Pregnancy cbc test results
Routine laboratory testing during pregnancy
Most general practitioners no longer offer lead maternity care, however, may still be involved with the initial confirmation of pregnancy and first laboratory tests and general care during pregnancy. The following article provides guidance on appropriate testing in early pregnancy, throughout pregnancy and information about common changes to testing reference ranges during pregnancy.
Blood tests included in the first antenatal screen
When a woman becomes pregnant, it is recommended that she receives a range of standard investigations. A first antenatal screen is required even if the woman is considering termination of pregnancy.
The “first antenatal screen” may be requested by the GP at the first appointment when pregnancy is confirmed,
and the results later forwarded to the chosen Lead Maternity Carer (LMC). If the woman is likely to enrol with a LMC in
the near future, the tests can be delayed, at the patient’s request, until her first appointment with the LMC.
Tests included in the first antenatal screen include:
- Complete blood count
- Blood group and antibody screen
- Rubella antibody status
- Syphilis serology
- Hepatitis B serology
- HIV
Prior to all laboratory testing in pregnancy, information should be provided to the pregnant woman about why the test is recommended, the implications of both a positive or negative result, the risk of disease transmission to the foetus (if relevant) and how the results will be delivered. Verbal consent (or decline) should be documented in the patients notes.1
Although the first antenatal screen usually occurs early in pregnancy, it may be requested at any stage of pregnancy, i.e. if a women presents for the first time late in pregnancy, she should still receive a first antenatal screen.
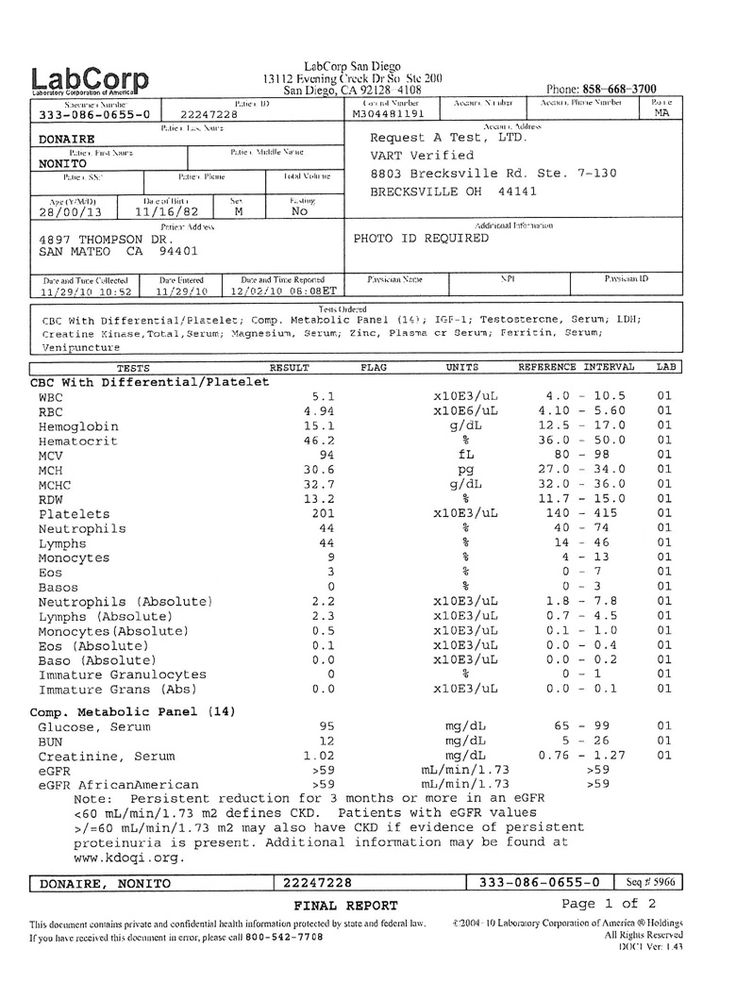
Complete blood count
A complete blood count (CBC) gives information on a number of haematological parameters, but generally
in pregnancy the most useful are the haemoglobin, platelets and white blood cell count. Most laboratories will provide
pregnancy adjusted reference ranges to enable easier interpretation.
Most laboratories will provide
pregnancy adjusted reference ranges to enable easier interpretation.
Very low or high haemoglobin levels are associated with increased foetal risk.2 Gestational age should be taken into account when assessing haemoglobin, as levels decrease during pregnancy due to haemodilution caused by increased plasma volume.2 The lower limit for haemoglobin is usually 115 g/L, but for pregnant women the lower limit is usually reported as 100 g/L.
Iron deficiency anaemia is the most frequent haematological concern during pregnancy and is usually characterised by decreased haemoglobin, mean cell volume (MCV) and mean cell haemoglobin (MCH) levels. When iron deficiency is suspected, a measurement of serum ferritin should be used to confirm the diagnosis.2
Changes in platelet levels are frequently seen during pregnancy. A decrease in the platelet count is
more common than an increase and is most obvious in women who had low levels prior to becoming pregnant. Platelets usually
decrease as a result of haemodilution, and this can become more pronounced as the pregnancy progresses from the second
to third trimester.3 A platelet level of 150 x 109/L or less is abnormally low and should be discussed with
a haematologist.
Platelets usually
decrease as a result of haemodilution, and this can become more pronounced as the pregnancy progresses from the second
to third trimester.3 A platelet level of 150 x 109/L or less is abnormally low and should be discussed with
a haematologist.
Elevated platelets levels during pregnancy are generally a reactive response to the pregnancy and do not usually suggest a clinical problem. However, due to the slightly increased risk of clotting, it would be advisable, when platelet levels are higher than 600 x 109/L, to discuss results with a haematologist.
The total white cell count will frequently be elevated in pregnancy due to increased numbers of neutrophils. Neutrophils can also demonstrate a “left shift” (increased number of band neutrophils). However, this neutrophilia is not usually associated with infection or inflammation.
The total white cell count can also be misleading in pregnant women and should be interpreted with care, e.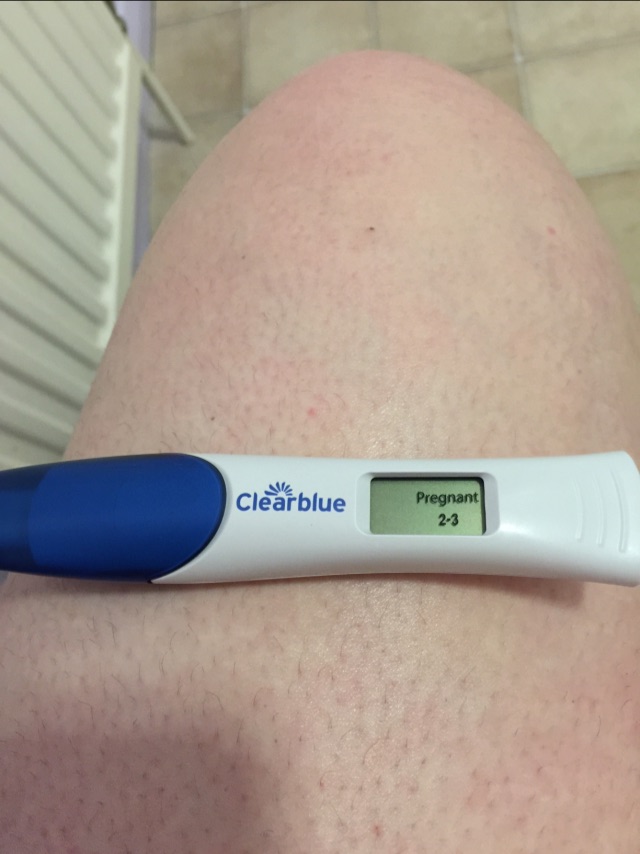 g. elevated
neutrophils with a low lymphocyte count may produce a total white count that falls within the reference range. Therefore
the absolute count of each cell type is more useful than the total white cell count.
g. elevated
neutrophils with a low lymphocyte count may produce a total white count that falls within the reference range. Therefore
the absolute count of each cell type is more useful than the total white cell count.
Maternity care funding for general practice
Within the funding of primary maternity services in New Zealand, a clinician who is not the lead maternity carer may access funding for one pregnancy-related visit during the first trimester. In general practice, this funding may be used, for example, when a patient presents for confirmation of pregnancy and the first antenatal screen.
N.B. Consultations regarding a potential pregnancy are not eligible for this funding if pregnancy is not confirmed.
Blood group and antibody screen
Identifying ABO blood group, rhesus D status and red cell antibodies in pregnant women is important to prevent “haemolytic disease of the newborn” in subsequent pregnancies.
If the foetus is rhesus D-positive (and the mother is negative), the mother may form anti-D antibodies, which may affect
a subsequent rhesus D-positive foetus.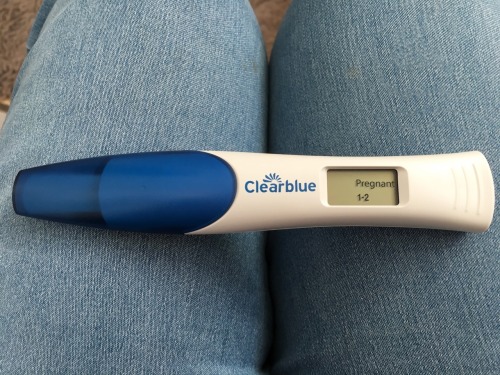 Anti-D antibodies can be formed during a range of situations, including amniocentesis,
chorionic villus sampling (CVS), external cephalic version (ECV), bleeding during the pregnancy, major abdominal trauma
and late miscarriage.
