Baby dry skin red patches
Baby Eczema: Symptoms, Causes and Treatments
Is there anything yummier than a baby’s soft, smooth skin? Though babies are known for exactly that, picture-perfect skin isn’t always the case, and baby eczema is often to blame.
Babies have extra-sensitive skin, so they’re more prone to rashes than older kids or adults. So the next time you spot some suspicious dry patches on your little one’s body, don’t be alarmed—there’s a good chance it might be baby eczema. But what causes it? Moreover, what does baby eczema look like? We’re sharing all the ins and outs of this common condition, plus some baby eczema treatments that will soon get baby comfortable in their own skin again. Read on to learn what baby eczema is, how to spot it and how to treat it.
In this article:
What is baby eczema?
What does baby eczema look like?
Baby eczema causes
Baby eczema treatment
Can breastfeeding prevent baby eczema?
When to contact a doctor about baby eczema
How long does baby eczema last?
What Is Baby Eczema?
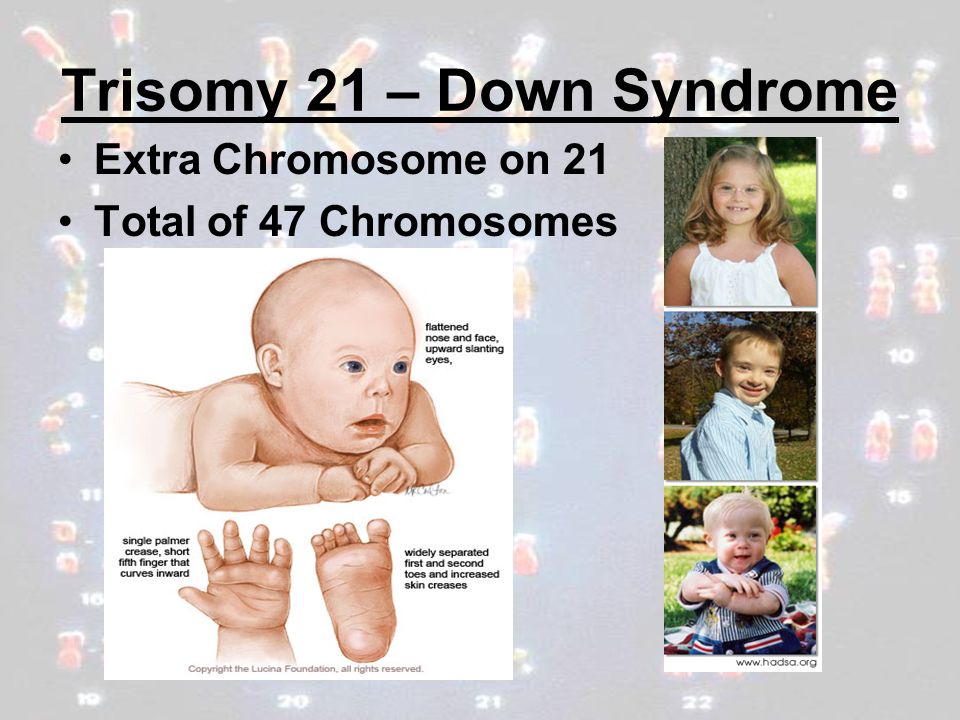
Baby eczema (or atopic dermatitis) appears as red or dry patches of skin, and it’s usually also itchy and rough. For babies who are predisposed to eczema, the first rashes typically appear around 2 to 4 months of age. “Baby eczema often starts as a pink, flaky rash on the cheeks and chin in young babies,” says Anna Bender, MD, a pediatric dermatologist at Weill Cornell Medicine and New York-Presbyterian in New York City. “Older babies who are of crawling age may develop the rash more on the outside of their arms and legs with dry, itchy, irritated skin patches. It may also feel rough to the touch like sandpaper.”
What are the different types of baby eczema?
While the National Eczema Association defines seven different types of the skin condition, baby eczema typically falls into one of four categories: atopic dermatitis, contact dermatitis, seborrheic dermatitis or dyshidrotic eczema.
• Atopic dermatitis: The most common type of eczema, atopic dermatitis is a chronic rash that’s usually hereditary, meaning there’s a family history of this condition or other allergies.
• Contact dermatitis: This type of rash is triggered by an outside element. Usually, the condition will go away once baby is no longer exposed to the offending ingredient or allergen. Chemicals, fragrances and soaps are a few examples of substances that can cause this type of rash.
• Seborrheic dermatitis: More widely known as cradle cap, this type of baby eczema is characterized by scaly skin patches on the scalp. It may be caused by genetics, hormones, oil buildup, yeast or a combination of these factors. Unlike most other forms of eczema, it’s not triggered by an allergy.
• Dyshidrotic eczema: This type of eczema appears on the hands and feet. It’s often caused by exposure to certain metals but can also be brought on by sweat and stress. While it can occur in babies and children, it’s more common in adults.
Is eczema common in babies?
The short answer is yes. Up to 20 percent of children in the United States may have some form of eczema, says Bender. According to the National Eczema Association, atopic dermatitis in particular affects 13 percent of children 18 and younger.
