Can breastfeeding while pregnant cause miscarriage
Breast‐feeding During Pregnancy and the Risk of Miscarriage
1. Yan J et al., The association between breastfeeding and childhood obesity: a meta‐analysis, BMC Public Health , 2014, 14(1):1267, 10.1186/1471-2458-14-1267. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
2. Horta BL, Loret de Mola C and Victora CG, Long‐term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta‐analysis, Acta Paediatrica , 2015, 104(467):30–37, 10.1111/apa.13139. [PubMed] [CrossRef] [Google Scholar]
3. Horta BL, Loret de Mola C and Victora CG, Breastfeeding and intelligence: a systematic review and meta‐analysis, Acta Paediatrica , 2015, 104(467):14–19, 10.1111/apa.13139. [PubMed] [CrossRef] [Google Scholar]
4. Kramer MS et al., Breastfeeding and child cognitive development: new evidence from a large randomized trial, Archives of General Psychiatry , 2008, 65(5):578–584, 10. 1001/archpsyc.65.5.578. [PubMed] [CrossRef] [Google Scholar]
5. Chowdhury R et al., Breastfeeding and maternal health outcomes: a systematic review and meta‐analysis, Acta Paediatrica , 2015, 104(467):96–113, 10.1111/apa.13102. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
6. Peres KG et al., Effect of breastfeeding on malocclusions: a systematic review and meta‐analysis, Acta Paediatrica , 2015, 104(467):54–61, 10.1111/apa.13103. [PubMed] [CrossRef] [Google Scholar]
7. Kennedy KI, Rivera R and McNeilly AS, Consensus statement on the use of breastfeeding as a family planning method, Contraception , 1989, 39(5):477–496, 10.1016/0010-7824(89)90103-0. [PubMed] [CrossRef] [Google Scholar]
8. World Health Organization (WHO) , Global Nutrition Monitoring Framework: operational guidance for tracking progress in meeting targets for 2025, Geneva: WHO, 2017, https://www.who.int/nutrition/publications/operational-guidance-GNMF-indicators/en. [Google Scholar]
[Google Scholar]
9. Bhutta ZA et al., What works? Interventions for maternal and child undernutrition and survival, Lancet , 2008, 371(9610):417–440, 10.1016/S0140-6736(07)61693-6. [PubMed] [CrossRef] [Google Scholar]
10. U.S. Office of Disease Prevention and Health Promotion, Healthy People 2020, Maternal, infant and child health: objectives, https://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-health/objectives.
11. Victora CG et al., Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect, Lancet , 2016, 387(10017):475–490, 10.1016/S0140-6736(15)01024-7. [PubMed] [CrossRef] [Google Scholar]
12. Centers for Disease Control and Prevention (CDC) , Nutrition, physical activity, and obesity—national immunization survey (breastfeeding), https://chronicdata.cdc.gov/Nutrition-Physical-Activity-and-Obesity/Nutrition-Physical-Activity-and-Obesity-National-I/8hxn-cvik/data.
13. CDC, National Center for Health Statistics, National Immunization Surveys 2000. –2014, https://www.cdc.gov/breastfeeding/data/NIS_data/index.htm.
–2014, https://www.cdc.gov/breastfeeding/data/NIS_data/index.htm.
14. López‐Fernández G et al., Breastfeeding during pregnancy: a systematic review, Women and Birth: Journal of the Australian College of Midwives , 2017, 30(6):e292–e300, 10.1016/j.wombi.2017.05.008. [PubMed] [CrossRef] [Google Scholar]
15. Cetin I et al., Breastfeeding during pregnancy: position paper of the Italian Society of Perinatal Medicine and the Task Force on Breastfeeding, Ministry of Health, Italy, Journal of Human Lactation , 2014, 30(1):20–27, 10.1177/0890334413514294. [PubMed] [CrossRef] [Google Scholar]
16. Molitoris J, Breastfeeding during pregnancy and its association with childhood malnutrition and pregnancy loss in low‐ and middle‐income countries, Lund Papers in Economic Demography , 2018, No. 3, https://www.ed.lu.se/media/ed/papers/working_papers/LPED%202018%203.pdf. [Google Scholar]
17. Boerma JT and Bicego GT, Preceding birth intervals and child survival: searching for pathways of influence, Studies in Family Planning , 1992, 23(4):243–256, 10. 2307/1966886. [PubMed] [CrossRef] [Google Scholar]
2307/1966886. [PubMed] [CrossRef] [Google Scholar]
18. Merchant K, Martorell R and Haas JD, Consequences for maternal nutrition of reproductive stress across consecutive pregnancies, American Journal of Clinical Nutrition , 1990, 52(4):616–620, 10.1093/ajcn/52.4.616. [PubMed] [CrossRef] [Google Scholar]
19. Ramachandran P, Maternal nutrition—effect on fetal growth and outcome of pregnancy, Nutrition Reviews , 2002, 60(5 Pt. 2):S26–S34, 10.1301/00296640260130704. [PubMed] [CrossRef] [Google Scholar]
20. Shaaban OM and Glasier AF, Pregnancy during breastfeeding in rural Egypt, Contraception , 2008, 77(5):350–354, 10.1016/j.contraception.2008.01.005. [PubMed] [CrossRef] [Google Scholar]
21. Briefel RR et al., Zinc intake of the U.S. population: findings from the third National Health and Nutrition Examination Survey, 1988–1994, Journal of Nutrition , 2000, 130(5S Suppl):1367S–1373S, 10.1093/jn/130.5.1367S. [PubMed] [CrossRef] [Google Scholar]
22. Butte NF and King JC, Energy requirements during pregnancy and lactation, Public Health Nutrition , 2005, 8(7A):1010–1027, 10.1079/PHN2005793. [PubMed] [CrossRef] [Google Scholar]
