Being induced into labor
Inducing labour - NHS
An induced labour is one that's started artificially. Every year, 1 in 5 labours are induced in the UK.
Sometimes labour can be induced if your baby is overdue or there's any risk to you or your baby's health.
This risk could be if you have a health condition such as high blood pressure, for example, or your baby is not growing.
Induction will usually be planned in advance. You'll be able to discuss the advantages and disadvantages with your doctor and midwife, and find out why they think your labour should be induced.
It's your choice whether to have your labour induced or not.
If your pregnancy lasts longer than 42 weeks and you decide not to have your labour induced, you should be offered increased monitoring to check your baby's wellbeing.
Why you might be induced
- if you're overdue
- if your waters have broken
- if you or your baby have a health problem
If you're overdue
Induction will be offered if you do not go into labour naturally by 42 weeks, as there will be a higher risk of stillbirth or problems for the baby.
If your waters break early
If your waters break more than 24 hours before labour starts, there's an increased risk of infection to you and your baby.
If your waters break after 34 weeks, you'll have the choice of induction or expectant management.
Expectant management is when your healthcare professionals monitor your condition and your baby's wellbeing, and your pregnancy can progress naturally as long as it's safe for both of you.
Your midwife or doctor should discuss your options with you before you make a decision.
They should also let you know about the newborn (neonatal) special care hospital facilities in your area.
If your baby is born earlier than 37 weeks, they may be vulnerable to problems related to being premature.
If your waters break before 34 weeks, you'll only be offered induction if there are other factors that suggest it's the best thing for you and your baby.
If you have a health condition or your baby is not thriving
You may be offered an induction if you have a condition that means it'll be safer to have your baby sooner, such as diabetes, high blood pressure or intrahepatic cholestasis of pregnancy.
If this is the case, your doctor and midwife will explain your options to you so you can decide whether or not to have your labour induced.
Membrane sweep
Before inducing labour, you'll be offered a membrane sweep, also known as a cervical sweep, to bring on labour.
To carry out a membrane sweep, your midwife or doctor sweeps their finger around your cervix during an internal examination.
This action should separate the membranes of the amniotic sac surrounding your baby from your cervix. This separation releases hormones (prostaglandins), which may start your labour.
Having a membrane sweep does not hurt, but expect some discomfort or slight bleeding afterwards.
If labour does not start after a membrane sweep, you'll be offered induction of labour.
Induction is always carried out in a hospital maternity unit. You'll be looked after by midwives and doctors will be available if you need their help.
How labour is induced
If you're being induced, you'll go into the hospital maternity unit.
Contractions can be started by inserting a tablet (pessary) or gel into your vagina.
Induction of labour may take a while, particularly if the cervix (the neck of the uterus) needs to be softened with pessaries or gels.
You will usually stay in the hospital maternity unit while you wait for it to work.
If you've had no contractions after 6 hours, you may be offered another tablet or gel.
If you have a controlled-release pessary inserted into your vagina, it can take 24 hours to work. If you are not having contractions after 24 hours, you may be offered another dose.
Sometimes a hormone drip is needed to speed up the labour. Once labour starts, it should proceed normally, but it can sometimes take 24 to 48 hours to get you into labour.
What induced labour feels like
Induced labour is usually more painful than labour that starts on its own, and you may want to ask for an epidural.
Your pain relief options during labour are not restricted by being induced. You should have access to all the pain relief options usually available in the maternity unit.
If you are induced you'll be more likely to have an assisted delivery, where forceps or ventouse suction are used to help the baby out.
If induction of labour does not work
Induction is not always successful, and labour may not start.
Your obstetrician and midwife will assess your condition and your baby's wellbeing, and you may be offered another induction or a caesarean section.
Your midwife and doctor will discuss all your options with you.
Natural ways to start labour
There are no proven ways of starting your labour yourself at home.
You may have heard that certain things can trigger labour, such as herbal supplements and having sex, but there's no evidence that these work.
Other methods that are not supported by scientific evidence include acupuncture, homeopathy, hot baths, castor oil and enemas.
