Frequent urination and diarrhea pregnancy
Pregnancy - signs and symptoms
Significant hormonal changes take place during pregnancy. These trigger a variety of symptoms. Some women experience many of the symptoms of pregnancy, while others may have only a few.
Symptoms of early pregnancy include missed periods, breast changes, tiredness, frequent urination, and nausea and vomiting (morning sickness). However, these symptoms may be caused by other factors and do not necessarily mean that you are pregnant, so if you suspect you are pregnant take a home pregnancy test and see your GP.
A wide range of changes can occur in your body in the later stages of pregnancy, including backache, headache, leg cramps or varicose veins, itch or tingling, constipation, haemorrhoids or indigestion, vaginitis or vaginal discharge, or mood changes or depression.
If you have any concerns don’t hesitate to talk to your GP. See your GP right away if you experience symptoms like vaginal bleeding or breaking waters, chronic pain, high temperature, severe headaches or vision loss.
The signs of early pregnancy can include:
- missed period
- nausea and vomiting (often called ‘morning’ sickness, but it can occur at any time)
- breast tenderness and enlargement
- fatigue
- passing urine more frequently than usual, particularly at night
- cravings for some foods, distaste for foods you usually like, and a sour or metallic taste that persists even when you’re not eating (dysgeusia).
Many of the signs of pregnancy, such as a missed period (amenorrhoea), nausea (morning sickness) or tiredness can also be caused by stress or illness, so if you think you are pregnant take a home pregnancy test (urine test) or see your GP, who will administer a urine test, blood test or ultrasound scan.
Missed period
Missing a period is often the first sign of possible pregnancy. However, some women experience light bleeding around the time of their expected period.
Nausea and vomiting
‘Morning’ sickness is a condition that affects more than half of all pregnant women. The symptoms include nausea and vomiting, and loss of appetite. Many women with morning sickness don’t just get symptoms in the morning but experience them throughout the whole day.
The symptoms include nausea and vomiting, and loss of appetite. Many women with morning sickness don’t just get symptoms in the morning but experience them throughout the whole day.
Morning sickness usually begins around the fourth to sixth week of pregnancy and may settle by week 12, although it can continue for longer or return at around 32 weeks.
Breast changes
During pregnancy, the breasts become fuller, swollen and tender. These changes are similar to those you may have noticed in the few days before your period. During pregnancy, the skin around the nipple becomes darker and the veins in the breast become more obvious.
Fatigue
Overwhelming tiredness is common in early pregnancy. This is most likely caused by the massive increase in the sex hormone progesterone. Progesterone is needed to maintain the pregnancy and help the baby to grow, but it also slows your metabolism.
Try to get some more sleep or rest when you can during this early stage. Your energy levels will probably rise again by around the fourth month of pregnancy when the placenta is well established.
Your energy levels will probably rise again by around the fourth month of pregnancy when the placenta is well established.
Tiredness during pregnancy can also be caused by anaemia, which is most commonly caused by iron deficiency. Eating iron-rich foods is important in the prevention of iron deficiency anaemia during pregnancy. Medical treatment of anaemia in pregnancy usually involves taking iron tablets. Sometimes an iron infusion (iron medicine given by a drip) is needed. This needs a hospital admission but only takes a few hours. Some iron infusions can be given by your GP.
Frequent urination
Pregnancy causes an increase in levels of body fluids and greater kidney efficiency. The swelling uterus also presses against the bladder. As a result, most women start experiencing more frequent urination within the first few weeks of becoming pregnant.
Food cravings
Cravings for certain foods are very common in pregnancy, especially for foods that provide energy and calcium, such as milk and other dairy products. You may also notice a sudden distaste for foods you previously liked.
You may also notice a sudden distaste for foods you previously liked.
Some women even develop an unusual taste for non-food items such as soil or paper. This is called ‘pica’ and may indicate a nutrient deficiency. Please speak to your GP or midwife if this develops.
Other symptoms of pregnancy
Many of these symptoms may also be indicative of other conditions. If in doubt, see your GP.
- backache
- breathlessness
- constipation
- haemorrhoids (piles)
- headaches
- heartburn and indigestion
- itchy skin
- leg cramps
- mood changes (such as unexplained crying)
- tingling and numbness in your hands
- vaginal discharge
- vaginitis
- varicose veins and leg oedema (swelling).
Backache
Back pain during pregnancy can affect more than 1 in 3 women. This is usually due to loosening of ligaments and change in posture due to the growing pregnancy.
You can help reduce back pain during pregnancy by wearing flat heeled shoes, using chairs with good back support, avoiding lifting heavy objects, and doing gentle exercise. Exercising in water can reduce back pain in pregnancy, and physiotherapy and acupuncture may also help.
Exercising in water can reduce back pain in pregnancy, and physiotherapy and acupuncture may also help.
Breathlessness
At the onset of pregnancy the hormone progesterone increases your lung capacity. This enables you to carry more oxygen to your baby and get rid of waste products such as the carbon dioxide that you both produce. At each breath you breathe more deeply and the amount of air you inhale (and exhale) increases significantly. This can make you feel short of breath.
In addition, as pregnancy approaches term, the pressure of the enlarging uterus and baby on your diaphragm can make your breathing feel more laboured.
Contact your doctor or midwife if you experience sudden onset of breathlessness associated with any of the following:
- pain
- palpitations (heart pounding)
- extreme tiredness
- exercise.
Constipation
Constipation refers to infrequent, hard bowel movements that are difficult to pass. Constipation is a common problem in pregnancy that may be caused by pregnancy hormones slowing your gastrointestinal movement, or by the pressure of your growing uterus on your rectum.
If you experience constipation during pregnancy, you are advised to:
- drink plenty of water every day.
- increase your dietary fibre (such as bran, wheat and fresh fruit and vegetables).
- do gentle, low impact exercise such as swimming, walking or yoga.
