Fundal placenta images
Is Placenta on Top a Problem?
The placenta is normally expelled or removed from the body after delivery. This occurs during the third stage of labor in vaginal births. People who have a retained placenta (when the placenta is not delivered within 30 minutes after birth) may experience certain post-delivery complications like bleeding or infection.
The placenta develops wherever the fertilized egg embeds in your uterus. This leads to a range of possible locations:
- Anterior position (on the front wall of your uterus, closest to the belly)
- Posterior position (on the back wall of your uterus, closest to the spine)
- Fundal position (on the top wall of your uterus)
- Lateral position (on the right or left side of your uterus)
- Low-lying placenta (low in the uterus, near to or partially covering the internal cervical os)
- Placenta previa (extending over the internal cervical os)
Take a quiz
Find out what you can do with our Health Assistant
Placental development stages
Since it can change over time, placenta positioning should be monitored throughout your pregnancy. It could move toward the upper region of the uterus as the uterus enlarges and the placenta’s attachment area stretches upward. During growth, the baby’s head starts to descend into the pelvis in preparation for labor and delivery. This movement adds pressure to the lower uterus, which causes its walls to stretch and become thinner. As a result, the placenta will usually ascend by the third trimester. In nine out of 10 cases, the placenta moves up by about 32 weeks of pregnancy.
What is a fundal placenta?
A fundal placenta appears in the fundus, or top region, of the uterus. Some people experience a combination of fundal-anterior or fundal-posterior positioning. Placental positioning is often checked between 18 and 21 weeks of pregnancy using an ultrasound.
Is it OK for the placenta to be on top?
Wherever the placenta grows, it can sufficiently nourish your baby throughout the pregnancy. As the pregnancy progresses, the placenta tends to migrate toward the upper region of the uterus. This is rarely a cause for concern unless it’s accompanied by other signs or symptoms.
This is rarely a cause for concern unless it’s accompanied by other signs or symptoms.
Fundal-anterior placenta
A fundal-anterior placenta is located mostly at the top of the uterus but also extends slightly toward the front (belly side).
Fundal-posterior placenta
A fundal-posterior placenta still appears mostly at the top of the uterus but extends slightly toward the back (spine side).
Fundal placenta complications
The most complex placental position is called placenta previa. In this condition, the cervix is covered during the third trimester of pregnancy. It can lead to severe bleeding and requires careful medical attention.
The main risk factors for placenta previa are:
- Previous placenta previa
- Previous cesarean delivery
- Multiple gestation
If the placenta covers the cervix during the third trimester, certain complications like bleeding can happen. According to researchers, placenta previa affects approximately four per 1000 births, but cases vary worldwide.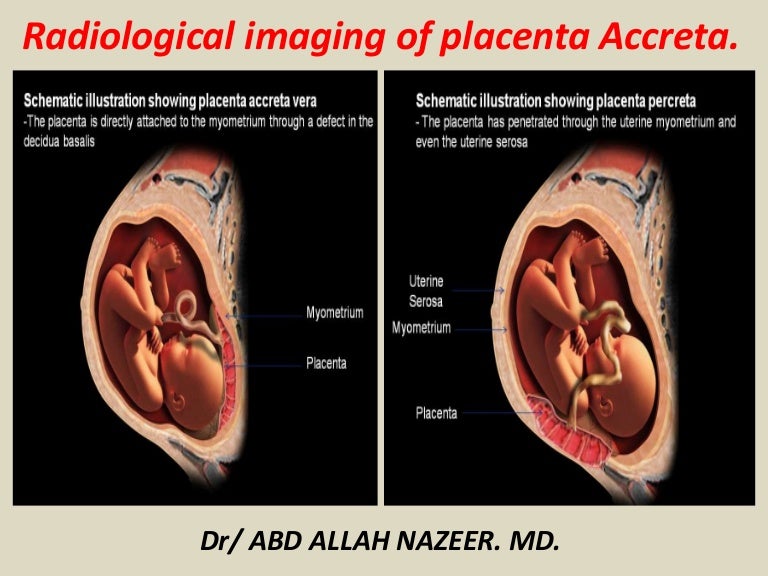
If the placenta is located anteriorly and the mother needs a cesarean section, the placenta may affect where the health care provider makes the incision.
Finally, if you’ve experienced an injury due to a fall or any other accident, it is important to undergo a physical examination. A health care provider can determine whether the health of your baby or placenta has been compromised. They may recommend extra monitoring of the position of your fetus and placenta, as well as your vital signs, to ensure a healthy pregnancy.
Fundal Placenta | Types | Position
Fundal Placenta | Types | Position | ComplicationsPress Enter
to Search
iCliniq / Health Articles / Fundal Placenta / Fundal Placenta | Types | Position | Complications
Pregnancy and Trying to conceive Data VerifiedWritten by
Dr. Preetha. J
and medically
reviewed by Dr.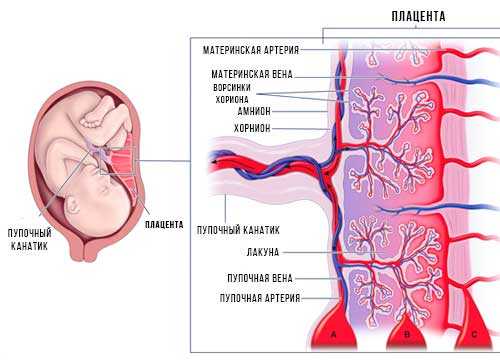 Sangeeta Milap
Sangeeta MilapPublished on Oct 22, 2021 and last reviewed on Sep 13, 2022 - 4 min read
Abstract
What does fundal placental position mean? Is it necessary to be concerned about it? And why? Get all your doubts cleared here.
Contents
What Is a Placenta?
What Is Fundal Placenta?
What Are The Types Of Fundal Placenta?
Is It Normal To Have A Fundal placenta?
What Happens If Your Placenta Is In A Bad Position?
Which Placental Position Is Good For Normal Delivery?
Will The Position Of The Placenta Keep Changing?
What Are The Complications Associated With Fundal Placental Position?
What Is a Placenta?
