambient temperature dropped from 36.6-37 ° C to 22-25 ° C, plus gravity, sounds, smells, bright light. And now you have to breathe (lungs) yourself, eat differently, and then also remove metabolic products. And just like that, it is not easy for a newborn to immediately switch from one lifestyle to another, it takes time. That is why, from the point of view of physiology, in the first month of life, “something happens all the time” with children, and much more often and brighter than in later life. These are the transitory (transitional, boundary) states. All of them surprise and even frighten young parents, especially since transition states appear and disappear very quickly. But for newborns, they are completely natural. What moms and dads see most often are transitional states of skin, stool, weight, plus or minus a couple more conditions.
These are the transitory (transitional, boundary) states. All of them surprise and even frighten young parents, especially since transition states appear and disappear very quickly. But for newborns, they are completely natural. What moms and dads see most often are transitional states of skin, stool, weight, plus or minus a couple more conditions.
How the skin changes
The child was born, and we see that he is all sort of bluish-purple, and then his skin color immediately turns red. On the second day after birth, the baby "blushes" the brightest. Doctors call this redness "erythema simple" and it appears due to the fact that the skin adapts to a new environment. Then the child's skin turns pale and by the end of the first week of life it becomes the pale pink color we are used to.
But that's not all. On the third or fifth day of life, the baby's skin may begin to peel off, especially on the abdomen and chest. What's this? Does the child lack vitamins, something with nutrition, is the air too dry in the house? No, this is also a transitional state - physiological peeling, and it is also associated with the fact that the skin is adapting to a new life. The skin flakes for about a week, and then everything goes away. You don't need to do anything with it. Of course, you can treat the skin with various softening lotions and creams, but there will be no significant effect from them. Very soon, the baby's skin will become smooth and soft on its own.
The skin flakes for about a week, and then everything goes away. You don't need to do anything with it. Of course, you can treat the skin with various softening lotions and creams, but there will be no significant effect from them. Very soon, the baby's skin will become smooth and soft on its own.
Most of all, parents are afraid of a rash on the baby's skin, which does not often, but sometimes still appears in the first week of life. This is the so-called toxic erythema - spots with grayish-yellow seals in the center. The rash is most often located on the extensor surfaces of the arms and legs around the joints, on the chest. Less often, such spots can be on the whole body (except for the palms, feet and mucous membranes). “Maybe it’s chickenpox, rubella, or some other disease?” parents are afraid. No, this is a kind of reaction of the skin of a newly born baby to its environment, especially to hypothermia, overheating, contact with clothes, food. Within one to three days, new spots may appear, but more often two or three days after the onset, they all disappear without a trace. At the same time, the child’s well-being is not disturbed, the body temperature is normal and he does not need any medication. The only thing is that you need to take care of the bubbles on the skin: for example, gently blot them after bathing. And you also need to make sure that the bubbles do not rub and they do not burst (otherwise an infection may join them).
At the same time, the child’s well-being is not disturbed, the body temperature is normal and he does not need any medication. The only thing is that you need to take care of the bubbles on the skin: for example, gently blot them after bathing. And you also need to make sure that the bubbles do not rub and they do not burst (otherwise an infection may join them).
Physiological jaundice
The changes that are visible on the skin do not end there. Very often (in 60-70% of children) on the second or third day of life, the skin turns yellow, the maximum of yellowness occurs on the third or fourth day, and by the end of the first week it disappears. This is how physiological jaundice of a newborn is manifested - a condition in which the amount of bile pigment, bilirubin, increases in a child. In some children, jaundice is similar to a light tan (parents may not notice it), while in others, the skin will turn bright yellow. Very quickly, the level of bilirubin returns to normal and the skin color becomes normal again. If jaundice is mild and passes quickly, then no additional treatment is needed. But if jaundice does not disappear or the skin color is intense yellow, you should consult a doctor.
If jaundice is mild and passes quickly, then no additional treatment is needed. But if jaundice does not disappear or the skin color is intense yellow, you should consult a doctor.