Butte NF and King JC, Energy requirements during pregnancy and lactation, Public Health Nutrition , 2005, 8(7A):1010–1027, 10.1079/PHN2005793. [PubMed] [CrossRef] [Google Scholar]
23. King JC, Physiology of pregnancy and nutrient metabolism, American Journal of Clinical Nutrition , 2000, 71(5, Suppl.):1218S–1225S, 10.1093/ajcn/71.5.1218s. [PubMed] [CrossRef] [Google Scholar]
24. Picciano MF, Pregnancy and lactation: physiological adjustments, nutritional requirements and the role of dietary supplements, Journal of Nutrition , 2003, 133(6):1997S–2002S, 10.1093/jn/133.6.1997S. [PubMed] [CrossRef] [Google Scholar]
25. Institute of Medicine , Report on Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids, Washington, DC: Institute of Medicine of the National Academies, 2002. [PubMed] [Google Scholar]
26. Merchant K, Martorell R and Haas J, Maternal and fetal responses to the stresses of lactation concurrent with pregnancy and of short recuperative intervals, American Journal of Clinical Nutrition , 1990, 52(2):280–288, 10. 1093/ajcn/52.2.280. [PubMed] [CrossRef] [Google Scholar]
1093/ajcn/52.2.280. [PubMed] [CrossRef] [Google Scholar]
27. Shaaban OM et al., Effect of pregnancy‐lactation overlap on the current pregnancy outcome in women with substandard nutrition: a prospective cohort study, Facts, Views & Vision in ObGyn , 2015, 7(4):213–221. [PMC free article] [PubMed] [Google Scholar]
28. Ayrim A et al., Breastfeeding throughout pregnancy in Turkish women, Breastfeeding Medicine , 2014, 9(3):157–160, 10.1089/bfm.2013.0086. [PubMed] [CrossRef] [Google Scholar]
29. S¸ engül Ö et al., The outcomes of the pregnancies of lactating women, Turkish Journal of Medical Sciences , 2013, 43(2):251–254. [Google Scholar]
30. Madarshahian F and Hassanabadi M, A comparative study of breastfeeding during pregnancy: impact on maternal and newborn outcomes, Journal of Nursing Research , 2012, 20(1):74–80, 10.1097/JNR.0b013e31824777c1. [PubMed] [CrossRef] [Google Scholar]
31. Moscone SR and Moore MJ, Breastfeeding during pregnancy, Journal of Human Lactation , 1993, 9(2):83–88, 10. 1177/089033449300900219. [PubMed] [CrossRef] [Google Scholar]
1177/089033449300900219. [PubMed] [CrossRef] [Google Scholar]
32. Ishii H, Does breastfeeding induce spontaneous abortion? Journal of Obstetrics and Gynaecology Research , 2009, 35(5):864–868, 10.1111/j.1447-0756.2009.01072.x. [PubMed] [CrossRef] [Google Scholar]
33. Sriraman NK, The nuts and bolts of breastfeeding: anatomy and physiology of lactation, Current Problems in Pediatric and Adolescent Health Care , 2017, 47(12):305–310, 10.1016/j.cppeds.2017.10.001. [PubMed] [CrossRef] [Google Scholar]
34. Bøhler E and Bergström S, Child growth during weaning depends on whether mother is pregnant again, Journal of Tropical Pediatrics , 1996, 42(2):104–109, 10.1093/tropej/42.2.104. [PubMed] [CrossRef] [Google Scholar]
35. CDC , What is stillbirth? 2019, https://www.cdc.gov/ncbddd/stillbirth/facts.html. [Google Scholar]
36. Lang K and Nuevo‐Chiquero A, Trends in self‐reported spontaneous abortions: 1970–2000, Demography , 2012, 49(3):989–1009, 10. 1007/s13524-012-0113-0. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
1007/s13524-012-0113-0. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
37. Jones RK and Kost K, Underreporting of induced and spontaneous abortion in the United States: an analysis of the 2002 National Survey of Family Growth, Studies in Family Planning , 2007, 38(3):187–197, 10.1111/j.1728-4465.2007.00130.x. [PubMed] [CrossRef] [Google Scholar]
38. Thulier D and Mercer J, Variables associated with breastfeeding duration, Journal of Obstetric, Gynecologic, and Neonatal Nursing , 2009, 38(3):259–268, 10.1111/j.1552-6909.2009.01021.x. [PubMed] [CrossRef] [Google Scholar]
39. García‐Enguídanos A et al., Risk factors in miscarriage: a review, European Journal of Obstetrics, Gynecology, and Reproductive Biology , 2002, 102(2):111–119, 10.1016/S0301-2115(01)00613-3. [PubMed] [CrossRef] [Google Scholar]
40. Singh GK, Kogan MD and Dee DL, Nativity/immigrant status, race/ethnicity, and socioeconomic determinants of breastfeeding initiation and duration in the United States, 2003, Pediatrics , 2007, 119(Suppl. 1):S38–S46, 10.1542/peds.2006-2089G. [PubMed] [CrossRef] [Google Scholar]
1):S38–S46, 10.1542/peds.2006-2089G. [PubMed] [CrossRef] [Google Scholar]
41. Love ER et al., Effect of interpregnancy interval on outcomes of pregnancy after miscarriage: retrospective analysis of hospital episode statistics in Scotland, BMJ , 2010, 341:c3967, 10.1136/bmj.c3967. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
42. Nybo Andersen A‐M et al., Maternal age and fetal loss: population based register linkage study, BMJ , 2000, 320(7251):1708–1712, 10.1136/bmj.320.7251.1708. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
43. Flink‐Bochacki R et al., Examining intendedness among pregnancies ending in spontaneous abortion, Contraception , 2017, 96(2):111–117, 10.1016/j.contraception.2017.05.010. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
44. Myers RJ, Errors and bias in the reporting of ages in census data, Transactions of the Actuarial Society of America, 1940, 41(Pt. 2 (104)):395–415.
