Miscarriage clots size
Miscarriage - Atlanta Gynecology and Obstetrics
Loss of pregnancy before 20 weeks is called a miscarriage. Spontaneous miscarriage is the most common complication of early pregnancy and the rate decreases as the pregnancy progresses.
Miscarriages occur in 8-20% of clinically-recognized pregnancies:
- 80% of these happen in the first 12 weeks of pregnancy
- The rate of loss for unrecognized or “chemical pregnancies” is 13-26%
- The overall risk of loss after 15 weeks is relatively low
Causes of miscarriage
Though it is difficult to identify what causes all miscarriages, most pregnancy losses are thought to be due to chromosomal defects.
- Chromosomal Abnormalities > 60%
- Maternal: Structural Abnormalities
- Uterine Fibroids, Septums, and Adhesions
- Trauma
- Acute Infections
- Blood Disorders (Thrombophilia)
- Unexplained
Loss of viability of the pregnancy usually occurs between 6-12 weeks. Recognition may not occur until weeks later. The course of treatment that you take will depend on your current condition, your desires, the size of your pregnancy, and your provider recommendations.
Factors associated with miscarriage
There can be many factors that affect the probability of having a miscarriage. In many cases, there is more than one factor that comes into play. If you know what these factors are, you can be more cautious.
- Age: Miscarriage risk increases with age. The risk can be as high as 40% at 40 years old and 80% after 45 years old
- Previous miscarriage: The rate of miscarriage increases with the number of previous miscarriages: 20% after one, 28% after two consecutive, and 43% after three or more consecutive losses
- Smoking: Increases the risk of loss
- Alcohol use: Studies have been inconsistent in proving that alcohol can cause an increased rate of pregnancy loss.
 One study indicated that there was an increase in miscarriages among women who drank more than 3 drinks a day
One study indicated that there was an increase in miscarriages among women who drank more than 3 drinks a day - Cocaine use
- Non-steroid anti-inflammatories (NSAIDs: Ibuprofen, Advil, Motrin): May be associated with an increased risk of miscarriage if used around the time of conception. The prostaglandin in NSAIDs may interfere with proper implantation
- Caffeine: The risks of miscarriage increase with high levels of consumption (>300mg /day)
Miscarriage at home
You may first note mild vaginal spotting and/or cramping. This bleeding and cramping will increase, at which point you may expel the tissue of the pregnancy. During the miscarriage, you may bleed heavily with large clots, soaking a pad every 10-20 minutes. The cramping may be significant. Tylenol and a heating pad are okay to use at this time. You should call the office or the on-call doctor if the heavy bleeding does not improve after two hours.
Once you have passed the pregnancy tissue, you will notice a decrease in bleeding and cramping. You may collect the passed tissue and store it in a clean and dry container and bring it to the office so that it may be sent out for pathological identification. You may call the office or the on-call doctor at any time for direction and advice.
Office Number: 404-299-9724 | After Hours Number: 404-487-2450
D&C at the hospital
A D&C is a surgical procedure performed under anesthesia to remove tissue from the uterus that has not started to or that has not entirely come out.
A D&C is an outpatient procedure that lasts for about 15-20 minutes. You usually go home about 1-2 hours after the procedure is completed. Most women return to light duties and activity the next day. Cramping and bleeding are common after a D&C. You may have bleeding for up to 2 weeks after your procedure.
