Genetic counseling in pregnancy
Genetic counseling | March of Dimes
Genetic counseling helps you understand how genes, birth defects and medical conditions run in families and how they affect your family’s health.
You may want genetic counseling if health conditions run in your family or if prenatal tests show your baby may be at risk for health conditions.
A genetic counselor can help you understand test results to help you make decisions about your pregnancy and your baby’s care.
You can get genetic counseling before or during pregnancy. Your health care provider can help you find a genetic counselor in your area.
What is genetic counseling?
Genetic counseling helps you understand how genes, birth defects and other medical conditions run in families, and how they can affect your health and your baby’s health.
Genes are parts of your body’s cells that store instructions for how your body grows and works. Genes are passed from parents to children. A birth defect is a health condition that’s present at birth. Birth defects change the shape or function of one or more parts of the body. They can cause problems in overall health, in how the body develops or in how the body works.
You get genetic counseling from a genetic counselor. Your counselor can be:
- A certified genetic counselor (also called a CGC). This is someone who has special training to be a genetic counselor.
- A doctor or nurse with special training in genetic counseling
You can get genetic counseling any time, before or during pregnancy. Your health care provider can help you find a genetic counselor in your area. Or contact the National Society of Genetic Counselors.
Who should get genetic counseling?
You may want genetic counseling if:
- You have or think you have a genetic condition, or you have a child with a genetic condition, like cystic fibrosis or sickle cell disease, or a birth defect, like a heart defect or cleft lip or palate.
:strip_icc():format(jpeg)/kly-media-production/medias/2785562/original/028627600_1556001360-shutterstock_1019963743.jpg) These conditions may run in your family or ethnic group. An ethnic group is a group of people, often from the same country, who share language or culture. Some genetic conditions run in ethnic groups. For example, people who are Ashkenazi Jews are more likely than others to have Tay-Sachs disease and other genetic conditions.
These conditions may run in your family or ethnic group. An ethnic group is a group of people, often from the same country, who share language or culture. Some genetic conditions run in ethnic groups. For example, people who are Ashkenazi Jews are more likely than others to have Tay-Sachs disease and other genetic conditions. - You’re 35 or older. If you’re older than 35 when you get pregnant, you’re more likely than younger women to have a baby with a birth defect.
- You and your partner are first cousins or other blood relatives. Blood relatives are related by birth (like children, brothers, sisters, cousins), not by marriage (like sister- or brother-in-law).
- Your job, lifestyle or medical history may increase your baby’s chances of having a genetic condition or birth defect. For example, working with certain chemicals, like weed killer or radiation, can cause problems for a baby during pregnancy. Using street drugs or abusing prescription drugs also can affect your baby.
 And some medicines you take to treat a health condition or infection can be harmful to your baby during pregnancy.
And some medicines you take to treat a health condition or infection can be harmful to your baby during pregnancy. - An ultrasound or other prenatal test shows that your baby may be at increased risk for a genetic condition or birth defect. An ultrasound uses sound waves and a computer screen to show a picture of your baby inside the womb. Prenatal tests are medical tests you get during pregnancy. They help your provider find out how you and your baby are doing.
- Your baby’s newborn screening results show that your baby may be at risk for genetic condition. Babies get newborn screening before they leave the hospital after birth to check for certain rare but serious health conditions.
- You’ve had two or more miscarriages or babies who died after birth. A miscarriage is the death of a baby in the womb before 20 weeks of pregnancy.
What happens at genetic counseling?
When you go to see a genetic counselor, she:
- Takes your family health history. Your counselor uses this information to see how your family’s health may affect you and your children.
- May set up appointments for you to have tests to check for genetic conditions. You can get some of these tests before pregnancy to help you understand your chances of passing a genetic condition to your baby.
- Helps you understand test results and your baby’s risk for genetic conditions. Your counselor works with you and your health care provider to help you make decisions about your baby’s health.
- Refers you to medical specialists, education resources and support groups that focus on your baby’s condition. A support group is a group of people who have the same kind of concerns who meet together to try to help each other.
