What can i take for a stuffy nose while pregnant
Which over-the-counter cold medications are safe during pregnancy? | Your Pregnancy Matters
Most people experience two to three colds during the winter and spring, and pregnant women are no exception. Colds are caused by viruses for which there is no real cure – you can treat the symptoms that make you feel crummy, but medicine doesn’t actually make the cold go away sooner.
Many over-the-counter (OTC) medications you can buy without a prescription come as multi-symptom formulas. These drugs are meant to treat every cold symptom: body aches, congestion, coughing, fever, headache, and sneezing. But not everyone develops every symptom of a cold, and pregnant women should avoid taking unnecessary drugs during pregnancy.
Instead of reaching for a multi-symptom drug, use the guidelines below to find an effective drug that’s safe for the symptoms you’re facing. And, as always, let your Ob/Gyn or nurse know about any OTC drug you take.
What to take for common cold symptoms
Cough
Dextromethorphan is a cough suppressant used in OTC medications such as Robitussin to reduce coughing. Cough suppressants can come in immediate-release and extended-release preparations. The maximum dose for pregnant women is 120 mg in 24 hours. The multi-symptom preparations that contain dextromethorphan often include “DM” in their name.
Guaifenesin is another medication frequently found in cough medications, such as Mucinex. It is an expectorant, so it helps thin mucus from your chest or throat so you can cough it up easier. It comes in immediate-release or extended-release formulations. The maximum dose you should take is 2,400 mg in 24 hours.
Cold medicines containing codeine were used in the past for cough suppression. I don’t recommend these for pregnant women because studies show they really don’t work well, and the fewer opioid-containing medications in our medicine cabinets, the better. For children, there is some evidence that honey can improve nighttime coughing. I certainly think this is an option for pregnant women as well. If you want to try honey, I suggest a spoonful of the real stuff – it’s not as clear that cold medicine with honey listed as a flavoring or ingredient is as effective.
Stuffy nose and sinus pressure
Decongestant medications reduce stuffiness and sinus pressure by constricting the blood vessels in your nose, which reduces swelling. Pseudoephedrine and phenylephrine are available over the counter as Sudafed and are safe for many women to use during pregnancy. However, women who have high blood pressure should not take pseudoephedrine without first talking to a doctor. The drug can raise blood pressure and can cause jitters and racing heartbeats.
Because pseudoephedrine can be used to manufacture methamphetamine, it’s now kept behind the pharmacy counter. You’ll have to provide identification to purchase it, and stores track how much you purchase. The maximum dose of a typical decongestant is 240 mg in 24 hours.
Sneezing, runny nose, and watery eyes
These symptoms are the result of histamine release, which is an immune response to an invading virus. Chlorpheniramine, such as Triaminic Allergy, and diphenhydramine, such as Benadryl, are safe to take during pregnancy. However, both can cause drowsiness, so these are best taken at bedtime. The maximum dosage for chlorpheniramine is 32 mg in 24 hours.
However, both can cause drowsiness, so these are best taken at bedtime. The maximum dosage for chlorpheniramine is 32 mg in 24 hours.
When compared to placebos, antihistamines have the most successful results within the first couple days of treatment. Patients didn’t report any relief of symptoms between days three and 10. Newer antihistamines, such as loratadine (Claritin), are approved for allergies, not colds, so there isn’t information about how well they work for cold symptoms.
Sore throat
Pregnant women can take acetaminophen (Tylenol) for a sore throat with a limit of 3,000 mg in 24 hours. An antihistamine may help if the sore throat is due to postnasal drip because it can dry up those secretions.
Sprays or lozenges that contain benzocaine, a local anesthetic, can help numb the throat. Menthol and phenol, such as Chloraseptic, are antiseptics that also help soothe throat discomfort. Sucking on hard candy can keep saliva flowing, which might reduce throat irritation.
A word about antibiotics
So many patients call asking for antibiotics for a cold, usually when they’ve had symptoms for several days. There are a few times when antibiotics are appropriate, for instance, strep throat or sinus infections caused by bacteria. But antibiotics simply don’t work against viruses that cause the common cold. Overprescribing antibiotics for viral illnesses leads to antibiotic resistance, which means the bacteria grow stronger over time and become tougher to beat with antibiotics.
If a doctor prescribes an antibiotic for cold symptoms, it’s usually a short, three-day round of drugs. The patient often feels better after finishing the medication but probably would have recovered in that timeframe anyway without the drug.
