Where does milk come out of the nipple
How Breast Milk is Made
Did you know your body gets ready for breastfeeding before you even give birth? While you are pregnant, your breasts change. These changes allow your breasts to make milk and may cause them to feel fuller and more tender.
Once your baby is born, their suckling releases hormones in your body that cause your breasts to make and release milk.
If you are concerned that your milk has not come in or that you are not making enough milk, speak with WIC breastfeeding staff.
Role of Your Breasts
Milk production occurs within the alveoli, which are grape-like clusters of cells within the breast. Once the milk is made, it is squeezed out through the alveoli into the milk ducts, which resemble highways. The ducts carry the milk through the breast.
The size of your breasts does not affect your ability to breastfeed. Women with small breasts make the same quantity and quality of milk as women with larger breasts.
Role of Your Brain
When your baby suckles, it sends a message to your brain. The brain then signals the hormones, prolactin and oxytocin to be released. Prolactin causes the alveoli to begin making milk. Oxytocin causes muscles around the alveoli to squeeze milk out through the milk ducts.
When milk is released, it is called the let-down reflex. Signs of milk release are:
- Tingling, fullness, dull ache, or tightening in the breasts (although some moms do not feel any of these sensations).
- Milk dripping from the breast.
- Uterine cramping after you put baby to the breast during the first few days after birth.
To encourage your milk to release, try these methods:
- Find ways to relax, such as going to a calm place or trying deep breathing.
- Place a warm compress on your breasts before breastfeeding.
- Massage your breasts and hand express a little milk.
After you've been breastfeeding for a while, the let-down reflex can happen for many other reasons, like when you hear your baby cry, or you see or think of your baby. It also can happen at the time of day you usually breastfeed your baby, even if your baby is not around.
It also can happen at the time of day you usually breastfeed your baby, even if your baby is not around.
Role of Your Baby
Your baby helps you make milk by suckling and removing milk from your breast. The more milk your baby drinks, the more milk your body will make. Frequent breastfeeding or milk removal (8-12 times or more every 24 hours), especially in the first few days and weeks of your baby's life, helps you make a good milk supply.
Your milk will continue to vary according to your baby's needs. Each time your baby feeds, your body knows to make more milk for the next feeding. The amount of milk you make will go up or down depending on how often your baby eats. By nursing for as often and as long as your baby wants, you are helping your body to make more milk. At first, it might feel like you are doing nothing but breastfeeding. Soon, you and your baby will get into a pattern that works for both of you.
10 interesting facts about breastfeeding
Think you know everything there is to know about breastfeeding? Think again! Even if you’ve already learned a lot about lactation, you might be surprised by some of the details of just how nature’s all-Baby-can-eat-buffet works. Some facts are fun, some are downright fantastic, and some might seem a little weird. But if you’re thinking of breastfeeding once your baby arrives, you’ll want to be aware of all that could be in store.
Some facts are fun, some are downright fantastic, and some might seem a little weird. But if you’re thinking of breastfeeding once your baby arrives, you’ll want to be aware of all that could be in store.
When you feed your baby, your body’s working overtime! Experts estimate that it takes about 25% more energy to make your breast milk for each day. That’s a serious increase — even from pregnancy — and you’ll feel the hunger and thirst. It’s important to eat well and get enough energy on board! It’s also estimated that protein requirements specifically go up by at least 15 grams. Pro tip: keep taking your prenatal vitamin and talk to your provider about other supplements you may need while breastfeeding!
Hearing a baby cry could make your breasts start to leakWhen your baby latches onto your breast, her sucking triggers release of the hormone oxytocin, which stimulates milk production. This release of breast milk, called the let-down reflex, usually happens after Baby has been sucking for about 1-2 minutes. Some people feel the let-down reflex as a tingling or a warmth and others don’t feel anything at all! But other stimuli can trigger the production of oxytocin too, including emotional ones like looking at a picture of Baby, thinking of her, or hearing a recording of her. Sometimes hearing any baby cry, not just your own, can trigger your let-down reflex. This can be awkward or messy, but it’s just your body’s way of knowing what to do when a baby needs milk!
