Newborn red spots
Common childhood rashes | Pregnancy Birth and Baby
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
Key facts
- There are many different types of childhood rashes. Many are not serious.
- If your child has a rash and fever, they should see their doctor.
- If your child has a meningococcal rash, go immediately to the emergency department.
Meningococcal rash
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
You can read more about serious childhood rashes here.
Rashes with no fever or itching
Milia (blocked oil glands)
Up to 1 in every 2 newborn babies develop small white spots called milia on their face, especially on the nose. These are just blocked pores, and they’re not itchy or contagious. They usually clear up without treatment within a few weeks.
Erythema toxicum
Many newborns develop a blotchy red skin reaction called erythema toxicum, which can appear between 2 days and 2 weeks after birth. Flat, red patches or small bumps often first appear on the face and spread to the body and limbs. The rash is harmless, not contagious, and will clear after a few days or a week.
Baby acne
Some babies get pimples on their cheeks and nose in the first three months of life. These pimples normally disappear without any treatment, usually within a few months.
Nappy rash
Nappy rash is inflammation of the skin in the nappy area. It can look red, sore and inflamed. Nappy rash is usually caused by urine (wee) or faeces (poo) irritating the skin.
To avoid nappy rash, keep the nappy area clean and dry with frequent nappy changes and nappy-free time. You can help protect the skin by putting on a barrier cream such as zinc or soft white paraffin at each nappy change.
Persistent nappy rash can be treated with a medicated cream. Don’t use talcum powder or antiseptics to treat nappy rash. If your baby develops a fungal infection, you’ll need to use an antifungal ointment. Ask your doctor or pharmacist for advice.
Erythema multiforme (minor)
Erythema multiforme is a rash triggered by an infection (most commonly herpes simplex virus), medicine or an illness. Your baby might feel unwell or have a mild fever before the rash appears. Red spots develop on the hands, feet, arms and legs and spread symmetrically across both sides of the body. The spots often become raised or blistered and then develop into classic target-like lesions.
Erythema multiforme is not contagious, and usually resolves without treatment in 3 to 6 weeks.
Keratosis pilaris (‘chicken skin’)
Keratosis pilaris is a harmless condition where the skin becomes rough and bumpy, as if permanently covered in goose pimples. These bumps most commonly occur on the upper arms and thighs. You can try several things to help the rash to clear up, including moisturising regularly.
You can try several things to help the rash to clear up, including moisturising regularly.
Rashes that might be itchy
Eczema (Atopic dermatitis)
Eczema is a very common skin condition affecting 1 in 3 Australians. It causes the skin to become itchy, red, dry and cracked, often in the creases at the knees and elbows.
Eczema commonly starts before a baby is 12 months old. Eczema follows a relapsing-remitting course. This means that there are flare-ups of the rash, followed by periods where there is no rash or a minimal rash.
Eczema management includes preventative treatment such as avoiding skin irritants, moisturising regularly and using bath oil. Treatment of flare-ups includes using steroid and anti-inflammatory creams.
Ringworm (tinea)
Ringworm is a common, contagious skin infection that causes a ring-like red rash with a clear centre. It commonly occurs on the scalp, feet and groin, but it can appear almost anywhere on the body.
Ringworm is caused by a fungus, not a worm, and is usually treated with over-the-counter antifungal creams. You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
Prickly heat (heat rash)
Heat rash might appear if your baby gets hot in a humid environment. The rash shows as tiny red bumps or blisters on the skin, which can be very itchy. Cooling your baby down and avoiding humidity is the best way to prevent heat rash, which usually clears within 2 to 3 days without treatment.
Impetigo (school sores)
Impetigo is a highly contagious bacterial infection of the skin. It causes red sores and blisters that form a yellow crust. It is very common in children aged 2 to 6, and it is not usually serious in this age group, but it can be dangerous for newborn babies.
If your child has impetigo, you should see your doctor, who might prescribe an antibiotic cream, ointment or tablet. This should clear the infection within 7 to 10 days. Keep your child home from childcare or school and away from young babies until the sores have dried up, usually a few days after treatment starts.