Weight loss
Do you think the baby will immediately be born well-fed, with folds and cute roundness? No, right after birth, this is still far away. In the first days of life, an already not too well-fed newborn will lose even more weight. Such weight loss is a natural process, the so-called physiological weight loss. Weight decreases because immediately after birth, the baby loses part of the water through the skin, its umbilical cord dries out, meconium (the first feces) and urine are excreted, and also because the baby still eats a small amount of milk. Maximum weight loss usually occurs by the third or fifth day and is normally no more than 6-8% of birth weight. At this time, mother and baby are usually discharged from the hospital, but there is no need to worry. By the seventh or tenth day of life, a healthy baby will restore its previous parameters.
chair changes
On the first or second day, all newborns pass the original stool (meconium): it is thick, viscous and dark green in color. Time passes, the baby begins to receive colostrum, and on the third or fourth day of life, a transitional stool appears. Now areas of dark green color alternate with greenish and yellow ones, and some lumps, mucus are also visible in the stool. It all looks like some kind of intestinal disorder, but it's not. It's just that the gastrointestinal tract is moving to a new job, now it's ready to digest food. By the end of the first week of life, the stool in most children is yellow, similar to gruel, and it will continue to be so.
Warm-cold
A typical fear of all grandmothers is that the child is freezing! Yes, indeed, in newborns, the body temperature regulation processes are still imperfect, so babies easily cool down, but they also overheat just as easily. For example, if a newborn is dressed too warmly or placed next to a heating battery, he will quickly overheat, even if this is the usual temperature in the room. At the same time, the child easily loses heat when he is undressed for a long time or he lies in wet clothes. Therefore, in the room where there is a newborn, the air temperature should be adequate - 20-22 ° C. And if she rises higher, and the child is warmly dressed, then this will also not be good.
At the same time, the child easily loses heat when he is undressed for a long time or he lies in wet clothes. Therefore, in the room where there is a newborn, the air temperature should be adequate - 20-22 ° C. And if she rises higher, and the child is warmly dressed, then this will also not be good.
Sometimes, very rarely (in 1% of newborns), body temperature on the third or fifth day may temporarily rise to 38–39 °C. There are no other symptoms of the disease, the body temperature quickly returns to normal, but the parents have time to get scared. It’s difficult to figure out what it is - temporary hyperthermia or still a disease - it’s difficult, so it’s better to call a doctor.
Hormonal crisis
An uncommon occurrence, but it also occurs occasionally. In some children, on the third or fourth day of life, the mammary glands become engorged (in both girls and boys). They increase as much as possible by the seventh or eighth day, and liquid discharge may even appear from them. Some girls have very little bloody discharge from the vagina for a very short time. This is the so-called hormonal crisis - it occurs due to the action of maternal hormones - estrogens (they penetrate through the placenta during childbirth). At the peak of estrogen action, the signs of a hormonal crisis are maximum, then the hormones are removed from the body and the symptoms gradually disappear. Therefore, you don’t need to apply a cabbage leaf to your chest, make compresses with camphor or something else: everything will pass by itself.
Some girls have very little bloody discharge from the vagina for a very short time. This is the so-called hormonal crisis - it occurs due to the action of maternal hormones - estrogens (they penetrate through the placenta during childbirth). At the peak of estrogen action, the signs of a hormonal crisis are maximum, then the hormones are removed from the body and the symptoms gradually disappear. Therefore, you don’t need to apply a cabbage leaf to your chest, make compresses with camphor or something else: everything will pass by itself.
Usually, all these transitional states are pronounced in the first week of life, less often, but it happens that they drag on for up to three to four weeks. One more thing - it is not necessary that the child will show all transitional states, but almost everyone has physiological weight loss and transitional stools. And many of the transitional states are completely invisible to parents, but they also exist, they can simply be identified only by laboratory methods.
So we are not in a hurry to be frightened, noticing that the child’s skin suddenly began to peel off or he turned slightly yellow. We remember that he must adapt to a new life, that in the first time after birth, the baby has the right to some changes. Especially if, with all this, the baby is cheerful, calm and eats well. Well, if you are still somehow anxious, ask your pediatrician questions. He will definitely be able to put everything in its place.
Inset
The maximum weight loss in a newborn usually occurs by the third or fifth day and normally amounts to no more than 6-8% of body weight at birth.
From the point of view of physiology, in the first month of life, “something happens all the time” with children, and much more often and brighter than in later life. These are the transitory (transitional, boundary) states.
In infants, the body temperature regulation processes are still imperfect, so they easily become overcooled and overheated. In this regard, in the room where there is a newborn, the air temperature should be about - 20–22 ° C.
