Pelvic floor after pregnancy
Female Pelvic Medicine and Reconstructive Surgery
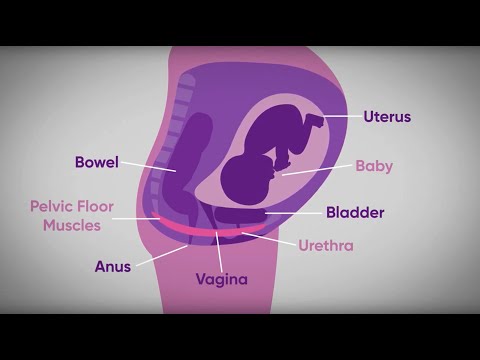
What Happens to Your Pelvic Floor After Childbirth: The Woman’s Center : Female Pelvic Medicine and Reconstructive SurgeryThe female pelvic system is a complex network of muscles and nerves, so it’s hardly surprising that giving birth can have lasting effects on the body. Luckily, as the field of urogynecology grows, doctors are better able to understand just how the pelvic system is impacted by pregnancy and childbirth, and how to help women who have sustained injuries as a result.
Here are several important things to know about childbirth injury, their causes, their symptoms, and how they can be treated.
Vaginal deliveries can result in damage to key muscles.
The levator ani muscle serves two major functions in the female body: supporting the vagina and pelvic organs and maintaining urinary and bowel continence. As a woman enters her third trimester and prepares for birth, these muscles become strained to support the baby’s growth and delivery. More than 30% of women who give birth vaginally will experience pelvic trauma that causes damage to this muscle group.
Vaginal delivery can also increase the risk of pelvic organ prolapse.
The levator ani is also responsible for supporting pelvic organs, so if those muscles and nerves are damaged, the uterus and vaginal walls may begin to collapse into the vaginal canal. According to the Women’s Health Foundation, there are quite a few risk factors that can also increase the likelihood of levator ani damage, such as:
- Delivery time (pushing more than 90 minutes can increase risk of damage)
- Large birth weight
- Forcep and vacuum deliveries
- Age of the mother
- Previous pelvic surgery
- Poor diet
- Smoking
Emptying disorders are also a common result of childbirth and pelvic injury.
Since the muscles that are responsible for controlling bladder and bowel urges can be damaged by pregnancy, women are likely to experience incontinence after giving birth. One study in Oregon found that 1 in 4 women experience involuntary passage of gas and bowel leakage within six months of childbirth. In addition, urinary incontinence can start during the third trimester and persist for months. If you or a loved one has experienced involuntary bowel leakage or urinary incontinence for more than three to six months after giving birth, it might be time to see a doctor and evaluate treatments, such as physical therapy or surgery.
One study in Oregon found that 1 in 4 women experience involuntary passage of gas and bowel leakage within six months of childbirth. In addition, urinary incontinence can start during the third trimester and persist for months. If you or a loved one has experienced involuntary bowel leakage or urinary incontinence for more than three to six months after giving birth, it might be time to see a doctor and evaluate treatments, such as physical therapy or surgery.
Most postpartum symptoms resolve themselves.
According to the Women’s Health Foundation, 70% of U.S. women who’ve just given birth find that certain symptoms of childbirth (like urinary incontinence and accidental bowel leakage) go away after a few months.
Physical therapy and pelvic floor exercise are crucial to preventing — and healing from — injury.
