Spina bifida unborn babies
Fetal spina bifida - Stanford Medicine Children's Health
The Stanford Medicine Children’s Health Fetal and Pregnancy Health Program’s team of specialists in maternal-fetal medicine, pediatric radiology, neonatology, pediatric neurosurgery, and pediatric surgery provide multidisciplinary evaluation, consultation, and therapy for fetal spina bifida.
What is fetal spina bifida?Spina bifida is a condition that happens when the fetus’s bony spine, which protects the spinal cord and nerves, doesn’t develop normally. The spinal cord and nerves are then exposed to the amniotic cavity, which leads to their ongoing damage during pregnancy. Due to this nerve damage, children with severe forms of spina bifida have difficulty with walking, and with bowel and bladder function.
Spina bifida also can cause the developing brain to herniate into the base of the skull, creating fluid buildup within the brain.
- This herniation is known as a Chiari II malformation, and increased fluid buildup in the brain is called hydrocephalus.
- Children with spina bifida often require a ventriculoperitoneal shunt or endoscopic third ventriculostomy after delivery in order to reduce the fluid in the brain and relieve the pressure that can build up in the skull.
Fetal spina bifida affects 3 to 4 out of 10,000 live births in the United States.
How is spina bifida diagnosed?Spina bifida can be tested with maternal blood tests, but the diagnosis is usually made with an ultrasound.
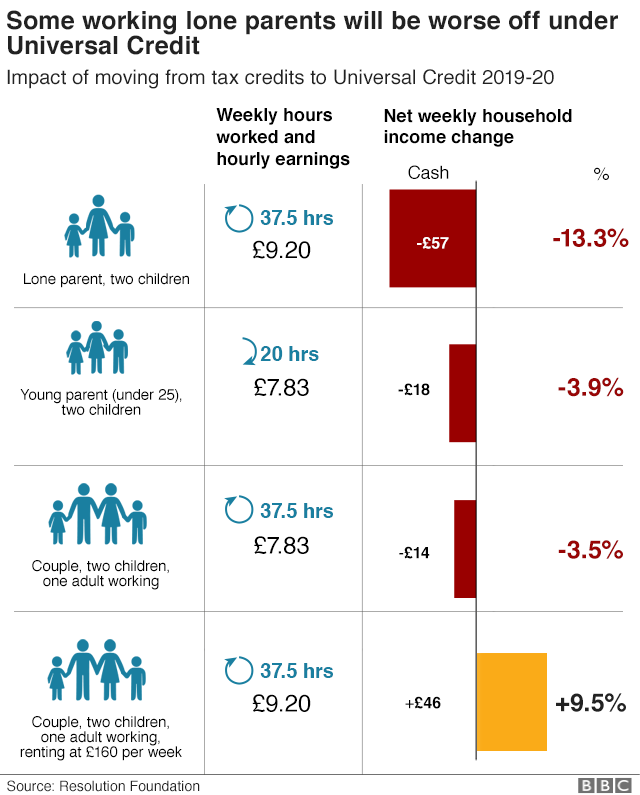
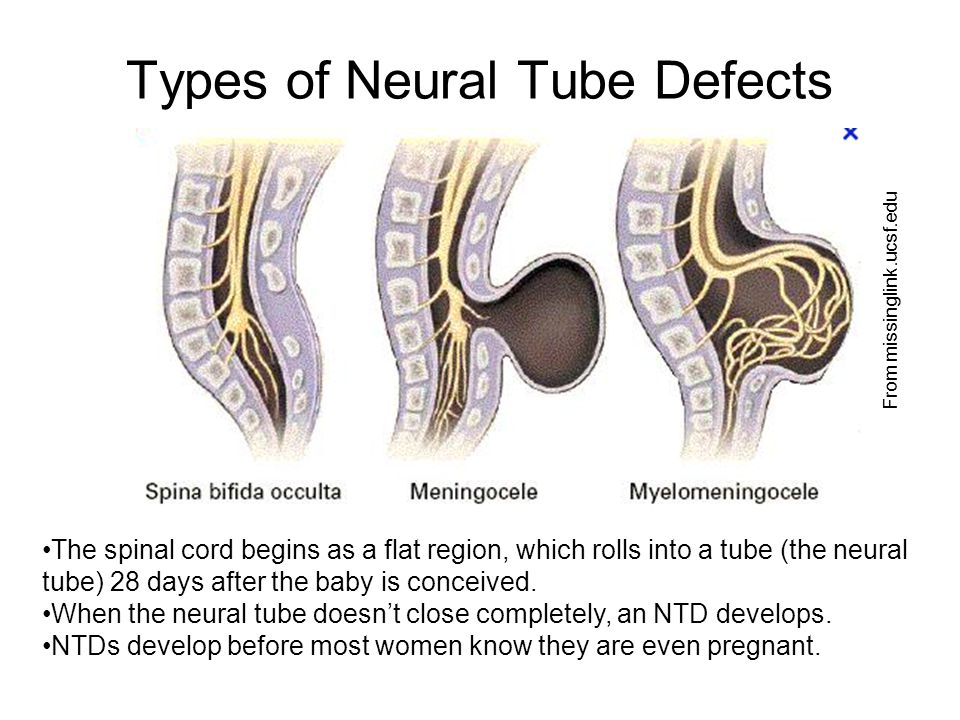
What are the most common types of spina bifida?- Spina bifida occulta. A mild form of spina bifida in which the skin covers the spinal defect, and the spinal cord and the nerves do not herniate into the amniotic cavity. This form of spina bifida may be characterized only by a hairy patch, dimple, or birthmark over the area of the defect after delivery. Some babies with this condition require surgery at 3 to 6 months of age to de-tether the spinal cord.
- Lipomyelomeningocele. A moderate form of spina bifida in which the skin covers the spinal defect, but there is a fatty lump under the skin that is tethered to the spinal cord. Infants with this condition require surgery at 3 to 6 months of age to repair the defect.