Anti-D antibodies can be formed during a range of situations, including amniocentesis,
chorionic villus sampling (CVS), external cephalic version (ECV), bleeding during the pregnancy, major abdominal trauma
and late miscarriage.
Haemolytic disease of the newborn in subsequent pregnancies, can be avoided by antenatal prophylaxis of commercial anti-D in the second and third trimesters, and post-natally.2
Rubella antibody status
All pregnant women should be screened for rubella antibodies. Contracting rubella during pregnancy presents a high risk of harm to the foetus. Congenital Rubella Syndrome occurs when the rubella virus infects the developing foetus, especially during the first trimester when up to 85% of affected infants will be born with a birth defect, e.g. deafness, eye defects, heart defects, mental retardation. The risk of birth defects is decreased when infection occurs after 20 weeks gestation.4
The aim of screening is to identify women who have not been immunised or have diminished immunity and are susceptible
to contracting rubella, so they can be immunised in the postnatal period to protect future pregnancies. 2,5 Rubella
vaccination cannot be given during pregnancy (as it is a live vaccine) and if a mother contracts rubella during pregnancy
there is no way to prevent transmission to the infant.2
2,5 Rubella
vaccination cannot be given during pregnancy (as it is a live vaccine) and if a mother contracts rubella during pregnancy
there is no way to prevent transmission to the infant.2
Rubella antibody titres should be measured at each pregnancy as levels may decline and fall below protection levels. This is more often seen in people only exposed to the virus through immunisation.6
Interpreting low rubella titres in previously immune women
A rubella antibody level greater than 10 IU/mL usually indicates protection from the disease, however, re-infection
with rubella has still been reported in women with antibody levels above 15 IU/mL. Therefore, pregnant women with rubella
antibody levels less than 15 IU/mL should be advised to avoid coming into contact with people with rubella. Women with
antibody levels less than 25 IU/mL, who have received only one dose of MMR, can be advised to have a second dose after
delivery. 7
7
Syphilis serology
All pregnant women should be screened for syphilis.2 Mothers infected with syphilis can experience long-term morbidity and the complications for pregnancy are significant; 70 to 100% of infants will be infected and one-third will be stillborn.2 In recent years rates of syphilis in New Zealand have been increasing (2006–2009).8 However, latest surveillance data show that although syphilis infection is still a concern, rates now appear to be decreasing.9
Mother-to-child transmission of syphilis in pregnancy is associated with non-immune hydrops (a life-threatening condition of severe oedema in the foetus and newborn infant), intrauterine growth retardation, malformations and perinatal death. Infected infants, who do survive, often have long-term disabilities.2
Universal screening for syphilis in newly pregnant women is recommended by the Royal Australian and New Zealand College
of Obstetricians and Gynaecologists (RANZCOG).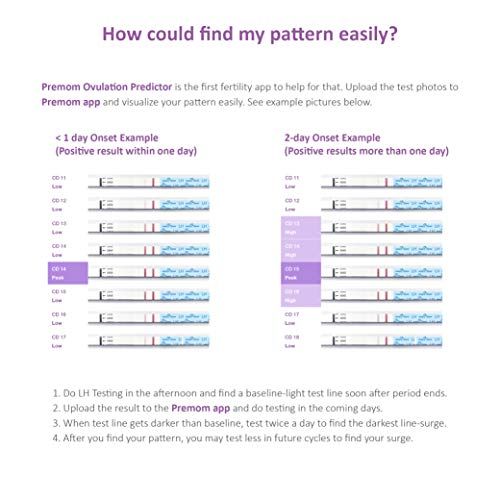 Women who test positive can then receive prophylactic antibiotic treatment.
Penicillin is a safe and effective treatment for syphilis in pregnancy and can prevent congenital syphilis.10
Women who test positive can then receive prophylactic antibiotic treatment.
Penicillin is a safe and effective treatment for syphilis in pregnancy and can prevent congenital syphilis.10
The RANZCOG recommends that a treponemal test, e.g. Treponema pallidum particle assay (TPPA), is used to screen for syphilis as this can detect primary or secondary infection.6
Hepatitis B serology
Up to 85% of infants born to mothers infected with hepatitis B (particularly mothers who are HBeAg positive, i.e. with active infection), will become carriers and will be more likely to develop chronic liver disease, including cirrhosis, liver failure or liver cancer.2,11 Transmission of the hepatitis B virus from mother to infant can be prevented by administration of the hepatitis B vaccine and immunoglobulin to the infant at birth, therefore screening is important.11,12
Women who are at increased risk of acquiring hepatitis B, e. g. women with sexual partners who are hepatitis B positive
or intravenous drug users, are recommended to be vaccinated during pregnancy.5
g. women with sexual partners who are hepatitis B positive
or intravenous drug users, are recommended to be vaccinated during pregnancy.5
HIV screening
All pregnant women should be screened for HIV. Women who are HIV positive can be given treatment to reduce the risk of HIV being transmitted to their infant (risk reduced from 32% to less than 1%).1 Interventions to reduce mother-to-child transmission of HIV infection include antiretroviral therapy, elective caesarean section delivery and the avoidance of breastfeeding.1,2
Any person undergoing a HIV test should be properly counselled about the implications of the test and the results, including how they wish to receive the results.
If a patient is considered at risk for HIV, hepatitis C screening should also be considered.
Best Practice Tip: In some DHB regions, HIV testing is automatically
included as part of the antenatal screen, while in others, mothers must “opt on” for screening. The standard
tick box for first antenatal screen does not always include HIV screening. Practices may wish to alter their electronic
lab form to include an HIV tick box as a reminder to counsel patients on HIV screening and to add the test to the standard
screen.
The standard
tick box for first antenatal screen does not always include HIV screening. Practices may wish to alter their electronic
lab form to include an HIV tick box as a reminder to counsel patients on HIV screening and to add the test to the standard
screen.
Additional testing in early pregnancy
Consider checking varicella antibody status in pregnant women with no (or uncertain) history of illness
(i.e. chicken pox or shingles) or vaccination.6 Contracting varicella during pregnancy is associated with a
significant risk of harm to both mother and infant. There is a 0.7–2% risk of congenital varicella syndrome if varicella
is contracted by the mother between eight and 20 weeks gestation.13 Congenital varicella syndrome can cause
blindness, growth retardation, limb and cranial malformations, delayed development, mental retardation, spontaneous abortion
or foetal death. Contracting varicella between 25 to 36 weeks gestation increases the risk of the infant developing herpes
zoster infection (shingles) after birth.13 There is a 17–30% risk of serious disease in a newborn infant if
the mother contracts varicella between five days before birth and two days after.13
Contracting varicella between 25 to 36 weeks gestation increases the risk of the infant developing herpes
zoster infection (shingles) after birth.13 There is a 17–30% risk of serious disease in a newborn infant if
the mother contracts varicella between five days before birth and two days after.13
As with the rubella vaccine, varicella is a live vaccine so cannot be given during pregnancy. Mothers with no (or diminished) immunity to varicella should consider immunisation to protect subsequent pregnancies.
If a mother with no history of varicella (and/or an absence of antibodies) is exposed to varicella during pregnancy, she may be offered either immunoglobulin (Zoster Immunoglobulin-VF) within 96 hours of exposure or acyclovir at the onset of symptoms. Treatment should be discussed with an infectious diseases physician. Zoster Immunoglobulin-VF is also recommended for:14
- Newborn infants who’s mother has had chicken pox seven days before to seven days after delivery (not shingles)
- Hospitalised pre-term infants who’s mothers have no history of chicken pox
A cervical smear may be considered at the first antenatal visit if the woman would be due for a routine
test during the pregnancy (because as the pregnancy progresses, it may cause more discomfort to perform the test).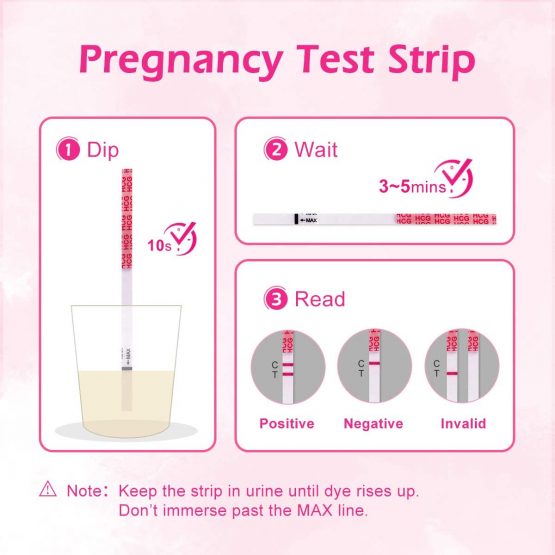 6 This
is recommended by the RANZCOG who also states that there is no evidence that performing a smear is harmful to the foetus
during pregnancy.6 However, other countries such as the United Kingdom recommend that in most cases pregnant
women should not have a cervical screening test, as pregnancy can make the results of the test more difficult to interpret
and potentially inaccurate.15 The decision whether to perform a routine cervical screening test during pregnancy
should be based on clinical judgement and patient preference, taking into consideration factors such as previous abnormal
smear results and time since last test.
