Pcos morning sickness
Severe Morning Sickness - What is Hyperemisis Gravidarum?
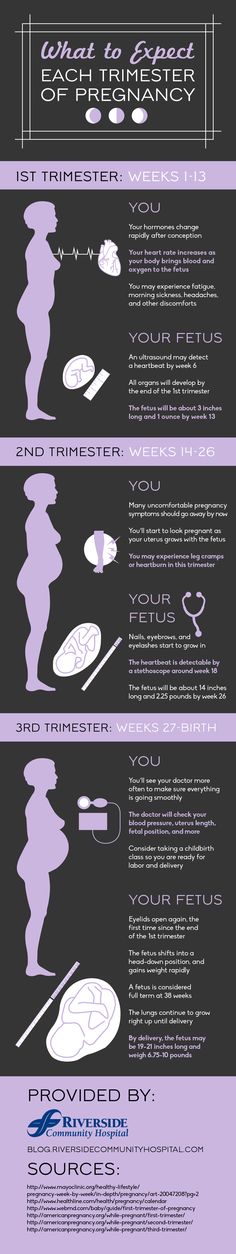
Some nausea and vomiting during the earlier stages of pregnancy is common. The discomfort is caused by levels of pregnancy hormones, specifically hCG, (human chorionic gonadotropin, the hormone responsible for helping to build your baby’s placenta) and estrogen in a woman’s body. Both of these increase rapidly during pregnacy. Hyperemisis Gravidarum is known as severe morning sickness. It is nausea and vomiting that goes beyond what is considered a normal level.
It might be Hyperemisis Gravidarum if:
- You are vomiting multiple times per day
- Food or liquid comes back up
- You feel lightheaded
- You show signs of dehydration (not urinating, dark yellow urine)
- You’re losing weight
- You see blood in the vomit
- You have low blood pressure or a high pulse rate
Hyperemisis Gravidarum occurs in less than one in 200 pregnancies. For those women, severe and continuous nausea and vomiting that becomes debilitating because it interferes with a woman’s ability to eat, drink, sleep, and work. Like most medical conditions, its Latin name describes what it is: The term comes from the Greek hyper-, meaning excessive, and emesis, meaning vomiting. Gravidarum means “pregnant woman.” The grav- part of the word means “heavy,” as in the English word “gravity.”
Severe cases can lead to extreme weight loss, malnutrition in both the mom and baby, and dehydration. Since the baby is affected by the mother’s inability to eat, hospitalization may be needed.
When does Hyperemisis Gravidarum start?
Severe morning sickness usually starts in the first trimester at around week 4 or 5 of pregnancy. Typical morning sickness usually starts around week 6. Hyperemisis Gravidarum can sometimes clear up on its own between weeks 12 and 20. In some cases, though, it can continue throughout a pregnancy.
Severe morning sickness seems to be most common in first-time mothers, very young mothers, and mothers carrying multiple babies. If a woman has had Hyperemisis Gravidarum with a previous pregnancy, she is more likely to have it with subsequent pregnancies. Also, women whose mothers had severe morning sickness are also more likely to have it themselves.
Also, women whose mothers had severe morning sickness are also more likely to have it themselves.
How can you avoid severe morning sickness?
Although it’s a mystery why some women get this and others don’t, there are some things that research tells us contributes to severe morning sickness. Severe emotional stress can be a factor. If you are experiencing an extremely stressful life situation, let your doctor know. Your doctor will be able to make suggestions on how to deal with or possibly improve the situation to remove the stress.
Hormonal imbalances or diseases that cause hormonal imbalance, such as polycystic ovarian syndrome, can increase your risk of severe morning sickness. Vitamin deficiencies or a bacterial stomach infection can also play a role. Looking at a woman’s overall physical and mental health is an important part of diagnosing and treating Hyperemisis Gravidarum.
How can you treat Hyperemisis Gravidarum?
