When to start ivf
IVF - NHS
In vitro fertilisation (IVF) is one of several techniques available to help people with fertility problems have a baby.
During IVF, an egg is removed from the woman's ovaries and fertilised with sperm in a laboratory.
The fertilised egg, called an embryo, is then returned to the woman's womb to grow and develop.
It can be carried out using your eggs and your partner's sperm, or eggs and sperm from donors.
Who can have IVF?
The National Institute for Health and Care Excellence (NICE) fertility guidelines make recommendations about who should have access to IVF treatment on the NHS in England and Wales.
These guidelines recommend that IVF should be offered to women under the age of 43 who have been trying to get pregnant through regular unprotected sex for 2 years. Or who have had 12 cycles of artificial insemination, with at least 6 of these cycles using a method called intrauterine insemination (IUI).
However, the final decision about who can have NHS-funded IVF in England is made by local integrated care boards (ICBs), and their criteria may be stricter than those recommended by NICE.
If you're not eligible for NHS treatment, or you decide to pay for IVF, you can have treatment at a private clinic. Costs vary, but 1 cycle of treatment may cost up to £5,000 or more.
Read more about the availability of IVF.
Speaking to your GP about IVF
If you're having trouble getting pregnant, you should start by speaking to your GP. They can advise on how to improve your chances of having a baby.
If these measures don't work, your GP can refer you to a fertility specialist for a treatment such as IVF.
Read more about getting started with IVF.
What happens during IVF
IVF involves 6 main stages:
- suppressing your natural cycle – your menstrual cycle is suppressed with medicine
- helping your ovaries produce extra eggs – medicine is used to encourage your ovaries to produce more than 1 egg at a time
- monitoring your progress and maturing your eggs – an ultrasound scan is carried out to check the development of the eggs, and medicine is used to help them mature
- collecting the eggs – a needle is inserted through your vagina and into your ovaries to remove the eggs
- fertilising the eggs – the eggs are mixed with the sperm for a few days to allow them to be fertilised
- transferring the embryo(s) – 1 or 2 fertilised eggs (embryos) are placed into your womb
Once the embryo(s) has been transferred into your womb, you'll need to wait 2 weeks before taking a pregnancy test to see if the treatment has worked.
Read more about what happens during IVF.
Chances of success
The success rate of IVF depends on the age of the woman having treatment, as well as the cause of the infertility (if it's known).
Younger women are more likely to have a successful pregnancy. IVF isn't usually recommended for women over the age of 42 because the chances of a successful pregnancy are thought to be too low.
In 2019, the percentage of IVF treatments that resulted in a live birth was:
- 32% for women under 35
- 25% for women aged 35 to 37
- 19% for women aged 38 to 39
- 11% for women aged 40 to 42
- 5% for women aged 43 to 44
- 4% for women aged over 44
These figures are for women using their own eggs and their partner’s sperm, using the per embryo transferred measure.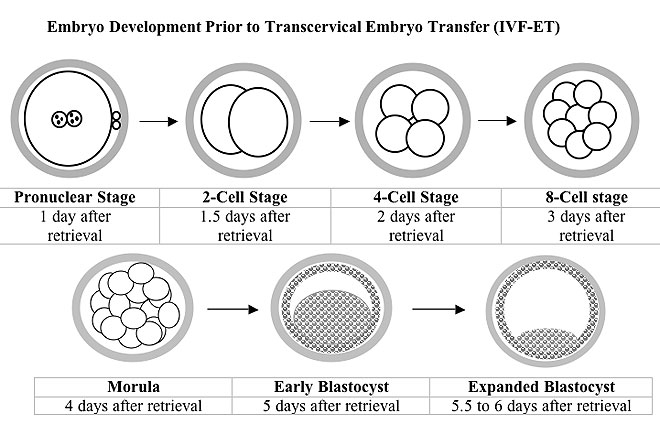
The Human Fertilisation and Embryo Authority (HFEA) has more information about in vitro fertilisation (IVF), including the latest success rates
Maintaining a healthy weight and avoiding alcohol, smoking and caffeine during treatment may improve your chances of having a baby with IVF.
Risks of IVF
IVF doesn't always result in pregnancy, and it can be both physically and emotionally demanding. You should be offered counselling to help you through the process.
There are also a number of health risks involved, including:
- side effects from the medicines used during treatment, such as hot flushes and headaches
- multiple births (such as twins or triplets) – this can be dangerous for both the mother and the children
- an ectopic pregnancy – where the embryo implants in the fallopian tubes, rather than in the womb
- ovarian hyperstimulation syndrome (OHSS) – where the ovaries overreact to the medicines used during IVF
Read more about support available during and after IVF and the risks of IVF.
Page last reviewed: 18 October 2021
Next review due: 18 October 2024
The Process of IVF | Step By Step Through An IVF Cycle
Your step-by-step guide to an IVF cycle
Step 1: Day 1 of your period
Let’s get started!
The first official day of your IVF treatment cycle is Day 1 of your period. Everyone’s body is different; your fertility nurse will help you understand how to identify Day 1.
