When does placenta attach to uterus
When Does the Placenta Form? All About This Unique Organ
Pregnancy involves some pretty wild changes to your body. Did you know that in addition to growing a human, you’re also growing a whole new organ?
While you’re over here dealing with fatigue, cravings, sore boobs, and nausea, behind the scenes, your body is tirelessly working on two very important things: a baby and a placenta.
It’s true: Even early on, the placenta — an organ that’s made of both fetal and maternal tissue — is growing right alongside your little one.
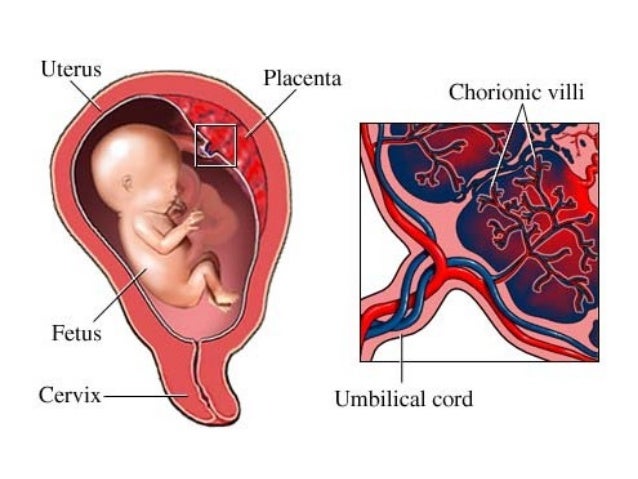
Your body goes through rapid changes during pregnancy — especially in the early months. To support this process, you need a lifeline to help your baby eat and breathe. The placenta, an organ that develops inside your uterus, provides a connection between you and your baby.
This connection (via the umbilical cord) is what helps to sustain your developing baby throughout pregnancy. Necessary nutrients, oxygen, and antibodies pass from the placenta through the umbilical cord and to your baby.
Your placenta also works in reverse, meaning that it removes waste products and carbon dioxide from the baby’s blood back to your blood.
Since the placenta keeps your blood separate from your baby’s blood, it also helps to keep some bacteria and viruses out of the womb, protecting the fetus from infections.
In addition to being a lifeline to your baby, the placenta also produces and secretes hormones directly into the bloodstream to help support pregnancy and fetal growth. These hormones include:
- progesterone
- estrogen
- oxytocin
- human chorionic gonadotropin
- human placental lactogen
Pregnancy involves a complex series of events, one of which is the formation of the placenta. In general, once the fertilized egg implants in the uterine wall, the placenta begins forming. But the ball starts rolling several days before implantation.
When you ovulate, an egg leaves the ovary to travel through the fallopian tube in hopes of being fertilized.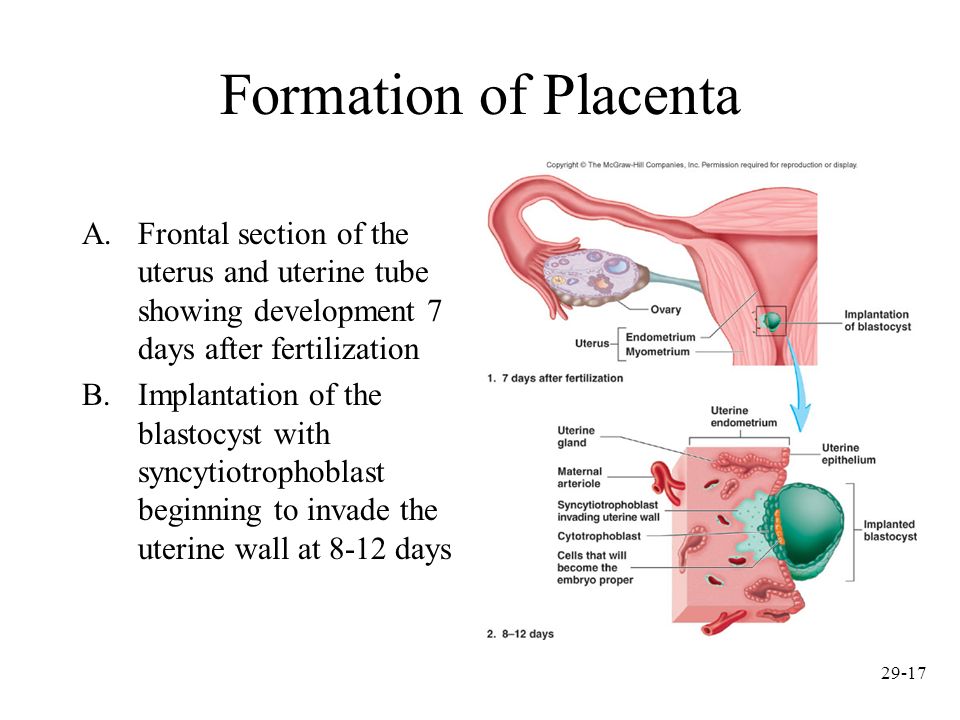 If successful, the ovulated egg meets up with a spermatozoid to begin formation of the fetus. This ovulated egg is called a zygote. Over the course of a few days, the zygote will complete many cell divisions in the fallopian tube.
If successful, the ovulated egg meets up with a spermatozoid to begin formation of the fetus. This ovulated egg is called a zygote. Over the course of a few days, the zygote will complete many cell divisions in the fallopian tube.
When the zygote reaches the uterus, these cell divisions continue, and then the zygote becomes a blastocyst. At this stage, some cells begin to form into the placenta and others begin to form the fetus. The blastocyst embeds in the endometrium (aka implantation).
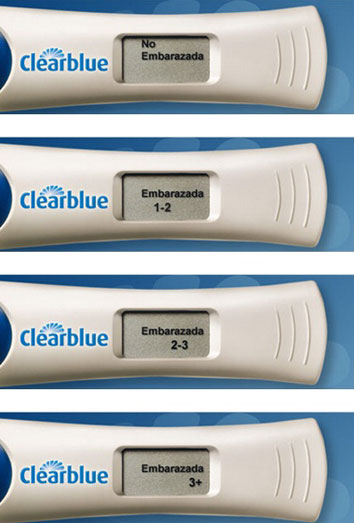
To help support pregnancy, the placenta produces a hormone called human chorionic gonadotropin (hCG). (This is the hormone measured by a pregnancy test, which is why you won’t get a positive test until after implantation.)
