Big hard boob
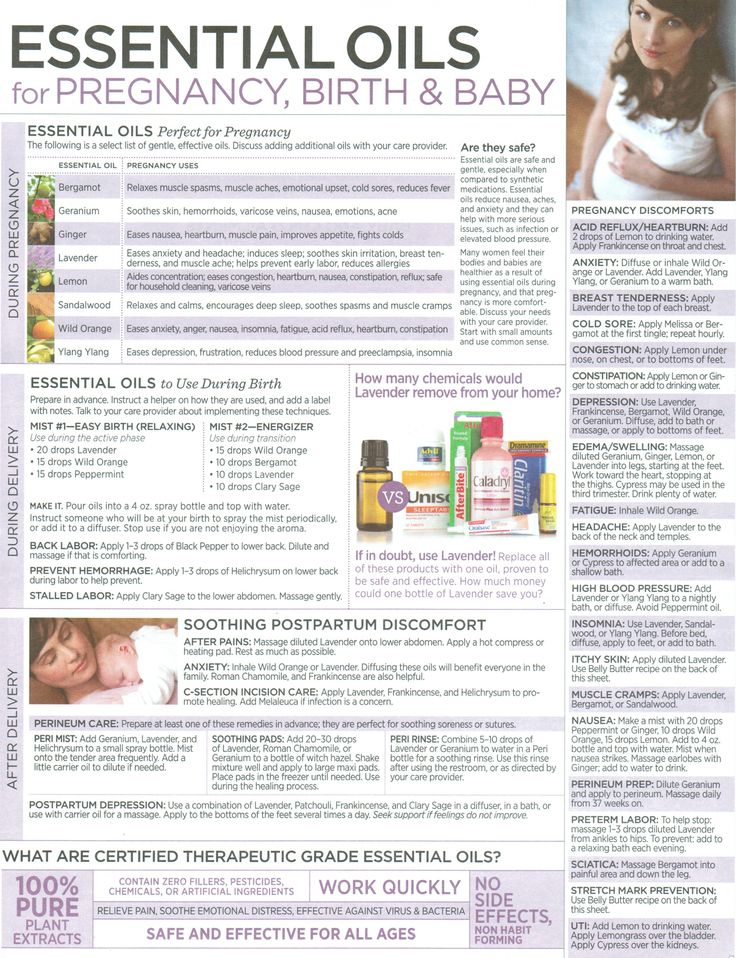
7 Possible Causes and When to See a Doctor
It’s natural to feel concerned when you notice changes in your breasts. But rest assured, breast changes are a normal part of female anatomy.
If your breasts are feeling heavier than usual, it’s probably not anything to worry about. Keep in mind that breast heaviness is rarely a sign of cancer.
Here’s the lowdown on some of the more common culprits behind breast heaviness.
Fibrocystic breast changes are very common. According to the Mayo Clinic, half of women experience them at some point in their lives. This noncancerous condition can cause a variety of changes in the breasts, including the accumulation of water in the breast tissue. When your breasts swell and fill with fluid, they’ll feel heavier than usual.
These changes can happen in one or both breasts. They might occur every month at a certain point in your cycle or follow no discernable pattern. In some cases, you might have constant symptoms.
Other common symptoms of fibrocystic breast changes include:
- free-moving lumps
- pain or tenderness that’s often worse right before your period
- pain that extends into your armpit or down your arm
- the appearance or disappearance of lumps or lumps that change size
- green or brown nipple discharge
As cysts appear and disappear in your breasts, they can cause a scarring and thickening of the breast tissue, called fibrosis (fibrosis). You can’t see these changes, but they can make your breasts feel lumpy or heavier than they used to.
Breast pain and swelling often follow a monthly pattern that’s clearly connected to your menstrual cycle. This is known as cyclical breast pain.
In the days leading up to your period, your estrogen and progesterone levels can fluctuate dramatically. Estrogen and progesterone increase the size and number of ducts and glands in the breast. They also cause your breasts to retain water, making them heavy and tender.