According to the National Eczema Association, atopic dermatitis in particular affects 13 percent of children 18 and younger.
What Does Baby Eczema Look Like?
It can be unnerving when you see raw and irritated skin patches on your infant, so being able to identify eczema can reduce your anxiety and get baby treatment faster. So what does baby eczema look like? It’s easy to confuse baby eczema vs. acne since both can appear on the cheeks. But baby acne typically appears earlier in life than eczema. “Baby acne can start soon after birth, while eczema may show the first signs around 2 to 5 months of age,” says Latanya Benjamin, MD, a Florida-based pediatric dermatologist and dermatologic surgeon and Society for Pediatric Dermatology board member. “Additionally, baby acne appears as classic pimples and small red pustules on the face usually with no symptoms. Eczema, on the other hand, affects both the face and body with dry or weepy red patches and is quite itchy.”
While eczema in babies with lighter skin typically looks pink, it may have a purple or gray tone in children with darker skin.
Another clue your little one may have this skin condition? Babies with eczema tend to rub their face with their hands or on their parents’ clothes, or rub their legs and feet or hands together.
Eczema in babies can be divided into three categories:
• Mild baby eczema: Minor cases usually appear as light pink, dry, itchy skin patches, Benjamin says, and can be treated with moisturizers alone.
Image: iStock
• Moderate baby eczema: More noticable cases feature hot spots that are redder. Plus, moderate eczema can affect more of the body surface, Benjamin says; baby may need a cortisone cream or ointment (see below for baby eczema treatments).
Image: iStock
• Severe baby eczema: This is the reddest and flakiest of all three varieties; it’s characterized by red, rough, thickened patches that are extremely itchy and often are crusty or have deep, scabbed cuts or cracks. Severe baby eczema is usually harder to control with over-the-counter products.
Image: Courtesy of Carla Bramley/Instagram
Baby Eczema Causes
Baby eczema is thought to be caused by a combination of (or, more specifically, an interplay of) genetic and environmental factors. “It occurs in families with a history of eczema, asthma and seasonal allergies,” explains Bender. “The immune system of people with eczema is more allergically prone.” What’s more, she says, the skin lacks a strong barrier to the outside world, so it can become easily irritated and dry. As a result, these babies are especially sensitive to certain factors that will incite a breakout. Different babies may be particularly vulnerable to different agents. A few common triggers of eczema in babies include:
• Dry skin (which is why eczema can be common in winter)
• Irritants (such as soaps, household detergents, wool, polyester)
• Heat and sweating
• Infection
• Allergens (pet dander, pollen, dust)
• Saliva (from drooling)
Baby Eczema Treatment
Mild baby eczema may need nothing more than an over-the-counter moisturizer, but more severe cases may require treatment from your pediatrician. “The severity of the eczema dictates what the best treatment should be,” Benjamin says. “But every form of eczema demands proper skin care, including effective moisturization and itch control.” Whatever the case may be, always check in with your pediatrician if baby breaks out. Depending on the severity, your doctor may suggest some or all of these baby eczema treatment options:
“The severity of the eczema dictates what the best treatment should be,” Benjamin says. “But every form of eczema demands proper skin care, including effective moisturization and itch control.” Whatever the case may be, always check in with your pediatrician if baby breaks out. Depending on the severity, your doctor may suggest some or all of these baby eczema treatment options:
• Creams: A gentle moisturizer is your first line of defense for baby eczema. “My son has eczema on his face and legs,” says one mom. “I use Aquaphor ointment on the patches for the flare-ups. Once that clears, we use regular Eucerin lotion after every bath, and his flare-ups have been really minimal.” Apply it all over baby’s body to soothe rough spots and also to improve the skin barrier function.
• Short baths with gentle cleansers: Proper daily skin care is crucial for keeping baby’s eczema-prone skin hydrated. Limit bathtime to 15 minutes and use warm—not hot—water. Choose gentle cleansers without fragrance, and avoid harsh soaps. After the bath, pat—don’t rub—baby’s skin dry within three minutes of taking them out of the water. Finally, apply moisturizer to their whole body.
Choose gentle cleansers without fragrance, and avoid harsh soaps. After the bath, pat—don’t rub—baby’s skin dry within three minutes of taking them out of the water. Finally, apply moisturizer to their whole body.
• Prescription creams and ointments: If the problem doesn’t go away, your pediatrician may suggest a prescription for a low- to medium-strength topical steroid ointment or cream, which can be used once to twice daily to help the inflammation and heal the skin. If you’re prescribed creams or ointments, it’s important to follow up with a doctor as directed to make sure it’s working properly. One mom we spoke to was given a cream that she applied four times a day on her daughter, who had dry, bumpy skin all over her arms, legs, belly and back. “It went away. Then it came back about three weeks after I stopped using the cream, but not nearly as bad as the first time,” she says. “I applied the cream a few more times, and it hasn’t been back since. It’s been about three weeks now. ”
”
• Diluted bleach baths: Inflamed skin is also more prone to infection. According to Benjamin, diluted bleach baths can not only safely manage infected eczema, but also help minimize the use of multiple courses of oral antibiotics for kids with repeated bacterial skin infections. She suggests adding ¼ to ½ cup of regular household bleach to a full-size bathtub with 1 inch of water. Talk to your pediatrician before trying a diluted bleach bath for baby eczema.