45. Grambsch PM and Therneau TM, Proportional hazards tests and diagnostics based on weighted residuals, Biometrika , 1994, 81(3):515–526, 10.1093/biomet/81.3.515. [CrossRef] [Google Scholar]
46. Regan L, Braude PR and Trembath PL, Influence of past reproductive performance on risk of spontaneous abortion, BMJ , 1989, 299(6698):541–545, 10.1136/bmj.299.6698.541. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
47. Maconochie N et al., Risk factors for first trimester miscarriage—results from a UK‐population‐based case‐control study, BJOG , 2007, 114(2):170–186, 10.1111/j.1471-0528.2006.01193.x. [PubMed] [CrossRef] [Google Scholar]
48. George L et al., Risks of repeated miscarriage, Paediatric and Perinatal Epidemiology , 2006, 20(2):119–126, 10.1111/j.1365-3016.2006.00703.x. [PubMed] [CrossRef] [Google Scholar]
49. Jacobsson B, Ladfors L and Milsom I, Advanced maternal age and adverse perinatal outcome, Obstetrics & Gynecology , 2004, 104(4):727–733, 10.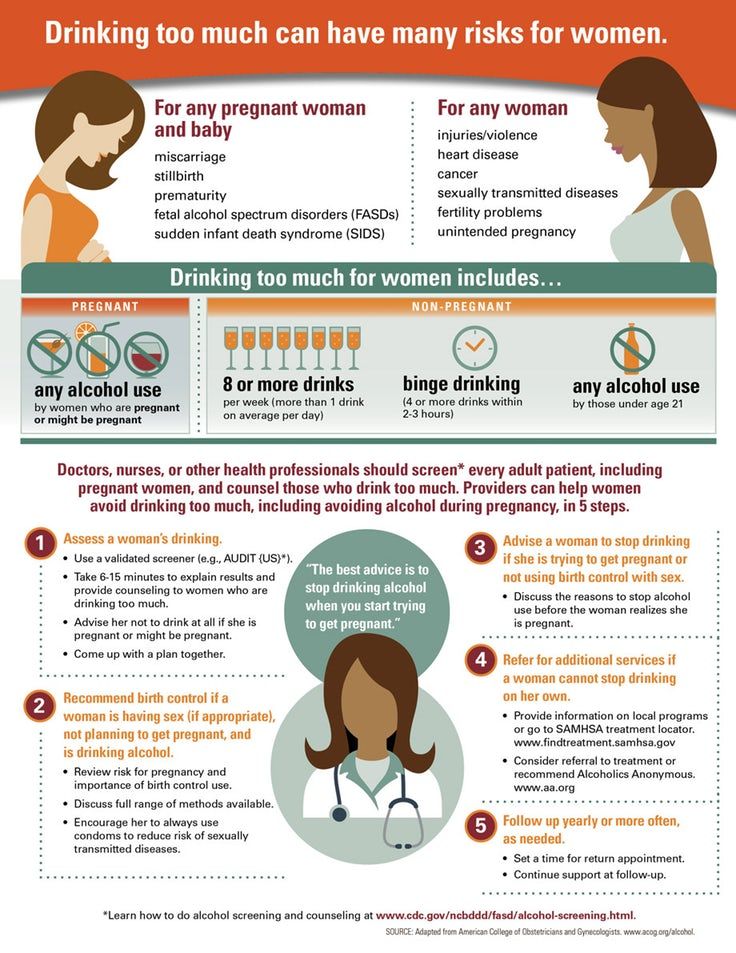 1097/01.AOG.0000140682.63746.be [PubMed] [CrossRef] [Google Scholar]
1097/01.AOG.0000140682.63746.be [PubMed] [CrossRef] [Google Scholar]
50. Cleary‐Goldman J et al., Impact of maternal age on obstetric outcome, Obstetrics & Gynecology , 2005, 105(5 Pt. 1):983–990, 10.1097/01.AOG.0000158118.75532.51. [PubMed] [CrossRef] [Google Scholar]
51. Gregory E, Drake P and Martin J, Lack of change in perinatal mortality in the United States, 2014–2016, Hyattsville, MD: National Center for Health Statistics, 2018. [Google Scholar]
52. Conde‐Agudelo A, Rosas‐Bermúdez A and Kafury‐Goeta AC, Birth spacing and risk of adverse perinatal outcomes: a meta‐analysis, Journal of the American Medical Association , 2006, 295(15):1809–1823, 10.1001/jama.295.15.1809. [PubMed] [CrossRef] [Google Scholar]
53. Amissah EA et al., Validation study of maternal recall on breastfeeding duration 6 years after childbirth, Journal of Human Lactation , 2017, 33(2):390–400, 10.1177/0890334417691506. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
54. Natland ST et al., Maternal recall of breastfeeding duration twenty years after delivery, BMC Medical Research Methodology , 2012, 12(1):179, 10.1186/1471-2288-12-179. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Natland ST et al., Maternal recall of breastfeeding duration twenty years after delivery, BMC Medical Research Methodology , 2012, 12(1):179, 10.1186/1471-2288-12-179. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
55. Bardos J et al., A national survey on public perceptions of miscarriage, Obstetrics & Gynecology , 2015, 125(6):1313–1320, 10.1097/AOG.0000000000000859. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
56. Sugiura‐Ogasawara M et al., Depression as a potential causal factor in subsequent miscarriage in recurrent spontaneous aborters, Human Reproduction , 2002, 17(10):2580–2584, 10.1093/humrep/17.10.2580. [PubMed] [CrossRef] [Google Scholar]
57. Bonari L et al., Perinatal risks of untreated depression during pregnancy, Canadian Journal of Psychiatry , 2004, 49(11):726–735, 10.1177/070674370404901103. [PubMed] [CrossRef] [Google Scholar]
58. Hemels ME et al., Antidepressant use during pregnancy and the rates of spontaneous abortions: a meta‐analysis, Annals of Pharmacotherapy , 2005, 39(5):803–809, 10. 1345/aph.1E547. [PubMed] [CrossRef] [Google Scholar]
