Baby induced at 37 weeks
Medical reasons for inducing labor
Topics
In This Topic
KEY POINTS
Inducing labor (also called labor induction) is when your provider gives you medicine or breaks your water to make labor start.
Your provider may recommend inducing labor if your health or your baby’s health is at risk or if you’re 2 weeks or more past your due date.
Inducing labor should only be for medical reasons. If your pregnancy is healthy, it’s best to wait for labor to start on its own.
If your provider recommends inducing labor, ask about waiting until at least 39 weeks to be induced so your baby has time to develop in the womb.
What is inducing labor?
Inducing labor (also called labor induction) is when your health care provider gives you medicine or uses other methods, like breaking your water (amniotic sac), to make your labor start. The amniotic sac (also called bag of waters) is the sac inside the uterus (womb) that holds your growing baby. The sac is filled with amniotic fluid. Contractions are when the muscles of your uterus get tight and then relax. Contractions help push your baby out of your uterus.
Your provider may recommend inducing labor if your health or your baby’s health is at risk or if you’re 2 weeks or more past your due date. For some women, inducing labor is the best way to keep mom and baby healthy. Inducing labor should be for medical reasons only.
If there are medical reasons to induce your labor, talk to your provider about waiting until at least 39 weeks of pregnancy. This gives your baby the time she needs to grow and develop before birth. Scheduling labor induction should be for medical reasons only.
What are medical reasons for inducing labor?
Your provider may recommend inducing labor if:
- Your pregnancy lasts longer than 41 to 42 weeks. After 42 weeks, the placenta may not work as well as it did earlier in pregnancy.
 The placenta grows in your uterus (womb) and supplies your baby with food and oxygen through the umbilical cord.
The placenta grows in your uterus (womb) and supplies your baby with food and oxygen through the umbilical cord. - Your placenta is separating from your uterus (also called placental abruption) or you have an infection in your uterus.
- Your water breaks before labor begins. This is called premature rupture of membranes (also called PROM).
- You have health problems, like diabetes, high blood pressure or preeclampsia or problems with your heart, lungs or kidneys. Diabetes is when your body has too much sugar (called glucose) in your blood. This can damage organs in your body, including blood vessels, nerves, eyes and kidneys. High blood pressure is when the force of blood against the walls of the blood vessels is too high and stresses your heart. Preeclampsia is a serious blood pressure condition that can happen after the 20th week of pregnancy or after giving birth (called postpartum preeclampsia).
- Your baby has a stopped growing. Or your baby has oligohydramnios.
 This means your baby doesn’t have enough amniotic fluid.
This means your baby doesn’t have enough amniotic fluid. - You have Rh disease and it causes problems with your baby’s blood.
What are the risks of scheduling labor induction for non-medical reasons?
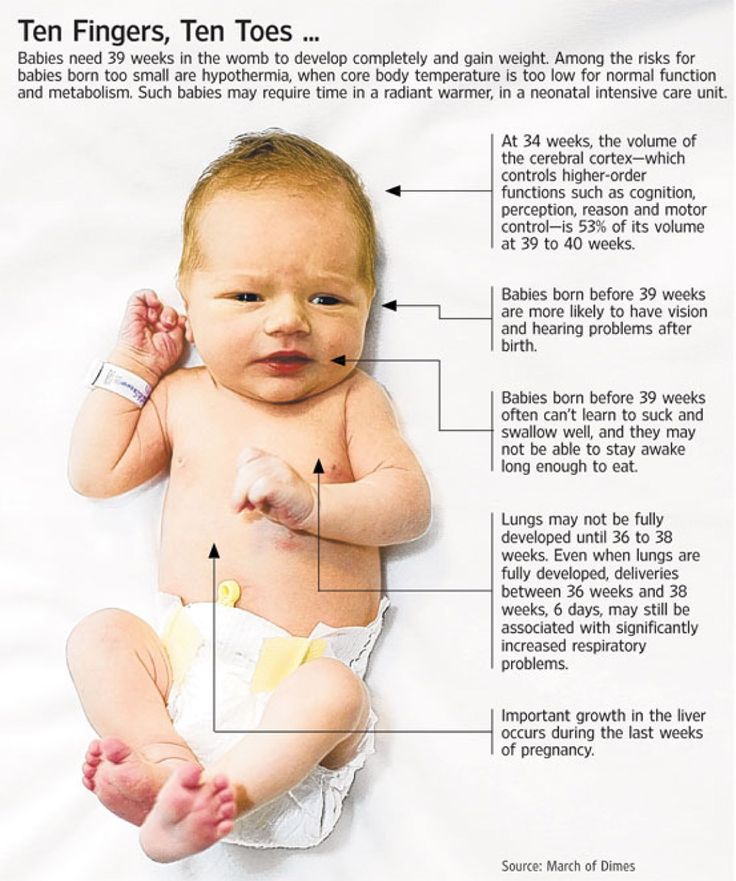
Scheduling labor induction may cause problems for you and your baby because your due date may not be exactly right. Sometimes it’s hard to know exactly when you got pregnant. If you schedule labor induction and your due date is off by a week or 2, your baby may be born too early. Babies born early (called premature babies) may have more health problems at birth and later in life than babies born on time. This is why it’s important to wait until at least 39 weeks to induce labor.