Over the course of your pregnancy, the placenta grows from a few cells into an organ that will eventually weigh about 1 pound. By week 12, the placenta is formed and ready to take over nourishment for the baby. However, it continues to grow throughout your pregnancy.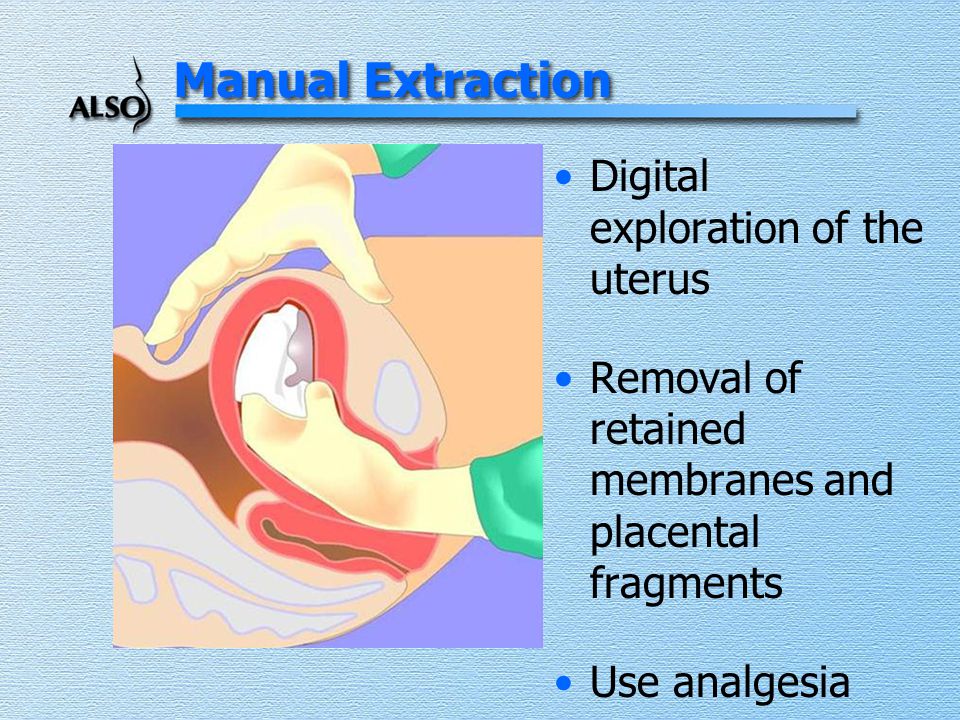 It’s considered mature by 34 weeks.
It’s considered mature by 34 weeks.
Under normal conditions, the placenta will attach to the wall of your uterus. As pregnancy progresses, it will move with your growing uterus.
Since the placenta plays such a significant role during pregnancy, it’s helpful to know when it takes over key functions such as hormone production and providing nutrients to your baby.
Although each pregnancy is different, you can expect the placenta to take over around weeks 8 to 12 of pregnancy, with 10 weeks being the average time for most women.
This doesn’t mean that your own hormone production and nutrition aren’t important. In fact, as far as nutrition goes, the placenta “taking over” means that what you consume can now reach your baby via the umbilical cord and placenta.
Those who get pregnant via in vitro fertilization or have hormone deficiencies may need progesterone supplementation in the first trimester. These individuals are often able to stop taking this hormone once the placenta begins its own production.
Many women look forward to the second trimester — energy levels rise, hormone levels begin to balance out, and morning sickness subsides. But why does everything seem to get better?
As already mentioned, towards the end of the first trimester (around week 10), the placenta takes over the production of progesterone. This helps reduce nausea and vomiting. For many mamas, this means an end to morning sickness.
And what if your morning sickness doesn’t go way? The placenta may play a role in that case, too.
If you happen to have a higher concentration of a protein called GDF15 in your blood, those frequent bouts of nausea and vomiting may continue for some time.
One study found that women who reported vomiting in the second trimester had a higher level of maternal circulating GDF15 concentrations around week 15 of pregnancy.
The good news? Researchers speculate that high levels of GDF15 could mean that the placenta is developing properly.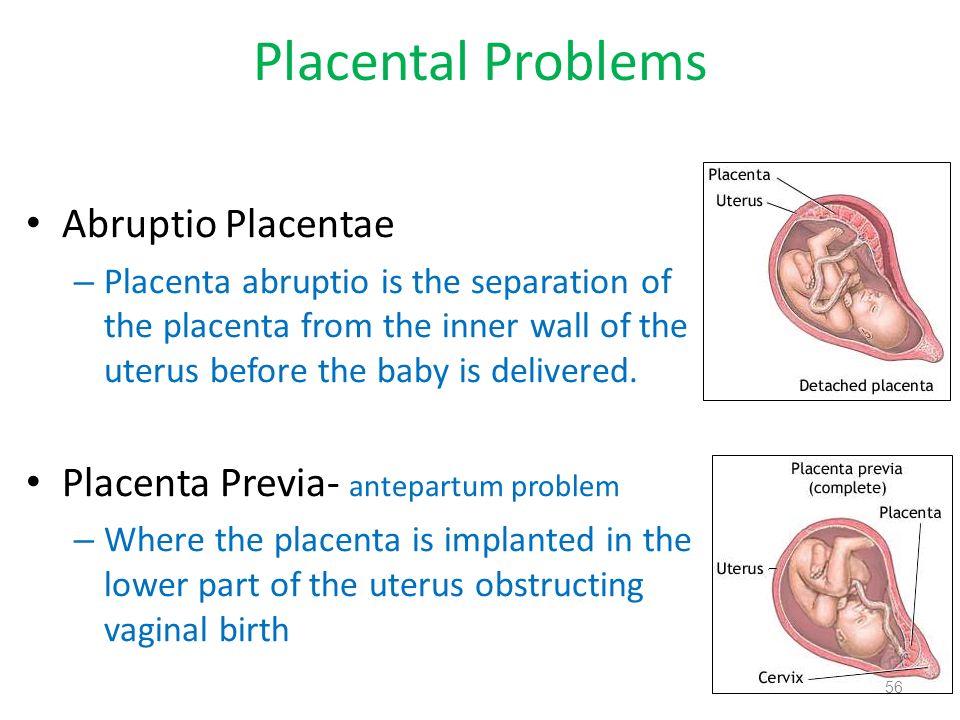 It could also help explain why some women have hyperemesis gravidarum, which is an extreme form of morning sickness.
It could also help explain why some women have hyperemesis gravidarum, which is an extreme form of morning sickness.
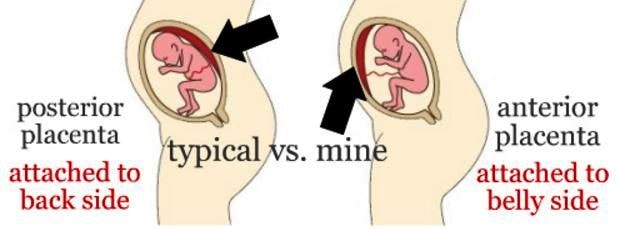
The placenta usually attaches to the side or at the top of the uterus, but this is not always the case. Sometimes, it can develop in the wrong location or attaches too deeply, leading to placenta disorders.
Even if you experience a healthy pregnancy, complications with the placenta can still occur. That said, these conditions typically happen as a result of factors, like:
- genetics
- maternal age
- high blood pressure
- carrying multiples
- previous cesarean deliveries
- substance use
- previous placental problems
- abdominal trauma
The good news is your doctor will monitor many of these conditions throughout your pregnancy and work with you on a delivery plan.
