Monoamniotic dichorionic twins
Types of twins | Pregnancy Birth and Baby
beginning of content2-minute read
Listen
There are two types of twins - fraternal twins and identical twins. Find out more about the difference between the two types and twin-twin transfusion syndrome.
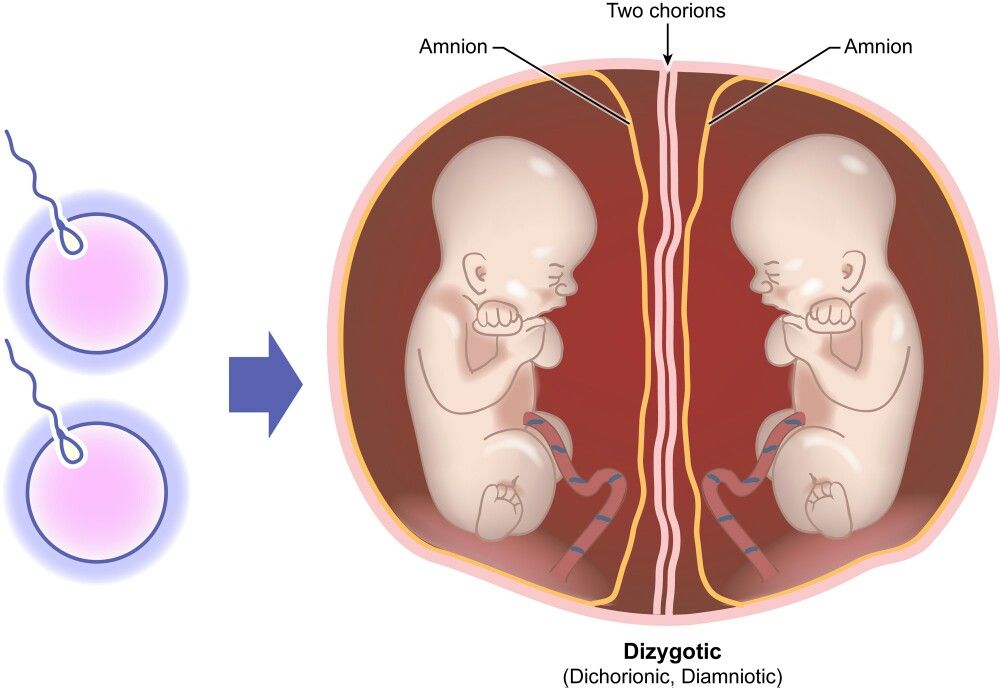
Fraternal twins
Fraternal twins are formed from the fertilisation of two eggs by two different sperm. They are also known as 'dizygotic twins', or 'non-identical twins'.
With fraternal twins, the two foetuses (developing babies) each have a separate placenta, inner membrane (the amnion) and outer membrane (the chorion). They don't usually look identical and might or might not be the same sex.
Identical twins
Identical twins are formed from the splitting of one embryo. They are also known as 'monozygotic twins'.
There are different types of identical twins, depending on what they share in the womb.
- Almost one third of identical twins have their own placenta, inner membrane, and outer membrane. The medical term for these twins is ‘dichorionic diamniotic’ or DCDA twins.
- Almost two-thirds of identical twins share the same placenta and chorion, but have their own amnion. These are ‘monochorionic diamniotic’ or MCDA twins.
- The rest — only about 4% of identical twins — share everything, and are called ‘monochorionic monoamniotic’ (MCMA) twins.
Although identical twins are the same sex and are genetically identical, they can develop quite different personalities. You can find a good description of the different types of monozygotic twins, with pictures, at the Twins Research Australia.
If you have triplets or more, the principles are similar.
Twin-twin transfusion syndrome
Identical twins who share the same placenta and chorion can sometimes share a condition called twin–twin transfusion syndrome (TTTS). In this condition, blood flows from one twin to the other, resulting in one baby getting too much blood and the other baby not getting enough. This affects the health of both babies, sometimes severely.
In this condition, blood flows from one twin to the other, resulting in one baby getting too much blood and the other baby not getting enough. This affects the health of both babies, sometimes severely.
Most identical twins don’t get TTTS. But if they do, it is more likely to happen to MCDA twins than to MCMA twins.
If your twins have TTTS, there are many different ways to treat it - ask your doctor for advice.
More information
Find more information about twins at the Twins Research Australia and the Australian Multiple Birth Association.