The placenta is an essential organ that is present only during pregnancy.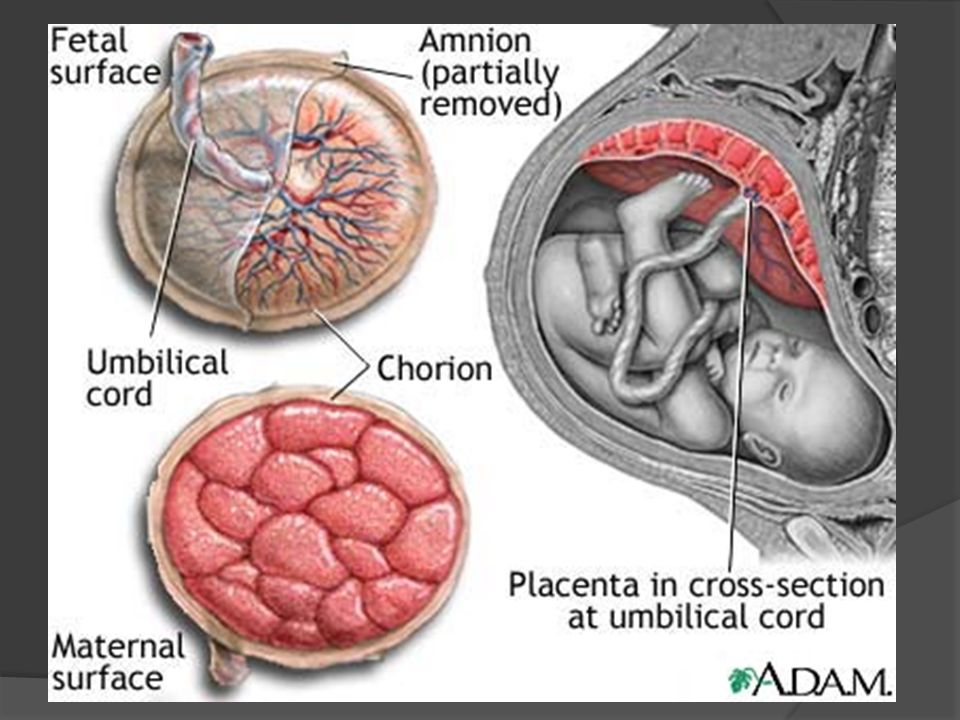 It plays a significant role in the development of the growing fetus. It helps transfer the oxygen, essential nutrients such as calcium and protein, and hormones to the growing baby and remove waste from the baby's blood.
It plays a significant role in the development of the growing fetus. It helps transfer the oxygen, essential nutrients such as calcium and protein, and hormones to the growing baby and remove waste from the baby's blood.
A placenta will usually develop in the third week of pregnancy. It can be visible as early as ten weeks during an ultrasound. The placenta is attached to the baby through an umbilical cord.
The placenta is commonly expelled from the body after the delivery, while in some cases, it is removed manually after vaginal birth. People who have a retained placenta can experience certain post-delivery complications like bleeding or infection.
The placenta is developed when the fertilized egg gets embedded in the uterus. The possible locations of the placenta are:
-
Anterior Position: On the (anterior) front wall of the uterus, which is very close to the belly.
-
Posterior Position: On the back wall of the uterus, which is very close to the spine.

-
Fundal Position: On the top wall of the uterus.
-
Lateral Position: On either side, right or left of the uterus.
-
Low-Lying Placenta: They are present low in the uterus, near or partly covering the internal cervical os (an opening in the uterus).
-
Placenta Previa: The placenta is extending over the internal cervical os. Depending upon how it has blocked the cervix, the treatment is planned, whether vaginal birth or cesarean section. Complications of placenta previa are bleeding from the placenta and preterm birth. If this does occur, close monitoring of both mother and baby should be done in the hospital.
What Is Fundal Placenta?
A fundal placenta, also called the fundic placenta, indicates that the placenta is formed in the top region of the uterus, in between the two fallopian tube openings, also known as the fundus.
The fundal placenta position is common, and the risk is low because the position alone will not pose any complications. As with any placental location, monitoring a fundal placenta's condition is essential to ensure that it provides your baby with the support they need. This will be done during a regular pregnancy ultrasound.
As with any placental location, monitoring a fundal placenta's condition is essential to ensure that it provides your baby with the support they need. This will be done during a regular pregnancy ultrasound.
A few people may experience a combination of fundal-anterior or fundal-posterior positions. Placental positioning is usually monitored between 18 and 21 weeks of pregnancy with the help of an ultrasound.
What Are The Types Of Fundal Placenta?
A fundic placenta can be classified as either:
Anterior Fundal Placenta:
A placenta formed at the top and continues down to the front of the uterus (near the belly) is called the anterior fundal placenta.
Posterior Fundal Placenta:
A placenta that is formed at the top and continues down to the back of the uterus (near the spine) is called the posterior fundal placenta.
Is It Normal To Have A Fundal placenta?
Yes, it is normal to have a fundal placenta because having a fundal placenta seems to be pretty straightforward.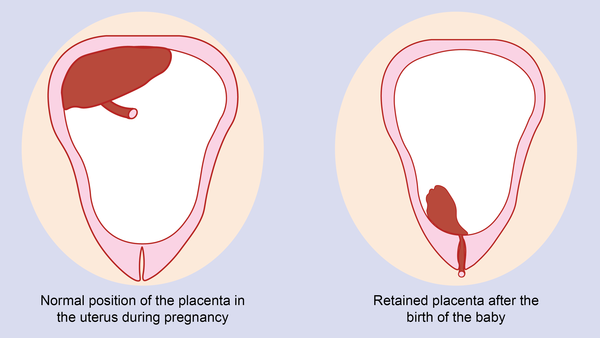 It is one of the most familiar placental locations. The placenta usually, while growing, can sufficiently nourish the growing fetus throughout the pregnancy. And as the pregnancy progresses, the placenta may tend to move toward the upper region of the uterus. Unless accompanied by any other signs or symptoms, it is rarely a cause for concern.
It is one of the most familiar placental locations. The placenta usually, while growing, can sufficiently nourish the growing fetus throughout the pregnancy. And as the pregnancy progresses, the placenta may tend to move toward the upper region of the uterus. Unless accompanied by any other signs or symptoms, it is rarely a cause for concern.
Having either anterior and posterior fundal placenta is normal, and it will not affect the growth and development of the growing fetus in the womb. It is better to have a posterior placenta than an anterior placenta because having the placenta on the back wall of the uterus, the mother can feel the baby's movements and kicks early and stronger. Furthermore, the posterior placenta is thought to be the best for the baby because it will allow the baby to grow and come down to the correct position to line up in the birth canal for a vaginal birth. The growing baby will face the mother's spine in the posterior placenta, and the crown will also come down to the birth canal with time.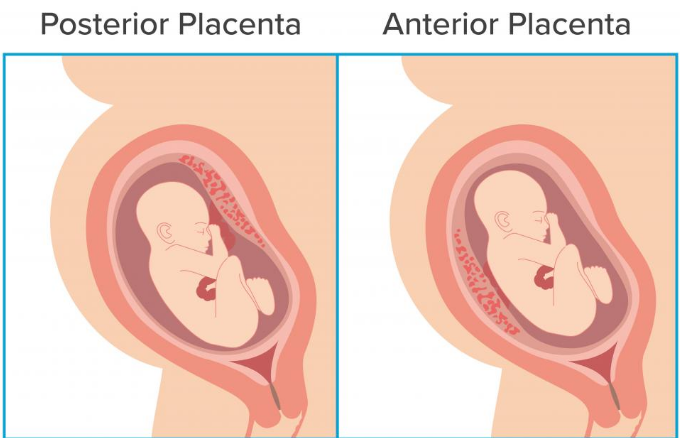
What Happens If Your Placenta Is In A Bad Position?
If your placenta is in a fundal position, there is no need to be concerned about it because the baby will still get the nourishment unless you have signs and symptoms. Such symptoms may include:
-
Bleeding.
-
Severe back pain.
-
Abdominal pain.
If you have these symptoms, please seek medical attention.
Which Placental Position Is Good For Normal Delivery?
The posterior placenta is often the perfect placental location for birth, but even having a fundal placenta or anterior placenta is not a problem.
The lateral placentas can increase the baby's chances of being in a breech position, leading to complications in the latter stages of pregnancy. The only placental position that requires a cesarean section is the placenta previa. Placenta previa can affect approximately one in 200 pregnancies and can be more likely if the pregnant woman is over 35 years or if it is not their first pregnancy and in women carrying multiples, or underwent previous uterine surgeries, like cesarean section.