Having sex will not cause harm, but you should avoid having sex if your waters have broken as there's an increased risk of infection.
For more information on induction, you can read the NICE information for the public on induction of labour.
Video: When would I be induced and what's involved?
In this video, a midwife describes what an induction of labour is and what is involved.
Media last reviewed: 20 March 2020
Media review due: 20 March 2023
Labor induction - Mayo Clinic
Overview
Labor induction — also known as inducing labor — is prompting the uterus to contract during pregnancy before labor begins on its own for a vaginal birth.
A health care provider might recommend inducing labor for various reasons, primarily when there's concern for the mother's or baby's health. An important factor in predicting whether an induction will succeed is how soft and expanded the cervix is (cervical ripening). The gestational age of the baby as confirmed by early, regular ultrasounds also is important.
The gestational age of the baby as confirmed by early, regular ultrasounds also is important.
If a health care provider recommends labor induction, it's typically because the benefits outweigh the risks. If you're pregnant, understanding why and how labor induction is done can help you prepare.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
To determine if labor induction is necessary, a health care provider will likely evaluate several factors. These include the mother's health and the status of the cervix. They also include the baby's health, gestational age, weight, size and position in the uterus. Reasons to induce labor include:
- Nearing 1 to 2 weeks beyond the due date without labor starting (postterm pregnancy).
- When labor doesn't begin after the water breaks (prelabor rupture of membranes).

- An infection in the uterus (chorioamnionitis).
- When the baby's estimated weight is less than the 10th percentile for gestational age (fetal growth restriction).
- When there's not enough amniotic fluid surrounding the baby (oligohydramnios).
- Possibly when diabetes develops during pregnancy (gestational diabetes), or diabetes exists before pregnancy.
- Developing high blood pressure in combination with signs of damage to another organ system (preeclampsia) during pregnancy. Or having high blood pressure before pregnancy, developing it before 20 weeks of pregnancy (chronic high blood pressure) or developing the condition after 20 weeks of pregnancy (gestational hypertension).
- When the placenta peels away from the inner wall of the uterus before delivery — either partially or completely (placental abruption).
- Having certain medical conditions. These include heart, lung or kidney disease and obesity.
Elective labor induction is the starting of labor for convenience when there's no medical need. It can be useful for women who live far from the hospital or birthing center or who have a history of fast deliveries.
It can be useful for women who live far from the hospital or birthing center or who have a history of fast deliveries.
A scheduled induction might help avoid delivery without help. In such cases, a health care provider will confirm that the baby's gestational age is at least 39 weeks or older before induction to reduce the risk of health problems for the baby.
As a result of recent studies, women with low-risk pregnancies are being offered labor induction at 39 to 40 weeks. Research shows that inducing labor at this time reduces several risks, including having a stillbirth, having a large baby and developing high blood pressure as the pregnancy goes on. It's important that women and their providers share in decisions to induce labor at 39 to 40 weeks.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Risks
Uterine incisions used during C-sections
Uterine incisions used during C-sections
A C-section includes an abdominal incision and a uterine incision. After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
Labor induction carries various risks, including:
- Failed induction. An induction might be considered failed if the methods used don't result in a vaginal delivery after 24 or more hours. In such cases, a C-section might be necessary.
- Low fetal heart rate. The medications used to induce labor — oxytocin or a prostaglandin — might cause the uterus to contract too much, which can lessen the baby's oxygen supply and lower the baby's heart rate.
- Infection. Some methods of labor induction, such as rupturing the membranes, might increase the risk of infection for both mother and baby. The longer the time between membrane rupture and labor, the higher the risk of an infection.
-
Uterine rupture. This is a rare but serious complication in which the uterus tears along the scar line from a prior C-section or major uterine surgery.
 Rarely, uterine rupture can also occur in women who have not had previous uterine surgery.
Rarely, uterine rupture can also occur in women who have not had previous uterine surgery.An emergency C-section is needed to prevent life-threatening complications. The uterus might need to be removed.