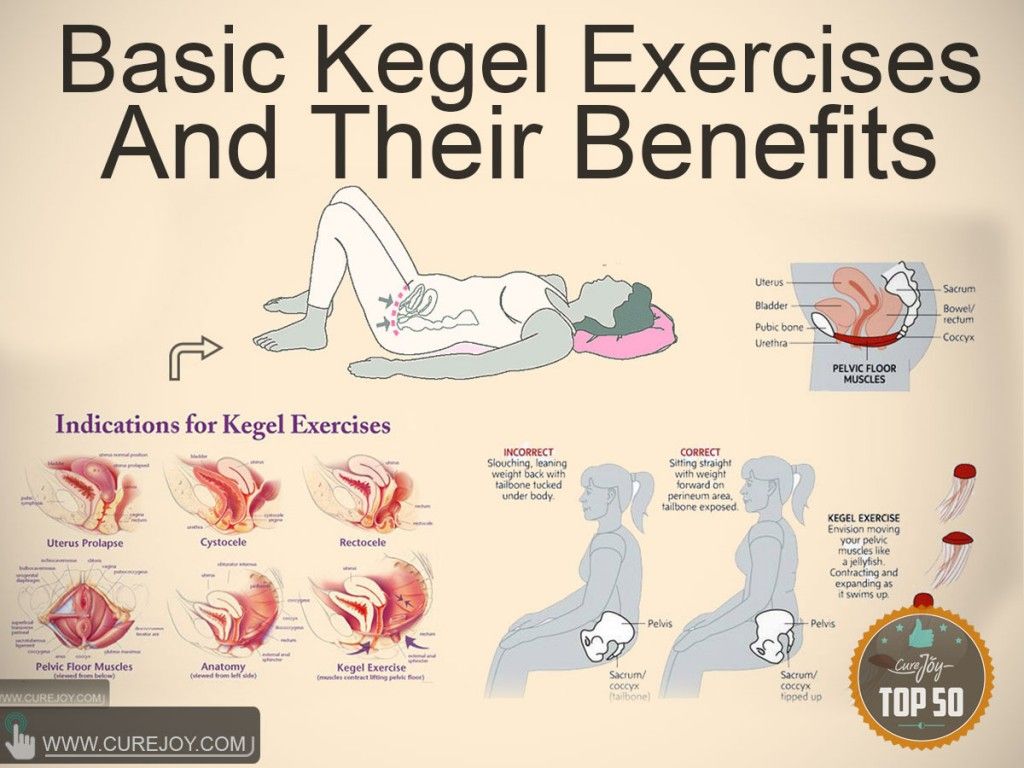
Pelvic floor exercises during and after pregnancy and physical therapy can help mitigate the stress that pregnancy and delivery places on the body. In one study, women who received pelvic floor therapy during their third trimester and after giving birth were less likely to report urinary incontinence. Doctors universally agree that Kegel exercises are vital to keep the pelvic floor muscles strong during and after pregnancy, and more comprehensive treatment can be given by a physical therapist.
In one study, women who received pelvic floor therapy during their third trimester and after giving birth were less likely to report urinary incontinence. Doctors universally agree that Kegel exercises are vital to keep the pelvic floor muscles strong during and after pregnancy, and more comprehensive treatment can be given by a physical therapist.
Surgery is often necessary to correct pelvic floor damage.
Every year, nearly 400,000 women in the U.S. undergo surgery for urinary incontinence or pelvic organ prolapse. It’s important to follow up with your doctors after the birth to assess any damages done to the pelvic floor and surrounding muscles. It might be necessary to seek corrective surgery to ensure that your body recovers from the strain of pregnancy and birth.
Dr. Ryan Stratford is board-certified in Female Pelvic Medicine and Reconstructive Surgery (FPMRS) as well as Obstetrics and Gynecology (Ob/Gyn) with a wealth of clinical and research experience.
You Might Also Enjoy...
Kegel Exercises: Benefits, Instructions, and Helpful Tips
Pelvic floor exercises, also called Kegel (kay-gull) exercises after Dr. Arnold Kegel who developed them, strengthen the pelvic floor muscles. These muscles play a role in supporting the bladder ad urethra.
Treatment Options For Overactive Bladder (OAB)
Is your daily schedule controlled by your bladder? Do you know where every single bathroom is within a 20-mile radius of your home? If you answered yes to either of these questions, you may have symptoms of overactive bladder (OAB).