The fundal position is the best because it will not get in the way of the labor or delivery process. But placentas covering the cervix can lead to life-threatening complications like bleeding during or before labor and can force the baby into a malpresentation like breech presentation.
Will The Position Of The Placenta Keep Changing?
The position of the placenta keeps changing throughout the pregnancy, either moving upward (as the baby comes down) or rarely downwards if the baby moves to the top. The placenta will take about 50 percent of the area in the uterus during the mid-term of pregnancy. It will take too little space as the baby grows and begins to come down during the later stage.
What Are The Complications Associated With Fundal Placental Position?
The most complicated placental position is called placenta previa. In this condition, the cervix is covered by the placenta during the third trimester of pregnancy. It can lead to severe complications like bleeding, and it requires careful medical attention.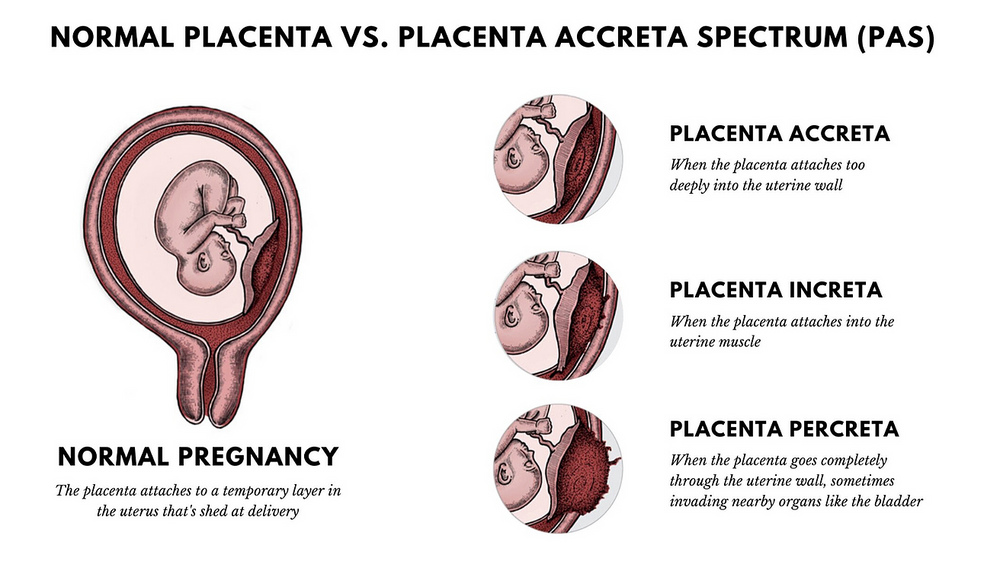
The risk factors for placenta previa are:
-
Previous cesarean delivery.
-
Multiple gestations.
-
Previous placenta previa.
1.Does the Fundal Placenta Position Carry Any Risk?
It is common for women to have a fundal placenta position, and it carries only low-risk. Also, it is important to monitor a fundal placenta as like other placental positions to ensure that the baby is provided with all the support they need, and it is done with routine pregnancy ultrasound.
2.Which Placenta Position Is Best for Normal Delivery? Posterior placenta refers to the placenta implanted onto the back of the uterus. The upper portion of the uterine back is one of the best locations for the fetus, and it helps them to move into the anterior position before birth. This position provides an advantage of feeling the baby's movements earlier, and, as said before, it allows the baby to get into the most optimum position, that is, the spine at the top of the belly (anterior) for birth. In addition, the posterior placenta does not interfere with the development of the fetus.
In addition, the posterior placenta does not interfere with the development of the fetus.
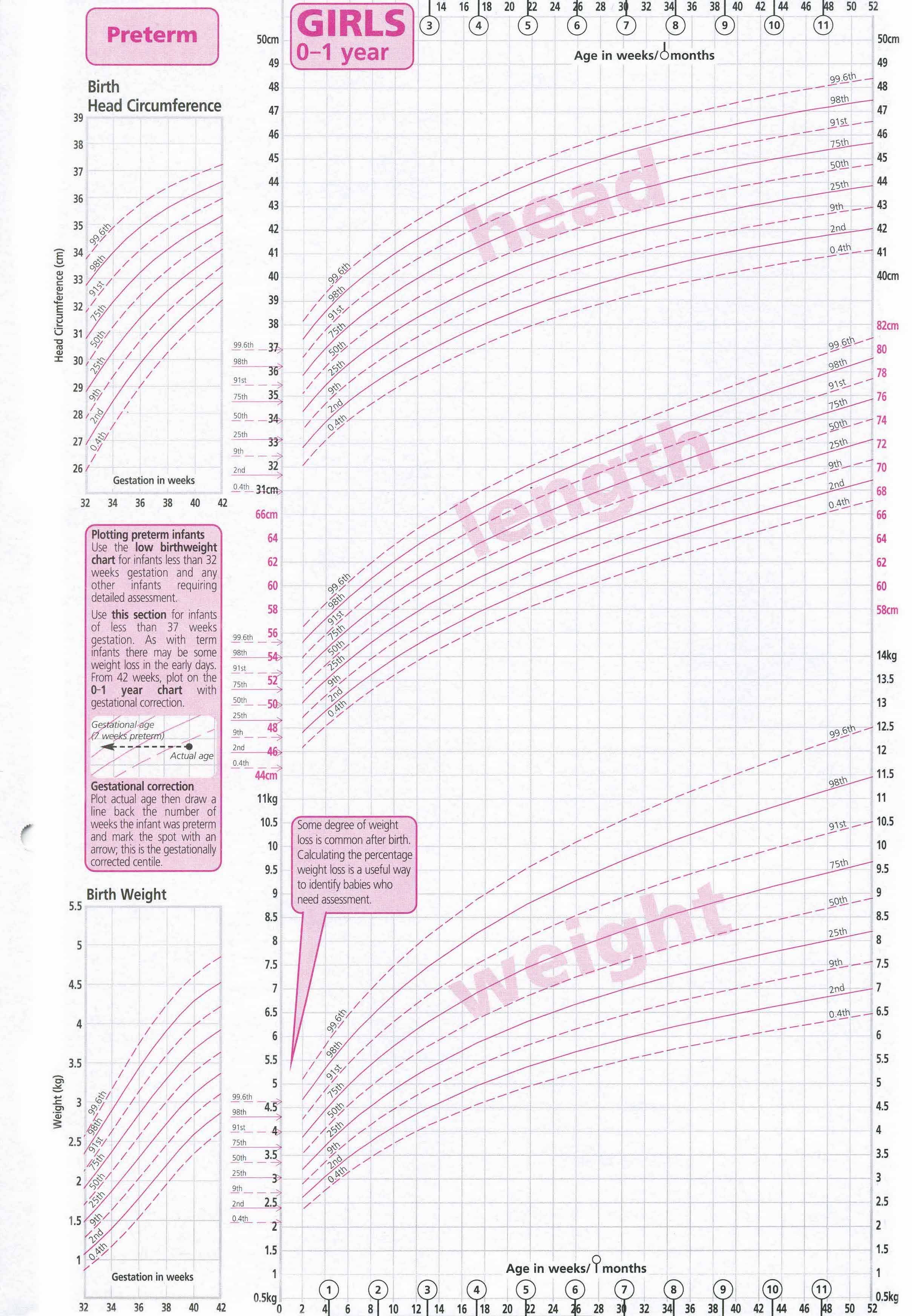
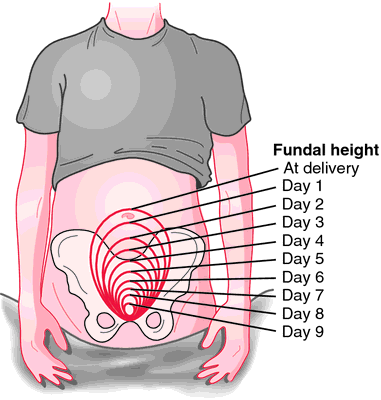
Fundal height measurement is usually done to determine the baby's height for its gestational age. Generally, the measurement is defined as the distance from the pubic bone to the top of the uterus in centimeters.