In this regard, in the room where there is a newborn, the air temperature should be about - 20–22 ° C.
Physiological jaundice of the newborn:
- occurs on the 2-3rd day of the baby's life, reaches a maximum on the 4-5th day, and disappears by the 10th day;
- the general condition of the child does not suffer;
- the level of bilirubin in the blood does not exceed 180 µmol/l.
Make an appointment
to the doctor - Babin Evgeny Aleksandrovich
Clinic "Mother and Child" KuntsevoClinic "Mother and Child" South-West
Pediatric surgeryChildren Medical examinationSupervision of children at homeObservation of children with special needs
By clicking on the send button, I consent to the processing of personal data
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital MD GROUPClinical Hospital Lapino-1 "Mother and Child"Children's Clinic KG "Lapino" on New Riga (branch)Clinic "Mother and Child" KuntsevoClinic "Mother and Child" SavelovskayaClinic "Mother and Child" South-WestClinic "Mother and Child" » Novogireevo
All directions
01.
Kinesiotherapy for children
02.
Specialist consultations (adults)
03.
Specialist consultations (children)
04.
Massage/manipulation for children
05.
Therapeutic research
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of tests by calling
Baby in the maternity hospital: the first days of life
Immediately after childbirth
As soon as the baby is born, the midwife takes him in her arms and immediately begins to care for him. And there are no trifles here. Imagine: a baby is born wet, he has just been in his mother's body, where the temperature was 36.6 ° C, now he enters the maternity block, where the air temperature is about 24 ° C. This is a warm and comfortable environment for you and me, and for a baby, the difference of these 12 ° C is quite large. Thermoregulation in young children is still imperfect, they do not retain heat well and quickly cool down, and then there is also moist skin and a sharp temperature drop. Therefore, the first thing the midwife does is wipe the baby with a warm diaper and lay it on the mother's stomach. Several factors come into play here: firstly, physical contact with the mother will maintain the child’s body temperature and warm him. Secondly, it will strengthen the psychological bond between mother and baby. And, thirdly, the child's sterile organism will be populated with new maternal microorganisms that will protect it from conditionally pathogenic or pathogenic microflora of the environment.
Thermoregulation in young children is still imperfect, they do not retain heat well and quickly cool down, and then there is also moist skin and a sharp temperature drop. Therefore, the first thing the midwife does is wipe the baby with a warm diaper and lay it on the mother's stomach. Several factors come into play here: firstly, physical contact with the mother will maintain the child’s body temperature and warm him. Secondly, it will strengthen the psychological bond between mother and baby. And, thirdly, the child's sterile organism will be populated with new maternal microorganisms that will protect it from conditionally pathogenic or pathogenic microflora of the environment.
The next important moment is that the umbilical cord is cut for the newborn, the neonatologist examines the baby and puts an Apgar score. This scale is needed in order to determine which children need more attention. According to this scale, the health status of each newborn is assessed on five indicators: heart rate, respiration, muscle tone, reflexes, and skin color of the baby. During the examination, for each sign (heart rate, breathing, muscle tone, reflexes and skin color) give 0, 1 or 2 points. A score of 2 points in the delivery room is considered the highest and means that the sign is pronounced, 1 point - weakly expressed, 0 points - the sign is absent. The child is evaluated on the Apgar scale at the 1st and 5th minutes of life, so there are always two scores, for example 8/9points or 9/10 points. Children rarely score the maximum 10 points in the first minute of life, and usually the first score is always lower than the second. But the second assessment can just be equal to 10 points. Children who score between 7 and 10 are considered to be in good condition and generally require only routine care. Those who score between 4 and 6 are in fair condition and may only need some resuscitation procedures. Immediate life-saving assistance is necessary for those whose score is below 4. Apgar score - no matter what it will be (low or high) - this is not a diagnosis.
During the examination, for each sign (heart rate, breathing, muscle tone, reflexes and skin color) give 0, 1 or 2 points. A score of 2 points in the delivery room is considered the highest and means that the sign is pronounced, 1 point - weakly expressed, 0 points - the sign is absent. The child is evaluated on the Apgar scale at the 1st and 5th minutes of life, so there are always two scores, for example 8/9points or 9/10 points. Children rarely score the maximum 10 points in the first minute of life, and usually the first score is always lower than the second. But the second assessment can just be equal to 10 points. Children who score between 7 and 10 are considered to be in good condition and generally require only routine care. Those who score between 4 and 6 are in fair condition and may only need some resuscitation procedures. Immediate life-saving assistance is necessary for those whose score is below 4. Apgar score - no matter what it will be (low or high) - this is not a diagnosis. This is a signal for the doctor about what measures are now needed or, conversely, the child does not need.
