9 month old baby temperature 38.6
High temperature (fever) in children
A high temperature is very common in young children. The temperature usually returns to normal within 3 or 4 days.
What is a high temperature?
Information:
A normal temperature in babies and children is about 36.4C, but this can vary slightly from child to child.
A high temperature is 38C or more.
A high temperature is the body's natural response to fighting infections like coughs and colds.
Many things can cause a high temperature in children, from common childhood illnesses like chickenpox and tonsillitis, to vaccinations.
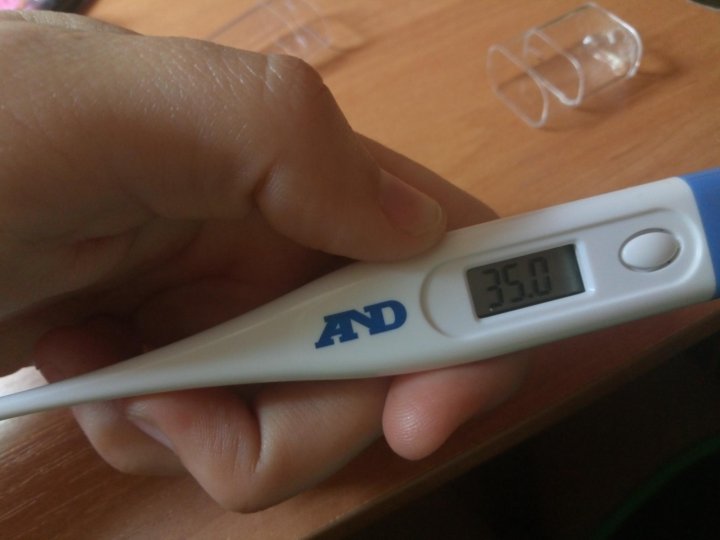
Checking a high temperature
Your child might:
- feel hotter than usual when you touch their back or chest
- feel sweaty
- look or feel unwell
Use a digital thermometer, which you can buy from pharmacies and supermarkets, to take your child's temperature.
- Place the thermometer inside the top of the armpit.
- Gently close the arm over the thermometer and keep it pressed to the side of the body.
- Leave the thermometer in place for as long as it says in the instruction leaflet. Some digital thermometers beep when they're ready.
- Remove the thermometer. The display will show your child's temperature.
If your child's just had a bath or been wrapped in a blanket, their temperature may be higher for a short time. Wait a few minutes then try again.
What to do if your child has a high temperature
You can usually look after your child or baby at home. The temperature should go down over 3 or 4 days.
Do
-
give them plenty of fluids
-
look out for signs of dehydration
-
give them food if they want it
-
check on your child regularly during the night
-
keep them at home
-
give them either paracetamol or ibuprofen if they're distressed or unwell – check the packaging or leaflet to make sure the medicine is suitable for your child, or speak to a pharmacist or doctor if you're not sure
-
get medical advice if you're worried about your child
-
try to keep your child at home and avoid contact with other people until they do not have a high temperature
Don’t
-
do not undress your child or sponge them down to cool them, a high temperature is a natural and healthy response to infection
-
do not cover them up in too many clothes or bedclothes
-
do not give aspirin to children under 16 years of age
-
do not combine ibuprofen and paracetamol, unless it has been recommended by a doctor
-
do not give paracetamol to a child under 2 months
-
do not give ibuprofen to a child under 3 months or under 5kg
-
do not give ibuprofen to children with asthma or chickenpox, unless it has been recommended by a doctor
Read more about giving medicines to children
Urgent advice: Call 111 or your GP surgery now if your child:
- is under 3 months old and has a temperature of 38C or higher, or you think they have a high temperature
- is 3 to 6 months old and has a temperature of 39C or higher, or you think they have a high temperature
- has other signs of illness, such as a rash, as well as a high temperature
- has a high temperature that's lasted for 5 days or more
- does not want to eat, or is not their usual self and you're worried
- has a high temperature that does not come down with paracetamol
- is dehydrated – such as nappies that are not very wet, sunken eyes, and no tears when they're crying
Immediate action required: Call 999 if your child:
- has a stiff neck
- has a rash that does not fade when you press a glass against it (use the "glass test" from Meningitis Now)
- is bothered by light
- has a fit (febrile seizure) for the first time (they cannot stop shaking)
- has unusually cold hands and feet
- has blue, pale or blotchy skin, lips or tongue
- has a weak, high-pitched cry that's not like their normal cry
- is drowsy and hard to wake
- is extremely agitated (does not stop crying) or is confused
- finds it hard to breathe and sucks their stomach in under their ribs
- is not responding like they normally do, or is not interested in feeding or normal activities
Video: Caring for children with fever at home
Watch this video on how to help a child with fever recover as quickly as possible.