- Bleeding after delivery. Labor induction increases the risk that the uterine muscles won't properly contract after giving birth, which can lead to serious bleeding after delivery.
Labor induction isn't for everyone. It might not be an option if:
- You've had a C-section with a classical incision or major uterine surgery
- The placenta is blocking the cervix (placenta previa)
- Your baby is lying buttocks first (breech) or sideways (transverse lie)
- You have an active genital herpes infection
- The umbilical cord slips into the vagina before delivery (umbilical cord prolapse)
If you have had a C-section and have labor induced, your health care provider is likely to avoid certain medications to reduce the risk of uterine rupture.
How you prepare
Labor induction is typically done in a hospital or birthing center. That's because mother and baby can be monitored there, and labor and delivery services are readily available.
What you can expect
During the procedure
There are various ways of inducing labor. Depending on the circumstances, the health care provider might use one of the following ways or a combination of them. The provider might:
-
Ripen the cervix. Sometimes prostaglandins, versions of chemicals the body naturally produces, are placed inside the vagina or taken by mouth to thin or soften (ripen) the cervix. After prostaglandin use, the contractions and the baby's heart rate are monitored.
In other cases, a small tube (catheter) with an inflatable balloon on the end is inserted into the cervix. Filling the balloon with saline and resting it against the inside of the cervix helps ripen the cervix.
- Sweep the membranes of the amniotic sac.
 With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor.
With this technique, also known as stripping the membranes, the health care provider sweeps a gloved finger over the covering of the amniotic sac near the fetus. This separates the sac from the cervix and the lower uterine wall, which might help start labor. -
Rupture the amniotic sac. With this technique, also known as an amniotomy, the health care provider makes a small opening in the amniotic sac. The hole causes the water to break, which might help labor go forward.
An amniotomy is done only if the cervix is partially dilated and thinned, and the baby's head is deep in the pelvis. The baby's heart rate is monitored before and after the procedure.
- Inject a medication into a vein. In the hospital, a health care provider might inject a version of oxytocin (Pitocin) — a hormone that causes the uterus to contract — into a vein. Oxytocin is more effective at speeding up labor that has already begun than it is as at cervical ripening.
 The provider monitors contractions and the baby's heart rate.
The provider monitors contractions and the baby's heart rate.
How long it takes for labor to start depends on how ripe the cervix is when the induction starts, the induction techniques used and how the body responds to them. It can take minutes to hours.
After the procedure
In most cases, labor induction leads to a vaginal birth. A failed induction, one in which the procedure doesn't lead to a vaginal birth, might require another induction or a C-section.
By Mayo Clinic Staff
Related
Products & Services
Forced childbirth / Health / Nezavisimaya gazeta
In Argentina, tens of thousands of people are demanding the legalization of abortion. Reuters photo
The fight against abortion comes one more round, despite the fact that abortions are becoming less and less. But it does not matter, the main thing is to achieve their complete ban. This is a convenient pretext for political speculation, populism. Moreover, it coincides with the desire of the Russian Orthodox Church and circles around the church and is in line with fashion trends towards moving towards housing construction.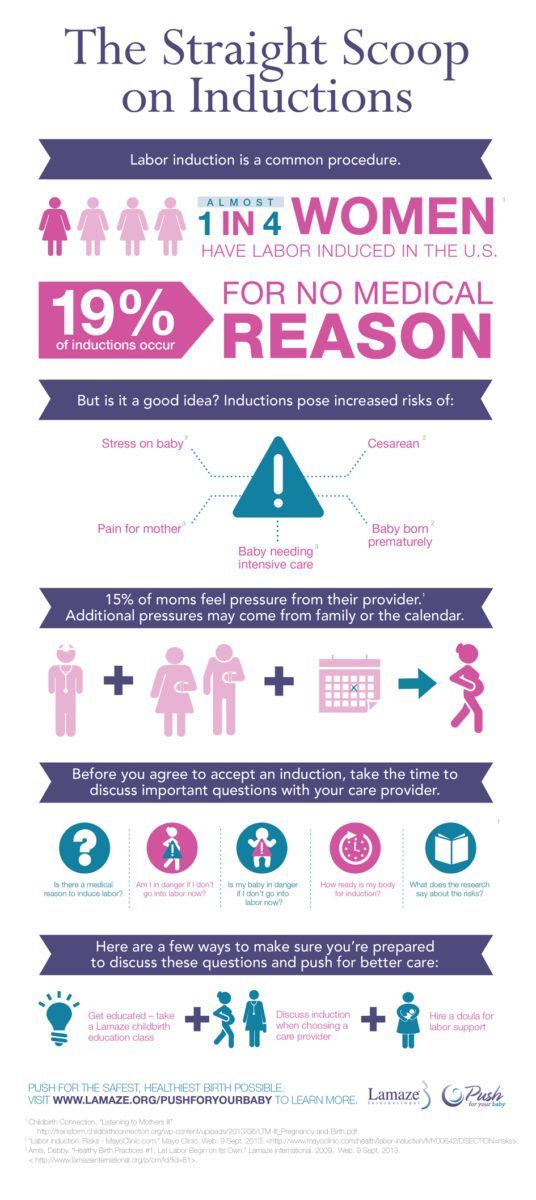 To do this, use any excuse.