Sources:
Cochrane Library (Planned caesarean section for women with a twin pregnancy), Cochrane Library (Regimens of ultrasound surveillance for twin pregnancies for improving outcomes), Cochrane Library (Interventions for the treatment of twin-twin transfusion syndrome), Twins Research Australia (Types of twins)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Preschool and twins
- Raising twins
- Giving birth to twins
- Pregnant with twins
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.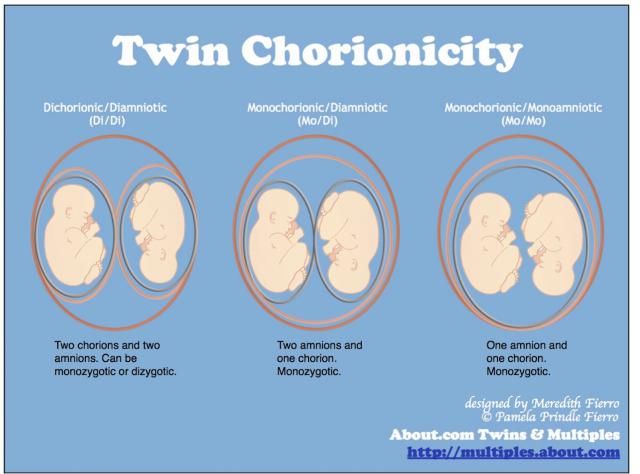
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Monoamniotic Twins | Pavilion for Women
Overview
Monoamniotic twins are identical twins that share an amniotic sac, the fluid-filled sac that holds the baby during pregnancy (also known as the “bag of waters”). Normally, identical twins each have their own amniotic sac.
Monoamniotic twins are a rare type of “monochorionic” twins, meaning they also share a placenta.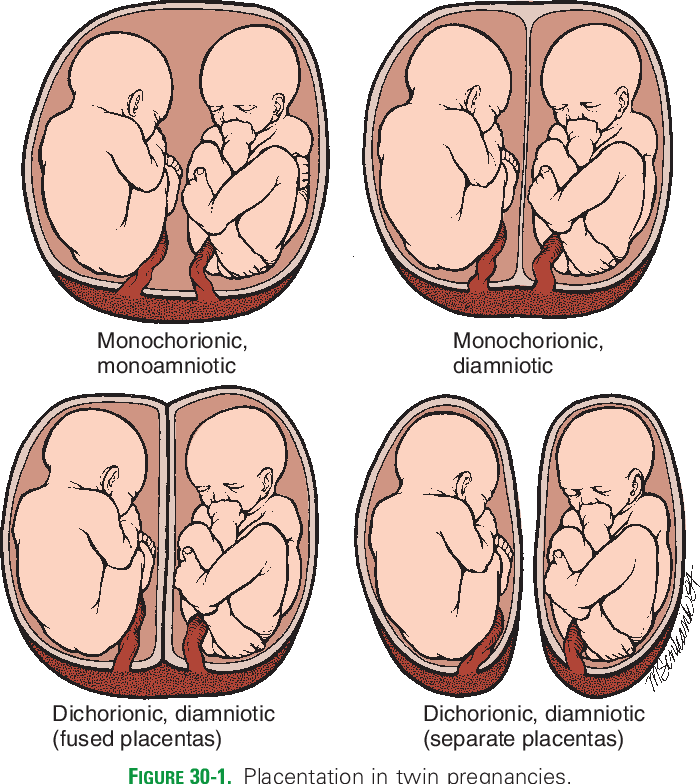 They are sometimes referred to as monochorionic-monoamniotic twins, or monoamniotic for short.
They are sometimes referred to as monochorionic-monoamniotic twins, or monoamniotic for short.
Twins that share both an amniotic sac and a placenta face increased risks compared to other twin pregnancies, with the potential for severe complications – including umbilical cord entanglement or compression – that can threaten the survival of one or both babies.
These uncommon pregnancies are estimated to occur in only 1 percent of identical twin pregnancies.
Diagnosis
Early diagnosis of monoamniotic twins is vital to recognizing the unique risks associated with these pregnancies, ensuring close monitoring for early detection of complications.