More information
- Centers for Disease Control and Prevention (CDC)
- CDC Show Your Love Campaign
- Einstein Victor Center for the Prevention of Jewish Genetic Diseases
- Genetic Alliance
- JScreen at Emory University
- National Center for Education on Maternal and Child Health
- National Organization for Rare Disorders (NORD)
- National Society of Genetic Counselors
Last reviewed: November, 2016
Prenatal Genetic Counseling - HealthyChildren.
 org
orgLog in | Register
Ages & Stages
Ages & Stages
Listen
Español
Text Size
What is Prenatal Genetic Counseling?Prenatal genetic counselors work with individuals, couples, or families who have an increased chance of having a child with a birth defect or genetic condition.
Those who are already pregnant or are considering having a child in the future can meet with a prenatal genetic counselor to learn more about the condition in question, understand their risks more clearly, and discuss options for prenatal screening, testing, and/or assisted reproduction techniques such as sperm and egg donation.
During pregnancy, if a baby is found to have a birth defect or genetic condition you may be referred to a prenatal genetic counselor. The counselor will help the expecting parent(s) understand the medical information, what to expect, how to prepare, and options.
The counselor will help the expecting parent(s) understand the medical information, what to expect, how to prepare, and options.
Prenatal counselors also help many families who do not have an increased chance of having a child with a birth defect or genetic condition to understand prenatal screening and testing options. Procedures such as blood tests and ultrasounds may be able to give a better idea if a developing baby has a chance of having birth defects or a genetic condition.
Why See a Prenatal Genetic Counselor?If you:
- Are worried about a genetic condition or a disease that runs in your family.
- Have a child who is affected with a genetic condition and are thinking about having another child in the future.
- Have family members with an intellectual disability or birth defects.
- Have a history of infertility or pregnancy losses (miscarriages or stillbirths).
- Are concerned that your health or lifestyle poses a risk to the pregnancy.

- Are concerned about risks to the pregnancy associated with increasing parental age.
- Receive abnormal prenatal screening or ultrasound results.
- Are concerned that you are at increased risk of being a carrier of a genetic condition because of your ethnic background (some diseases are more common in certain ethnicities).
- Are pregnant and the baby has been diagnosed with a birth defect or genetic condition.
- Have taken a medication or drug during pregnancy or have been exposed to a chemical and are concerned that it might cause a problem for the baby.
Depending on the reason for the visit, some things a genetic counselor may do during an appointment are:
- Go over your family and medical history with you.
- Figure out and explain your chances of having a child with specific genetic conditions.
- Help you explore and make decisions about your options for screening and testing before and during pregnancy.
- Help you interpret screening or testing results.

- Help you understand medical and genetic information.
- Provide you with information about any problems detected during pregnancy and help you understand your options.
- Provide counseling and emotional support.
- Refer you to support and advocacy networks.
- Your Family Health History & Genetics
- Detecting Genetic Abnormalities
- Reduce the Risk of Birth Defects
- Tests During Pregnancy
- Ethical and Policy Issues in Genetic Testing and Screening of Children (AAP Policy Statement)
- Last Updated
- 9/13/2013
- Source
- Adapted from Making Sense of Your Genes: A Guide to Genetic Counseling (Copyright © 2008 National Society of Genetic Counselors)
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Medical genetic counseling - articles from the specialists of the clinic "Mother and Child"
Belkovskaya Marina Edmundovna
Ultrasound doctor
Clinic "Mother and Child" Savelovskaya, Clinical Hospital MD GROUP, Clinical Hospital Lapino-1 "Mother and Child"
Given that in the course of its intrauterine life, the fetus may be at risk of developmental pathology, ideally, every married couple planning a pregnancy or already expecting an addition to the family should undergo medical genetic counseling.
How to help a future mother avoid the birth of a sick child?
Today, modern methods of genetic examination of a pregnant woman make it possible to suspect and exclude the presence of most malformations and chromosomal diseases in the fetus at the level of its intrauterine development.
At the stage of pregnancy planning, a genetic consultation will help spouses find out the prognosis for the birth of a child with a pathology.
Especially, this applies to married couples who have close relatives with hereditary diseases, in consanguineous marriages, if the family has already had cases of the birth of a child with a chromosomal pathology or malformations.