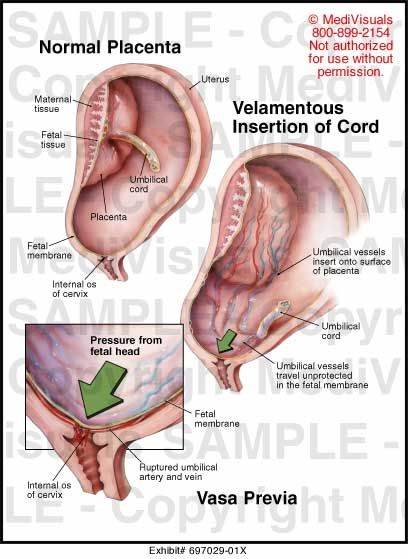
Placenta previa is a condition that causes the placenta to grow in the lowest part of the womb, typically within 2 centimeters from the cervical opening.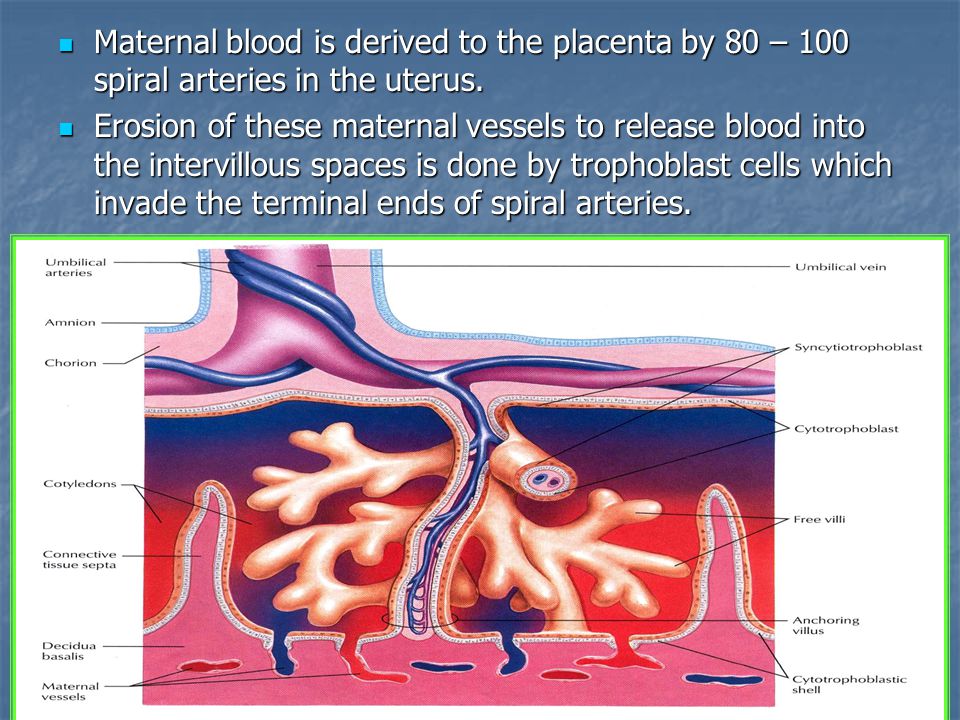 As a result, the placenta covers all or part of the cervix. If the placenta is completely covering the cervix, this can cause bleeding during delivery and most likely will require a C-section for delivery.
As a result, the placenta covers all or part of the cervix. If the placenta is completely covering the cervix, this can cause bleeding during delivery and most likely will require a C-section for delivery.
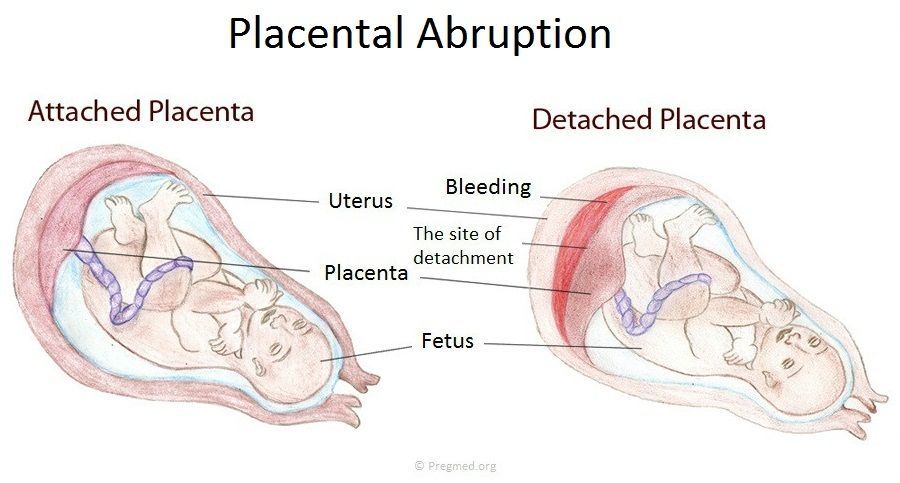
Placental abruption is a serious condition that causes the placenta to detach from the wall of the uterus during pregnancy or birth. Symptoms include vaginal bleeding and back or abdominal pain.
Placenta accreta happens when part or all of the placenta is embedded too deep into the uterine wall.
Anterior placenta indicates that the placenta has attached to the front of the stomach. Typically, this isn’t an issue — it’s really just a normal variant — but tell your doctor if you feel decreased fetal movement.
Retained placenta indicates that part of the placenta is still in the womb after childbirth. If the placenta does not deliver within a certain amount of time, generally 30 minutes (but can be as long as 60 minutes), your doctor will perform a procedure to remove the placenta.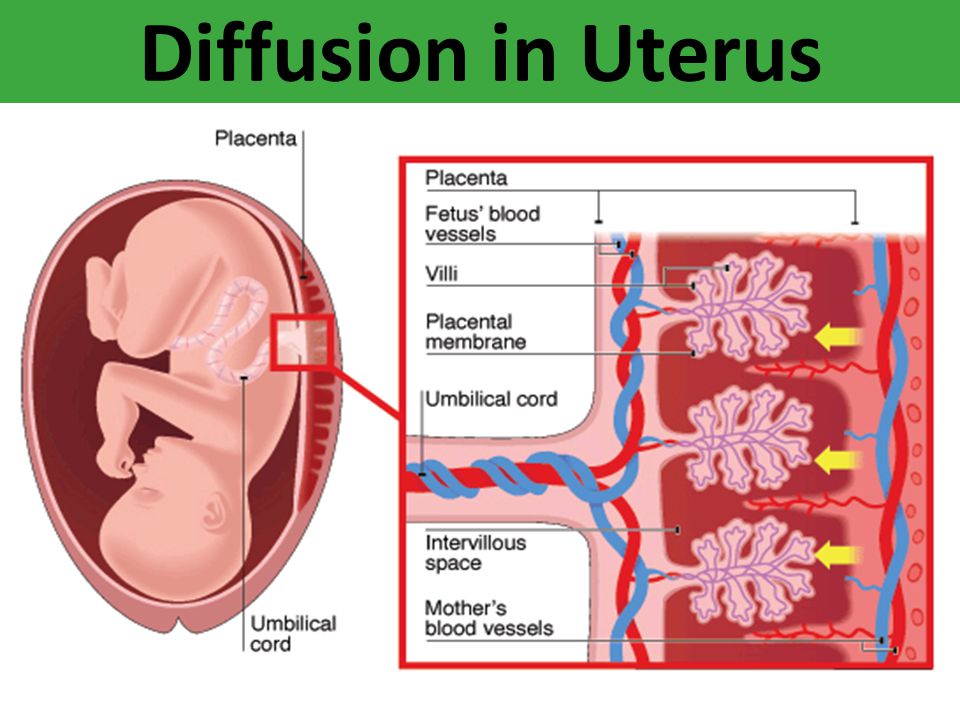
Placental insufficiency is diagnosed when the placenta cannot deliver an adequate supply of oxygen and nutrients to the fetus, which can result in pregnancy complications. Your doctor will monitor this condition throughout pregnancy.
If this is your first pregnancy, then you might be surprised to learn that delivering your baby is not the only stage of childbirth. After setting your sights on that beautiful bundle of joy, get ready for stage three of childbirth — delivering the placenta.
During this last leg of delivery, your uterus will continue to contract, allowing the placenta to separate from the uterine wall and eventually through the birth canal for delivery.