To sum up …
If you come down with a cold while pregnant and you want to take something for symptom relief, look for medications that are formulated for your specific symptoms. Avoid multi-symptom formulas, especially those containing acetaminophen. It can be easy to take more acetaminophen in a day than is safe because it’s in so many medications. Finally, be patient with cold symptoms – it can take a week or more for a cold to go away.
Avoid multi-symptom formulas, especially those containing acetaminophen. It can be easy to take more acetaminophen in a day than is safe because it’s in so many medications. Finally, be patient with cold symptoms – it can take a week or more for a cold to go away.
Sign up to receive Your Pregnancy Matters email alerts when we publish new stories.
Are decongestants safe during pregnancy?
Skip to main content
Allergies plague many of us every year. In fact, one in five adults suffers from allergies. Allergens are often called hay fever, or seasonal allergic rhinitis, and the most common symptoms are sneezing, stuffiness, a runny nose and itchiness in the mouth, throat, eyes or ears. Allergies often do not stop when women become pregnant; the question of whether the use of decongestants are safe during pregnancy is often an unclear answer to many women suffering from allergies.
Decongestants are medications that help shrink the blood vessels in the nasal membranes, allowing air passages to open. Congestion begins once blood vessels in the membrane of the nose and air passages become dilated, swollen or expanded. The membranes have a large capacity for expansion, which means they can have an abundant supply of blood vessels. This can allow the membranes to become engorged and cause congestion in the nose, sinuses or chest.
Congestion begins once blood vessels in the membrane of the nose and air passages become dilated, swollen or expanded. The membranes have a large capacity for expansion, which means they can have an abundant supply of blood vessels. This can allow the membranes to become engorged and cause congestion in the nose, sinuses or chest.
Over-the-counter decongestants are, for the most part, safe during pregnancy, physicians advise. Most decongestants do not contain enough medication to cause problems with baby, especially if used for short periods. Nasal spray decongestants are even safer since the medication is almost entirely absorbed within the nose and does not travel through the body. As a general rule, physicians advise patients if they can buy it without visiting the pharmacy counter, short-term use will not harm the baby during pregnancy.
Many health care providers recommend using medication that is considered a Category B drug, such as a decongestant or an antihistamine when allergies strike. Category B drugs have been shown through animal testing to not harm an unborn baby when the mother takes the medication during pregnancy. If a runny nose is more of a problem than a congested one, antihistamines such as diphenhydramine, loratadine or cetirizine are all safe to take during pregnancy.
Category B drugs have been shown through animal testing to not harm an unborn baby when the mother takes the medication during pregnancy. If a runny nose is more of a problem than a congested one, antihistamines such as diphenhydramine, loratadine or cetirizine are all safe to take during pregnancy.
However, there are also other health considerations when starting a new medication. As with any new medication, patients should discuss possible side effects with their health care provider, prior to taking it. Some decongestants, especially ones that contain pseudoephedrine, can cause elevations in blood pressure, so patients with chronic or pregnancy-induced high blood pressure should stay away from those medications. Other treatments that can help with nasal congestion include vapor rub, humidifiers (especially during dry winters) and saline nasal sprays. Physicians caution against using nasal pot during pregnancy, as the nasal flushing can strain an already weakened immune system.
The best solution is to avoid exposure to triggers in allergies, use over-the-counter nasal spray to ease nasal dryness, bleeding or congestion, include physical activity in a daily routine to reduce nasal inflammation, as well as trying over-the-counter nasal strips at night to keep nasal passages clear while sleeping.
Allergies can be uncomfortable and, often times, unbearable, and, although much of the advice regarding the use of decongestants while pregnant remains muddled, most doctors agree you should contact your individual physician before beginning the use of any medication that treats allergies. Only your physician will be able to assess individual risks and determine the safest decongestant or method of treatment to relieve allergy symptoms.
To find a Utica Park Clinic provider near you, please call 918-579-DOCS (3627) or click here.
Treatment of acute respiratory viral infections, acute respiratory infections and influenza in pregnant women in the clinic Health Territory
The first signs of acute respiratory viral infections - what should a future mother do?
How to help your body cope with illness, how not to harm the unborn child, and when serious professional help is needed? To help mothers, the specialists of our Center (obstetrician-gynecologist, midwives, homeopaths, ENT, naturopath and aromatherapist) offer an algorithm of actions that is consistent with all modern data from international recommendations.
But, most importantly, remember that an expectant mother, like no one else, is very important emotional mood - positive emotions will help you quickly cope with all the troubles.
Let's repeat, following our specialists: "Word and thought are material!".