Your post-pregnancy body - NHS
Having a baby changes your body. Here’s some advice to help you feel comfortable with your body.
Physical problems after pregnancy
There may be physical problems after having a baby.
They can be related to pregnancy or birth, or the things you do while caring for young children, such as lifting and bending.
For some problems, you can do a lot to help yourself. For example, if you have a leaky bladder (incontinence) or a heavy feeling between your vagina and anus, you may need to strengthen the muscles around your bladder by doing pelvic floor exercises.
Also, if you have back pain, you may need to learn how to look after your back and do some exercises to strengthen it.
If a physical problem is bothering you, ask a GP or health visitor for help at any time. They can advise you and the GP can refer you to a specialist if necessary.
Your postnatal check
Your postnatal check at around 6 to 8 weeks after the birth of your baby is a good time to talk to the GP about any physical or mental health problems you've had since the birth.
Find out more about what happens at your postnatal check.
Separated stomach muscles
It's common for the 2 muscles that run down the middle of your stomach to separate during pregnancy. This is called diastasis recti, or divarication.
The amount of separation can vary. It happens because your growing womb (uterus) pushes the muscles apart, making them longer and weaker.
The separation between your stomach muscles will usually go back to normal by the time your baby is 8 weeks old.
After you have had your baby, you can check the size of the separation with this simple technique:
- Lie on your back with your legs bent and your feet flat on the floor.
- Raise your shoulders off the floor slightly and look down at your tummy.
- Using the tips of your fingers, feel between the edges of the muscles, above and below your belly button.
 See how many fingers you can fit into the gap between your muscles.
See how many fingers you can fit into the gap between your muscles.
Do this regularly to check that the gap is gradually getting smaller.
If the gap is still obvious 8 weeks after the birth, contact the GP as you may be at risk of back problems. The GP can refer you to a physiotherapist, who will give you some specific exercises to do.
Regular pelvic floor and deep stomach muscle exercises can help to reduce the size of the separation between your stomach muscles. It's also important to stand up tall and be aware of your posture.
Pelvic floor muscle exercises
Pelvic floor muscle exercises strengthen the muscles around your bladder, vagina and bottom. This can help to stop incontinence, improve prolapse and make sex better too.
You can do these exercises lying down, sitting or standing. With practice, they can be done anywhere and at any time:
With practice, they can be done anywhere and at any time:
- Squeeze and draw in your bottom as if you're holding in wind.
- Squeeze around your vagina and bladder (urethra) as if you're stopping the flow of urine or squeezing during intercourse.
- Long squeezes – hold for as long as you can, but no longer than 10 seconds, then relax.
- Short squeezes – quickly squeeze the muscles and then let them go immediately. Do this until your muscles get tired.
Aim to build up to 10 repeats of each exercise, at least 3 times a day.
It's important to keep breathing normally while you do these exercises. Make sure you don't pull in your stomach when you squeeze.
Sitting on the toilet can be a good reminder to do your exercises. Just make sure you do them after you've finished.
Visit the Chartered Society of Physiotherapists website for more tips to strengthen your pelvic floor.
Stomach exercise
This exercise can help you tone your stomach muscles:
- Lie on your side with your knees slightly bent.
- Let your tummy relax and breathe in gently.
- As you breathe out, gently draw in the lower part of your stomach like a corset, narrowing your waistline.
- Squeeze your pelvic floor muscles at the same time.
- Hold for a count of 10, breathing normally, then gently release.
Repeat up to 10 times.
Ways to ease back pain
These practical tips may help to relieve an aching back:
- while feeding your baby, sit with your back well supported and straight. Put a small pillow or cushion behind your waist to support your lower back.