Alternatively, we offer appropriate candidates a procedure called a Mechanical Vacuum Aspiration (MVA).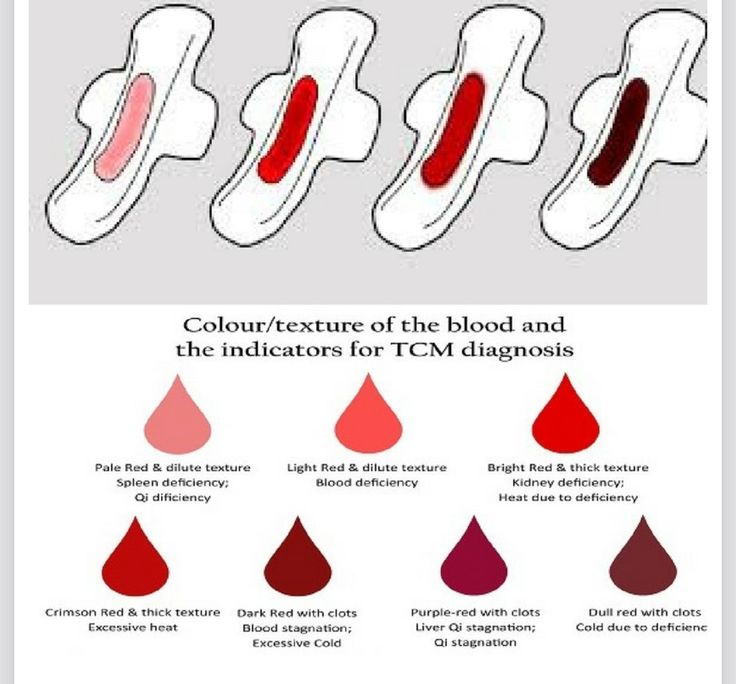 This procedure is similar to the D&C, but it can be done in the office under local anesthesia. Recovery and warning signs are similar to those of the D&C procedure.
This procedure is similar to the D&C, but it can be done in the office under local anesthesia. Recovery and warning signs are similar to those of the D&C procedure.
With either of these procedures, we recommend that you do not put anything in the vagina (no tampons, douching, or intercourse) until you are seen again in the office.
Warning signs after a miscarriage or D&C
Call the office if you have:
- Temperature > 100.4
- Nausea and vomiting for > 12 hours
- Increasing pain or bleeding
- Foul-smelling vaginal discharge
Coping with the loss of pregnancy
Emotional healing can take longer than physical healing. Grief after a pregnancy loss is a normal response. In the days and weeks after your pregnancy loss, you may experience a loss of appetite, emotional changes, irritability, sleep disturbances, and inability to focus on daily tasks. This is all normal and should resolve in a few weeks or months. If you find that these symptoms are severe or that you are unable to cope with these feelings, please call and make an appointment to talk to a provider in our practice. We will be able to help you and make any other referrals you may need.
If you find that these symptoms are severe or that you are unable to cope with these feelings, please call and make an appointment to talk to a provider in our practice. We will be able to help you and make any other referrals you may need.
The next pregnancy
Your next period should come within 4-6 weeks after your miscarriage. We recommend that you use contraception until after you have had a normal period. You may continue prenatal vitamins during and after this time. You may also discuss birth control at your post-miscarriage visit if you do not desire to become pregnant again.
Miscarriage - what you might actually see and feel
Miscarriage - what you might actually see and feel | Pregnancy Birth and Baby beginning of content7-minute read
Listen
WARNING — This article contains some graphic descriptions of what you might see during a miscarriage.
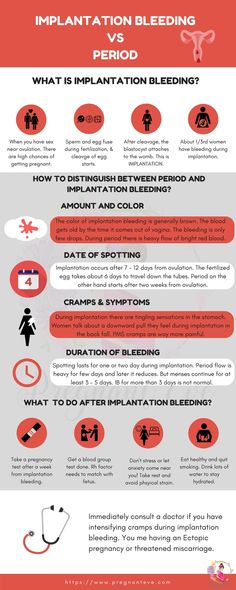
A miscarriage requires prompt medical care. If you think you are having a miscarriage, call your doctor or midwife for advice and support. Go to the Emergency Department if:
- you are bleeding very heavily (soaking more than 2 pads per hour or passing clots larger than golf balls)
- you have severe pain in your tummy or shoulder
- you have a fever (a temperature above 38 degrees C)
- you are dizzy, fainting or feel like fainting
- you notice fluid coming from your vagina that smells bad
- you have diarrhoea or pain when you have a bowel motion (do a poo)
Miscarriage is a very unfortunate and sad outcome of pregnancy that takes a significant emotional and physical toll on a woman. It also happens more frequently than many people think. It's important to recognise that there's no right or wrong way to feel about a miscarriage.
Despite close to one in 5 pregnancies ending in miscarriage, what actually happens and what a woman needs to know and do when faced with a possible miscarriage are subjects that rarely get discussed.
This article aims to give you an idea of what happens and what a woman needs to know and do at different stages in her pregnancy.
Please call Pregnancy, Birth and Baby on 1800 882 436 if you have any concerns or wish to discuss the topic further.
What might I feel during a miscarriage?