4.Is the Fundal Placenta Normal?The fundal placenta is normal and is actually one of the common placental locations. Normally, a fundal placenta is classified as either an anterior fundal placenta or a posterior fundal placenta.
5.What Determines the Position of the Placenta? An ultrasound is used to determine the position of the placenta. Usually, at the 12 th week and the 20 th week scans, an ultrasound is used. Most commonly, the placenta is located at the fundus (the top of the uterus) and anteriorly (front wall).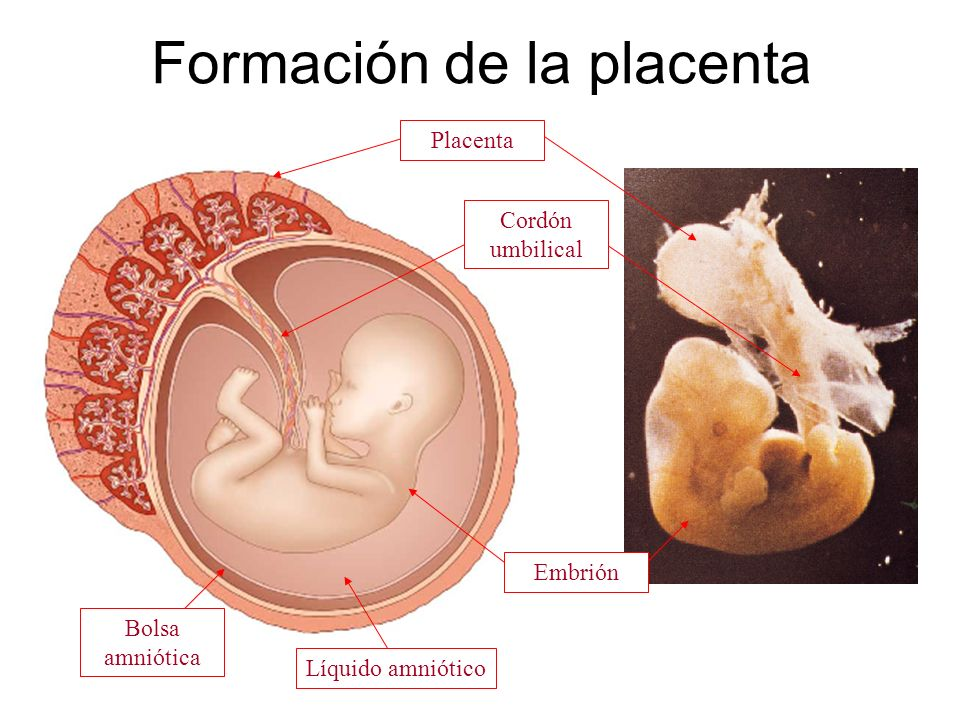
Usually, the position of the placenta does not affect the fetus or the pregnancy unless the placenta blocks the cervix. This is called placenta previa.
7.Can Baby Position Affect Fundal Height? The following factors related to the baby's position can affect the fundal height,
- The position of the baby lying.
- The shape of the tummy muscles.
- Height of the mother.
When the placenta blocks the cervix (placenta previa), it is graded into four categories, from major to minor. In the case of grade 1 or 2, a vaginal birth may be possible, but grade 3 or 4 will require a cesarean section. Despite any grade of placenta previa, you will need to live near or in places where hospitals are easily accessible in case you start bleeding.
9. Does Placenta Position Affect Bump Size?
Does Placenta Position Affect Bump Size?There is indeed an extra layer of cushioning when the placenta is positioned toward the front of the body. However, it does not increase the size of the bump.
10.Can the Placenta Position Change from Anterior to Posterior?It is common for the placenta to change its position as the uterus stretches and grows. In the case of an anterior placenta, it migrates toward the sides, top, or back of the uterus when the weeks go on.
11.What Is the Correct Position of the Placenta?Normally the placenta positions are either at the top or side of the uterus. It is possible for the placenta to attach to the front of the stomach, known as an anterior placenta, and the back of the uterus, near the spine, known as a posterior placenta.
12.What Is the Best Position for Delivery? The best position for delivery is the head down, facing the back so that the back of the fetus is towards the front of the tummy.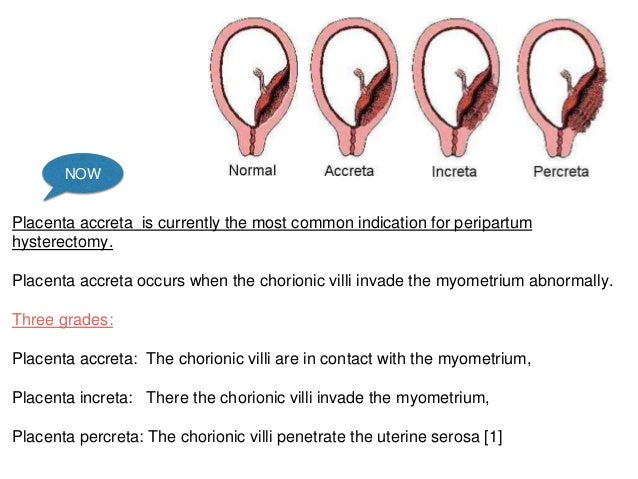 This position is called the occipito-anterior, and it allows them to move more quickly through the pelvis.
This position is called the occipito-anterior, and it allows them to move more quickly through the pelvis.
During pregnancy, a posterior placenta is associated with increased short-term complications such as a longer hospital stay.
- Placental location and pregnancy outcomes in nulliparous women: A population-based cohort study
https://pubmed.ncbi.nlm.nih.gov/30767210/ - Anterior placental location influences onset and progress of labor and postpartum outcome
https://pubmed.ncbi.nlm.nih.gov/25573094/ - What complications can affect the placenta?
https://www.nhs.uk/pregnancy/labour-and-birth/what-happens/placenta-complications/
Last reviewed at:
13 Sep 2022 - 4 min read
RATING
Give your rating
❤ 15
Dr. Sangeeta Milap
Obstetrics And Gynaecology
Tags:
- Fundal Placenta
Comprehensive Medical Second Opinion.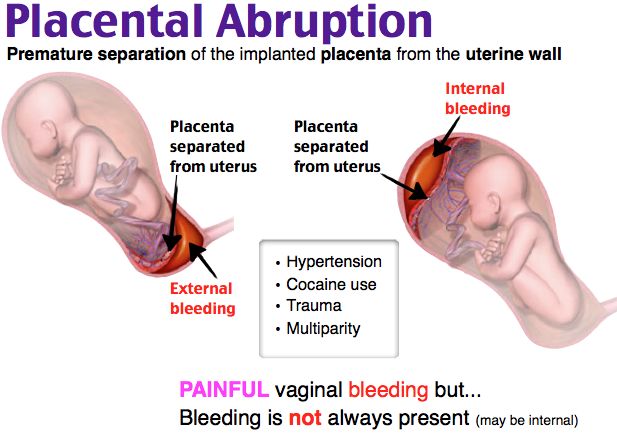 Submit your Case
Submit your Case
Most Popular Articles
Do you have a question on Fundal Placenta or ?