If your pregnancy is healthy, it’s best to let labor begin on its own. If your provider talks to you about inducing labor, ask if you can wait until at least 39 weeks to be induced. This gives your baby’s lungs and brain all the time they need to fully grow and develop before he’s born.
If there are problems with your pregnancy or your baby’s health, you may need to have your baby earlier than 39 weeks. In these cases, your provider may recommend an early birth because the benefits outweigh the risks. Inducing labor before 39 weeks of pregnancy is recommended only if there are health problems that affect you and your baby.
If your provider recommends inducing labor, ask these questions:
- Why do we need to induce my labor?
- Is there a problem with my health or the health of my baby that may make inducing labor necessary before 39 weeks? Can I wait to have my baby closer to 39 weeks?
- How will you induce my labor?
- What can I expect when you induce labor?
- Will inducing labor increase the chance that I'll need to have a c-section?
- What are my options for pain medicine?
Last reviewed: September, 2018
See also: 39 weeks infographic
') document. write('
write('
Nutrition, weight & fitness
') document.write('') }
') document.write('') }
Induction at 37 Weeks: The Why's and How's
Having a labor induction before or at 37 weeks is something each pregnant woman and her partner should consider carefully. This article will review WHY you might want/need to be induced, how it might happen, and why you might want to wait if possible.
How do I know about inductions?
Hi, I’m Hilary — The Pregnancy Nurse 👩⚕️. I have been a nurse since 1997 and I have 20 years of OB nursing experience, I am also the curly head behind Pulling Curls and The Online Prenatal Class for Couples. 🩺 I have helped thousands of families start and deliver via inductions, so it’s something I REALLY understand.
In fact, I have so many people asking for more information I made a mini class that is aimed to get you prepared for your induction.
The objectives of this quick class (only takes 15-30 minutes) are:
- Chat about what an induction is (and what a MEDICAL induction is)
- How inductions happen at the hospital (including cytotec and a few other ways)
- What to expect from an induction
- The outcomes of an induction
It’s SUPER helpful — I love what Sarah said about my teaching:
Her very approachable, down to earth personality made the course feel personal and easy to watch
Anyway, it’s priced for any couple to be able to afford it — I hope you’ll come join me!
Medical Reasons for an Early Induction
Full term for a pregnancy is 40 weeks of pregnancy, so a 37 weeks (or before) induction is pretty early.
While 3 weeks might not SEEM like a long time, when you are trying to create an entire human inside your body, every hour counts.
Also, something to keep in mind is that even early ultrasounds are not 100% accurate. Most predict your due date plus or minus 2 weeks. Which means at a point where you think you are 37 weeks, you could actually be 35 or 39 weeks (and anywhere in between). Which could be a big difference!
Most predict your due date plus or minus 2 weeks. Which means at a point where you think you are 37 weeks, you could actually be 35 or 39 weeks (and anywhere in between). Which could be a big difference!
This early, you’d want to be sure to get informed consent before scheduling an induction. That means you understand the potential risks, benefits, and any alternatives of the procedure. That way you can make an informed decision.
This early, you would be induced mainly if your health or the health of your baby was severely impacted.
Baby is Too Small
This is also known as IUGR (intra-uterine growth restriction) or SGA (small for Gestational Age). At this point in time for this early of an induction, you would likely have had several ultrasunds that would chart that the baby in’t growing well (or blood flow studies called doppler scans) that show baby isn’t getting enough blood flow.
They do often induce for big babies, but rarely would they do that at 37 weeks.