Many women have a miscarriage early in their pregnancy without even realising it. They may just think they are having a heavy period. If this happens to you, you might have cramping, heavier bleeding than normal, pain in the tummy, pelvis or back, and feel weak. If you have started spotting, remember that this is normal in many pregnancies — but talk to your doctor or midwife to be safe and for your own peace of mind.
Later in your pregnancy, you might notice signs like cramping pain, bleeding or passing fluid and blood clots from your vagina. Depending on how many weeks pregnant you are, you may pass tissue that looks more like a fetus, or a fully-formed baby.
In some types of miscarriage, you might not have any symptoms at all — the miscarriage might not be discovered until your next ultrasound. Or you might just notice your morning sickness and breast tenderness have gone.
Or you might just notice your morning sickness and breast tenderness have gone.
It is normal to feel very emotional and upset when you realise you’re having a miscarriage. It can take a while to process what is happening. Make sure you have someone with you, for support, and try to be kind to yourself.
What happens during a miscarriage?
Unfortunately, nothing can be done to stop a miscarriage once it has started. Any treatment is to prevent heavy bleeding or an infection.
Your doctor might advise you that no treatment is necessary. This is called 'expectant management', and you just wait to see what will happen. Eventually, the pregnancy tissue (the fetus or baby, pregnancy sac and placenta) will pass naturally. This can take a few days or as long as 3 to 4 weeks.
It can be very hard emotionally to wait for the miscarriage because you don’t know when it will happen. When it starts, you will notice spotting and cramping and then, fairly quickly, you will start bleeding heavily.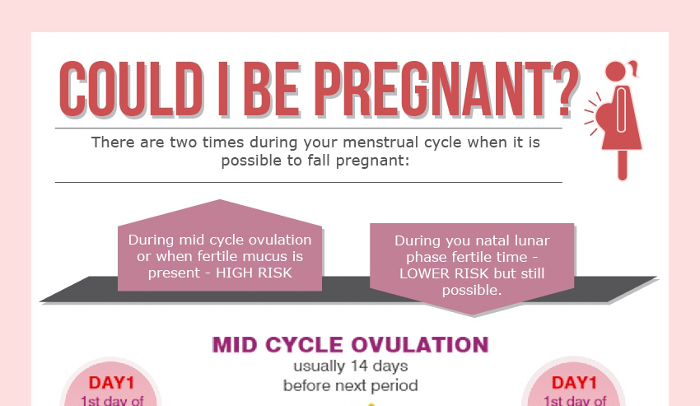 The cramps will get worse until they feel like contractions, and you will pass the pregnancy tissue.
The cramps will get worse until they feel like contractions, and you will pass the pregnancy tissue.
Some women opt to have medicine to speed up the process. In this case, the pregnancy tissue is likely to pass within a few hours.
If not all the tissue passes naturally or you have signs of infection, you may need to have a small operation called a ‘dilatation and curettage’ (D&C). You may need to wait some time for your hospital appointment. The operation only takes 5 to 10 minutes under general anaesthetic, and you will be able to go home the same day.
While you are waiting for a miscarriage to finish, it’s best to rest at home — but you can go to work if you feel up to it. Do what feels right for you. You can use paracetamol for any pain. If you are bleeding, use sanitary pads rather than tampons.
What might I see during a miscarriage?
In the first month of pregnancy, the developing embryo is the size of a grain of rice so it is very hard to see. You may pass a blood clot or several clots from your vagina, and there may be some white or grey tissue in the clots. The bleeding will settle down in a few days, although it can take up to 2 weeks.
You may pass a blood clot or several clots from your vagina, and there may be some white or grey tissue in the clots. The bleeding will settle down in a few days, although it can take up to 2 weeks.
At 6 weeks
Most women can’t see anything recognisable when they have a miscarriage at this time. During the bleeding, you may see clots with a small sac filled with fluid. The embryo, which is about the size of the fingernail on your little finger, and a placenta might be seen inside the sac. You might also notice something that looks like an umbilical cord.
At 8 weeks
The tissue you pass may look dark red and shiny — some women describe it as looking like liver. You might find a sac with an embryo inside, about the size of a small bean. If you look closely, you might be able to see where the eyes, arms and legs were forming.
At 10 weeks
The clots that are passed are dark red and look like jelly. They might have what looks like a membrane inside, which is part of the placenta. The sac will be inside one of the clots. At this time, the developing baby is usually fully formed but still tiny and difficult to see.