6 This
is recommended by the RANZCOG who also states that there is no evidence that performing a smear is harmful to the foetus
during pregnancy.6 However, other countries such as the United Kingdom recommend that in most cases pregnant
women should not have a cervical screening test, as pregnancy can make the results of the test more difficult to interpret
and potentially inaccurate.15 The decision whether to perform a routine cervical screening test during pregnancy
should be based on clinical judgement and patient preference, taking into consideration factors such as previous abnormal
smear results and time since last test.
Testing for chlamydia and gonorrhoea should be considered for those who may be at increased risk based on age (e.g. less than 25 years) and sexual history.6
Vitamin D is required for normal bone growth development in the foetus.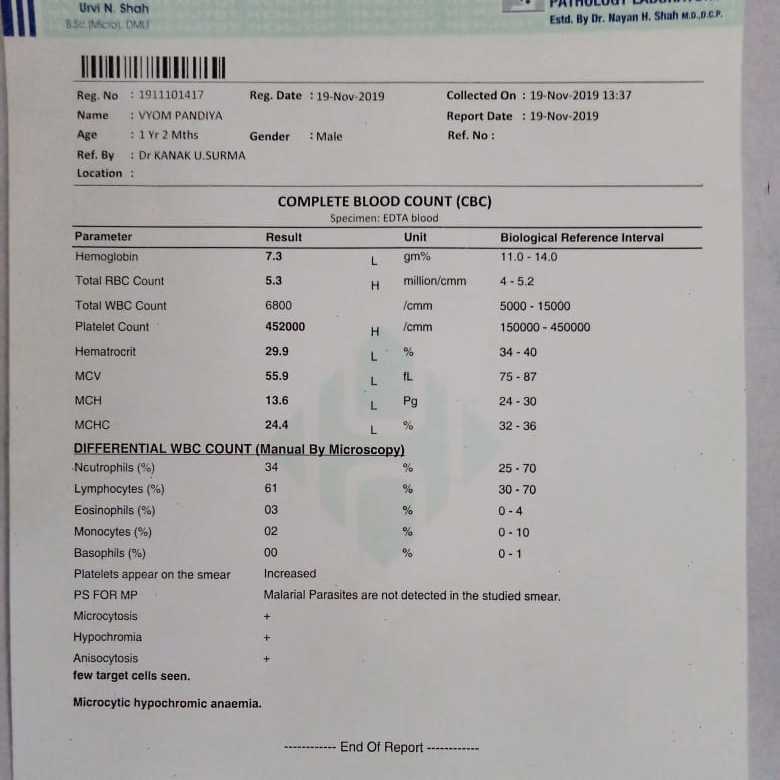 Mothers with known vitamin
D deficiency, or who are at risk for deficiency (e.g. dark skinned women, women who wear a veil) should receive vitamin
D supplementation (cholecalciferol) without the need for testing.
Mothers with known vitamin
D deficiency, or who are at risk for deficiency (e.g. dark skinned women, women who wear a veil) should receive vitamin
D supplementation (cholecalciferol) without the need for testing.
For further information see "Vitamin D supplementation: navigating the debate", BPJ 36 (June, 2011), and "Correspondence: Use of vitamin D during pregnancy", BPJ 38 (September, 2011).
N.B. Screening for toxoplasmosis or CMV infection during pregnancy is not routinely recommended in New Zealand.
Blood tests included in the second antenatal screen
At 26–28 weeks gestation, a second round of blood tests, commonly referred to as the “second antenatal” tests, is advised for pregnant women. In most cases the LMC will arrange these tests.
The second antenatal screen includes:
- 50 g glucose tolerance test (the ”polycose” test)
- CBC
- Blood group antibodies
Screening for gestational diabetes
Updated information on screening for gestational diabetes can be found here: http://www. bpac.org.nz/BT/2015/July/diabetes.aspx
bpac.org.nz/BT/2015/July/diabetes.aspx
Gestational diabetes affects 5–8% of pregnant women and is associated with hypertensive disorders, macrosomia, shoulder dystocia, increased rates of caesarean delivery and the development of maternal diabetes later in life.5,16
In New Zealand, it is recommended that testing for gestational diabetes occurs for all women between 26 and 28 weeks of gestation. Women at particularly high risk of gestational diabetes may be tested earlier.17 Factors which increase the risk of gestational diabetes include; gestational diabetes in a previous pregnancy, family history of diabetes, belonging to a high risk ethnic group for diabetes, e.g. Māori, Pacific or South Asian (Indian).17
A 50 g glucose tolerance test (the polycose test) is used to screen for gestational diabetes. A 50 g glucose load is
given to the non-fasting patient, and a glucose level is determined after one hour.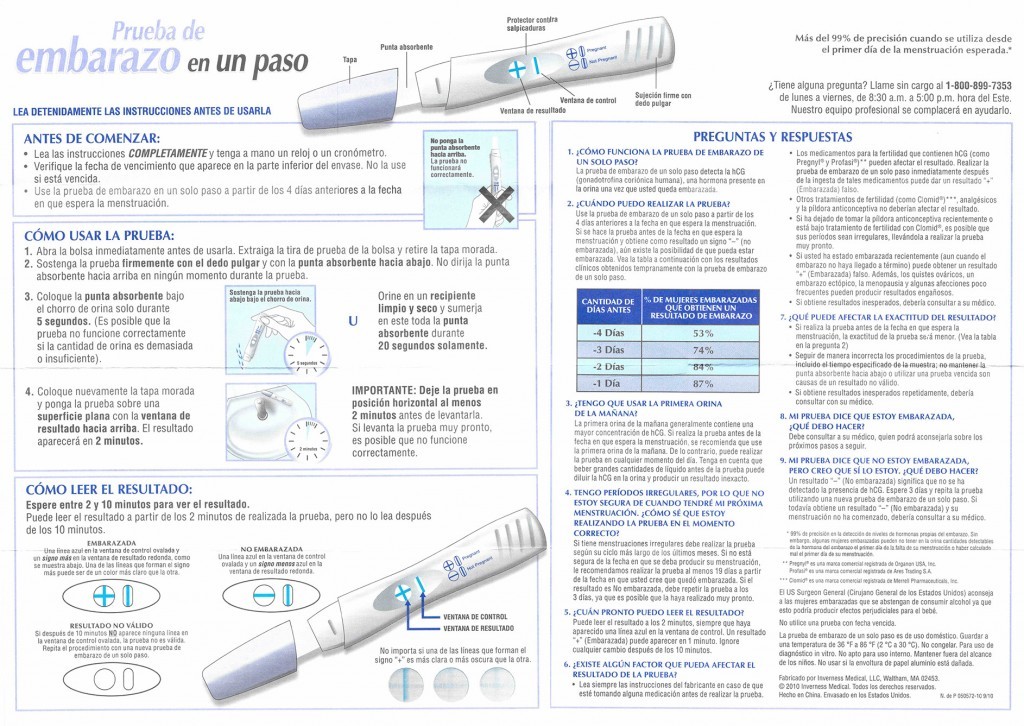 Women with an elevated result should
be followed up with a 75 g oral glucose tolerance test (OGTT).
Women with an elevated result should
be followed up with a 75 g oral glucose tolerance test (OGTT).
Women who have had gestational diabetes during pregnancy should undergo an OGTT six to eight weeks after delivery. Even if not found to have diabetes at this time, women who have had gestational diabetes have an increased risk of developing type 2 diabetes within 15 years,18 and should be screened with a fasting glucose test every one to two years.17
Repeat CBC and antibody screening
The CBC should be repeated at 28 weeks gestation, in particular to check haemoglobin and platelet levels (see commentary in previous section on how to interpret and manage these levels in pregnancy).
Antibody screening should also be repeated at 28 weeks gestation, to ensure no additional antibodies have developed.