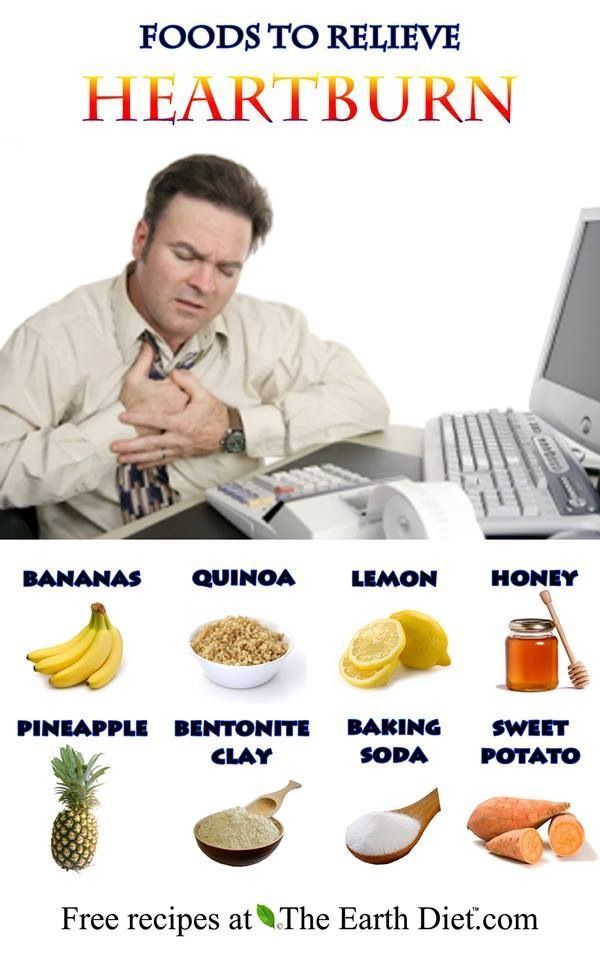
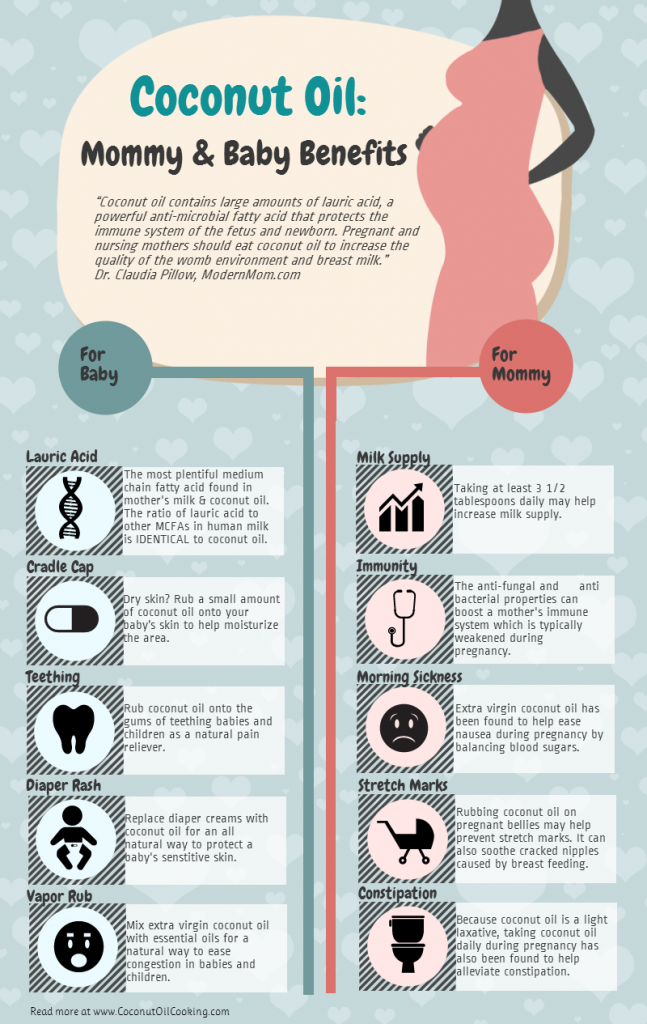
Try traditional treatments for nausea first. This may include eating ginger or drinking ginger tea. Any foods or drinks that are disagreeable to you (make you feel sick) should be avoided. Although with Hyperemisis Gravidarum it can seem like everything makes you feel sick! Drink fluids regularly to avoid becoming dehydrated. There are some prescription medications for anti-nausea that you and your doctor can talk about.
This may include eating ginger or drinking ginger tea. Any foods or drinks that are disagreeable to you (make you feel sick) should be avoided. Although with Hyperemisis Gravidarum it can seem like everything makes you feel sick! Drink fluids regularly to avoid becoming dehydrated. There are some prescription medications for anti-nausea that you and your doctor can talk about.
Polycystic Ovarian Syndrome (PCOS) and Pregnancy: Symptoms
Polycystic Ovarian Syndrome (PCOS) and Pregnancy: SymptomsMedically reviewed by Suzanne Falck, M.D., FACP — By Chaunie Brusie on November 1, 2016
Polycystic ovarian syndrome (PCOS) is a condition that affects between 6 and 15 percent of women of childbearing age. If you’re diagnosed with PCOS, it may be more difficult to become pregnant. And if you’re able to become pregnant, you’re at risk for more complications during pregnancy, labor, and delivery.
Women with PCOS are three times more likely to have a miscarriage, as compared to women who don’t have PCOS. They are also more likely to develop preeclampsia, gestational diabetes, and have a larger baby and premature delivery. This could lead to difficulty during delivery or a cesarean delivery.