Hives (urticaria)
Hives is a raised, red, itchy rash. It is common on the chest, stomach and back, as well as the throat and limbs, but it can appear on any part of the body. Hives usually disappears within a few days without any treatment. Antihistamines can be given to relieve itching. If the rash doesn't go away, you should see your doctor.
Hives isn’t usually serious, but it can be a sign of a more serious allergic reaction (anaphylaxis). If your child develops hives after eating, or together with other symptoms such as vomiting, dizziness or trouble breathing, you should seek urgent medical attention.
If your child has symptoms of a serious allergic reaction (anaphylaxis), call triple zero (000) immediately and ask for an ambulance.
Pityriasis rosea
Pityriasis rosea is a mild skin rash that sometimes appears after a sore throat, cold or fever. It begins with a single pink or tan-coloured patch on the chest or back. Red, oval-shaped patches, which may be itchy, then appear on the chest or back and limbs over the next weeks.
The exact cause of pityriasis rosea is unclear, and it is not thought to be contagious. The rash usually clears up within a couple of months without treatment.
If you are pregnant, pityriasis rosea can in rare cases lead to complications. See your doctor if you are pregnant and have contact with a child who has pityriasis rosea.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that is spread by skin-to-skin contact or by sharing swimming pool water, bath water or towels.
Molluscum contagiosum spots look like pimples and grow into round pearly white lumps, usually 2 to 5 millimetres in size. They can be itchy. They usually heal without treatment within 6 months, but sometimes longer.
Rashes with fever
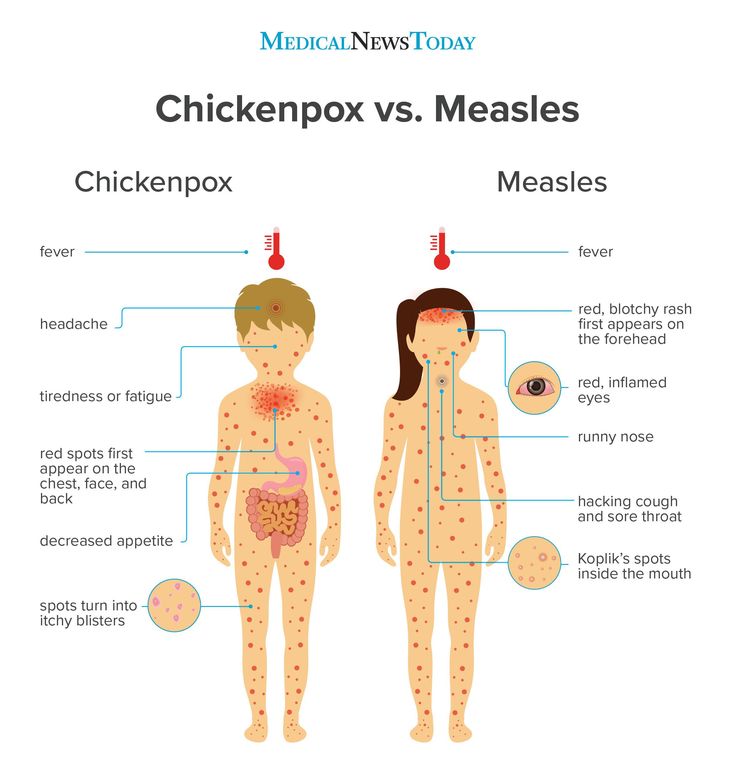
Slapped cheek disease (fifth disease)
Slapped cheek disease is a viral infection that mainly affects pre-school and school-age children. It typically causes a bright red rash on both cheeks that spreads as a ‘lacy’ rash on the body and limbs. Occasionally, it causes a fever.
Occasionally, it causes a fever.
Slapped cheek disease is usually mild and clears up in a few days without treatment. The child is contagious before the rash appears, but not once it has appeared.
If you are pregnant and catch the virus, it may cause a type of anaemia in your unborn baby. It can also cause miscarriage. If you suspect you or your child has slapped cheek disease, you should avoid contact with people who might be pregnant.