Don't take over-the-counter laxatives without first consulting your midwife or GP. If changes to your diet and lifestyle don't make a difference then your GP or midwife can prescribe a laxative that is safe to use in pregnancy.
Haemorrhoids (piles)
You may develop haemorrhoids (also known as piles) as a result of straining from constipation or the pressure of your baby’s head. Be reassured, symptoms usually resolve on their own soon after birth.
If you have bleeding from haemorrhoids, itching, discomfort or pain it is recommended that you:
- Alleviate or prevent constipation by increasing your daily water and fibre intake.
- Sit in warm salty water for about 15 minutes, especially after a bowel motion.

- Apply haemorrhoid cream.
If the bleeding or pain continues, talk with your GP (doctor) or midwife.
Headaches
Contact your GP or midwife if you have a headache during pregnancy that is not relieved by paracetamol (such as Panadol), especially in the second half of pregnancy.
A persistent headache can be associated with pre-eclampsia – a condition that can affect your kidneys and thus increase blood pressure and decrease blood flow to your baby.
Heartburn and indigestion
Heartburn, reflux or indigestion is the pain and discomfort associated with acid from the stomach entering and ‘burning’ the oesophagus.
Indigestion is more common during pregnancy due to the pressure of the enlarging uterus on the organs of the abdomen and the action of the hormone progesterone that relaxes the muscle between the oesophagus and stomach.
If you are experiencing heartburn, reflux or indigestion, it is recommended that you:
- Eat small and more frequent meals.

- Avoid eating just before going to bed.
- Sleep with extra pillows so your head is raised.
- Wear loose-fitting clothing.
- Avoid any food or fluid that aggravates symptoms – such as fatty foods (including fried foods, fatty meats and pastry), spicy foods (including curry and chilli), alcohol and caffeine (including tea, coffee, chocolate and cola).
- Consult your doctor before taking antacids.
If these strategies do not relieve your symptoms, please consult your GP, who may prescribe a medication that will safely reduce the secretion of acid.
Itchy skin
Widespread itching over the body is not common in pregnancy but it can be very distressing, interfering with sleep and enjoyment of pregnancy. Dry skin and eczema are the most common causes but sometimes there may be no apparent cause for the itching. In rare cases, where the palms of the hands and soles of the feet are itchy, it may be due to serious liver disease – a blood test can be done to check for this.
An itchy rash in the later part of pregnancy is thought to be caused by the body’s reaction to the stretching of the skin. This is called PUPPS. Itching can be controlled by using moisturisers and antihistamines. Ask your doctor or midwife what antihistamines are safe in pregnancy.
Leg cramps
Leg cramps occur due to a build-up of acids that cause involuntary contractions of the affected muscles. They are experienced by up to half of pregnant women, usually at night. Leg cramps are more likely in the second and third trimesters.
If you experience leg cramps, it is recommended that during an episode you:
- Walk around.
- Stretch and massage the affected muscle(s) to disperse the build-up of acids.
- Apply a warm pack to the affected muscle(s).
If you find cramps troublesome, discuss with your GP or midwife the option of taking magnesium lactate or citrate morning and evening.
Mood changes
Some newly pregnant women experience mood changes such as irritability. Other pregnant women experience feelings of elation. It is thought that the pregnancy hormones influence chemicals in the brain, causing mood changes.
Other pregnant women experience feelings of elation. It is thought that the pregnancy hormones influence chemicals in the brain, causing mood changes.
During pregnancy, 1 in 10 women experience depression. Depression is treatable, so if you are feeling depressed or ‘down’ during pregnancy it is extremely important to get help early. Please contact your GP (doctor), midwife or maternal and child health nurse as soon as possible.
Tingling and numbness in your hands (carpal tunnel syndrome)
Carpal tunnel syndrome – tingling and numbness in your hands – affects up to 60 per cent of women during pregnancy. It is caused by compression of the median nerve due to an increase in the tissue fluids during pregnancy.
Carpal tunnel syndrome may be mild, intermittently painful, or severe, which may cause partial paralysis of the thumb or loss of sensation. Symptoms usually resolve on their own soon after birth.
If you are experiencing tingling and numbness in your hands, inform your doctor or midwife.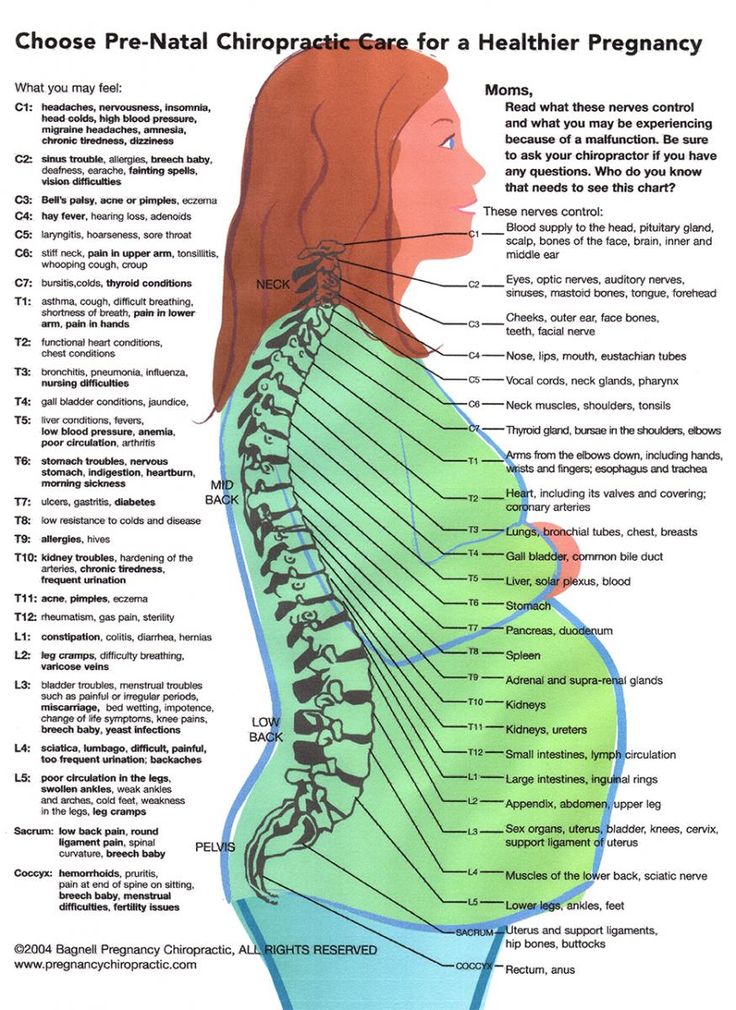 In very severe cases, your doctor may recommend corticosteroid injections or surgical treatment.