Your step-by-step guide to an IVF cycle
Step 2: Stimulating your ovaries
The stimulation phase begins on Day 1. In a natural monthly cycle, your ovaries would normally produce one egg. With an IVF cycle, you’ll take medication for eight to 14 days to encourage the follicles in your ovaries (where the eggs grow) to produce more eggs.
Your specialist will prescribe medication specific to your body and treatment plan. This medication usually takes the form of injections. These injections can vary from one-two for the entire cycle, to one-two per day.
These injections can vary from one-two for the entire cycle, to one-two per day.
The idea of injecting yourself can feel daunting at first - we completely understand this. That’s why your fertility nurse will take you through the process step-by-step, showing you exactly how and where to give the injections. It’s a great idea to get your partner or a support person involved too. That way you can watch and learn together. Also take comfort knowing we have additional resources online to guide you when at home.
Trust us - what seems daunting at first quickly becomes a habit. You’ll be an expert in no time.
The most common hormones contained in the injections are:
- follicle-stimulating hormone (FSH)
- luteinizing hormone (LH)
Throughout your cycle, your specialist and fertility nursing team keep a close eye on your ovaries and how the follicles are developing with blood tests and ultrasounds. They’ll adjust your medication if needed. It’s common to have some transvaginal ultrasounds, where a probe is inserted internally to view the ovaries and developing follicles to help fine tune your treatment during the stimulation phase. Our team are there to support you and make you as comfortable as we can.
Our team are there to support you and make you as comfortable as we can.
We’ll monitor you more frequently towards the end of the stimulation phase to time the ‘trigger injection’ perfectly.
The trigger injection is a crucial step in the process. It readies the eggs for ovulation - the natural process where your eggs are released. Your fertility nurse will tell you exactly when to give the trigger injection. The timing is critical, as your fertility specialist needs to perform the egg retrieval before you ovulate.
Your step-by-step guide to an IVF cycle
Step 3: Egg retrieval
The egg retrieval - also known as the egg ‘pick up’ (EPU) - is a hospital day procedure where your fertility specialist collects the eggs from your ovaries. An anaesthetist will give you a general anaesthetic so that you’re asleep for the procedure, which takes about 20-30 minutes.
Your specialist uses the latest ultrasound technology to guide a needle into each ovary.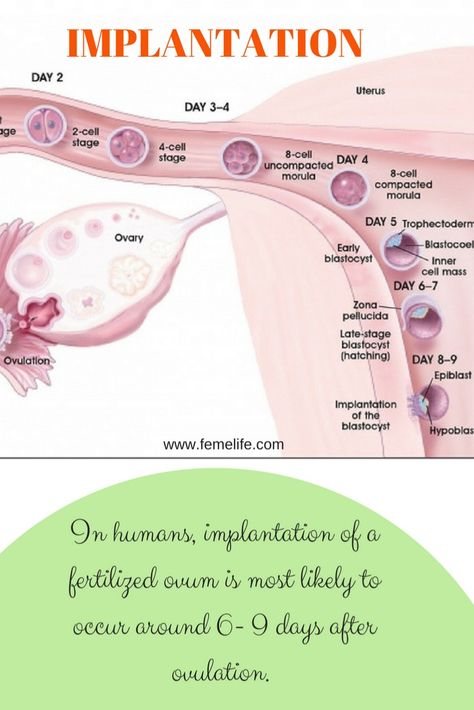 It’s delicate work where every millimetre counts. Our specialists are experts in the field. Eggs are invisible to the naked eye - they’re contained in the fluid-filled follicles in your ovaries. So your specialist will remove fluid from the follicles that look like they’ve grown enough to have an egg inside.
It’s delicate work where every millimetre counts. Our specialists are experts in the field. Eggs are invisible to the naked eye - they’re contained in the fluid-filled follicles in your ovaries. So your specialist will remove fluid from the follicles that look like they’ve grown enough to have an egg inside.
Your fertility team has been monitoring you closely throughout your cycle, so they’ll have a fair idea of how many eggs they expect to retrieve in your procedure. The average number of eggs collected is eight-15, however this is also dependant on your age and clinical history.
After your procedure, you’ll wake up in recovery, where we’ll keep you warm and comfortable. About 30 minutes later you’ll be able to walk out on your own. It’s a good idea to have a support person with you as you won’t be able to drive after the EPU.
Your step-by-step guide to an IVF cycle
Step 4: The sperm
If you’re a couple planning on using fresh sperm, the male will produce a sample the morning of the egg retrieval. If you are using frozen or donor sperm our scientists will have it ready in the lab.
If you are using frozen or donor sperm our scientists will have it ready in the lab.