Media last reviewed: 1 June 2020
Media review due: 1 June 2023
Page last reviewed: 21 December 2020
Next review due: 21 December 2023
Fever (0-12 Months)
Is this your child's symptom?
- An abnormal high body temperature
- Fever is the only symptom. Your child has a true fever if:
- Rectal (bottom), Ear or Forehead temperature: 100.4° F (38.0° C) or higher
- Under the arm (armpit) temperature: 99° F (37.2° C) or higher
- Caution: Ear temperatures are not accurate before 6 months of age
- Caution: Forehead temperatures must be digital. Forehead strips are not accurate.
Causes of Fever
- Overview. Almost all fevers are caused by a new infection. Viruses cause 10 times more infections than bacteria. The number of germs that cause an infection are in the hundreds. Only a few common ones will be listed.
- Viral Infections.
 Colds, flu and other viral infections are the most common cause. Fever may be the only symptom for the first 24 hours. The start of viral symptoms (runny nose, cough, loose stools) is often delayed. Roseola is the most extreme example. Fever may be the only symptom for 3 to 5 days. Then a rash appears.
Colds, flu and other viral infections are the most common cause. Fever may be the only symptom for the first 24 hours. The start of viral symptoms (runny nose, cough, loose stools) is often delayed. Roseola is the most extreme example. Fever may be the only symptom for 3 to 5 days. Then a rash appears. - Bacterial Infections. A bladder infection is the most common cause of silent fever in girls.
- Vaccine Fever. Fever with most vaccines begins within 12 hours. It lasts 2 to 3 days. This is normal and harmless. It means the vaccine is working.
- Newborn Fever (Serious). Fever that occurs during the first 3 months of life can be serious. All of these babies need to be seen as soon as possible. The fever may be due to sepsis (a bloodstream infection). Bacterial infections in this age group can get worse quickly. They need rapid treatment.
- Meningitis (Very Serious). A bacterial infection of the membrane that covers the spinal cord and brain.
 The main symptoms are a stiff neck, headache and confusion. Younger children are lethargic or so irritable that they can't be consoled. If not treated early, can suffer brain damage.
The main symptoms are a stiff neck, headache and confusion. Younger children are lethargic or so irritable that they can't be consoled. If not treated early, can suffer brain damage. - Overheated. The fever is usually low grade. Can occur during heat waves or from being overdressed. The temp becomes normal in a few hours after moving to a cooler place. Fever goes away quickly with rest and drinking extra fluids.
- Not Due to Teething. Research shows that "getting teeth" does not cause fevers.
Fever and Crying
- Fever on its own shouldn't cause much crying.
- Frequent crying in a child with fever is caused by pain until proven otherwise.
- Hidden causes can be ear infections, kidney infections, sore throats and meningitis.
Normal Temperature Range
- Rectal. A reading of 98.6° F (37° C) is just the average rectal temp. A normal low can be 96.8° F (36° C) in the morning. It can change to a high of 100.
 3° F (37.9° C) late in the day. This is a normal range.