In very severe cases, your doctor may recommend corticosteroid injections or surgical treatment.
Vaginal discharge
An increase in vaginal discharge is a common change during pregnancy. If it is associated with itchiness, pain, a bad odour or pain on passing urine then it may be due to an infection. Seek treatment from your GP.
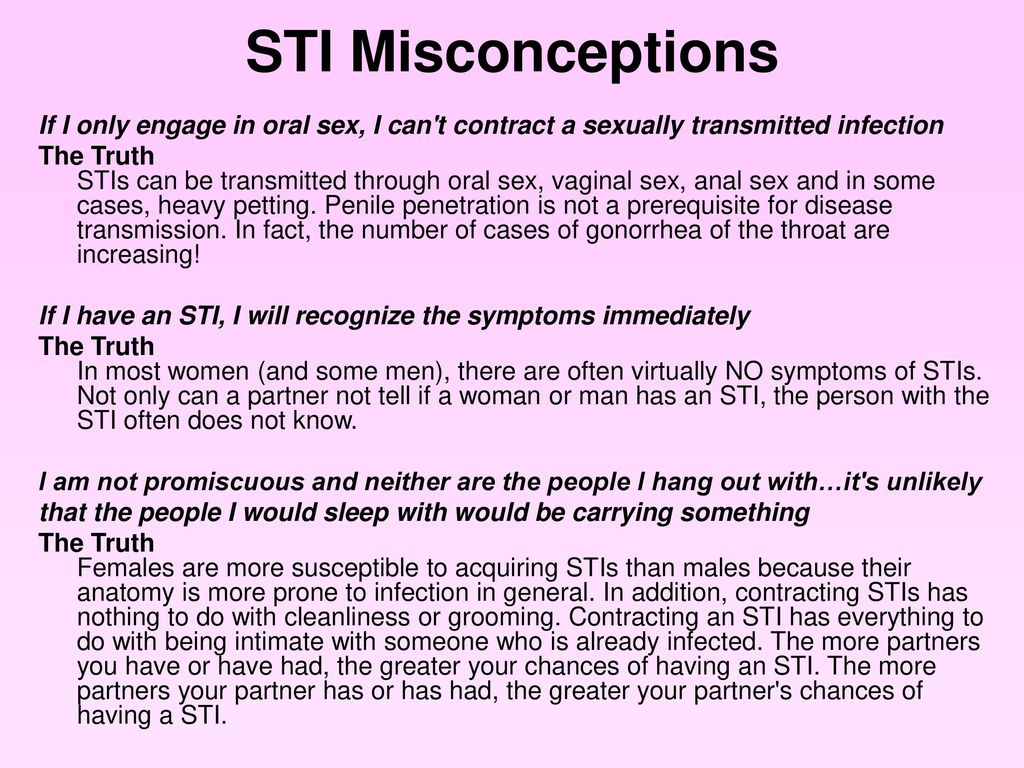
Vaginitis
Vaginitis is inflammation of the vagina, and is a distressing complaint for many women. It is more frequent during pregnancy. Some causes of vaginitis include vaginal thrush, bacterial vaginosis, trichomoniasis and chlamydia. See your GP for diagnosis and treatment
Varicose veins and leg oedema (swelling)
Varicose veins of the legs are very common in pregnancy due to a combination of factors, including increased volume of circulating blood during pregnancy, and pressure of the pregnant uterus on the larger veins. This increased pressure on the veins can also result in swelling of the legs (oedema) that can cause pain, feelings of heaviness, cramps (especially at night) and other unusual sensations.
If you have varicose veins, it is recommended that you:
- Wear support stockings.
- Avoid standing for long periods.
- Exercise gently and regularly (walking or swimming).
- Lie down to rest with feet elevated, when you can.
- Try massaging your legs.
- Tell your doctor or midwife at your next pregnancy visit.
It is recommended that you contact your hospital or carer if you are worried or if you have any of the following during pregnancy:
- vaginal bleeding
- less movement of your baby than usual
- severe stomach pain
- pain that doesn’t go away
- leaking amniotic fluid (that is, if your waters break)
- a high temperature
- vomiting that will not stop
- a headache that will not go away
- vision loss or blurred vision
- widespread itching of the skin
- sudden swelling of face, hands and feet.