 Make sure your feet can reach the floor
Make sure your feet can reach the floor - kneel or squat (do not bend your back) to do tasks that are near the floor, such as picking up toys or bathing your baby
- change a nappy on a raised surface. You could kneel on the floor next to a sofa or bed. Never leave your baby unattended on a raised surface, in case they fall off
- keep your back straight and bend your knees when lifting
- Keep your back straight when you push your pram or buggy. Or, carry your baby in a well-fitting sling
More on your wellbeing after birth:
- Coping with stress after having a baby
- Keeping fit and healthy after a baby
- Managing sleep and tiredness
Page last reviewed: 22 October 2019
Next review due: 22 October 2022
Sex after childbirth: training intimate muscles
These muscles are often referred to as the intimate muscles. Well-developed pelvic floor muscles are the key to sexual pleasure: their volume and tone affect the degree of closure of the genital gap and, accordingly, the strength of arousal and orgasm. But very often after pregnancy and childbirth, these muscles weaken and lose their tone. Why is this happening?
Well-developed pelvic floor muscles are the key to sexual pleasure: their volume and tone affect the degree of closure of the genital gap and, accordingly, the strength of arousal and orgasm. But very often after pregnancy and childbirth, these muscles weaken and lose their tone. Why is this happening?
NO MOTION
“Almost half of women leave the maternity hospital with weakness of the pelvic floor muscles (and even more if it is a repeated birth), says gynecologist Elena Silantyeva. - After all, the muscles of the pelvic floor, like all striated muscles, develop only in work, in active movement. But what kind of life do we lead? Most often - sedentary, which is why the muscles are inactive and atrophy. And during childbirth, when the birth canal is stretched, these flaccid muscles are more quickly stretched and injured. For this reason, a woman may experience a syndrome of "wide vagina" (vaginal relaxation). An infection easily penetrates into a wide open genital slit, thrush, colpitis or vaginitis may develop.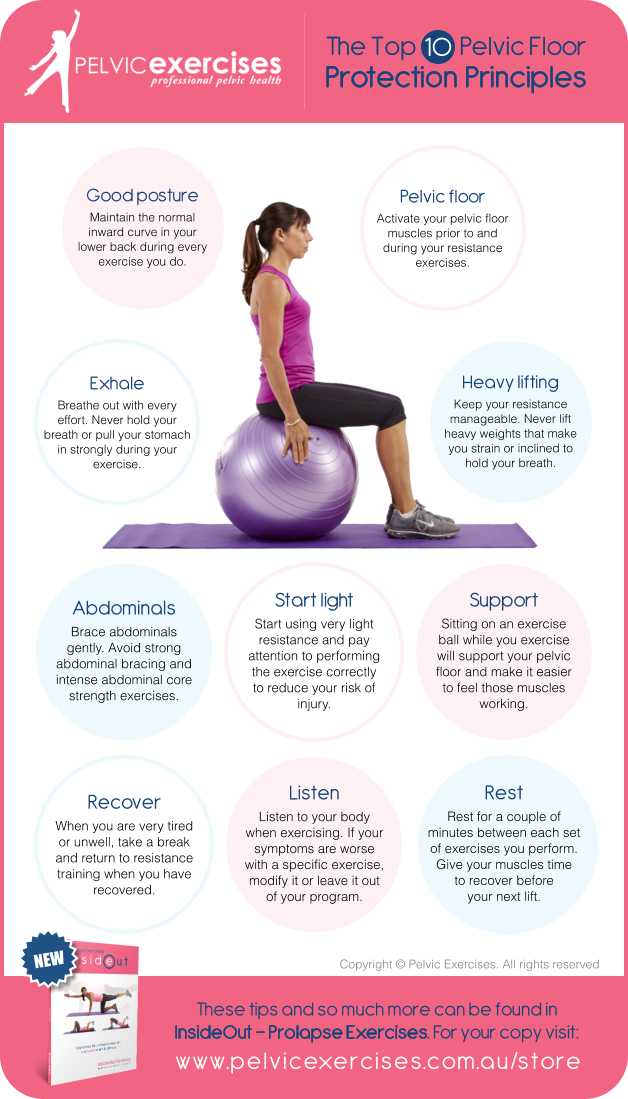 And close contact of the vaginal mucosa with linen leads to its drying and partial atrophy. It is not surprising that the sensitivity of the mucosa as an erogenous zone is reduced. Moreover: during the love act, there is no tight fit of the partner's penis to the inner walls of the vagina. And as a result, not only the woman herself ceases to feel any pleasure during contact, but also the man (especially the elderly one): after all, the strength of his erection largely depends on the degree of fit.