While blood group testing does not need to be repeated for subsequent pregnancies, the antibody screen should still be
repeated. 2,6
2,6
Summary of routine antenatal tests
| Laboratory | ||
| Initial tests “First antenatal” |
CBC | |
| Blood group and antibodies | ||
| Rubella | ||
| Syphilis | ||
| Hepatitis B serology | ||
| HIV | ||
| Urine culture | ||
| 26–28 weeks “Second antenatal” |
CBC | |
| Polycose | ||
| Antibodies | ||
| Urine culture | ||
| 35–37 weeks Group B streptococcal (GBS) infection (if risk factors) |
Vaginal swab | |
| Urine culture | ||
| Testing for genetic conditions (only one option applies) | ||
| First trimester screening 11– <14 weeks |
NT scan | |
| Blood tests for PAPP-A, βhCG (3–4 days before scan) | ||
Second trimester screening |
βhCG | |
| AFP | ||
| µE3 | ||
| Inhibin A | ||
Additional tests during pregnancy
Sub-clinical urine infection
It is recommended that all women have a mid-stream urine culture at the time of the first antenatal screen, again at
the second antenatal screen and then at 36 weeks gestation, to exclude a sub-clinical urine infection (asymptomatic bacteriuria).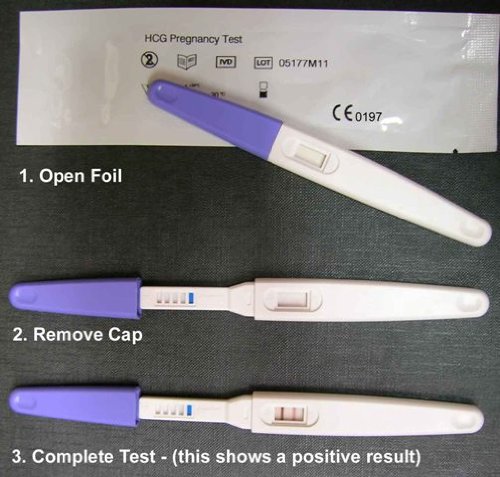 Asymptomatic bacteriuria occurs in 2% to 10% of pregnancies and can lead to maternal pyelonephritis and may contribute
to low birth-weight infants and pre-term birth (≤ 37 weeks).19
Asymptomatic bacteriuria occurs in 2% to 10% of pregnancies and can lead to maternal pyelonephritis and may contribute
to low birth-weight infants and pre-term birth (≤ 37 weeks).19
Screening for Group B Streptococcus
Group B streptococcal (GBS) infection is a significant cause of serious neonatal infection. Approximately 15–25% of women will be carriers, and one in 200 of these women will have infants who develop neonatal sepsis.20
Women may have a vaginorectal culture collected at 35 to 37 weeks gestation. Swabs may be collected by the patient, who has been instructed to swab the lower vagina first, and then rub the swab over the floor of the perineum to the anus, i.e. in a front-to-back direction. If positive for GBS, the mother should receive intrapartum antibiotic prophylaxis.20
Risk factors for GBS that would identify the need for intrapartum antibiotic prophylaxis include:20
- Pre-term labour, gestation ≤ 37 weeks
- Prolonged rupture of membranes ≥ 18 hours
- Maternal fever ≥ 38°C
- Previous GBS infected infant (prophylaxis required in all subsequent pregnancies)
- GBS bacteriuria during pregnancy (prophylaxis required in all subsequent pregnancies)
Testing for Down syndrome and other genetic conditions
Screening for Down syndrome, other chromosomal abnormalities and neural tube defects is offered to all pregnant women
in New Zealand and testing can occur in either the first or second trimester of pregnancy.
Women need to be provided with enough information to make an informed decision about screening. Information should include the following:
- Reassurance that screening is voluntary
- Details of which screening options are available, the tests involved, the timing of the tests and where to go to get the tests
- Limitations of the tests, e.g. not all infants with the condition(s) being tested for will be identified, false positives are possible, testing is for specific conditions only and other abnormalities may be present
- Pamphlets explaining the different screening options are available from the National Screening Unit: www.nsu.govt.nz
First trimester screening is based on the combination of results of the following tests:
- Pregnancy-associated plasma protein A (PAPP-A)
- Beta-human chorionic gonadotropin (βhCG])
- Nuchal translucent (NT) scan
The PAPP-A and βhCG tests must be taken between nine and 13 weeks gestation (ideally between 10 and 12 weeks),
and the NT scan carried out after 11 and before 14 weeks gestation.
Second trimester screening can be offered to all women who present after 14 weeks gestation but before 20 weeks, who have not completed first trimester screening (bloods are ideally taken between 14 to 18 weeks gestation). This serum screen measures βhCG, alpha-fetoprotein (AFP), unconjugated oestriol (µE3), and inhibin A.
If the results of either first or second trimester screening indicate an increased risk of foetal abnormalities, the mother should be referred to an obstetrician.
N.B. Women can only access one publically funded screening option. If they have the first trimester screening option,
the blood tests will be fully funded and there is no cost to the patient, however, the NT scan may have a part-charge.
The second trimester blood tests will be fully funded providing the women has not already accessed the first trimester
screening. All sections of the laboratory referral form need to be filled out (including maternal age and weight, gestation
and family history) to allow for an accurate risk prediction.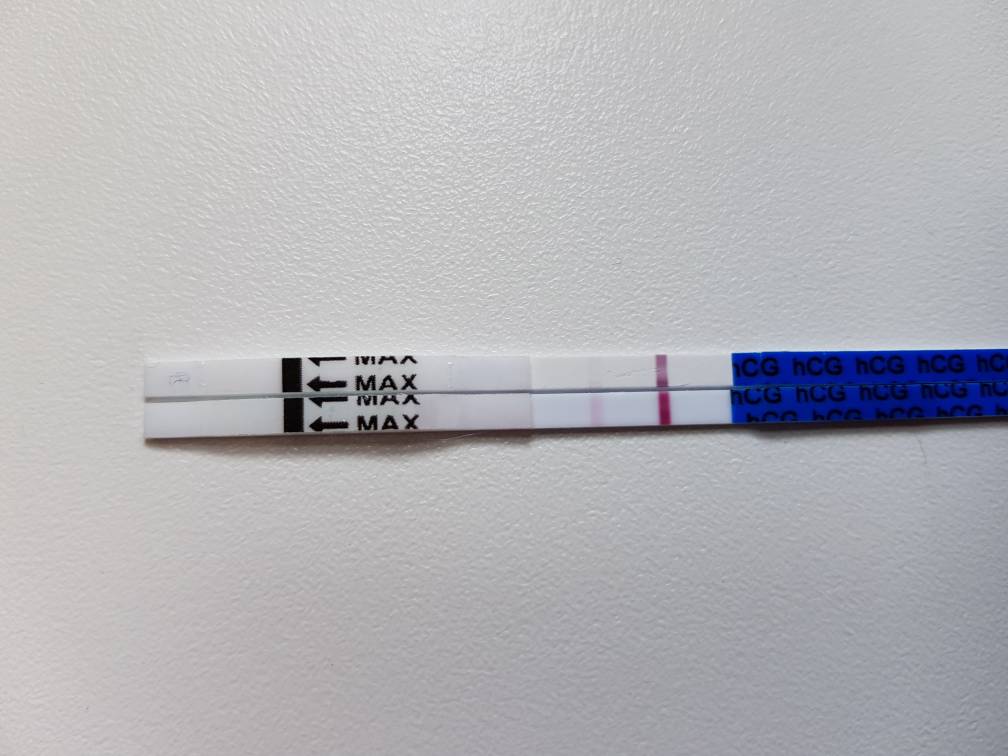
Woman at increased risk of foetal chromosomal abnormality, i.e. aged 35 years and over or have a family history of chromosomal disorder, should be referred to an obstetrician early in their pregnancy, to discuss the option of chorionic villus sampling (CVS) or amniocentesis. CVS is usually performed at 11–12 weeks gestation and amniocentesis at 14–18 weeks gestation. These tests allow a more accurate prenatal diagnosis of chromosomal abnormality, but are associated with an increased risk of harm to the foetus including; infection, amniotic fluid leakage and miscarriage.
An ultrasound scan is offered to all pregnant women at 18–19+ weeks gestation to check foetal anatomy for any abnormalities.