We grade the sperm using four different levels of quality. The laboratory will prepare the samples to collect the most viable sperm from the sample for combining with your eggs, all so our scientists can spot the best sperm under powerful microscopes. We take great care in preparing the sperm prior to introduction to the eggs with multiple methods at our disposals tailored to each patients sample. The ideal sperm is not too fat or too thin, with a tail that’s not too long or too short and is referred to as having normal morphology (shape/structure). Being able to identify morphologically normal sperm is a skill that our scientists develop over many years, with constant fine tuning, to select the ideal sperm for every egg. Once the sample is prepared we have it ready and we have it ready and waiting in the lab for the next step We then introduce the prepared sperm to the eggs collected in your egg pick up.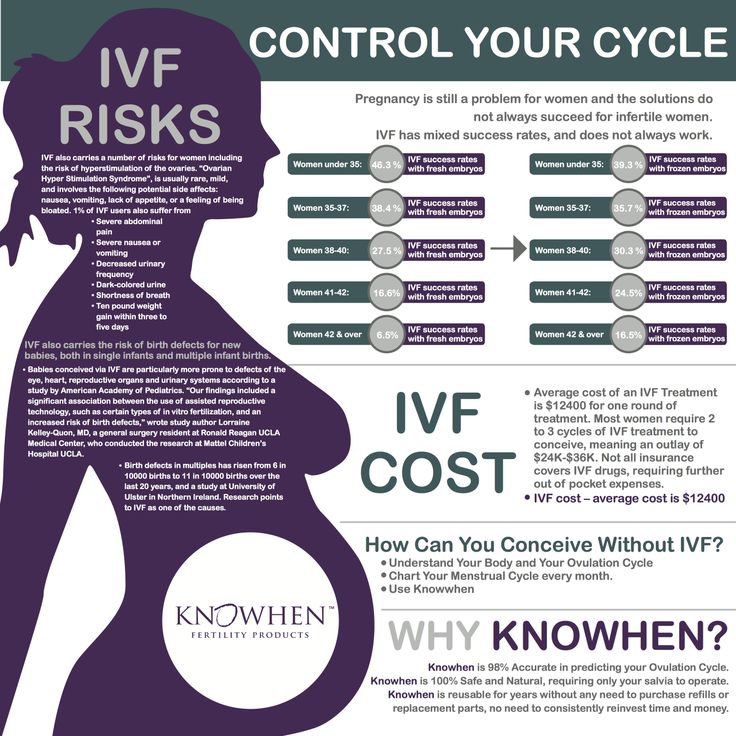
Your step-by-step guide to an IVF cycle
Step 5: Fertilisation
Your fertility specialist gives our scientists the eggs they’ve retrieved from your ovaries. The eggs are contained in tubes of follicular fluid taken from your ovaries. Our scientists use powerful microscopes to find the eggs in the fluid so that they can remove them.
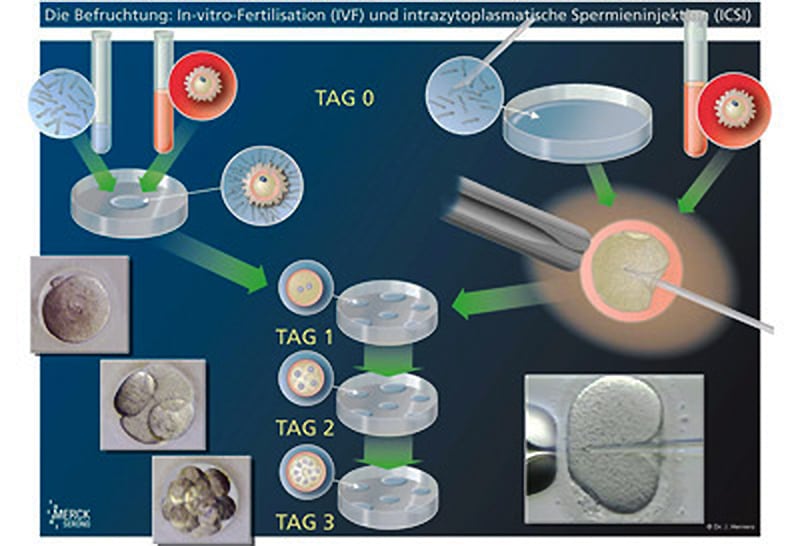
Once the eggs are removed, we culture the eggs in the ideal environment prior to combining with sperm (inseminating) with either standard insemination or Intracytoplasmic sperm injection (ICSI) or a combination of both. Our scientists will either place the eggs and sperm together in a culture dish to fertilise naturally as they would within your own body. This is known as Standard IVF insemination. Another method of insemination is for our scientists to hand select a single “ideal” sperm to inject directly into each individual egg known as ICSI. The method of fertilisation will be directed by your specialist in discussion with your situation to optimise your fertilisation and pregnancy chances in each cycle.