- Meningocele. A moderate form of spina bifida in which only a fluid-filled sac herniates outside the spine, and the spinal nerves do not. This condition may require early repair after birth or in the first six months of the patient’s life, depending on the skin overlying the meningocele.
- Myelomeningocele. A severe form of spina bifida in which the nerves herniate through the bony defect outside of the body and are covered by a thin fluid-filled sac. The nerves that are exposed to the amniotic cavity are damaged over time, leading to difficulty walking and problems with bladder and bowel function.
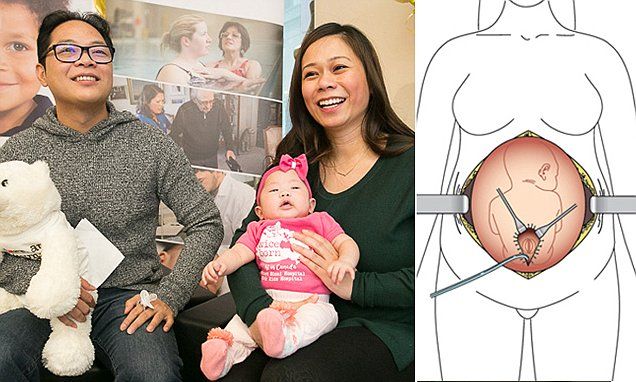
We offer patients in utero spina bifida repair either through open fetal surgery or a minimally invasive fetoscopic approach under a Stanford Institutional Review Board–approved study.
The traditional approach of in utero repair is done through open fetal surgery.
- This approach has been validated using a large prospective clinical trial that highlighted significant neonatal benefits.
- Unfortunately, because of the uterine incision, open fetal surgery carries risks to the mother, including bleeding, pulmonary edema, a thinning of the uterine incision during the pregnancy, a need for cesarean delivery in the current and all future pregnancies, preterm rupture of the membranes, preterm delivery, and traumatic uterine rupture during future pregnancies.
While still in the investigational stages, fetoscopic fetal spina bifida repair may lower the risks of the traditional form of repair by reducing the need for a uterine incision. Other benefits include faster maternal recovery, potential for vaginal trial of labor, and potential for delivery at later gestational ages, as compared with open fetal surgery.
When is an in utero repair performed?- Isolated spinal lesion starting at or above S1.
- Chiari II malformation (herniation of the posterior fossa [cerebellum] into the base of the skull).
- Surgery must be performed before 25 6/7 weeks.
- Normal karyotype or microarray testing via amniocentesis.
- No contraindications to in utero surgery—no prior myomectomy or any surgery on the uterus (other than cesarean).
- Low risk for preterm birth—no history of preterm birth, normal cervical length.
- Evaluation includes ultrasound, MRI, fetal echocardiogram, amniocentesis, and multidisciplinary consultation.
Spina bifida could be associated with long-term complications, including paralysis, the inability to walk, excess fluid on the brain (hydrocephalus), neurocognitive delays, spinal deformities, and neurocognitive disability. However, prenatal surgery can improve overall outcomes, such as an improved ability to walk independently and better neuromotor development.
About fetal spina bifida (PDF) >
Spina bifida | Pregnancy Birth and Baby
Spina bifida | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Spina bifida is a condition that affects the normal development of a baby’s spine early in pregnancy. This page provides information about spina bifida and how it might affect a baby born with the condition.
About spina bifida
A baby’s spine and brain begin to develop from the neural tube of the embryo during the first month of pregnancy. Spina bifida occurs when the neural tube has a defect and fails to close completely, leaving a gap in the baby’s spine.
This gap can interfere with messages that pass between the body, the nerves within the spine and the brain.
Spina bifida only affects the part of the body that receives its nerve supply from the open area of the spine or below that area.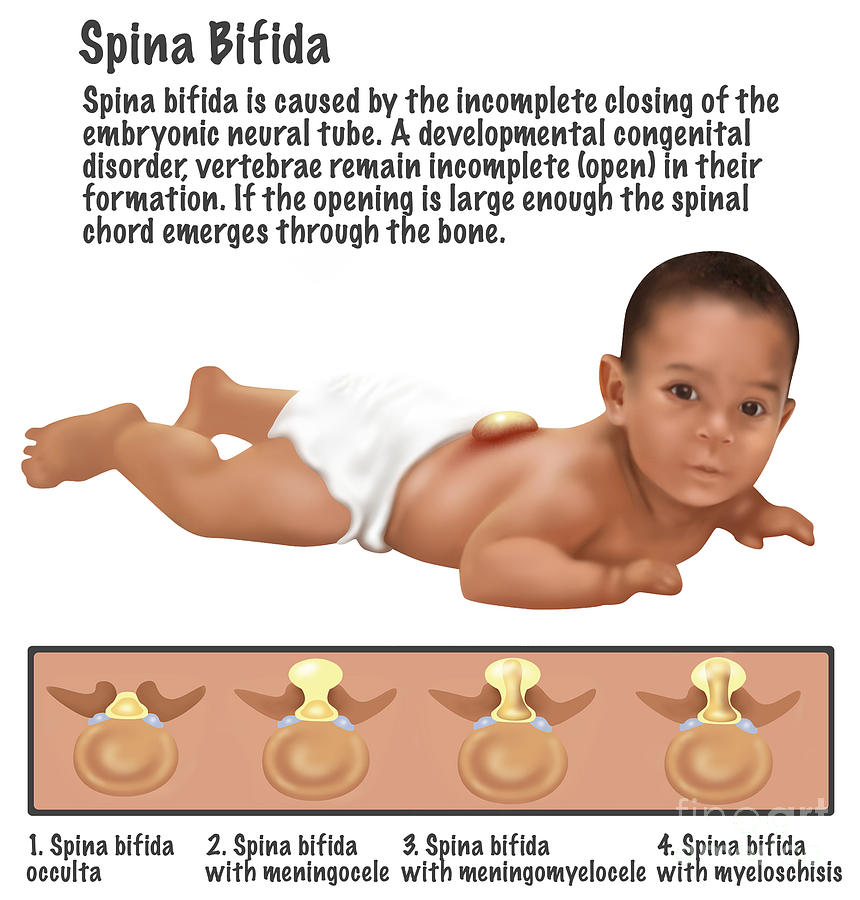 It doesn’t affect the brain, heart, chest or arms.