The diagnosis is typically made during a routine prenatal ultrasound in the first trimester that shows a single amniotic sac containing two fetuses. In some cases the ultrasound may show the twins’ umbilical cords are entangled, an indication the fetuses share a single amniotic sac. In these cases, the imaging should also detect a shared placenta.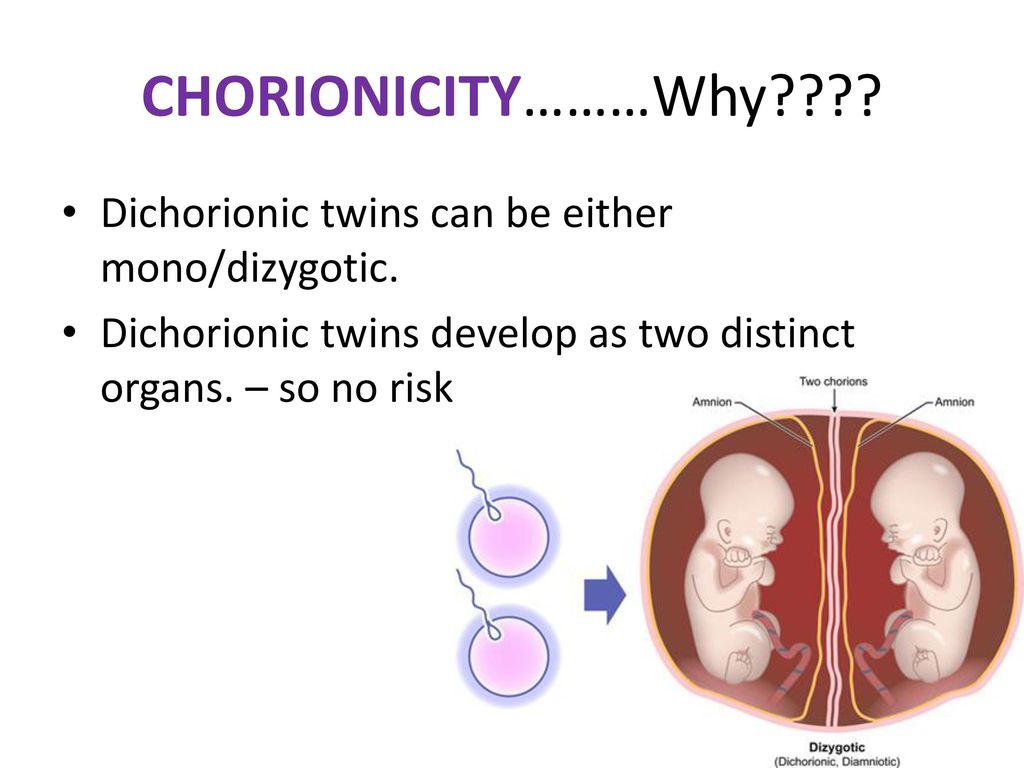
A misdiagnosis of monoamniotic twins sometimes occurs early in a twin pregnancy because the membrane that separates two amniotic sacs is so thin it may not be visible, giving the appearance of a single sac. A follow-up ultrasound that detects the dividing membrane will reveal the twins are in two separate sacs, changing the diagnosis to “diamniotic” twins (two amniotic sacs). Transvaginal ultrasonography may be needed to confirm the diagnosis of a monoamniotic twin pregnancy.
Potential Complications
In addition to the risks common to all twin pregnancies, such as preterm birth, monoamniotic twins are at increased risk of serious complications caused by both the shared amniotic sac and the shared placenta. The shared amniotic sac can result in the twins’ umbilical cords becoming entangled, with severe consequences, while the shared placenta allows the fetuses to share a blood supply, placing the twins at risk of uneven blood flow and uneven blood volume that can threaten their growth and survival.
Potential complications include:
- Umbilical cord entanglement or compression, which can restrict or cut off the blood supply to the fetuses leading to death of one or both twins
- Preterm birth, a leading cause of infant death and childhood disability
- Selective fetal growth restriction (sFGR) - poor growth and development in one twin caused by unequal sharing of the placenta
- Twin-twin transfusion syndrome (TTTS) - a relatively rapid transfer of blood from one fetus to the other that, if untreated can lead to fetal heart failure and death of one or both twins
- Twin anemia polycythemia sequence (TAPS) - a relatively slow transfer of fetal red blood cells from one fetus to the other, that if untreated can threaten the survival of one or both babies
- Twin reversed arterial perfusion (TRAP) sequence - abnormal blood flow patterns that result in one healthy twin and one severely malformed (acardiac) twin
- Amniotic fluid abnormalities, typically polyhydramnios (too much fluid), which may be an early sign of TTTS in monoamniotic twin pregnancies
- Congenital malformations, including heart defects, neural tube defects, and brain abnormalities
- Developmental delays
- Intrauterine death of one or both twins
- Conjoined twins
- Preeclampsia - maternal high blood pressure with signs of organ damage
- Postpartum hemorrhage
Specialized Evaluation and Prenatal Care
If monoamniotic twins are diagnosed, you may be referred to a fetal center for further evaluation.
At Texas Children’s Fetal Center, we arrange for you to visit as quickly as possible for a comprehensive assessment by a team of specialists experienced in the diagnosis and treatment of these rare and complex twin pregnancies, including maternal-fetal medicine physicians (OB/GYNs specializing in high-risk pregnancies), fetal surgeons, fetal imaging experts, fetal cardiologists, and neonatologists.