During pregnancy, all women must undergo research to identify those patients whose risk of having a child with a pathology exceeds the average.
A special risk group is made up of expectant mothers whose age is over thirty-five years.
At the first level of the survey, prenatal screening is used, which allows you to examine the level of biochemical markers (PAPP-A-protein, β-hCG, AFP) in the mother’s blood and calculate the individual risk of having a child with such serious diseases as Down syndrome, Edwards syndrome and malformations brain.
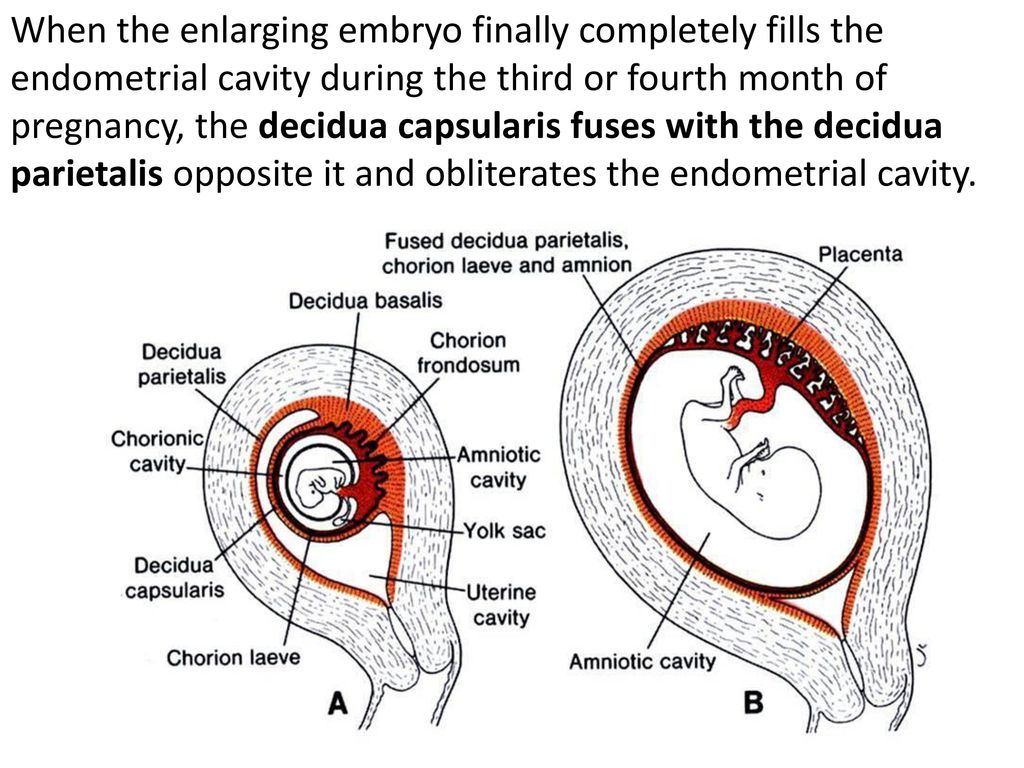
Prenatal screening is carried out at 10-13 and 16-20 weeks of pregnancy.
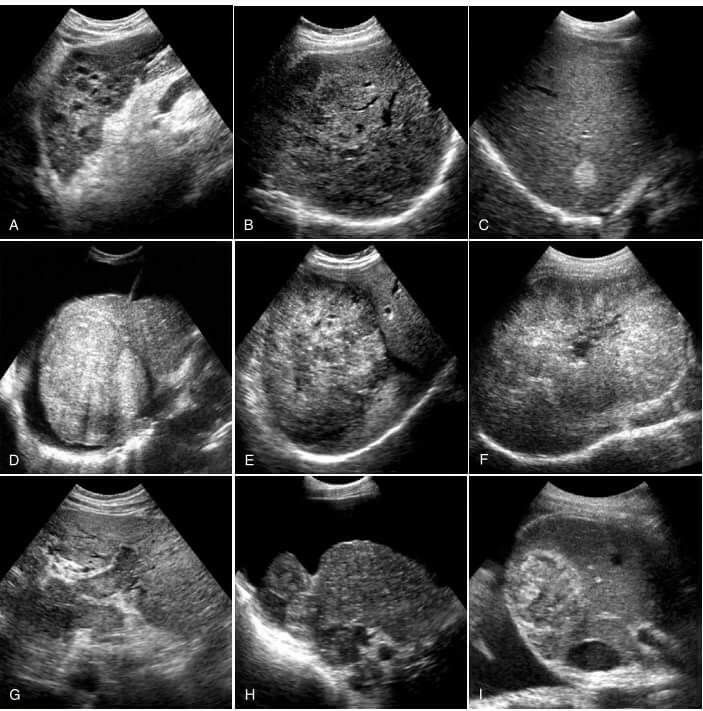
A huge role in the prenatal examination of pregnant women is played by ultrasound (ultrasound) in terms of 11-13 and 22-24 weeks.