If you had a vaginal birth, this process takes about 30 minutes. For mamas that deliver via cesarean, your doctor will remove the placenta.
To move things along, your doctor may ask you to push, or they may massage your uterus. In some cases, they may give you Pitocin to help make the uterus contract.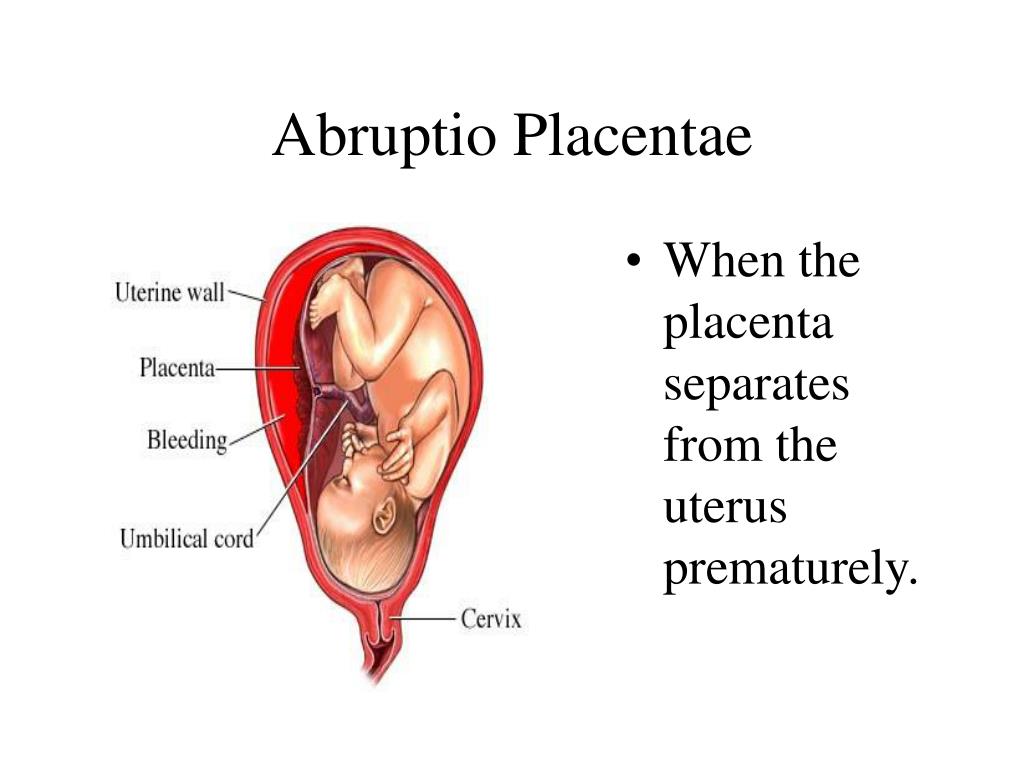 Or, they may recommend a little skin-to-skin contact with your baby to help your uterus contract.
Or, they may recommend a little skin-to-skin contact with your baby to help your uterus contract.
The placenta is an essential organ that provides oxygen and nutrients to your developing baby. It also plays a significant role in the health of your pregnancy.
Throughout your pregnancy, the placenta grows and changes shape. If you experience any symptoms such as bleeding from the vagina, abdominal pain, or back pain, contact your doctor immediately. These may be signs of a more serious condition like placenta previa.
When does the placenta form, and what does it do? Learn all about the placenta.
One of the many remarkable things about pregnancy is that you're not only growing a new human being, but also an entirely new organ. And pretty much everything your baby needs to develop and thrive flows through it. Find out all about the amazing placenta, including when it forms and what it does.
What is the placenta?
The placenta is a pancake-shaped organ that develops within the wall of your uterus and connects to your baby though the umbilical cord. By the end of pregnancy, it grows to be about 9 inches in diameter and about an inch thick at the center.
By the end of pregnancy, it grows to be about 9 inches in diameter and about an inch thick at the center.
What does the placenta do?
- It delivers oxygen and nutrients (such as vitamins, glucose, and water) from your body to the baby's, and processes the waste products from your baby.
- It produces the hormones that help your baby grow and develop.
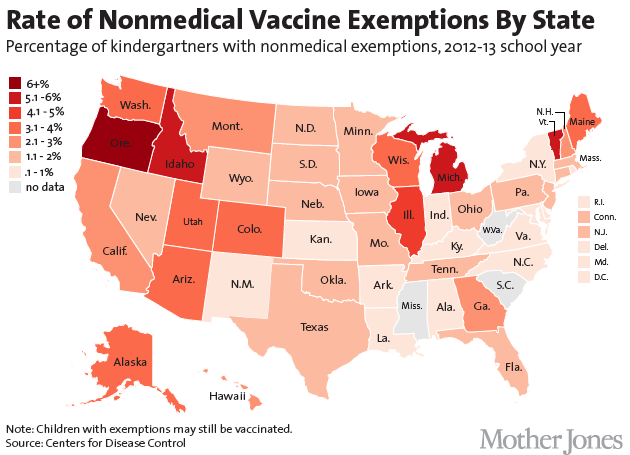
- It allows antibodies to pass to your baby from your bloodstream. These antibodies protect against certain bacterial infections and viral illnesses, like diphtheria and measles, until after your baby is born and old enough to get their first vaccinations.
When does the placenta form?
The placenta starts forming as early as six days after fertilization. At this point your baby-to-be is a hollow ball of several hundred cells called a blastocyst. The blastocyst attaches to the lining of the uterus, usually near the top. This is called implantation, and it's completed by day 9 or 10.
The wall of the blastocyst is one cell thick except in one area, where it's three to four cells thick.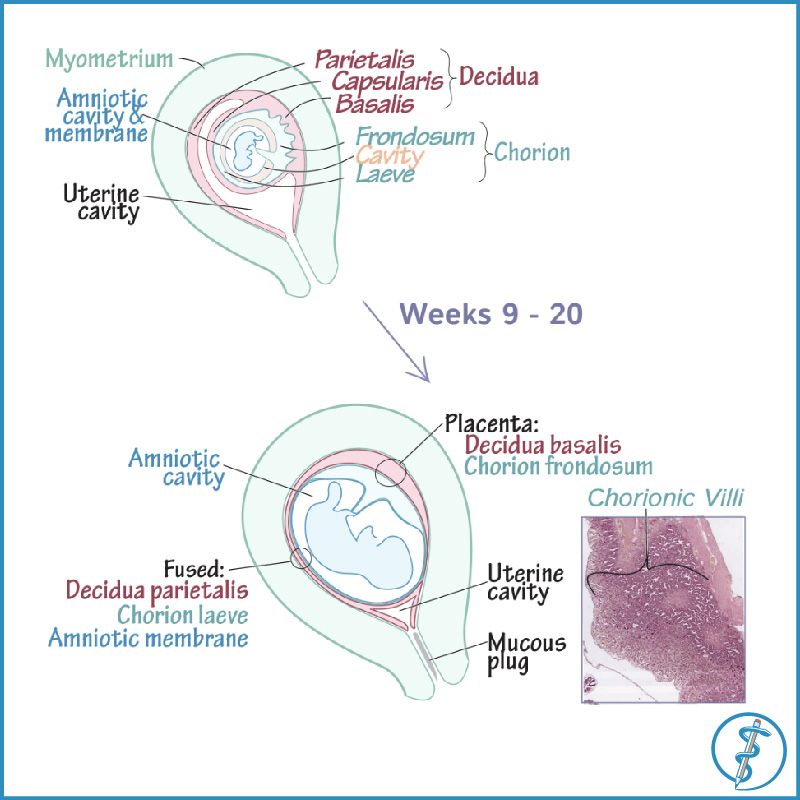 In the thickened area, the inner cells develop into the embryo. The outer cells throughout the embryo burrow into the lining of the uterus and develop into the placenta.