Ask a Doctor Online* guaranteed answer within 4 hours.
Disclaimer: No content published on this website is intended to be a substitute for professional medical diagnosis, advice or treatment by a trained physician. Seek advice from your physician or other qualified healthcare providers with questions you may have regarding your symptoms and medical condition for a complete medical diagnosis. Do not delay or disregard seeking professional medical advice because of something you have read on this website. Read our Editorial Process to know how we create content for health articles and queries.
"Placental" genes help malignant metastases
The same genes that help the mother to connect with the embryo help cancer cells to settle in a new place.
Malignant tumors occur not only in humans, but also in other mammals. But different mammals are affected differently. For example, elephants almost never get cancer, although they should - not only do elephants live long, they are also very large, and the likelihood of malignant cell transformation increases with increasing body size. The reason for the resistance of elephants to cancer is a whole set of antitumor genes. nine0003
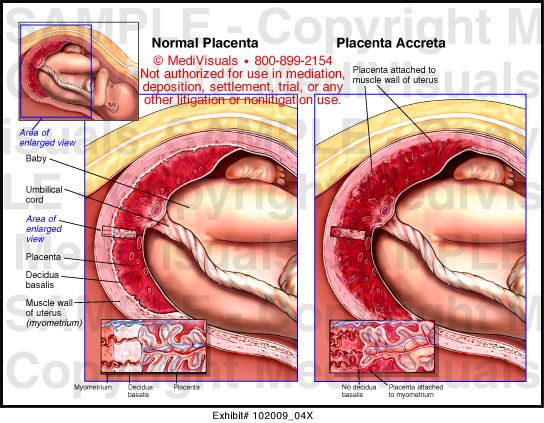
The fetus is connected through the umbilical cord to the placenta (above) - a temporary organ through which the child interacts with the mother's body. (Illustration: sciencepics / Depositphotos)
View full size
‹
›
But, for example, cows, pigs and horses get cancer, but it rarely metastasizes in them. For example, if we compare melanoma in ungulates and in humans, then in humans it will be a very aggressive tumor that is actively spreading throughout the body, while in ungulates it will sit still, as if it were not allowed anywhere else. nine0003
And this is true: wandering cancer cells in horses and cows simply cannot break into new tissue.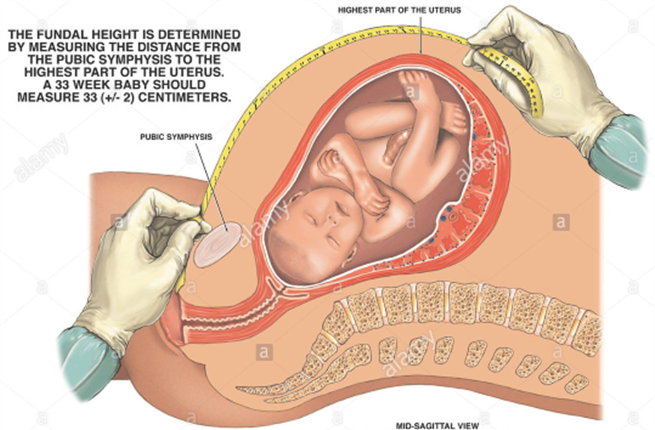 The Yale researchers decided to take a closer look at the genes that allow metastases to take root in a new place, and compare their activity in ungulates and in humans. It turned out that these are the same genes that help form the placenta. Recall that the placenta is a special organ that appears only during pregnancy and which connects the circulatory systems of the fetus and mother. Through the placenta, the embryo is supplied with nutrients and oxygen; removal of metabolic products also goes through the placenta. In addition, it helps to coordinate the work of immune systems: skipping the mother's antibodies to the child, it still prevents immune conflicts between the fetus and the mother's body. nine0003
The Yale researchers decided to take a closer look at the genes that allow metastases to take root in a new place, and compare their activity in ungulates and in humans. It turned out that these are the same genes that help form the placenta. Recall that the placenta is a special organ that appears only during pregnancy and which connects the circulatory systems of the fetus and mother. Through the placenta, the embryo is supplied with nutrients and oxygen; removal of metabolic products also goes through the placenta. In addition, it helps to coordinate the work of immune systems: skipping the mother's antibodies to the child, it still prevents immune conflicts between the fetus and the mother's body. nine0003
Almost all animals have a placenta, but in different species it is formed in different ways. It develops from special cells of the embryo, and as it develops, it literally grows into the wall of the uterus. And if we compare the placenta in horses, cows, pigs, etc., on the one hand, and in humans, on the other, we will see that in these animals the connection between the placenta and the mother's organism is not so close compared to people.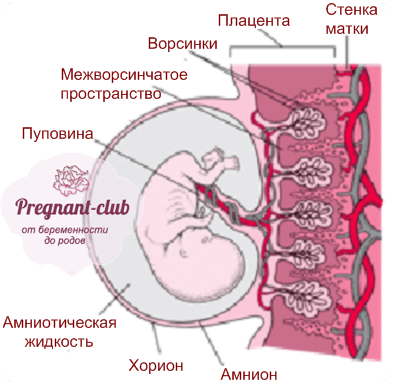
A well-developed placenta ensures better contact of the embryo and better, if I may say so, embryonic development. But at the same time, genes that help the placenta better take root in maternal tissues play into the hands of malignant cells. When the placenta grows into the uterus, the cells of the uterus must give way to it and help it take root; accordingly, certain genes are activated in the receiving tissue. Just these genes work differently in humans and in ungulates. nine0003