Additional testing will be performed using state-of-the-art imaging technologies and techniques that provide detailed views of your twins’ condition, for the most accurate diagnosis and treatment planning. Testing may include:
- High-resolution anatomy ultrasound to confirm the diagnosis and screen for abnormalities such as twin-twin transfusion syndrome (TTTS) or other signs of complications
- Ultra-fast MRI for a more detailed view of fetal anatomy
- Fetal echocardiogram to evaluate the babies’ hearts
- Doppler ultrasonography to examine blood flow between the twins
- Amniocentesis and chromosomal analysis to identify any chromosomal anomalies
Our specialists will then meet with you about the results, discuss treatment recommendations and answer any questions your family has, to help you make the most informed decisions regarding your twins’ care and treatment.
Treatment During Pregnancy
Mother and babies will be closely monitored throughout pregnancy with frequent ultrasounds and fetal echocardiograms to assess fetal growth, fetal heart function, umbilical cord entanglement, and amniotic fluid levels, among other factors, for early detection of complications.
Treatment during pregnancy depends on the health of the mother and babies. In general, treatment strategies in monoamniotic twin pregnancies may include:
- Steroids to accelerate fetal lung development, in case of early delivery
- Laser surgery if you develop advanced twin-twin transfusion syndrome
- Radiofrequency ablation, umbilical cord occlusion or laser surgery in you develop TRAP sequence
- Amnioreduction, a procedure used to reduce the amniotic fluid level, decreasing the risk of preterm labor
- Medications to stop preterm labor contractions
- Hospitalization in some cases to monitor the twins more closely
If complications occur during these pregnancies, they are often complex conditions that require accurate diagnosis and specialized care to ensure proper treatment. If fetal intervention is recommended, talk with your healthcare team about the potential benefits and risks, to help you make the best decision for your family.
If fetal intervention is recommended, talk with your healthcare team about the potential benefits and risks, to help you make the best decision for your family.
Delivery
Delivery should take place at a center with the expertise and resources required to treat these rare twin pregnancies and deliveries, including the highest level neonatal intensive care unit (NICU) for premature and critically ill newborns.
Preterm delivery is common in monoamniotic pregnancies. A cesarean delivery may be necessary if umbilical cord complications occur.
Delivery timing and postnatal care should be carefully planned and coordinated, balancing the risk of complications to the twins in utero with the risks associated with preterm birth. Our Fetal Center team works closely with pediatric experts from Texas Children’s Hospital, consistently ranked one of the best children’s hospitals in the nation by U.S. News & World Report.
Treatment After Birth
Treatment after birth depends on the health of the newborns. Monoamniotic twins often require a stay in the NICU for breathing support, feeding assistance, or other needs associated with prematurity, or for treatment of complications that occurred during pregnancy.
Monoamniotic twins often require a stay in the NICU for breathing support, feeding assistance, or other needs associated with prematurity, or for treatment of complications that occurred during pregnancy.
Additional treatment may be required for any congenital defects present.
Depending on your babies’ condition, their postnatal care team may include:
- Neonatologist
- Pediatric cardiologist
- Primary pediatrician
- Pediatric surgeon
Preterm birth is a leading contributor to childhood disability, as many of the baby’s vital organs – including the lungs, brain, and heart – are still developing. Monoamniotic twins may require long-term care and follow-up due to complications associated with preterm birth.
Why Texas Children’s Fetal Center?
- A single location for expert maternal, fetal, and pediatric care. At Texas Children’s Hospital, mother and babies receive the specialized care required for the diagnosis and treatment of monoamniotic twin pregnancies and complications all in one location, including immediate access to our level IV NICU, if needed.
- A skilled, experienced team with proven outcomes. We have a dedicated team of maternal-fetal medicine (MFM) specialists, fetal surgeons, fetal imaging experts, neonatologists, pediatric cardiologists, and others who work in concert to care for you and your babies every step of the way, using proven protocols we’ve developed over the years. With their combined expertise and unified approach, this team offers the best possible care for pregnancies involving monoamniotic twins.
- We care for your children’s needs at every stage of life. Our comprehensive approach starts with your first prenatal visit and continues through delivery, postnatal care, and childhood, as needed, thanks to one of the nation’s leading teams of fetal and pediatric specialists for the care and treatment of fetal conditions and abnormalities.
Videos
- Texas Children’s Fetal Center: Our care began before he/she was born
Additional Resources
- 6 things to consider when choosing a fetal center
- The Women’s Place
This is pregnancy, when not one fetus develops in the mother's body, but several at once. A multiple pregnancy is identical or dizygotic twins (triplets and more children).
A multiple pregnancy is identical or dizygotic twins (triplets and more children).