To do this, use any excuse.
We have just taken advantage of the “Give me life” fund of the Prime Minister's wife Svetlana Medvedeva. The meaning of the action is not to interrupt the pregnancy and generally give birth more. It is supported by the Ministry of Health. To show their dedication to the initiative of the Prime Minister's wife, several regions announced that they would not perform abortions in medical institutions for several days. So it was, for example, in Ryazan, in Yakutia, in the Primorsky Territory. In Primorye, such additional days of the prohibition of termination of pregnancy took place from July 31 to August 3, in Ryazan in July - almost a week. Explanations of regional authorities are different. In the Ministry of Health of Yakutia, for example, where they usually hold the action "Give me life!" within the framework of health education work, the number of abortions after the action does not decrease. Therefore, this year they were going to introduce a ban on abortions in a new perinatal center in Yakutsk.
But there were reports in the media that neither the Ministry of Health of the Russian Federation nor the Svetlana Medvedeva Foundation had in mind a ban on abortions - only educational events. Stopping operations for a few days is a local initiative. Immediately, the regional authorities began to disown this initiative. The Ministry of Health of Yakutia denied reports of a moratorium on abortions, accusing the media of distorting information.
It would seem that three or four days, and even a week - it doesn't matter. But no, it's actually very important. Academician Vladimir Serov, president of the Russian Society of Obstetricians and Gynecologists, believes that declaring a moratorium on abortion is the wrong decision. After all, abortion is allowed until the 12th week. This is followed by serious complications and increased risk. If a woman goes to the doctor at 12 weeks and gets a moratorium, then at the 13th week she will not have an abortion.