They are also more likely to develop preeclampsia, gestational diabetes, and have a larger baby and premature delivery. This could lead to difficulty during delivery or a cesarean delivery.
Risks for moms-to-be with PCOS
Having PCOS might make it harder for you to get pregnant. Hormonal imbalances might be to blame.
Women with PCOS are more likely to be obese and to rely on reproductive technology to get pregnant. One study found that 60 percent of women with PCOS are obese. Almost 14 percent required reproductive technology to get pregnant.
Women with PCOS have an increased risk of developing several medical complications throughout life, including:
- insulin resistance
- type 2 diabetes
- high cholesterol
- high blood pressure
- heart disease
- stroke
- sleep apnea
- possibly an increased risk of endometrial cancer
For pregnant women, PCOS brings an increased risk of complications. This includes preeclampsia, a dangerous condition for both mother and baby-to-be. The recommended treatment to resolve symptoms is delivery of the baby and placenta. Your doctor will discuss the risks and benefits regarding timing of delivery based on the severity of your symptoms and your baby’s gestational age. If you develop preeclampsia during your pregnancy, you will have to be monitored extremely closely. Other concerns include pregnancy-induced hypertension (high blood pressure) and gestational diabetes.
The recommended treatment to resolve symptoms is delivery of the baby and placenta. Your doctor will discuss the risks and benefits regarding timing of delivery based on the severity of your symptoms and your baby’s gestational age. If you develop preeclampsia during your pregnancy, you will have to be monitored extremely closely. Other concerns include pregnancy-induced hypertension (high blood pressure) and gestational diabetes.
Having gestational diabetes could lead to you having a larger-than-average baby. This could lead to problems during delivery. For example, larger babies are more at risk for shoulder dystocia (when the baby’s shoulder gets stuck during labor).
Most PCOS symptoms during pregnancy can be treated with careful monitoring. If you develop gestational diabetes, insulin may be required to keep your blood sugar levels stable.
Risks for baby
Unfortunately, having PCOS during pregnancy makes things a little more complicated. It will require more monitoring for both you and your baby.
The potential risks with PCOS for the baby include:
- premature birth
- large for gestational age
- imiscarriage
- lower Apgar score
If your baby is a girl, some studies have shown that there is up to a 50 percent chance that she will also have PCOS.
Women with PCOS are also more likely to deliver by cesarean because they tend to have larger-sized babies. Other complications may also come up during labor and delivery.
Getting pregnant with PCOS
Some women may not realize they have PCOS until they try to conceive. PCOS often goes unnoticed. But if you’ve been trying to conceive naturally for over a year, you should speak to your doctor about getting tested.
Your doctor can help you develop a plan for getting pregnant. Some strategies, such as losing weight, healthy eating, and in certain cases, medications, can increase your chances for getting pregnant.
PCOS and breast-feeding
If you’re diagnosed with PCOS, you may need to continue to manage symptoms even after pregnancy. But symptoms and severity can vary. Sometimes the hormonal fluctuations after pregnancy and breast-feeding can change the symptoms, so it may be awhile before you settle into your new “normal.”
But symptoms and severity can vary. Sometimes the hormonal fluctuations after pregnancy and breast-feeding can change the symptoms, so it may be awhile before you settle into your new “normal.”
It’s safe to breast-feed with PCOS, even if you’re on insulin medication to help control your blood sugar. Women who have gestational diabetes are at risk for developing type 2 diabetes later in life, but breast-feeding can help lower that risk.
Breast-feeding has many benefits for both you and your baby, so if it fits your family, be sure to explore the options and available resources so you can have a successful breast-feeding experience.
What is PCOS?
PCOS, also known as Stein-Leventhal syndrome, is a hormonal imbalance that affects women. It’s characterized by the production of too many androgens, or “male” hormones.
PCOS can cause women to develop excessive hair and acne. It can also cause cysts on the ovaries and interrupt normal menstrual cycles.
It’s a tricky condition because there’s not one single test to diagnose it. Instead, doctors look at the clues of what’s going on in your body. Excessive hair growth or irregular periods might be signs. Doctors can then piece together a picture of PCOS.
Instead, doctors look at the clues of what’s going on in your body. Excessive hair growth or irregular periods might be signs. Doctors can then piece together a picture of PCOS.
PCOS symptoms
PCOS often gets missed in women because of the difficulty of making a diagnosis. The symptoms can vary and occur in many different types of women.
Obesity or weight gain, for example, can be a frequent occurrence with PCOS. But it’s not a given. Many women with PCOS have lean body shapes.
Unfortunately, up to 50 percent of women who have PCOS never actually get diagnosed. Because of this, PCOS is sometimes called the silent killer.