These types of cyclical breast changes usually affect both breasts. Symptoms may get progressively worse in the two weeks leading up to your period, and then disappear.
You may notice:
- swelling and heaviness
- a heavy, dull, and aching pain
- lumpy breast tissue
- pain that radiates to the armpit or outside the breast
Breast swelling is sometimes one of the first signs of pregnancy. Your breasts can begin to swell about one to two weeks after conception.
Swelling occurs because of the hormonal changes happening in your body. They can cause the breasts to feel heavy, achy, and tender. Your breasts might also appear larger than usual.
If you have breast swelling and heaviness accompanied by a late period, then you may want to consider taking a pregnancy test.
Other early symptoms of pregnancy include:
- missing one or more periods
- light spotting
- nausea or vomiting
- fatigue
If you’re pregnant, your breasts will continue to grow up to, and even past, your due date. In the final stretch of your pregnancy, they may become even heavier as your body prepares for breastfeeding. Learn more about breast changes during pregnancy.
If you’re breastfeeding, then you’re probably getting used to the feeling of full, heavy breasts and painful nipples. Breastfeeding is challenging, but it can be particularly difficult when you experience an oversupply of milk.
The feeling of fullness and heaviness can sometimes progress into a condition called engorgement. Engorgement happens when too much milk builds up in your breast. It can be very painful.
Engorgement happens when too much milk builds up in your breast. It can be very painful.
Other symptoms of engorgement include:
- breast hardness
- tenderness
- warmth
- throbbing pain
- redness
- flattened nipple
- low-grade fever
Engorgement is common during the first week of breastfeeding, but it can happen at any time. It’s more likely to occur when you aren’t feeding your baby or pumping often enough.
Certain medications can cause breast-related side effects. The most common sources are hormonal medications such as birth control pills, fertility treatments, and hormone replacement therapy.
Hormonal medications work in different ways to regulate your hormone levels. Fluctuations in your levels of either estrogen or progesterone can cause fluid retention in your breasts, making them feel heavy.
Certain antidepressants have also been connected with breast symptoms, namely pain. These include selective serotonin reuptake inhibitors (SSRIs), such as sertraline (Zoloft) and citalopram (Celexa).
Breast infections, known as mastitis, are most common among those who are breastfeeding. Mastitis can cause inflammation, leading to swelling and feelings of heaviness in the affected breast.
It tends to happen when milk becomes stuck in the breast, allowing bacteria to grow out of control. This can happen because of a blocked milk duct or when bacteria from your skin or your baby’s mouth enter your breast through your nipple.
Symptoms of mastitis include:
- tenderness
- breasts that are warm to the touch
- swelling
- pain or burning (can be constant or only while breastfeeding)
- a lump in the breast or thickening of breast tissue
- redness
- sick, rundown feeling
- fever
Heaviness usually isn’t a breast cancer symptom. The exception to this is inflammatory breast cancer. Still, it’s the least likely cause breast heaviness.
Inflammatory breast cancer is very rare, making up only about 1 to 5 percent of all breast cancers, according to the National Cancer Institute. It’s an aggressive cancer that often comes on quickly. As a result, you’ll likely experience some other symptoms as well.
It’s an aggressive cancer that often comes on quickly. As a result, you’ll likely experience some other symptoms as well.
This type of breast cancer causes redness and swelling of the breast tissue. Sometimes the breast can increase dramatically in size and weight in a matter of weeks.
Other symptoms of inflammatory breast cancer include:
- swelling and redness covering a third or more of the breast
- breast skin that looks bruised, purplish, or pink
- breast skin that resembles an orange peel
- burning or tenderness
- nipple turning inward
- swollen lymph nodes
It’s perfectly normal for your breasts to feel heavy from time to time, but it never hurts to get things checked out. If you’re worried it could be something serious, speaking with a doctor will definitely help. If you don’t already have a primary care provider, you can browse doctors in your area through the Healthline FindCare tool.