3° F (37.9° C) late in the day. This is a normal range.
When to Call for Fever (0-12 Months)
Call 911 Now
- Not moving
- Can't wake up
- Severe trouble breathing (struggling for each breath; can barely speak or cry)
- Purple or blood-colored spots or dots on skin
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Trouble breathing, but not severe
- Great trouble swallowing fluids or spit
- Fever in baby less than 12 weeks old. Caution: Do NOT give your baby any fever medicine before being seen.
- Fever over 104° F (40° C)
- Shaking chills (shivering) lasting more than 30 minutes
- Nonstop crying or cries when touched or moved
- Won't move an arm or leg normally
- Dehydration suspected. No urine in over 8 hours, dark urine, very dry mouth and no tears.
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.

- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Age 3-6 months old with fever
- Age 6-12 months old with fever that lasts more than 24 hours. There are no other symptoms (such as cough or diarrhea).
- Fever lasts more than 3 days
- Fever returns after gone for more than 24 hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Fever with no other symptoms and your child acts mildly ill
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Fever
- What You Should Know About Fever:
- Having a fever means your child has a new infection.

- It's most likely caused by a virus.
- You may not know the cause of the fever until other symptoms develop. This may take 24 hours.
- For infants more than 3 months old, most fevers are good for sick children. They help the body fight infection.
- Use the ranges below to help put your child's level of fever into perspective:
- 100° - 102° F (37.8° - 39° C) Low grade fever: helpful, good range. Don't treat.
- 102° - 104° F (39 - 40° C) Average fever: helpful. Treat if causes discomfort.
- Over 104° F (40° C) High fever: causes discomfort, but harmless. Always treat.
- Over 106° F (41.1° C) Very high fever: important to bring it down. Rare to go this high.
- Over 108° F (42.3° C) Dangerous fever: fever itself can be harmful.
- Having a fever means your child has a new infection.
- Treatment for All Fevers - Extra Fluids:
- Fluids alone can lower the fever. Reason: being well hydrated helps the body give off heat through the skin.
- For shivering (or the chills), give your child a blanket.
 Make them comfortable.
Make them comfortable. - Offer your child extra water or other fluids by mouth. Cold fluids are better. Until 6 months old, only give extra formula or breastmilk.
- For all children, dress in 1 layer of light weight clothing, unless shivering. Reason: also helps heat loss from the skin.
- For shivering (or the chills), give your child a blanket. Make them comfortable.
- Caution: if a baby under 1 year has a fever, never overdress or bundle up. Reason: Babies can get over-heated more easily than older children.
- Fever Medicine:
- Caution: Do not give a baby under 3 months any fever medicine. Most of these babies will need to be seen.
- For fevers 100°-102° F (37.8° - 39°C), fever meds are not needed. Reason: fevers in this range help the body fight the infection. Fevers turn on the body's imune system. Fevers don't cause any discomfort. Fever meds are mainly needed for fevers higher than 102° F (39° C).
- Give an acetaminophen product (such as Tylenol).

- Another choice is an ibuprofen product (such as Advil) if over 6 months old.
- Goal of treatment: keep the fever at a helpful level. Most often, the fever meds lower the fever by 2° to 3° F (1 - 1.5° C). They do not bring it down to normal. It takes 1 or 2 hours to see the effect.
- Do not use aspirin. Reason: Risk of Reye syndrome, a rare but serious brain disease.
- Do not use both acetaminophen and ibuprofen together. Reason: Not needed and a risk of giving too much.
- Pain: fever does not cause pain. If your child also has pain, it's from the infection. It may be a sore throat or muscle pain. Treat the pain, if it's more than mild.
- Return to Child Care:
- Your child can return to child care after the fever is gone. Your child should feel well enough to join in normal activities.
- What to Expect:
- Most fevers with viral illnesses range between 101° and 104° F (38.4° and 40° C).