Some of the more common symptoms of PCOS include:
- “string of pearl” cysts on the ovaries
- insulin resistance
- high testosterone causing excessive hair growth, male pattern baldness, and acne
- suppressed ovulation
- excessive weight gain
- weight gain on the waistline
- dark, thick patches of skin on the neck, arms, breasts, or thighs
- skin tags in the armpits or neck area
- pelvic pain
- anxiety or depression
- sleep apnea
Treatment
There’s currently no cure for PCOS. But it’s possible to manage symptoms.
But it’s possible to manage symptoms.
Options to help manage symptoms include:
- birth control pills
- weight loss
- spironolactone
- other androgen blockers
Along with other fertility drugs, metformin, which helps to control blood sugar, is commonly prescribed to help induce ovulation.
Note: You’ll need to stop taking some of these medications if you become pregnant. Work with your doctor to develop a plan that fits your needs.
Next steps
The most important thing to know about PCOS and pregnancy is that complications are very real. That’s why it’s more important than ever to take steps to have a healthy pregnancy.
Talk to your doctor, follow a pregnancy-safe exercise and diet program, and take medication as directed. These are all recommended regimens for controlling PCOS during pregnancy.
Share on Pinterest
Last medically reviewed on November 2, 2016
- Parenthood
- Pregnancy
- Pregnancy Complications
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations.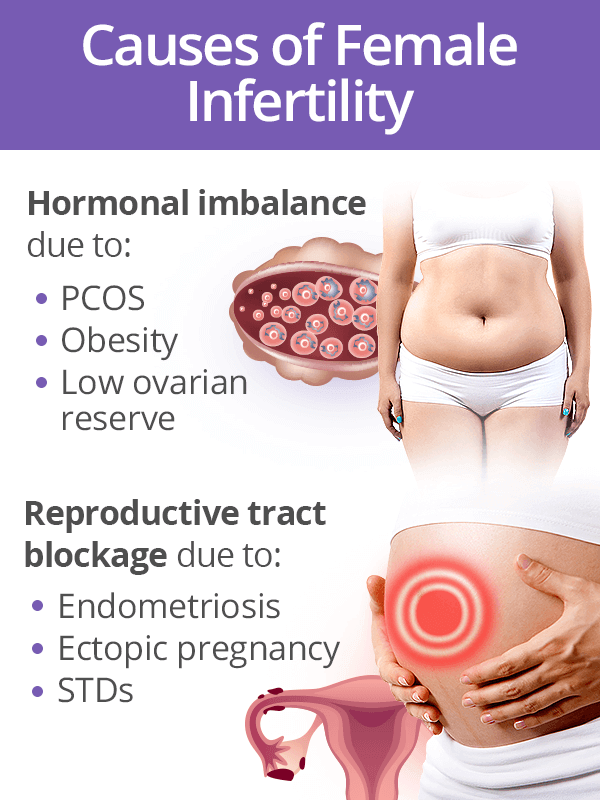 We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Does PCOS affect pregnancy? (2013, May)
nichd.nih.gov/health/topics/PCOS/conditioninfo/Pages/pregnancy.aspx - Mayo Clinic Staff. (2014, September 3). Polycystic ovary syndrome (PCOS)
mayoclinic.org/diseases-conditions/pcos/basics/treatment/con-20028841 - PCOS pregnancy and delivery complications. (2016)
pcosaa.org/pcos-pregnancy-and-delivery-complications - Polycystic ovary syndrome (PCOS) fact sheet. (2014, December)
- Roos, N. (2011, October 13).Risk of adverse pregnancy outcomes in women with polycystic ovary syndrome: population based cohort study. British Medical Journal, 343. Retrieved from
bmj.com/content/343/bmj.d6309 - Trikudanathan, S. (2015, January). Polycystic ovarian syndrome. Medical Clinics of North America, 99(1), 221–235
ncbi.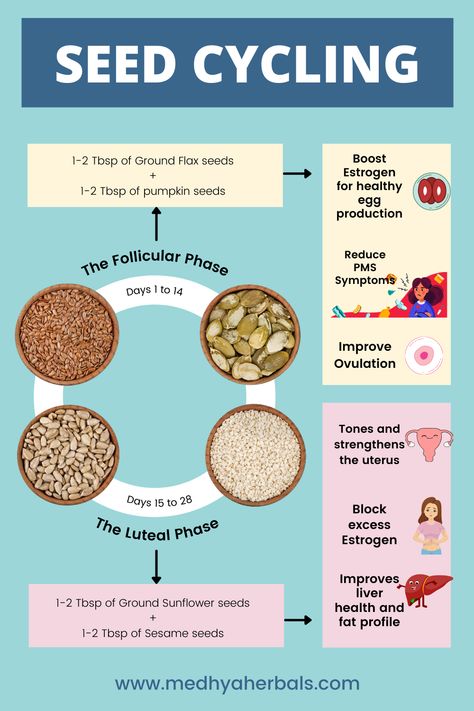 nlm.nih.gov/pubmed/25456652
nlm.nih.gov/pubmed/25456652 - What is polycystic ovary syndrome? (2015)
pcosfoundation.org/what-is-pcos
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Nov 2, 2016
Written By
Chaunie Brusie
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Suzanne Falck, MD
Share this article
Medically reviewed by Suzanne Falck, M.D., FACP — By Chaunie Brusie on November 1, 2016
related stories
Polycystic Ovary Syndrome (PCOS): Symptoms, Causes, and Treatment
Taking a Pregnancy Test When You Have PCOS: What to Know
PCOS and Anxiety Can Often Show Up Together. Here’s Why
What You Need to Know About Doing Pilates During Pregnancy
Can Ectopic Pregnancy Be Diagnosed With Ultrasound?