Keeping track of how your breasts feel throughout the month may also provide some peace of mind if you find that the heaviness seems to occur the week or so before your period. If that’s the case, an over-the-counter pain reliever, like ibuprofen (Advil), should offer some relief.
If that’s the case, an over-the-counter pain reliever, like ibuprofen (Advil), should offer some relief.
But in some cases, it’s definitely best to make an appointment as soon as possible. Infections, for example, can only be treated with prescription antibiotics.
If you’re in pain, either constantly or intermittently, your doctor can help figure out the cause of your pain, whether its your menstrual cycle or something else. They can recommend medications that will help regulate your hormones or dosage adjustments that may work better than your current treatments.
If you’re taking an SSRI, your doctor may recommend switching to a different antidepressant with fewer side effects or adjusting your dosage.
If you’re having trouble breastfeeding, your best bet is to speak with a lactation consultant. They can advise you on how often to feed or pump each breast and how to be sure your breast empties. You can ask your doctor for a referral or search the International Association of Lactation Consultant Association’s directory.
Any new lump that doesn’t resolve on its own within a few weeks should be checked out by a doctor. It can be hard to tell the difference between a benign cyst and a cancerous tumor.
Fibrocystic breast changes can be alarming, and it isn’t possible for you to tell the difference between a cyst from a tumor. While cysts tend to be softer, more painful, and easier to move, that’s not always the case. Only a doctor can tell you for sure.
Warning signs
Keep in mind that breast heaviness alone is very rarely a sign of a serious problem.
But if you notice the following symptoms, it’s best to see a doctor as soon as possible:
- a hard, pain-free lump
- redness or discoloration of your breast
- pain or burning while breastfeeding
- a fever
- a flattening or inversion of the nipple
- blood leaking from your nipples
- severe fatigue or rundown feeling
As well, see a doctor if your family has a history of breast cancer or you’ve had breast surgery in the past.
What Does a Hard Lump in the Breast Mean?
Breast lumps are very common. Fortunately, they’re not always a cause for concern. Ordinary reasons such as hormonal changes can cause breast lumps that appear and disappear on their own.
Over 1 million women have breast biopsies each year. According to the U.S. Agency for Healthcare Research and Quality, these tests show that up to 80 percent of lumps are benign, or noncancerous.
While you can’t determine on your own whether a lump is cancerous or not, you can learn some signs to look out for. These signs can tell you if a lump might be concerning and help you decide when to seek medical care.
You might be worried if you discover a lump in your breast, but lumps aren’t always a sign of a serious condition. Most breast lumps aren’t caused by cancer, especially if you’re under 40 years old and haven’t had breast cancer in the past.
Breasts are made up of many parts, including:
- nerves
- blood vessels
- connective tissue
- glandular tissue
- milk glands
- milk ducts
- fat
Together, these can make breasts feel uneven and lumpy.
Hard breast lumps will feel different from your typical breast tissue. They often have several harmless causes, including:
- hormonal changes during your menstrual cycle
- clogged milk ducts
- infections
Typically, noncancerous lumps will be easy to move and roll between your fingers. Lumps you can’t move and roll with your fingers have a greater chance of being cancerous and are a cause for concern.
Benign breast lumps
A variety of conditions can cause lumps in your breast tissue. Some causes, such as menstrual cycle changes, can create breast lumps that form briefly and go away on their own. Other causes might need medical attention but are not cancer.
Some common and benign reasons for breast lumps include:
- Cysts. A cyst is a fluid-filled sac. They’re generally 1 to 2 inches wide, smooth, and round, with clear, defined edges. Cysts may be tender to the touch, especially during your period. Cysts will often come and go throughout your menstrual cycle.
 But large or painful cysts might need further medical care.