Some people feel the let-down reflex as a tingling or a warmth and others don’t feel anything at all! But other stimuli can trigger the production of oxytocin too, including emotional ones like looking at a picture of Baby, thinking of her, or hearing a recording of her. Sometimes hearing any baby cry, not just your own, can trigger your let-down reflex. This can be awkward or messy, but it’s just your body’s way of knowing what to do when a baby needs milk!
Not only does Baby’s sucking cause the release of oxytocin so that your milk can flow freely, but oxytocin also creates uterine contractions. Some people don’t really notice these cramps. Others might feel them kick in like clockwork while nursing in the early days after delivery. Although they can be painful, these cramps (also called afterpains) are helpful. When you’re pregnant, your uterus — a super strong muscle — has to grow much larger to make room for Baby, and the contractions that cause cramps also help to squeeze your uterus back to its pre-pregnancy size.
Though you might assume otherwise, milk glands are what matter when it comes to milk production, not breast size. The larger the breast size, the more fatty tissues that exist, but it doesn’t change the milk glands at all, so someone with an A-cup can actually make the same amount of milk as someone with a double D, they just have less fatty tissue compared to glandular (milk-making) tissue. Even if your bust is on the smaller side, you’re just as likely to be able to make plenty of milk for Baby as someone with a larger size!
Your nipples may get uncomfortableThis isn’t a fun fact, but it’s the truth. While you might hope that breastfeeding will be nothing but smooth sailing, things can be somewhat sore for the first few weeks or longer. Getting Baby to latch onto your breast at all, let alone correctly, can take time, and those initial 8-12 feeding sessions a day with a newborn can leave your nipples feeling sensitive and sore. The discomfort can range from slight tenderness to cracked and bleeding skin as you and your baby learn to latch successfully.
The discomfort can range from slight tenderness to cracked and bleeding skin as you and your baby learn to latch successfully.
Fortunately, most people find that their nipples do feel comfortable in just a few weeks, and as Baby grows and her mouth gets bigger, you might find even more comfort, as she latches on more expertly. In the meantime, you can use nipple salves or balms like lanolin, nipple shields, or warm or cool compresses to provide some relief. Even if those early days are a bit tender, it’s important to get Baby to latch on correctly and have enough time feeding at your breast.
However, certain types of breast pain could be evidence of infection or other problems. And since every person’s experience with breastfeeding is different, do speak to your healthcare provider if you have any questions about what’s normal in terms of discomfort and what might help you feel better. If nipple tenderness or soreness has turned to nipple pain while feeding, that might be a sign that you could use some expert help. A board certified lactation consultant is a great place to start!
A board certified lactation consultant is a great place to start!
The nutritional composition of your milk will change over time to keep up with Baby‘s nutritional needs. The first few days after she is born, instead of what you might usually think of as milk, you’ll actually produce a fluid called colostrum that is rich in protein and antibodies. It will help your baby’s new digestive system function properly, pass along immunity, and help her gain weight. In just a few days, this colostrum will transition to mature milk, first thin and watery and then thicker and creamier. As you continue to feed your baby over the coming months, the composition of this milk will continue to change, providing just the nutrients that Baby needs at that particular time.
Your milk comes from many holes, not just the obvious oneIf you had to guess the spot where breast milk comes out, you might guess that it’s right in the center of the nipple. In reality, milk comes from many openings in the nipple. Called milk duct orifices, these tiny holes usually number from around four to twenty per breast. Babies who are correctly latched onto the breast will have their mouths covering the entire areola, not just the tip of the nipple, so they can drink the milk from these multiple holes without a problem and without too much mess.
In reality, milk comes from many openings in the nipple. Called milk duct orifices, these tiny holes usually number from around four to twenty per breast. Babies who are correctly latched onto the breast will have their mouths covering the entire areola, not just the tip of the nipple, so they can drink the milk from these multiple holes without a problem and without too much mess.
Many folks with breast implants can still breastfeed successfully. Implant incisions made through the armpit or underneath the breast tend to interfere with breastfeeding the least, whereas incisions around the areola can potentially increase problems with feeding like reduced nipple sensitivity or blocked milk ducts. And implant placement below the pectoralis muscle usually leaves the milk glands intact for future feeding.