This is a signal for the doctor about what measures are now needed or, conversely, the child does not need.
Next, the neonatologist continues to examine the newborn. The doctor looks at how the baby is formed, whether he has any developmental anomalies or any other problems. After that, the newborn is washed, measured, weighed, and a tag with the name of the mother and the time of birth is attached to the handles. Then the child is wrapped in a diaper and applied to the mother's breast. Almost always at this time (within 10–20 minutes after birth), the baby calms down and falls asleep. What happens next depends on the design of the maternity hospital. In some maternity hospitals, for the next two hours, the mother and the newborn are in the maternity ward, in others the child is taken to the children's ward. In any case, if there is an opportunity to be together, you must ask to leave the baby next to you, if the child feels well, this is quite possible.
With mother or in the children's department
Now almost everywhere you can be with a child both together and separately. But again, it all depends on the device of the maternity hospital. If a woman lies separately from the baby, then she will take him for feeding. The sisters of the children's department will take care of the child, wash, change diapers, change clothes. But you need to understand that they do this according to a schedule that is the same for all children in the department, and not according to the individual needs of the child.
But again, it all depends on the device of the maternity hospital. If a woman lies separately from the baby, then she will take him for feeding. The sisters of the children's department will take care of the child, wash, change diapers, change clothes. But you need to understand that they do this according to a schedule that is the same for all children in the department, and not according to the individual needs of the child.
If the child lies with his mother, then his regimen is already determined by her. Mom can feed the baby on demand, and not by the hour, as with a separate stay. And she also changes the diaper or changes it when it is really necessary (the child peed and the diaper is full), and not according to some schedule that is the same for everyone. It turns out that a connection is established between mother and child faster, it is easier for a woman to understand what the baby needs, why he is crying and what to do with him. If a mother already at the maternity hospital learns to wash and change a child, change his diaper, upon returning home, she will adapt much easier to a new life and a new daily routine. The second important plus of living together is that breastfeeding is established faster, and when feeding on demand, milk will come faster.
The second important plus of living together is that breastfeeding is established faster, and when feeding on demand, milk will come faster.
Some women believe that after giving birth they need to rest, be apart from the child, they say, they are taking care of him in the children's department, and for now I will come to my senses and get used to my new state. Yes, if the birth was difficult and the mother endured it hard, then you need to rest. But since childbirth is still a physiological process, a woman recovers very quickly and even after a difficult birth, on the second day, she may well take the child to her ward. After all, judge for yourself - she won’t have to do anything special: she doesn’t cook dinner (the maternity hospital provides food), then she doesn’t wash the dishes, she doesn’t clean or wash anything (the maternity hospital even gives out clean clothes daily). Almost all newborns do not cry in the first days after childbirth, but sleep all the time, and it turns out that the only concern of the mother is to breastfeed the baby several times a day and change the diaper. So a woman will have enough time to rest, and why not use it for business? And one more thing: those who gave the child to the children's department like to blame later that he was supplemented with formula there, although the woman asked not to do this. But imagine the situation: the child cried, his sister examined him - he was washed, changed clothes, that is, everything is in order with him, but he, nevertheless, cries. What will mom do - take the baby in her arms, shake, calm. But the sister of the children's department has many more children nearby, they also need to be looked after. What is the way out - either give a bottle with a mixture or wait for other children to “turn on” from the endless crying of the child.
So a woman will have enough time to rest, and why not use it for business? And one more thing: those who gave the child to the children's department like to blame later that he was supplemented with formula there, although the woman asked not to do this. But imagine the situation: the child cried, his sister examined him - he was washed, changed clothes, that is, everything is in order with him, but he, nevertheless, cries. What will mom do - take the baby in her arms, shake, calm. But the sister of the children's department has many more children nearby, they also need to be looked after. What is the way out - either give a bottle with a mixture or wait for other children to “turn on” from the endless crying of the child.