But large or painful cysts might need further medical care. - Lipomas. A lipoma is a fatty lump that can form in your breast tissue. These lumps are generally painless, soft, and easy to move with your fingers. Lipomas are always benign, but your doctor might order a biopsy to confirm the lump is a lipoma and not cancer.
- Fibroadenoma. These benign lumps are most common during your 20s and 30s, but can occur at any age. A fibroadenoma lump generally will be hard and round. You’ll be able to move the lump with your fingers. Sometimes, your doctor will biopsy or remove fibroadenoma lumps to make sure they’re not cancerous. In many cases, they can be left untreated without causing harm.
- Fibrocystic changes. These changes are caused by hormonal fluctuations and are very common in women ages 30 to 50. They can cause your breasts to feel tender, fibrous, and rubbery. They might also cause fluid-filled cysts to form. Fibrocystic changes often occur in middle age and can sometimes be treated with birth control or dietary changes.

- Fat necrosis. Fat necrosis happens when the fatty tissue of your breast is injured. It can cause round, firm lumps or cysts to form. Fat necrosis lumps sometimes need surgical removal.
- Mastitis. Mastitis is an infection of the breast tissue, such as a milk duct. It’s most common in women who are breastfeeding. Mastitis can cause your breast to be lumpy, swollen, warm, and red, and may give you a fever. In most cases, it can be treated with antibiotics. In some cases, your doctor might want to do a biopsy to make sure your symptoms aren’t caused by cancer.
Precancerous breast lumps
Some breast lumps are caused by conditions that aren’t cancer but still call for medical attention. If these lumps don’t get treatment, they can increase your risk of cancer or even progress into cancerous tumors.
Common types of precancerous breast lumps include:
- Intraductal papillomas. These tumors form in the milk ducts and are usually benign.
 However, they are associated with an increased risk of cancer. They often cause nipple discharge along with lumps.
However, they are associated with an increased risk of cancer. They often cause nipple discharge along with lumps. - Hyperplasia. Breast hyperplasia can be located in the fatty tissue of your breast (lobular hyperplasia) or the ducts (ductal hyperplasia). It causes lumps that aren’t cancerous, but can become cancerous without treatment. Hyperplasia lumps need to be removed as soon as possible.
- In situ tumors. Just like hyperplasia lumps, in situ tumors can form in the fatty tissue (lobular carcinoma in situ) or ducts (ductal carcinoma in situ). These tumors aren’t invasive and are considered stage 0 cancer. They need to be removed before they can progress to an invasive cancer stage.
Breast cancer lumps
Breast cancer lumps are invasive. They’re caused by atypical breast tissue cells that can grow and spread to the rest of your breast, lymph nodes, and other organs.
Early breast cancer usually doesn’t have any signs or symptoms because of its small size. In these cases, it’s most commonly identified on routine screening tests.
In these cases, it’s most commonly identified on routine screening tests.
When breast cancer advances, it often first appears as a single, hard, one-sided lump or thick area under your skin with irregular borders. Unlike benign lumps, you generally can’t move a breast cancer lump with your fingers.
Breast cancer lumps usually aren’t tender or painful to the touch. They most often appear in the upper section of your breast in the area toward your armpit. They can also appear in your nipple area or the lower half of your breast.
Other signs that might point to breast cancer include:
- a lump that is irregularly shaped
- a lump with a dimpled or bumpy surface
- a change in the appearance of your nipples
- a change in the texture of your breasts
- a change in the shape of your breasts, including asymmetry
- open wounds that develop on your breasts without any injuries
- nipple discharge
- nipple tenderness
- nipples that are inverted
- swollen glands in your armpits
Men can also experience hard lumps in their breast tissue. Similar to lumps in women’s breast tissue, lumps aren’t necessarily cancer or a serious condition. For example, lipomas and cysts can cause lumps in men’s breast tissue.
Similar to lumps in women’s breast tissue, lumps aren’t necessarily cancer or a serious condition. For example, lipomas and cysts can cause lumps in men’s breast tissue.