If ultrasound data are detected for abnormalities in the development of the fetus or an increased risk of chromosomal diseases during screening, the expectant mother is offered an invasive prenatal diagnosis.
By gentle intrauterine intervention, placental tissue, amniotic fluid or fetal cord blood is taken in order to exclude or confirm chromosomal and gene diseases.
And, despite the fact that invasive diagnostics has a small risk of complications for the further course of pregnancy, it is necessary to accurately exclude such chromosomal diseases as Down syndrome, Edwards, Patau, as well as hemophilia, cystic fibrosis, myodystrophy, etc.
We would like to recommend our patients to be more attentive to their health and the health of their unborn child and to undergo all the necessary stages of prenatal genetic testing during pregnancy.
Make an appointment
to the doctor - Belkovskaya Marina Edmundovna
Clinical Hospital MD GROUP Clinical Hospital Lapino-1 "Mother and Child" Clinic "Mother and Child" Savelovskaya
Diagnostics
By clicking on the send button, I consent to the processing of personal data
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital MD GROUPClinical Hospital Lapino-1 "Mother and Child"Clinic "Mother and Child" SavelovskayaClinic "Mother and Child" Lefortovo
All directionsGenetic research (additional)Specialist consultations (adults)
01.
Genetic testing (additional)
02.
Specialist consultations (adults)
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
When is the best time to see a geneticist?
The best time to seek medical genetic counseling is when the family is still planning the birth of their first child. Such counseling is called prospective.
Such counseling is called prospective.
Medico-genetic counseling of families where the birth of a child with a hereditary or congenital pathology has already been noted is called retrospective. Ideally, this counseling should also take place between pregnancies.
You can also seek advice during pregnancy, but this option is somewhat worse, especially if the family does not apply in the first, but in the second trimester of the current pregnancy.
And finally, in some situations, premarital medical genetic counseling is useful - for example, if there are hereditary diseases in the family, or diseases with family accumulation, as well as in the consanguinity of spouses or a certain ethnicity (for example, there are hereditary diseases that are much more common in families where the spouses have a certain ethnicity).
Required recommendations
What recommendations can be given to the family as a result of medical genetic counseling
If counseling is provided before pregnancy , then after a quantitative assessment of the risk of hereditary and congenital pathology in the offspring, the family receives recommendations on:
- optimal preparation of spouses for pregnancy;
- and individual observation of the expectant mother during pregnancy;
- the ability to confirm or exclude specific hereditary diseases in the fetus in the first or second trimesters of pregnancy.
If counseling is carried out already "on the fact" of the onset of pregnancy , then, of course, we are talking only about recommendations for observation and prenatal diagnosis.
Pre-marital counseling may give advice on examining a marriage partner, and if the counselee is interested, advice on choosing a marriage partner.
The final stage of counseling (the advice of a geneticist) requires the most careful attention. As noted by some authors, many subjects are not ready to perceive genetic information. All persons who come to the consultation want to have a child and expect a positive response from the consultants. Often their requests are unrealistic, because they do not know about the capabilities of a genetic consultant and expect practical help from him.
The goal of genetic counseling is to reduce the burden of pathological heredity , and the purpose of a separate consultation is to help the family make the right decision about family planning.