It is known that cancer cells are somewhat similar to embryonic ones, and when in a person metastases from a primary melanoma tumor come to a new area of \u200b\u200bthe skin or to the same uterus, they are perceived in a new place as partly embryonic cells that need to be allowed to grow here. And when the same thing happens, say, in a cow, then metastatic cells stumble upon an indifferent reception - because the genes that help the placenta grow in work poorly, and cancer cells stumble upon a cold reception.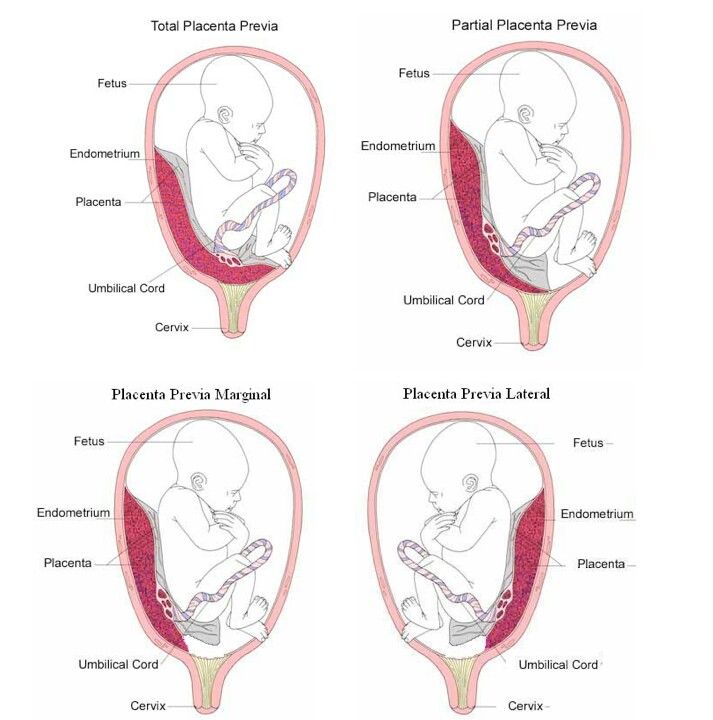 nine0003
nine0003
Nature Ecology & Evolution describes experiments with skin cells and uterine cells that have been encountered with metastatic melanoma cells. If in human cells of the skin and uterus the activity of “placental” genes (that is, those that open the way to the placenta) was lowered to the level of a cow, then human cells stopped letting melanoma metastases in. Of course, it is possible that cancer cells somehow force the “placental” genes to turn on even where they should not work. However, the bottom line is that in humans, these genes are initially well-behaved for deception - simply because humans have acquired a more perfect placenta in the course of evolution. Perhaps in the future it will be possible to make some kind of drug that would act on “placental” genes throughout the body, blocking the entrance to metastases. nine0003
Pathology of the placenta in COVID-19
Like all categories of the population, pregnant women are susceptible to coronavirus infection. In such cases, the risks of developing organ and tissue lesions typical of the SARS-CoV-2 virus on the part of both the mother and the fetus are always considered. The link between the two organisms is the placenta. The study of changes in the tissue and vascular bed of the placenta is of particular interest to researchers. At the recent fourth congress of pathologists in Minsk, a report on this topic was made by the head of the department of pediatric pathology of the City Clinical Pathological Bureau of Minsk, Ph.D. Sciences Ivan Sakharov. nine0032
In such cases, the risks of developing organ and tissue lesions typical of the SARS-CoV-2 virus on the part of both the mother and the fetus are always considered. The link between the two organisms is the placenta. The study of changes in the tissue and vascular bed of the placenta is of particular interest to researchers. At the recent fourth congress of pathologists in Minsk, a report on this topic was made by the head of the department of pediatric pathology of the City Clinical Pathological Bureau of Minsk, Ph.D. Sciences Ivan Sakharov. nine0032
Ways of penetration of the infection into the fetus
According to Ivan Sakharov, with any infections, the most obvious are two ways of penetration of the infectious agent into the fetus. First, by ingestion or aspiration of infected amniotic fluid, which usually occurs with bacterial infections. The ascending pathway of the spread of the bacterial agent in the fetal tissue causes a classic infectious process.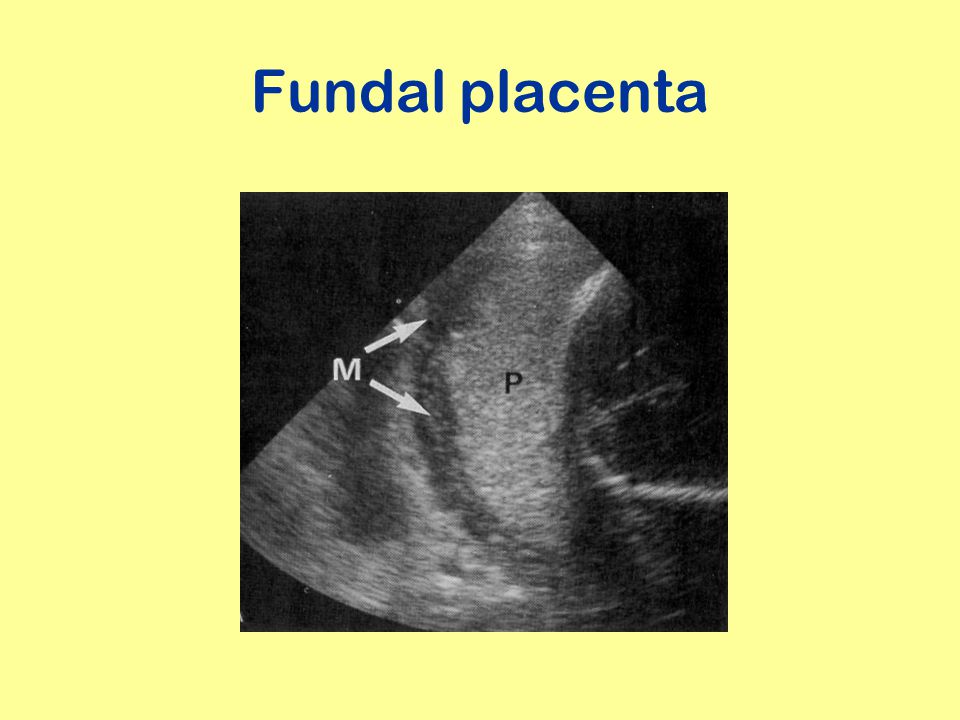
Most viral infections (and some bacterial ones) are characterized by the second path: the infectious agent overcomes the placental barrier and enters the blood of the fetus with the development of infection, and immediately a generalized form, with clinical and morphological manifestations.
Ivan Sakharov:
There is another way that the pathological infectious process in the mother's body affects the fetus, it is realized through the defeat of the placenta. In this case, the infectious agent does not penetrate the fetal bloodstream, but pathological changes developing in the placenta can lead to fetal death. Two pathogenic mechanisms may be involved in mediated fetal injury across the placenta ( see fig. 1 ).
Infection of the placenta leads to inflammatory changes, which is accompanied by the release of inflammatory mediators. Circulating in the fetal body, they cause clinical manifestations of the infectious process, although there is no infectious agent in the fetal body.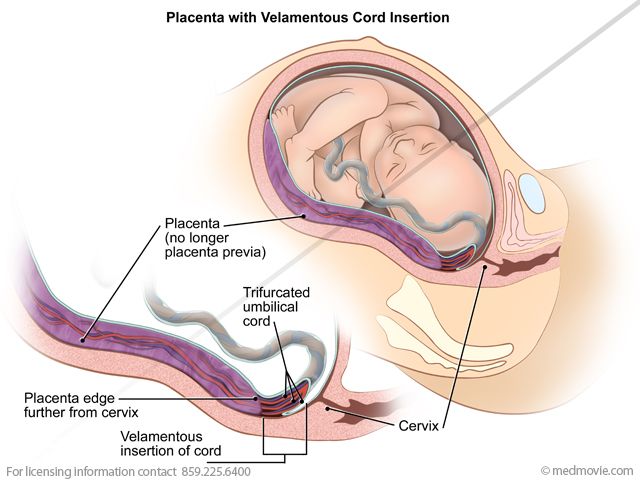 The second mechanism is realized due to violations of placental blood flow, which leads to fetal hypoxia. These two mechanisms do not exclude each other, they can be combined, including with the implementation of pathways for the penetration of the pathogen into the fetal bloodstream. nine0003
The second mechanism is realized due to violations of placental blood flow, which leads to fetal hypoxia. These two mechanisms do not exclude each other, they can be combined, including with the implementation of pathways for the penetration of the pathogen into the fetal bloodstream. nine0003
Figure 1. Pathogenetic mechanisms of fetal damage through the placenta.