It doesn’t affect the brain, heart, chest or arms.
There are different types of spina bifida. The mildest form is a defect in the fusion of the bones of the spine that surround an otherwise healthy spinal cord. A person with mild spina bifida might have few or no symptoms.
In the most serious form, the spinal cord and its protective covering bulge through the gap in the baby's spine. It can lead to a number of problems with things like leg weakness and movement, sensation, bladder and bowel control and learning difficulties.
What causes spina bifida?
The cause of spina bifida is not fully understood. It appears to be a combination of genetic, environmental and nutritional factors.
Your baby is more at risk of spina bifida if your family has a history of neural tube defects. There is also greater risk if you have insulin-dependent diabetes and don't control your blood sugar well, are obese, or take certain medications such as valproate or carbamazepine. It’s important to speak to your doctor about medications if you are planning to become pregnant.
One way you can reduce the risk of your baby having spina bifida is to take a folate supplement and eat folate-rich foods if you are planning to become pregnant. You should take a folate supplement for at least 1 month before becoming pregnant and for the first 12 weeks of pregnancy.
How do I know if my baby might have spina bifida?
Spina bifida can be diagnosed with an ultrasound or blood test around the 16th and 18th weeks of pregnancy.
What if my baby has spina bifida?
If your baby has spina bifida, you will need to find out as much as you can about what it will mean for you and your unborn child.
Talk to your doctor about what the diagnosis means for both you and your baby. If the condition is serious enough, you might also wish to seek advice and information on whether to have the baby or to consider terminating the pregnancy. Pregnancy, Birth and Baby on 1800 882 436 can also offer advice.
You may also want to ask your doctor for a referral to a genetic counsellor who can help you understand more about the spina bifida and to plan for the future.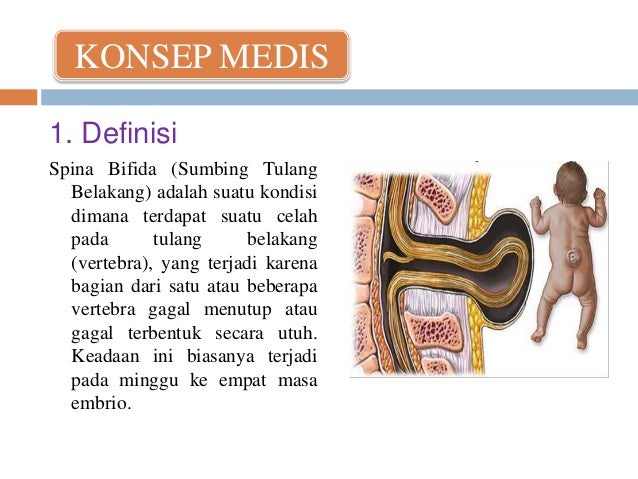
What happens when my baby is born?
Your baby will need special care at the time of birth. Medical staff will usually wrap the spinal opening with sterile dressings and plastic wrap and attach a drip to a vein in your baby’s arm to provide fluids and antibiotics. Your baby will be placed in an incubator for warmth.
If severely affected, your baby may be transferred to the hospital’s neonatal intensive care unit. If necessary, an operation can be done within the first few days to repair the spine or drain fluid from the baby’s brain.
Depending on the type of spina bifida, your baby might need continuing care from different specialists working in a hospital or your community. They might need to help your child with practical matters such as movement and learning how to go to the toilet.
What assistance is available?
If you are caring for a child with spina bifida, there are support groups in the different states. You can also get practical advice from a maternal child health nurse at Pregnancy, Birth and Baby on 1800 882 436.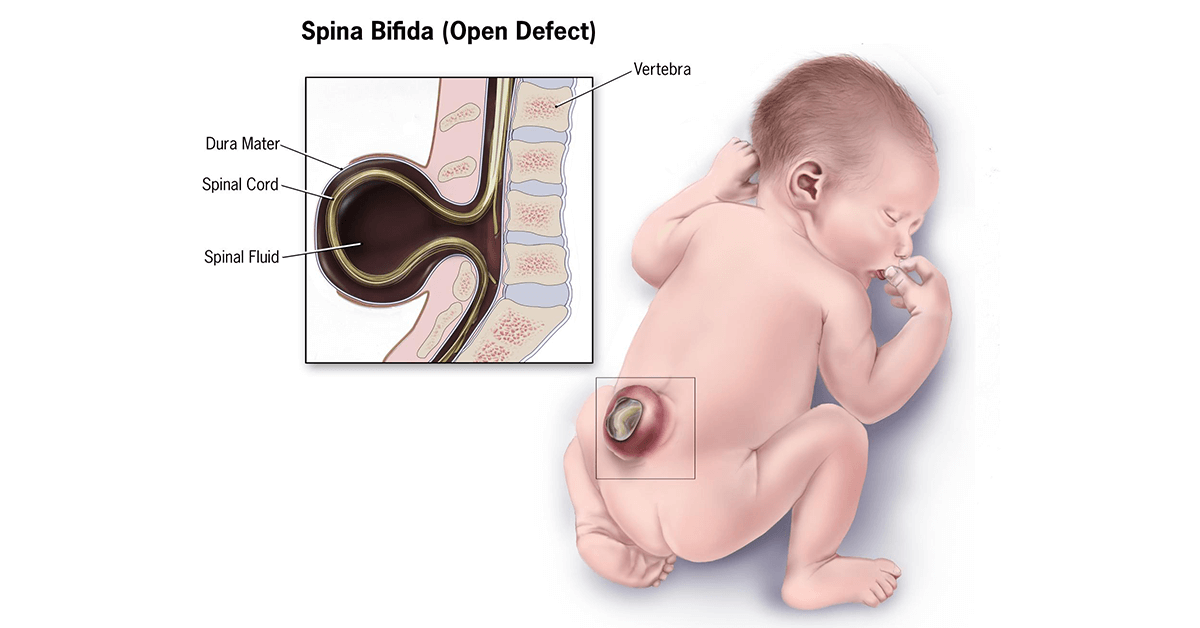
The Australian Government’s Carer Gateway provides general advice and different states have support groups. Your child may qualify for support from the National Disability Insurance Scheme.