- They may last for 2 or 3 days.

- They are not harmful.
- Call Your Doctor If:
- Your child looks or acts very sick
- Any serious symptoms occur such as trouble breathing
- Fever goes above 104° F (40° C)
- Any fever occurs if less than 12 weeks old
- Fever without other symptoms lasts more than 24 hours
- Fever lasts more than 3 days (72 hours)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 10/18/2022
Last Revised: 09/18/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
If a child has a fever, what should I do?
home
Articles
Health
Kurilova Alina Petrovna Pediatrician
14. 05.2019
05.2019
Before you start taking antipyretics, you need to answer a few questions:
-
what is the age of the child?
-
How does a child tolerate an increase in a particular temperature?
-
Have there been any family or child history of febrile seizures?
-
Are there any other symptoms of the disease besides fever?
An increase in temperature or fever is a protective and adaptive reaction of the body in response to the effects of pathogenic stimuli, which results in a restructuring of thermoregulation processes, leading to an increase in body temperature, which stimulates the body's natural resistance.
An increase in temperature affects the child's body both positively and negatively.
The positive effect of is that when the temperature rises in the child's body, the immune system is activated, phagocytosis increases, the production of antibodies increases and the level of interferon increases, which helps to stop the reproduction of pathogenic microorganisms and overcome the infection.
Negative influence high temperature in a child is manifested in the occurrence of convulsions (febrile), increased stress on the baby's cardiopulmonary system (heart rate and respiratory rate become more frequent). Therefore, fever is dangerous for children with malformations of the heart and bronchopulmonary system, heart rhythm disturbance. Also, when the temperature rises, the work of the brain, liver, stomach, kidneys and other internal organs suffers, which is dangerous for children with chronic pathologies of internal organs, symptoms of dehydration, developmental disorders and diseases of the nervous system.
Fever varies:
-
with the flow:
-
acute (fever up to 2 weeks),
-
subacute (up to 6 weeks),
-
chronic (over 6 weeks).
-
-
by the degree of increase of the indicator:
-
subfebrile (increase to +38.
 0 degrees)
0 degrees) -
febrile (from +38.0 to +39.0 degrees),
-
pyretic (from + 39.0 to + 41.0 degrees),
-
hyperpyretic (over +41.0 degrees).
-
-
according to the type of temperature curve:
-
constant (temperature fluctuations during the day are not higher than 1 degree).
-
laxative (daily fluctuations up to 2 degrees),
-
atypical (fluctuations are chaotic, different and irregular),
-
debilitating (a combination of laxative and atypical fever with fluctuations during the day more than 2-3 degrees),
-
intermittent (a combination of short periods of temperature increase and decrease to normal numbers),
-
return (alternation of periods of temperature increase with periods of temperature normalization from 2 to 7 days).
-
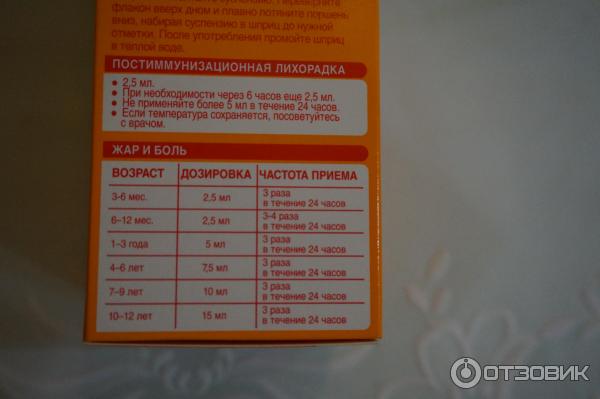
On the recommendation of the WHO (World Health Organization), antipyretics are prescribed for children according to age:
-
from the moment of birth to 2 months at a temperature of +38.