1345/aph.1E547. [PubMed] [CrossRef] [Google Scholar]
59. Tennant PWG, Rankin J and Bell R, Maternal body mass index and the risk of fetal and infant death: a cohort study from the north of England, Human Reproduction , 2011, 26(6):1501–1511, 10.1093/humrep/der052. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
60. Landres IV, Milki AA and Lathi RB, Karyotype of miscarriages in relation to maternal weight, Human Reproduction , 2010, 25(5):1123–1126, 10.1093/humrep/deq025. [PubMed] [CrossRef] [Google Scholar]
61. Pineles BL, Park E and Samet JM, Systematic review and meta‐analysis of miscarriage and maternal exposure to tobacco smoke during pregnancy, American Journal of Epidemiology , 2014, 179(7):807–823, 10.1093/aje/kwt334. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
62. Ness RB et al., Cocaine and tobacco use and the risk of spontaneous abortion, New England Journal of Medicine , 1999, 340(5):333–339, 10. 1056/NEJM199902043400501. [PubMed] [CrossRef] [Google Scholar]
1056/NEJM199902043400501. [PubMed] [CrossRef] [Google Scholar]
63. Jutte DP et al., The ripples of adolescent motherhood: social, educational, and medical outcomes for children of teen and prior teen mothers, Academic Pediatrics , 2010, 10(5):293–301, 10.1016/j.acap.2010.06.008. [PubMed] [CrossRef] [Google Scholar]
64. Conde‐Agudelo A et al., Effects of birth spacing on maternal, perinatal, infant, and child health: a systematic review of causal mechanisms, Studies in Family Planning , 2012, 43(2):93–114, 10.1111/j.1728-4465.2012.00308.x. [PubMed] [CrossRef] [Google Scholar]
New Study on Breastfeeding and Miscarriage: Cause for Concern?
Categories: Breastfeeding Today
By Hilary Flower, Ph.D., and Gemma López
According to a new study reported on in Perspectives on Sexual Reproductive Health, exclusive breastfeeding during pregnancy may elevate the risk of miscarriage to a similar degree as conceiving after age 40. 1 Importantly, in the same study, mothers exhibited no added risk if they were giving their children complementary foods while breastfeeding and pregnant.
1 Importantly, in the same study, mothers exhibited no added risk if they were giving their children complementary foods while breastfeeding and pregnant.
Several people have asked for our response to this new research, since we have both published on the topic. Although it can be disconcerting to see the words breastfeeding, miscarriage, and risk all together like that, I believe there is no cause for alarm.
Before we unpack the study’s conclusions, I believe it is important to understand them within the context of existing research and the limitations of the study. First, when considering the safety of an overlap of breastfeeding with pregnancy, the answer differs depending on whether the mother is well-nourished, and whether the pregnancy is low risk. A growing body of medical research2-6 and official recommendations7-9 have indicated that breastfeeding during pregnancy appears to overlap safely with low risk pregnancies for well-nourished mothers. However, when nutritional status is poor, breastfeeding during pregnancy may raise the risk of adverse pregnancy outcomes.10 And when it comes to high-risk pregnancies, there is simply no medical research, and caution is generally advised.