Cholestasis of Pregnancy
This is where the bile duct is blocked. Women often have a rash/itchiness on belly and abdomen. Your health care provider would then order bile salts tested to see if that is the issue.
Because there is a high incidence of stillbirths, depending on the severity of you blockage, they can induce at 37 weeks.
FYI, once baby is delivered the rash/itching usually goes away.
Learn more about cholestasis here.
Too Little Amniotic Fluid in the Amniotic Sac
If they do an ultrasound (often what’s called a BPP — and I go into most of the 3rd trimester testing in this free course) they might find that you don’t have enough fluid.
This can be problematic as fluid gives the baby and umbilical cord more room in the womb.
There are ways to try to increase the fluids. We find many women are severely dehydrated (especially since I practice in Phoenix) and fluids can help you get closer to full term.
If your water breaks before 37 weeks it would be considered premature rupture of membranes (PROM), and they’d decide if they should induce contractions or wait to see if baby can grow more in a healthy environment. Keeping in mind that there is always an increased risk of infection once your water breaks.
Keeping in mind that there is always an increased risk of infection once your water breaks.
Preeclampsia
Preeclampsia is a smooth muscle disorder that is diagnosed through lab work and blood pressures taken at rest. Most often is is characterized by high blood pressure found in the doctors office.
The only way to cure it is to deliver the baby and the placenta.
It can cause issues (including seizures) and can restrict the baby’s growth similar to IUGR if not taken care of. While they would proabably prefer you got closer to 38 weeks, sometimes they will induce you at 37 weeks.
Learn more about preeclampisa on my sister site.
Gestational hypertension would also be a reason for an early induction if it can not be controlled with medication. That is high blood pressure, without the other lab indictors that it is preeclampsia.
Diabetes
Diabetes is a very common reason for an early induction.
There are two types of diabetes. Both of which are tested for by the glucose test.
Both of which are tested for by the glucose test.
Gestational Diabetes
This is diabetes that happens just during pregnancy. Some people are diagnosed early on or at around 30 weeks.
Most women, if controlled, can go past 37 weeks but if their sugars aren’t controlled they might need to be induced early.
Type 1 or Type 2 diabetic
These people have had diabetes before pregnancy and will continue to have it afterwards as well. Their body has more health-related concerns, and they will often be induced ahead of time.
Previous Stillborn
Having a previous stillborn baby can be a reason for an early delivery. While 37 week is pretty early, it can be the best option for maternal and fetal well being.
A history of a stillborn makes your entire pregnancy different. Doctors are aware you’ll be extra nervous.
Other Reasons
While these are some of the most common reasons, there are other reasons for an induction of labor including congenital anomalies they found on the ultrasound, issues with the baby’s heart rate and other medical conditions.
There are other reasons you might be induced. I go into the vast majority in my full online prenatal course.
An elective induction (an induction without a medical indication) should not happen at 37 weeks. ACOG (American College of Obstetricians — their professional organization in the USA) recommends against it, it can put both mom and baby at an increased risk.
Remember the main reason they would induce you early is if staying in the womb would be bad for baby’s health.
Making the choice to HAVE an induction is SO important. It is one of the objectives to help you with in my Induction Mini-Class. Come join us at a great price!
How They Induce You at 37 Weeks
An induction of labor is meant to start uterine contractions. They can do that in a variety of ways (your particular induction process will depend on doctor’s preference and your initial cervical exam):
Manual Induction Methods
There are couple of manual induction methods (manual meaning something physical happens to your cervix):
Foley Bulb
As long a your cervix is open enough that they can get the tube in, they can insert a foley bulb.
That’s basically a tube with a balloon at the end. They fill the balloon with water and that manually opens the cervix with time.
Normally, it goes in for 12 hours. Some doctors will place it in the office, and some place it in the hospital.
It is mildly uncomfortable, but it isn’t too invasive.
Rupture Your Amniotic Fluid Bag
Your doctor can rupture your membranes (break your amniotic fluid sac) to see if that will get labor started. Most often, at 37 weeks this isn’t enough to get you going. Often, once you have had a cervical ripening agent (see below) they will break your water after that to hurry things along.
While many people include a membrane sweep in the manual induction methods, it is not usually chosen for an early induction because it isn’t very effective at putting you into labor and we need to choose something more likely to work (and more controlled).