If your body mods include nipple piercings, the hole created as a result shouldn’t interfere with feedings either. As mentioned above, breastmilk comes from many holes at once, so extra holes won’t cause a problem. Just make sure that you remove your nipple jewelry before breastfeeding. And keep in mind that newer piercings have an increased risk of infection, so they should be fully healed before you attempt breastfeeding.
As mentioned above, breastmilk comes from many holes at once, so extra holes won’t cause a problem. Just make sure that you remove your nipple jewelry before breastfeeding. And keep in mind that newer piercings have an increased risk of infection, so they should be fully healed before you attempt breastfeeding.
Although your breasts will look and feel different as they take on the responsibility of feeding baby, the way your partner views your breasts might not change much. Chances are your breasts may still be a turn-on even though your perspective on your breasts — and sex in general — may be ice cold. For some people, breastfeeding hormones decrease libido or make it feel like your breasts shouldn’t be looked at or touched sexually. It’s important to honor your feelings and communicate with your partner about potentially new, and likely temporary, boundaries for your body.
You might get turned onSpeaking of getting turned-on, arousal during breastfeeding can be a common, if confusing, occurrence. The fact of the matter is that the nipple is an erogenous zone, and erogenous zones usually feel good when stimulated; this doesn’t stop just because you’ve had a baby. Rest assured knowing that even if it’s taboo to talk about and many people experience this physical response. Most importantly, the physical arousal you feel is totally separate from how you feel emotionally towards your baby, so there’s really no need to be weirded out.
The fact of the matter is that the nipple is an erogenous zone, and erogenous zones usually feel good when stimulated; this doesn’t stop just because you’ve had a baby. Rest assured knowing that even if it’s taboo to talk about and many people experience this physical response. Most importantly, the physical arousal you feel is totally separate from how you feel emotionally towards your baby, so there’s really no need to be weirded out.
Have you added a bump picture in Ovia? Try the feature by tapping here!
Reviewed by the Ovia Health Clinical Team
Breastfeeding Bootcamp videos
Read more
- How often should a baby breastfeed?
- How breast milk changes as your baby grows
Sources
- Lisa Marasco. “Common breastfeeding myths.” llli.org. La Leche League International, November 4 2012. Retrieved July 18 2017. http://www.llli.org/nb/lvaprmay98p21nb.html.
- Jahaan Martin. “Nipple Pain: Causes, Treatments, and Remedies.
 ” llli.org. La Leche League International, July 17 2016. Retrieved July 18 2017. http://www.llli.org/llleaderweb/lv/lvfebmar00p10.html
” llli.org. La Leche League International, July 17 2016. Retrieved July 18 2017. http://www.llli.org/llleaderweb/lv/lvfebmar00p10.html - Mayo Clinic Staff. “Breast-feeding tips: What new moms need to know.” Mayo Clinic. Mayo Foundation for Medical Education and Research, November 23 2016. Retrieved July 18 2017. http://www.mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/in-depth/breast-feeding/art-20047138.
- Mayo Clinic Staff. “Post-partum care: What to expect after a vaginal delivery.” Mayo Clinic. Mayo Foundation for Medical Education and Research, March 24 2015. Retrieved July 18 2017. http://www.mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/postpartum-care/art-20047233.
What does the discharge from the nipples say?
Enroll
July 02, 2021 read 3-5 minutes
Are you not pregnant or breastfeeding, but have you noticed discharge from your nipples? They can be both completely harmless and speak of a serious illness. The first thing you should pay attention to is their color. And in any case, you should consult a mammologist. By the way, and without any unpleasant symptoms, you should visit it annually. nine0003
The first thing you should pay attention to is their color. And in any case, you should consult a mammologist. By the way, and without any unpleasant symptoms, you should visit it annually. nine0003
What does the color say?
Dairy
The most common. Galactorrhea is a condition in which a woman has milk or milky discharge from her nipples, even if she is no longer breastfeeding. This is the result of an overproduction of the pituitary hormone prolactin. Also, milky discharge may be associated with a recent cessation of breastfeeding or hormonal changes before menopause. Hormone therapy (birth control pills) and sedatives can also affect the breasts in a similar way. Abundant milky discharge from both nipples can be caused by a benign tumor of the pituitary gland (prolactinoma). nine0003
Bloody
One of the reasons is a benign tumor (papilloma), which can irritate the tissues inside the milk duct. In rare cases, spotting has been associated with breast cancer, especially in older women.