Viral damage to cells
Ivan Sakharov:
viruses infect cells differently. Many DNA viruses (CMV, HSV types 1 and 2, rubella virus, HIV, Zika virus) are able to cross the placental barrier and cause characteristic changes with a specific morphological pattern. nine0003
Thus, CMV and HSV cause chronic lymphoplasmacytic villitis and intervillitis, as well as characteristic cell changes that are detected by immunohistochemical methods. In Zika virus infection, there is no inflammatory response, but macrophage proliferation may be observed.
RNA viruses are much more difficult to diagnose - they do not have a specific morphology of the lesion. An examination of the placenta reveals inflammation in the intervillous space - nonspecific intervillitis, as well as massive prolapse of fibrin, which leads to impaired blood flow. nine0032
The specialist recalled that this is not the first time humanity has encountered coronavirus infections. So, in 2002-2004, during an outbreak of SARS-CoV infection, about 100 pregnant women were infected. The infection was accompanied by an increased risk of maternal death and miscarriage. At the same time, only violations of maternal and fetal blood flow were detected in the placenta without a specific morphological pattern.
The second outbreak of the MERS-CoV coronavirus infection, known as the Middle East Respiratory Syndrome, is of a slow nature, has continued since 2012 and is limited to the countries of the Middle East. It spreads as an anthroponosis, with the transmission of viruses from camels to humans.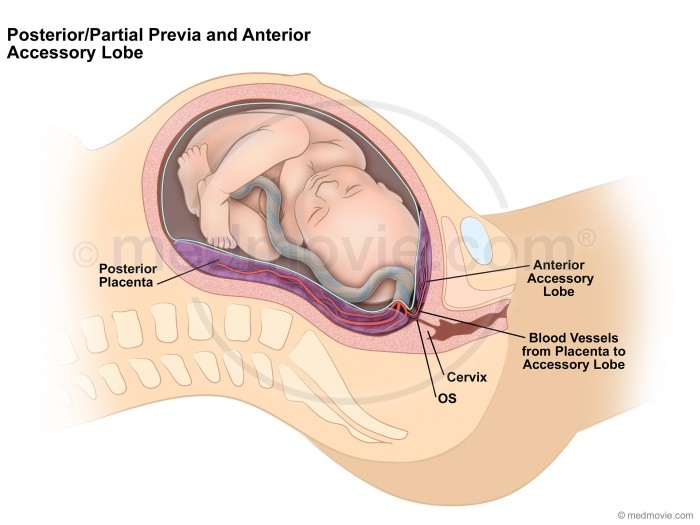 Described about 1 900 sick, including 5 pregnant women.
Described about 1 900 sick, including 5 pregnant women.
Fetal blood flow in normal
Ivan Sakharov:
The uniqueness of the placenta structure is that two blood flow that is not mixed, this moment is fundamental. Fetal blood flow is provided through the vessels of the umbilical cord, everything is normal here: the arteries pass into the arterioles, the arterioles branch into capillaries in the villi, the blood collects in the venous vessels and then flows through the umbilical vein through the umbilical cord. nine0003
Maternal circulation is organized differently. Blood flow is carried out through the maternal uterine arteries, which end not in capillaries, but in the intervillous space. Arterial blood arrives in the villi, and is collected in the uterine veins, bypassing the capillary bed, that is, from the arteries it goes directly to the veins ( see Fig. 2 ).
Figure 2.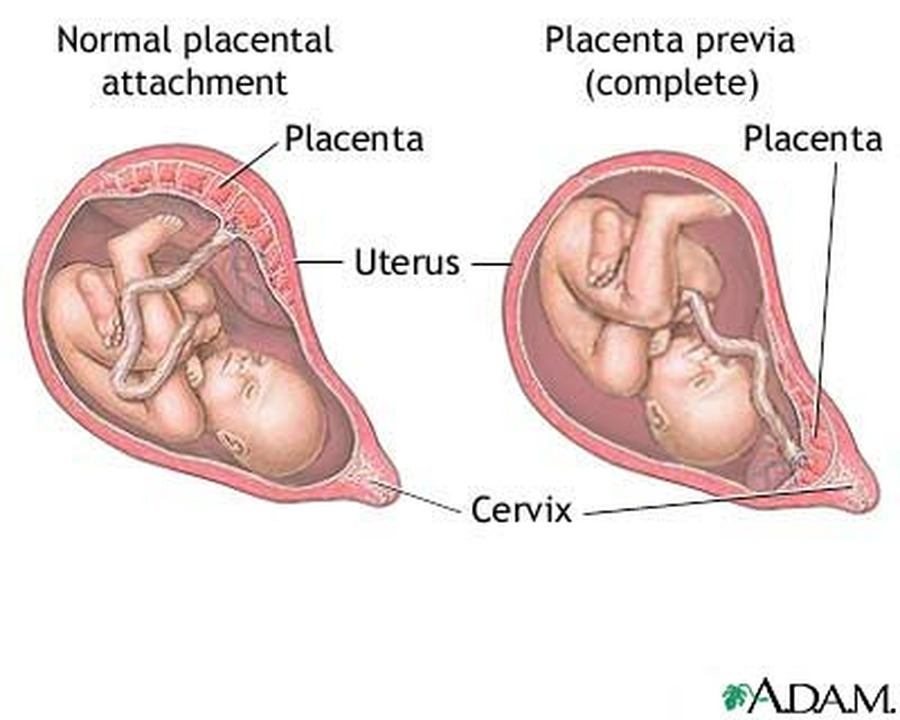 Blood flow in the placenta is normal.
Blood flow in the placenta is normal.
Pregnant women and SARS-COV-2
From the very beginning of the COVID-19 pandemic, articles about infection of pregnant women and pathology of the placenta began to appear. The researchers stated that in most placentas from pregnant women with confirmed coronavirus infection, there are no or minimal changes, usually in the 3rd trimester. The relationship of placental injury with the severity of the infection has not been established. However, such data were in 2020 and early 2021, when the alpha, beta, and gamma strains were circulating. Later, more severe manifestations of coronavirus lesions of the placenta were described, which coincided in time with the appearance of the delta strain. nine0003
Ivan Sakharov:
For the first time we have seen the damage to the tissue and blood vessels of the placenta at the macro- and microscopic level.