Sources:
Centre for Genetics Education, NSW Health (Fact Sheet No. 60 - Neural tube defects – spina bifida and anencephaly), Cochrane (Folic acid supplements before conception and in early pregnancy (up to 12 weeks) for the prevention of birth defects), Cochrane (Spina bifida repair and infant and maternal health), Sydney Children’s Hospitals Network (Spina bifida)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2020
Back To Top
Related pages
- Disability and chronic illness
- Prenatal screening and testing
Need more information?
Spina bifida | Novita
Major effects of spina bifida Paralysis of the legs There may be complete paraplegia, or partial or minor paralysis depending on the level of the spinal injury
Read more on Novita Services website
Spina Bifida | Sydney Children's Hospitals Network
Spina Bifida comes from a latin term which means “split spine”
Read more on Sydney Children's Hospitals Network website
Hydrocephalus and Spina Bifida | Sydney Children's Hospitals Network
Many people living with Spina Bifida also have a condition called Hydrocephalus
Read more on Sydney Children's Hospitals Network website
Spina Bifida - Adolescents and adults with Spina Bifida | Sydney Children's Hospitals Network
Independence Being independent is an important life skill
Read more on Sydney Children's Hospitals Network website
Maternal screening - Pathology Tests Explained
Why and when to get tested for maternal screening
Read more on Pathology Tests Explained website
Why do you need to take folic acid when pregnant? | Queensland Health
Learn about why folic acid is important in pregnancy.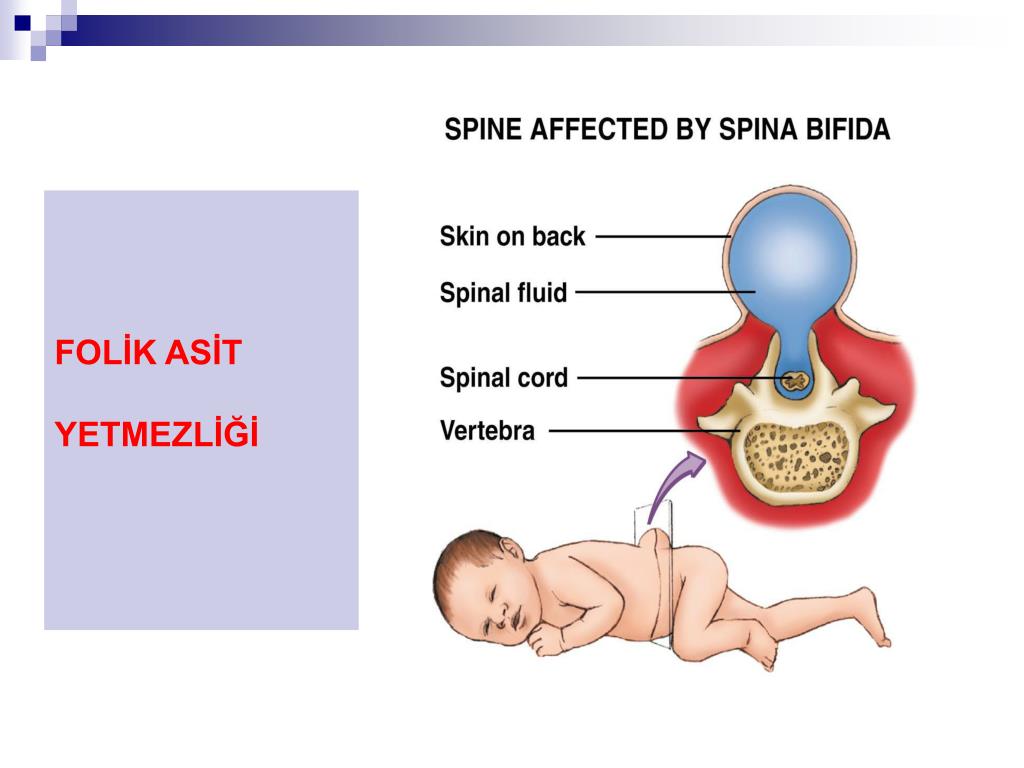
Read more on Queensland Health website
Pregnancy checkups, screenings and scans
Knowing what check-ups, screenings and scans to have and when to have them during your pregnancy is important information for every pregnant woman.
Read more on Pregnancy, Birth & Baby website
Neural tube defects: children & teens | Raising Children Network
Neural tube defects are brain and spinal cord abnormalities, including spina bifida, encephalocele and anencephaly. Read how they affect children.