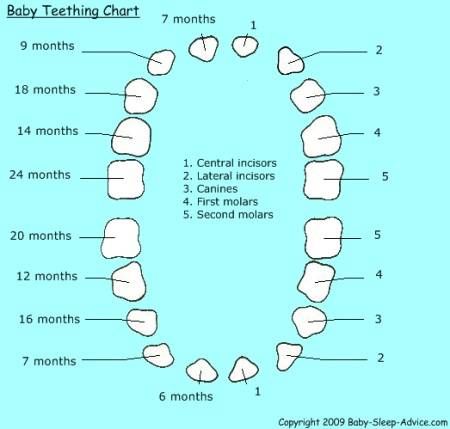
After the insemination procedure, we place the inseminated egg(s) into our specialised culture incubators to assess for fertilisation approximately 17 hours later the next day. We are looking for signs of normal fertilisation - 2 pronuclear bodies known as ‘pronuclei’. These pronuclei are the genetic nucleus from the egg and sperm, so we need to see only two pronuclei. One from the egg and one from the sperm. If the egg does not present with 2 pronuclei, then the egg has not fertilised and will not produce an embryo.
Your step-by-step guide to an IVF cycle
Step 6: Embryo development
Ideally, after combining a sperm with the egg, approximately17 hours later it will fertilise and begin forming an embryo. Our scientists will culture the developing embryo(s) in a special incubator, where the conditions for growth and development are optimised to grow the best possible embryos. .
We create these perfect growing conditions using a special mix of amino acids, and nutrients similar to the ones your own body would use to nurture the embryo. Our goal is to mimic the body’s natural processes as closely as possible.
Our goal is to mimic the body’s natural processes as closely as possible.
Our scientists keep a close eye on the embryo’s development over the next five-six days. They’re aiming to see:
- a two- to four-cell embryo on day two
- a six- to eight-cell embryo on day three (called the cleavage stage)
- an embryo of roughly 100 cells by day five or six (called the blastocyst stage)
Our goal is to grow all embryos to the blastocyst stage. We know that transferring more robust and developed embryos into the uterus boosts your chances of a successful pregnancy.
Unfortunately, not all eggs will fertilise and reach each embryo stage. The eggs might not be mature, or the sperm mightn’t be strong enough.
We know you’ll be eager for news along the way. Rest assured, we’ll keep you up-to-date on how your eggs, sperm and embryos are developing. In the meantime, if you have any questions—our friendly team are just a phone call away.
Your step-by-step guide to an IVF cycle
Step 7: Embryo transfer
If your embryo develops in the lab, the next step is to transfer it into your uterus in a simple procedure known as an ‘embryo transfer’.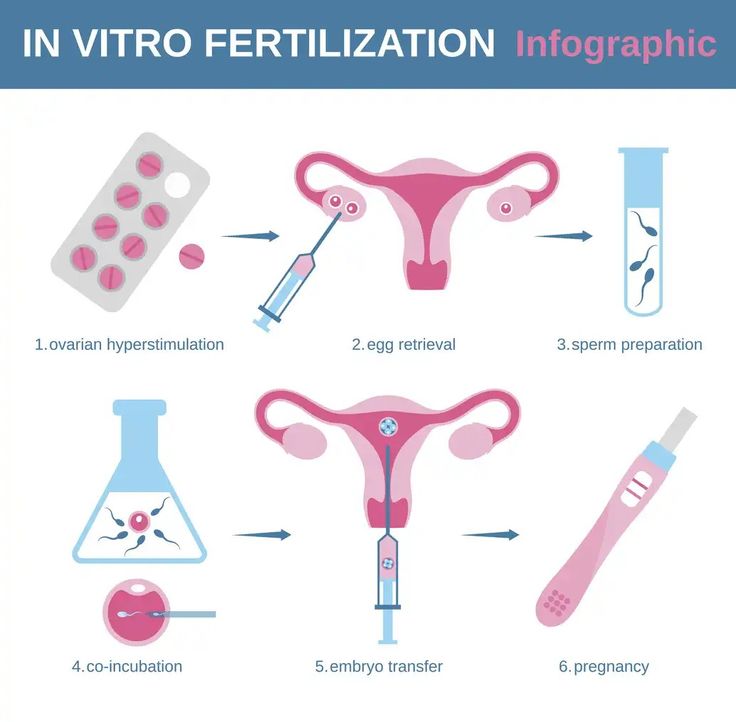
Your fertility nurse will contact you with some easy instructions on how to prepare.
The embryo transfer is a very simple process—similar to a pap smear. The procedure itself only takes about five minutes. A scientist prepares your embryo by placing it in a small tube called a catheter. It’s critical this is done by an expert in order to disturb the embryo as little as possible.
Your fertility specialist places the catheter through your cervix and into your uterus.
And that’s it!
You’ll be awake, there’s no anaesthetic, and you can get up straight away. Feel free to continue with your day; the embryo is secure within your uterus and won’t fall out if you stand up or go to the toilet.