Hand, foot and mouth disease
Hand, foot and mouth disease is a mild but highly contagious viral illness. It causes a rash on the palms of the hands and soles of the feet and blisters in the mouth. It is not the same as the foot-and-mouth disease that affects farm animals.
The disease is common in childcare and kindergartens. Your child might feel unwell and have a fever and blisters on the hands and feet and in the mouth and in the nappy area. The illness usually lasts about 7 to 10 days. Children with hand, foot and mouth disease should stay away from childcare or school until all the blisters have dried up.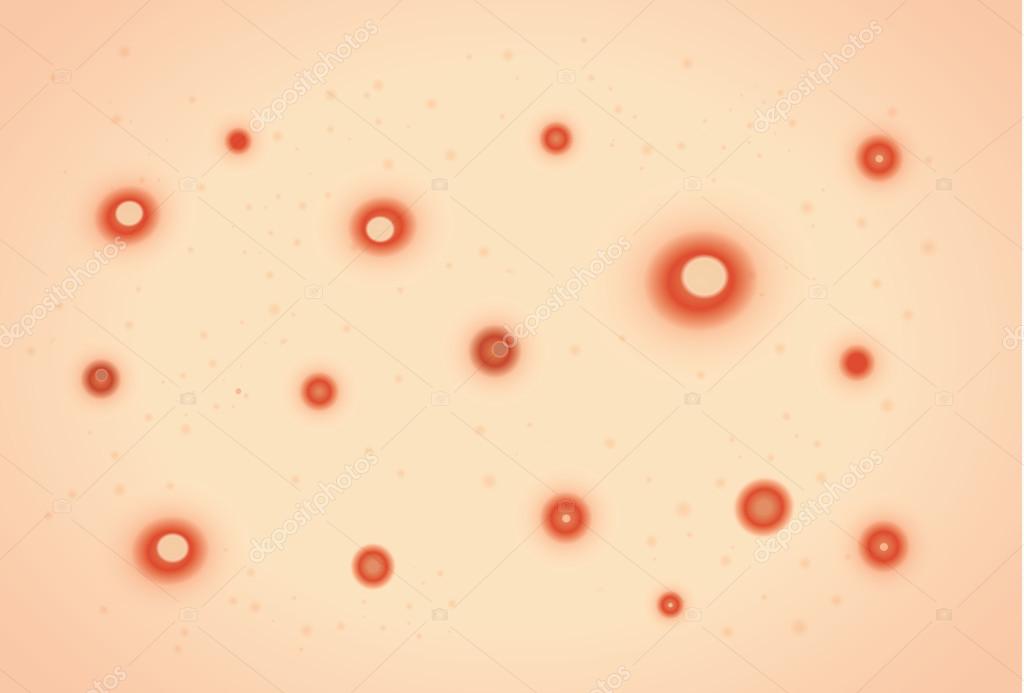
Hand, foot and mouth disease usually resolves on its own without complications. In rare cases, it can be more serious, especially if you have a weakened immune system or are pregnant. Complications can include infections of the brain and heart muscle and miscarriage.
Roseola infantum
Roseola infantum is a contagious viral infection that can cause cold-like symptoms and a high fever. The high fever may last for a few days. Roseola infantum can also cause some children to have a febrile convulsion (seizure).
Children with roseola infantum develop a rash after the fever has resolved. The rash looks like raised pink spots that start on the chest, stomach and back and spread to the limbs. The child is contagious before the rash appears, but not after. The rash usually lasts 3 to 5 days.
Febrile convulsions can look scary but are generally not harmful.
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
When to seek help
Many babies develop a skin rash in their first days or weeks of life as their sensitive skin adapts to a new environment. Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Whatever their age, you should take your child to the doctor if they have a rash and persistent high temperature, cold or cough symptoms or swollen neck glands.
Treatment of common childhood rashes
If you think your child might be contagious, they should stay at home. Keep them away from school, childcare and other children. You should also keep them away from people who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
You can use paracetamol or ibuprofen (in babies aged over 3 months) to reduce fever — read the packet instructions carefully to ensure your child receives the right amount for their age and weight.
Your pharmacist can advise you on treating the symptoms of common rashes. For example, you can use over-the-counter creams to prevent itchiness.