Baby eczema natural remedies
Since babies have extra-sensitive skin, it’s natural to want to treat it, well, naturally. But, Bender says, “even natural products have the potential to cause a worsened rash called contact dermatitis, so check with your doctor first before applying something new to baby’s skin.” Furthermore, Bender advises testing a new product before first-time use, and opting for “gentle products with simple ingredient lists.” Here are a couple natural baby eczema remedies that are safe for baby:
• Coconut oil is a natural moisturizer.
• Medical grade honey can help shallow cuts and prevent a local skin infection, Benjamin suggests.
• A home remedy for baby eczema is “wet wrap therapy” (also called wet pajama therapy). Bathe your child, and then apply a thick moisturizer to the slightly damp skin. Dampen a pair of cotton pajamas in warm water, wring them out and slip them on baby, right over the thick layer of moisturizer. After that, put on a second dry pair of cotton pajamas. Keep baby wrapped like this for a few hours or longer.
Can Breastfeeding Prevent Baby Eczema?
Good news for nursing moms: There may be a correlation between breastfeeding and lower incidence of baby eczema. A study found that babies who were exclusively breastfed for the first three months of life were less likely to develop eczema through age 6. While breastfeeding may not completely prevent these rashes, it could potentially reduce some flareups.
When to Contact a Doctor About Baby Eczema
If this is the first time baby is experiencing red or irritated skin, it’s best to contact your doctor to confirm whether it’s baby eczema or another condition. Once you get a diagnosis, you can start taking the appropriate steps and trying some baby eczema treatments.
Once you get a diagnosis, you can start taking the appropriate steps and trying some baby eczema treatments.
But if the skin irritation is accompanied by a fever, or the bumps and patches start to ooze, scab or blister, it may be a sign of infection, and you’ll want to consult your child’s doctor right away.
How Long Does Baby Eczema Last?
According to the American Academy of Pediatrics, while some babies may continue to experience eczema through adulthood, many will outgrow it around age 4.
Baby eczema may also evolve as your little one gets older. According to the National Eczema Association, it might appear on baby’s face in early infanthood but pop up in key areas like the knees, elbows and hands as they get older. As they approach big-kid territory, eczema often hides in knee folds or elbow creases and other sweat-prone spots.
Whether eczema is an acute or perpetual problem for your child, it’s reassuring to know that there are many baby eczema treatments and preventive measures you can take to reduce the symptoms and alleviate the itch.
No one likes to see their baby in discomfort—and the appearance of any rash can be disconcerting. But if you recognize eczema, you can rest assured that it’s common and treatable.
About the experts:
Anna Bender, MD, is a pediatric dermatologist at Weill Cornell Medicine and New York-Presbyterian in New York City. She received her medical degree at the Columbia University College of Physicians and Surgeons.
Latanya Benjamin, MD, FAAD, FAAP, is a Florida-based pediatric dermatologist and dermatologic surgeon and Society for Pediatric Dermatology board member. She earned her medical degree at Drexel University College of Medicine in Philadelphia, Pennsylvania.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Your Ultimate Guide to Baby Rashes
Bummed Out! How to Treat and Prevent Diaper Rash
Cradle Cap 101: How to Spot and Treat It
Baby Eczema: Symptoms, Causes and Treatments
Is there anything yummier than a baby’s soft, smooth skin? Though babies are known for exactly that, picture-perfect skin isn’t always the case, and baby eczema is often to blame.
Babies have extra-sensitive skin, so they’re more prone to rashes than older kids or adults. So the next time you spot some suspicious dry patches on your little one’s body, don’t be alarmed—there’s a good chance it might be baby eczema. But what causes it? Moreover, what does baby eczema look like? We’re sharing all the ins and outs of this common condition, plus some baby eczema treatments that will soon get baby comfortable in their own skin again. Read on to learn what baby eczema is, how to spot it and how to treat it.
In this article:
What is baby eczema?
What does baby eczema look like?
Baby eczema causes
Baby eczema treatment
Can breastfeeding prevent baby eczema?
When to contact a doctor about baby eczema
How long does baby eczema last?
What Is Baby Eczema?
Baby eczema (or atopic dermatitis) appears as red or dry patches of skin, and it’s usually also itchy and rough. For babies who are predisposed to eczema, the first rashes typically appear around 2 to 4 months of age. “Baby eczema often starts as a pink, flaky rash on the cheeks and chin in young babies,” says Anna Bender, MD, a pediatric dermatologist at Weill Cornell Medicine and New York-Presbyterian in New York City. “Older babies who are of crawling age may develop the rash more on the outside of their arms and legs with dry, itchy, irritated skin patches. It may also feel rough to the touch like sandpaper.”