And close contact of the vaginal mucosa with linen leads to its drying and partial atrophy. It is not surprising that the sensitivity of the mucosa as an erogenous zone is reduced. Moreover: during the love act, there is no tight fit of the partner's penis to the inner walls of the vagina. And as a result, not only the woman herself ceases to feel any pleasure during contact, but also the man (especially the elderly one): after all, the strength of his erection largely depends on the degree of fit.
HEALING ORGASM
Weak sensitivity of erogenous zones leads to another serious problem: a woman may experience a pronounced sexual desire, but cannot get an orgasm. And it's pretty bad for her reproductive system. After all, an orgasm not only gives pleasure and provides emotional release, but also supports women's health. “Orgasm causes an instant spasm of the smallest vessels of the arterial bed, blood renewal, an increase in the tone of the venous system,” explains Elena Silantyeva. - If discharge does not occur, then the outflow of venous blood slows down and congestion develops in the vessels of the small pelvis, which manifest themselves later in various painful sensations. And gynecologists treat these pains with antibiotics, which in turn destroy the microflora of the vagina, and a more serious infection enters the body. Actually, this is another reason to establish a harmonious sex life.
- If discharge does not occur, then the outflow of venous blood slows down and congestion develops in the vessels of the small pelvis, which manifest themselves later in various painful sensations. And gynecologists treat these pains with antibiotics, which in turn destroy the microflora of the vagina, and a more serious infection enters the body. Actually, this is another reason to establish a harmonious sex life.
INTIMATE MUSCLES TRAINERS
What should a woman do if her pelvic floor muscles have weakened after childbirth and “wide vagina” syndrome has developed? Elena Silantieva offers several methods.
- Physiotherapy. First of all, immediately after childbirth, in the first day or two, a woman needs restorative treatment using classical types of physiotherapy - a magnetic field, UHF and others that reduce inflammation and quickly heal damaged, stretched muscle tissue.
- Physical exercise. As soon as the muscles have healed (not earlier than a month after the birth), you can gradually start working with them.
 But when exactly - only the doctor decides. Any physical activity that has no contraindications is welcome. But Pilates, yoga, and physiotherapy exercises, which were so popular in Soviet times, are especially useful - these complexes usually include exercises that at least indirectly involve the muscles of the pelvic floor.
But when exactly - only the doctor decides. Any physical activity that has no contraindications is welcome. But Pilates, yoga, and physiotherapy exercises, which were so popular in Soviet times, are especially useful - these complexes usually include exercises that at least indirectly involve the muscles of the pelvic floor.
- biofeedback therapy. This is a hardware-computer complex, with the help of which women learn to do Kegel exercises, specially designed for training intimate muscles. Of course, these exercises can be done at home, but it is very important to master the correct technique under the supervision of a specialist, because women often confuse muscles and pump the wrong thing at all. If the muscles have not worked for many years, how can you know how these muscles feel, how to put them into work? For this, BOS-therapy is needed. What is its essence? An individual electrode is inserted into the vagina.
 And when the woman tenses and relaxes the corresponding muscles, the electrode receives an electrical impulse from them, and the data is displayed on the computer screen. If a woman does not relax her muscles well or by mistake uses the muscles of the anterior abdominal wall, the doctor, looking at the screen, coordinates her work, gradually changing and complicating the task. For 15-20 sessions, you can develop a stable skill in order to continue to practice at home on your own. As a result of such exercises, the volume, strength, endurance of intimate muscles, their ability to relax and stretch increases. There is nothing surprising and mysterious in this: just as a man in the gym, pumping up his biceps, increases their volume, so a woman can double - and this is easily confirmed by ultrasound diagnostics - the volume of her levators (those muscles that lie around the entrance to the vagina) . The genital gap closes and becomes tight, the sensitivity of the erogenous zones is restored.