However, when nutritional status is poor, breastfeeding during pregnancy may raise the risk of adverse pregnancy outcomes.10 And when it comes to high-risk pregnancies, there is simply no medical research, and caution is generally advised.
Where does this new study fit in? First, it is not a medical study; the author Joseph Molitoris is an economic historian. And the data are not medical data, but demographic data mined from the U.S. National Survey of Family Growth (NSFG). In contrast to medical data, these data are based on mothers’ recollections during a 60 to 80 minute interview, sometimes regarding pregnancies a decade or more prior. This is not the most solid ground for basing medical advice.
Second, the mothers’ nutritional status is unknown, because the NSFG survey did not include it. We do know that the mothers whose breastfeeding overlapped their pregnancy in this study were more likely to be younger, less educated, born abroad, and less likely to be white. This may raise the possibility that their social status was lower and perhaps also their nutritional status. These results may not have relevance to most breastfeeding mothers in the U.S.
This may raise the possibility that their social status was lower and perhaps also their nutritional status. These results may not have relevance to most breastfeeding mothers in the U.S.
Further, this study is not focused on low risk pregnancies. To the extent possible, the researcher accounted for miscarriage risk factors, but the NSFG survey does not allow for a clear distinction between low versus high risk pregnancies. The inability to exclude key complications and risk factors from this study means that this study cannot speak directly to low risk pregnancies.
Finally, the increased risk of miscarriage reported in this study was specific to mothers exclusively breastfeeding during pregnancy. Very, very few mothers exclusively breastfeed during pregnancy. Most mothers do not get pregnant until after their child has started solids, because exclusive breastfeeding tends to delay the return of fertility following birth. Those that do, and who are exclusively breastfeeding at the outset of pregnancy, are unlikely continue for long because either their child hits the six month mark and starts complementary feeding, or because their milk dries up. Most women (70% in one study) notice a decline in milk production usually evident by mid-pregnancy, and sometimes beginning in the first month. A minority of women report drying up entirely (18% in one study), and many women say that by mid-pregnancy “there isn’t a whole lot there.”11 Of the mothers who contributed to my book, most of those who had closely spaced babies found they had to supplement for much of their pregnancy.
Most women (70% in one study) notice a decline in milk production usually evident by mid-pregnancy, and sometimes beginning in the first month. A minority of women report drying up entirely (18% in one study), and many women say that by mid-pregnancy “there isn’t a whole lot there.”11 Of the mothers who contributed to my book, most of those who had closely spaced babies found they had to supplement for much of their pregnancy.
So, should mothers who are exclusively breastfeeding be concerned about an elevated risk of miscarriage? Perhaps. But this study leaves open the possibility that their risk may depend on their nutrition status and whether they have one of several “high risk” factors or pregnancy complications not controlled for in this study. Even with added risk, the help of a cautious but discerning caregiver in evaluating how the overlap is going could make all the difference in the pregnancy outcome.
In this study, Molitoris designed a complex model with a large dataset, and took care to control as many confounding variables as he could. It is exciting to see new research, even if it raises more questions than it answers. I think the best “take-home” message from this study is to remember that we do not know everything about breastfeeding overlapping with pregnancy. We would benefit from more medical research on the safety of breastfeeding during pregnancy for a variety of women in different settings, different pregnancy risk factors, and different intensity of breastfeeding. More research will allow us to make more informed, individual-based assessments about added risks when it comes to breastfeeding during pregnancy.
It is exciting to see new research, even if it raises more questions than it answers. I think the best “take-home” message from this study is to remember that we do not know everything about breastfeeding overlapping with pregnancy. We would benefit from more medical research on the safety of breastfeeding during pregnancy for a variety of women in different settings, different pregnancy risk factors, and different intensity of breastfeeding. More research will allow us to make more informed, individual-based assessments about added risks when it comes to breastfeeding during pregnancy.
Hilary Flower, Ph.D., is the author of Adventures in Tandem Nursing: Breastfeeding During Pregnancy and Beyond. She expects to release the second edition in December 2019. In addition to her writing, Hilary serves as an Assistant Professor of Environmental Studies at Eckerd College in Florida, and holds a Ph.D. in Ecohydrology. Author Hilary Flower, Photographer: Ramsay Flower
Gemma López is a midwife and the first author of the peer reviewed article Breastfeeding during pregnancy: A systematic review, published in Women and Birth.
References
- Molitoris, J., Breastfeeding During Pregnancy and the Risk of Miscarriage. Perspectives on sexual reproductive health 2019; 51(3): 153-163.
- Ishii, H., Does breastfeeding induce spontaneous abortion? Journal of Obstetrics and Gynaecology Research 2009; 35(5):864-868.
- Albadran, M. M., Effect of Breastfeeding during Pregnancy on the Occurrence of Miscarriage and Preterm Labour. Iraqi Journal of Medical Sciences 2013; 11(3).
- Ayrim, A.; Gunduz, S.; Akcal, B.; Kafali, H., Breastfeeding throughout pregnancy in Turkish women. Breastfeeding Medicine 2014; 9(3):157-160.
- Madarshahian, F.; Hassanabadi, M., A comparative study of breastfeeding during pregnancy: impact on maternal and newborn outcomes. Journal of Nursing Research 2012; 20(1):74-80.