 0 degrees,
0 degrees, -
children from 3 months to 24 months at a temperature of +38.5 degrees,
-
children from 1 to 5 years old at a temperature of +39.0 degrees,
-
children over 5 years old with indicators of + 39.5- + 40.0 degrees.
On the other hand, the approach to each child should be individual.
If a child
- restless or feeling weak,
- cannot tolerate muscle pain, headache,
- have nausea,
- no appetite,
then you must first apply physical methods to improve the well-being of the child :
-
put to bed - so the body will save strength to fight the infection, calm the child;
-
drink fractionally with water or sweetened warm herbal tea with chamomile, linden, cranberry juice;
-
provide access to fresh air;
-
to feed in the presence of appetite in small portions of warm food (for example, soup, liquid porridge on the water, a light breakfast).

Also, according to the clinical variant of the course of fever, apply additional cooling measures.
With "red" or "pink" fever
- the child's body feels hot to the touch,
- skin red or pink, moist,
- the child himself does not complain about his well-being, he is active, his appetite does not disappear.
In this case, child needs
- undress,
- wipe with a towel soaked in water at room temperature,
- apply a cool compress to the forehead,
- drink water at room temperature
- and be sure to call a doctor.
With "white or pale" fever
- the child's limbs and body are cold to the touch,
- lips and nail beds become bluish,
- pale and dry skin,
- there is a violation of well-being: the child is lethargic, delirium is possible.
In this case child needs
- warm by rubbing the limbs with hands or using warm water (no other means!),
- put on socks,
- cover with a blanket
- and drink warm tea or water.

The use of antipyretics for such symptoms is ineffective - you need to urgently call a doctor!
An exception is children at risk, who have their temperature reduced above 37.1 degrees. These are children,
- with diseases of the nervous system,
- experiencing convulsions due to fever,
- suffering from chronic diseases of the circulatory system, respiratory organs or with hereditary metabolic diseases and other risks (overheating, symptoms of dehydration, etc.).
Febrile convulsions are diagnosed more often in children under 6 years of age with temperatures above +38 degrees, as well as in children with pathology of the nervous system at any temperature. For such children, it is recommended to lower the temperature to febrile levels (not higher than +38.0) or to those values recommended by a neuropathologist.
Usually, against the background of an increase in temperature, the child's heart rate and respiratory rate increase: the respiratory rate increases by 4 respiratory movements for every degree above +37. 0 degrees, and the pulse rate - by 20 beats per minute for every degree. However, against the background of diseases of the cardiovascular system and respiratory organs, such as malformations or cardiac arrhythmias, inadequate increases or slowdowns in heart rate and respiration are possible. Such children, on the recommendation of a cardiologist and pulmonologist, are prescribed antipyretic drugs to febrile numbers (ie, not higher than +38.0 degrees).
0 degrees, and the pulse rate - by 20 beats per minute for every degree. However, against the background of diseases of the cardiovascular system and respiratory organs, such as malformations or cardiac arrhythmias, inadequate increases or slowdowns in heart rate and respiration are possible. Such children, on the recommendation of a cardiologist and pulmonologist, are prescribed antipyretic drugs to febrile numbers (ie, not higher than +38.0 degrees).
Children with hereditary metabolic diseases (diseases of the thyroid gland, kidneys, liver, disorders in the immune system, and others) and children with imperfect compensatory mechanisms of thermoregulation during fever (these are some children from birth to 2 months) are also prescribed antipyretic drugs on the recommendation of related specialists means to febrile digits.
Overheating - increase in body temperature due to additional exposure to heat
- prolonged sun exposure,
- use of excess clothing,
- excessive wrapping of children).

The danger of overheating is associated with the risk of heat stroke. It manifests itself
- not only in elevated temperature,
- but also in impaired consciousness, convulsions,
- disorders of the heart and breathing.
First aid is to call the ambulance "112".
Until the doctor arrives
- undress the child,
- move to a cool place or shade,
- supply fresh air or fan (not cool air!),
- apply a cold compress to the forehead,
- Wipe the body with cool water or cover with a sheet dampened with cool water.