Read more about problems that can occur during pregnancy.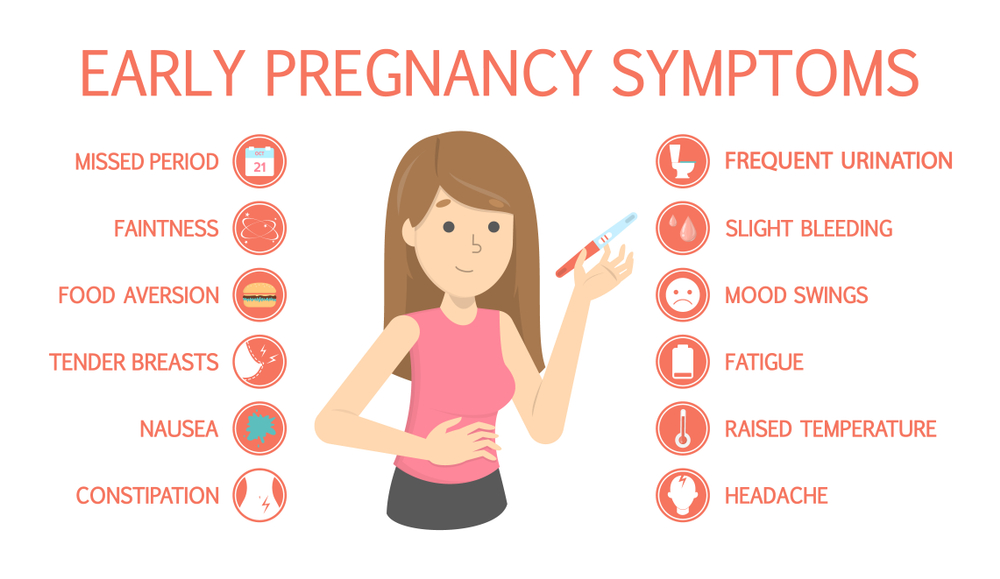
Where to get help
- In an emergency, call 000 for an ambulance
- Your GP (doctor)
- Midwife
- Obstetrician
- Your maternity hospital
- Your maternal and child health nurse
- Pharmacist
- Sexual Health Victoria Tel. 1800 013 952
- Sexual Health Victoria - Our Clinics
Varicose veins and spider veins
Veins carry deoxygenated blood back to our heart. In our legs, blood is collected in the superficial veins, just below the skin surface, and delivered to deeper veins that run within our calf muscles. The muscular action of our calves helps to pump the blood against the force of gravity towards the heart. One-way valves inside the veins prevent the blood from travelling backwards.
If these valves fail to close properly, blood pools in the superficial veins. Over time, the affected veins distend with blood (become ‘varicose’). Varicose veins are knobbly, twisted and darkish-blue in appearance.
Spider veins are like varicose veins, but smaller and closer to the surface of the skin. They are often red or blue, and can look like tree branches or spider webs. They are mostly found on a person’s legs or face. They may cover a small or large area.
These problem veins can be treated in two main ways. Surgery is usually used on only the larger varicose veins, while sclerotherapy can help with smaller veins.
Treatment of varicose veins and spider veins is not just for cosmetic reasons. Varicose vein disease can cause many health problems, such as blood clots, venous eczema, skin breakdown and ulceration, and, rarely, skin cancers.
Causes of varicose veins and spider veins
We do not know the causes of varicose veins and spider veins. However, in many cases, they run in families. Women seem to get the problem more often than men. Changes in oestrogen levels in a woman’s blood may have a role in the development of varicose veins. Such hormonal changes occur during puberty, pregnancy, breastfeeding and menopause.
Such hormonal changes occur during puberty, pregnancy, breastfeeding and menopause.
Factors that may increase your risk of developing varicose veins include:
- standing or sitting for long periods
- being immobile for long periods – for example, being confined to bed
- lack of exercise
- obesity.
Symptoms of varicose veins
Problems can occur if the faulty valves are located within the veins that go through the calf muscles (deep veins). Associated problems may include:
- aching in the legs
- skin rashes such as eczema
- brownish ‘stains’ on the skin surface, caused by the eruption of capillaries
- skin ulcers
- blood clots forming within veins (thrombophlebitis).
Prevention of varicose veins and spider veins
Some suggestions that may help to prevent varicose and spider veins include:
- Wear support stockings.
- Maintain good weight control.

- Get regular exercise.
- Avoid wearing high heels, as they affect the proper functioning of the larger veins.
Treatment of varicose veins and spider veins
Some varicose veins and spider veins can be treated by sclerotherapy, which is the injection of irritant chemicals (sclerosants) into the affected vein. The irritant prompts the vein to spasm and collapse in on itself. In time, the walls of the collapsed vein heal together, and the sealed vein can no longer carry blood.
Leg veins clear up slowly after sclerotherapy and may take up to two to six months to resolve, depending on their size. A compression stocking worn on the leg helps to speed this process. Small veins need compression for around three to six days, while bigger veins need about six weeks.
Sclerotherapy procedure
The actual sclerotherapy procedure takes at least one-and-a-half hours. Afterwards, you need to allow extra time for walking around. The process includes:
The process includes:
- The surgeon marks the site of injection on your legs while you stand.
- The surgeon gives you the injections while you are lying down.
- You put on compression bandages and stockings immediately after the injections. The bandages are meant to be tight.
- You should then walk for about half an hour.
The fine needle used for injecting does not cause much pain, only a mild pinprick sensation. Some people may experience a burning sensation after the injection. This disappears after a few seconds.
Each vein may need several injections, given some weeks apart. Many different veins can be injected in one treatment session. Allergic reactions to the sclerosants are very rare.
If the problem vein isn’t visible to the eye, the surgeon will use an ultrasound machine to help guide the needle (echosclerotherapy). This enables the surgeon to clearly see both normal and abnormal veins underneath the skin. Ultrasound-guided sclerotherapy is best for people with:
Ultrasound-guided sclerotherapy is best for people with:
- varicose veins
- spider veins that haven’t responded to standard injections
- leg ulcers
- other complications of varicose veins, such as pigmentation and eczema.
After sclerotherapy for varicose or spider veins
To improve blood circulation in the deep veins, it is essential to walk after the treatment. You should wear a compression stocking to reduce the risk of bruising and swelling, and other complications such as inflammation and clots. Regular exercise, weight control and the use of support stockings (if practical) are recommended between treatments and after treatment.