- Flower, H., Breastfeeding during Pregnancy and Tandem Nursing: Is it Safe? Breastfeeding Today April 2016: https://www.
 llli.org/breastfeeding-during-pregnancy-and-tandem-nursing-is-it-safe/.
llli.org/breastfeeding-during-pregnancy-and-tandem-nursing-is-it-safe/. - AAFP, American Academy of Family Physicians Position Paper: Family Physicians Supporting Breastfeeding, Appendix 2: Additional Breastfeeding Considerations. Leawood, KS: AAFP 2008: http://www.aafp.org/about/policies/all/breastfeeding-support.html
- Cetin, I.; Assandro, P.; Massari, M.; Sagone, A.; Gennaretti, R.; Donzelli, G.; Knowles, A.; Monasta, L.; Davanzo, R., Breastfeeding during pregnancy: position paper of the Italian Society of Perinatal Medicine and the Task Force on Breastfeeding, Ministry of Health, Italy. Journal of Human Lactation 2014; 30(1):20-27.
- López-Fernández, G.; Barrios, M.; Goberna-Tricas, J.; Gómez-Benito, J., Breastfeeding during pregnancy: A systematic review. Women and Birth 2017.
- Merchant, K.; Martorell, R.; Haas, J., Maternal and fetal responses to the stresses of lactation concurrent with pregnancy and of short recuperative intervals.
 The American Journal of Clinical Nutrition 1990; 52(2):280-288.
The American Journal of Clinical Nutrition 1990; 52(2):280-288. - Moscone[sic], S. R.; Moore, M. J., Breastfeeding during pregnancy. Journal of Human Lactation 1993; 9(2):83-88 [The first author’s name was misspelled in the publication. Her actual name is Sherrill Moscona].
Breastfeeding pregnancy: first signs
0-6 months
Article
0 reviews
Is it possible to get pregnant during lactation? There is an opinion that this is impossible. However, in practice, such cases are not uncommon. How to recognize the first signs of pregnancy while breastfeeding and what are the risks? More on this later in the article.
4 min. for reading Feb. 17, 2022
What happens in the body of a breastfeeding woman
Immediately after the birth of a child, the amount of a special hormone, oxytocin, increases in a woman's body. It causes the uterus to contract after childbirth and is also responsible for the production of breast milk. The more often you breastfeed your baby, the higher the concentration of oxytocin in the blood. Interestingly, the same hormone is a provocateur of lactational amenorrhea. In other words, it is he who is to blame for the absence of menstruation.
It causes the uterus to contract after childbirth and is also responsible for the production of breast milk. The more often you breastfeed your baby, the higher the concentration of oxytocin in the blood. Interestingly, the same hormone is a provocateur of lactational amenorrhea. In other words, it is he who is to blame for the absence of menstruation.
It is generally accepted that as long as you are breastfeeding your baby and there are no periods, it is impossible to get pregnant. After all, there is no menstruation, no ovulation. No ovulation - no egg ready for fertilization. Everything is logical. In some women, amenorrhea can last a year or two, and in some - a month. And to understand when it ended is extremely difficult. The main sign of the restoration of fertility (ability to reproduce) is menstruation. But menstruation begins two weeks after ovulation. Therefore, a sexually active nursing mother can become pregnant again at any time, without even knowing it.
In addition to oxytocin, the amount of prolactin in the body of a nursing woman also increases. It blocks the growth of follicles and ovulation, but there is no guarantee that the follicle will not start growing. Therefore, it is also impossible to exclude the possibility of fertilization during this period.
It blocks the growth of follicles and ovulation, but there is no guarantee that the follicle will not start growing. Therefore, it is also impossible to exclude the possibility of fertilization during this period.
Pregnancy while breastfeeding: how it is possible
Unplanned fertilization during lactation can occur, doctors say. The fact is that during breastfeeding, fertility decreases, but does not freeze completely. And if a woman is breastfeeding her baby on schedule rather than on demand, or if she alternates between breastfeeding and formula, the chances of getting pregnant again are quite high.
Longer intervals between feedings or complete weaning of the baby from the breast reduces the level of oxytocin and prolactin in the blood. This, in turn, starts the process of follicle growth and ovulation, the resumption of the menstrual cycle. If you are not planning a second child in the first year after the birth of the first, consider contraception.
Symptoms of pregnancy while breastfeeding
How to determine pregnancy during lactation? It's not easy enough. Breastfeeding mothers often simply do not notice the classic signs of the birth of a new life in the womb, attributing them to the natural postpartum state of the body. Indeed, insomnia, anxiety, excessive fatigue, nausea and back pain are quite typical phenomena for a woman who has recently given birth. And the most obvious symptom of pregnancy - the absence of menstruation - is completely written off, since they are not there anyway. How do you know if you are pregnant or not?
Breastfeeding mothers often simply do not notice the classic signs of the birth of a new life in the womb, attributing them to the natural postpartum state of the body. Indeed, insomnia, anxiety, excessive fatigue, nausea and back pain are quite typical phenomena for a woman who has recently given birth. And the most obvious symptom of pregnancy - the absence of menstruation - is completely written off, since they are not there anyway. How do you know if you are pregnant or not?