Your step-by-step guide to an IVF cycle
Step 8: The pregnancy blood test
Approximately two weeks after your embryo transfer, you’ll have a blood test to measure your levels of the hormone hCG (human chorionic gonadotropin). hCG in your bloodstream usually indicates a positive pregnancy test.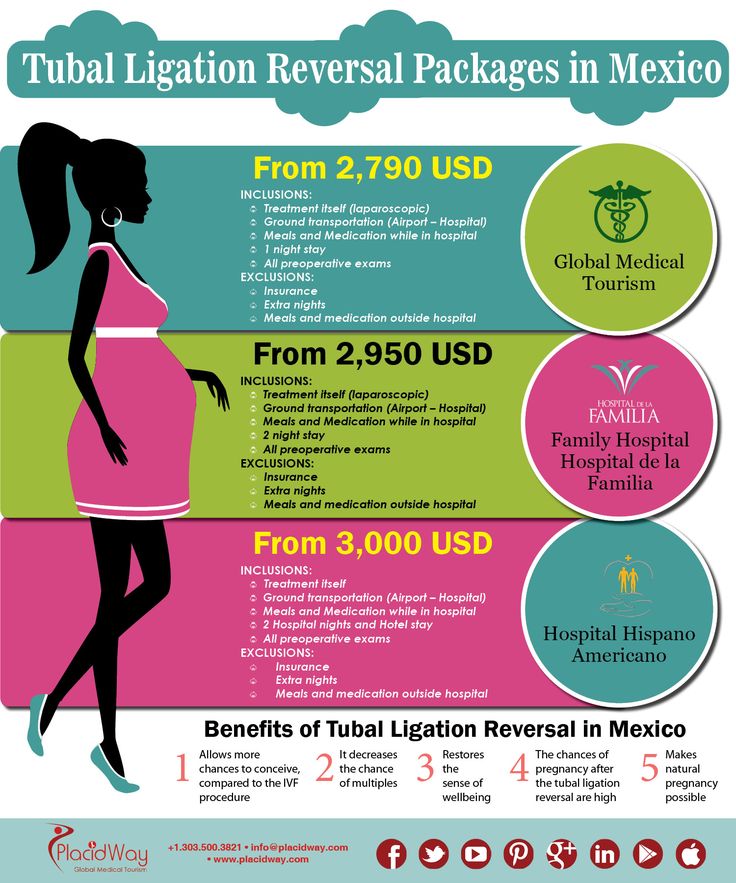 Your nurse will let you know exactly when to have your blood test, as it may vary for some patients.
Your nurse will let you know exactly when to have your blood test, as it may vary for some patients.
We understand that the lead-up to this final blood test can be an anxious time. That’s why it’s a good idea to distract yourself if possible. You may even like to plan a fun event around the time you’re expecting your result. A weekend away or a special lunch can ease stress and give you something to look forward to.
short, standard and long schemes of artificial insemination in the Clinic of the Central Clinical Hospital of the Russian Academy of Sciences
A couple who are planning artificial insemination are faced with the term "IVF protocol". In fact, this is a step-by-step program of the order of events and medication, selected depending on the characteristics of each woman. It takes into account her age, health and the reasons for which in vitro fertilization will be carried out.
Natural and stimulating protocols are applied. Second, can be long and short. nine0003
nine0003
Standard. IVF long protocol
The scheme of the long IVF protocol assumes the longest path of all used. The protocol is drawn up in detail and is designed for at least five weeks. Its peculiarity and main advantage is the ability to control the hormonal background, which allows you to get the largest number of eggs. Their number can reach up to 20.
Successful IVF requires not only a large number of eggs, but also their good quality. The maturation process is interconnected with the chosen ovulation stimulation scheme. For the successful completion of this task, it is the long protocol that is the most effective. nine0003
For the appointment of patients with a long protocol, there are certain indications:
- Pathology of the uterus;
- Obesity;
- Endometriosis;
- High secretion of androgens.
Another reason is an unsuccessful IVF attempt using a short protocol.
The steps by which the long protocol is implemented are:
- a week before menstruation, the ovaries are put into external control mode by medication - their natural functions are blocked; nine0016
- further, the growth of follicles is stimulated to the desired size, the maturation process takes place against the background of taking trigger drugs;
- follicle puncture, embryo transfer, condition control until the desired result is obtained.
The method has a serious drawback: the risk of developing ovarian hyperstimulation syndrome, leading to undesirable consequences.
IVF short protocol
Its beginning is a stimulating phase on the 3rd day from the onset of menstruation. The difference of the technique is the absence of the regulation phase. As a result, uneven maturation of a smaller number of follicles. Their quality may also vary. nine0003
How a short IVF protocol is built by day:
- Ovarian block resolves during the entire process, but to a milder degree;
- Two days after the start of the protocol, the patient starts taking gonadotropins for a period of two weeks;
- HCG preparations are prescribed to prepare the follicles for ovulation;
- In the period from 14 to 20 days from the beginning of menstruation, a puncture is performed.
Starting from this moment, the short and long protocols are the same. nine0003
This scheme can be used if:
- The patient has no problems with the appendages;
- Her age is not young;
- When using a long protocol without results.

The advantage of the technique is a short period of use - about a month, which ensures relatively easy portability.
One variation of the short protocol is the ultrashort version, where GnRH agonists are replaced by antagonists. The purpose of this decision is to reduce the likelihood of getting premature ovulation, since the puncture is performed after two weeks. nine0003
Interestingly, the feelings of a woman with a successful embryo transfer do not differ from those of a natural pregnancy.