Read more on raisingchildren.net.au website
Folate and pregnancy
Folate and folic acid are important for pregnancy since they can help prevent birth defects known as neural tube defects, such as spina bifida.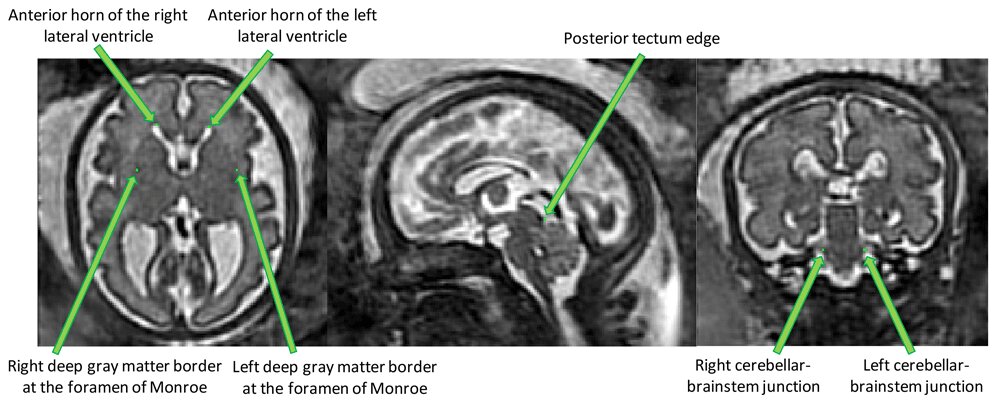
Read more on Pregnancy, Birth & Baby website
Sweat Chloride Test - Pathology Tests Explained
Prenatal screening provides pregnant women with the option to refine the probability of having a fetus with a common fetal chromosomal anomaly such as Down syndrome or a structural defect such as spina bifida.
Read more on Pathology Tests Explained website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Spina bifida (spina bifida) - treatment, symptoms, causes, diagnosis
Spina bifida (spina bifida) is a complex congenital defect in the development of the spinal cord and spine. This is a type of open neural tube defect in which there is an abnormal development of the back of the spine, the spinal cord, the surrounding nerves, and/or the fluid-filled sac that surrounds the spinal cord.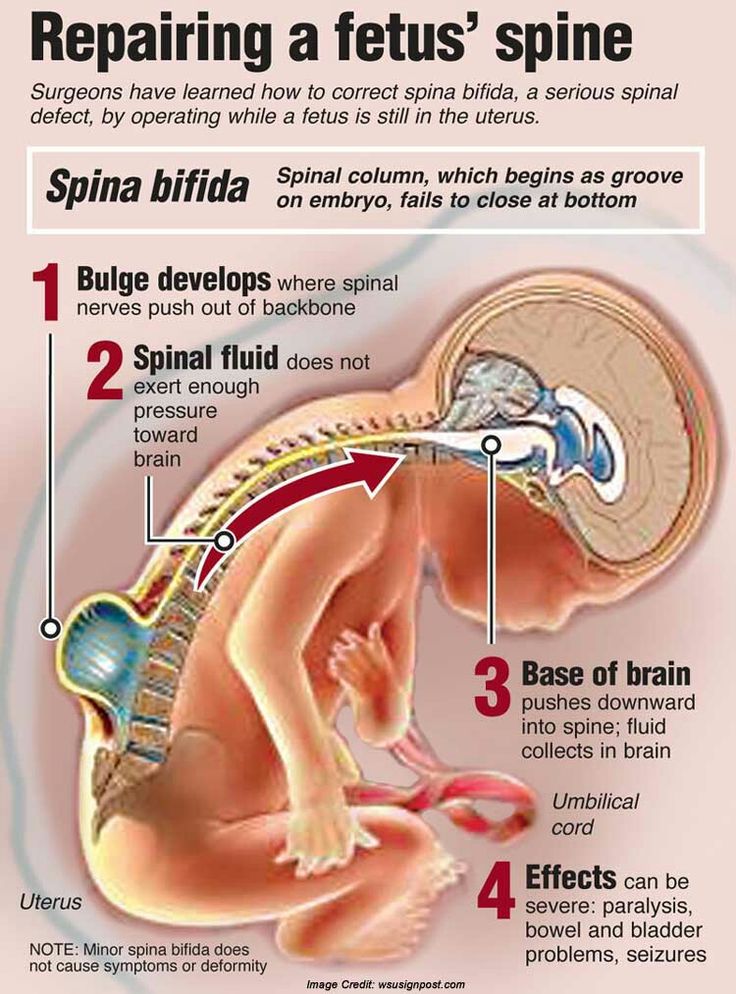
Spina bifida (back bifida) is an incurable, life-long condition that affects the neuromuscular and musculoskeletal systems.
This defect varies by type and ranges from moderate to severe.
Children with this defect may need corsets as the body grows, and in severe cases, a wheelchair.
Treatment is mainly aimed at slowing down the deformity and maintaining motor activity.
The defect may occur along the entire length of the spine and may present as part of the spinal cord and surrounding tissues protruding outward rather than inward. Approximately 85 percent of defects occur in the lower back and 15 percent in the neck and thoracic region. Surgically, it is possible to restore the integrity of the spinal column, but nerve damage cannot be restored, and if they are pronounced, then patients have various degrees of paresis of the lower extremities. The higher the defect on the spinal column, the more severe the nerve damage and movement disorders (paresis and paralysis).
According to studies, this developmental anomaly occurs in 7 cases per 10,000 newborns. There are several types of spina bifida that have varying degrees of severity.
- Latent spina bifida (spina bifida occulta) - the most moderate form, in which there are no obvious signs of malformation and changes in the skin. In this form, at least one vertebra changes, but the nerves and spinal cord do not bulge. A child at birth may have a spot or depression in the area of the anomaly. And usually, the baby will not have symptoms. With this form of anomaly (as well as with others), there may be an anomaly in the development of the spinal cord, characterized by attachment of the spinal cord to the spine to the end of the lumbar region, when normally the spinal cord ends at the level of the first lumbar vertebrae and sags freely without attachment to the spine.
- Meningocele is a moderate (and the most common) anomaly in which the spinal canal is not properly closed and the meninges (membranes that cover the spinal cord) bulge outside the bony structures of the spinal canal, but the spinal cord itself remains intact.