- At the first sign of a cold (sore throat when swallowing, hoarseness or sore throat, runny nose, headache, body aches, weakness) - stay at home, keep a gentle regime, put on masks for all family members, remind everyone wash your hands more often.
- If it is impossible to get to a homeopath for the exact prescription of an individual remedy, you can take complex homeopathic remedies: "Ocillococcinum" once (!) Or homeopathic remedies "Agri" (according to the scheme in the instructions), "Influenza-Heel" (also according to the instructions).
- For pain in the throat, drugs - Tonsilotren, Tonsilgon or Angin-Heel will help. Necessarily - regular gargling with infusions of herbs (eucalyptus, calendula, chamomile) three to seven times a day.

- With a runny nose - "Corizalia" (with the first symptoms of a runny nose with strong discharge). You can use nose drops - hypertonic solutions of sea water, "Pinosol" (if there is no allergy). With nasal congestion - alkaline inhalation. If it helps you to breathe over boiled potatoes, then you can breathe.
- For coughs and colds, you can drink ginger tea - pour half a glass of grated ginger on a coarse grater to the top with good honey, insist for a day. Drink by adding 1-2 tsp. mixture per cup of hot water. Useful cranberry juice. With a dry cough, homeopathic preparations "Bronhalis-Heel" and "Tartefedrel" can be used.
- If hypothermia occurs and you feel chilly, drink hot tea with dried raspberries or raspberry jam. Chicken broth (strictly fresh) also helps.
- Aromatherapy will help not only to alleviate the symptoms, but also to cope with bacteria. Have an antiviral and antibacterial effect - noble laurel, peppermint, eucalyptus. Oils can and should be mixed (up to 8 drops per “portion”).
 To the above, you can add orange or lemon oil. And for evening-night spraying, add a soothing one to antiviral and microbial ones - lavender oil or tangerine oil. To treat a runny nose, cough, sore throat, you can prepare the following mixture: 4 tablespoons of peach oil (used as a base), 1 drop of lavender, 2 drops of eucalyptus, 1 drop of tea tree. This mixture is instilled into the nose 1-2 drops after washing the nose with a sea water spray.
To the above, you can add orange or lemon oil. And for evening-night spraying, add a soothing one to antiviral and microbial ones - lavender oil or tangerine oil. To treat a runny nose, cough, sore throat, you can prepare the following mixture: 4 tablespoons of peach oil (used as a base), 1 drop of lavender, 2 drops of eucalyptus, 1 drop of tea tree. This mixture is instilled into the nose 1-2 drops after washing the nose with a sea water spray. - Motor mode (at the first sign - stay at home, but if you feel well, do not refuse a short walk in nature, in the park (not in the mall!).
- Mood. To improve your mood, you can hang garlands of Christmas trees (a variant of natural aromatherapy), pine twigs, cones. Let the sun into the house - light candles, and put bright fruits in places you can see - in the bedroom, for example - oranges, lemons, grapefruits, pomelo (again, natural aromatherapy) or pineapples - any favorite fruit. To wake up in the morning and immediately see a lot of bright “suns” by the bed, which accumulated all this joyful energy for us.
 ”
” - And most importantly - be sure to tell your doctor about your health! The doctor will recommend you what is especially important for you.
- “If the temperature does not exceed 38.5, do not take antipyretics. If you have a very high temperature, severe weakness, bad breath, severe cough and any deviation from the course of a common cold, and if there is no improvement within THREE DAYS, be sure to consult a doctor "(chief physician of the Health Territory, obstetrician-gynecologist Alexander Sergeevich Gavrilenko).
For help in preparing the material, we thank the obstetrician-gynecologist of the Health Territory Irina Stepanovna Arefyeva.
Additions and recommendations of our specialists:
- Elena Lvovna Ten, ENT, homeopath.
“If the cold has penetrated deeply, then there is a watery coryza or sore throat, and then a cough. Then you can drip into the nose "Derinat" (not contraindicated for pregnant women, but recommended after consultation with a doctor) or "Pinosol". Gargle with calendula, and I also recommend gargling with NATURAL (!) apple cider vinegar (2 teaspoons per glass of water) 3-4 r / d. it is necessary to treat the whole body, to understand the cause of the cough! Is it just from hypothermia? Then it will pass quickly. But, if there is a “weak link” in the respiratory (lungs) or genitourinary (kidneys) systems, or there may be a problem in the intestines, then the treatment must be comprehensive.