Cervical Ripening Methods
This means that your cervix is less than 3 cm and needs to ripen (yes, like fruit) so that it will open up as we make you have harder/faster contractions.
All of these start with smaller contractions and don’t normally put you into labor on their own (but sometimes they do). The idea is to give these medications until your cervix is 3 centimeters and then we move to Pitocin (see below).
Misoprostil / Cytotec
This is a small pill that is given orally, placed by your gums/under your tongue to disolve or vaginally.
Prepedil
This is a gel we place in your vagina. It’s similar to a Monistat plunger I have used for a yeast infection before.
Cervidil
This is like a tiny flattened tampon (or a tiny stiff tea bag) that is placed in your vagina next to your cervix for 12 hours and then removed.
Induction Methods
Pitocin is the main induction method. It can also be given before the cervical ripening agents — it is up to your doctor.
Pitocin is the synthetic form of oxytocin, the hormone that makes your uterus contract.
It is given in the IV and is more high risk than the other method. Your blood pressure and fetal well being are more frequently assessed with pitocin (and you will need to be monitored continuously).
Your blood pressure and fetal well being are more frequently assessed with pitocin (and you will need to be monitored continuously).
All that being said, we use pitocin frequently in labor and delivery, it isn’t unusual at all — and we are educated on how to use it safely. I have a whole article on Pitocin inductions.
I know, that last section was a lot, and seems pretty complicated. This class has a video where I walk you through all the ways they could induce you. It’s really pretty simple once someone with a lot of experience breaks it down for you.
What to expect at an induction
An early induction is usually a bit of an “uphill” battle as your cervix and mother nature are not normally on your side (this is totally different if you go into labor that early on your own).
Bishop’s Score
This is a method of ranking how conducive to an induction your cervix is. It takes into account how many centimeters you are, how soft your cervix is and how effaced (or thin) it is. I go into all the info on vaginal exams in this post on my other site.
I go into all the info on vaginal exams in this post on my other site.
While a low bishop’s score wouldn’t stop us from inducing someone who really needed it done, it can tell you how long it might take, and that information is worth discussing with your doctor. A low bishop’s score before an induction would be a risk factor for a caesarean section instead of a vaginal delivery.
And yes, understanding how the bishop’s score applies to you is part of this.
How long will a 37 week induction take?
The textbook case once you are in labor is 1 centimetre per hour plus 2 hours of pushing on your first baby (much less on subsequent babies).
However, that only starts once you’re IN labor. That means your cervix is actively opening. That might take a while to get mother nature on your side with medication (and cervical softening by the agents we listed above).
Risks of an early induction
The risk of an early induction is similar to the risks of induction at any stage.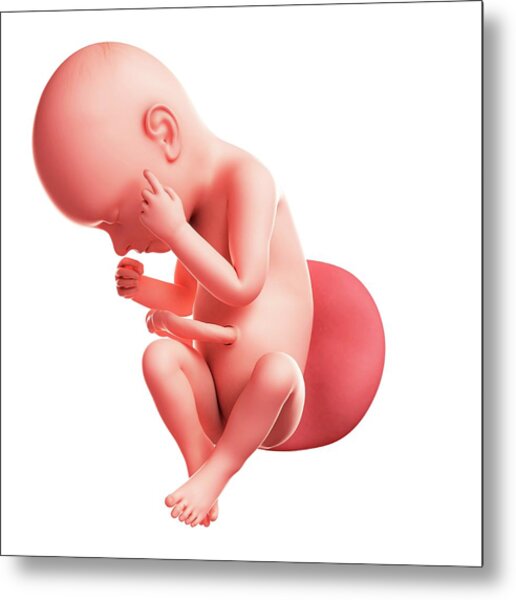 Once you add any intervention at any stage it does increase the risks.
Once you add any intervention at any stage it does increase the risks.
Your induction is also likely to be lengthier than an average induction where someone is closer to 40 weeks gestation.
AND, there is always the chance it will fail and you will need a cesarean section. With an elective induction, there is always the chance that if you fail you can go home and wait a few days, possibly try again. If you NEED the baby out, they will need to do a cesarean section.
Why Not to Get Induced at 37 Weeks
Going full term is best for you and your baby, if your doctor recommends an induction early, be sure to understand why and if it can be pushed later.
Remember that “natural labor” (some people use that term to mean labor with less interventions) does put you at a lower risk for complications, and potential risks — so we try to aim for that when possible.