Changes to reference ranges during pregnancy (adapted from Kyle, 2008)
21| Analyte | Effect of pregnancy | Notes |
| Alpha-fetoprotein (AFP) | Peaks in last trimester | |
| Alkaline phosphatase (ALP) | Marked increase due to placental izoenzyme | |
| Blood volume | Increases by 20–30% | |
| Ca125 (tumour marker) | 2–2.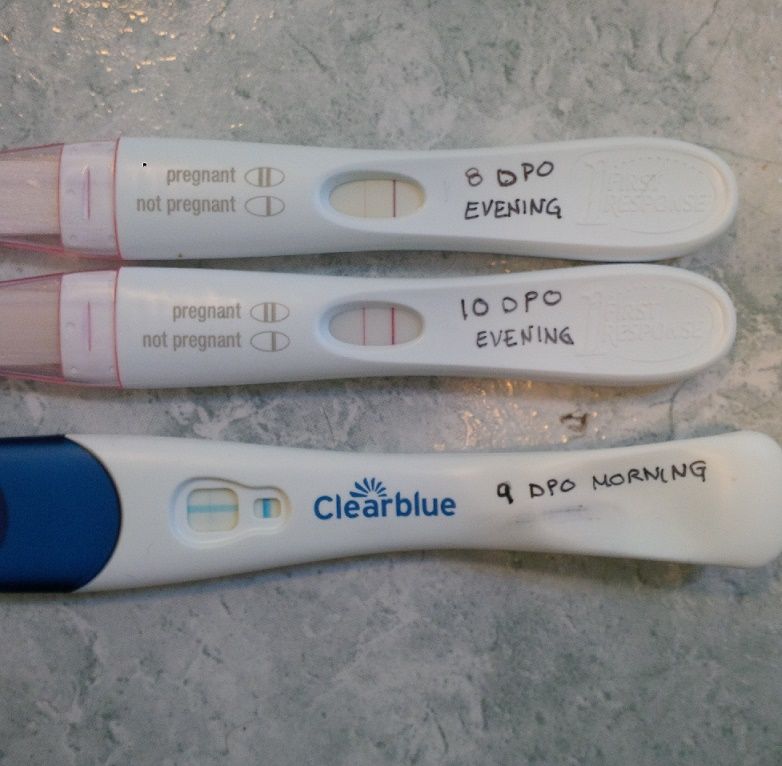 5 times increase in first trimester 5 times increase in first trimester |
|
| Cholesterol | Up to 40% increase | |
| Creatinine clearance | ||
| ESR | Increasing to 30–60 mm/hr as pregnancy progresses | |
| Iron binding | Significant increase | |
| White blood count | May increase to 15–18 x109/L | |
| CRP | ||
| Haemoglobin | Decreases as a result of haemodilution due to greater blood volume | |
| FT4 | May decrease up to 20% in late pregnancy | |
| TSH | Often decreases first trimester, but then returns to normal levels |
Prenatal Testing & Screening - Women's Health of Central Massachusetts
If you think you may be pregnant or already know you are, we’re here to help you have a healthy pregnancy and delivery.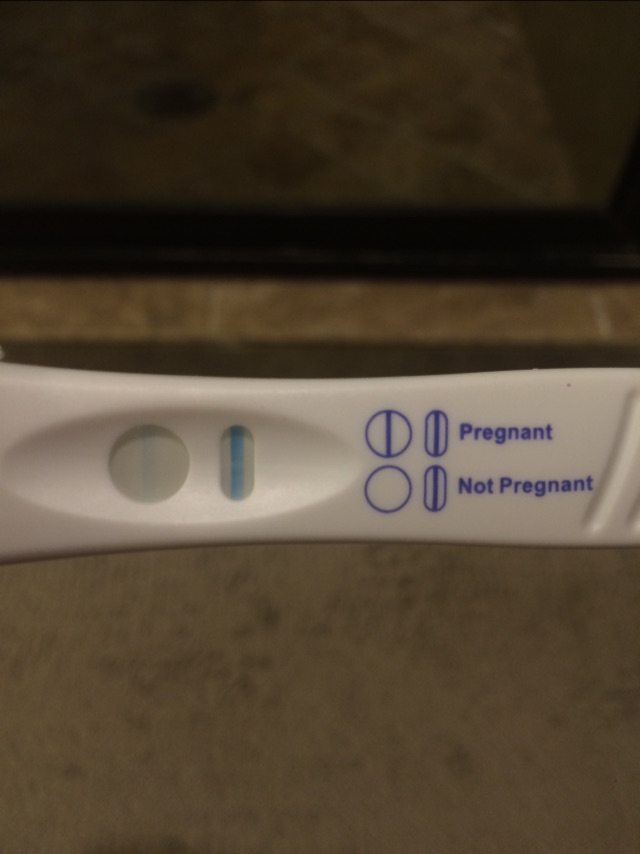 An essential part of ensuring your health and that of your baby is having certain prenatal and screening tests throughout your pregnancy.
An essential part of ensuring your health and that of your baby is having certain prenatal and screening tests throughout your pregnancy.
First Things First: Tests to Confirm that You’re Pregnant
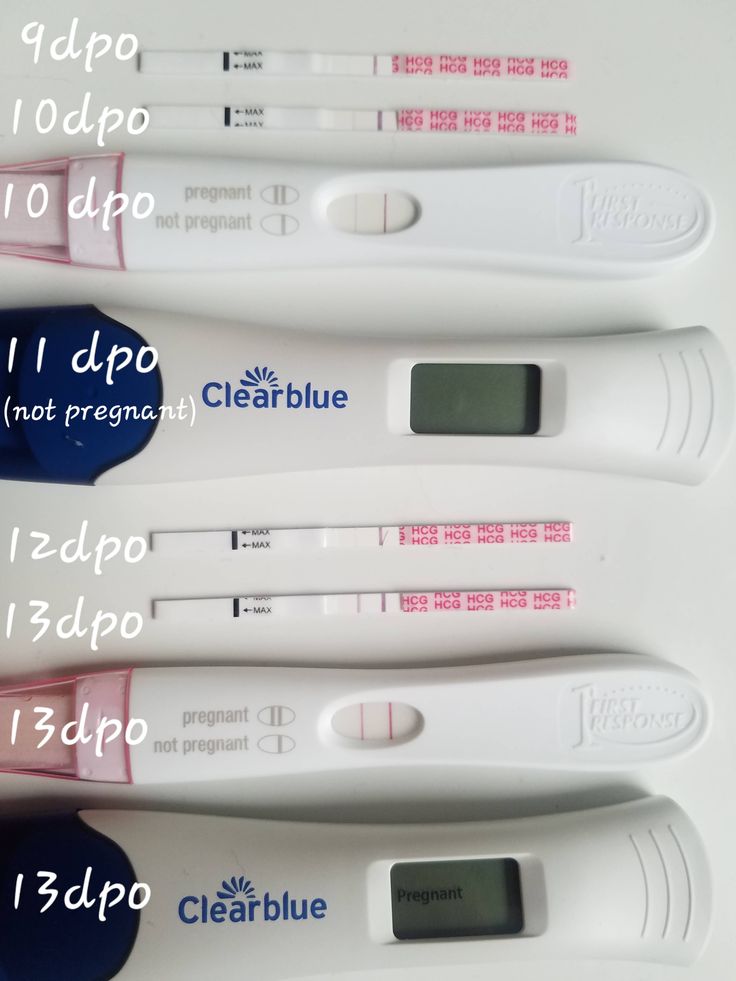
All pregnancy tests work by detecting a hormone in your blood or urine that’s there only if you’re pregnant. This hormone – human chorionic gonadotropin (hCG) – is produced when a fertilized egg implants in your uterus.
There are two types of pregnancy tests:
- A urine test can be performed at your doctor’s office or with a home pregnancy test
- Urine tests can usually tell if you’re pregnant about one week after a missed period
- A blood test checks your blood for hCG, and you need to see a doctor to have this test
- Blood tests can detect hCG earlier in a pregnancy than urine tests, usually 6 to 8 days after you ovulate
If a home pregnancy test shows that you’re pregnant, call your doctor right away. He or she can use a more sensitive test along with a pelvic exam to confirm it. Plus, seeing your doctor early in your pregnancy helps you and your baby stay as healthy as possible (visit our Prenatal Care & Delivery page to learn more about care during pregnancy).
He or she can use a more sensitive test along with a pelvic exam to confirm it. Plus, seeing your doctor early in your pregnancy helps you and your baby stay as healthy as possible (visit our Prenatal Care & Delivery page to learn more about care during pregnancy).
Routine Tests During Pregnancy
Certain laboratory tests are recommended for all women as part of routine prenatal care. These tests can help detect conditions that might put you or your fetus at risk of complications, and allow for timely treatment.
Tests Done in Early Pregnancy
- Complete Blood Count (CBC) with Differential/Platelet – Measures the numbers of different types of cells that make up your blood to check for anemia, infection and your blood-clotting ability
- Urinalysis and Urine Culture – Detects urinary tract disease, infection, glucose (high levels may be a sign of diabetes) and protein.
- Hepatitis B – Pregnant women with Hepatitis B virus (which infects the liver) can pass the virus to their babies
- Rubella (German Measles) – Can cause birth defects if a woman is infected during pregnancy.
 Your blood is tested to see if you’ve had a past rubella infection or if you’ve been vaccinated against it.
Your blood is tested to see if you’ve had a past rubella infection or if you’ve been vaccinated against it. - HIV – Pregnant women infected with HIV can be given medication and take other steps that greatly reduce the chance of passing the virus to their babies
- Varicella Zoster V Antibodies (Chicken Pox) – This test is done to detect whether a women is immune to varicella (chicken pox).
- Blood Typing – Determines your blood type and Rh factor (a protein on the surface of red blood cells). Blood types are either A, B, AB or O, and the Rh factor is either positive or negative.Problems can occur if a woman is Rh negative and her baby is Rh positive.
- Antibody Screen – If you are Rh negative, your immune system can develop an antibody that attaches to the Rh-positive antigens on your fetus’ red blood cells, targeting them for destruction. An antibody screen is used to detect these antibodies. The first Rh-positive baby is unlikely to become ill, but antibodies produced during a first pregnancy will affect future Rh-positive babies
- Sexually Transmitted Disease (STD) Testing – Pregnant women are screened for syphilis (a test called rapid plasma reagin, or RPR) and chlamydia early in pregnancy because these STDs can be passed to their babies and cause other complications.
- Thyroid Stimulating Hormone (TSH) – Because thyroid problems are associated with pregnancy complications, women are tested to ensure that their thyroid is functioning properly. This is tested in patients with specific family or medical history.