Read this next
Polycystic Ovary Syndrome (PCOS): Symptoms, Causes, and Treatment
Medically reviewed by Amanda Kallen, MD
Many women with polycystic ovarian syndrome are unaware they have it.
 Learn more about symptoms, treatment, and tips to help keep your ovaries healthy.
Learn more about symptoms, treatment, and tips to help keep your ovaries healthy.READ MORE
Taking a Pregnancy Test When You Have PCOS: What to Know
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Can PCOS make pregnancy testing problematic? We'll give you all the details, from when to test to why you may get a false result.
READ MORE
PCOS and Anxiety Can Often Show Up Together. Here’s Why
Medically reviewed by Marney A. White, PhD, MS
Polycystic ovary syndrome (PCOS) and anxiety can often appear together. Hear one woman's story about how she learned to manage her anxiety while…
READ MORE
What You Need to Know About Doing Pilates During Pregnancy
Medically reviewed by Amy Elizabeth Wolkin, PT, DPT, MBA
Pilates during pregnancy can be very beneficial to both parent and baby if you keep a few considerations in mind! Here's all you need to know about…
READ MORE
Can Ectopic Pregnancy Be Diagnosed With Ultrasound?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Ectopic pregnancy is a serious condition that requires accurate and swift diagnosis.
 Ultrasound for ectopic pregnancy diagnosis is just one tool your…
Ultrasound for ectopic pregnancy diagnosis is just one tool your…READ MORE
Is It Safe to Consume Flaxseeds During Pregnancy?
Given the inconclusive and conflicting stances about eating flaxseeds during pregnancy, it might be better to err on the side of caution.
READ MORE
Pregnancy After Miscarriage: Answers to Your Questions
Medically reviewed by Amanda Kallen, MD
Getting pregnant after a miscarriage can be an emotional experience, filled with joy but also anxiety and guilt. Learn more about pregnancy after…
READ MORE
What Is a Nurse Midwife and How to Tell If They Are Right for You
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
A nurse midwife is a nurse with education, training, and certification to provide prenatal, delivery, and women's care.

READ MORE
Your 6-Week Ultrasound: What to Expect
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
We'll tell you all about the 6-week ultrasound, including why your doctor may have ordered it, what the risks are, and what it means if no heartbeat…
READ MORE
Does Swaddling Increase the Risk of SIDS?
Medically reviewed by Mia Armstrong, MD
Is swaddling safe, or is it a risk factor for SIDS? Here's what the most recent research says.
READ MORE
Nausea in pregnancy - Reprolife Kyiv
What can we advise you?Page Contents
Many pregnant women perceive morning sickness as an inevitable fact: it is the body's reaction to important processes occurring in it during the first months of pregnancy. The only thing they can do in such a situation is to wait patiently for it to expire. Well, this common belief is not entirely true, since toxicosis requires significant medical attention.
The only thing they can do in such a situation is to wait patiently for it to expire. Well, this common belief is not entirely true, since toxicosis requires significant medical attention.
What are the causes of toxicosis in the first trimester?
There is no single, scientifically proven opinion about the causes of toxicosis: is it a reaction of the immune system or this condition can be caused by hormones, namely, a high concentration of the hormone hCG, estradiol, progesterone in the blood. Moreover, all causes of toxicosis in early pregnancy are due to natural causes. The most proven factor is the reaction to the growth of progesterone in the body. Progesterone is known to be very important for relaxing the uterus and protecting the baby. But in some women, in addition to the uterus, progesterone reacts to excessive relaxation and the gallbladder. As a result of this, its complete reduction does not occur, stagnation and nausea occur. That is why it is very important to avoid fried and fatty foods in early pregnancy. Which causes stress on the gallbladder.
Which causes stress on the gallbladder.