Remember that you think you are 37 weeks, but you could be just 35 weeks, and baby’s lungs might not be ready to breathe in the air (which is always a risk of an early induction).
If you and your provider decide that an induction of labor is not in your best interest, please don’t try “natural ways” like spicy food, castor oil, or nipple stimulation. There is a reason your baby is inside, and it would be best to not try and induce yourself (and I NEVER recommend castor oil, and I think spicy food just gives you heartburn).
However, if you go into spontaenous labor around 37 weeks, we most often have good outcomes.
Ok, I KNOW you think you’re prepared after reading this article — but I promise you that you need someone who takes you from how to make the decision to possible induction outcomes. This class does just that in about 30 minutes time you can be prepared!
Don’t waste your time combing the internet for more info — come join that class with all of it in one place.
Or, join The Online Prenatal Class for Couples where I can prepare you in just 3 hours for your WHOLE birth. The choice is up to you!
And, if you’re not quite sure you’re ready for that whole thing, check out my free prenatal class. It’s your first step toward getting in the driver’s seat of your birth.
It’s your first step toward getting in the driver’s seat of your birth.
- About the Author
- Latest Posts
Hilary Erickson, BSN RN
A nurse since 1997, she has worked in various fields including pediatrics, geriatrics & hospice.
She has 20 years of labor and delivery experience in the San Jose, CA and Phoenix, AZ areas.
She is also the curly head behind the website Pulling Curls and is the creator of The Online Prenatal Class for Couples — the #1 hospital-based prenatal class on the internet.
37-40 weeks of pregnancy
37th week of pregnancy for a baby
At 37 weeks of gestation, the baby is approximately 48 cm tall and weighs 2,600 g. facial features, pronounced cartilage tissue. The accumulation of subcutaneous fat at this stage of pregnancy makes the outline of the body softer and more rounded. The skin of the child is gradually smoothed out, it is no longer as pink as in the previous weeks of intrauterine development, the integument gradually brightens. The body of the baby is still abundantly covered with grease, but the amount of fluff is noticeably reduced, fluff hair remains only on the shoulders and back, in some babies they disappear almost completely.
The body of the baby is still abundantly covered with grease, but the amount of fluff is noticeably reduced, fluff hair remains only on the shoulders and back, in some babies they disappear almost completely.
Fat accumulation continues this week. It reaches a maximum of 15% of the total body weight of the child. It is difficult to overestimate the importance of adipose tissue for newborns, it is it that protects the child from overheating or hypothermia, since the baby's thermoregulation system after childbirth is still not sufficiently formed and continues to develop in the first months of a small person's life.
At this time, not only the volume of subcutaneous fat increases, but muscles and skeleton also develop intensively. The child constantly moves arms and legs. These unique workouts help increase muscle mass. Also, the baby makes rhythmic respiratory movements that strengthen the intercostal muscles and the diaphragm, and prepare the respiratory organs for childbirth.
Pregnant woman at 37 weeks
As the due date approaches, pregnant women begin to notice the appearance of their precursors, that is, certain signs, changes that occur under the influence of hormones. The body of a woman is preparing to give birth to a child, progesterone gives way to the dominant role of the birth hormone estrogen, the state of health of the pregnant woman changes.
From the 37th week expectant mothers can observe the following changes:
- slight weight loss;
- abdominal shrinkage;
- the appearance of training or "false" contractions and the increase in their intensity;
- discharge of mucus from the cervix.
The nature of the stool changes, it becomes looser, aching pains in the lower back of varying intensity may appear, the fundus of the uterus descends. A woman notes some signs on her own, others are observed by a gynecologist during a routine examination.
Harbingers do not appear in all women. Some expectant mothers notice only some of the above symptoms, while others observe signs of an impending birth not two or three weeks before their date, but just a few hours. Both the appearance of precursors at the 37th week and their absence are a variant of the norm and depend on the individual characteristics of the woman's body.
Some expectant mothers notice only some of the above symptoms, while others observe signs of an impending birth not two or three weeks before their date, but just a few hours. Both the appearance of precursors at the 37th week and their absence are a variant of the norm and depend on the individual characteristics of the woman's body.