- Monochorionic monoamniotic twins - when there is a common placenta and there is no septum between the twins, it is always identical twins.
- Monochorionic diamniotic twins - when the common placenta and septum, i.e. each fetus has its own amniotic sac.
- Dichorionic diamniotic twins - when each fetus has its own placenta and its own amniotic bladder.
Identical twins are always the same sex, have the same blood type, and are very similar in appearance. Accordingly, the opposite is true for fraternal twins. They have phenotypic differences (eye color, facial features), there may be a different blood type. Fraternal twins may be of different sexes.
Fraternal twins are formed when different eggs are fertilized by different spermatozoa.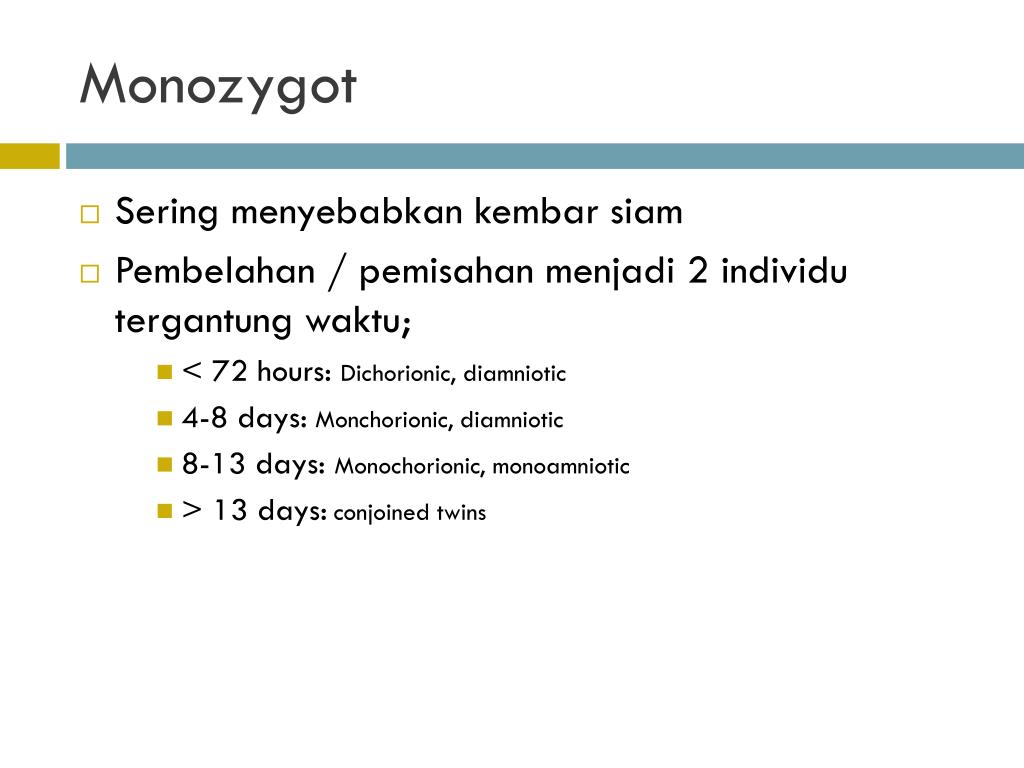 Most often, this occurs under the influence of hormonal ovarian stimulation (ovulation stimulation, assisted reproductive technologies), when several follicles with eggs are formed at once or one follicle with several eggs at the same time. Accordingly, each egg will be fertilized by a separate sperm.
Most often, this occurs under the influence of hormonal ovarian stimulation (ovulation stimulation, assisted reproductive technologies), when several follicles with eggs are formed at once or one follicle with several eggs at the same time. Accordingly, each egg will be fertilized by a separate sperm.
The development of identical twins occurs when one egg is fertilized by one sperm, but in the process of division of the fetal egg into two, three or four parts at different stages of its development. In this case, each part develops as a separate organism. It is assumed that such separation can occur when the implantation (attachment) of the fetal egg is delayed due to oxygen deficiency. Also, the occurrence of identical twins is also associated with the fertilization of an egg that had two or more nuclei.
Most often, identical twins do not have a septum between them and the fetuses have one common placenta. But depending on the stage of development, separation has occurred; identical twins can be separated by a septum from each other and may have different placentas or one common placenta, but each is in its own amniotic bladder.
But depending on the stage of development, separation has occurred; identical twins can be separated by a septum from each other and may have different placentas or one common placenta, but each is in its own amniotic bladder.
Theoretically, it is possible to fertilize two eggs of different ovulation periods. That is, in the first weeks of a pregnancy that has already occurred, if ovulation occurs again (an extremely rare case), the sperm enters the fallopian tubes and fertilizes a new egg.