Why do some women have toxicosis, while others do not?
This can be explained by the general condition of the whole organism: chronic diseases of the gastrointestinal tract, liver, gallbladder, pancreas, thyroid gland, bad habits, malnutrition - lasted long before pregnancy. If you have mild nausea in the morning or intermittently during the day and this does not affect your performance, you do not lose weight and feel generally good, then do not worry. Take this condition as a temporary period of successful development of pregnancy and a positive sign that the baby is growing and developing.
Toxicosis can change the baby's excellent waiting period. To alleviate your condition, we have prepared effective and practical advice:
- Diet is a very important factor. However, remember that your meal plan during this period should be well balanced and contain sufficient amounts of proteins, fats and carbohydrates.

- Breakfast in bed. If vomiting usually occurs in the morning, eat breakfast after waking up in bed (light snack - avocado bread or toast, banana, a slice of fatty cheese, sugar-free cookies). After a light breakfast in a semi-sitting position, you should stay in bed for another 20-30 minutes.
- Eat often, but in small portions.
- Chew your food thoroughly and slowly.
- Eat cool and easily digestible foods, avoid hot foods.
- Drink enough water. The volume of daily fluid can be calculated individually: 30-40 ml per kilogram of body weight. Drink often and in small sips, not hot and not too cold.
- Coffee drinkers should avoid daily drinking.
- Exclude spicy, pickled, canned, fatty foods, spices from the daily diet. Limit your consumption of sweets.
- Don't expect to feel hungry. Hunger increases nausea.
- Avoid strong odors, save all perfumes, dispensers, aroma oils for later. Use hypoallergenic products for daily care.
- Ventilate the room at least 4 times a day, spend time outdoors.
- Chew but do not swallow 1 small mint leaf or translucent thin slice - ginger. Thus, we exclude the general effect of these substances on the whole organism in the early period, but their quantity is sufficient to stop the feeling of nausea.
- Avoid exhaustion, both physical and nervous. Sometimes fatigue can provoke nausea - this happens more often in the afternoon. Early toxicosis usually disappears completely after the 12th week of pregnancy, less often it can last up to 16 weeks.
- Pharmaceutical preparations in the composition of B vitamins, ginger extract can only be used as prescribed by a doctor and show a good effect.
Early toxicosis usually completely disappears after 12 weeks of pregnancy, less often it can last up to 16 weeks. Be patient and be attentive to the nuances of your well-being - this is very important not only for your health, but also for the health of the baby.
The absence of toxicosis is also a common condition. Don't worry if you feel great and don't experience nausea in the first trimester of pregnancy.
If toxicosis progresses, combined with repeated vomiting - a thorough medical assessment of the woman's health in the first trimester of pregnancy is required. This is the most important rule, which in no case should be neglected.
Enjoy every day of your curious state!
Category
See also:
ESHRE Reproductive Science Meeting in Milan
11/07/2022
On July 03-06, an important event took place - the ESHRE Reproductive Science Congress in Milan. We actively participated in this conference and want to share the main European trends in the treatment of infertility. We see how many important areas there are that truly inspire us in order to achieve the main goal together with the couple - the birth of healthy children in families!
Is it possible to get pregnant with a diagnosis of PCOS? Part 1
06/23/2022
Polycystic ovary syndrome (PCOS) is indeed one of the most common causes of female endocrine infertility.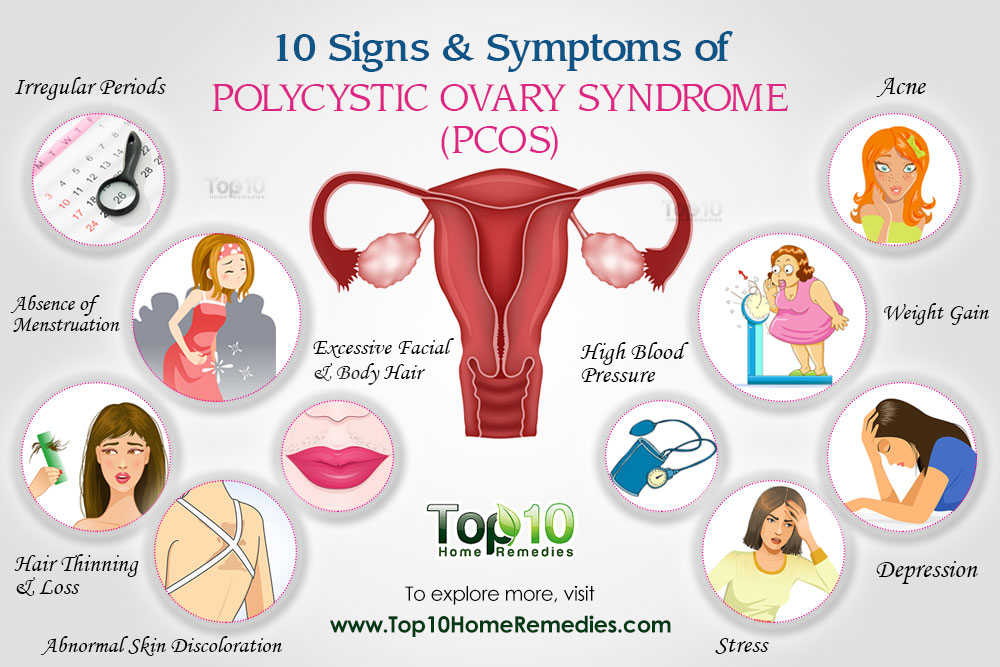 But this absolutely does not mean that there is no chance of having a desired pregnancy at all.