The sac will be inside one of the clots. At this time, the developing baby is usually fully formed but still tiny and difficult to see.
At 12 to 16 weeks
If you miscarry now, you might notice water coming out of your vagina first, followed by some bleeding and clots. The fetus will be tiny and fully formed. If you see the baby it might be outside the sac by now. It might also be attached to the umbilical cord and the placenta.
From 16 to 20 weeks
This is often called a 'late miscarriage'. You might pass large shiny red clots that look like liver as well as other pieces of tissue that look and feel like membrane. It might be painful and feel just like labour, and you might need pain relief in hospital. Your baby will be fully formed and can fit on the palm of your hand.
After the miscarriage
You will have some cramping pain and bleeding after the miscarriage, similar to a period. It will gradually get lighter and will usually stop within 2 weeks.
The signs of your pregnancy, such as nausea and tender breasts, will fade in the days after the miscarriage. If you had a late miscarriage, your breasts might produce some milk. You will probably have your next period in 4 to 6 weeks.
Remember, it’ll be normal to feel very emotional and upset at this time.
More information
Read more about miscarriage:
- What is a miscarriage?
- What happens after a miscarriage
- Emotional support after miscarriage
- Fathers and miscarriage
- Experiencing a pregnancy loss
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
KidsHealth (Understanding miscarriage), The Royal Women's Hospital (Treating miscarriage), Pink Elephants Support Network (Sorry for your loss), Women’s and Children’s Health Network (Miscarriage), Patient. com (Miscarriage and bleeding in early pregnancy), Pink Elephants Support Network (Treatments and procedures), New Kids Center (Blood Clots of Miscarriage: What It Looks Like?), Babycenter Australia (Understanding late miscarriage)
com (Miscarriage and bleeding in early pregnancy), Pink Elephants Support Network (Treatments and procedures), New Kids Center (Blood Clots of Miscarriage: What It Looks Like?), Babycenter Australia (Understanding late miscarriage) Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: March 2022
Back To Top
Related pages
- Fathers and miscarriage
- Emotional support after miscarriage
- What happens after miscarriage
- Miscarriage
- Experiencing a pregnancy loss
Need more information?
Miscarriage
Miscarriage Despite being common and widespread, miscarriage can be a heartbreaking experience – with up to one in five pregnancies ending before week 20