Antipyretic therapy for children should be prescribed strictly individually, taking into account clinical and anamnestic data.
It is important to know that taking antipyretic drugs does not shorten the duration of the febrile period. At the end of the drug, the temperature rises again.
Antipyretics have a lot of side effects:
- allergic reactions,
- bleeding,
- damage to the stomach (vomiting, regurgitation),
- Reye's syndrome (against the background of rash, vomiting, psychomotor agitation occurs).

In addition, the decrease in body temperature should not be critical, it is not necessary to achieve normal performance. It is enough to lower the temperature by 1.0 or 1.5 degrees, which will improve the child's well-being and avoid collapse.
The collapse develops with a critical (rapid and sharp) decrease in temperature for a short time (from 40-41 degrees to 37-36.0 degrees) by 2.5 - 3.0 degrees or more.
The result is
- acute cardiovascular insufficiency, accompanied by vasospasm and circulatory disorders.
Child feels
- cold or chilly,
- severe weakness,
- headache,
- thirsty,
- he has pale skin up to a bluish tint,
- sticky sweat,
- cold extremities,
- insomnia,
- shortness of breath up to shallow breathing,
- palpitations,
- lowering blood pressure,
- convulsions,
- loss of consciousness.

First aid before the arrival of the doctor:
- put the child in such a way that the head is not raised, and the legs are on the pillow (30-40 cm above the head).
- Warm up by covering the child with heating pads,
- shelter,
- rub limbs with hands,
- drink warm sweetened herbal tea, water,
- change underwear and bed linen.
It is also important to know that antipyretics should not be used in courses, as this makes it difficult to diagnose a child's disease. An increase in temperature is often the only manifestation of a violation of the child's health. Therefore, a doctor's examination and additional examinations are necessary.
Constipation in children. Prevention. Diet therapy
Medical examination before kindergarten and school
Return to the list
Child has high temperature. What to do?
High temperature is a protective reaction of the body, which enhances the immune response.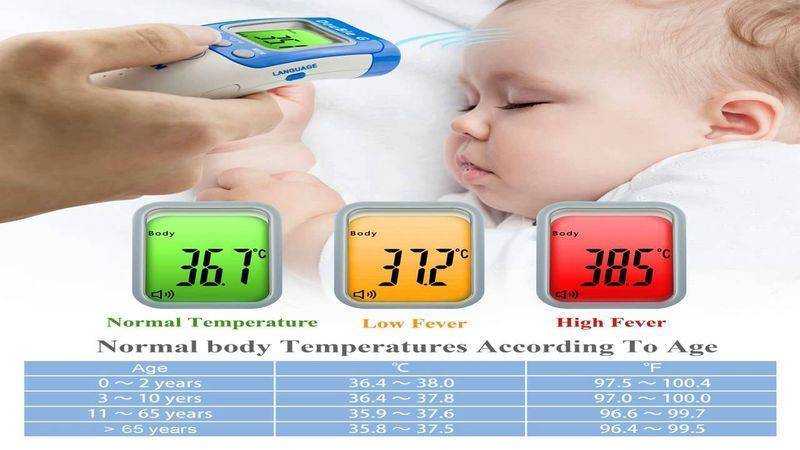
In our body, the hypothalamus is responsible for the mechanism of temperature regulation.
This tiny area in the head is made up of a huge number of nerve cells. They regulate the activity of the cardiovascular, endocrine, digestive and excretory systems of a person.
The hypothalamus is responsible for sleep, wakefulness, hunger, thirst, the reproductive system, pleasure, expression of emotions, social interaction and regulates body heat exchange.
Normally, the hypothalamus maintains the temperature of a healthy person within 36-37°C. Through receptors on the skin, it reacts to cold or heat, and also to any changes in blood temperature.