Tests Done Mid-Pregnancy
- Glucose Tolerance Test – This measures the level of glucose (sugar) in your blood; a high level may be a sign of gestational diabetes
- Hemoglobin and Hematocrit – It’s not uncommon to develop anemia as your pregnancy progresses, so your blood will be tested in your late second trimester or early third trimester
- RPR (Syphilis screen #2) – All women receive a second test to screen for syphilis in their second trimester
Tests Done in Late Pregnancy
- Group B Strep (GBS) Culture – GBS is a type of bacteria that lives in the vagina and rectum. Many women carry GBS without having symptoms, but it can be passed to a baby during birth and cause serious health problems.
 Antibiotics can be given during labor to help prevent infection of the baby.
Antibiotics can be given during labor to help prevent infection of the baby.
Tests to Screen for Birth Defects
Today there are several noninvasive screening tests available to you in the first and second trimesters of pregnancy to assess the chances that your fetus may have a genetic (inherited) disorder and/or birth defects. If you are at risk, your doctor will discuss these optional tests with you.
- Sequential Screen – A two-stage screening that assesses the risk of several chromosomal abnormalities including Down syndrome. The first stage (combining ultrasound and blood testing) can be performed between 11 weeks and 13 weeks and 6 days. The second stage (blood testing) can be performed between 15 and 22 weeks.
- Maternal Serum Quad Screen– A maternal blood screening test that looks for four specific substances in the blood
- Alpha Fetoprotein (AFP) – This blood test checks the level of AFP in a pregnant woman’s blood during the second trimester
- Carrier Screening – Testing that’s done to see if you or your partner carry a genetic mutation that could cause a serious inherited disorder (such as cystic fibrosis) in your baby
- Non-invasive prenatal testing (NIPT) – Also called cell free DNA testing (cfDNA), this blood test analyzes fetal DNA circulating in a pregnant woman’s blood; it can be performed at 10 weeks.
 The American Congress of Ob/Gyn does not recommend NIPT in pregnancies when there is more than one fetus (twins, triplets, etc…).
The American Congress of Ob/Gyn does not recommend NIPT in pregnancies when there is more than one fetus (twins, triplets, etc…).
It’s important to understand that these screening tests do not diagnose a problem; they only signal that further testing (such as amniocentesis or chorionic villus sampling) should be done.
Because many of these tests are done in women who are at high risk for having a child with a chromosomal abnormality or birth defect, we often recommend that they undergo genetic counseling to understand their options.
Questions about Prenatal Testing and Screening?
The physicians and nurses at WOMEN’S HEALTH of Central Massachusetts are here to provide answers. Simply contact us.
Our LocationsWEBSTER LAKE
325 Thompson Road
Webster, MA 01570
508-755-4861
Mon-Fri 8:30-5:00
View Location Details
MARLBOROUGH
340 Maple Street, Suite 125
Marlborough, MA 01752
508-755-4861
Mon-Fri 8:30-5:00
View Location Details
WORCESTER
328 Shrewsbury Street, Suite 100
Worcester, MA 01604
508-755-4861
Mon-Fri 8:30-5:00
View Location Details
STURBRIDGE
118 Main Street, Suite 1
Sturbridge, MA 01566
508-755-4861
Mon-Fri 8:30-5:00
View Location Details
Connect With UsUnderstanding Chorionic Villus Testing (CVS)
Now that you're pregnant, you have many plans. Part of that is the prenatal care you'll need.
Part of that is the prenatal care you'll need.
Depending on your age, health, and other factors, your doctor may recommend routine and individual prenatal tests to monitor the health of your growing baby.
The two main categories of tests you can have during pregnancy are screening and diagnosis. Screening tests are more general and help the doctor determine the health of your baby in the womb.
If your doctor suspects that a developing fetus may have a health problem, they may recommend special diagnostic tests to confirm screening test results.
The Chorionic Villus Sample (CVS) is an example of a diagnostic test that checks for certain genetic conditions in a fetus.
Chorionic villus sampling (CVS) is a prenatal diagnostic test that checks genetic or chromosomal status during the first trimester of pregnancy.
Doctors use this test to examine cells in the lining of the placenta to determine the health of the baby.
CVS will check the conditions such as:
- cystic fibrosis
- Down Syndrome (Trisomia 21)
- Duchenne Muscular Distrophy
- Edwards syndrome (Trisomy)
- Patau Syndrome (Trisomiya 13) 900
- Phoenilketoneuria (FCU) sickle cell anemia
- Tay-Sachs disease
- thalassemia
The CVS test is completely optional.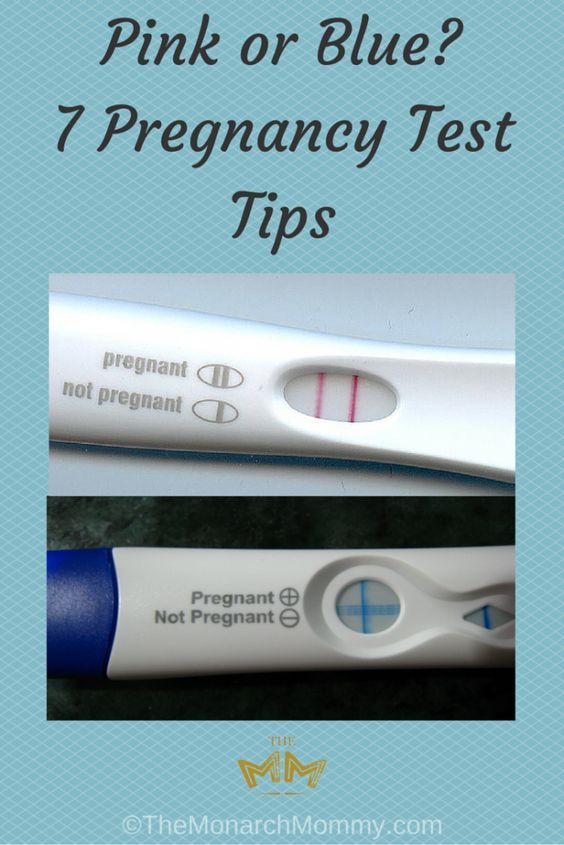 You can reject it. Parents may choose not to have additional testing for many reasons, from religious beliefs to feeling more comfortable with unexpected pregnancy outcomes.
You can reject it. Parents may choose not to have additional testing for many reasons, from religious beliefs to feeling more comfortable with unexpected pregnancy outcomes.
CVS is not a test offered to everyone during pregnancy. This may be done if, based on the results of other screening tests, the child is thought to be at risk for a genetic disorder.
If you are pregnant, your doctor may recommend CVS if you have a family history of certain genetic conditions or if a first trimester screening test shows results that may indicate a genetic disorder.
Before recommending a CVS test, a doctor will usually check for certain risk factors, such as:
- abnormal screening blood test results
- abnormal follow-up ultrasound
- family history of a genetic disease
- medical history of your other children
- high-risk pregnancy from other causes
- mother's oldest age at the time of pregnancy (35 years or older)
HEALTH FACT SHEET
during pregnancy
Parenthood helps you take care of yourself with the support and advice you'll find in our weekly newsletter.
I am expecting
I am a new parent
One of the main advantages of CVS is that it can be performed earlier in pregnancy, between 10 and 13 weeks.
The results of the CVS can be used to decide whether to continue the pregnancy in the first trimester. If the fetus has a genetic or chromosomal problem, it can lead to other diseases or complications.
Another benefit of determining if a baby has a certain genetic disorder is the ability to plan for any medical needs these conditions may cause during and after birth.
You can also learn more about any medical condition your child has and start looking for resources such as support groups and other healthcare providers that your child may need.
During the CVS test, several cells in the placenta's inner lining, called chorionic villi, are removed, carefully examined, and tested.
During an amniocentesis, another type of diagnostic test, a small sample of amniotic fluid—the fluid that surrounds a growing fetus—is taken and then examined.
Amniocentesis checks the fetal cells found in the amniotic fluid and the levels of certain proteins to check for certain genetic changes.
If you choose to have a CVS test, it can be done earlier in your pregnancy than amniocentesis, which is usually done a few weeks later, at about 15 weeks.
Unlike the CVS test, amniocentesis can be used to test for other conditions, including spina bifida, brain and spinal cord conditions.
Nothing needs to be done to prepare for CVS. You can eat and drink as usual. You won't be sedated during the test, so you can drive to and from the doctor's office on your own.
Ask your doctor about what to expect during and after the test. Also discuss other diagnostic options for the CVS test.
Your doctor will likely refer you to a genetic counselor who can provide detailed information about genetic disorders that may run in certain families or occur on their own.