Read more on Gidget Foundation Australia website
Miscarriage
A miscarriage is the loss of a baby, usually during the first three months or first trimester of pregnancy.
Read more on Pregnancy, Birth & Baby website
Fathers and miscarriage
A miscarriage can be a time of great sadness for the father as well as the mother.
Read more on Pregnancy, Birth & Baby website
Emotional support after miscarriage
It is important to know that there is no right or wrong way to feel after experiencing a miscarriage.
Read more on Pregnancy, Birth & Baby website
What happens after miscarriage
There are a number of things you may need to consider after a miscarriage.
Read more on Pregnancy, Birth & Baby website
Miscarriage | SANDS - MISCARRIAGE STILLBIRTH NEWBORN DEATH SUPPORT
Helping you understand the complex range of emotions you may experience during fertility treatment or after miscarriage or early pregnancy loss
Read more on Sands Australia website
Miscarriage: a guide for men | Raising Children Network
This Dads Guide to Pregnancy covers miscarriage, the grief men might experience after miscarriage, and how to support partners after pregnancy loss.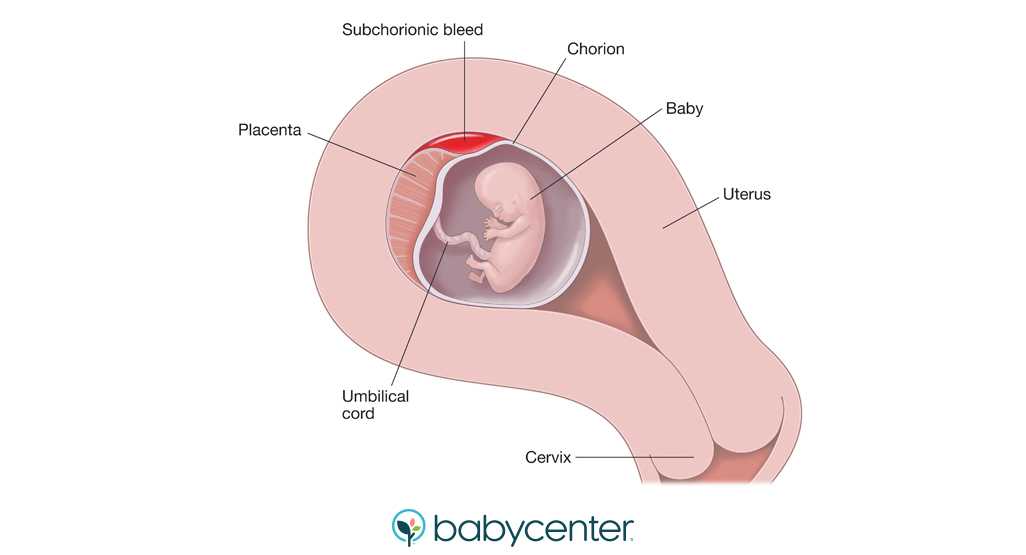
Read more on raisingchildren.net.au website
The Pink Elephants Support Network - Medical Options for Recurrent Miscarriage
In some cases, a medical reason for miscarriage or recurrent miscarriage can be found through testing
Read more on Pink Elephants Support Network website
New research on vitamin B3 and miscarriages
Pregnant women are being warned not to start taking vitamin B3 supplements, despite a recent study that suggests it might reduce the risk of miscarriages and birth defects.
Read more on Pregnancy, Birth & Baby website
Pregnancy: miscarriage & stillbirth | Raising Children Network
Have you experienced a miscarriage or stillbirth? Find articles and videos about coping with the grief of losing a pregnancy or having a stillbirth.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.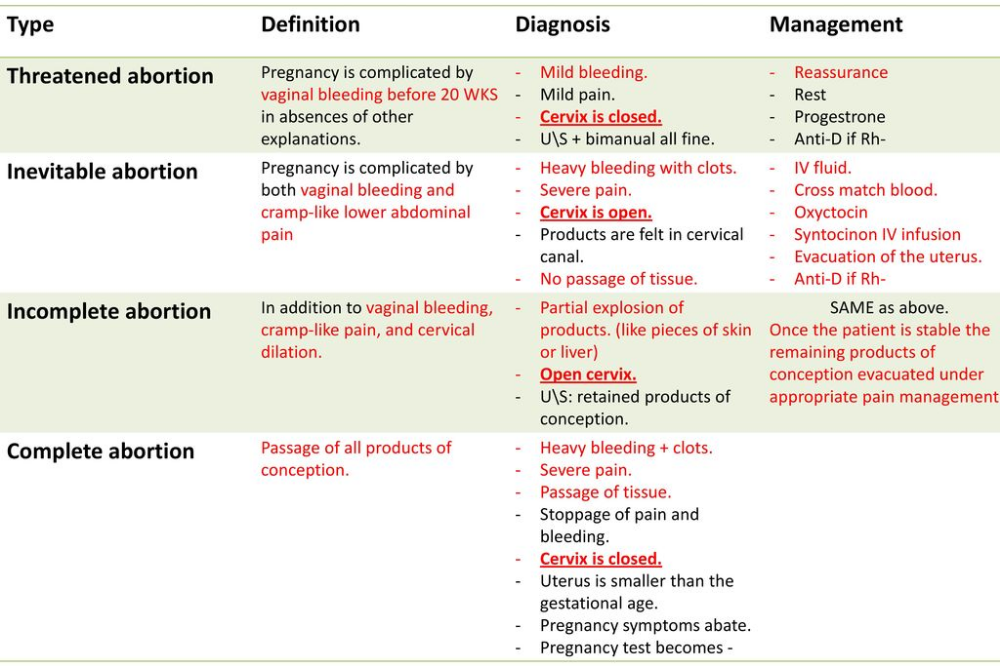
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Spontaneous abortion (miscarriage)
If the pregnancy is terminated naturally before the fetus reaches gestational age, this is called a spontaneous abortion or miscarriage. More than half of miscarriages occur no later than 12 weeks of gestation due to fetal abnormalities. The rest falls on the period up to 20 weeks and is associated with pathologies of pregnancy. If the pregnancy is terminated in the second half, it is called preterm labor.
If the pregnancy is terminated in the second half, it is called preterm labor.