In the thickened area, the inner cells develop into the embryo. The outer cells throughout the embryo burrow into the lining of the uterus and develop into the placenta.
The placenta produces several hormones that help maintain the pregnancy, including human Chorionic Gonadotropin (hCG), which prevents the ovaries from releasing eggs and stimulates the ovaries to produce estrogen and progesterone continuously. (Home pregnancy tests measure levels of hCG in your urine.)
The placenta is fully formed by 18 to 20 weeks but continues to grow throughout pregnancy. At delivery, it weighs about 1 pound.
How the placenta works
The placenta connects to the umbilical cord through thousands of microscopic "fingers" of tissue (chorionic villi) containing a network of blood vessels that connect to the embryo's circulatory system. The villi are formed by 6 weeks of pregnancy, and your blood fills the spaces around them by 12 weeks. When your blood comes in contact with the villi, nutrients are exchanged for waste through the villi walls.
The villi also act as a filter, preventing some viruses and bacteria from reaching your baby, while allowing molecules of everything you ingest as well as antibodies and gases to pass through.
How do babies get nutrients in the womb?
Your baby needs nourishment from the get-go. Until the placenta is developed enough to provide nutrients, your baby receives nutrients from the lining of the uterus, called the endometrium. (These same endometrial cells will quickly multiply to form the placenta.)
In the early weeks of pregnancy, glands in the uterine lining secrete glucose, which it stores as glycogen. At first, this glycogen is the only source of nourishment for your baby.
At about 8 to 12 weeks into pregnancy, the placenta takes over as a nutrient source for your baby. (And at this point the uterus stops secreting glycogen.) Here's how it works:
- When you eat, the food travels to your stomach, where it's broken down (digested) into glucose, fats, vitamins, minerals, and protein.
- The nutrients are absorbed into your bloodstream and travel to the placenta.
- Blood vessels in the umbilical cord pass the nutrients from the placenta to vessels that flow from the umbilical cord to the baby. At this point, your baby will begin to gain weight more quickly. The umbilical cord also returns waste products from your baby to the placenta and into your circulation for elimination.
Wondering how fast the food you eat reaches your baby? It depends on how quickly the food is digested and enters your bloodstream. Some foods may take several hours, while substances like caffeine can enter your bloodstream and cross the placenta in a very short time. For more information, watch our video on how food reaches your baby.
Harmful substances that cross the placenta
Along with all the good things that are transferred to your baby, some harmful ones can cross the placenta too. These include alcohol, nicotine, and illegal drugs as well as some medications.
No safe level has been established for alcohol consumption during pregnancy, and experts recommend not drinking any amount while you're expecting. The same goes for smoking and using illegal drugs. Although marijuana is legal in some states, experts recommend against using it during pregnancy.
Use caution when taking prescribed and over-the-counter medications during pregnancy because most cross the placenta. Although many medications are considered safe for your baby, a few are known to cause birth defects. And for many drugs, there simply is not enough research to know their effects on an unborn baby. Your provider can help you determine whether the benefits of a certain drug outweigh the risks in your case.
Although the placenta acts as a barrier to most bacteria, some viruses and small bacteria can cross it. Many have no effect, but others can be harmful to a developing baby. That's one reason why it's important to get all recommended vaccinations before and during pregnancy, including a flu shot and a Tdap vaccine to protect against tetanus, diphtheria, and pertussis (whooping cough).
Both the flu and pertussis can be life-threatening for babies, and getting these vaccines while you're pregnant enables antibodies to pass through the placenta that will protect your newborn from catching these illnesses. Getting your COVID vaccine and boosters will help protect you from infection and will also provide your baby with antibodies through the placenta (and your breast milk, if you breastfeed).
Here are a few other things you can do to promote a healthy placenta and a healthy baby:
- Go to all your prenatal checkups and work with your healthcare provider to manage any health conditions, such as high blood pressure, which can cause problems with the placenta.
- Don't smoke or use drugs. Placental problems, like placental abruption, are more common in women who smoke, use illegal drugs (like cocaine and heroin), or abuse medications (like opioids).
Delivering the placenta
A few minutes after your baby is born, the placenta detaches from the wall of your uterus and is delivered through your vagina.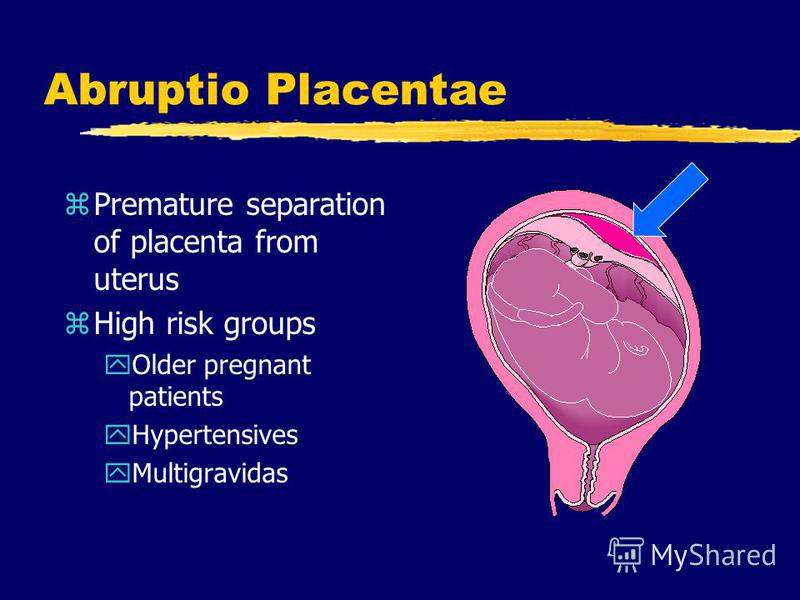 This is called the "afterbirth."
This is called the "afterbirth."
You'll have a few contractions, but this stage of childbirth usually lasts only about five to 30 minutes and feels more like menstrual cramps than labor pains. (If you're having a c-section, your doctor will remove the placenta manually.)
If you want, and if you've made prior arrangements with your provider, you can save the placenta. Some women believe that encapsulating and eating the placenta after birth helps them recover faster, though there's no scientific evidence to support this claim.
Also note that some experts think eating the placenta may be harmful, as there are potential risks, including infection and heavy metal contamination. Be sure to discuss this topic with your provider if it's something you're considering.