As soon as the body is attacked by viruses or bacteria, our cells release pyrogens - substances that raise the temperature.
A person begins to shiver - so the muscles contract in the hope of warming up, and the vessels in the skin narrow to reduce heat loss.
That is why an increase in temperature in both adults and children is accompanied by:
- lethargy - active movement leads to heat loss
- shivering - muscles contract to keep body warm
- pallor due to spasm of peripheral vessels
- desire to wrap up warmly
Why is the temperature rising?
The anterior part of the hypothalamus contains thermosensitive nerve cells that respond to any changes in blood temperature and impulses from heat/cold receptors on the skin.
Under the influence of bacteria and viruses, our cells release pyrogens - substances that raise the temperature. When the thermoregulatory center “decides” that there is a need to maintain a higher body temperature than usual, the body begins to “think” how to achieve this.
You can do this in two ways:
1. Increasing heat generation (try to keep warm).
2. Reduced heat transfer (prevent heat from escaping from the body).
Then the following happens. Because of the impulses running through the muscle fibers, a person begins to shiver - this is how the muscles contract in the hope of warming up. At the same time, the vascular-motor center receives information that it is necessary to block the loss of heat. To do this, the vessels in the skin "overlap" (spasm), and heat transfer decreases. Bottom line: the hypothalamus is “happy” that the body temperature remains around 39.0°C.
Thus, a standard feverish child is obtained. He:
He:
- sluggish - the hypothalamus does not allow active movement, because this will lead to heat loss
- trembling - muscle contractions increase heat generation
- pale - pale skin due to spasm of peripheral vessels
- wants to wrap up warmer
But the body is very finely structured - it will not allow you to overheat to a critical point. Therefore, when the temperature set by the hypothalamus is exceeded, the vessels on the periphery expand, the sweat glands are activated, and heat transfer increases.
Now the child blushes, sweats profusely and tries to throw off the blanket as soon as possible.
High body temperature will be maintained until the cause of its increase (infection, tumor, etc.) is eliminated. After the disappearance of the cause, the hypothalamus sets the parameters for a new normal temperature.
How to deal with temperature?
First of all, do not worry and do not rush to bring down the temperature.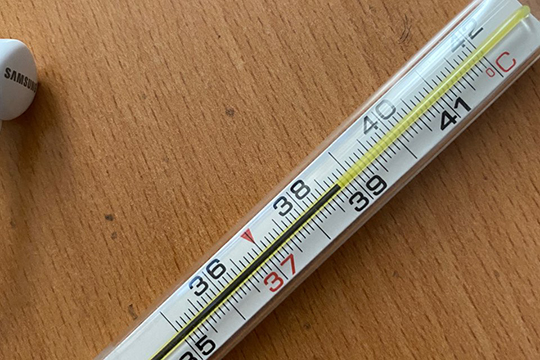 It is important to remember that this is a natural defensive reaction of the body. The child's immune system begins active synthesis of protective substances only at temperatures above 38.5°C.
It is important to remember that this is a natural defensive reaction of the body. The child's immune system begins active synthesis of protective substances only at temperatures above 38.5°C.
First of all, you need to assess the well-being of the child as a whole, his behavior and appearance. This will help you make an informed decision about what to do next.
Fever - always accompanied by other symptoms.
Regardless of the degree of temperature and the age of the baby, there are symptoms that require an immediate examination by a pediatrician:
- atypical behavior - high-pitched crying, drowsiness, groans
- severe headache
- convulsions
- disturbance of consciousness
- lowering blood pressure
- persistent vomiting or diarrhea
- abdominal pain
- sore throat or ear
- impossibility of bending the head to the chest (this causes sharp crying)
With the manifestation of such conditions, one antipyretic therapy is not enough. It can even hurt. Timely examination by a pediatrician and a thorough diagnosis are necessary.
It can even hurt. Timely examination by a pediatrician and a thorough diagnosis are necessary.