You can learn more about the protocols and get any other information about in vitro fertilization at the Central Clinical Hospital of the Russian Academy of Sciences in Moscow by making an appointment with a reproductive medicine doctor (499) 400-47-33.
IVF procedure: all stages - from examination to confirmation of pregnancy
Home/About clinic/Useful/IVF stages
August 21, 2017
The first stage of IVF is a visit to a reproductive specialist - a doctor who specializes in the treatment of infertility.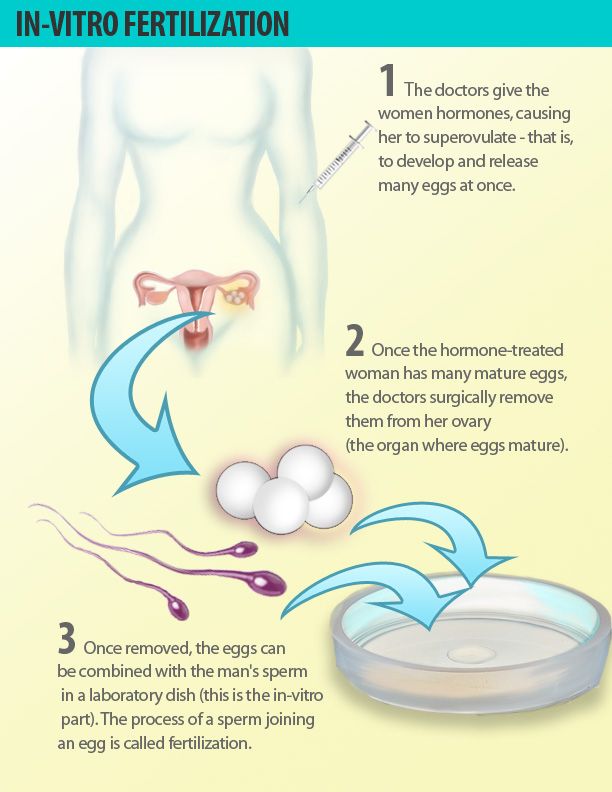
The process of conception involves a man and a woman. If, as a result of sexual intimacy, pregnancy does not occur, then the reason for this may be both from the side of the man and from the side of the woman. Therefore, it is advisable to come to the reception together.
If pregnancy does not occur within 6-12 months of sexual life without contraception, then we can talk about infertility. Timely contacting a specialized clinic will solve the problem as efficiently as possible. nine0003
At the first appointment, the doctor will talk to the couple, take an anamnesis, examine the woman and assess her ovarian reserve using ultrasound. Then he will schedule an examination.
Basic examinations for women:
- Ultrasound of the pelvic organs
- Evaluation of the patency of the fallopian tubes
- Folliculometry
- Ultrasound of the thyroid gland (according to indications)
- Ultrasound of the mammary glands (according to indications)
- laboratory tests.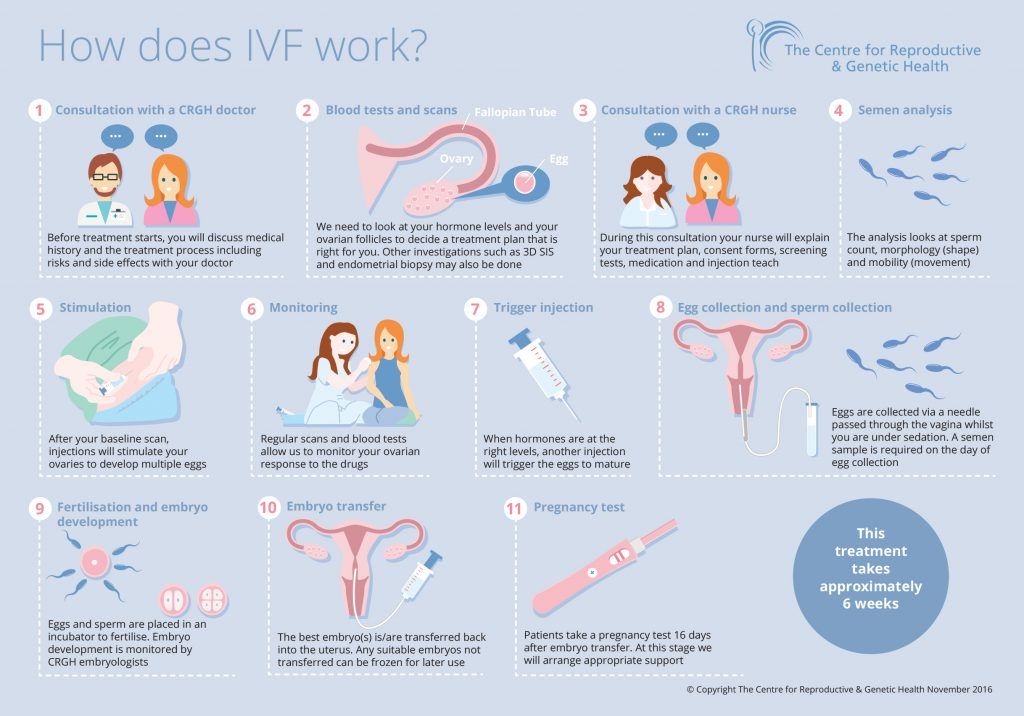
A man will definitely need to pass a spermogram and undergo an appointment with a urologist-andrologist. The results of complex diagnostics determine the indications for a particular treatment method. If there are indications for IVF, then the stage of preparation for the protocol begins. nine0003
The IVF protocol is a scheme that takes into account the sequence, duration, frequency and types of drugs administered, as well as their dosages. There are 2 main types of IVF protocols: short and long. There is also such a type of protocol as segmented with cryopreservation. To date, they are the most effective.