Side effects of sclerotherapy for varicose or spider veins
Some of the possible side effects and complications of sclerotherapy include:
- bruising – usually at the site of the injection. This will disappear in a few weeks
- Brown lines or spots – these may appear on the skin at the site of the injected blood vessels.
 This can occur when blood escapes from the treated vein into the skin. In most cases, this discoloration will disappear in time. In a small number of people (fewer than five per cent), the brown lines may last up to a year or longer. It is best not to take iron supplements while receiving sclerotherapy, as brown lines are caused by the iron content of the red blood cells. Laser therapy can treat stubborn lines or spots, although this treatment cannot be guaranteed to work
This can occur when blood escapes from the treated vein into the skin. In most cases, this discoloration will disappear in time. In a small number of people (fewer than five per cent), the brown lines may last up to a year or longer. It is best not to take iron supplements while receiving sclerotherapy, as brown lines are caused by the iron content of the red blood cells. Laser therapy can treat stubborn lines or spots, although this treatment cannot be guaranteed to work - lumps – may occur in larger injected veins. These are called ‘trapped blood’ and are not dangerous. They will either be removed a few weeks after the injection or will clear by themselves
- swelling – may occur in people who have had large veins treated. To prevent swelling, it is best to wear compression stockings after the treatment
- matting – a network of fine blood vessels can develop after sclerotherapy. This can be due to a number of reasons including lack of compression, inadequate compression, hormonal supplements, vitamin E supplements, use of anti-bruising creams or creams containing vitamin E, and inadequate treatment of underlying veins.
 Matting may resolve spontaneously but this may take a year or longer. It can also be treated using special injection techniques
Matting may resolve spontaneously but this may take a year or longer. It can also be treated using special injection techniques - ulcers (large sores) – these may form at the site of the injection. They can occur immediately after injection or a few days later. They are rare, but can be painful and usually leave scars after they heal
- inflammation (phlebitis) and blood clots – can affect the treated large veins
- allergy to the irritant solution
- irritation to veins other than the intended varicose vein
- accidental injection of irritant solution into an artery, causing tissue damage.
Inflammation (phlebitis) and blood clots can occur after sclerotherapy if:
- no compression has been applied
- the applied compression has not been enough
- you are on the contraceptive pill or hormone replacement therapy
- you have an underlying tendency to clotting
- the treatment has been performed just after long-distance travel or a major operation
- the underlying source of leakage in the vein has not been treated adequately
- the inflammation extends to the deep veins, causing deep vein thrombosis (DVT).
 DVT is a rare but serious complication of sclerotherapy. It can extend to the lungs, causing pulmonary embolism (clots in the lungs) and even death
DVT is a rare but serious complication of sclerotherapy. It can extend to the lungs, causing pulmonary embolism (clots in the lungs) and even death - it is recommended that women stop all hormonal supplements before sclerotherapy (check with your doctor).
Surgery for varicose veins
Major surface veins (long or short saphenous veins) that are varicose are usually treated surgically. Generally, a surgeon makes numerous small incisions (cuts) to reach the vein, rather than one large cut. Depending on the location of the varicose vein, these incisions may, for example, be in the groin or behind the knee.
Surgical techniques include:
- ligation and stripping – the surgeon cuts and ties off the vein (this is called ligation). Stripping the vein involves inserting a slender instrument into the vein through a small incision. The vein is then pulled out through a second incision
- phlebectomy – the surgeon makes small incisions, then removes the veins with a special hook.

Medical issues before varicose vein surgery
Doctors use a number of tests to decide which type of surgery is best for you. These tests include a physical examination and an ultrasound scan. You need to discuss a range of issues with your doctor or surgeon including:
- your medical history, since some pre-existing conditions may influence decisions about surgery and anaesthetic
- any medications you take on a regular basis, including over-the-counter preparations
- any bad reactions or side effects you have experienced from any medications
- whether or not you are pregnant. Varicose vein surgery is generally not advised for women during pregnancy.
Immediately after varicose vein surgery
After a varicose vein operation, you can expect:
- firm bandaging on your legs, to reduce bruising
- pain-relieving medication
- being encouraged to walk around
- a hospital stay of one or two days.

Side effects of varicose vein surgery
Some of the common side effects of varicose vein surgery include:
- swelling, which may take a few weeks to disappear. This is most likely on the feet and ankles
- scarring, although scars tend to be less noticeable than the varicose veins were. The scars fade with time
- brown staining of the skin, although this tends to fade with time
- pain, swelling and bruising in the skin and the calf muscle
- injuries to nerves, causing patches of numbness or ‘pins and needles’. These patches may recover in time (up to two years in some cases) or they may be permanent.
Complications of varicose vein surgery
Varicose vein surgery is considered to be safe, but all surgery has some degree of risk. Possible complications may include:
- infection, particularly if you had skin ulcers
- blood clots forming within deep veins
- bleeding or bruising.

Self-care at home after varicose vein surgery
Be guided by your doctor, but general self-care suggestions include:
- Allow for one (or perhaps two) weeks off work following surgery. You will need to avoid any hard physical exertions during this time.
- Don’t remove your bandages yourself. Leave bandages for your doctor to remove.
- To keep your bandages dry while showering, wrap your bandaged leg in plastic.
- Take at least a half-hour walk every day.
- Sunburn can make scars look worse. Avoid sun exposure if possible for six months.
- Wear a compression stocking for as long as your doctor advises.
- Avoid long periods of standing, or sitting with your legs crossed.
- You may need support stockings if your legs continue to ache.
Long-term outlook after varicose vein surgery
You will need to have a check-up a few weeks after surgery and, again, several months later. About 20 per cent of people who have varicose vein surgery will develop new crops of varicose veins over time.
About 20 per cent of people who have varicose vein surgery will develop new crops of varicose veins over time.
Other forms of treatment for varicose veins
Some other forms of treatment for varicose veins include:
- The veins are sealed by electrical current (electrodessication).