It is important to consider the age of the child with fever.
It is better not to postpone a visit to the doctor:
If it seems to mom or dad that something is wrong with the child, it is better to play it safe and get an examination as soon as possible.
When is it necessary to lower the temperature?
1. The child, regardless of the height of the temperature, does not feel well (the main task is to alleviate his condition).
2. A child with chronic somatic diseases (pathologies of the heart, lungs, brain or nervous system).
If a child older than 3 months has a rectal temperature below 38.9 ° C and at the same time feels well, it is not advisable to bring down the temperature. It is important to understand that an increase in body temperature is a natural protective reaction of the human body. The immune system begins active synthesis of various protective substances only at a temperature of about 39°C.
In any case, if there is no certainty in the need for antipyretic therapy, you should seek the advice of a pediatrician.
How to lower the temperature?
It is important to understand that taking antipyretics is aimed at alleviating the discomfort of the child. It does not shorten the duration of the disease and does not reduce the risk of complications.
At home, children can bring down the temperature with only two drugs - paracetamol (from 3 months) and ibuprofen (from 6 months).
All antipyretic drugs should be dosed not by age, but by weight of the baby.
A single dosage of paracetamol is calculated at 10-15 mg/kg of weight, ibuprofen 5-10 mg/kg of weight.
If the antipyretic in the form of a suspension is ibuprofen (in 5 ml - 100 mg), paracetamol (in 5 ml - 120 mg), then you need to divide the amount calculated by weight in mg by the amount of the drug in 1 ml.
Ibuprofen can be taken - 3-4 times a day, paracetamol - 4-5 times.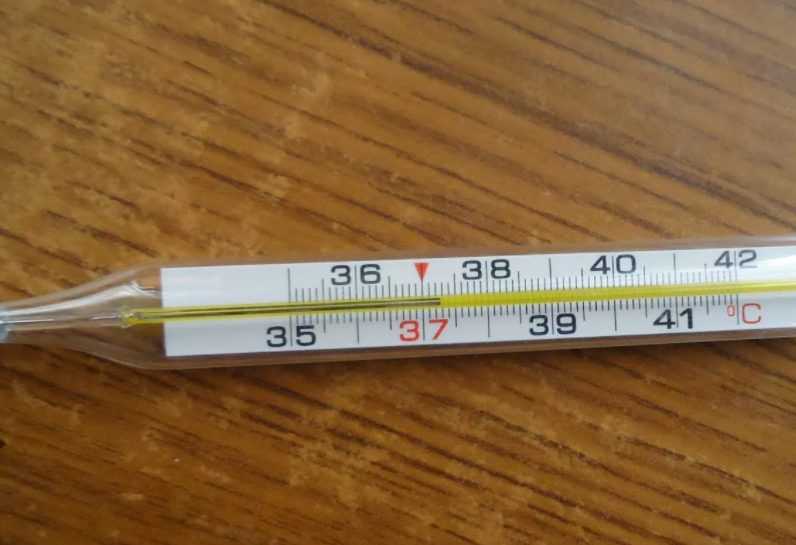
Let's note one important nuance. Do not bring down the temperature with ibuprofen to a child with chickenpox (chickenpox). This drug can lead to a more severe course of the disease.
How to give an antipyretic?
There are several rules for taking antipyretic drugs:
1. Give an antipyretic no more than 5 times a day.
2. A child under 3 months old should not bring down the temperature without a doctor's examination.
3. Do not give combined antipyretic drugs, such as ibuprofen + paracetamol.
4. Carefully read labels and instructions for preparations.
5. Shake the vial before giving the drug to a child.
6. Before taking the drug, make sure that the dosage is correct. A small dosage will lead to a decrease in effectiveness, and an overdose can cause various side effects.
7. Do not use a teaspoon for calculation (different spoons have different capacities). For measurement, it is better to give preference to a measuring spoon or dosing syringe.