And what will happen next? The expectation that, having received a refusal to perform an abortion in a medical institution, the patient will refuse to terminate the pregnancy and decide to give birth.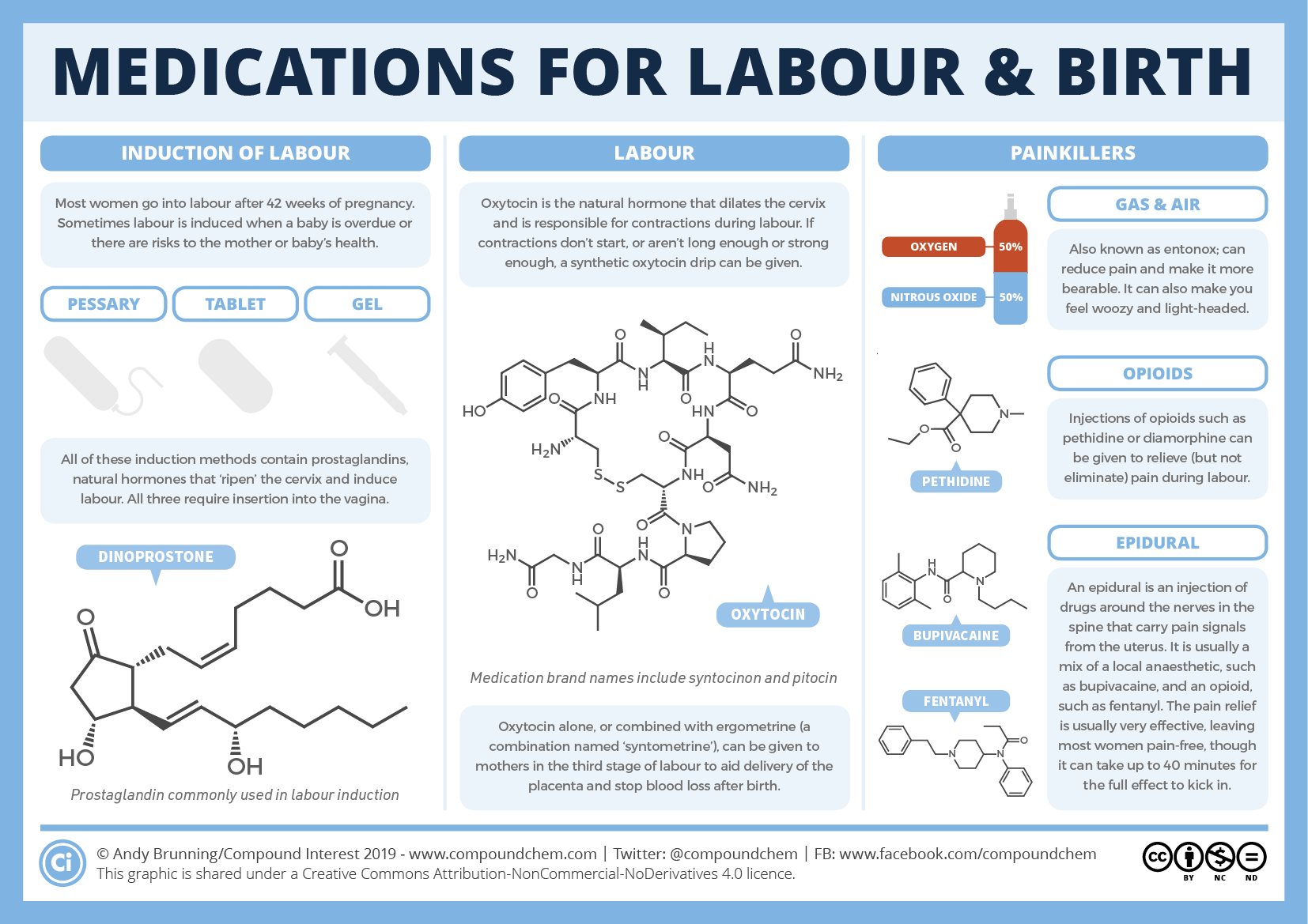 Suppose that in some rare cases this will happen, but in most cases she will still have an abortion, only this time unofficially - where she can be found, from someone who agrees. And then she will try to terminate the pregnancy. The methods known among women are one more dangerous to health than the other.
Suppose that in some rare cases this will happen, but in most cases she will still have an abortion, only this time unofficially - where she can be found, from someone who agrees. And then she will try to terminate the pregnancy. The methods known among women are one more dangerous to health than the other.
It is no coincidence that doctors, unlike the clergy, are against the ban on abortion. The clergy are partly, so to speak, in the heights, the doctors are on the sinful earth and directly face the consequences of a criminal abortion. Veronika Skvortsova might be glad to meet the desire of the Russian Orthodox Church to ban abortions, but she understands what such a ban will lead to.
It is always useful to take advantage of other people's experience. And such is the experience. On July 9, in Argentina, the Senate held a debate on the abolition of the ban on abortion. There, abortion is allowed only if the woman became pregnant as a result of rape or if her life is in danger. According to the law in force since 1921, both the doctor and the pregnant woman herself are punished for abortion, the dpa news agency points out. From 2007 to 2016, 63 people were convicted under this article in Argentina. The Argentine Ministry of Health estimates that in a country of about 44 million, more than 350,000 illegal abortions occur each year, with about 50,000 women admitted to hospital due to complications resulting from abortions.