- The veins are destroyed by laser or high-intensity light.
Where to get help
- Your doctor
- Your surgeon
- Dermatologist
- Australasian College of Dermatologists Tel. 1300 361 821 or (02) 8765 0242
Toxemia, Intestinal Problems, and Heartburn
Find out how pregnancy affects your digestive tract, which trimesters are more likely to cause indigestion and nausea, and what to do to manage them.
During pregnancy, the burden on the mother's body increases. The body needs more nutrients, the body produces additional hormones. And the growing fetus puts pressure on neighboring organs, including the stomach and intestines. We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn.
We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn.
Contents:
- 2. Toxicosis and pregnancy
- 3. Causes, risks and treatment of diarrhea during pregnancy
- 4. Heartburn and stomach pain during pregnancy
- 5. Bloating, constipation and microbiota during pregnancy
- 6. Note
Changes in the work of the gastrointestinal tract by trimesters of pregnancy
The average duration of pregnancy is 40 weeks, which are usually divided into trimesters in accordance with the stages of intrauterine development of the child.
Each trimester is accompanied by a number of changes in the body, including in the gastrointestinal tract:
| The first trimester 1–13 weeks | 900 26 weeks | Third trimester of pregnancy 27–40 weeks |
| Morning sickness Morning sickness Zapor Intestinal disorder increased appetite TREAM to certain products Acid Reflux |
The Atlas genetic test will help you find out how your genes affect the level of female sex hormones necessary for fertility and pregnancy.
Causes of gastrointestinal problems during pregnancy
Every pregnancy is accompanied by inevitable changes in the functioning of the digestive system. They are most often caused by hormonal changes and increased stress on the organs, but they can also be associated with lifestyle and health conditions, for example:
- Sedentary lifestyle and unbalanced diet;
- Certain drugs, including calcium or aluminum antacids;
- Viral and bacterial infections;
- Intolerance to certain nutrients and allergic reactions;
- Stress;
- Diseases of the thyroid gland.
If you have chronic diseases of the gastrointestinal tract and you are planning a pregnancy, try to consult your doctor in advance. Symptoms of conditions such as irritable bowel syndrome (IBS) or acid reflux are more likely to get worse during pregnancy. Your doctor will help prepare your body and create a prevention plan to help relieve symptoms during this time.
Irritable bowel syndrome, or IBS, is a functional bowel disease that causes frequent abdominal pain, impaired peristalsis, bloating, constipation, or diarrhea.
Morning sickness, vomiting and general malaise during pregnancy
Morning sickness and morning sickness during early pregnancy are common, because the body undergoes important changes necessary for the development of the child.
up to 90%
women experience nausea during pregnancy
Doctors find it difficult to say with certainty why pregnant women feel sick in the morning. The main theory is hormonal changes. But there are some patterns associated with an increased risk of morning sickness:
- Multiple pregnancy;
- Toxicosis during previous pregnancy;
- History of morning sickness during pregnancy in close relatives;
- Tendency to motion sickness in transport;
- Use of oral contraceptives containing estrogen before pregnancy;
- Frequent migraines;
- BMI 30 and above;
- Elevated levels of stress hormones
Risks of severe morning sickness and how to reduce nausea
Nausea and vomiting are usually not associated with a risk for mother and child and disappear by 16-20 weeks of pregnancy, but it is not necessary to wait so long - there are ways that can help reduce nausea and enjoy the process of waiting for a new person:
- Get plenty of rest - fatigue increases toxicosis;
- Avoid smells and foods that cause nausea;
- Eat something right after waking up.
 A toast or a slice of bread will help reduce nausea;
A toast or a slice of bread will help reduce nausea; - Avoid hunger - empty stomach increases nausea. Eat small meals often, prefer low-fat, high-carbohydrate foods;
- Try ginger - studies show it helps with nausea;
- Sip as often as possible and prefer still water.
In rare cases, pregnant women may develop hyperemesis gestationis or excessive vomiting. This is a serious condition that can lead to dehydration, kidney damage, seizures, abnormal heart rhythms, and even death.
Signs of dehydration include dry mouth, dizziness, dark urine, infrequent urination and/or dizziness.
Symptoms of excessive pregnancy vomiting:
- frequent nausea for a long time and regular vomiting after meals;
- dry skin and lips;
- sudden weight loss;
- low blood pressure (below 90/60).
If symptoms of excessive pregnancy vomiting occur, do not wait until the condition resolves on its own. It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
0.5–2%
pregnant women experience excessive vomiting
Diarrhea in pregnancy
The word "diarrhea" comes from the Greek language and literally means "to flow through". This is a condition during which bowel movements or bowel movements occur three times a day or more often. This phenomenon is especially typical for the third trimester of pregnancy, but it can also occur earlier.
Symptoms of diarrhea:
- Three or more bowel movements per day
- Urgent urge to have a bowel movement
- Abdominal pain and cramps
- Bloating
Causes of diarrhea during pregnancy poisoning, dysbacteriosis, bacterial and viral infections:
| Gastroenteritis | Use of lactose and gluten in case of intolerance to these nutrients |
| Bacterial infections: listeriosis or salmonella | Chronic gastrointestinal diseases: Crohn's disease, IBS, ulcerative colitis |
| Certain antibiotics and antacids to reduce acidity | Laxatives |
| Sugar substitutes such as sorbitol | Overconsumption of certain foods |
Tip: If you have recently returned from a holiday in an exotic country with nausea and diarrhea and find out you are pregnant, see your doctor as soon as possible.
Gastroenteritis
One common cause of diarrhea during pregnancy is gastroenteritis or stomach flu. It is caused by bacterial or viral infections: norovirus, rotavirus, E. coli, salmonella, which enter the body through contact with contaminated surfaces, dishes, food and water.