Often, hard breast lumps in men are caused by a condition called gynecomastia. This condition causes men’s breast tissue to become enlarged and can cause a lump to form under the nipple. The lump is often tender and can occur in both breasts.
In some cases, this condition is brought on by hormonal imbalances or a medication, but in other cases, no clear cause can be found.
Fortunately, gynecomastia doesn’t cause medical harm, but it can damage the self-confidence and self-esteem of affected men. Treatment depends on the cause, and might include:
- medications
- weight loss
- surgery
Many causes of breast lumps are benign and can even go away on their own. However, it’s always a good idea to have a breast lump checked out by a medical professional.
For more benign lumps, this can mean simply bringing the lump up with your doctor at your next regularly scheduled appointment. For lumps that might be cancer, it’s best to make an appointment right away.
For lumps that might be cancer, it’s best to make an appointment right away.
There are several signs to look for that can indicate that a lump may be cancerous. Use them to decide when to seek treatment.
When to bring a lump up at your next physical
Some breast lumps aren’t harmful and can wait to be discussed with your doctor. These include lumps that:
- shrink and grow during your menstrual cycle
- are tender or painful
- can be easily moved with your fingers
It’s best to always trust your instincts when it comes to a breast lump. If your lump meets these criteria, but something doesn’t feel right, make a medical appointment right away. While most breast lumps aren’t cancer, it’s a good idea to get something checked out, especially if you’re concerned about it.
When to make an appointment for a breast lump
If a breast lump could be harmful, make an appointment for a medical professional to evaluate it soon. Don’t wait until your next appointment. Signs it’s a good idea to make an appointment include breast lumps that:
Signs it’s a good idea to make an appointment include breast lumps that:
- can’t be moved with your fingers
- grow over time
- don’t cause pain or tenderness
- have bumpy surfaces
When a breast lump is an emergency
A breast lump along with other signs could mean you should seek emergency care. If you have breast cancer that has begun to spread, an appointment can’t wait. It’s best to seek urgent medical care if you have a hard breast lump and:
- you are experiencing bloody nipple discharge
- your nipples have changed appearance or become inverted
- you have a fever
- the glands under your arms are swollen
A lump along with any of these signs doesn’t always mean you have invasive breast cancer or even breast cancer at all. However, because breast cancer is most treatable when it’s caught early, it’s important not to wait.
Again, it’s always best to follow your instincts. If you have a hard lump in your breast and are concerned something is seriously wrong, make an appointment.
Many hard lumps in breast tissue are harmless. They can be caused by hormonal changes and might come and go on their own. These lumps are often easily moved with your fingers and might be tender to the touch. Lumps caused by breast cancer generally don’t cause pain and can’t be easily moved.
It’s a good idea to mention any lump you feel in your breasts to a medical professional. They might want to order a biopsy to find out exactly what it is and get you the best treatment.
Firm breasts: what you need to know?
The female breast consists of three main components: glandular tissue that forms lobules, ducts and connective tissue, which can be either adipose or fibrous. Some women have more fibrous tissue in their breasts than fatty tissue: in such cases, the doctor can diagnose them with dense breasts. nine0006
Some women have more fibrous tissue in their breasts than fatty tissue: in such cases, the doctor can diagnose them with dense breasts. nine0006
Because dense breasts can make cancer detection difficult, it is especially important for women to be aware of their breast density.
Breast density is measured by the amount of adipose tissue in the breast: the more adipose tissue, the less density. According to statistics, 40-50% of women aged 40 to 74 have dense breasts.
According to the National Cancer Institute (USA), women with dense breasts are more likely to have false-negative mammograms. Research has also linked dense breasts to an increased risk of breast cancer. nine0006
Although dense breasts do not in any way guarantee the development of breast cancer, this feature can contribute to its occurrence. Today, doctors are conducting research in which they are trying to find a link between breast density and the occurrence of cancer.