This week the woman's body is intensified preparation for the birth of a child. If the fetus is located correctly, head down, it gradually descends, goes to the lower part of the uterus, presses to the body and bends the limbs, intuitively taking the most comfortable position for passing the birth canal. The consequence of the movement of the fetus is the omission of the bottom of the uterus. The abdomen drops, the pressure on the diaphragm significantly decreases, the pregnant woman can breathe easily, the shortness of breath that haunted her in previous weeks disappears. The pressure on the stomach also decreases, heartburn disappears, a feeling of heaviness after eating and other unpleasant sensations. Moving the baby can put pressure on the bowels and bladder. A pregnant woman at this time often experiences the urge to urinate, may suffer from frequent loose stools. The reason for frequent bowel movements is not only the mechanical effect of the uterus on it, but also an increase in the content of estrogens in the body, hormones that contribute to the excretion of fluid. At the 37th week, the expectant mother can empty her intestines up to 3-4 times a day and at the same time observe a significant liquefaction of feces.
Moving the baby can put pressure on the bowels and bladder. A pregnant woman at this time often experiences the urge to urinate, may suffer from frequent loose stools. The reason for frequent bowel movements is not only the mechanical effect of the uterus on it, but also an increase in the content of estrogens in the body, hormones that contribute to the excretion of fluid. At the 37th week, the expectant mother can empty her intestines up to 3-4 times a day and at the same time observe a significant liquefaction of feces.
38th week of pregnancy: the development of the future baby
At the 38th week, the fetus is fully formed, so childbirth at this time is no longer dangerous for both the mother and the baby. The weight of the fetus is about 3 kg, but this indicator can vary significantly for different babies, the weight depends on the individual characteristics of the mother and child, the structural features of the body and other factors. The body length of a newborn is approximately 50 cm.
All organs and systems at 38 weeks of age are characterized by physiological and morphological maturity, they are fully ready for work. At this time, the child prepares for childbirth, makes respiratory movements and prepares the intercostal muscles for breathing. The tissues of the lungs are bathed in amniotic fluid, which helps maintain the right level of surfactant that coats the baby's lungs from the inside. All elements of the respiratory system are ready for use. With the first breath after birth, the alveoli begin to transfer oxygen from the air to the blood, gas exchange occurs, the respiratory and circulatory systems begin to work intensively.
Pregnant woman
The body of a pregnant woman continues to actively prepare for the birth of a baby, the estrogen content rapidly increases, and the progesterone level decreases significantly. A change in the hormonal background contributes to the softening of the tissues of the birth canal and cervix. Throughout pregnancy, the lumen of the cervical canal is closed by a plug of thick mucus, which protects the baby from infection, and the uterine cavity protects against the penetration of microorganisms dangerous to health. In the last weeks of pregnancy, the consistency of the mucus changes, it becomes more liquid and begins to gradually flow out. In some women, mucus leaves gradually, while in other women in labor at the same time. The discharge resembles colorless egg white in its consistency and appearance. Sometimes the mucus is colored pinkish, brown or yellow. The discharge of the cork is painless, a woman may experience a slight feeling of discomfort in the lower abdomen. More abundant vaginal discharge than during the entire pregnancy can signal the passage of the cork.
In the last weeks of pregnancy, the consistency of the mucus changes, it becomes more liquid and begins to gradually flow out. In some women, mucus leaves gradually, while in other women in labor at the same time. The discharge resembles colorless egg white in its consistency and appearance. Sometimes the mucus is colored pinkish, brown or yellow. The discharge of the cork is painless, a woman may experience a slight feeling of discomfort in the lower abdomen. More abundant vaginal discharge than during the entire pregnancy can signal the passage of the cork.
A woman should carefully monitor the color and volume of discharge, since too much colorless discharge may indicate not only the cork has come off, but also be one of the symptoms of amniotic fluid leakage. Indicator pads and amnio tests or test strips will help determine the cause of the discharge. Pads are sold in many pharmacies and can be easily used at home. If amniotic fluid leakage is confirmed, you should immediately consult a doctor.
After the mucus plug has passed, you should stop visiting the pool and swimming in open water, as the risk of infection of the child increases significantly. It is also necessary to exclude sexual contact.
39th week of pregnancy: what happens to the fetus?
At 39 weeks, the baby weighs 3100-3500 g and is 50-52 cm tall. Height and weight are very relative and can vary significantly. The baby is rapidly preparing for the most important test of his life - birth, which requires endurance and considerable effort. During this period of pregnancy, the size and weight of the child's adrenal glands, that is, the glands of the endocrine system, which are responsible for the reaction of the human body to stress factors, increase. It is the hormones adrenaline and norepinephrine produced by the adrenal glands that help the child quickly adapt to new temperature conditions, tactile, sound and light impulses.