Transparent
Discharge from both mammary glands, as a rule, does not pose a threat to health, but if you find them in only one breast, you should contact an oncologist. nine0003
Greens
This color may be a symptom of a cyst, a blocked milk duct, or an infection in the breast. It is also one of the signs of fibrocystic disease.
yellow
Mastitis is a breast infection that causes a yellow-green, pus-like discharge accompanied by fever and chest pain. If the discharge has an unpleasant odor, this may indicate an abscess. nine0003
Not only in women
Men can also experience discharge from the nipples. Some of the common causes include: testosterone deficiency, gynecomastia, a condition that causes breasts to become enlarged and tender, a pituitary tumor, and breast cancer.
How is the examination carried out?
First of all, the specialist will conduct a clinical examination of the breast.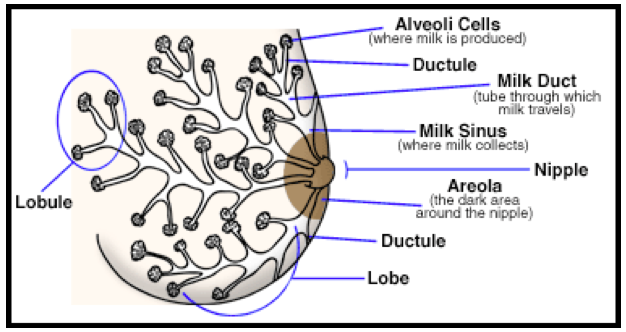 Then, perhaps, he will prescribe a mammogram and an ultrasound of the mammary glands to find the source of the discharge, and also take a smear for cytology. Can offer a ductogram (an X-ray method with the introduction of a contrast agent into the ducts of the mammary gland). nine0003
Then, perhaps, he will prescribe a mammogram and an ultrasound of the mammary glands to find the source of the discharge, and also take a smear for cytology. Can offer a ductogram (an X-ray method with the introduction of a contrast agent into the ducts of the mammary gland). nine0003
The data obtained will tell you if a biopsy is needed. In non-pregnant patients who have abundant milk discharge from both breasts, a blood test is taken to measure the level of the hormone prolactin.
Ultrasound specialist Mammologist Oncologist
Source Ornament
Other articles by this author
How to monitor the health of the mammary glands? nine0047
Text provided incomplete. You can read the entire article on FORM - SBER EAPTEKI's blog. There are many methods for checking mammary glands, but not all of them are effective. We tell you what tests mammologists recommend and why they are needed, as well as at what age and with what complaints they should be done.
Do It Like It Was: Why Celebrities Are Getting Rid of Breast Implants
Text not provided in full. You can read the entire article on RBC Style. Removal of breast implants is a trend that has been gaining momentum over the past couple of years. Together with a mammologist, we understand why the stars go for it and how the operation affects breast health. nine0003 Read article
What should I do if my breasts are out of shape?
Galina Reshettsova, a mammologist at GMS Clinic, Candidate of Medical Sciences, told why breasts sag and whether it is possible to somehow maintain the shape of the breast.