First examinations, tests, vaccinations
While the newborn is in the hospital, he will be examined by a neonatologist every day. The doctor will either come to the ward to see the mother and the baby, or the child will be taken to the children's department. The doctor must coordinate all manipulations, appointments with the mother, and be sure to tell about all the results of the examination. But he himself will not be able to guess what exactly the woman is interested in, so doctors usually say the main thing, for example: "Everything is in order with the child, he has been examined, no pathology has been detected, he is gaining weight." If you need a more detailed answer, formulate your questions in advance, let's say again: the doctor does not know what interests you - how to care for the navel or why the child has a red spot on his face.
The doctor must coordinate all manipulations, appointments with the mother, and be sure to tell about all the results of the examination. But he himself will not be able to guess what exactly the woman is interested in, so doctors usually say the main thing, for example: "Everything is in order with the child, he has been examined, no pathology has been detected, he is gaining weight." If you need a more detailed answer, formulate your questions in advance, let's say again: the doctor does not know what interests you - how to care for the navel or why the child has a red spot on his face.
If necessary, the child will be examined by other specialists: an ophthalmologist or a neurologist. The newborn will be required to determine the blood type and Rh factor, and also take a blood test for severe congenital diseases (the so-called screening). The fact that these tests have been carried out will be indicated in the children's part of the exchange card (it will be issued upon discharge). The child may also be assigned some additional studies: a general and biochemical blood test, a general urine test. Also, if necessary, the newborn will undergo an ultrasound examination of the abdominal organs, brain (neurosonography), heart (echocardiography).
The child may also be assigned some additional studies: a general and biochemical blood test, a general urine test. Also, if necessary, the newborn will undergo an ultrasound examination of the abdominal organs, brain (neurosonography), heart (echocardiography).
As for vaccinations, according to the national vaccination calendar, the first vaccinations are done at the maternity hospital. On the first day of life - from hepatitis B, on the full second day - from tuberculosis. If parents do not want to be vaccinated, then you must inform the doctor about this in advance and write a refusal to vaccinate.
Upon discharge from the maternity hospital, the mother will be given two parts of the exchange card. One of them will contain information about childbirth, and it will have to be taken to the antenatal clinic. The second part of the exchange card will contain data on the child, screening, vaccinations and examinations - it is given to the children's clinic. The next day after the mother and baby return home from the maternity hospital, they will be visited by the health visitor of the polyclinic, and the next day by the pediatrician. And now the specialists of the children's polyclinic will monitor the newborn.
And now the specialists of the children's polyclinic will monitor the newborn.
As you can see, the child in the maternity hospital will be under control all the time. Mom, doctors, children's sisters - they will all give him the attention he needs. The main thing for a woman in a maternity hospital is to be active, ask doctors, nurses, learn how to care for a baby, and establish breastfeeding. And then she will return home as a confident and savvy mom!
- Apgar score - no matter what it will be (low or high) - this is not a diagnosis. This is a signal for the doctor about what measures are now needed or, conversely, the child does not need
- If a woman lies separately from the baby, then she will take him to feed. The sisters of the children's department will take care of the child, wash, change diapers, change clothes. But you need to understand that they are doing this according to a schedule that is the same for all children in the department, and not according to the individual needs of the child
- Laying the baby on his stomach after childbirth will maintain his body temperature, strengthen the psychological bond between mother and baby.
 And the child’s sterile organism will be populated with new maternal microorganisms that will protect it from conditionally pathogenic or pathogenic microflora of the environment
And the child’s sterile organism will be populated with new maternal microorganisms that will protect it from conditionally pathogenic or pathogenic microflora of the environment
Memo for mothers
While you are in the hospital
- If possible, take the child to your room. So you will quickly get used to it, establish breastfeeding and learn how to care for the baby.
- If you don't know how to wash, change or swaddle your baby, ask the Nursing Nurse to show you how to do it. Do it yourself at least a few times.
- Ask your midwife in the postnatal unit to show you how to properly latch your baby to your breast.
- Ask the neonatologist what examinations the child has undergone and what he would like to do in the future.
- Be active - ask the doctor and nurses any questions about the baby.
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital IDKChildren's Clinic "Mother and Child" Samara
All directionsSpecialist consultations (children)Massage / manual therapy for childrenTherapeutic research
01.