According to the law in force since 1921, both the doctor and the pregnant woman herself are punished for abortion, the dpa news agency points out. From 2007 to 2016, 63 people were convicted under this article in Argentina. The Argentine Ministry of Health estimates that in a country of about 44 million, more than 350,000 illegal abortions occur each year, with about 50,000 women admitted to hospital due to complications resulting from abortions.
The majority of the population of Argentina is Catholic. Catholicism does not allow abortion. Nevertheless, the Chamber of Deputies approved the initiative to legalize abortion in the first 14 weeks of pregnancy. In the Senate, after a stormy 16-hour discussion, the bill was rejected by a small majority. During the debate, tens of thousands of people gathered outside the Senate building, after the announcement of the results of the vote, the crowd went berserk, so that the police had to use tear gas.
At the end of May, the majority of the population of another traditionally Catholic country, Spain, voted for the abolition of the abortion ban.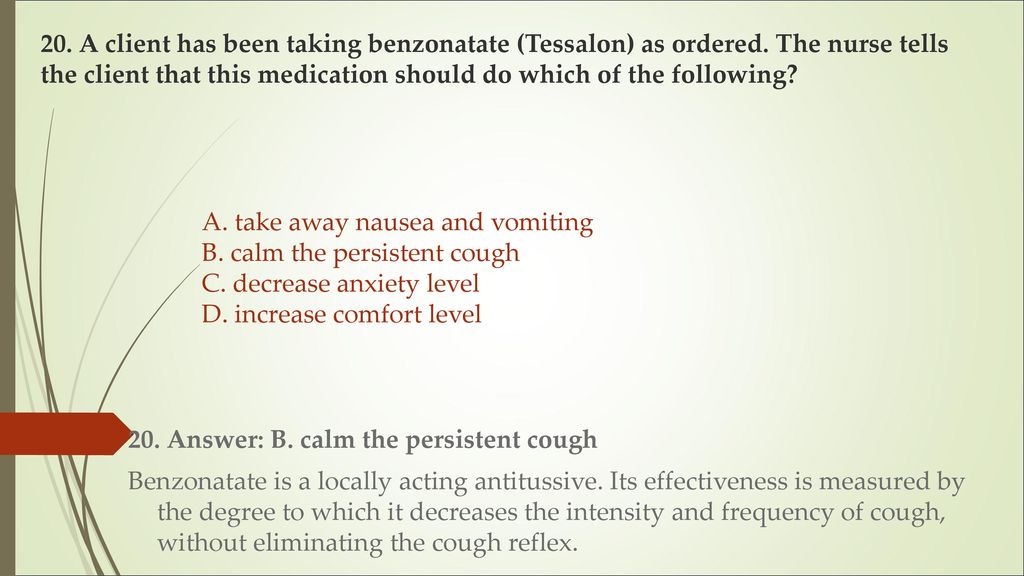
On the other hand, there are quite a few opponents of abortion in the world, and very aggressive ones at that. In our country, where universal atheism was suddenly replaced by demonstrative religiosity, some doctors also declare that their convictions do not allow them to perform abortions. And recently in England, medical school students refused to teach the part of gynecology that talks about abortion. The decision was made tolerant, but decisive: if you don't want to, don't study, but you won't get a diploma without such knowledge.
Abortion is not fun. Nobody likes it. For a woman - a lot of stress. However, this is the lesser of evils for a woman who has decided not to have a baby. Educational events and lectures on the happiness of motherhood, as explained, do not work. Maybe it's better to educate how to prevent unwanted pregnancy?
what it is and how to know if you are a victim of it
When hearing the phrase “reproductive abuse” for the first time, some people think that it is about the brutal actions of midwives during childbirth (this is part of obstetric violence). But the term doesn't really refer to what happens in the hospital, but to a whole range of things that happen long before a baby is born. Let's sort it out in order.