For babies who are predisposed to eczema, the first rashes typically appear around 2 to 4 months of age. “Baby eczema often starts as a pink, flaky rash on the cheeks and chin in young babies,” says Anna Bender, MD, a pediatric dermatologist at Weill Cornell Medicine and New York-Presbyterian in New York City. “Older babies who are of crawling age may develop the rash more on the outside of their arms and legs with dry, itchy, irritated skin patches. It may also feel rough to the touch like sandpaper.”
What are the different types of baby eczema?
While the National Eczema Association defines seven different types of the skin condition, baby eczema typically falls into one of four categories: atopic dermatitis, contact dermatitis, seborrheic dermatitis or dyshidrotic eczema.
• Atopic dermatitis: The most common type of eczema, atopic dermatitis is a chronic rash that’s usually hereditary, meaning there’s a family history of this condition or other allergies.
• Contact dermatitis: This type of rash is triggered by an outside element. Usually, the condition will go away once baby is no longer exposed to the offending ingredient or allergen. Chemicals, fragrances and soaps are a few examples of substances that can cause this type of rash.
• Seborrheic dermatitis: More widely known as cradle cap, this type of baby eczema is characterized by scaly skin patches on the scalp. It may be caused by genetics, hormones, oil buildup, yeast or a combination of these factors. Unlike most other forms of eczema, it’s not triggered by an allergy.
• Dyshidrotic eczema: This type of eczema appears on the hands and feet. It’s often caused by exposure to certain metals but can also be brought on by sweat and stress. While it can occur in babies and children, it’s more common in adults.
Is eczema common in babies?
The short answer is yes. Up to 20 percent of children in the United States may have some form of eczema, says Bender. According to the National Eczema Association, atopic dermatitis in particular affects 13 percent of children 18 and younger.
According to the National Eczema Association, atopic dermatitis in particular affects 13 percent of children 18 and younger.
What Does Baby Eczema Look Like?
It can be unnerving when you see raw and irritated skin patches on your infant, so being able to identify eczema can reduce your anxiety and get baby treatment faster. So what does baby eczema look like? It’s easy to confuse baby eczema vs. acne since both can appear on the cheeks. But baby acne typically appears earlier in life than eczema. “Baby acne can start soon after birth, while eczema may show the first signs around 2 to 5 months of age,” says Latanya Benjamin, MD, a Florida-based pediatric dermatologist and dermatologic surgeon and Society for Pediatric Dermatology board member. “Additionally, baby acne appears as classic pimples and small red pustules on the face usually with no symptoms. Eczema, on the other hand, affects both the face and body with dry or weepy red patches and is quite itchy.”
While eczema in babies with lighter skin typically looks pink, it may have a purple or gray tone in children with darker skin.
Another clue your little one may have this skin condition? Babies with eczema tend to rub their face with their hands or on their parents’ clothes, or rub their legs and feet or hands together.
Eczema in babies can be divided into three categories:
• Mild baby eczema: Minor cases usually appear as light pink, dry, itchy skin patches, Benjamin says, and can be treated with moisturizers alone.
Image: iStock
• Moderate baby eczema: More noticable cases feature hot spots that are redder. Plus, moderate eczema can affect more of the body surface, Benjamin says; baby may need a cortisone cream or ointment (see below for baby eczema treatments).
Image: iStock
• Severe baby eczema: This is the reddest and flakiest of all three varieties; it’s characterized by red, rough, thickened patches that are extremely itchy and often are crusty or have deep, scabbed cuts or cracks. Severe baby eczema is usually harder to control with over-the-counter products.
Image: Courtesy of Carla Bramley/Instagram
Baby Eczema Causes
Baby eczema is thought to be caused by a combination of (or, more specifically, an interplay of) genetic and environmental factors. “It occurs in families with a history of eczema, asthma and seasonal allergies,” explains Bender. “The immune system of people with eczema is more allergically prone.” What’s more, she says, the skin lacks a strong barrier to the outside world, so it can become easily irritated and dry. As a result, these babies are especially sensitive to certain factors that will incite a breakout. Different babies may be particularly vulnerable to different agents. A few common triggers of eczema in babies include:
• Dry skin (which is why eczema can be common in winter)
• Irritants (such as soaps, household detergents, wool, polyester)
• Heat and sweating
• Infection
• Allergens (pet dander, pollen, dust)
• Saliva (from drooling)
Baby Eczema Treatment
Mild baby eczema may need nothing more than an over-the-counter moisturizer, but more severe cases may require treatment from your pediatrician. “The severity of the eczema dictates what the best treatment should be,” Benjamin says. “But every form of eczema demands proper skin care, including effective moisturization and itch control.” Whatever the case may be, always check in with your pediatrician if baby breaks out. Depending on the severity, your doctor may suggest some or all of these baby eczema treatment options:
“The severity of the eczema dictates what the best treatment should be,” Benjamin says. “But every form of eczema demands proper skin care, including effective moisturization and itch control.” Whatever the case may be, always check in with your pediatrician if baby breaks out. Depending on the severity, your doctor may suggest some or all of these baby eczema treatment options:
• Creams: A gentle moisturizer is your first line of defense for baby eczema. “My son has eczema on his face and legs,” says one mom. “I use Aquaphor ointment on the patches for the flare-ups. Once that clears, we use regular Eucerin lotion after every bath, and his flare-ups have been really minimal.” Apply it all over baby’s body to soothe rough spots and also to improve the skin barrier function.