The CVS test is done early in pregnancy, usually between 10 and 13 weeks.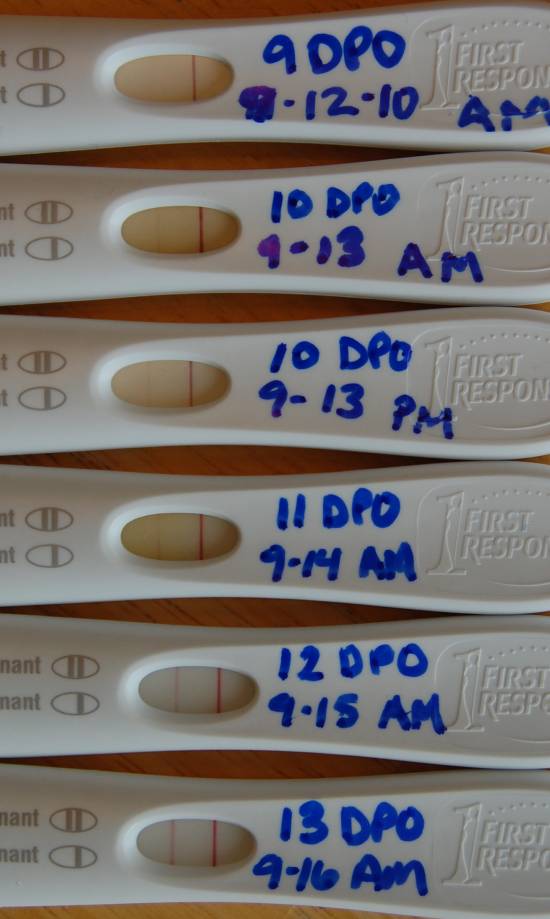 During this small procedure, your doctor safely removes a tiny sample of cells from the placenta using one of two methods:
During this small procedure, your doctor safely removes a tiny sample of cells from the placenta using one of two methods:
- Transabdominal CVS: A sample of the placenta is taken by inserting a needle through the abdomen into the uterus and placenta.
- Transcervical CVS: A sample of the placenta is taken by inserting a thin tube through the cervix into the placenta.
The method used to obtain the sample will depend on several factors such as the location of the placenta and your body weight.
The most common method is transabdominal CVS. Both methods are very fast and the procedure is usually painless. You may feel mild discomfort and cramping after the test.
CVS test results will only take a week or two. If a rarer condition is present, testing may take longer. In most cases, CVS test results are considered accurate by almost 99% .
Call your doctor right away if you experience any unusual side effects such as:
- bleeding
- fever
- fluid leakage
- contractions
There are several rare but serious side effects caused by CVS.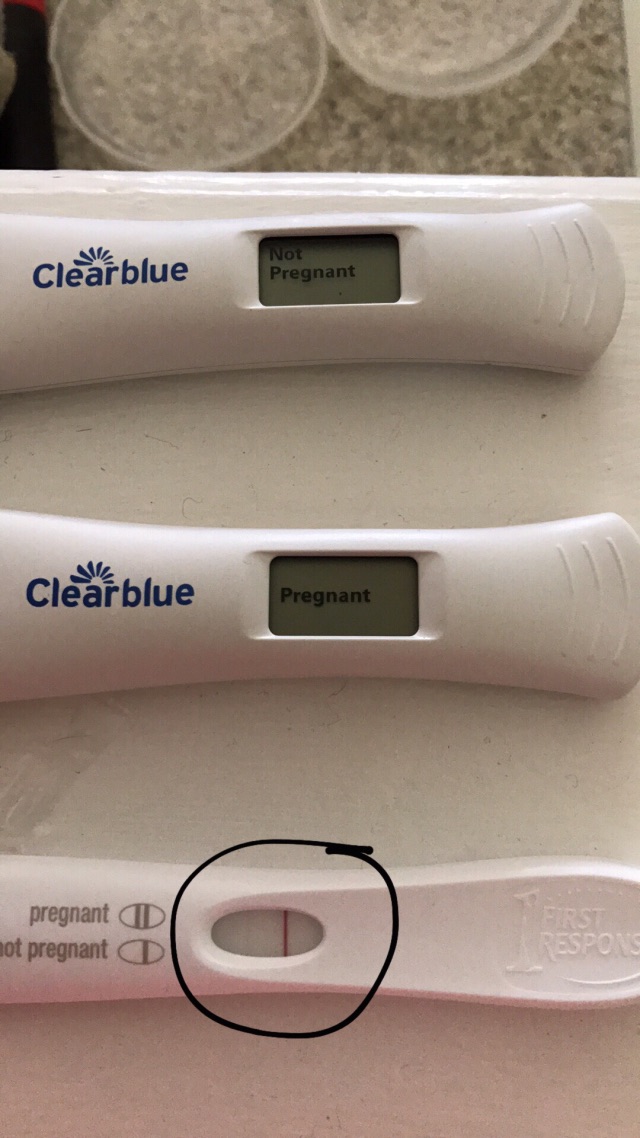
Your doctor will tell you about side effects you may experience. You and your partner can ask them any questions to decide if you want to proceed with the procedure.
Main risks of this procedure:
- miscarriage
- infectious disease
- Rh sensitization
- repeat the procedure and check if the sample is too small
In some cases, it may be necessary to retest if the results are uncertain.
Roughly 1% Reliable source of pregnant people who complete this test may have a miscarriage. This risk is more common with a transcervical procedure.
Your CVS test results can tell if your baby will be born with certain medical conditions.
It is important to note that CVS can only be used to detect certain conditions. In the future, you may need additional blood tests to check for other conditions, including neural tube changes.
Pregnancy can be an exciting and uncertain journey for any parent. Prenatal testing is designed to help you have a healthy and informed pregnancy. Tests such as CVS can help diagnose some genetic changes before the baby is born.
Tests such as CVS can help diagnose some genetic changes before the baby is born.
It is important to have an open dialogue with your doctor about any problems you have. Remember that the CVS test is an option for you. You can refuse the test if you are concerned about the procedure.
Explanation of the results of 1 pregnancy screening
Combined prenatal screening is carried out at 11-14 weeks of gestation with an embryo size of at least 45 mm and not more than 84 mm. This is a comprehensive examination of the fetus to assess the parameters of its development. Its main task is the early detection of fetal malformations, the prevention of childhood disability, and the reduction of infant and child mortality.
The first screening consists of an instrumental part - an ultrasound scan and a laboratory one - a blood test to determine the concentration of chorionic gonadotropin (βhCG) and pregnancy-associated protein A (PAPP-A). The cumulative results of these indicators allow you to plan the tactics of pregnancy management.
Why is the examination carried out at 11-14 weeks
The first trimester is the period of formation of all organs and structures of the body. By the end of the first trimester, the embryonic period ends and the fetal period of fetal development begins. It is in the period from 11 weeks 1 day to 13 weeks 6 days of pregnancy that echographic markers of chromosomal abnormalities are best visualized.
Who needs to be tested
According to the results of the study, it is possible to judge the risk of giving birth to children with chromosomal diseases and congenital malformations, therefore it is recommended to carefully consider the issue and examine all pregnant women. Indications for mandatory prenatal screening of the first trimester are:
- Women with a history of spontaneous abortions, ectopic and missed pregnancies, premature births, stillbirths, the birth of a child with developmental anomalies.
- Hereditary diseases in the family of the mother or father of the child
- First trimester illness treated with antibiotics or drugs contraindicated during pregnancy.
- Marriage between relatives.
- Woman over 35 years of age.
- Presence of occupational hazards
How to prepare
Preparation for the first screening is expressed in a sparing diet. Nutritional errors can affect the general condition of a woman and reduce the accuracy of the results. One week before the examination:
- Salty, spicy, fatty, fried foods should be excluded from the diet.
- Do not eat allergenic foods.
- Avoid carbonated drinks.
One day before screening:
- Do not eat chocolate, seafood, fatty meat, flour, limit sweets.
- If the study is scheduled for the morning, eat a light dinner no later than 20:00 hours.
It is advisable to observe moderate physical activity, if there are no contraindications for this. Walking and proper rest are also important.
Survey
A blood test and ultrasound are performed on the same day to avoid errors due to time differences.
- Ultrasound screening is performed first, as its results allow you to determine the exact gestational age, which affects the normative values of hormone levels. The study is carried out both transabdominally and transvaginally. The procedure is painless, safe for women and children, has no contraindications.
- Blood is taken from a vein on an empty stomach or 4 hours after a meal. The material is taken on the day of the ultrasound. The study determines the concentration of hormones and compares with standard indicators.
Only by deciphering the results of ultrasound and hormone analysis, a conclusion is made about possible risks.
What ultrasound shows
At screening during pregnancy, fetometry of the fetus is performed - determination of the size of body parts and all anatomical structures are evaluated.
The results obtained are compared with a statistical table, which indicates the percentile of falling into the sample of standard values. With indicators less than 5 and more than 95, additional examinations are prescribed.
With indicators less than 5 and more than 95, additional examinations are prescribed.
During an ultrasound examination in the 1st trimester, the following parameters are evaluated: the bones of the cranial vault and the brain, the spine, the anterior abdominal wall, the limbs of the fetus, the structures of the face, the organs of the chest and abdominal cavity, as well as the main echographic markers of chromosomal abnormalities.
Collar space thickness (TVP)
The area between the inner surface of the skin of the fetus and the outer surface of the soft tissues covering the cervical spine. TVP is considered the most important marker of chromosomal abnormalities.
This space begins to decrease after 13 weeks, so it can only be assessed at the first screening.
| Gestational age | Collar thickness in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 0. 8 8 | 1.6 | 2.4 | |
| 12 weeks | 0.7 | 1.6 | 2.5 | |
| 13 weeks | 0.7 | 1.7 | 2.7 | |
The discrepancy between the results and the normative values indicates an increased risk of developing chromosomal pathologies. Depending on the formed set of chromosomes, it can be Down syndrome, Patau, Edwards, Shereshevsky-Turner. To clarify the diagnosis in this case, a biopsy of the chorion or placenta, an analysis of cord blood, and amniotic fluid may be prescribed. Only after additional research can an accurate diagnosis be made.