If you are concerned about your child’s rash, call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse, or call Healthdirect on 1800 022 022 to talk to a registered nurse. Alternatively, contact your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Newborn Rashes and Birthmarks
Is this your child's symptom?
- Normal skin rashes and birthmark questions about newborns
Newborn Rashes - Topics Covered
If your baby is healthy, skip the "What to Do" section. Go directly to the topic number that relates to your question for advice.
- Acne. Small red bumps on the face (onset 2-4 weeks).
- Drooling or Spit-Up Rash. Rash around the mouth and on the chin (onset anytime).

- Erythema Toxicum. Red blotches with small white "pimple" in the center (onset 2-3 days).
- Skin Injury from Birth Process. From forceps, scalp electrode or birth canal (present at birth).
- Milia. Tiny white bumps on the nose and cheeks (present at birth).
- Mongolian Spots. Bluish-green birthmark, often on buttock (present at birth).
- Stork Bites (Pink Birthmarks). On back of neck or bridge of nose (present at birth).
- Strawberry Hemangiomas. Raised red birthmarks (onset 2-4 weeks).
- Port-wine Stains. Dark red or purple flat birthmarks (present at birth).
Newborn Face Rashes: Most Common Ones
- Erythema Toxicum 50% (onset day 2 or 3)
- Milia 40% (present at birth)
- Baby Acne 30% (onset week 2 to 4)
- Drooling or Spit-up Rash (common and onset any time)
- Heat Rash (common and onset any time)
Heat Rash
- Many newborn rashes that have no clear cause are heat rashes.
- Heat rashes are a pink blotchy area with tiny bumps.

- They mainly occur on the face, neck and chest.
- During hot weather, most temporary newborn rashes are heat rashes.
- Cause: blocked off sweat glands. The openings are so tiny in newborns, that any irritation can block them. Examples are getting any ointment on the skin, friction from clothing or being overheated. Being held against the mother's skin while nursing causes many face rashes.
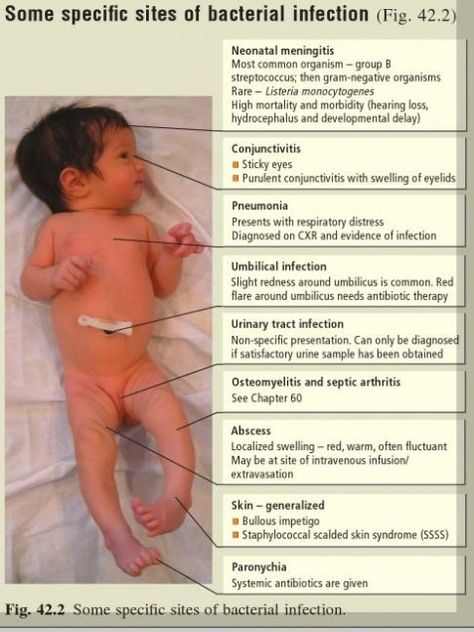
Herpes Simplex: Serious Newborn Rash
- Appearance. Several water blisters or pimples grouped in a cluster. They look like the cold sores (fever blisters) that adults get on their lip. After several days, they crust over.
- Location. Just one part of the body, usually the scalp or face.
- Redness. The base can be pink. The pinkness does not extend beyond the cluster of vesicles.
- Onset. Within the first 2 weeks of life.
- Importance. Early treatment with anti-viral drugs can prevent serious problems.
 If you think your newborn's rash looks like herpes, call your child's doctor now.
If you think your newborn's rash looks like herpes, call your child's doctor now. - Imitator. Although herpes can be confused with erythema toxicum, they look very different.
When to Call for Newborn Rashes and Birthmarks
Call 911 Now
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way
- Fever in baby less than 12 weeks old. Caution: do NOT give your baby any fever medicine before being seen.
- Purple or blood-colored spots or dots not present at birth
- Tiny blisters (little bumps that contain clear fluid)
- Pimples (little bumps that contain pus). Exception: looks like erythema toxicum which occurs in half of newborns.