• Short baths with gentle cleansers: Proper daily skin care is crucial for keeping baby’s eczema-prone skin hydrated. Limit bathtime to 15 minutes and use warm—not hot—water. Choose gentle cleansers without fragrance, and avoid harsh soaps. After the bath, pat—don’t rub—baby’s skin dry within three minutes of taking them out of the water. Finally, apply moisturizer to their whole body.
Choose gentle cleansers without fragrance, and avoid harsh soaps. After the bath, pat—don’t rub—baby’s skin dry within three minutes of taking them out of the water. Finally, apply moisturizer to their whole body.
• Prescription creams and ointments: If the problem doesn’t go away, your pediatrician may suggest a prescription for a low- to medium-strength topical steroid ointment or cream, which can be used once to twice daily to help the inflammation and heal the skin. If you’re prescribed creams or ointments, it’s important to follow up with a doctor as directed to make sure it’s working properly. One mom we spoke to was given a cream that she applied four times a day on her daughter, who had dry, bumpy skin all over her arms, legs, belly and back. “It went away. Then it came back about three weeks after I stopped using the cream, but not nearly as bad as the first time,” she says. “I applied the cream a few more times, and it hasn’t been back since. It’s been about three weeks now. ”
”
• Diluted bleach baths: Inflamed skin is also more prone to infection. According to Benjamin, diluted bleach baths can not only safely manage infected eczema, but also help minimize the use of multiple courses of oral antibiotics for kids with repeated bacterial skin infections. She suggests adding ¼ to ½ cup of regular household bleach to a full-size bathtub with 1 inch of water. Talk to your pediatrician before trying a diluted bleach bath for baby eczema.
Baby eczema natural remedies
Since babies have extra-sensitive skin, it’s natural to want to treat it, well, naturally. But, Bender says, “even natural products have the potential to cause a worsened rash called contact dermatitis, so check with your doctor first before applying something new to baby’s skin.” Furthermore, Bender advises testing a new product before first-time use, and opting for “gentle products with simple ingredient lists.” Here are a couple natural baby eczema remedies that are safe for baby:
• Coconut oil is a natural moisturizer.
• Medical grade honey can help shallow cuts and prevent a local skin infection, Benjamin suggests.
• A home remedy for baby eczema is “wet wrap therapy” (also called wet pajama therapy). Bathe your child, and then apply a thick moisturizer to the slightly damp skin. Dampen a pair of cotton pajamas in warm water, wring them out and slip them on baby, right over the thick layer of moisturizer. After that, put on a second dry pair of cotton pajamas. Keep baby wrapped like this for a few hours or longer.
Can Breastfeeding Prevent Baby Eczema?
Good news for nursing moms: There may be a correlation between breastfeeding and lower incidence of baby eczema. A study found that babies who were exclusively breastfed for the first three months of life were less likely to develop eczema through age 6. While breastfeeding may not completely prevent these rashes, it could potentially reduce some flareups.
When to Contact a Doctor About Baby Eczema
If this is the first time baby is experiencing red or irritated skin, it’s best to contact your doctor to confirm whether it’s baby eczema or another condition. Once you get a diagnosis, you can start taking the appropriate steps and trying some baby eczema treatments.
Once you get a diagnosis, you can start taking the appropriate steps and trying some baby eczema treatments.
But if the skin irritation is accompanied by a fever, or the bumps and patches start to ooze, scab or blister, it may be a sign of infection, and you’ll want to consult your child’s doctor right away.
How Long Does Baby Eczema Last?
According to the American Academy of Pediatrics, while some babies may continue to experience eczema through adulthood, many will outgrow it around age 4.
Baby eczema may also evolve as your little one gets older. According to the National Eczema Association, it might appear on baby’s face in early infanthood but pop up in key areas like the knees, elbows and hands as they get older. As they approach big-kid territory, eczema often hides in knee folds or elbow creases and other sweat-prone spots.
Whether eczema is an acute or perpetual problem for your child, it’s reassuring to know that there are many baby eczema treatments and preventive measures you can take to reduce the symptoms and alleviate the itch.
No one likes to see their baby in discomfort—and the appearance of any rash can be disconcerting. But if you recognize eczema, you can rest assured that it’s common and treatable.
About the experts:
Anna Bender, MD, is a pediatric dermatologist at Weill Cornell Medicine and New York-Presbyterian in New York City. She received her medical degree at the Columbia University College of Physicians and Surgeons.
Latanya Benjamin, MD, FAAD, FAAP, is a Florida-based pediatric dermatologist and dermatologic surgeon and Society for Pediatric Dermatology board member. She earned her medical degree at Drexel University College of Medicine in Philadelphia, Pennsylvania.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Your Ultimate Guide to Baby Rashes
Bummed Out! How to Treat and Prevent Diaper Rash
Cradle Cap 101: How to Spot and Treat It
Atopic dermatitis in a child: causes, symptoms and treatment
Approximately 10-20% of children worldwide have atopic dermatitis, a chronic but non-contagious skin disease that also affects adults. It is also called atopic eczema. Typical symptoms of atopic dermatitis are dry, irritated skin that occasionally flares up with moderate to severe itching, inflammation, and pain. Although there is still no cure for atopic dermatitis, regular and consistent care can help ease symptoms and prolong flare-free periods.