But the term doesn't really refer to what happens in the hospital, but to a whole range of things that happen long before a baby is born. Let's sort it out in order.
A number of experts propose to divide reproductive violence into two types. In the first, we are dealing with violence at the state level. If in some country a woman cannot have an abortion of her own free will, then this is just such a case. For example, today abortion is legally prohibited in Angola, Bangladesh, Egypt and many other countries (most often, exceptions are possible only if the pregnancy poses a threat to the life of a woman, but in general, abortion is likened to murder).
Termination of pregnancy is currently permitted in the Russian Federation and is included in the system of compulsory medical insurance. Abortions can be performed at the request of a woman at an early stage, up to the 12th week, as well as for medical reasons at any time during pregnancy. But under pressure from pro-lifers and some church organizations, the topic is regularly discussed in society that it is time to ban abortions or at least stop paying for them in the CHI system.
But under pressure from pro-lifers and some church organizations, the topic is regularly discussed in society that it is time to ban abortions or at least stop paying for them in the CHI system.
So the legal norms in this matter may still change: for example, in 2011, a draft law was introduced in the State Duma stating that in order to undergo an abortion procedure, a woman must bring her husband's consent to doctors. But in the end, the deputies, we must give them their due, this innovation was nevertheless rejected.
The second type of reproductive violence is violence within a family or within a couple: this group includes a whole range of actions - from annoying comments by relatives to a woman that the clock is ticking and it's time to give birth (here we are rather talking about reproductive pressure) to contraceptive sabotage and forced abortion. Reproductive violence can be committed by both men and women. Previously, a woman was often condemned in society (“she flew in to keep a man”), but today we are increasingly convinced that reproductive violence is often done by men, as well as other relatives, who force women to have children with their remarks and behavior.
Knowing the specifics of our country, I have to add that somewhere between these two types is the reproductive pressure of doctors. Unfortunately, many gynecologists offer the “give birth” treatment option as a universal cure for all problems (do not believe it - three years after the birth, these same doctors will say that now you have all the diseases from childbirth). We do not want to generalize and say that all doctors, without exception, adhere to such an ideology, but there are still many similar cases in the vastness of the Russian Federation.
Psychological pressure can be called a mild form of reproductive violence in the family: for example, a partner sends hundreds of photos of smiling babies in a messenger, and potential grandparents sing songs all day long about how they would like to have grandchildren.
In a severe form of family reproductive violence, it becomes physical from a purely psychological one. This type includes not only rape, but also beatings - a woman can be swung at because she does not want to have children or because she became pregnant with a child of the wrong sex, which was expected in the family.
This type includes not only rape, but also beatings - a woman can be swung at because she does not want to have children or because she became pregnant with a child of the wrong sex, which was expected in the family.
Another type of reproductive violence within a couple is contraceptive sabotage. There are quite a few options here too. The partner may try to dissuade the woman from using contraception during sex. He may refuse to wear a condom on principle. Or he can convince a woman that her health / mood will deteriorate from hormonal remedies / a third leg will grow (underline as necessary). Or a man may hide oral contraceptives or substitute other pills for them. Contraceptive sabotage is dangerous because it often takes place in a hidden form. The classic practice is to pierce condoms. But the secret always becomes clear, and sometimes it is even criminally punishable. So in Germany in 2018, for the first time, a man was convicted of taking off a condom during intercourse without warning his partner.
It is important to say that reproductive violence within the family is about power, not about sex. If a woman has not been able to conceive naturally, she may be forced to undergo an endless number of IVF procedures. And, of course, they can force not only to become pregnant, but also to have an abortion. What is important is not the result, but who owns the right to control the issue of "to give birth or not to give birth."
Unfortunately, studies show that between 8 and 30 percent of women experience some form of reproductive violence. Some of them begin to use an intrauterine device, someone buys birth control pills in other countries so that a man cannot understand what kind of medication his partner is taking. Many respondents say that, faced with reproductive violence, they lacked the sensitive attitude of doctors and their support.
The American Foundation for the Fight against Domestic Violence in 2010 urged gynecologists to pay more attention to this problem when examining women.