Read articleThe structure of the mammary glands | Lactating mammary gland | Study
Dr. Donna Geddes of the University of Western Australia began to have doubts about textbook anatomical images while doing an ultrasound scan of her lactating breasts. The standard model of the mammary gland was based on the anatomical dissection of cadavers, which was carried out in 1840 by Sir Astley Cooper.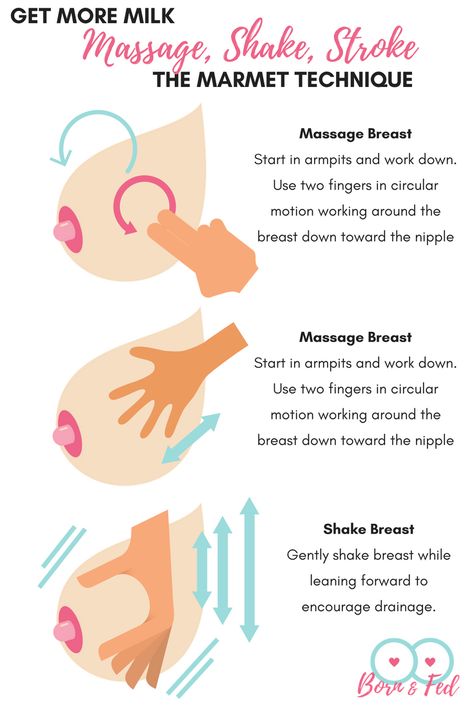 With the support of Medela, additional state-of-the-art studies have been carried out, and their results have changed our understanding of the lactating breast. nine0003
With the support of Medela, additional state-of-the-art studies have been carried out, and their results have changed our understanding of the lactating breast. nine0003
Share this information
Key Findings
A study by the University of Western Australia has led to some groundbreaking discoveries that have significantly changed much of the previous understanding of the structure of the lactating mammary gland.
Main results of the study
- The mammary gland has from 4 to 18 duct openings (previously it was thought that there were 15–20 of them). nine0071 Closer to the nipple, the ducts branch.
- Traditionally described lactiferous sinuses do not exist.
- Ducts may be located closer to the surface of the skin, which allows them to be more easily compressed.
- Most of the glandular tissue is located within 30 mm of the nipple.
The illustration developed by Medela based on these new discoveries is now used in many textbooks and websites.
Practical value
There are three main points to consider when it comes to lactation.
- A quick initial milk flow is essential for effective milk extraction.
- Breast shields must be individually sized for each mother.
- When supporting the breast during pumping, hand position is very important.
1. A quick and efficient initial milk flow is essential for optimal milk recovery
Since the study did not confirm the presence of the lactiferous sinuses, large volumes of milk cannot be stored in the ducts, therefore, only a very small amount of milk can be extracted before the flow of milk. It is known that at the beginning of feeding the baby sucks quickly, which stimulates the secretion of milk. Research shows that an initial rapid rush of milk then causes a succession of subsequent flushes. In fact, when using a breast pump with biphasic pumping technology, at the most comfortable level of vacuum, 80% of the milk is extracted from the breast in the first 7 minutes (Kent et al 2008).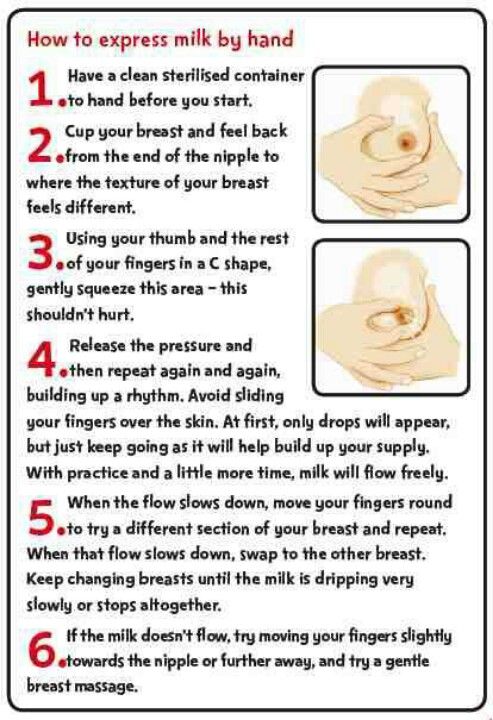 nine0003
nine0003
That is why it is important to ensure that the baby is properly latch-on and to use a breast pump that can effectively stimulate milk production in order to stimulate the flow of milk during breastfeeding.
2. Breast shields must be individually sized.
A properly fitting breast shield will not compress the superficial milk ducts and will ensure efficient breast emptying.
3. Hand position for breast support or pumping
Since 65% of the glandular tissue is within 30 mm of the nipple and the milk ducts are fairly close to the surface, it is important to consider the position of the hands and fingers when feeding or pumping. Constriction of the ducts and tissues can interfere with the free movement of milk from the breast, lead to blockage and, in turn, to swelling of the mammary glands, and then to a decrease in the amount of milk. When milk is not removed from the breast, a protein called a feedback lactation inhibitor (FIL) is produced.