Gargle with calendula, and I also recommend gargling with NATURAL (!) apple cider vinegar (2 teaspoons per glass of water) 3-4 r / d. it is necessary to treat the whole body, to understand the cause of the cough! Is it just from hypothermia? Then it will pass quickly. But, if there is a “weak link” in the respiratory (lungs) or genitourinary (kidneys) systems, or there may be a problem in the intestines, then the treatment must be comprehensive.
- Olga Bannikova, obstetrician.
“You can turn on the aroma lamp for a long time (for the whole night, for example). But if you are not sure about the body's response, try turning it on for 2 hours, then wait a few hours and turn it on for another 2 hours. It is better to use ultrasonic aroma lamps (they are more efficient and, unlike those heated by a candle, are designed for a large area of application - 20-30 sq.m)”.
- Yulia Krushanova, microbiologist, Ph.D., specialist in medical aromatherapy and Ayurveda:
“You can prepare a universal solution for an aroma lamp: 5 ml of alcohol, 200 ml of water and 10 drops of a mixture of oils: coniferous oils, oils of lemon, leuzea, bergamot, grapefruit. This aroma mixture is good for both prevention and treatment. There is some correction for oils for the aroma lamp: you can’t evaporate thyme in the lamp (too active oil, can give bronchospasm), the aroma of orange increases appetite (it would be better to use lemon, grapefruit, bergamot), leuzea oil can only be used cold (that is, without heating in an aroma lamp with candles). In general, cold water sprays are preferable to heating, since when heated in an aroma lamp, some components of essential oils undergo changes and are destroyed, without having a beneficial effect. For the same reason, an ultrasonic aroma lamp is preferable to an aroma lamp heated by candles. It is very important that the aroma lamp heated by candles does not run out of water in the bowl, since it is clear that the oil should not burn, it should evaporate from the surface of the water.
This aroma mixture is good for both prevention and treatment. There is some correction for oils for the aroma lamp: you can’t evaporate thyme in the lamp (too active oil, can give bronchospasm), the aroma of orange increases appetite (it would be better to use lemon, grapefruit, bergamot), leuzea oil can only be used cold (that is, without heating in an aroma lamp with candles). In general, cold water sprays are preferable to heating, since when heated in an aroma lamp, some components of essential oils undergo changes and are destroyed, without having a beneficial effect. For the same reason, an ultrasonic aroma lamp is preferable to an aroma lamp heated by candles. It is very important that the aroma lamp heated by candles does not run out of water in the bowl, since it is clear that the oil should not burn, it should evaporate from the surface of the water.
- Laima Lankmane, naturopath and herbalist:
“It is especially important for a pregnant woman to carefully read all the instructions for herbal preparations - first of all, this applies to the first trimester, when the body of the expectant mother is extremely sensitive to everything and undergoes a strong hormonal restructuring. But even during the entire pregnancy, one should be careful with herbal remedies and it is better to consult with your doctor before use. With hypothermia, the first signs of the disease, you can - ginger with lemon, honey (better bite, because when heated above 40-50 degrees, it not only loses many of its nutritional properties, but can also harm a sensitive stomach), green teas and all natural drinks with a lot of vitamin C (for example, rosehip broth helps well). Leaves of linden and dry raspberries - yes, but raspberry jam (unless, of course, it is a frozen berry) will not bring much benefit. Unfortunately, during prolonged cooking, berries lose many of their antibacterial and phyto-properties. In addition, in the jam, in addition to the taste “from childhood”, there is a lot of excess sugar that you don’t need now. However, if a cup of tea with a spoonful of such jam lifts your mood and spirit, then definitely this is a medicine! And do not forget that the word and thought are material!” Source: Bone, K.
But even during the entire pregnancy, one should be careful with herbal remedies and it is better to consult with your doctor before use. With hypothermia, the first signs of the disease, you can - ginger with lemon, honey (better bite, because when heated above 40-50 degrees, it not only loses many of its nutritional properties, but can also harm a sensitive stomach), green teas and all natural drinks with a lot of vitamin C (for example, rosehip broth helps well). Leaves of linden and dry raspberries - yes, but raspberry jam (unless, of course, it is a frozen berry) will not bring much benefit. Unfortunately, during prolonged cooking, berries lose many of their antibacterial and phyto-properties. In addition, in the jam, in addition to the taste “from childhood”, there is a lot of excess sugar that you don’t need now. However, if a cup of tea with a spoonful of such jam lifts your mood and spirit, then definitely this is a medicine! And do not forget that the word and thought are material!” Source: Bone, K. (2003), A Clinical Guide to Blending Liquid Herbs, Churchill Livingstone, USA
(2003), A Clinical Guide to Blending Liquid Herbs, Churchill Livingstone, USA
Health Territory doctors will always be happy to answer your questions! 8 (495) 988 52 52
Prolonged nasal congestion (rhinitis) in pregnant women
Article rating
3.62 (Votes: 13)
Contents
- Causes of prolonged nasal congestion and rhinitis in pregnant women
- The frequency of occurrence of rhinitis of pregnant women
- What are we afraid of in pregnancy rhinitis?