Only after additional research can an accurate diagnosis be made.
Coccyx-parietal size (KTR)
Shows the distance between the coccygeal and parietal bones. According to this parameter, the exact gestational age is determined on ultrasound, and the ratio of the mass of the fetus to its CTE is also established.
A slight deviation from the norm indicates the features of the physique and is not a cause for concern.
| Gestational age | Coccyx-parietal size in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 34 | 42 | fifty | |
| 12 weeks | 42 | 51 | 59 | |
| 13 weeks | 51 | 63 | 75 | |
If screening during pregnancy showed results that exceed the norm, this indicates that the fetus is quite large. The indicator says much less either about an incorrectly determined gestational age (in this case, a re-examination is carried out after 1-1.5 weeks), or about a slowdown in development due to intrauterine death, impaired hormonal levels or an infectious disease of the mother, genetic abnormalities.
The indicator says much less either about an incorrectly determined gestational age (in this case, a re-examination is carried out after 1-1.5 weeks), or about a slowdown in development due to intrauterine death, impaired hormonal levels or an infectious disease of the mother, genetic abnormalities.
Skull bones and brain
Already from the 11th week, ultrasound examination can detect defects in the bones of the skull, which indicates severe fetal malformations that are incompatible with life. The evaluation of the brain is based on the study of the so-called "butterfly" - the choroid plexus of the lateral ventricles. A clear visualization and its symmetry indicates the normal development of the brain.
| Gestational age | BPR, LZR in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 13.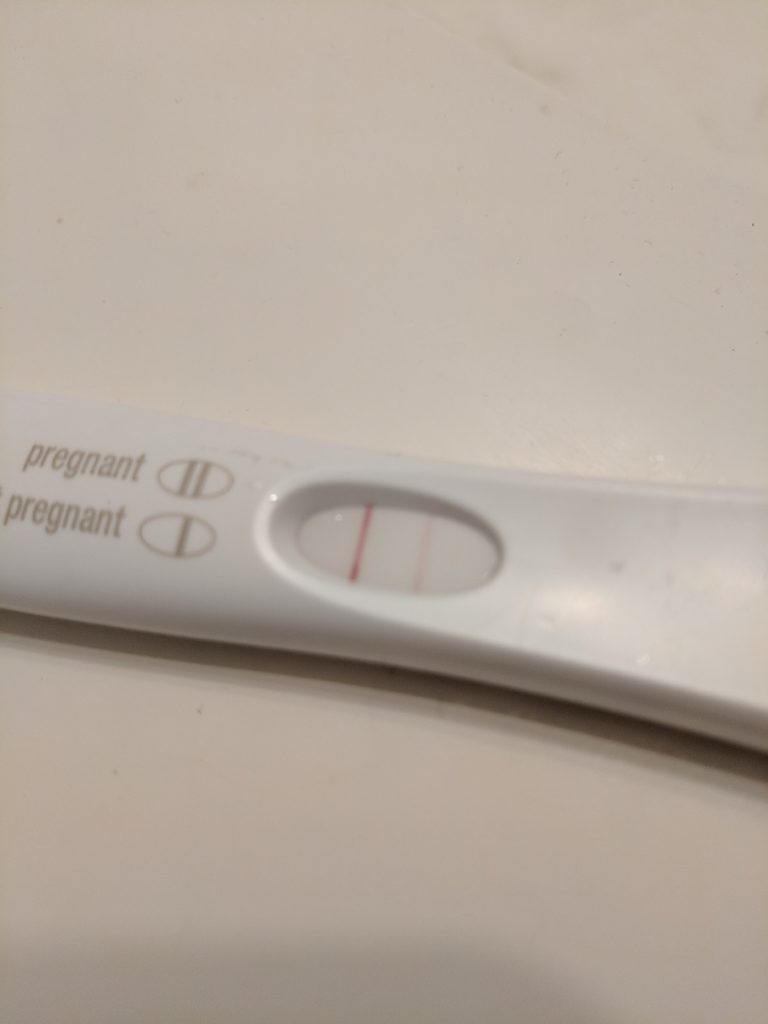 19 19 | 17.21 | 21.23 | |
| 12 weeks | 19.22 | 21.24 | 24.26 | |
| 13 weeks | 20.26 | 24.29 | 28.32 | |
Nasal bone
By the end of the trimester, it should be formed, clearly visualized.
| Gestational age | Nasal bone in mm | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | visualized, not measured | visualized, not measured | visualized, not measured | |
| 12 weeks | 2 | 3. 1 1 | 4.2 | |
| 13 weeks | 2 | 3.1 | 4.2 | |
The pathology of the nasal bone is its absence, hypoplasia (very small size) and a change in its echogenicity.
The diameter of the chest, the circumference of the head and abdomen, the length of the femur also make it possible to judge the proportionality of development.
Heart condition
When examining the heart, its location is assessed, the presence of four chambers of the heart is established - two atria and two ventricles, and their symmetry is assessed. The heart rate is measured.
| Gestational age | Heart rate in beats per minute | |||
| Percentile 5 | 50 percentile | 95 percentile | ||
| 11 weeks | 153 | 165 | 177 | |
| 12 weeks | 150 | 162 | 174 | |
| 13 weeks | 147 | 159 | 171 | |
The venous duct (VP) is a direct communication between the umbilical vein and the central venous system. In a normally developing pregnancy, the blood flow in the EP is a three-phase curve. The appearance of reverse blood flow may indicate the presence of fetal pathology.
In a normally developing pregnancy, the blood flow in the EP is a three-phase curve. The appearance of reverse blood flow may indicate the presence of fetal pathology.
What a blood test shows
Ultrasound results are compared with maternal plasma pregnancy-associated protein A (PAPP-A) and human chorionic gonadotropin (hCG). The values are given in the table:
| Gestational age | hCG in ng/ml | PAPP-A in mU/l |
| 11 weeks | 17.4 - 130.4 | 0.46 - 3.73 |
| 12 weeks | 13.4 - 128.5 | 0.79 - 4.76 |
| 13 weeks | 14.2 - 114.7 | 1.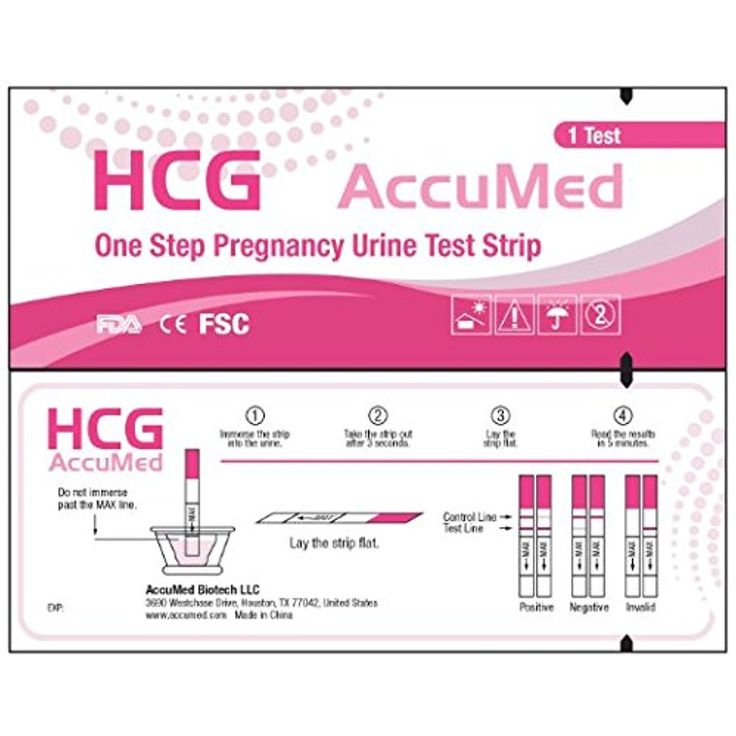 03 - 6.01 03 - 6.01 |
Differences from the reference values \u200b\u200bmay indicate pathologies of the mother or fetus.
| Deviation | hCG | PAPP-A |
| Above normal |
|
|
| Below normal |
|
|
Survey interpretation
The first study is evaluated only by the totality of all indicators. A single parameter cannot be the basis for an accurate conclusion. The protocol records ultrasound data, hormone analysis, the risks of probable diseases and the complex median coefficient MoM. It indicates the cumulative deviation of the obtained results from the average values. The coefficient must be in the range from 0.5 to 2.5. It is calculated by specialized programs.
What can affect the result
- Incorrect preparation, peculiarities of the woman's condition.
- Obsolete equipment with poor measurement accuracy and insufficient resolution.
- Qualification of the doctor of the ultrasound room, errors in decoding.
- Correctness of MoM calculation algorithms.
Modern diagnostic equipment makes it possible to evaluate more than 15 fetal parameters, build its volumetric reconstruction for examining organs in the early stages of development, and calculate possible risks with high accuracy.