All the senses of the baby are developed at 39 weeks. Within a few moments after birth, the baby can focus his eyes, he reacts to bright light and moving objects, many scientists claim that newborns distinguish colors, see the faces of parents and doctors. The hearing of the baby in the last weeks of intrauterine life is also fully developed; after birth, he reacts to loud sounds and noise. A newborn baby is able to determine the main shades of taste, recognize sour, bitter, sweet and salty.
The hearing of the baby in the last weeks of intrauterine life is also fully developed; after birth, he reacts to loud sounds and noise. A newborn baby is able to determine the main shades of taste, recognize sour, bitter, sweet and salty.
In the womb, the baby is in an aquatic environment that minimizes contact. Immediately after birth, the baby experiences many tactile sensations, unlike intrauterine life, he feels the touch of his mother's hands and diapers, towels, dressings and other materials. Babies especially like the touch of skin to skin, so in a modern maternity hospital, newborns must be laid out on their mother's stomach even before cutting the umbilical cord. The child adapts to the new environment more easily, feels protected. Laying out a child has not only a psychological aspect, since it contributes to the colonization of microorganisms from the mother's skin to the skin and mucous membranes of the baby, and increases its immunity.
Pregnant woman
In the last weeks of pregnancy, the expectant mother strives to prepare her apartment or house as much as possible for the arrival of a new family member. Scientists call this sign of impending birth the nesting syndrome. Many women observe signs of the syndrome from the thirtieth week of pregnancy, however, nesting reaches its maximum point at the 39-40th week. Pregnant women tend to do general cleaning and repairs, re-paste the wallpaper and purchase a lot of new things that, in their opinion, are simply necessary in the house. After giving birth, many purchases are puzzling. The reason for this behavior is an increase in the level of adrenaline and norepinephrine in the body. These hormones are produced by the adrenal glands, they are necessary not only for the woman, but also for the baby to prepare for the upcoming birth.
Scientists call this sign of impending birth the nesting syndrome. Many women observe signs of the syndrome from the thirtieth week of pregnancy, however, nesting reaches its maximum point at the 39-40th week. Pregnant women tend to do general cleaning and repairs, re-paste the wallpaper and purchase a lot of new things that, in their opinion, are simply necessary in the house. After giving birth, many purchases are puzzling. The reason for this behavior is an increase in the level of adrenaline and norepinephrine in the body. These hormones are produced by the adrenal glands, they are necessary not only for the woman, but also for the baby to prepare for the upcoming birth.
40th week of pregnancy: how does the baby develop?
40 weeks - term pregnancy. The weight of a child who was born at such a period ranges from 2,600 g to 4,400 g, and his body length is 48-53 cm. These indicators are very arbitrary, since miniature babies weighing 2,600 g and real heroes are born at 40 weeks, whose body weight approaches 5,000 g. The length of the newborns can also vary from 45 to 55 cm.
The length of the newborns can also vary from 45 to 55 cm.
Most women give birth exactly at 40 weeks. At this time, the baby is completely ready for birth, it meets all the parameters of a full-term baby. Before childbirth, the child closely presses the arms and legs to the body, bends the head as much as possible and presses against the exit from the uterus. This position allows you to make it possible to pass the birth canal with the narrowest part of the skull. In the course of labor, with each contraction, the child gradually moves down, he does not move in a straight line, but makes helical-translational movements, as if screwing into the mother's birth canal. During the progress of the newborn, the complete descent of his head, the cervix fully opens. This is followed by attempts, that is, contractions of the uterus, which advance the child through the birth canal. Gradually, the head of the baby is shown, and after it - his torso. Childbirth is a complex mechanism that is aimed not only at the safe passage of the birth canal by the child, protecting him from accidental injuries due to increased pressure, but also at preventing ruptures of the woman's soft tissues.
Pregnant woman
The long wait for meeting her unborn child is coming to an end, and the 40th week of pregnancy is the last for most women. Every day, the anxiety of the expectant mother increases, a long wait affects the mood and well-being. Women strive to have a baby as soon as possible so that pregnancy and painful contractions are a thing of the past. Every pregnant woman dreams of meeting a baby, wants to hug him to her chest and stroke the delicate head.