Quite often, before the IVF program, a woman is shown weight correction. Optimal body weight increases the effectiveness of the procedure. nine0003
So let's get into the protocol.
FIRST STAGE: superovulation stimulation
For this, a woman is prescribed special hormonal drugs. They cause the simultaneous maturation of several follicles in the ovaries, which increases the chances of pregnancy.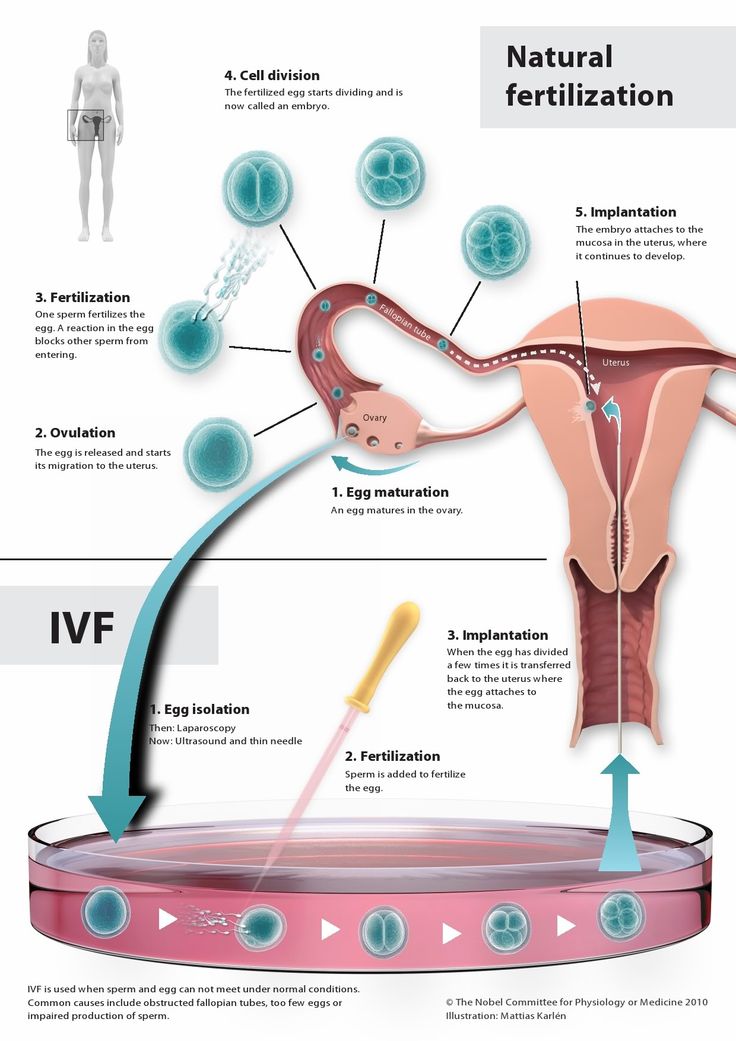 One ovum matures in each follicle. Egg retrieval is carried out by puncture of the follicle.
One ovum matures in each follicle. Egg retrieval is carried out by puncture of the follicle.
Compliance with the exact schedule of injections of drugs is extremely important to obtain the result - a sufficient number of quality eggs. Therefore, be precise and obligatory, do not miss the scheduled dates and times of visits. nine0003
The first ultrasound monitoring after the start of the IVF program is usually carried out on the 5th or 6th day of superovulation stimulation. Its task is to assess the response of the ovaries (follicle growth dynamics) and the thickness of the endometrium (uterine lining). Before the active growth of follicles begins (until they reach a size of 10 mm or more), ultrasound is performed once every 4-5 days, then the ovaries are examined more often - once every 2-3 days.