Medical genetic counseling is most effective when given as a prospective (long-term follow-up) counseling. In this case, the risk of having a sick child is determined before the onset of pregnancy or in its early stages. Such consultations are carried out in case of consanguinity of the spouses, with aggravated heredity through the husband or wife, exposure to possible or known teratogens in the first three months of pregnancy, unsuccessful pregnancy and repeated spontaneous abortions.
Retrospective counseling is carried out after the birth of a sick child (congenital malformations, physical retardation and mental retardation), as well as if the spouses themselves or their relatives have congenital malformations, hereditary diseases, mental retardation, regarding the health of future children. In principle, each a married couple must undergo medical genetic counseling before planning a childbearing. With the widespread introduction of medical genetic counseling, some reduction in the frequency of hereditary diseases, as well as mortality (especially for children), can be achieved. The main result of medical genetic counseling is moral - for those families in which sick children were not born or healthy ones were born.
The main result of medical genetic counseling is moral - for those families in which sick children were not born or healthy ones were born.
Ideally - this type of medical care is shown to all spouses planning childbearing. Counseling of all families can be recognized as the optimal approach, since in a number of countries this practice has significantly reduced the number of disabling diseases, which means that it has prevented many human tragedies. But total medical genetic counseling is extremely rare. In the vast majority of countries, families turn to a geneticist only if there are risk factors - family history, spouses' lifestyle, their state of health. Statistics show that there are about 10% of such “families at risk”. This approach is more economical, but its effectiveness largely depends on the degree of medical and biological education of the population. Specifically, it depends on the ability of the spouses to assess whether their family is in the aforementioned risk group.
Indications for genetic counseling:
- the birth of a child with congenital malformations;
- established or suspected hereditary disease in the family;
- delayed physical development or mental retardation in a child;
- repeated spontaneous abortions, miscarriages, stillbirths;
- closely related marriages;
- mother's age over 35;
- adverse effects of environmental factors in the early stages of pregnancy (infectious diseases, especially viral etiology, massive drug therapy, x-ray diagnostic procedures, work at enterprises that are harmful to health).
How is the risk of hereditary and congenital pathology in offspring assessed?
At the appointment with a geneticist, all the main components of the above risk are “weighed”. In fact, each person carries an average of 4 hereditary disease genes. This is an extremely rough estimate, but in fact, the number of pathological mutations in the genome of any person is much greater. Assessing the risks of genetic diseases begins with the compilation of the pedigree of this family. The pedigree allows you to estimate how many relatives the geneticist will have to "work with", determine the type of inheritance of diseases in this family (if any) and provide a lot of useful information. You can come to an appointment with a specialist with a ready-made pedigree. This will allow more rational use of time at the reception. After compiling a pedigree, a hereditary history is assessed, the presence of certain diseases in the family.
Assessing the risks of genetic diseases begins with the compilation of the pedigree of this family. The pedigree allows you to estimate how many relatives the geneticist will have to "work with", determine the type of inheritance of diseases in this family (if any) and provide a lot of useful information. You can come to an appointment with a specialist with a ready-made pedigree. This will allow more rational use of time at the reception. After compiling a pedigree, a hereditary history is assessed, the presence of certain diseases in the family.
After clarifying all the necessary information, the segregation genetic load of the consulted family emerges. And already depending on this load, the specialist gives recommendations. In addition to the burden of pathological heredity, environmental factors are also assessed that may adversely affect the genome of the germ cells of the spouses, as well as the development of the fetus. Many points are taken into account - industrial and domestic hazards, the state of health of spouses, their diseases and their intake of various medications in the period preceding conception or directly during pregnancy, etc.
Risk Assessment
What is the risk of having a child with a hereditary disease or congenital deformity?
Any married couple is at risk of having a child with a hereditary disease or congenital malformation in every pregnancy.
This risk is made up of many components:
- hereditary cargo inherited from many generations of ancestors;
- fresh mutations occurring in the DNA of our eggs and sperm;
- adverse physical, chemical and other environmental influences on the body of a developing embryo;
- similar effects on the embryo from the maternal organism (infectious, endocrine and other diseases of the mother).
The simplest assessment "offhand" will show - any of us has the above risk factors. Therefore, a quantitative assessment of their danger to the offspring of a particular family is needed. Fortunately, in most cases, the risk of having a child with a hereditary disease is low - less than 5%.