A common misconception about tight breasts is that the breasts are hard or large. However, firm breasts are not necessarily dense. The density of a woman's breasts can change over time. For example, hormonal changes as a woman ages can cause an increase in breast fat. nine0006
However, firm breasts are not necessarily dense. The density of a woman's breasts can change over time. For example, hormonal changes as a woman ages can cause an increase in breast fat. nine0006
There are several risk factors, including:
- Age. The younger the woman, the denser her breasts. Older women usually have less dense breasts.
- Treatment. Women taking hormone replacement therapy after menopause may notice an increase in breast density.
- Genetics. Most likely, mothers and grandmothers of women with dense breasts also had dense breasts.
- Menopause. Due to metabolic and hormonal changes between the ages of 50 and 55, the breast loses its balance between the glandular and fibrous part and fat. nine0007
- Sedentary lifestyle. An increase in body weight increases the risk of dense breasts.
In general, doctors believe that the density of breast tissue is usually determined by genes.
Dense breasts are usually detected during an X-ray examination - mammography, which also uses diagnostic methods such as magnetic resonance imaging, tomosynthesis and ultrasound. A mammogram is an x-ray image of the breast that allows the doctor to identify potentially malignant lesions as well as dense breast tissue. nine0006
A mammogram is an x-ray image of the breast that allows the doctor to identify potentially malignant lesions as well as dense breast tissue. nine0006
Doctors classify the density of breast tissue into four categories:
- Mostly fatty: The breasts are made up primarily of fatty tissue.
- Scattered Density: The breast consists of a small amount of adipose tissue, but there are several areas of fibrous and glandular tissue.
- Consistent density: the breast has many areas of fibrous and glandular tissue that are evenly distributed throughout the breast
- Very dense: the breast contains a lot of fibrous and glandular tissue. nine0007
Although physicians use these four categories to classify breast tissue density, there is no exact formula for classifying breast density into one category or another.
Typically, breast fat will appear dark on x-rays and cancerous lesions will appear white. Very dense breast tissue will also appear white on an X-ray, a similarity that can make it difficult to identify potentially malignant lesions.
There is a possibility that during diagnosis, the doctor may mistake an area of very dense tissue for a tumor. Techniques such as MRI or 3D tomosynthesis may be required to accurately diagnose dense breast tissue or tumors.
There is no way to prevent the development of dense breast tissue. However, a woman can make lifestyle choices that help her reduce her risk of developing breast cancer:
- maintaining a healthy weight
- regular physical activity
- smoking cessation
- alcohol restriction
No drug has yet been developed to reduce breast density and therefore reduce the risk of breast cancer in women.
Your doctor will most likely look at the additional risks of breast cancer at your appointment and recommend the frequency of mammograms. For example, if a woman has dense breasts or has a family history of breast cancer, more frequent mammograms may be needed. nine0006
Women with dense breasts are much more likely to develop breast cancer. Women with dense breasts are 4 to 5 times more likely to develop breast cancer, according to data published by the National Cancer Institute.
Women with dense breasts are 4 to 5 times more likely to develop breast cancer, according to data published by the National Cancer Institute.
Another study published in the journal Cancer shows that women with dense breasts who are diagnosed with breast cancer in one breast are at greater risk of developing cancer in the other.
Women with dense breasts should consult their doctor about their individual risk of developing breast cancer. In this case, her general health and family history must be taken into account. If necessary, the doctor will schedule scanning studies to assess the condition of the breast. nine0006
For example, the American Cancer Society recommends that women aged 45-54 have a mammogram every year. After age 55, some women may switch to a 2-year screening regimen.
In the Professor's Clinic, you can perform diagnostic procedures such as breast ultrasound and analysis for breast cancer tumor markers.
The clinic also receives patients oncologist-mammologist, doctor of the highest qualification category Obolensky Alexander Andreevich, from whom you can get advice on the risks arising from dense breasts.
 P. £r
P. £r  B1
B1  flv
flv  com
com