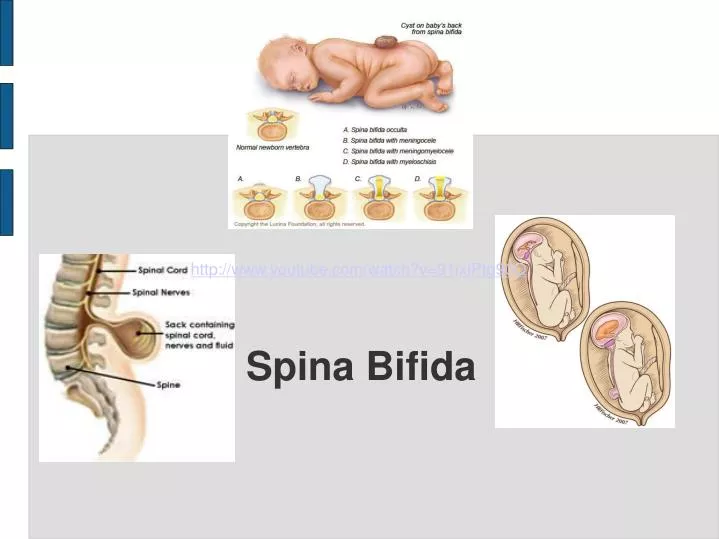 The cystic mass is covered with skin. Most children with meningocele have normal limb function, but may have partial paresis or abnormalities of the bladder or bowel. With this anomaly, there is often underdevelopment of the spinal cord. Almost all patients with this anomaly require surgery to close the defect and free the spinal cord.
The cystic mass is covered with skin. Most children with meningocele have normal limb function, but may have partial paresis or abnormalities of the bladder or bowel. With this anomaly, there is often underdevelopment of the spinal cord. Almost all patients with this anomaly require surgery to close the defect and free the spinal cord. - Lipomeningocele is an anomaly in which fatty tissue is attached to the spinal cord and puts pressure on it. Children with this form of anomaly may not have severe nerve damage, but bladder and bowel function may be impaired. In these cases, surgical treatment is also often used.
- Myelomeningocele: the most severe common form and associated with spina bifida. The spinal canal is not closed, and the bulging mass consists of the meninges, pathologically altered spinal cord, and nerves. In addition, in this area the skin is also underdeveloped. In children with this form of spinal cord splitting, paresis below the defect and dysfunction of the pelvic organs are observed in whole or in part.
 In addition, nerve damage and other pathologies are observed.
In addition, nerve damage and other pathologies are observed.
Symptoms
The symptoms of spina bifida vary greatly, depending on the form and severity of the individual child. For example, at birth:
- In latent splitting (spina bifida occulta), there may be no obvious signs or symptoms—only a small spot, depression, or birthmark.
- With a meningocele, there will be a sac-like protrusion that will be located on the back in the spinal region.
- With myelomeningocele, there will also be a protrusion, but with altered skin, there will be a release of nerves and spinal cord.
In severe spina bifida with localization in the lumbar spine, the following symptoms may occur: paralysis of the lower extremities, dysfunction of the bladder, intestines. In addition, these patients usually have other developmental anomalies:
- Hydrocephalus occurs in 75 percent of myelomeningocele cases and this condition requires operative endoscopic treatment in order to restore normal CSF flow or a shunt to drain excess fluid from the brain.

- Chiari anomaly (displacement of the brain into the upper cervical vertebrae) can cause pressure on the brainstem, which can manifest as impaired speech, swallowing, and motor disorders in the limbs.
- Underdevelopment of the spinal cord Orthopedic problems including scoliosis, kyphosis, hip dysplasia (congenital dislocation), combined deformities, clubfoot, etc.
- Precocious puberty (especially in girls with spina bifida and hydrocephalus).
- depression and other neurotic conditions
- obesity
- dermatological problems
- developmental anomalies of the urinary tract.
- heart disease
- vision problems
Diagnosis
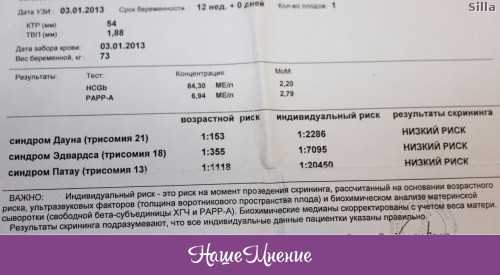
Diagnosis may be performed during pregnancy to evaluate the fetus for spina bifida. These include:
- Amniocentesis: A procedure in which a long, thin needle is inserted through the mother's abdomen into the amniotic sac to remove a small amount of amniotic fluid for examination.
 The fluid is analyzed to determine the presence or absence of an open neural tube defect. Although the analysis is very reliable, it does not allow diagnosing small or closed defects.
The fluid is analyzed to determine the presence or absence of an open neural tube defect. Although the analysis is very reliable, it does not allow diagnosing small or closed defects. - Prenatal ultrasound: this technique, being absolutely harmless, allows you to non-invasively assess the condition and visualize the internal organs, vessels, tissues of the fetus. Sometimes it is possible to diagnose not only spina bifida, but also other anomalies.
- Blood tests: It is recommended that blood tests be performed between 15 and 20 weeks of gestation for all women who have not previously had a child with an open neural tube defect and who have no family history of the condition. A blood test for alpha-fetoprotein and other biochemical parameters can determine how high the risk of developing spinal anomalies is.
- At birth, severe cases of spina bifida are evident by the presence of a fluid-filled sac bulging on the back of the newborn. Visual indicators of mild forms (spina occulta) may be a hairy patch on the skin or a depression along the spine.
Unusual weakness or lack of coordination in the lower extremities also suggests spina bifida. In children and adults, this anomaly is often diagnosed during routine studies or, if necessary, to differentiate neurological symptoms using instrumental research methods (MRI, CT, radiography).
Causes
During pregnancy, the human brain and spinal column begin to form as a flat sheet of cells that folds into a tube called the neural tube. If all or part of the neural tube fails to close, then the open area is called an open neural tube defect. An open neural tube is open in 80 percent of cases, and is covered by bone or skin in 20 percent of cases. The cause of spina bifida (spina bifida and other defects) remains unknown, but is most likely the result of a combination of genetic, nutritional, and environmental factors, such as:
- maternal dietary deficiency of folic acid (vitamin B) during pregnancy (sufficient folic acid intake during pregnancy may reduce the risk of this anomaly).