- Skin looks infected (such as spreading redness, sores or pus)
- Rash is painful to touch
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Mild newborn rash, but cause is not clear
- You have other questions or concerns
Self Care at Home
- Normal newborn rashes or birthmarks
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Newborn Rashes and Birthmarks
- Acne:
- More than 30 percent of newborns develop baby acne of the face. Acne consists of small red bumps.
- This baby acne begins at 2 to 4 weeks of age. It lasts until 4 to 6 months of age.
- The cause appears to be the transfer of maternal hormones just prior to birth.
- Since it goes away on its own, no treatment is needed.
 Baby oil or ointments make it worse.
Baby oil or ointments make it worse.
- Drooling or Spit-up Rash:
- Many babies have a rash on the chin or cheeks that comes and goes. This is often due to contact with food. It's more common after starting baby foods. In newborns, it can also be from stomach acid that has been spit up. Prolonged contact with spit-up during sleep can cause the rash to get worse.
- Other temporary rashes on the face are heat rashes. These can occur in areas held against the mother's skin during nursing. Heat rashes are more common in the summertime.
- Rinse the face with water after all feedings or spitting up. During hot weather, change the baby's position more often. Also, put a cool wet washcloth on the rash. Do this for 10 minutes.
- Erythema Toxicum:
- More than 50 percent of babies get a rash called erythema toxicum. It starts on the second or third day of life.
- It's a harmless baby rash that doesn't need to be seen.

- The rash is made up red blotches. They are ½ inch to 1 inch (1 to 2.5 cm). The blotches have a small white or yellow "pimple" in the center.
- They look like insect bites, but are not. Red blotches are the main feature.
- They can be numerous, keep occurring, and look terrible. They can occur anywhere on the body surface, except the palms and soles.
- Their cause is unknown, but they are not an infection.
- They go away by 1-2 weeks of age.
- No treatment is needed. Ointments or baby oil make it worse.
- Skin Injury from Forceps, Scalp Electrode or Birth Canal:
- The pressure of a forceps on the skin can leave marks. You may see bruises or scrapes anywhere on the head or face.
- During birth, skin overlying bony prominences can become damaged. You might see this on the sides of the skull bone. This is from pressure from the birth canal. Even without a forceps delivery, you may see bruises or scrapes.
- Scalp electrodes can also cause scalp scrapes and scabs.

- The bruises and scrapes will be noted at birth. They will be more noticeable by day 2. They heal over or go away by 1 - 2 weeks of age.
- A fat tissue injury won't appear until day 5 to 10. Look for a firm coin-shaped lump. It will be under the skin and sometimes with a scab. This lump may take 3 or 4 weeks to go away.
- For any breaks in the skin, apply an antibiotic ointment (such as Polysporin). No prescription is needed. Use 3 times per day until healed.
- Call Your Doctor If:
- It becomes tender to the touch
- Becomes soft in the center
- Starts to looks infected
- Milia:
- Milia are tiny white bumps that occur on the face. The nose and cheeks are most often involved. Milia can also be seen on the forehead and chin.
- Milia occur in 40 percent of newborn babies. Present at birth.
- Milia are many in number. They occur equally on both sides of the face.
- Although they look like pimples, they are much smaller (pinhead size).
 They are not infected.
They are not infected. - They do not look like water blisters.
- They are blocked-off skin pores. They will open up.
- Milia will go away by 1 to 2 months of age.
- No treatment is needed. Ointments or creams can make them worse.
- Mongolian Spots:
- A Mongolian spot is a normal bluish-green or bluish-gray flat birthmark. They occur in over 90 percent of Native American, Asian, Hispanic, and African American babies. They are also seen in 10 percent of Caucasians, especially those of Mediterranean descent.
- They are present at birth.
- They occur most commonly over the back and buttocks. However, they can be present on any part of the body.
- They vary greatly in size and shape.
- They do not indicate illness or any disease.
- Most fade away by 2 or 3 years of age. A trace may last into adult life.
- Stork Bites (Pink Birthmarks):
- Flat pink birthmarks that occur over the bridge of the nose or the eyelids.
 You can also find them on the back of the neck ("stork bites"). The ones in front are often referred to as "an angel's kiss".