But this absolutely does not mean that there is no chance of having a desired pregnancy at all.
Is it necessary to do DNA analysis of spermatozoa fragmentation?
20/06/2022
The Reprolife Clinic's experienced and competent team recommends only the most necessary tests and studies that have a scientific basis. We are able to lead you to the dream of becoming parents!
Hysteroscopy is an operation without incisions and sutures.
19/06/2022
Hysteroscopy allows you to get rid of uterine causes of infertility, mechanical obstacles to pregnancy, pathological conditions of the endometrium and cervical canal at any age. The Reprolife Clinic has a medical team specialized in endoscopic surgery.
What are the main causes of embryo implantation failure?
06/13/2022
A successful pregnancy depends on a number of events, among which the implantation of the embryo is one of the most important. The success of implantation and pregnancy is influenced by many reasons. Often these reasons can be combined. With faith and the right mindset for the main result, the teamwork of the couple and the reproductologist, such situations as RIF are surmountable.
The success of implantation and pregnancy is influenced by many reasons. Often these reasons can be combined. With faith and the right mindset for the main result, the teamwork of the couple and the reproductologist, such situations as RIF are surmountable.
〚 When will it end? How long does toxicity last? 〛|| Blog BABYSTART
January 26, 2020
You feel like you're on a rocking boat when you drive to work, sit in meetings, take your kids to bed. Will it ever end?
The good news is that this will most likely end - and relatively soon. Here's what to expect.
Morning sickness usually lasts 6 to 12 weeks with a peak of 8 to 10 weeks. According to an oft-cited study from 2000, 50 percent of women have completed this unpleasant phase by 14 weeks of pregnancy, or around the time they enter their second trimester. The same study showed that 90 percent of women are past morning sickness by 22 weeks.
Although these weeks may seem awfully long, it can be a strange consolation that this means the hormones are doing their job and the baby is thriving. In fact, a 2016 study found that women who had at least one prior pregnancy loss and nausea and vomiting during week 8 were 50 percent less likely to have a miscarriage.
In fact, a 2016 study found that women who had at least one prior pregnancy loss and nausea and vomiting during week 8 were 50 percent less likely to have a miscarriage.
However, it should be noted that this was a correlational study and therefore cannot suggest cause and effect. This means that the opposite is not true: the absence of symptoms does not necessarily mean a higher chance of miscarriage.
The same study also found that about 80 percent of these women experienced nausea and/or vomiting during the first trimester. So you are not alone, to put it mildly.
How long does morning sickness last?
If you're in the middle of it, you can probably attest to the fact that morning sickness definitely doesn't just happen in the morning. Some people are sick all day, while others struggle during the day or evening.
The term "morning sickness" comes from the fact that after waking up all night without food, you may wake up worse than usual. But only 1.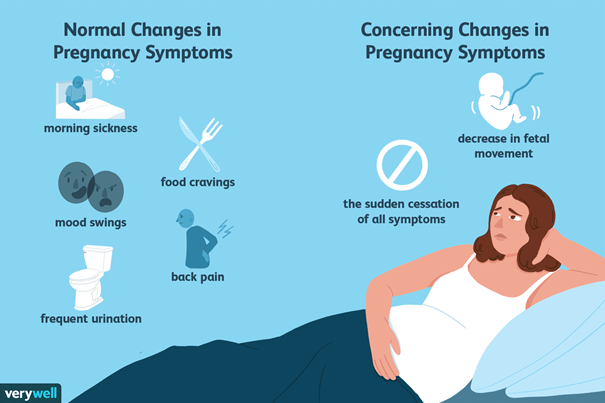 8 percent of pregnant women only get sick in the morning, according to this 2000 study. Some health professionals have begun to name a group of symptoms of NVP, nausea and vomiting during pregnancy.
8 percent of pregnant women only get sick in the morning, according to this 2000 study. Some health professionals have begun to name a group of symptoms of NVP, nausea and vomiting during pregnancy.