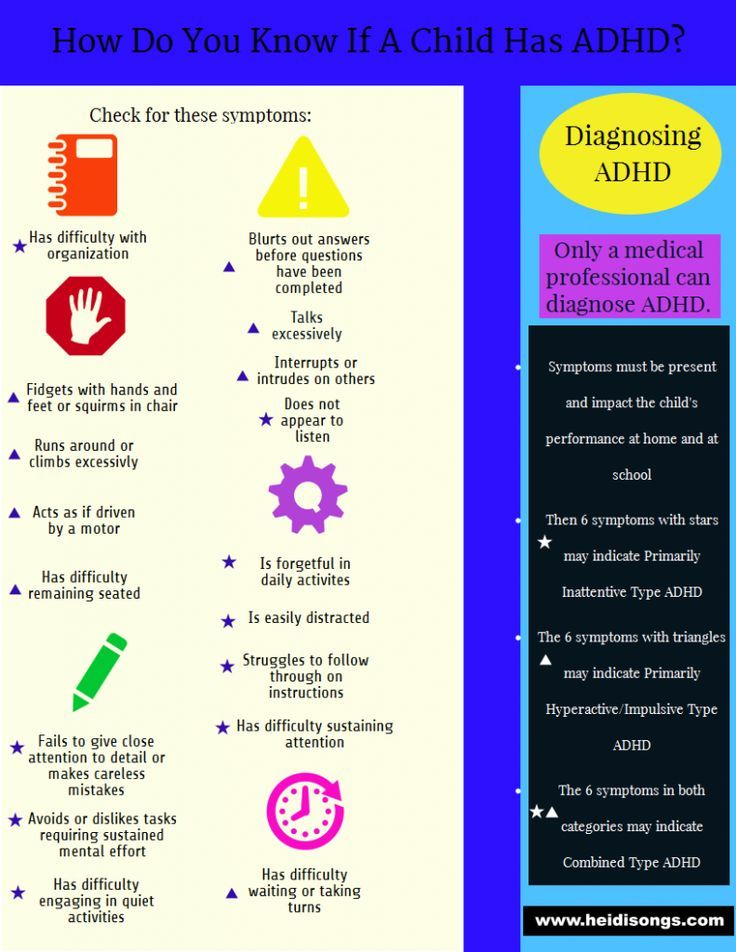
Signs and symptoms
Atopic dermatitis (or atopic eczema) is an uncomfortable and sometimes tiring long-term skin condition that is very common in children around the world, although predominantly in Western countries. While only 2-5% of adults suffer from this disease, its prevalence in children and infants is 10-20%. The majority of those who get atopic dermatitis (90%) start getting sick before the age of five, and many children later outgrow the disease.
The majority of those who get atopic dermatitis (90%) start getting sick before the age of five, and many children later outgrow the disease.
Atopic dermatitis usually manifests itself in two alternating "phases". In the dormant phase, the skin is very dry, irritated and can flake, and therefore must be moisturized daily. The active phases (or exacerbations, "flashes") are more painful, and at this time it is necessary to apply topical medications to calm the skin and stop itching.
Atopic dermatitis looks and feels different in infants, children and adults:
• Newborns may develop symptoms as early as 2-3 months of age. The rash may appear suddenly, making the skin dry, flaky and itchy. In the acute phase, fluid may ooze from the infected skin.
• If the disease develops in older children (from two years to puberty), it manifests itself in the form of a rash, dry skin that itches, scaly patches form. As a rule, the skin is uneven, thickened and rough to the touch.
• Atopic dermatitis in adults, which usually begins in childhood, is characterized by very dry, scaly skin and persistent itching.
Most often, atopic dermatitis in infants occurs on the face and scalp (especially on the cheeks) and on the body (elbows and knees).
In children who continue to be ill from early childhood, the rash often begins on the body - on the crooks of the elbows or knees - it is also quite common to see young patients with atopic skin on the neck, wrists, ankles and / or in the folds between the buttocks and legs .
Atopic dermatitis is made worse by scratching because nails rupture the skin barrier, allowing bacteria to enter the skin where inflammation develops. Babies often rub their skin against bedding or carpeting to relieve itching, and in children of all ages, the itching can become so unbearable that they cannot sleep. Worried about the child, parents may feel helpless, unable to help, and this, in turn, causes psychological stress. But the good news is that effective treatment and quality skin care can greatly alleviate all the troubles.
But the good news is that effective treatment and quality skin care can greatly alleviate all the troubles.
If you are not sure about your symptoms, please consult your doctor or dermatologist.
Causes and factors contributing to atopic dermatitis
Dermatologists have identified several factors that cause and exacerbate symptoms, for example:
Girls are more likely to develop atopic dermatitis than boys.• Family members have atopic dermatitis, hay fever and/or asthma . A link has been established between atopic dermatitis, hay fever and asthma, and experience shows that if one or both parents suffer from one or all of these diseases, their children will be more prone to developing atopic dermatitis.