You can also find them on the back of the neck ("stork bites"). The ones in front are often referred to as "an angel's kiss". - They occur in more than 50 percent of newborns. They are present at birth.
- All the birthmarks on the bridge of the nose and eyelids clear completely. Those on the eyelids clear by 1 year of age. Those on the bridge of the nose may last for a few more years. Those on the forehead from the nose up to the hairline usually last into adulthood. Laser treatment during infancy should be considered. Most birthmarks on the nape of the neck also clear. But, 25 percent can last into adult life.
- Flat pink birthmarks that occur over the bridge of the nose or the eyelids.
- Strawberry Hemangiomas:
- Strawberry hemangiomas are red birthmarks that are raised or increasing in size.
- Onset usually between 2-4 weeks of age. Most often, start after 3 weeks of age. Sometimes (although rare), they don't appear until the second month of life.
- They become larger for 1 year. Then, they fade away over 6 to 8 years without any treatment.

- They run a small risk of bleeding with trauma. Any bleeding should stop with 10 minutes of direct pressure.
- Discuss with your child's doctor on the next regular visit. Call sooner if you are concerned.
- Port-Wine Stain Birthmarks:
- Present at birth in 1 out of 200 newborns
- Deeper in color (dark red or purple) than stork bites (salmon patches)
- Flat, smooth surface
- Natural course: Do not fade or disappear like stork bites. May become darker.
- Grow with the child, but cover the same area
- Treatment: May refer to dermatologist for laser treatments early in infancy
- Call Your Doctor If:
- Your baby starts to look or act abnormal in any way
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 12/17/2022
Last Revised: 01/13/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
Stork sting. What are newborn mothers afraid of? Society news
Any seemingly insignificant change in the baby's condition can frighten the newly-made mom and dad. Although sometimes nothing really bad happens. In the first month of life, neonatologists observe babies. It is on them that a flurry of parental fears falls.
“There is such a thing as a transient state of newborns. This is an intermediate period between the time when the child was in the mother's womb and the time when he begins to settle down outside, says Lina Komisar . - When a woman who has given birth asks: “How is the baby?”, We answer: “He is in the period of adaptation.” A transient state is not a diagnosis, not a disease! This condition is also called borderline, since with defects in care or a breakdown in adaptation, it can turn into a pathological one.
Therefore, neonatologists daily, and sometimes twice a day, examine children in the neonatal department.”
Body weight
“Sometimes mothers tell doctors: “My baby has lost weight. Probably because he didn't eat." But this happens not only for this reason. In the first three days, the child receives only a small amount of colostrum and, due to a lack of total fluid volume, loses weight. nine0003
In addition, at this time, the umbilical residue dries up and the original feces are excreted, due to which the baby also loses grams.
Lina Komisar / Photo: Natalia Malyihina
Read also 17 Aug 2022 11:08
Small does not mean sick. Does the weight of a newborn affect its further development 28 May 2022 09:eleven
Doctors in Belgorod gave birth to two residents of the Kharkiv region 29 Mar 2022 10:52
2 boys and 1 girl were born on New Year's Eve in Belgorod 01 Jan 2022 10:49 nine0025 Since the beginning of the year, the 2021st baby was born in the Belgorod region 05 Mar 2021 17:04
The maximum loss occurs before the third or fourth day.
If a child was born weighing 3 kg, then he can lose up to 300 g. Such a loss is not a contraindication for discharge from the hospital. Everything will be restored.
From the fourth day, a gradual increase begins. The mother receives more milk, the child becomes more active, sleeps less and adds 10–50 g daily.” nine0003
"It was scary. I prayed." Moms - about the first days of life of children born prematurely
Jaundice
“I can say right away that if a child develops jaundice, this is not a consequence of hepatitis B vaccination, as some parents believe.
There is a special kind of jaundice that occurs only in newborns.
Pathological jaundice occurs with Rh conflicts, liver dysfunction, infections and other abnormalities. It is very rare. nine0003
Physiological jaundice begins due to the difference between the hemoglobin of the fetus and the child who has already been born.