In this situation, multiple uterine pregnancy may develop, but it is possible to have both uterine and ectopic pregnancies at the same time.
The chance of multiple pregnancies increases if pregnancy occurs with the help of drugs that stimulate ovulation, or with the help of assisted reproductive technologies (IVF), as well as when pregnancy occurs immediately after discontinuation of hormonal contraceptives.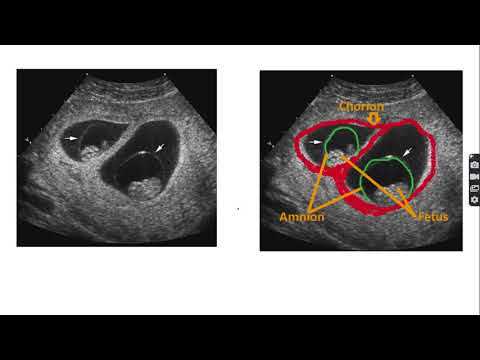 All this increases the chances of developing twins or triplets, BUT does not give a 100% guarantee. Also, the likelihood of developing twins is higher in those women in whose family there have already been multiple pregnancies.
All this increases the chances of developing twins or triplets, BUT does not give a 100% guarantee. Also, the likelihood of developing twins is higher in those women in whose family there have already been multiple pregnancies.
From a medical point of view, it is impossible to plan a multiple pregnancy on your own.
My monochorionic monoamniotic twins
Sonya Shevyrtalova
October 29, 2020 at 09:58 Pregnancy and childbirth 13422 7 minutes
We will give you 20 points for reading the article. To credit points to your account, you need to log in.
Article
“At the ultrasound, we were told that with a probability of 90% we are expecting girls, and these are mono-mono (monochorionic monoamniotic) twins: the children have one placenta and one fetal bladder. This is a rare type of twin. And, unfortunately, there is a high risk of negative consequences for children and mothers.”
This is a rare type of twin. And, unfortunately, there is a high risk of negative consequences for children and mothers.”
For as long as I can remember, I have always wanted children. And when in 2019 my husband and I saw the cherished two stripes, our happiness knew no bounds. My husband really wanted a daughter. He dreamed of how they would play with her in the evenings, go shopping and choose lovely princess dresses.
I went to the first ultrasound at the antenatal clinic alone because my husband couldn't take time off from work. The doctor looked at the monitor for a long time, moved the sensor from side to side and did not say anything. These five minutes seemed like an eternity to me, given that there was no additional monitor. After conducting a study, the doctor said that everything is fine - we are expecting twins. And on the screen he showed two small dots with pulsating hearts.
To say I was shocked is an understatement. When I left the office, I had tears of joy and happiness. Having calmed down a little, I called my husband and told him the news. He, too, was amazed. In the evening, the husband arrived from work earlier than usual, and his first question was about the day's news. The husband still did not believe, but the ultrasound picture put everything in its place. We decided not to say anything to our relatives for as long as possible. I didn’t want unnecessary discussions, mother-in-law’s lamentations about the difficulties that await us. We ourselves understood that all the difficulties were still ahead. I decided to register with a regular antenatal clinic. At the first screening, the doctor again examined the babies for a very long time and at the end of the study she said to come in a couple of days for a second ultrasound. However, she did not explain anything. At the next visit, the doctor again said nothing and made an appointment a week later.
Having calmed down a little, I called my husband and told him the news. He, too, was amazed. In the evening, the husband arrived from work earlier than usual, and his first question was about the day's news. The husband still did not believe, but the ultrasound picture put everything in its place. We decided not to say anything to our relatives for as long as possible. I didn’t want unnecessary discussions, mother-in-law’s lamentations about the difficulties that await us. We ourselves understood that all the difficulties were still ahead. I decided to register with a regular antenatal clinic. At the first screening, the doctor again examined the babies for a very long time and at the end of the study she said to come in a couple of days for a second ultrasound. However, she did not explain anything. At the next visit, the doctor again said nothing and made an appointment a week later.