Spontaneous abortion, otherwise known as miscarriage, is one of the most common complications during pregnancy, accounting for 10-20% of diagnosed pregnancies, and is the rejection of a fetus weighing no more than 500 grams. and less than 22 weeks. Unfortunately, with such indicators, the fetus is not viable. Usually 80% of the total number of spontaneous abortions occurs before the 12th week of pregnancy. nine0003
Types of spontaneous abortion
1. Threat of miscarriage - characterized by mild uterine cramps, pulling pain in the lower abdomen and sometimes mild bloody discharge from the vagina.
2. A miscarriage that has begun - is characterized by more severe pain and profuse bleeding. At the same time, the tone of the uterus is slightly increased, and the internal os is closed.
3. Inevitable miscarriage - accompanied by dilatation of the cervix - a fetal egg can be distinguished - with profuse bleeding and severe cramps in the lower abdomen. nine0003
nine0003
4. Incomplete miscarriage - part of the fetus comes out. The bleeding is so profuse that it can lead to the death of a woman.
5. Completed miscarriage - the fetal egg and the fetus itself are completely out. After that, the bleeding and spasms stop.
The etiology of miscarriage is due to many factors. Among them:
- genetic disorders;
- previous induced abortions;
- too little time has passed since the previous pregnancy; nine0003
- inflammatory infections in the mother, endocrine disorders;
- blood conflict between mother and fetus;
- taking hormonal contraceptives and certain medications;
- smoking during pregnancy and drinking alcohol;
- unknown causes.
To prevent miscarriage, it is necessary to give up bad habits, not to have abortions and to be regularly examined by a doctor.
Spontaneous abortion begins with the appearance of cramping, drawing pains, similar to pain during menstruation. Then bleeding from the uterus begins. At first, the discharge is slight or moderate, and then, after detachment of the fetal egg, abundant discharge with bloody clots begins. The appearance of these symptoms requires urgent hospitalization. nine0003
Then bleeding from the uterus begins. At first, the discharge is slight or moderate, and then, after detachment of the fetal egg, abundant discharge with bloody clots begins. The appearance of these symptoms requires urgent hospitalization. nine0003
After examining a woman in a hospital, having determined the degree of detachment of the embryo, one of the following diagnoses will be made:
- the threat of pregnancy - detachment is only outlined or is completely insignificant. In this case, the pregnancy can be saved;
- a miscarriage that has begun - detachment is already quite decent with a pronounced pain syndrome. And in this case, the fetus can be saved;
- abortion in progress - detachment with displacement progresses, labor-like contractions begin. Pregnancy cannot be saved, cleaning is required; nine0003
- incomplete miscarriage - independent exit of a part of the fetus and membranes, curettage is necessary for the final curettage of the uterus;
- late abortion - premature delivery of an unviable baby.
After a spontaneous abortion, it is recommended to take a short break in planning and take preventive measures to avoid recurrence.
In case of repeated miscarriage, a thorough comprehensive examination is necessary to determine the causes of miscarriage and eliminate them. nine0003
A miscarriage is a severe psychological trauma, especially during the first pregnancy. But do not give up, with a competent approach to planning and bearing, the next pregnancy will certainly end with the appearance of a long-awaited baby.
Causes of spontaneous abortion
1. Doctors call various chromosomal pathologies one of the main reasons: monosomy, autosomal trisomies, polyploidy. They account for 82-88% of spontaneous miscarriages.
2. The second most common cause is disorders in the female genital area: endometritis - inflammation of the uterine mucosa - preventing the implantation of the fetal egg and its development and polycystic ovaries. nine0003
3. Hormonal disorders, namely progesterone deficiency.
Hormonal disorders, namely progesterone deficiency.
4. Chronic diseases - uncontrolled diabetes mellitus, high blood pressure.
5. Viral infections rubella, chlamydia and others.
Treatment
In case of severe blood loss, ultrasound is performed to determine the viability of the fetus and rule out an ectopic pregnancy. A woman is prescribed bed rest and is treated with antispasmodic drugs to relax the uterine myometrium and stop bleeding. nine0003
If doctors still diagnose a spontaneous abortion that has begun, then the actions are reduced either to expectant tactics (within 2-6 weeks the fetal egg should come out by itself), or to prescribing drugs that accelerate the delivery of the fetus, or to vacuum aspiration (medical abortion ).