In a newborn, fetal hemoglobin breaks down, transforming, among other things, into bilirubin. But due to the fact that the baby's liver is immature (this organ is formed before the age of five), it does not have time to utilize this bilirubin. Here the child turns yellow. If certain indicators are not exceeded, this condition does not require special treatment. Bilirubin will be excreted naturally. nine0003
One child may turn yellow on the second day, the other on the fifth. Jaundice disappears from the beginning of the second to the end of the third week, sometimes it can last up to a month.
Hyperthermia
“It happens that the baby turns red, screams, and the mother cannot calm him down. This is due to the immature nervous system and thermoregulation center. Roughly speaking, babies accept the temperature of the environment: they dressed warmly - overheated, opened - cooled down.
If the child's temperature is above 37.5°, you need to untie him and bathe him, remove the diaper and just keep him in a thin diaper.
And everything will pass. Antipyretics are prescribed only in very rare cases. nine0003
Photo: pixabay.com
Sexual crisis
“On the third or fourth day, the external genitalia of girls increase, the scrotum of boys swells. In children, the mammary glands may increase, there will be discharge from them. Girls can also have false periods, which is especially frightening for mothers. This is not scary, because every child receives a lot of hormones during pregnancy and childbirth. Everything will go by itself."
Physiological dysbacteriosis
“Mother calls me to the ward with the words: “My child has diarrhea, what should I do? This is probably because of the antibiotics that they inject me!” No, it's not because of the antibiotics. This is a transition chair.
The baby is born with sterile intestines. During the first day of life, after being applied to the mother's breast, it is populated by the maternal microflora.
The sterile intestine reacts to lacto- and bifidobacteria. It's not a disease."
Skin problems
“Most of the time mothers ask why the baby is so red. So, red is the physiological color of the skin in the first three days. The protective lubricant was removed from the baby, and his skin is thin, and the capillaries are close. In fact, it is very good that the baby is red, and not some other color. nine0003
It happens that a child has white pimples on his nose, chin and cheeks. Some mothers are very worried when they are discharged: “God, I have a photo session, what should I do?! Why is he so ugly!” Don't worry, you have a beautiful baby! He just has thin skin and no subcutaneous fat layer. In the area of the face, he has clogged immature sebaceous glands. Nothing needs to be done about it.
Some babies have red spots on the forehead, eyelids and back of the head. People say that redness in front is the kiss of an angel, and behind it is the bite of a stork, that is, the bird took the baby by the neck and carried it to the parents. They also say that these are birthmarks, but this is not so. These are pathologically dilated capillaries. Up to a year they will pass, but they will appear in the heat, with screaming and crying. All of these are not diagnoses either.” nine0003
They also say that these are birthmarks, but this is not so. These are pathologically dilated capillaries. Up to a year they will pass, but they will appear in the heat, with screaming and crying. All of these are not diagnoses either.” nine0003
Photo: pixabay.com
Toxic erythema
“If the baby is covered with pimples, most likely it is toxic erythema - a transitional skin condition. It can be caused by toxicosis in the mother, disorders of the endocrine system, the mother taking certain drugs, heredity.
The rash resolves on its own. It has a migratory character: it disappeared on the arm, appeared on the leg. You just need to keep the baby dry and not overheat it.” nine0003
Urinary crisis
“It happens that on the first day the baby does not pee. This is fine. He can urinate at the end of the first day or on the second day. In the first three days, he will go to the toilet a little, but then the diapers will be wet four to six times a day.
And if you see something red in a diaper, don't be afraid that it's blood. This is a consequence of uric acid diathesis. The kidneys began to work actively, so salts of uric acid are released. Boys before urination may cry for the first three days, as the grains have a painful effect on the urethra. nine0003
Photo: pixabay.com
VRF News
What are the types of infantile (infantile) hemangiomas?