Learn more:
Placenta previa
Placenta accreta
Slideshow: Fetal development, week by week
advertisement | page continues below
Development of the placenta and uterus | Clinic Elite
backET RU EN LV LT SE FIN
Ask for the time of the visit- Placenta
- Uterus
- Uterine contractions
- Fetal examination
Placenta
The placenta begins to develop at the moment when the egg, a few days after fertilization, attaches itself to the wall of the uterus.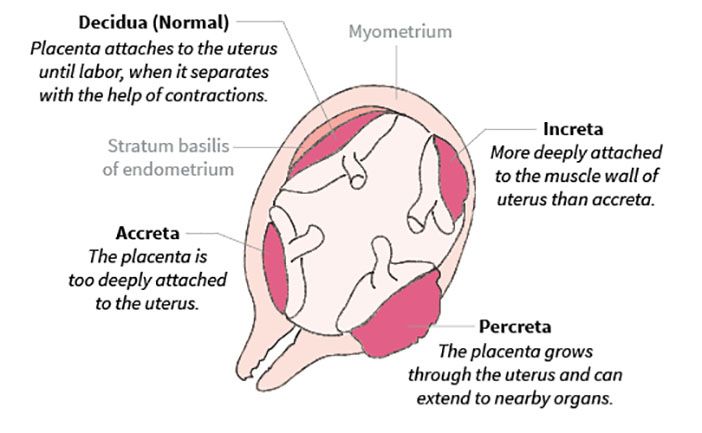 Its development is completed by the end of the fourth month of pregnancy. The placenta performs the functions of the lungs, liver, intestines, kidneys and serves as an intermediary in the transfer of nutrients from the mother to the fetus in the uterus. The normal work of the placenta is the basis for the growth and development of the fetus.
Its development is completed by the end of the fourth month of pregnancy. The placenta performs the functions of the lungs, liver, intestines, kidneys and serves as an intermediary in the transfer of nutrients from the mother to the fetus in the uterus. The normal work of the placenta is the basis for the growth and development of the fetus.
From the placenta, nutrients and oxygen are transferred through the umbilical cord to the fetus. The umbilical cord blood vessels carry fetal blood to the placenta for oxidation and simultaneously remove many waste products from the fetus into the maternal circulation. All metabolism occurs through a thin mucous membrane. A fully formed placenta weighs about 500-600 g. The placenta is flat in shape. what its Latin name says - placenta, or flat cake.
back to index
Uterus
Before pregnancy, the uterus weighs only 50-70 g. Its length is 7-9 cm. At the end of pregnancy, the weight of the uterus is about one kilogram, its capacity is about 5 liters.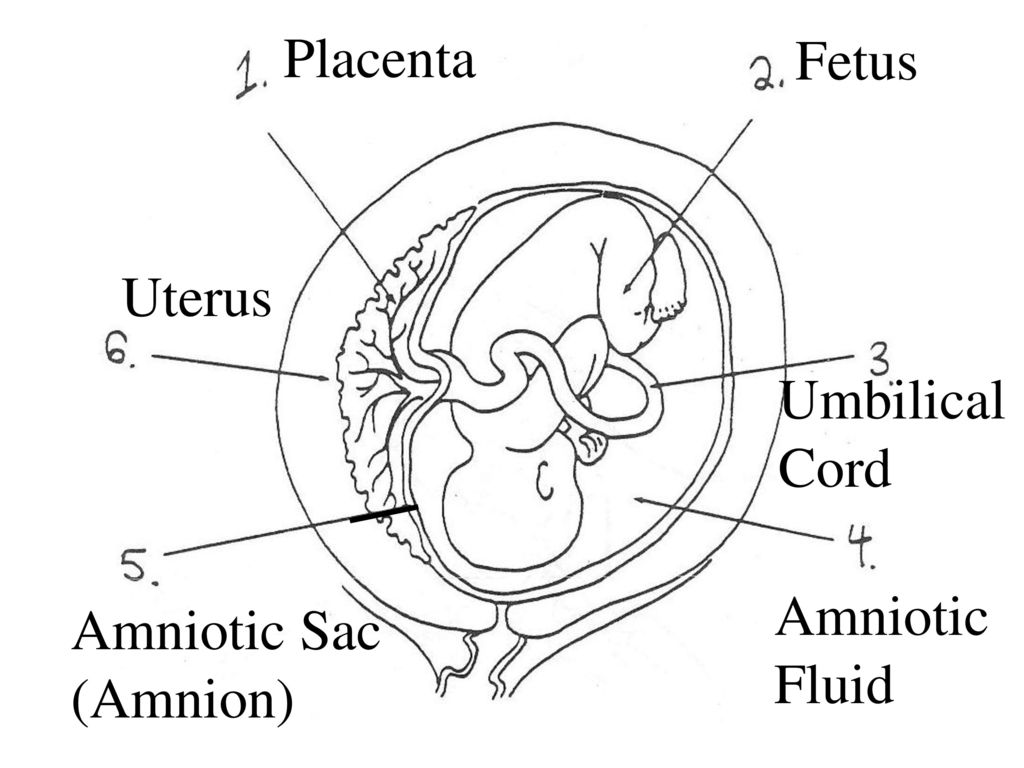 The uterus grows during pregnancy as the fetus grows. During the fourth month of pregnancy, she rises up and begins to shape the appearance of the pregnant mother. At the sixteenth week of pregnancy, the bottom of the uterus is located in the middle between the navel and the pubic joint, at the 24th week of pregnancy at the height of the navel and at the 36th week at the costal arch. Normal growth of the uterus indicates the normal functioning of the placenta, accelerated growth is often a sign of a twin pregnancy. back to index
The uterus grows during pregnancy as the fetus grows. During the fourth month of pregnancy, she rises up and begins to shape the appearance of the pregnant mother. At the sixteenth week of pregnancy, the bottom of the uterus is located in the middle between the navel and the pubic joint, at the 24th week of pregnancy at the height of the navel and at the 36th week at the costal arch. Normal growth of the uterus indicates the normal functioning of the placenta, accelerated growth is often a sign of a twin pregnancy. back to index
Uterine contractions
The uterus is gradually preparing for childbirth. During the last weeks of pregnancy, uterine contractions begin to appear, in which the abdomen "hardens". At first, contractions last only a few seconds, but at the end of pregnancy, they can be as short as half a minute. The purpose of the contractions is to prepare the cervical canal for childbirth. In the last month of pregnancy, the cervix of the uterus can open by one centimeter, in a multiparous woman even by four centimeters.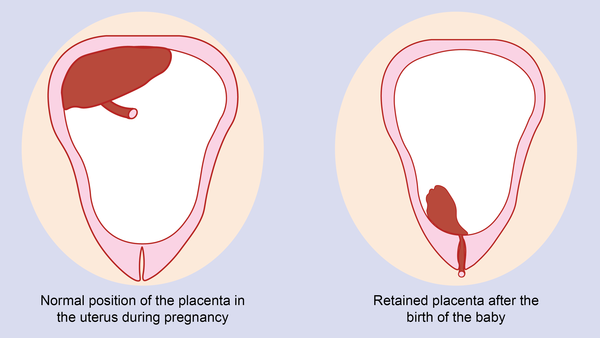 The bottom of the uterus, as a rule, falls two weeks before childbirth and the uterus acquires a spherical shape. At the same time, the fetus is installed in the mother's pelvis, usually head down.