- What to do if you are pregnant and you are suffering from a persistent runny nose and nasal congestion?
One of the most common distressing problems of pregnant women is rhinitis of pregnancy (swelling of the nasal mucosa, accompanied by difficulty in nasal breathing, in some cases with increased mucus production or without it).
Causes of chronic nasal congestion and rhinitis in pregnant women
- Increased hormonal levels of progesterone, estrogen.
- Emotional stress (which is pregnancy itself)
- An increase in the volume of circulating blood, which increases blood filling, including the lower nasal conchas.
- Gastroesophageal reflux - reflux of acidic contents of the stomach into the esophagus and nasopharynx due to an increase in the volume of the uterus (change in acidity causes the development of swelling of the nasal mucosa.)
Frequency of occurrence of rhinitis in pregnant women
The incidence of rhinitis during pregnancy is very high, every fifth pregnant woman experiences more or less pronounced symptoms of prolonged (more than 6 weeks) nasal congestion, which can develop at any period of pregnancy, but most often in the II-III trimesters of pregnancy (from 12 38 weeks), which is understandable, based on the listed reasons for its occurrence.
A feature of rhinitis of pregnancy is that its symptoms completely disappear 2 weeks after delivery.
What are we afraid of in pregnancy rhinitis?
Despite the fact that prolonged nasal congestion and rhinitis in pregnant women accompanies a large number of women, unfortunately, if left unattended, these symptoms can lead to serious complications:
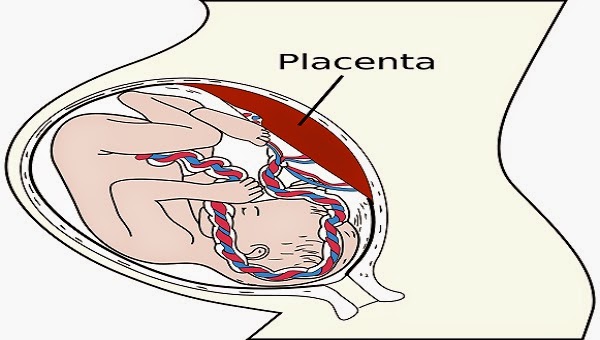
- First, it is very easy to get naphthyzinum if a woman independently and uncontrollably uses vasoconstrictor drops, and this is highly undesirable during pregnancy, since the part of the drug that enters the bloodstream causes vasoconstriction and the entire vascular system and internal organs, including placental vessels, especially this it is dangerous if a pregnant woman has high blood pressure and a rapid heartbeat, these indicators may worsen while taking drops.
- Secondly: against the background of a pronounced prolonged edema and blockage of the fistulas of the paranasal sinuses, with hypothermia or contact with an infection, it is possible to develop inflammation in the sinuses: sinusitis, sinusitis, frontal sinusitis, which will entail serious treatment, antibiotic therapy and infectious intoxication of the mother and fetus.

- Thirdly: prolonged obstruction of nasal breathing naturally entails the formation of moderate hypoxia (lack of oxygen in the blood) from which both the woman herself suffers (headaches, fatigue, mood depression) and the fetus.
What to do if you are pregnant and you suffer from persistent runny nose and nasal congestion?
Be sure to contact a specialized ENT clinic or an ENT office, an otorhinolaryngologist, who, first of all, will conduct a safe and permitted diagnosis during pregnancy.
For example, in the ENT clinic plus 1, you will have an endoscopy of the ENT organs, including the deep sections of the nose and nasopharynx; to exclude inflammation of the paranasal sinuses, an ultrasound of the paranasal sinuses will be done; if necessary, laboratory diagnostic methods will be carried out. All these methods are absolutely painless, do not require any preparation and have no contraindications at any stage of pregnancy.
After making a diagnosis and prescribing (if necessary) drug therapy, you will be offered methods of hardware treatment, which are also allowed at any stage of pregnancy and are highly effective in removing blockage of nasal breathing: UZOL-therapy, photochromotherapy.