SECOND STAGE: follicle puncture
After the ovarian stimulation is completed, it is necessary to obtain eggs from the follicles.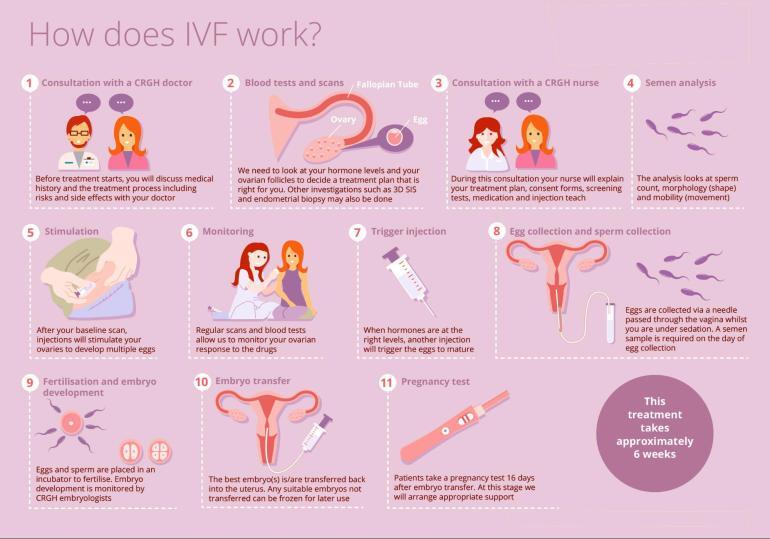 For this, a puncture is performed, 34-35 hours after the introduction of the trigger (hCG). The procedure takes place under ultrasound control in the operating room and under intravenous anesthesia, and lasts an average of 10-15 minutes.
For this, a puncture is performed, 34-35 hours after the introduction of the trigger (hCG). The procedure takes place under ultrasound control in the operating room and under intravenous anesthesia, and lasts an average of 10-15 minutes.
After graduation, you will remain in the clinic under observation for at least 2 hours. Sperm collection is carried out on the same day and time as the puncture. In cases where it is impossible to use the cells of the parents, donor material comes to the rescue (IVF with a donor egg)
THIRD STAGE: egg fertilization and embryo culture
In the laboratory, after 3-4 hours, the embryologist fertilizes the received eggs with processed sperm. The day of the beginning of the cultivation of embryos is considered the next day after the puncture of the follicles.
FERTILIZATION
It takes place in a Petri dish. In classical IVF, an egg is placed there and then specially processed sperm is added.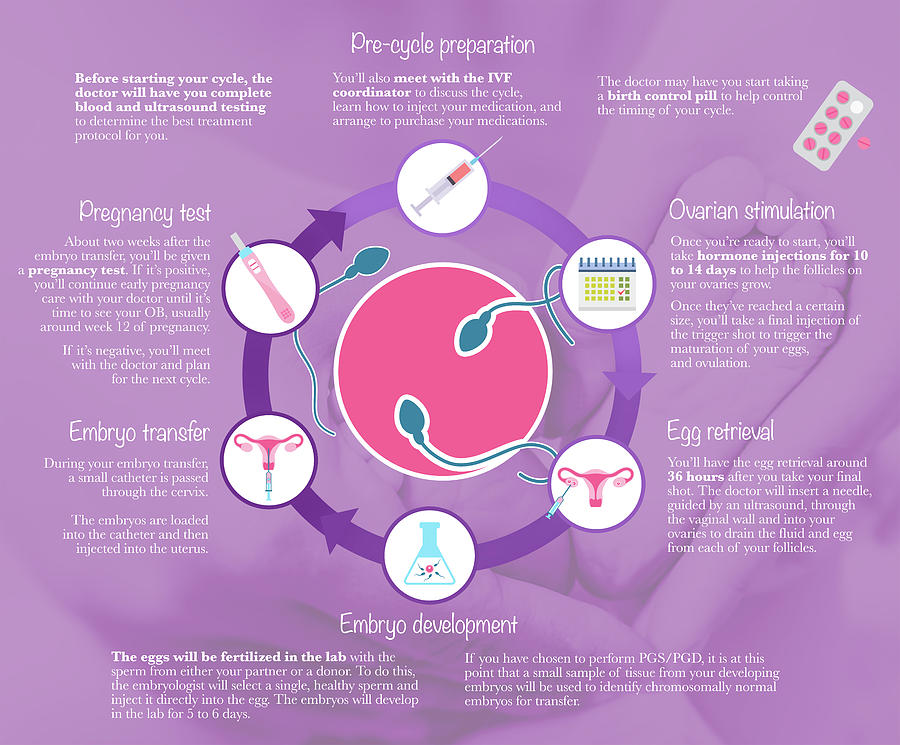 nine0089
nine0089
"Genome" mainly uses the ICSI method, in which the sperm is injected into the egg, which increases the likelihood of fertilization. PICSI is also used - an improved ICSI technique with additional selection of spermatozoa based on biochemical criteria.
Embryos obtained as a result of fertilization are cultivated up to 5-6 days, the blastocyst stage. They are then either transferred to the uterus or cryopreserved (frozen). To increase the chance of successful implantation, the shell of the embryo is sometimes thinned, a procedure called assisted hatching. nine0003
STAGE FOUR: Embryo Transfer
Technically, the embryo transfer procedure is quite simple and is carried out under ultrasound control, which allows you to track the course of the catheter with embryos. A set of embryos for transfer is carried out in the laboratory. Then the doctor exposes the cervix in the mirrors and inserts a catheter with embryos through the cervical canal into the uterine cavity.