If you find yourself in the unfortunate group of people who are nauseated all day, you are not alone - and again the symptoms should disappear after the first trimester.
What if I'm still sick after 14 weeks?
If you have morning sickness during pregnancy for longer than usual, or if you are vomiting severely, call your doctor.
A condition called Hyperemesis gravidarum occurs in 0.5 to 2 percent of pregnancies. This includes severe and persistent vomiting, which can lead to hospitalization for dehydration.
Women experiencing this condition lose more than 5 percent of their body weight, and it is the second most common reason for pregnant women to stay in the hospital. Most of these rare cases resolve before the 20-week mark, but 22 percent of them persist until the end of the pregnancy.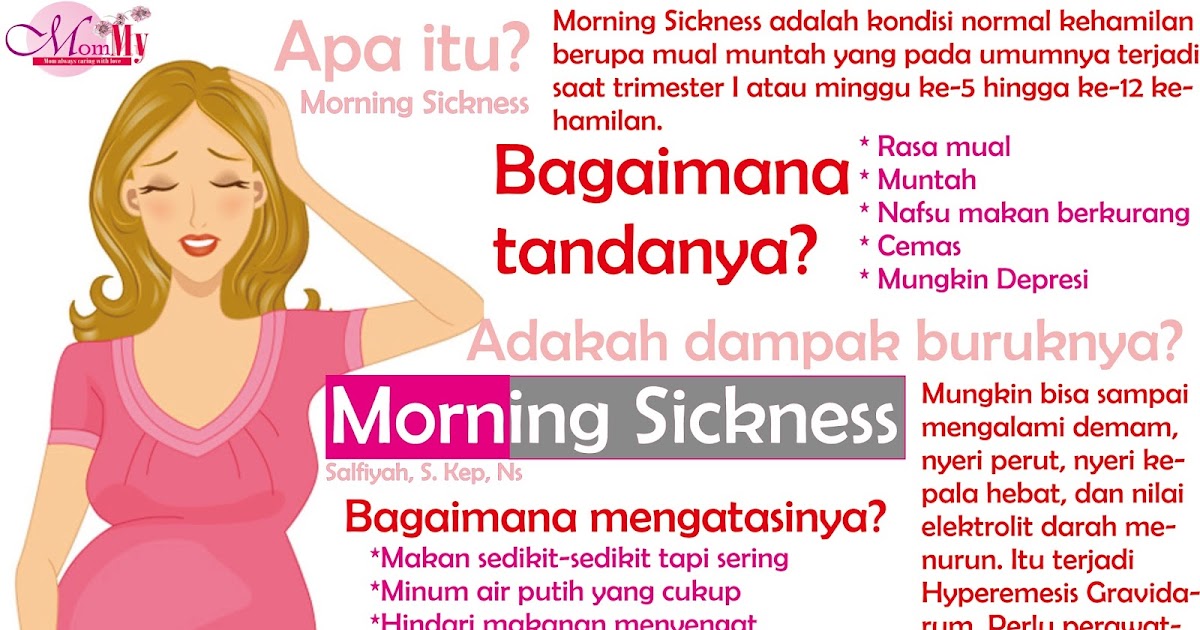
If you have had it once, you have a higher risk of having it in future pregnancies. Other risk factors include:
- family history of the condition
- young age
- pregnancy for the first time
- twins
- be overweight or obese
What causes morning sickness?
Although the cause is not entirely clear, medical professionals believe that morning sickness is a side effect of human chorionic gonadotropin (hCG), commonly referred to as the "pregnancy hormone." When the hormone levels rise, as they do in the healthy first trimester of pregnancy, it is thought to cause nausea and vomiting.
This theory is further supported by the idea that people who have twins often experience more severe morning sickness.
It is also possible that morning sickness (and food aversion) is a way to protect the child's body from potentially harmful bacteria in food. But, in particular, hCG levels peak towards the end of the first trimester, and then levels off - and even decreases. This is further evidence for the hCG theory, which may also be the cause of these food aversions.
This is further evidence for the hCG theory, which may also be the cause of these food aversions.
Who is more susceptible to morning sickness?
Some women experience little to no morning sickness, while others are at increased risk of a more severe condition.
Those who are pregnant with twins or more may have more severe symptoms as their hormone levels are higher than a pregnancy with one child.
It may be helpful to ask female family members, such as your mother or sister, about their experience of nausea and vomiting, as this can run in the family. Other risk factors include:
- History of migraine or motion sickness
- previous pregnancy with severe morning sickness
- be a pregnant girl (but don't use the severity of morning sickness to determine your baby's gender!)
How to Manage Morning Sickness
Ironically, food is one of the most recommended ways to help with morning sickness, no matter what time of day you experience it.