And when the woman tenses and relaxes the corresponding muscles, the electrode receives an electrical impulse from them, and the data is displayed on the computer screen. If a woman does not relax her muscles well or by mistake uses the muscles of the anterior abdominal wall, the doctor, looking at the screen, coordinates her work, gradually changing and complicating the task. For 15-20 sessions, you can develop a stable skill in order to continue to practice at home on your own. As a result of such exercises, the volume, strength, endurance of intimate muscles, their ability to relax and stretch increases. There is nothing surprising and mysterious in this: just as a man in the gym, pumping up his biceps, increases their volume, so a woman can double - and this is easily confirmed by ultrasound diagnostics - the volume of her levators (those muscles that lie around the entrance to the vagina) . The genital gap closes and becomes tight, the sensitivity of the erogenous zones is restored.
- Laser vulvo-vaginal rejuvenation and intimate cosmetology (plasma therapy and mesotherapy) are modern technologies that involve laser exposure or intradermal injections in the intimate area. They are designed to improve the quality of the mucosa of the external genital organs (and, if desired, change their aesthetic characteristics), improve their flora, and increase the sensitivity of erogenous zones.
Questionnaires conducted by physicians after these procedures have shown that women experience more intense sensations during sex as a result, more satisfaction at the moment of orgasm, and the orgasmic discharge itself occurs more often than before.
Intimate vaginal reconstruction after pregnancy and childbirth
Intimate vaginal reconstruction after pregnancy and childbirth
- Description
- Video
- Organization of treatment
- Cost of treatment
Description
The birth of a child is one of the most significant and long-awaited events in a woman's life. Unfortunately, sometimes some physiological changes occur in the mother's body, which reduce the quality of life, causing a number of complaints and functional disorders. One of these problems is postpartum changes in the pelvic floor, or, more simply, the prolapse of the walls of the vagina.
Unfortunately, sometimes some physiological changes occur in the mother's body, which reduce the quality of life, causing a number of complaints and functional disorders. One of these problems is postpartum changes in the pelvic floor, or, more simply, the prolapse of the walls of the vagina.
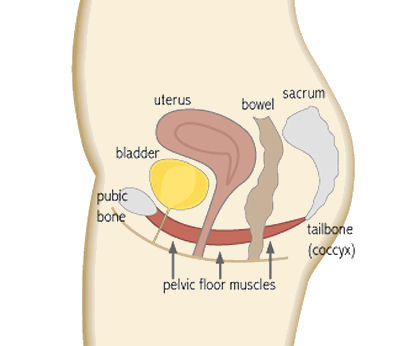
The pelvic floor is a complex muscular-connective-tissue structure, which, on the one hand, must effectively resist intra-abdominal pressure, close the lumen of the tubular urethra, rectum and, partly, the vagina, and, on the other hand, determine the correct anatomical position of all pelvic organs, without which it is impossible to correct functioning. At the same time, muscles and fascia act in a well-played duet (they are even anatomically connected to each other) and it is impossible to clearly say which structure contributes more (see Fig. 1).
1).
Fig. 1. Pelvic floor anatomy
Causes
During pregnancy and childbirth, both components of the pelvic floor are damaged to varying degrees. It is customary to distinguish two groups of factors leading to pathology.
- The first is predisposing factors. This is, first of all, a genetic predisposition, i.e. features of genes encoding the composition and properties of connective and muscle tissue in women. Someone recovers after childbirth easily and fully, someone takes a long time and not fully.