See also: The second child in the family
The first signs of pregnancy during breastfeeding may be:
- You are more tired than usual and constantly want to sleep.
This symptom can be attributed to sleep deprivation at night and baby care, which takes all your strength. However, if you notice that you are getting tired more than usual and in the morning you feel completely overwhelmed, even if the baby did not wake up at night, buy a pregnancy test.
- Often run to the toilet
This may be due to cystitis or kidney disease, or it may be one of the symptoms of a new pregnancy. Our body is designed in this way: as soon as a new life is born in the womb, the body increases blood flow to provide the unborn baby with all the necessary substances. This in turn causes the kidneys to produce more urine. Do you often go to the toilet? Make an appointment with a gynecologist and buy a pregnancy test.
- You feel pain in your chest
This may be due not only to stagnation of milk, but also to a new pregnancy. Changes in the amount of estrogen and progesterone cause those very painful sensations in the mammary glands. Are you seeing this symptom in yourself? Buy a test.
- You feel sick in the morning.
Anything can make you feel sick, including an increase in the concentration of hCG in the blood. This hormone increases during pregnancy. Take blood tests and take a pregnancy test. It will respond to changes in the composition of urine, even during lactation.
It will respond to changes in the composition of urine, even during lactation.
- The baby refuses to breastfeed.
When a new pregnancy occurs, the hormonal background changes. Because of this, the taste of breast milk changes, its consistency thickens and it becomes smaller. Therefore, your baby may refuse to take the breast, will be naughty and constantly demand to eat.
Pregnancy during lactation: pros and cons
Another baby in the family is a joy. You should be aware of the possible risks and positive aspects that a new pregnancy promises.
It is much easier to bring up children who are the same age as children with a difference in age of several years. They have a common daily routine, common interests and toys for two. It will be easier for you to adjust.
Possible risks:
- A woman's body needs at least 2 years to fully recover after childbirth. A new child may simply not have enough resources for growth and development.
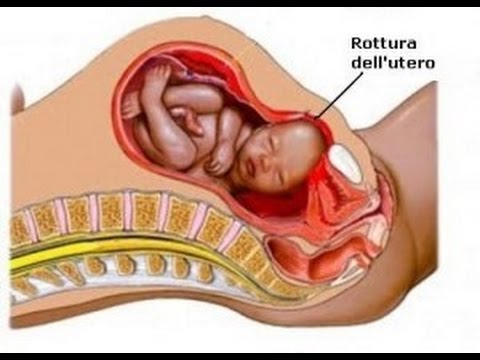
- If the delivery was by caesarean section, the uterus may not be ready. There is a risk of fetal death and irreversible consequences for the woman's health.
- Breastfeeding causes uterine contractions, which can cause miscarriage.
Keeping an unplanned pregnancy or not is entirely up to you. If the first pregnancy and first birth went without complications, it is quite possible to bear a healthy child.
Related Articles:
Sex During Pregnancy
Latest Reviews
Average Customer Rating
0 customer ratings
Snapshot of community ratings
- 5 0
- four 0
- 3 0
- 2 0
- one 0
New pregnancy while breastfeeding - what to do?
Number of views: 135 279
You are pregnant while breastfeeding. You are faced with a difficult choice: you do not plan to terminate the pregnancy, and the first-born is still too small to wean him from the breast. How to be? Is it possible to breastfeed during pregnancy? What is it fraught with?
You are faced with a difficult choice: you do not plan to terminate the pregnancy, and the first-born is still too small to wean him from the breast. How to be? Is it possible to breastfeed during pregnancy? What is it fraught with?
Pregnancy while breastfeeding - the heart of the matter
Until 300 years ago, there were no questions about stopping breastfeeding during pregnancy. The woman had no choice - a small child needs food, and there were practically no alternatives to mother's milk.
Today, a pregnant woman can receive a categorical recommendation from doctors as a matter of urgency to wean first-born from the breast. Yes, sometimes the termination of breastfeeding is dictated by the interests of pregnancy . But more often than not, it's overkill. Except in cases of clear medical indications, whether to feed or not during pregnancy, and if so, for how long - the decision of the parents , and not doctors and relatives.
Medical side of the issue
Very Caution Women who have experienced preterm labor, recurrent spontaneous miscarriages, or are currently being diagnosed with risk of preterm birth . Here it is important to carefully weigh all the pros and cons, listen to the opinion of your doctor.
Physicians recommending interruption of breastfeeding fear that the onset of pregnancy during breastfeeding may end in miscarriage or the fetus will not grow and develop harmoniously.
The reason doctors fear miscarriage or premature delivery is the effect of oxytocin on the uterus. Hormone oxytocin causes flushes of milk and uterine contractions . That is, theoretically, each time breastfeeding, a woman can provoke uterine contractions, which will lead to a miscarriage. But in practice, things don't quite work out that way.
Yes, frequent nipple stimulation can trigger labor pains in a full-term woman. And putting the newborn to the chest allows the uterus to contract after childbirth and return to its previous state.
And putting the newborn to the chest allows the uterus to contract after childbirth and return to its previous state.
But nature is wise and in most cases breastfeeding does not harm women with normal pregnancies. Once again, we note that we are talking about the norm !