I can't express in words how frightened I was. Immediately after leaving the antenatal clinic, she called her husband and told him everything.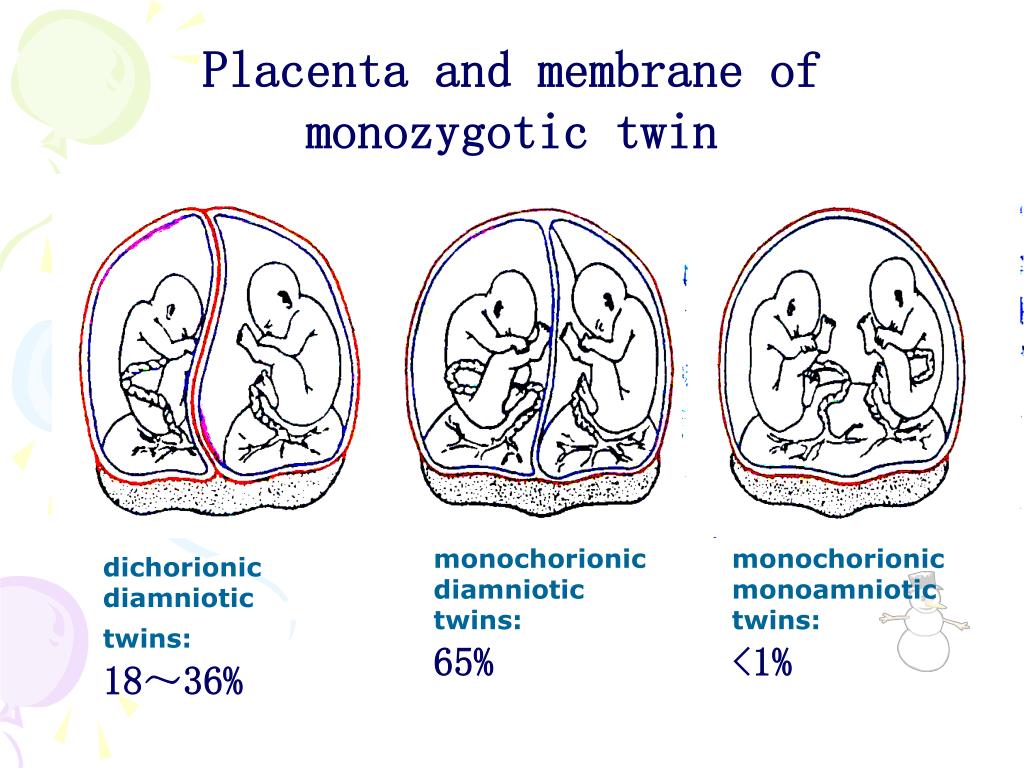 He, hearing through the phone that I was excited, took time off from work, and we went to the best private medical center in our city. After listening to our story, the administrator took us to the ultrasound room and asked us to wait a bit. Literally five minutes later I was invited to an appointment, my husband remained sitting in the corridor.
He, hearing through the phone that I was excited, took time off from work, and we went to the best private medical center in our city. After listening to our story, the administrator took us to the ultrasound room and asked us to wait a bit. Literally five minutes later I was invited to an appointment, my husband remained sitting in the corridor.
I told the doctor everything that happened in the antenatal clinic. He listened carefully and began to investigate. For the first time I saw my babies on an additional monitor. The doctor commented on everything that happened on the screen. At some point, he fell silent and began to examine something carefully. The entire study took about 30 minutes. Then he asked to invite her husband. We were happily announced that with a probability of 90% we are expecting girls, and this is monochorionic monoamniotic twins. My husband was in seventh heaven, and I began to ask the doctor for more details. He was laconic, but said that the children had one placenta and one amniotic sac.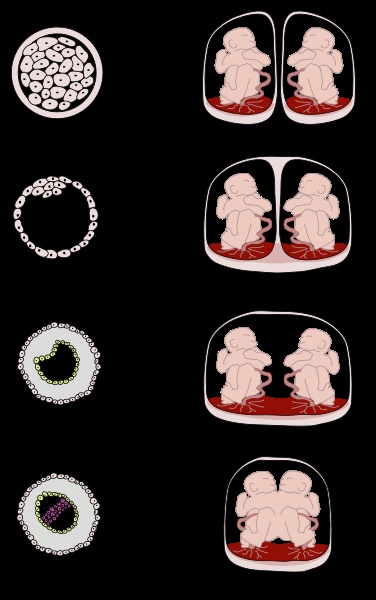 This is a fairly rare type of twin. According to statistics, there are 2 of this type per 1000 twins. And the risk of negative consequences for children and mothers is very high, so constant monitoring and ultrasound monitoring every two weeks is necessary.
This is a fairly rare type of twin. According to statistics, there are 2 of this type per 1000 twins. And the risk of negative consequences for children and mothers is very high, so constant monitoring and ultrasound monitoring every two weeks is necessary.
After the reception, I could not recover for a long time. On the way home I read a lot about this type of twins. They wrote on medical forums that with mono-mono twins, there is a high risk of tangling the umbilical cord, lagging behind in the development of one of the fetuses, and even death.