The bottom of the uterus, as a rule, falls two weeks before childbirth and the uterus acquires a spherical shape. At the same time, the fetus is installed in the mother's pelvis, usually head down.
back to index
Fetal examination
The state of health of the fetus can also be examined while it is in the uterus. Participation in all such studies is voluntary. With the help of ultrasound, an increased risk of disease or injury can be established. In many places of residence, women over 37 years old are offered the opportunity to have a chromosome test at the municipal medical center, since the older the mother of the unborn child, the greater the risk of chromosome damage. In some communes, it is also possible to study the serum with a blood test. Establishing an increased risk does not always mean that a child will be born with a disease or injury. On the other hand, not all diseases can be detected in research. The more accurate the diagnosis, the older the mother of the unborn child.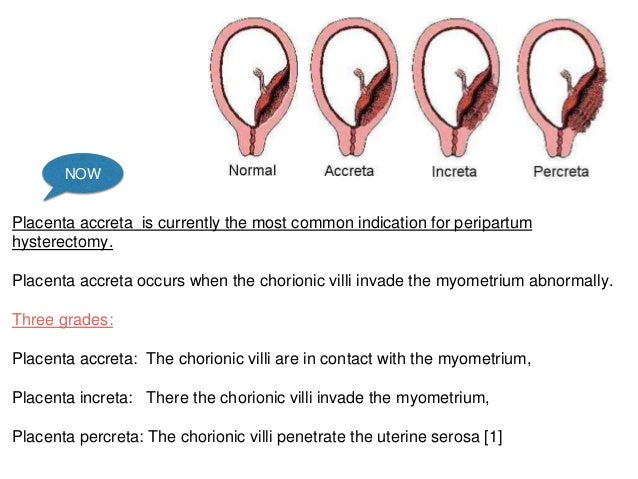 Women identified in the group of women at increased risk are offered the opportunity for a more detailed examination of the amniotic fluid or placenta. The study must be done before the 20th week of pregnancy, since no later than this week a decision must be made to terminate the pregnancy based on fetal injury. In any case, the mother will have the right to continue the pregnancy despite its riskiness. In this case, the decision will be easier to make after a thorough consideration of the various outputs already before the study.
Women identified in the group of women at increased risk are offered the opportunity for a more detailed examination of the amniotic fluid or placenta. The study must be done before the 20th week of pregnancy, since no later than this week a decision must be made to terminate the pregnancy based on fetal injury. In any case, the mother will have the right to continue the pregnancy despite its riskiness. In this case, the decision will be easier to make after a thorough consideration of the various outputs already before the study.
back to index
What is the placenta
It connects two organisms - the mother and the fetus, providing it with the necessary nutrients.
Where is the placenta located and what does it look like?
In a normal pregnancy, the placenta is located in the body of the uterus along its posterior (more often) or anterior wall. It is fully formed by the 15-16th week of pregnancy, after the 20th week, active exchange begins through the placental vessels.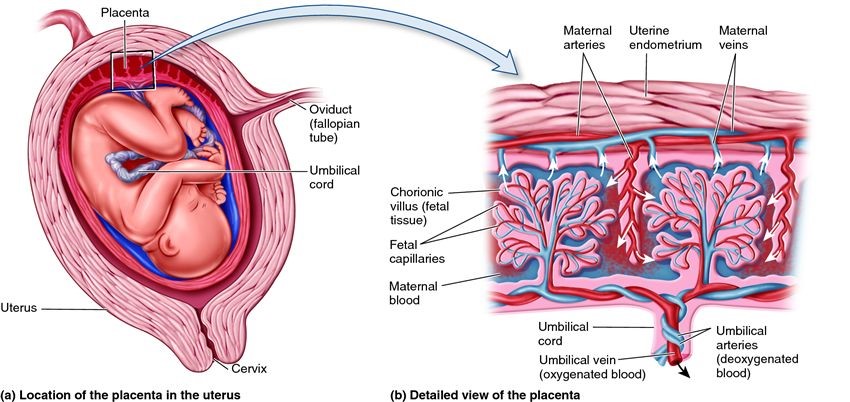 From the 22nd to the 36th week of pregnancy, an increase in the mass of the placenta occurs, and by the 36th week it reaches full functional maturity.
From the 22nd to the 36th week of pregnancy, an increase in the mass of the placenta occurs, and by the 36th week it reaches full functional maturity.
In appearance, the placenta looks like a round flat disk. By the time of delivery, the weight of the placenta is 500-600 g, the diameter is 15-18 cm and the thickness is 2-3 cm.
Functions of the placenta
Photo: zffoto / freepik.com- First, gas exchange occurs through the placenta: oxygen penetrates from the mother's blood to the fetus, and carbon dioxide is transported in the opposite direction.
- Secondly, the fetus receives through the placenta the nutrients necessary for its growth and development. It must be remembered that many substances (alcohol, nicotine, drugs, many drugs, viruses) easily penetrate through it and can have a damaging effect on the fetus.
 In addition, with its help, the fetus gets rid of the products of its vital activity.
In addition, with its help, the fetus gets rid of the products of its vital activity. - Thirdly, the placenta provides immunological protection to the fetus, delaying the cells of the mother's immune system, which, having penetrated to the fetus and recognized a foreign object in it, could trigger its rejection reactions. At the same time, the placenta passes maternal antibodies that protect the fetus from infections.
- Fourthly, the placenta plays the role of an endocrine gland and synthesizes hormones (human chorionic gonadotropin (hCG), placental lactogen, prolactin, etc.) necessary to maintain pregnancy, growth and development of the fetus.
Normally, the placenta together with the membranes (afterbirth) is born 10-15 minutes after the birth of the fetus. She is carefully examined and sent for a morphological study. First, it is very important to make sure that the whole placenta was born (that is, there are no damages on its surface and there is no reason to believe that pieces of the placenta remained in the uterine cavity).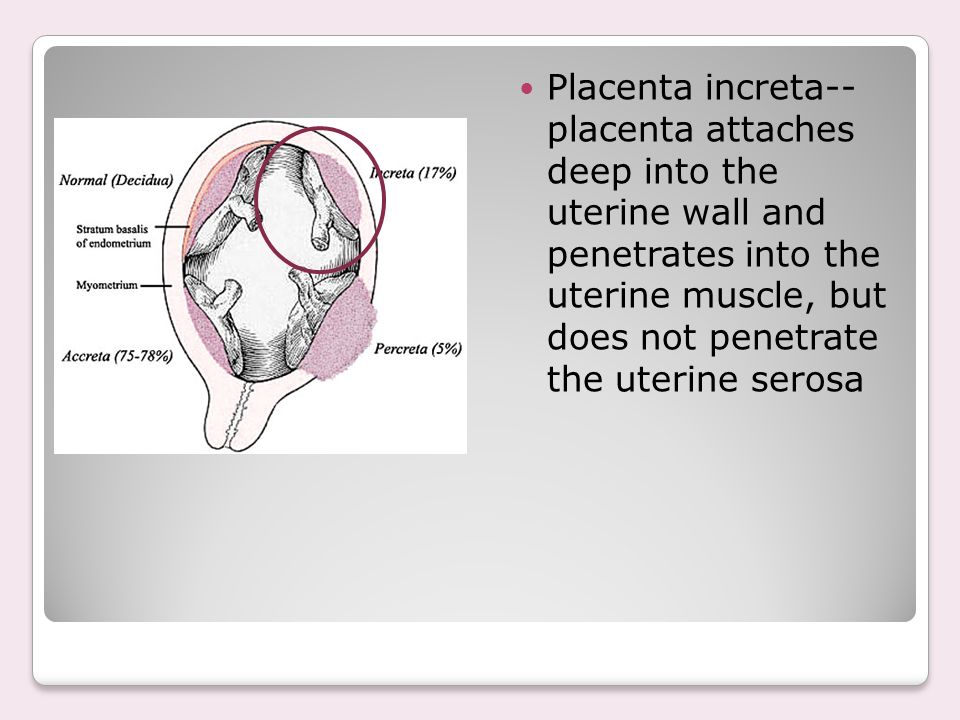 Secondly, according to the state of the placenta, one can judge the course of pregnancy (whether there was an abruption, infectious processes, etc.).
Secondly, according to the state of the placenta, one can judge the course of pregnancy (whether there was an abruption, infectious processes, etc.).