- The second group is provoking factors. This is, first of all, how the birth goes, how correctly the process is managed both by the staff and by the woman in labor: the duration of the head standing, the timeliness of the episiotomy, the fullness of the restoration of the perineum, etc.
Diagnosis
| Types of pelvic floor defects are very different: from complete eversion of the vagina (eversion) to a uniform moderate increase in the size of all structures (“relaxed vagina”). These injuries significantly increase the volume of the vagina and expand the entrance, which leads to a characteristic set of complaints: loss of the sensation of "girth" during sexual activity, deterioration in sensitivity, air and water entering the vagina, difficulty emptying the rectum (up to the need for manual assistance), incontinence of gases. Diagnosis usually does not cause any particular problems. Inspection by a qualified person is sufficient (See Fig. 2.) | Fig. 2. Click the picture to view |
Intimate plastic surgery for women after pregnancy and childbirth
Considering that the problem of vaginal prolapse after pregnancy and childbirth is quite widespread, there are a lot of “suggestions” for its “simple” solution on the medical services market, as, unfortunately, there are many frankly poorly trained professionals offering their services.
Most technologies are really “simple” and designed for a very mediocre doctor rather than truly effective. However, they are often overpriced.
Start talking about treatment should be with the training of the pelvic floor muscles ( TMTD ). This approach, when performed correctly under the guidance of an instructor (!) , is in any case very effective in restoring muscle tone, improving blood supply and sensitivity, the ability to compress the vaginal lumen with an arbitrary effort, and improve the function of continence of urine and rectal contents.
In our clinic, two specialists - Martyanova Alexandra Alexandrovna and Staroseltseva Olga Yurievna can consult on the subject of TMTD . At the same time, a hardware approach based on biofeedback (BFB-therapy) is also widely used.
However, it was said above that most often in women after childbirth there is an anatomical defect in the tendon body of the perineum and the posterior wall of the vagina (specifically, the rectovaginal fascia that separates the rectum from the vagina). In principle, it is impossible to eliminate this defect solely by training the muscles of the pelvic floor.
In principle, it is impossible to eliminate this defect solely by training the muscles of the pelvic floor.
Here we can talk about two fashionable and "simple and less traumatic" technologies that are designed to reduce the lumen and narrow the entrance to the vagina.
- First of all, these are various technologies of thread plastics of the entrance, when with the help of special self-fixing threads “without cuts” the tissues in the perineal area are brought together and a visual effect of narrowing is achieved.
- The second approach is the introduction of hyaluronic acid derivatives under the vaginal mucosa, the so-called. fillers (including “G-spot augmentation”, etc.).
Undoubtedly, these approaches will find their fans both among physicians, especially among those who do not have experience in reconstructive pelvic floor surgery, and among patients who strive for a minimally invasive procedure.
The cosmetic, superficial nature of the above interventions and the likely lack of long-term effectiveness are obvious to any professional.At least, there is no evidence for these approaches in the serious literature.
Laser "rejuvenation" of the vagina, which was offered a few years ago as a panacea for the "relaxed" vagina syndrome, not only did not fully justify itself, but also caused a whole range of side effects if used incorrectly. There are even FDA warnings about this in the US.
Extended subfascial colpoperineoplasty (vaginal and perineal plasty)
| In our opinion, a full-fledged extended subfascial colpoperineoplasty, provided that it is performed correctly, remains the most effective approach in restoring the pelvic floor after childbirth. However, we have always been dissatisfied with the “classical” approach in this field, professed by most gynecologists, when the vagina is reconstructed essentially only at the entrance, where a characteristic “curtain” or “pocket” is created, and the back wall remains almost unchanged or is reconstructed to a depth of 2-3 cm, while sutures are often applied to the "levators", that is, to fragments of the muscle that lifts the anus, which often leads to prolonged pain and even dyspareunia (refusal of sexual activity). Women very often ask to cut through the “terrible” partition at the entrance (Fig. 3), which not only prevents a normal sexual life, but also leads to an extremely unpleasant side effect when, during urination, urine partially enters the “ pocket", and after getting up from the toilet, it flows out of the vagina. | Fig. 3. The forceps are immersed in the "pocket" created earlier during the "classic" posterior colporrhaphy (intraoperative photo) To view, click on the picture |
Based on the above and having experience of more than 5 thousand reconstructive operations on the pelvic floor, by the beginning of 2018, we had developed an original technology for the physiological reconstruction of the rectovaginal fascia and perineum. The method was based on single thread subfascial colporrhaphy, which migrated from the well-established hybrid technique for pelvic floor reconstruction, first applied in 2015.