Gastroenteritis usually lasts about three days. However, severe illness is a health hazard, especially during pregnancy, as it can cause dehydration, electrolyte imbalance, and lead to preterm labor.
The main symptoms of gastroenteritis are diarrhea without blood, nausea and vomiting, stomach cramps and pain, slight fever, headache and muscle pain.
Take extra precautions to reduce your risk of getting sick: frequent handwashing and surface disinfection. If the expectant mother has small children, they are not recommended to use the same cutlery.
Risks of diarrhea during pregnancy
Usually diarrhea during pregnancy is not a cause for concern. However, you should consult a doctor if the following symptoms occur during this period:
However, you should consult a doctor if the following symptoms occur during this period:
- Diarrhea for more than two days;
- Blood or mucus stools;
- Sudden weight loss;
- Pain in the abdomen;
- Dehydration.
How to treat diarrhea during pregnancy
If you have diarrhea during pregnancy, drink plenty of fluids, avoid foods high in fat and sugar, avoid dairy products, and caffeinated drinks.
Dehydration is a serious risk, especially during pregnancy, so electrolyte balance should be restored first with fluids and simple foods:
| Moderate fruit juices | Drinks without alcohol and caffeine |
| Bananas | Potato |
| Rice | Toast |
| Rusks | Light soups and broths |
| Pasta | Applesauce |
Find out about your body's ability to break down lactose and gluten with the Atlas Microbiota Test.
Stomach pain and heartburn during pregnancy
Many women experience stomach pain during pregnancy, especially the upper part of the stomach, as well as heartburn - a burning sensation in the chest and esophagus.
This is more common in the third trimester, after about 27 weeks. This is an unpleasant but natural phenomenon during pregnancy: the baby grows inside the uterus and presses on other organs, including the stomach. And hormones cause the muscles to relax, which causes acid from the stomach to enter the esophagus and irritate it. In addition, pain can be caused by problems with certain organs such as the gallbladder, or inflammation of the pancreas.
Symptoms of heartburn during pregnancy:
- Burning in chest and esophagus;
- Feeling of overeating, heaviness or bloating;
- Belching, including with acid and/or food particles;
- Nausea.
It is unlikely that you will be able to avoid cramps and heartburn during pregnancy. However, some tips can help reduce their frequency:
However, some tips can help reduce their frequency:
Nutrition : try to avoid overeating - eat easily digestible food in small portions; do not eat three hours before bedtime; watch your posture while eating - so the pressure on your stomach will be less.
Smoking and alcohol: In addition to known harms to mothers and babies, tobacco smoke also relaxes the muscles in the lower esophagus, allowing acid to enter the esophagus. And alcohol provokes heartburn and acid reflux.
Although stomach pain and heartburn often accompany pregnancy, abdominal pain, especially in the third trimester, should be taken seriously. It can be a sign of preterm labor or placental abruption, and puts mother and baby at risk.
If you experience severe abdominal pain during pregnancy that is accompanied by the following symptoms, seek medical attention as soon as possible:
| Abdominal pain and fever | Bleeding |
| Regular convulsions | Unusual vaginal discharge / spotting |
| Vomiting | Low back pain |
| Pain or burning when urinating | Severe pain that lasts 30-60 minutes |
Bloating, constipation and microbiota during pregnancy
Excessive gas and constipation during pregnancy can be caused by hormonal changes, such as increased production of progesterone. This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
Flatulence - bloating of the abdomen due to the accumulation of gases.
Here are a few simple rules that will help improve intestinal motility and avoid constipation and bloating:
- If you don't usually eat a lot of fiber and indigestible foods like legumes, try to gradually introduce them into your diet;
- Avoid carbonated drinks and fatty foods;
- Move more;
- Drink plenty of fluids.
If bloating and constipation are accompanied by severe pain that lasts more than 30 minutes, or if you have been constipated for two or more weeks, see your doctor.
Gut microbiota and bacteria during pregnancy
A woman's body goes through many changes during pregnancy, and this can affect the microbiota, the bacterial ecosystem that lives in the gut. Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
The additional influx of female hormones that accompanies pregnancy alters gut function and affects the microbiota. This is good, because the bacterial community is constantly adjusting to external and internal conditions in order to keep up with the needs of the body.
To keep your gut bacteria running smoothly, they need your help. Provide them with healthy foods and plant fibers. Fruits, vegetables, whole grains, nuts, and seeds contain prebiotics, special substances that beneficial bacteria feed on. When properly balanced, the bacteria even increase your body's defenses against harmful microorganisms that can cause gastroenteritis during pregnancy.
The Atlas Microbiota Test helps you understand how to prepare your gut for future pregnancies and reduce the risk of digestive problems.
☝️ Take note
Now you have all the necessary knowledge and tools to help you deal with digestive problems during pregnancy. They are quite varied and quite natural, but in some cases it is necessary to immediately seek medical help:
- Vomiting blood;
- Blood in stool;
- Diarrhea for more than two days;
- Constipation for more than two weeks;
- Sudden weight loss;
- Severe pain interfering with daily activities;
- Difficulty breathing;
- Pain when swallowing or difficulty swallowing;
- Excessive fatigue.
More articles on the causes of digestive problems on the blog:
- 7 foods that cause gas and bloating
- Leaky intestines
- When the intestines are upset
- 08 Mayo Clinic, sick0108
- Lindsey J Wegrzyniak, Treatment of Hyperemesis Gravidarum, 2012
- Edwards A. et al., The Maternal Gut Microbiome During Pregnancy, 2018
- National Health and Safety (NHS), Vomiting and morning sickness in pregnancy
- Kudzai Kanhutu, Travel and pregnancy: an infectious diseases perspective, 2011
- CDC, Pregnant travelers
- U.