• The child lives in a developed country , or in a city where the level of pollutants is higher than usual, or lives in a country with a cold climate. Interestingly, Jamaican children living in London are twice as likely to develop atopic dermatitis as those living in Jamaica.
• She is a girl . Girls are slightly more likely to develop the disease than boys.
• The mother gave birth to a child at a late age . There is evidence that children born in the later stages of their mother's childbearing years are more prone to atopic dermatitis.
There are a number of reasons why symptoms worsen or flare up after an injury. Patients have a deficiency of natural moisturizing factors (PUF) (such as amino acids) and impaired epidermal lipid metabolism. This explains why their skin is usually dry and its protective function is impaired.
Problems often arise from the atopic skin cycle. It starts when a child scratches a place that itches and breaks an already fragile skin barrier.
This allows bacteria, namely Staphylococcus aureus, to multiply and infect the skin. The infection causes inflammation, which again causes itching. The cycle starts again.
Skin care helps break the cycle of atopic skin.
Factors contributing to the development of atopic dermatitis
Certain foods, drinks, fabrics and materials are considered to be triggers for the manifestations of atopic skin.
These include :
Parents should avoid foods, materials and fabrics that can trigger symptoms of atopic dermatitis in children. • Materials like wool and nylon, which can be abrasive and cause skin irritation and sweating
• Food allergies, most commonly to dairy, nuts, and shellfish (check with your doctor before removing any foods from your child's diet)
• Allergy to house mites, dust, or pollen
• Detergents and cleaners
• Make-up (although brands targeting sensitive skin should be fine)
• Second-hand smoke (cigarette smoke)
Some additional effects of the disease - such as stress and insomnia - can also worsen symptoms.
Find out more about the factors that affect the skin.
Solutions
It can be very frustrating for parents to see their child suffer, and although there is no cure for atopic dermatitis, regular and consistent care can help prevent the disease from worsening, soothe the skin by reducing pain and itching, reduce emotional stress, prevent infections, and stop thickening of the skin.
The action plan will most likely include the development of a skin care regimen as well as some lifestyle changes.
For inactive phases, the daily use of emollients is extremely important.
Softeners
Emollients or moisturizers include lotions, creams, face creams, bath and shower oils, all of which are used for the same purpose - to keep the skin hydrated, supple and protected from irritants. Their regular use is fundamental to the care of atopic skin and can prolong the inactive phases of the disease. Children and infants with atopic dermatitis on the face should apply moisturizing facial creams twice a day.
To continue the active phases of the disease, among other things, the regular use of moisturizers is important.Main softening ingredients:
• Omega-6 fatty acids from evening primrose and grape seed extract. They soothe and nourish affected skin while restoring the skin's natural protective barrier.
• Licochalcone A (licorice root extract). It is a natural antioxidant with anti-inflammatory action that reduces redness and soothes inflammation.
Active Care
When flare-ups occur, emollients should be used in conjunction with active care products such as topical anti-itch creams and sprays. These topical creams usually contain corticosteroids such as hydrocortisone.
The use of hydrocortisone to relieve symptoms of exacerbation of atopic dermatitis in children is acceptable. Long-term use is not recommended as hydrocortisone may thin the skin. Hydrocortisone is known to be effective and fast-acting in relieving itching during flare-ups. However, many parents complain that with prolonged use of it on children's skin, various negative side effects can occur. In addition, the product loses its effectiveness if applied continuously, and it can also be used on large areas of the skin.
Eucerin AtopiControl Soothing Atopic Skin Cream has been clinically proven to protect skin and significantly improve the appearance of skin during flare-ups. This remedy helps limit the use of hydrocortisone during flare-ups. Clinical studies show that Eucerin AtopiControl Soothing Atopic Skin Cream has the same cosmetic effect on the face as creams based on 1% hydrocortisone. Eucerin AtopiControl Soothing Cream for Atopic Skin is not a pharmaceutical product and is not a substitute for it.
Additional advice for parents of children with atopic dermatitis on the face
• Use lukewarm water for washing, not hot water.
• Pat leather almost dry and apply emollient immediately.
• Apply softener twice a day.
• Cut children's nails short and smooth so that the child cannot scratch or pierce the skin.
• Wear cotton gloves at night to prevent your child from scratching his face while sleeping.
• Keep the room temperature cool and the humidity low.
• It is sometimes helpful to give a child a doll that can be scratched, as this may reduce the need to scratch their own skin.
Take care of your baby's skin
The skin of babies and children is much more fragile and sensitive than adults. Many mothers are wondering how to properly care for their skin. child to be as healthy as possible. To keep skin healthy baby and protect the skin from irritants, parents should be vigilant and careful in choosing care products.
There is a difference between the needs of the skin of a newborn baby, baby up to 3 years and a child from 3 to 10-12 years. As a general rule, children and infants should not use hygiene products and skin care products intended for for adults.
What are the features skin of babies and children?