| In the new technology, thanks to the use of a number of know-how, an approach has been developed in which it is possible to restore the posterior wall of the vagina along the entire functional extent, as well as the structures of the urogenital diaphragm and the tendon center of the perineum, with a single long-term absorbable thread (Fig. 4.). | Fig. 4. Stages of extended subfascial colpoperineoplasty . Click on the picture to view |
| At the same time, the entrance to the vagina is completely devoid of all kinds of pockets, the vagina is narrowed evenly throughout, and the perineum is fully restored (Fig. 5.). | Fig. 5 Results of extended subfascial colpoperineoplasty. Click on the picture to view |
The results of this operation turned out to be so impressive that in our clinic we began to use it not only as an independent type of assistance, but also in addition to standard hybrid anterior-apical reconstructions in almost all patients, which significantly increased both the efficiency of operations and the quality of life of patients. . In 2018 alone, more than 600 surgical interventions of this type. Currently, on average, more than 120 of them are performed monthly.
. In 2018 alone, more than 600 surgical interventions of this type. Currently, on average, more than 120 of them are performed monthly.
The operation performed according to this method does not in any way limit subsequent pregnancies and childbirth in the traditional way.
The duration of extended subfascial colpoperineoplasty is no more than 20-30 minutes with an average blood loss of 50-70 ml. Patients are allowed to sit neatly on the evening of the operation. The statement is made the next day or the next day. Sex life is possible after 2 months. In the future, vaginal delivery is possible, but a caesarean section is advisable to preserve the results of the operation. The main advantages of the presented approach:
- maximum approximation of the results of the operation to the anatomy of the vagina "before childbirth",
- minimal pain syndrome,
- quick rehabilitation,
- high quality of sexual life and a high percentage of elimination of functional disorders of the rectum (according to international standard questionnaires),
- complete absence of foreign bodies (grids, etc.
 ).
).
Video
Organization of treatment
Hospitalization for the purpose of surgical treatment is carried out according to the principle "one window" . It is enough for the patient (or the person representing him) to write a letter with the wording of his question. At any time (both before hospitalization and after), you can ask questions of interest to the staff of the department.
CHI and VMP treatment
Citizens of the Russian Federation can receive free treatment under the CHI program for most diseases
No matter where you live
80% of patients come to us from the regions of the Russian Federation and countries of near and far abroad
Many years of experience
Every year more than 2200 operations of any complexity are performed in the Department of Urology
At any time (both before hospitalization and after), you can ask questions of interest to the staff of the department.
1. Online consultation with a specialist
The organization of hospitalization for the purpose of surgical treatment is carried out according to the principle of "one window". To do this, it is enough for the patient (or the person representing him) to write a letter with the wording of his question.
Write a letter
2. Appointment of the date of hospitalization
After the consultation, our administrator will contact you within a few days to make an appointment for hospitalization.
3. Examination before hospitalization
Preoperative examination should be carried out only after the approval of the date of hospitalization. You can get most of the examinations at the antenatal clinic or polyclinic at the place of residence free of charge, under the CHI policy.
 Most often, there are defects in the tendon center of the perineum (or the body of the perineum) and the posterior wall of the vagina.
Most often, there are defects in the tendon center of the perineum (or the body of the perineum) and the posterior wall of the vagina.