 S. Department of Health and Human Services, Agency for healthcare research and quality, Abdominal Pain in Early Pregnancy
S. Department of Health and Human Services, Agency for healthcare research and quality, Abdominal Pain in Early Pregnancy - Robyn Horsager-Boehrer, M.D., UT Southwestern Medical Center, Should pregnant moms be concerned about gastroenteritis?, 2018
- International Foundation for Gastrointestinal Disorders, Pregnancy and Irritable Bowel Syndrome, 2016
- NHS Vomiting and morning sickness in pregnancy
- NHS, Severe vomiting in pregnancy
- Lindsey J Wegrzyniak et al., Treatment of Hyperemesis Gravidarum, 2012
- Karen Miles, Diarrhea during pregnancy, 2020
- Cleveland Clinic, Diarrhea
- You and your hormones, Progesterone
- Traci C. Johnson, MD, Pregnancy, Bloating, 2020
Signs of pregnancy - Clinic Zdorovye 365 Yekaterinburg
Symptoms of pregnancy - what is it?
Symptoms of pregnancy or signs of pregnancy are, as a rule, a combination of certain physiological changes in the body that a woman notices in herself already in the early stages of pregnancy.
Sometimes one hears that it is wrong to say “pregnancy symptoms”, because if there are symptoms, then there is an illness, and pregnancy is not an illness. But if we dig into dictionaries, we find that the word “symptom” comes from the Greek sýmptoma, i.e. "sign", "case", "coincidence". Thus, "pregnancy symptoms" is just a synonym for the phrase "signs of pregnancy", which is absolutely correct. The symptoms of early pregnancy or the first symptoms of pregnancy are different from the symptoms that occur in the later stages.
Knowing the signs of pregnancy allows a woman in the early stages to show increased attention to her health, and, consequently, to the health of the unborn baby, a pregnant woman will be able to determine pregnancy in the earliest possible time and, accordingly, resolve the issue for herself in time about its prolongation (preservation, continuation).
Every woman is remarkably different, so the symptoms a woman may experience during pregnancy may vary. Some women feel pregnant even before the test is positive. Below are nine symptoms of pregnancy.
Some women feel pregnant even before the test is positive. Below are nine symptoms of pregnancy.
The first symptom of pregnancy is implantation bleeding.
This is one of the earliest symptoms. On the sixth - twelfth day after conception, the introduction (attachment, implantation) of the embryo into the wall of the uterus occurs. Some women notice a small amount of red discharge (spots), which may be pink or reddish brown. If you have pain along with spotting or bleeding, see your doctor immediately as this could be a sign of an ectopic pregnancy.
The second symptom of pregnancy, also the main one, is the delay in menstruation
This symptom must be present during a normal pregnancy. You should know that sometimes bleeding occurs during pregnancy. The main thing is not to confuse them with menstruation, especially on those days when you should have started your period, that is, at 4, 8, 12 weeks of pregnancy. Bleeding during pregnancy is a sign of a threatened abortion. Therefore, if you notice this symptom in yourself, then immediately contact a specialized medical institution. With timely treatment, there is every chance to save the desired pregnancy. Menstruation does not occur throughout pregnancy and, as a rule, during breastfeeding.
Bleeding during pregnancy is a sign of a threatened abortion. Therefore, if you notice this symptom in yourself, then immediately contact a specialized medical institution. With timely treatment, there is every chance to save the desired pregnancy. Menstruation does not occur throughout pregnancy and, as a rule, during breastfeeding.
The third symptom of pregnancy is increased basal body temperature.
Basal body temperature rises above 37 degrees during pregnancy. If you notice some symptoms of pregnancy in yourself or even confirmed it with a doctor and at the same time observe a decrease in basal temperature, consult a doctor. A decrease in basal temperature may be due to the threat of miscarriage. For the result to be reliable, measure the temperature correctly. It should be measured in the rectum, immediately after waking up, in the morning.
The fourth symptom of pregnancy is heavy discharge.
In this case, we mean non-bleeding. Women know that normal vaginal discharge is odorless and almost colorless. Their number increases during ovulation and, as you now know, during pregnancy. On 9/10, you are pregnant if you have a missed period, heavy discharge, and an elevated basal body temperature.
The fifth symptom of pregnancy - swelling and (or) increased sensitivity of the mammary glands.
Many women say that the sensitivity of the mammary glands changes. This symptom may appear 1 to 2 weeks after conception. Swelling and increased sensitivity of the breast may appear not only as a result of pregnancy. Other causes are: premenstrual syndrome (PMS), birth control pills, or hormonal imbalances.
The sixth symptom of pregnancy is toxicosis.
Nausea or vomiting in the morning usually does not occur in the early stages, but some women experience nausea as early as the third week. Many women believe that toxicosis is morning sickness and vomiting. But it is not so. In addition to nausea and vomiting, signs of toxicosis include a heightened sense of smell and aversion to certain foods. Many pregnant women cannot tolerate certain smells during early pregnancy. A heightened sense of smell is a side effect of a rapidly rising level of estrogen in your blood. Aversion to certain foods is even more common than cravings for certain foods during pregnancy. You may suddenly find that certain foods, even your favorites, disgust you.
Many women believe that toxicosis is morning sickness and vomiting. But it is not so. In addition to nausea and vomiting, signs of toxicosis include a heightened sense of smell and aversion to certain foods. Many pregnant women cannot tolerate certain smells during early pregnancy. A heightened sense of smell is a side effect of a rapidly rising level of estrogen in your blood. Aversion to certain foods is even more common than cravings for certain foods during pregnancy. You may suddenly find that certain foods, even your favorites, disgust you.
The feeling of fatigue, which will be discussed below, is also referred to by some obstetricians as manifestations of toxicosis. Toxicosis, most often, goes away on its own by 12-14 weeks of pregnancy.
The seventh symptom of pregnancy is feeling tired.
Fatigue can be as pronounced as if you had run a marathon. Fatigue is caused by increased levels of progesterone and other hormones necessary for the development of the child.