At the repeated ultrasound in the antenatal clinic, several specialists looked at me at once: the head of the antenatal clinic and the doctor who was in charge of my pregnancy. The study took a very long time, then they confirmed to me that I had mono-mono twins. This pregnancy was the first in our city, so I received close attention from the antenatal clinic. I went to appointments every two weeks, before that I always did an ultrasound and took tests.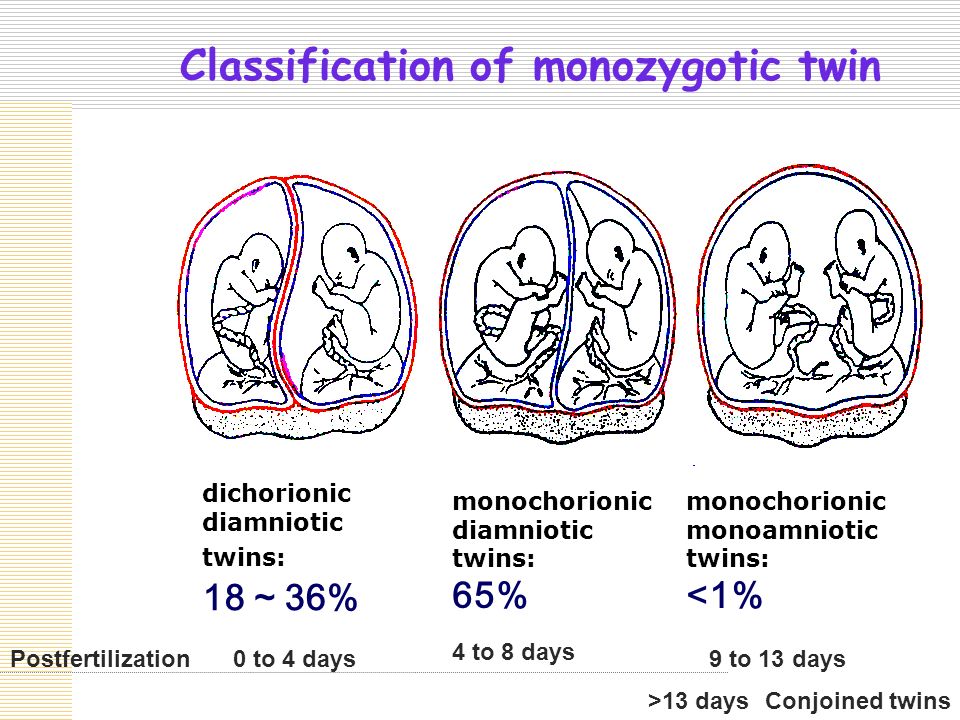 The pregnancy proceeded without toxicosis and tone. Everything was fine, until at the second screening (at the 20th week) by ultrasound, they found that one baby did not have enough nutrition, and she was about a week behind the second.
The pregnancy proceeded without toxicosis and tone. Everything was fine, until at the second screening (at the 20th week) by ultrasound, they found that one baby did not have enough nutrition, and she was about a week behind the second.
I was admitted to the hospital. From that moment began a new adventure in our lives. In the hospital, they took a huge number of tests from me, did an ultrasound of the fetuses, all my organs, prescribed droppers with vitamins and magnesia every other day. So I stayed for 10 days. The baby grew up a little, and they let me go home.
But not even two weeks had passed before I ended up in the hospital again. This time I was overtaken by a terrible tone, hemoglobin greatly decreased. More drips, injections, pills, 10 days out of the house on a terribly hard bed.
Words cannot express how happy I was to be discharged from the hospital. But I left with a bunch of appointments. Every day I had to take a handful of pills, and I began to go to the appointment every week.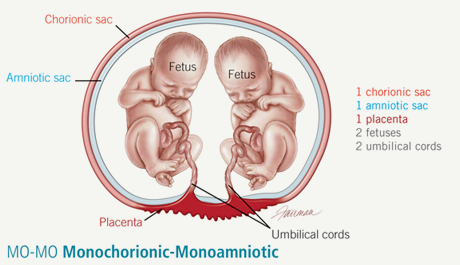
So a month has passed, and it is time to go on maternity leave. I said goodbye to my colleagues for the next three years and with a calm soul went to prepare for the upcoming birth.
The next weeks passed practically in a lying position: as soon as I started to walk more, a strong tone immediately appeared. And from 30 weeks I had terrible training contractions, besides, one baby was still a week behind the other. I was again admitted to the hospital and they did not want to let me out until the birth. But I agreed with the manager to transfer me to a day hospital: it was simply impossible to stay in the hospital for such a long time.
At home I continued to stay in bed and went to the procedures every two days. So we made it to 36 weeks. One baby still lagged behind in development. No injections and pills helped, so at the next consultation, the doctors decided to perform the operation in the near future. The date of the operation was set for February 5, 2020, but my crumbs decided differently: on February 2, at 4 am, my water broke.