The state of the uterus at the beginning of pregnancy is different from the state "before delivery or immediately after". She has a low ability to absorb oxytocin. Between the 1st and 3rd trimesters of pregnancy, the number of oxytocin receptors increases 12-fold. The low ability of the uterus to absorb oxytocin at the beginning of pregnancy suggests that HBs will not cause effective contractions.
One of the reasons recently given by doctors advocating for stopping breastfeeding during pregnancy was the impossibility of prescribing medications . Now the list of drugs allowed for hepatitis B has expanded significantly. Women have the opportunity to receive medical care in the required volume.
Women have the opportunity to receive medical care in the required volume.
Nutrition of the expectant mother
Will the body of a nursing mother be able to provide fetus with all the substances necessary for harmonious development? ok and is balanced a feeding woman will have no problems meeting the needs of the baby and the unborn child. Of course, she needs a nutritious diet , as well as vitamins that the doctor will prescribe. The problem will arise in case of a lack of nutrients. The deficit will be satisfied at the expense of the resources of the mother's body. The kids will get theirs, but the woman may be emaciated.
Challenges to be faced
Breastfeeding during a new pregnancy is:
- 's nipples become very sensitive. A woman may feel unexpected attacks of pain in the nipples or breasts, they are provoked by hormonal changes in the body.
 You can solve the problem with the help of lanolin . Due to its viscosity, it blocks the nerve endings on the nipple and reduces the sensitivity of . Lanolin can be applied a few minutes before feeding in a thin layer.
You can solve the problem with the help of lanolin . Due to its viscosity, it blocks the nerve endings on the nipple and reduces the sensitivity of . Lanolin can be applied a few minutes before feeding in a thin layer.
- Increased fatigue level . In the first trimester, women often feel elevated drowsiness , and an actively crawling toddler will not let you relax. Mom's fatigue is associated with hormonal changes during pregnancy, and not with breastfeeding. The condition will improve as the pregnancy progresses.
- Becomes less milk . 7 out of 10 mothers confirm that the volume of breast milk is reduced during subsequent pregnancies.
- Breast milk changes taste . Sometimes the firstborn refuses the breast on his own, because the milk has changed. The onset of pregnancy during breastfeeding leads to hormonal changes in the body. As a result, the amount of lactose in milk is reduced, but the amount of sodium increases.
 The taste of milk changes.
The taste of milk changes. - A woman may feel uterine contractions while breastfeeding. Most often, they do not pose any threat to the mother or fetus. But in case of painful sensations , you must immediately consult a doctor !
- In the late term, due to the large belly, it is difficult to find a comfortable position for feeding . Sometimes it is difficult for the baby to reach the mother's breast. Here you need to experiment, a suitable option is sure to be found.
Arguments in favor
Breastfeeding for a child is not only food , but also contact with mother , comfort. There are situations (illness, stress) when it is better to leave baby on breastfeeding . The ability to suck on his mother's breast has a beneficial effect on his emotional and physical condition. If mommy can organize the feeding of the eldest without harming herself and the unborn baby, this will be the best way out.
Pregnancy while breastfeeding means very little difference between babies. Jealousy and competition for mother's attention are inevitable here. Many women find that Tandem Feeding helps the cope with older jealousy and childcare issues with small age gaps. An article about tandem feeding will soon appear in the online magazine MamExpert.
Comment of a tandem-feeding mother
One of the mothers of the MamExpert community shared her own experience with us. We gratefully publish her opinion:
“I breastfed during my pregnancy and in tandem for over a year. And all this period I had to listen to scoldings, starting from the gynecologist in the LCD consultation and up to the head of the department of the 2nd maternity hospital (from her after the birth). Moreover, in the period from 36 weeks until delivery (41.1), the doctors were glad that I was breastfeeding, hoping that this would stimulate labor early, since the fetus was large.
The first contraction really came during feeding, but already at 41.1. The boy was born 57 cm 4375 gr. Then even the dermatologist tried to stick his nose into my breastfeeding. And about pediatricians who strictly say that after a year there is nothing to feed children with breast milk, I generally keep quiet. This is a personal matter for everyone, and sticking your nose into someone else's GV is at least not competent! Only one doctor in the ambulance could explain to me why our doctors demand so much to stop breastfeeding early: to make it easier to treat mothers if they get sick. If someone would give me some more intelligible argument against breastfeeding after a year, and this applies to both state institutions and adult and pediatric medicine, as well as paid centers.
Both young and experienced mothers have many questions about breastfeeding. Each baby is individual and with him parents can get into a situation that did not arise with older children! MamExpert courses will help you not to succumb to difficulties and find a solution to any issue.
Come to our breastfeeding course! Here you will gain knowledge that will give you a real understanding of what breastfeeding is. You will understand what to do if something goes wrong. Gain self-confidence and be able to enjoy breastfeeding.⠀
Course Speaker
-
Inna Shabelnikova - certified lactation consultant, leading lecturer MamExpert and mother of three children - Every day I come across mothers who have been told that they are "not dairy", that their milk is not nutritious enough for the baby and much more .. . utter. These are all myths! The limits are only in your head! You will be able to feed, enjoy it and give the child all the best!
Would you like to take a course? Sign up here: https://www.mamexpert.by/ochnye-kursy/ or call +375 44 553 20 50!
Pregnancy while breastfeeding is not uncommon.