Blood clots during menstruation, why large blood clots can occur during menstruation, what to do
Contents
- Physiological causes
- Predisposing factors
- When do blood clots during menstruation indicate gynecological pathology?
Normal menstruation is the basis of a woman's reproductive health. The concept of the norm includes regular (every 21–35 days) painless menstruation, during which 40–150 ml of blood is released within 3–7 days. Menstrual flow has a dark red or brownish (at the end of the cycle) color and a uniform consistency. 1
The concept of the norm includes regular (every 21–35 days) painless menstruation, during which 40–150 ml of blood is released within 3–7 days. Menstrual flow has a dark red or brownish (at the end of the cycle) color and a uniform consistency. 1
Any deviation from the specified parameters should alert the woman. One of the most common concerns is blood clots during menstruation
PHYSIOLOGICAL CAUSES
Menstruation occurs after the egg produced by the female body has not been fertilized. The inner layer of the uterus (endometrium), where the embryo was supposed to be fixed, is rejected. Menstrual flow is thicker than normal blood, precisely due to the content of endometrial tissue in them. Why can blood clots form during menstruation in absolutely healthy women? The fact is that when walking and other active movements, menstruation comes out gradually and freely. However, after a night's sleep or sitting for a long time, a woman may notice the release of one or more jelly-like clots.:max_bytes(150000):strip_icc()/hemorrhage-in-miscarriage-meaning-2371523-FINAL-f2ab04cab1cc491e964a45e682f93da5.png) This happens because the blood lingers in the uterus and has time to clot. Also, the appearance of thickening contributes to a large amount of secretions. The alternation of heavy and scanty menstruation is characteristic of periods of hormonal changes (puberty, premenopause). nine0003
This happens because the blood lingers in the uterus and has time to clot. Also, the appearance of thickening contributes to a large amount of secretions. The alternation of heavy and scanty menstruation is characteristic of periods of hormonal changes (puberty, premenopause). nine0003
PREDISPOSING FACTORS
In order to understand why menstruation comes with blood clots, we list the possible causes of this process:
Hormone therapy, taking oral contraceptives. The appearance of such a side effect of drugs as increased menstrual bleeding is often observed with the independent use of drugs without consulting a gynecologist.
Hormone therapy, oral contraceptives. The appearance of such a side effect of drugs as increased menstrual bleeding is often observed with the independent use of drugs without consulting a gynecologist. nine0003
First menses after abortion or gynecological surgery.
Heavy periods may be the only symptom of early miscarriage. Elements of the fetal egg, which look like a small clot, can be detected by a woman, but more often go unnoticed.
WHEN DO THE BLOOD CLOTTS DURING THE TIME SAY ABOUT GYNECOLOGICAL PATHOLOGY?
The main pathological causes of this process are:
- Endometriosis is the growth of endometrial-like tissue outside the uterus. A variation of this disease is adenomyosis, in which the inner lining of the uterus grows into its muscle tissue. Both of these pathologies are accompanied by pain in the lower abdomen and heavy prolonged menstruation. If during menstruation a large blood clot came out, resembling a liver in appearance, then there is reason to suspect that the patient has one of these diseases. nine0082
- Polyps of the uterus - focal hyperplasia of the endometrium in the form of single or multiple formations on a wide base or on a stalk. One of the manifestations of the disease is an increase in the amount of menstrual flow. The appearance of large clots is especially often caused by a polyp, which is located on the cervix, as it prevents the timely release of secretions.
- Uterine fibroids. The growth of this benign tumor-like formation leads to the appearance of pain, as well as lengthening and intensification of menstrual bleeding. nine0082
In addition, the blood during menstruation may be released more slowly and thicken in some congenital pathologies. These include such anomalies in the structure of the female genital organs, such as a saddle, bicornuate or septate uterus.
WHAT TO DO IF THERE IS BLOOD CLOTS?
In case of any changes in the nature of menstruation (their frequency, duration, consistency, etc.), a woman should visit a gynecologist. In the event that large blood clots come out during menstruation, this must be done as quickly as possible. The doctor will interview the patient in detail, conduct a gynecological examination and prescribe the necessary laboratory and instrumental studies to the patient. After identifying the exact cause of the phenomenon, treatment of the underlying disease is prescribed, which led to the appearance of thickening of menstrual blood.