Erstellt am 2017/10/19, last modified: 2017/10/19 https://kinderkrebsinfo.de/doi/e195094
Contents
- Local infantile hemangiomas
- Segmental infantile hemangiomas
- Special forms
Typically, infantile hemangiomas (that is, hemangiomas in newborns and infants, and many doctors use the term infantile hemangiomas) appear in the first days or weeks after the birth of a child. First, the first symptoms appear (specialists talk about the precursor forms of hemangiomas) - dilated subcutaneous vessels in a limited area of \u200b\u200bthe skin (telangiectasia in the language of specialists), or, for example, very pale spots, or spots of bright red or cyanotic color, or changes in the skin, similar to red birthmarks (doctors talk about vascular nevus). The classic infantile hemangioma at the birth of a child does not yet look like a tumor, it becomes one after some time. nine0133
The classic infantile hemangioma at the birth of a child does not yet look like a tumor, it becomes one after some time. nine0133
Good to know: infantile (infantile) hemangioma goes through three stages:
- Active growth phase: the first stage lasts from 6 to 9 months
- Growth arrest phase: tumor size no longer changes
- Regression phase (gradual reverse development of hemangioma, that is, the tumor begins to “resolve”, the recovery process is underway): as a rule, recovery ends by the 9th year of the child's life.
Local infantile hemangiomas
90% of all infantile hemangiomas are local. This means that they have clear boundaries and grow from one central point.
Local infantile hemangiomas are divided into:
- superficial skin infantile hemangiomas. They grow on the surface of the skin (flat) or may protrude above the skin (convex, i.e. do not grow deep)
- deep subcutaneous hemangiomas.
 They grow deep under the skin
They grow deep under the skin - combined hemangiomas. That is, a mixed type, when an infantile hemangioma simultaneously grows as a superficial skin and deep subcutaneous
Usually, at birth, an infantile hemangioma is not yet visible in a child. But then, during repeated examinations in the first weeks after birth, a small spot of red color becomes noticeable. Some infantile hemangiomas do not change for weeks or months. Others begin to grow rapidly and grow to enormous size. Most infantile hemangiomas (60%) appear in the head and neck.
Segmental infantile hemangiomas
Segmental infantile hemangiomas (that is, a large hemangioma will grow in a certain area of the body) are less common than local ones. They can appear both in the head and neck, and in the region of the lumbar spine and in the coccyx. Usually the size of segmental infantile hemangiomas is larger than that of local forms. In addition, they often appear when abnormal development of blood vessels or internal organs begins in the body (in this case, doctors talk about malformations or developmental anomalies). Characteristic of segmental hemangiomas is that they are very large and cover a certain department (segment) of the body. They are almost invisible at birth. But they can grow very quickly and then the baby often has various health problems. nine0133
Characteristic of segmental hemangiomas is that they are very large and cover a certain department (segment) of the body. They are almost invisible at birth. But they can grow very quickly and then the baby often has various health problems. nine0133
For example, segmental infantile hemangiomas in the face or shoulder region are associated with the so-called PHACES syndrome (P.H.A.C.E.S. syndrome is a set of several congenital malformations, each letter of the abbreviation denotes a specific malformation). First, anomalies in the development of the chest, aorta, as well as heart defects and cysts in the brain (in the language of specialists, the so-called Dandy-Walker variant) are found in the baby, and then a segmental hemangioma appears. Another complication is a tendency to form ulcers and a tendency to frequent infections. nine0133
Hemangiomas that grow in the perineum are part of the PELVIS (in the pelvis) and SAKRAL (in the sacrum) syndromes. They are accompanied by skin growths, as well as anomalies in the development of the bladder, spinal cord and spinal cord membranes, and abnormal development of the anus.
In rare cases, infantile hemangiomas can also grow in the area of internal organs, such as the liver or kidneys.
Special shapes
"Rapid Involuting Congenital Hemangioma / abbreviated as RICH":
These forms may also be referred to as congenital rapidly regressing hemangiomas. Already at the birth of a child, they are fully developed (doctors say “fully formed”) and quickly (in English " rapid " ) completely disappear, usually by the third year of a baby's life (doctors often use the term "involution “ , from the English term "involuting" , which means reverse development of ).
"Congenital non-involuting hemangioma (Non involuting congenital hemangioma / abbreviated NICH)"
These infantile hemangiomas may also be referred to as congenital nonregressive hemangiomas. They don't disappear on their own, but they don't grow either.
Benign neonatal hemangiomatosis
A child has many small hemangiomas on the skin that look like small millet.