What do doctors want to know about the placenta?
During pregnancy, it is important to look for signs of placental dysfunction - placental insufficiency. To do this, during an ultrasound study, the structure of the placenta, its location in the uterine cavity, thickness, and the correspondence of the size of the fetus to the gestational age are studied. In addition, the blood flow in the placental vessels is studied.
Degree of maturity
Photo: wavebreakmedia-micro / freepik.comThis parameter, as doctors say, is "ultrasonic", that is, it depends on the density of the structures of the placenta determined by ultrasound.
There are four degrees of placental maturity:
- Normally, up to 30 weeks of pregnancy, the zero degree of placental maturity should be determined.
- The first degree is considered valid from 27 to 34 weeks.
- Second - from 34 to 39.
- Starting from 37 weeks, the third degree of placental maturity can be determined.
At the end of pregnancy, the so-called physiological aging of the placenta occurs, accompanied by a decrease in the area of its exchange surface, the appearance of areas of salt deposition.
Place of attachment
Photo: kuprevich / freepik.com Determined by ultrasound. As mentioned above, during a normal pregnancy, the placenta is located in the body of the uterus. Sometimes, during an ultrasound examination in the first half of pregnancy, it is found that the placenta is located in the lower parts of the uterus, reaching or even overlapping the area of the internal os of the cervix. In the future, as pregnancy progresses, the placenta most often shifts from the lower sections of the uterus to the top. However, if after 32 weeks the placenta still overlaps the area of the internal os, this condition is called *placenta previa**, which is a serious complication of pregnancy.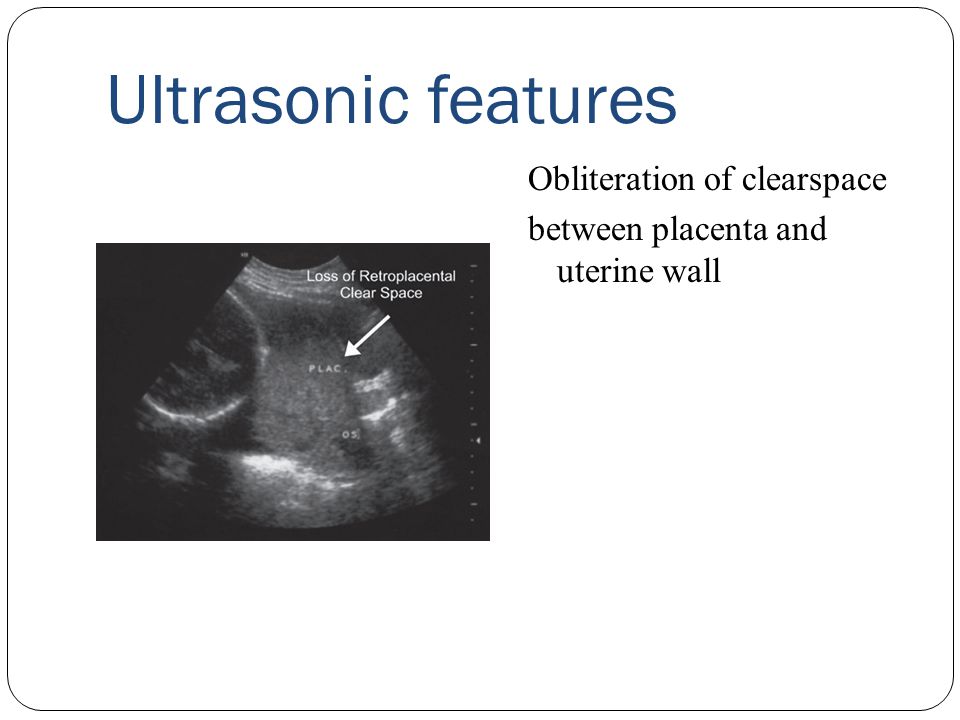
Placenta previa can lead to bleeding, which can occur during the second or third trimester of pregnancy or during childbirth.
Ultrasound with placenta previa. Turk J Obstet Gynecol / ResearchGate (Creative Commons Attribution 2.5 Generic license)Thickness
It is also determined by ultrasound - placentometry: after establishing the place of attachment of the placenta, the area where it has the largest size is found, which is determined. The thickness of the placenta, as already mentioned, continuously increases until 36-37 weeks of pregnancy (by this time it ranges from 20 to 40 mm). Then its growth stops, and in the future the thickness of the placenta either decreases or remains at the same level.
Deviation from the norm of at least one of these indicators may indicate trouble during pregnancy.
References
- Tiwari D., Das CR., Sultana R., Kashyap N., Islam M., Bose PD., Saikia AK., Bose S. Increased homocysteine mediated oxidative stress as a key determinant of hepatitis E virus ( HEV) infected pregnancy complication and outcome: A study from Northeast India.
 // Infect Genet Evol - 2021 - Vol - NNULL - p.104882; PMID:33905889
// Infect Genet Evol - 2021 - Vol - NNULL - p.104882; PMID:33905889 - Salmanian B., Belfort M.A., Shamshirsaz A.A. The risk of placenta accreta spectrum in women with in vitro fertilization in different populations. // Am J Obstet Gynecol - 2021 - Vol - NNULL - p.; PMID:33905744
- Olmos-Ortiz A., Olivares-Huerta A., García-Quiroz J., Zariñán T., Chavira R., Zaga-Clavellina V., Avila E., Halhali A., Durand M., Larrea F., Díaz L. Placentas associated with female neonates from pregnancies complicated by urinary-tract infections have higher cAMP content and cytokines expression than males. // Am J Reprod Immunol - 2021 - Vol - NNULL - p.e13434; PMID:33905581
- Tandl V., Hoch D., Bandres-Meriz J., Nikodijevic S., Desoye G., Majali-Martinez A. Different regulation of IRE1α and eIF2α pathways by oxygen and insulin in ACH-3P trophoblast model. // Reproduction - 2021 - Vol - NNULL - p.; PMID:33904834
- Ji S., Gumina D., McPeak K., Moldovan R., Post MD.
 , Su EJ. Human placental villous stromal extracellular matrix regulates fetoplacental angiogenesis in severe fetal growth restriction. // Clin Sci (Lond) - 2021 - Vol - NNULL - p.; PMID:33904582
, Su EJ. Human placental villous stromal extracellular matrix regulates fetoplacental angiogenesis in severe fetal growth restriction. // Clin Sci (Lond) - 2021 - Vol - NNULL - p.; PMID:33904582 - Shmeleva EV., Colucci F. Maternal natural killer cells at the intersection between reproduction and mucosal immunity. // Mucosal Immunol - 2021 - Vol - NNULL - p.; PMID:33903735
- Moreno-Sepulveda J., Espinós JJ., Checa MA. Lower risk of adverse perinatal outcomes in natural versus artificial frozen-thawed embryo transfer cycles: a systematic review and meta-analysis. // Reprod Biomed Online - 2021 - Vol - NNULL - p.; PMID:33903031
- Owen M.D., Cassidy A.L., Weeks AD. Why are women still dying from obstetric hemorrhage? A narrative review of perspectives from high and low resource settings. // Int J Obstet Anesth - 2021 - Vol - NNULL - p.102982; PMID:33903002
- Liu CN., Yu FB., Xu YZ., Li JS., Guan ZH., Sun MN., Liu CA., He F., Chen DJ. Prevalence and risk factors of severe postpartum hemorrhage: a retrospective cohort study.