- maternal uncontrolled diabetes
- Certain medicines (antibiotics, anticonvulsants).
- A genetic factor is usually only relevant in 10 percent of cases.
- Mother's age
- What kind of births on the account (firstborns are more at risk).
- Socioeconomic status (children born in lower socioeconomic families are at higher risk).
- ethnicity
- obesity or excessive consumption of alcohol by a pregnant woman
- When exposed to pregnant hyperthermia in the early stages (sauna, jacuzzi).
Treatment
Spina bifida can be treated immediately after birth. If this defect is diagnosed prenatally, then a caesarean section is recommended in order to reduce possible damage to the spinal cord during the passage of the birth canal. Newborns with meningocele or myelomeningocele are recommended to have surgery within 24 hours of birth. With such an operation, the bone defect is closed and it is possible to preserve the function of the intact part of the spinal cord. Unfortunately, surgical treatment cannot restore the function of damaged nerves as they are irreversible.
Unfortunately, surgical treatment cannot restore the function of damaged nerves as they are irreversible.
Currently, there are clinics that perform prenatal surgery to close the defect, but the techniques have not yet found wide application. The main task of treatment, both in a non-severe form and in the postoperative period, is to preserve the functions of both the musculoskeletal system and the functions of the bladder and intestines. If necessary, orthoses, therapeutic exercises, physiotherapy are used.
In cases where spina bifida is detected by chance during X-ray (MRI, CT) examination, measures must be taken to reduce the risk of spinal cord injury in the area of the spine where this defect exists.
Operative treatment in adults is used only in the presence of complications. Basically, treatment in adults is aimed only at preventing possible complications (exercise therapy, physiotherapy, wearing a corset).
Spina bifida - prices for treatment, symptoms and diagnosis of the disease in the clinic "Mother and Child" in Moscow
The priority direction of the Center for the treatment of miscarriage is the treatment of complications of pregnancy with monochorionic twins.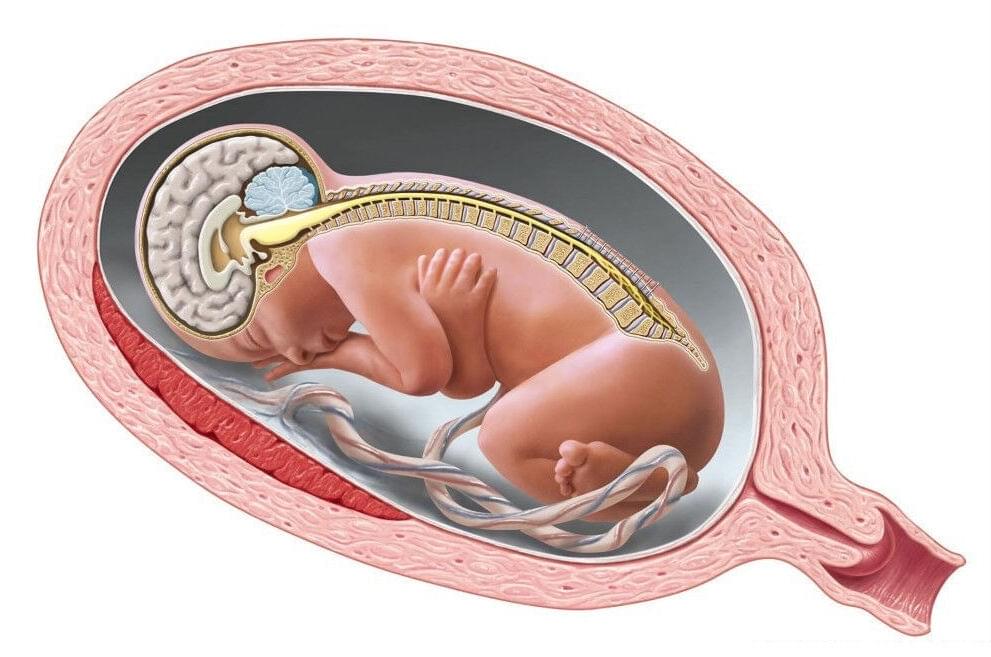 This is a complication of pregnancy with monochorionic twins, in which, due to the peculiarities of the angioarchitectonics of the placenta, blood from one fetus (donor) is discharged through vascular anastomoses to another fetus (recipient), as a result of which the “donor” will lack blood, oxygen and nutrients necessary for a full-fledged development, and the "recipient" will suffer from an excess of fluid in the vascular bed. SFTS complicates about 15% of pregnancies with a monochorionic placenta and the risk of losing one or both babies is about 80%. All patients with monochorionic twins undergo regular ultrasound screening aimed at identifying complications, including TTTS.
This is a complication of pregnancy with monochorionic twins, in which, due to the peculiarities of the angioarchitectonics of the placenta, blood from one fetus (donor) is discharged through vascular anastomoses to another fetus (recipient), as a result of which the “donor” will lack blood, oxygen and nutrients necessary for a full-fledged development, and the "recipient" will suffer from an excess of fluid in the vascular bed. SFTS complicates about 15% of pregnancies with a monochorionic placenta and the risk of losing one or both babies is about 80%. All patients with monochorionic twins undergo regular ultrasound screening aimed at identifying complications, including TTTS.