Many women, especially primiparas, are afraid that labor will begin unnoticed, but such cases are extremely rare. A woman feels the onset of childbirth, feels regular contractions, which are repeated at regular intervals and gradually increase, the time interval between them is reduced.
Labor may be preceded by prenatal rupture of amniotic fluid, which occurs in a certain percentage of women in labor. After the waters break, contractions may be quite weak or completely absent. Regardless of the intensity of contractions, the outpouring of water is one of the signs of the onset of labor and requires immediate contact with specialists, hospitalization of a woman in a maternity hospital or hospital, since when the water breaks, the integrity of the bladder is violated and the risk of penetration of microorganisms dangerous to the health of the child increases into the uterine cavity. It is important that after the water breaks, the baby is born in a maximum of 10-12 hours.
It is important that after the water breaks, the baby is born in a maximum of 10-12 hours.
A pregnant woman should properly tune in to childbirth, concentrate on the desired result and believe in her own strength, fulfill the task assigned to her by nature. The right psychological attitude and theoretical knowledge will help a woman become a mother, successfully go through all the stages of childbirth and press the long-awaited child to her heart.
Induction of labor in women with normal pregnancies of 37 weeks or more
Does the policy of inducing labor at 37 weeks of gestation or more reduce the risks for infants and their mothers compared with a policy of waiting until later in pregnancy or until will there be indications for labor induction?
This review was originally published in 2006 and subsequently updated in 2012 and 2018.
What is the problem?
The average pregnancy lasts 40 weeks from the start of a woman's last menstrual period. Pregnancies lasting more than 42 weeks are described as "post-term" and therefore the woman and her doctor may decide to give birth by induction. Factors associated with postnatal pregnancy and delayed delivery include obesity, first birth, and maternal age over 30 years.
Pregnancies lasting more than 42 weeks are described as "post-term" and therefore the woman and her doctor may decide to give birth by induction. Factors associated with postnatal pregnancy and delayed delivery include obesity, first birth, and maternal age over 30 years.
Why is this important?
Protracted (term) pregnancy may increase risks for infants, including a greater risk of death (before or shortly after birth). However, induction (stimulation or induction) of labor can also pose risks to mothers and their babies, especially if the woman's cervix is not ready for delivery. Current diagnostic methods cannot predict risks to babies or their mothers per se, and many hospitals have specific policies regarding how long a pregnancy can last.
What evidence did we find?
We searched for evidence (July 17, 2019) and identified 34 randomized controlled trials in 16 different countries involving more than 21,500 women (mostly at low risk of complications). The trials compared a policy of induction of labor after 41 completed weeks of gestation (>287 days) with a policy of waiting (expectant management).
The trials compared a policy of induction of labor after 41 completed weeks of gestation (>287 days) with a policy of waiting (expectant management).
Labor induction policies were associated with fewer perinatal deaths (22 trials, 18 795 babies). Four perinatal deaths occurred in the induction policy group compared with 25 perinatal deaths in the expectant management group. Fewer stillbirths occurred in the induction group (22 trials, 18,795 infants): two in the induction group and 16 in the expectant management group.
Women in the induction of labor groups in the included studies were probably less likely to deliver by caesarean section than in the expectant management groups (31 studies, 21,030 women), and there was probably little or no difference when compared with assisted vaginal delivery (22 studies, 18,584 women).
Fewer infants were admitted to the neonatal intensive care unit (NICU) in the induction policy group (17 trials, 17,826 infants; high-certainty evidence). A simple test of the baby's health status (Apgar score) at five minutes after birth was likely to be more favorable in the induction groups than expectant management (20 trials, 18,345 infants).
A simple test of the baby's health status (Apgar score) at five minutes after birth was likely to be more favorable in the induction groups than expectant management (20 trials, 18,345 infants).
An induction policy may make little or no difference for women who have had a perineal injury, and likely has little or no effect on the number of women with postpartum hemorrhage or breastfeeding at hospital discharge. We are uncertain about the effect of induction or expectant management on length of stay in the maternity hospital due to the very low certainty of the evidence.
Among newborns, the number of children with trauma or encephalopathy was similar in both groups (moderate and low-certainty evidence, respectively). None of the studies reported the development of neurodevelopmental problems during follow-up of children and postpartum depression in women. Only three trials reported some measure of maternal satisfaction.
What does this mean?
An induction policy compared with expectant management is associated with fewer infant deaths and probably fewer caesarean sections; and probably has little or no effect on assisted vaginal delivery.