Morphological signs of placental lesions
The specialist summarized all the possible types of pathology described in the literature that occur in the placenta with COVID-19.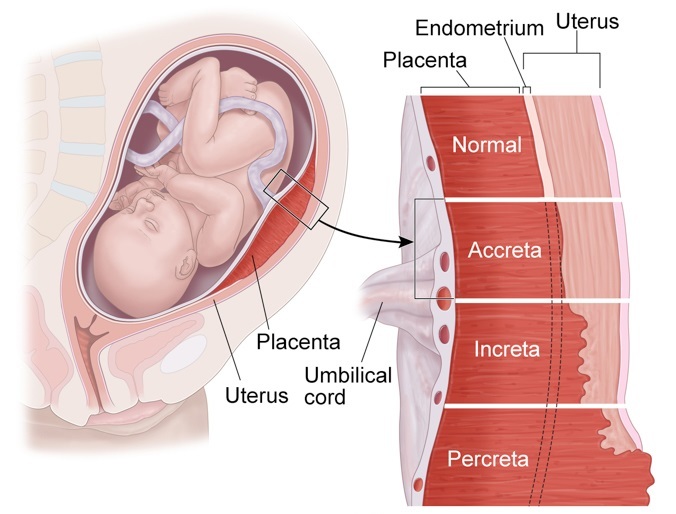 As a rule, maternal blood flow disorders and inflammatory changes predominate, the rest are less common. nine0003
As a rule, maternal blood flow disorders and inflammatory changes predominate, the rest are less common. nine0003
Massive loss of fibrin ( see Fig. 3 ) is a very noticeable and striking sign. Sometimes the villi are so walled up by the precipitated fibrin that it is difficult to find and examine them, the maternal blood circulation is disturbed. Gas exchange in the placenta is significantly reduced or completely stopped, which leads to hypoxia and fetal death.
Intervillous space thrombosis ( see Fig. 4 ). Layered thrombi are formed in the vessels, pushing villi to the periphery, which cease to participate in gas exchange. nine0003
Ivan Sakharov noticed that the changes are so bright that they are visible at the macroscopic level. If normally the placental tissue is loose, saturated red and resembles a blood-soaked sponge, then with thrombosis it becomes yellowish-gray, very dense and dry.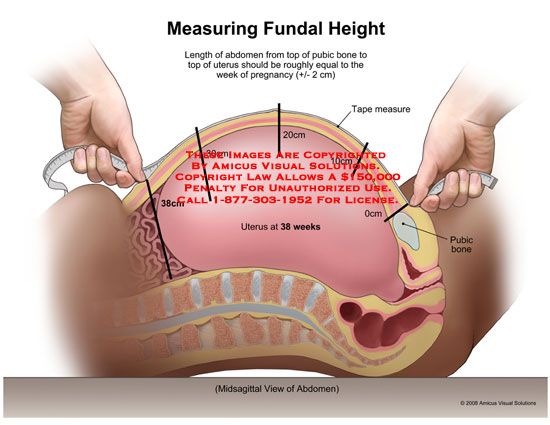 It contains areas filled with blood - these are hemorrhages and forming blood clots.
It contains areas filled with blood - these are hemorrhages and forming blood clots.
Decidual arteriopathy ( see Fig. 5 ) is a characteristic finding. Fibrinoid necrosis and inflammatory infiltration are observed in the walls of arterial vessels. nine0003
Lymphohistiocytic villitis, thrombosis ( see fig. 6, 7 ).
In the intervillous space, accumulations of inflammatory infiltrate, thrombosis of the vessels of the villi, violations of the maturation of the villous chorion are visible.
“The stereotypical reaction of the placenta to damage is a violation of maturation. Both according to the literature and our own experience, we have encountered this with confirmed COVID-19. In contrast to mature placental tissue, a very loose stroma is visible. With severe lymphohistiocytic villitis, as a rule, thrombosis of vessels is observed - both large and capillaries.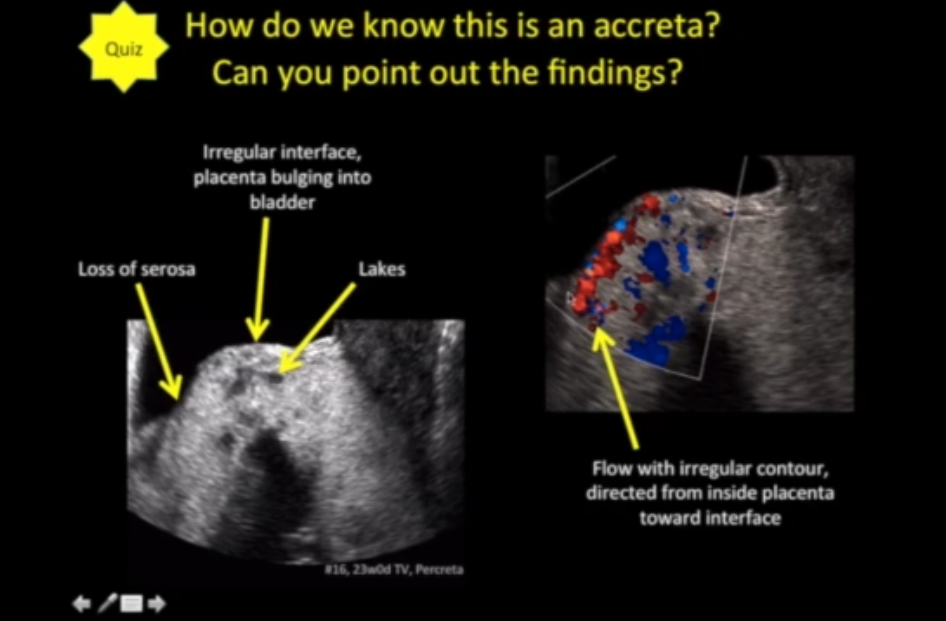 nine0032
nine0032
Patterns of pathology
Ivan Sakharov presented the results of his own observations of placental pathology in pregnant women with COVID-19. The analysis of the data obtained made it possible to determine the patterns of lesions of the placental tissue.
Ivan Sakharov:
Scanning histological preparations at low magnification, we saw large areas of thrombosis with massive loss of fibrin in the intervillous space. At high magnification in the periphery of thrombosis sites, inflammatory infiltration is observed in the villi and intervillous space. You can see how fibrin literally seals the villi. nine0003
Mostly fresh fibrin, although there are also areas of more mature fibrin. That is, at the morphological level, we assume that the defeat of the placenta occurs quickly enough and leads to the death of the fetus. All this is confirmed by clinical data.
Investigating the inflammatory infiltration of the intervillous space, we performed specific staining.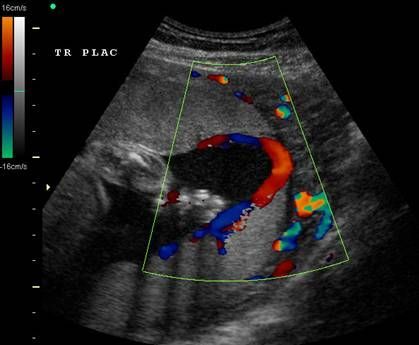 The infiltrate was predominantly CD68-positive, with few CD20-positive cells, with virtually no CD3 staining. nine0003
The infiltrate was predominantly CD68-positive, with few CD20-positive cells, with virtually no CD3 staining. nine0003
Summarizing all the signs of placental damage in COVID-19, they can be divided into three groups: maternal blood flow, fetal blood flow and inflammatory changes.
Maternal malperfusion - infarction, massive fibrin prolapse and thrombosis in the intervillous space, accelerated maturation of the villi, decidual arteriopathy.
Fetal malperfusion - thrombosis/stenosis of the vessels of the villi, avascular villi, delayed maturation of the villi. nine0003
Inflammatory changes - chronic villitis, fetal vasculitis, intervillitis, basal deciduitis.
Ivan Sakharov:
The available literature data and our own studies indicate a nonspecific lesion of the placenta in COVID-19. We see nonspecific inflammatory infiltration and impaired blood flow.