Spina bifida in Moscow:
Clinical Hospital Lapino-1 "Mother and Child"
The diagnosis is established by ultrasound based on discordance in the volume of amniotic fluid in fetuses: in the donor fetus, the maximum vertical pocket (MVP) is less than 2 cm (oligohydramnios) , in the recipient fetus more than 8 cm before 20 weeks and more than 10 cm after 20 weeks (polyhydramnios).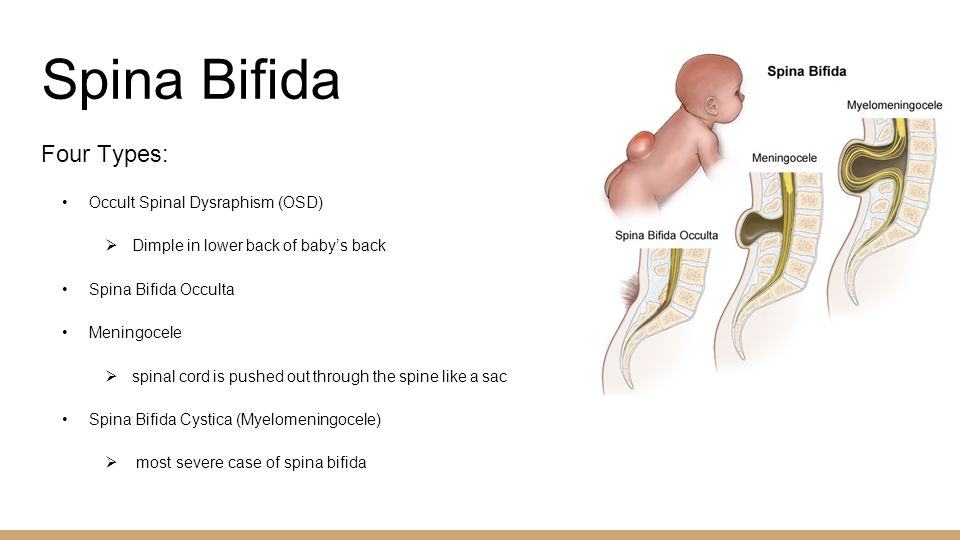
Ask a question or book a consultation:
In the Clinical Hospital "Lapino" of the Group of Companies "Mother and Child" in the Department of Fetal Medicine, diagnostics and open operations for intrauterine correction of spinal hernia (spina bifida) are carried out, followed by rehabilitation after birth.
Spina bifida is spina bifida and herniated spinal cord in the fetus. Spina bifida is classified into mild and severe forms. With a mild form, there is a slight defect in the vertebral arches and no protrusion of tissues is observed, usually it does not have serious consequences.
Severe forms, in which there is a significant hernial protrusion of the tissues of the spinal cord, adjacent tissues and membranes, are much more common.
Myelomeningocele (Chiari II anomaly) is the most severe and most common form in which the spinal cord and adjacent nerves bulge into the skin defect.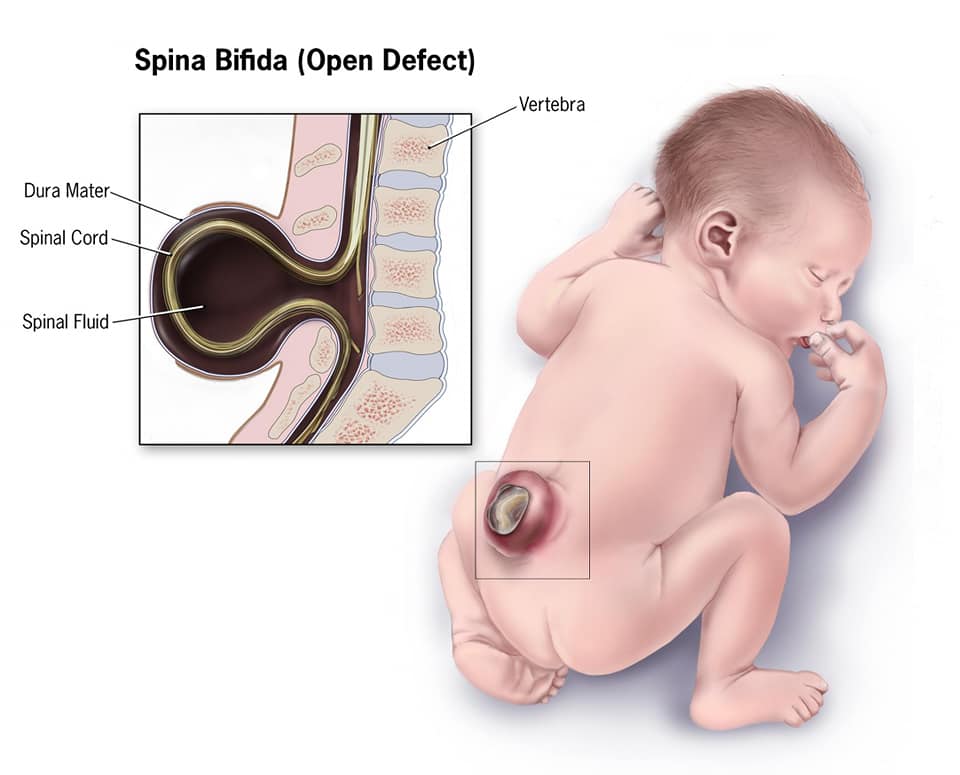 This is the only form in which the spinal cord comes into contact with the amniotic fluid, which leads to its not only mechanical damage, but also chemical.
This is the only form in which the spinal cord comes into contact with the amniotic fluid, which leads to its not only mechanical damage, but also chemical.
Severe forms are complicated by hydrocephalus (an increase in the volume of the ventricles of the brain), paralysis, impaired swallowing and breathing, dysfunction of the pelvic organs, developmental delay.
After birth, newborns with spina bifida require surgical treatment, and 98% of patients undergo ventriculoperitoneal shunting (cerebrospinal fluid is removed into the abdominal cavity using tube systems). Surgical intrauterine correction of this defect allows to reduce the severity and volume of complications both in the prenatal and postnatal periods. According to a multicenter randomized study conducted over 7 years in a number of US hospitals, intrauterine correction significantly reduces the risk of developing hydrocephalus, reduces the need for ventriculoperitoneal shunting after birth by 2 times, and significantly improves physical and mental development.