"Skin like a baby" is an expression commonly used when talking about about soft and velvety skin, but this is not entirely true. At birth, the baby's skin is already fully formed, but it is thinner and more vulnerable, than an adult, and is not able to effectively perform its barrier function. A few weeks after birth, the baby's skin stops producing sebum, and the sebaceous glands in the skin are not activated until adolescence. Thus, the hydrolipidic layer becomes thinner, and therefore less its barrier function becomes effective. As a result, the skin becomes drier and more susceptible to pathogens and allergens.
A few weeks after birth, the baby's skin stops producing sebum, and the sebaceous glands in the skin are not activated until adolescence. Thus, the hydrolipidic layer becomes thinner, and therefore less its barrier function becomes effective. As a result, the skin becomes drier and more susceptible to pathogens and allergens.
The skin of babies and toddlers is highly absorbent, so all products applied to children's skin, are absorbed and enter the bloodstream faster than adults. Therefore, for the hygiene of the child's skin, it is important to use gentle products, which guarantee very good tolerability and have a high level safety while meeting strict production requirements.
Children's skin and atopic dermatitis
Various external irritants such as wind, cold, hard water and heating, weaken the skin of the child, make it more dry and reactive. With atopic dermatitis the child's skin is very dry and rough, sometimes with red spots. Leather becomes itchy, the child's sleep is disturbed.
Atopic dermatitis is a very common type of dermatosis that can start in the second or third month of life and in most cases disappears after some years. Atopic skin suffers from increased permeability of the horny layer due to lipid deficiency and therefore ceases to properly perform a barrier function. This causes inflammation and an outbreak of atopic dermatitis, most often accompanied by severe itching.
When scratching the affected areas, wounds are formed that are harmful skin. Children's skin becomes more permeable to allergens. atopic dermatitis occurs in two successive phases - exacerbation (spots, itching, risk of infection) and remission (symptoms improve but skin remains dry and itchy). There are 3 main types of environmental allergens that are more common cause acute inflammatory reactions in total:
Aeroallergens: dust mites, pollen, mold and fungal spores, wool cats and dogs
Food allergens
Contact allergens: nickel, fragrances
Skin irritation around the mouth
Irritation around the mouth is characterized by redness, small pimples, dryness and roughness. Perioral dermatitis occurs around the mouth under the influence of profuse salivation, with prolonged use of a pacifier, thumb sucking, or during teething teeth. The enzyme amylase, which is found in saliva, increases irritation. In winter, perioral dermatitis is aggravated by cold and wind.
Perioral dermatitis occurs around the mouth under the influence of profuse salivation, with prolonged use of a pacifier, thumb sucking, or during teething teeth. The enzyme amylase, which is found in saliva, increases irritation. In winter, perioral dermatitis is aggravated by cold and wind.
What's right care for the skin of babies and children?
1. Daily attention
Pay attention to risk areas: face, skin around the mouth, the area under the diaper and all the folds on the skin.
· Always consult your pharmacist or pediatrician when choosing your care products.
Avoid wool and synthetics when choosing tight clothing.
Make sure that the air in the room where the baby, not too dry, and the air temperature does not exceed 20 ° C.
2. Hygiene
Use a mild hygiene product, do not containing soap that protects the skin child and does not irritate the skin and eyes. When bathing a child, make sure that the temperature of the water in the bath was not higher than 35 ° C, as heat increases dryness skin.
Dry skin thoroughly and gently after bathing baby with a soft towel, paying special attention to the folds.
Then apply moisturizer to baby's delicate skin cream with very high tolerance.
To cleanse the skin of a child's face, you can use cotton pads and soap-free hygiene products such as micellar water. it help to avoid contact with the city hard water, which can irritate the skin.
3. Care
The skin of babies and children is very delicate, so it is important to learn how to properly protect it from external stimuli. Use moisturizing and nourishing creams or milks with a high level of safety and portability.
If the child has normal skin, daily Apply a moisturizing milk that nourishes and protects the skin.
If your skin tends to be dry, choose extra nourishing creams that restore the barrier function of the skin, prevent itching and provide instant comfort.
BIODERMA ABCDerm - baby and baby skin care
special cleaning and care products. To support and restore the natural physiological balance of the delicate skin of babies, BIODERMA has created a line of 9 products0125 ABCDerm , suitable for infants from birth (excluding preterm infants) children).
To support and restore the natural physiological balance of the delicate skin of babies, BIODERMA has created a line of 9 products0125 ABCDerm , suitable for infants from birth (excluding preterm infants) children).
To wash the body, face and hair of a child, use ABCDerm Gel Moussant - gentle cleansing gel, without soap, which maintains the integrity of the skin barrier. In addition, it forms a light foam for a pleasant bathing baby.
To moisturize the skin use ABCDerm Hydratant - gentle moisturizer milk that creates a protective layer and strengthens the natural skin barrier, and also limits factors that cause irritation.
For daily cleansing use micellar water ABCDerm h3O or micellar wipes ABCDerm h3O Lingettes , which are very convenient and practical when you the baby is away from home. Extra gentle micellar water supports natural balance, soothes and softens the skin.