Rubella test during pregnancy
Rubella Test | Labcorp
View Sources
Sources Used for Current Review
May 2015 reviewer: Zhen Zhao, PhD, DABCC, Director of General Chemistry, Department of Laboratory Medicine, NIH Clinical Center.
Centers for Disease Control and Prevention. Epidemiology and Prevention of Vaccine-Preventable Diseases. Hamborsky J, Kroger A, Wolfe S, eds. 13th ed. Washington D.C. Public Health Foundation, 2015, Chapter 20, Rubella. Available online at http://www.cdc.gov/vaccines/pubs/pinkbook/downloads/rubella.pdf through http://www.cdc.gov. Accessed May 2015.
CDC Manual for the Surveillance of Vaccine-Preventable Diseases. 5th Edition, 2012. Chapter 14: Rubella.
WHO Manual for the laboratory diagnosis of measles and rubella virus infection. 2nd Edition, 2007.
Simon R Dobson. Congenital rubella syndrome: Clinical features and diagnosis. UpToDate (updated: June 02, 2014).
Sources Used in Previous Reviews
Thomas, Clayton L. , Editor (1997). Taber's Cyclopedic Medical Dictionary. F.A. Davis Company, Philadelphia, PA [18th Edition].
Pagana, Kathleen D. & Pagana, Timothy J. (2001). Mosby's Diagnostic and Laboratory Test Reference 5th Edition: Mosby, Inc., Saint Louis, MO., Pp 751-752.
(© 2005). Rubella Antibodies, IgG and IgM. ARUP's Guide to Clinical Laboratory Testing. Available online at http://www.arup-lab.com/guides/clt/tests/clt_192b.jsp#1147292 through http://www.aruplab.com.
Ben-Joseph, E. (2003 October, Reviewed). Rubella (German Measles). Familydoctor.org. Available online at http://www.kidshealth.org/PageManager.jsp?dn=familydoctor&lic=44&article_set=22917 through http://www.kidshealth.org
CDC (2005). Achievements in Public Health: Elimination of Rubella and Congenital Rubella Syndrome - United States, 1969-2004. Medscape, from MMWR. 2005; 54 (11): 279-282. Available online at http://www.medscape.com/viewarticle/501956 through http://www.medscape.com
A. D.A.M. editorial, Reviewed (2003 September 26, Reviewed). Previously reviewed by Adam Ratner. Rubella. MedlinePlus Medical Encyclopedia. Available online at http://www.nlm.nih.gov/medlineplus/ency/article/001574.htm through http://www.nlm.nih.gov/medlineplus/encyclopedia.html
D.A.M. editorial, Reviewed (2003 September 26, Reviewed). Previously reviewed by Adam Ratner. Rubella. MedlinePlus Medical Encyclopedia. Available online at http://www.nlm.nih.gov/medlineplus/ency/article/001574.htm through http://www.nlm.nih.gov/medlineplus/encyclopedia.html
Mayo Clinic Staff (2004 June 16). Rubella. MayoClinic.com. Available online at http://www.mayoclinic.com/invoke.cfm?id=DS00332 through http://www.mayoclinic.com
Stevens, L. (2002). Rubella. Medem Medical Library, JAMA Patient Page, from JAMA. 2002; 287:542. Available online at http://www.medem.com/MedLB/article_detaillb.cfm?article_ID=ZZZV5AZLMWC&sub_cat=286 through http://www.medem.com
Hughes, H. and Wharton, M. (2002). K. Rubella. VPD Surveillance Manual, 3rd Edition, Chapter 19, Laboratory Support for the Surveillance of VPDs: 19-16. PDF available for download at http://www.cdc.gov/nip/publications/surv-manual/chpt19_lab_support.pdf through http://www.cdc.gov
Hirsch, Lisa. Rubella (German Measles). (Reviewed July 2006). Familydoctor.org. Available online at http://www.kidshealth.org/PageManager.jsp?dn=familydoctor&lic=44&article_set=22917 through http://www.kidshealth.org. Accessed April 2008.
(Reviewed July 2006). Familydoctor.org. Available online at http://www.kidshealth.org/PageManager.jsp?dn=familydoctor&lic=44&article_set=22917 through http://www.kidshealth.org. Accessed April 2008.
Averhoff F, et al. Adequacy of surveillance to detect endemic rubella transmission in the United States. Clin Infect Dis. 2006; 43 Suppl 3:S151-7. Available online at http://www.medscape.com/medline/abstract through http://www.medscape.com. Accessed April 2008.
(July 9, 2007) Mayo Clinic Staff. Rubella. MayoClinic.com. Available online at http://www.mayoclinic.com/health/rubella/DS00332/DSECTION=1 through http://www.mayoclinic.com. Accessed April 2008.
(June 20, 2007) Centers for Disease Control and Prevention. Travelers Health: Yellow Book, Chapter 4: Prevention of Specific Infectious Diseases, Rubella. Available online at http://wwwn.cdc.gov/travel/yellowBookCh5-Rubella.aspx through http://wwwn.cdc.gov. Accessed April 2008.
Jin L, Thomas B. Application of molecular and serological assays to case based investigations of rubella and congenital rubella syndrome. J Med Virol. 2007; 79(7):1017-24. Available online at http://www.medscape.com/medline/abstract/17516526 through http://www.medscape.com. Accessed April 2008.
J Med Virol. 2007; 79(7):1017-24. Available online at http://www.medscape.com/medline/abstract/17516526 through http://www.medscape.com. Accessed April 2008.
(Updated May 2007) Centers for Disease Control and Prevention. Guidelines for Vaccinating Pregnant Women. Available online at http://www.cdc.gov/vaccines/pubs/preg-guide.htm#rubella through http://www.cdc.gov. Accessed online April 2008.
Centers for Disease Control and Prevention. MMWR (March 21, 2008) 51(53). Summary of Notifiable Diseases - United States 2006. Available online at http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5553a1.htm through http://www.cdc.gov. Accessed online April 2008.
Centers for Disease Control and Prevention. Travelers’ Health, Chapter 3 Infectious Diseases Related To Travel, Rubella. Available online at http://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-3-infectious-diseases-related-to-travel/rubella.htm through http://wwwnc.cdc.gov. Accessed October 2011.
Mayo Clinic Staff (2011 July 9) Rubella. MayoClinic.com [On-line information]. Available online at http://www.mayoclinic.com/print/rubella/DS00332/DSECTION=all&METHOD=print through http://www.mayoclinic.com. Accessed October 2011.
MayoClinic.com [On-line information]. Available online at http://www.mayoclinic.com/print/rubella/DS00332/DSECTION=all&METHOD=print through http://www.mayoclinic.com. Accessed October 2011.
(Updated 2011 January 3). Rubella: Make Sure Your Child Is Fully Immunized. Centers for Disease Control and Prevention [On-line information]. Available online at http://www.cdc.gov/features/rubella/ through http://www.cdc.gov. Accessed October 2011.
Kaneshiro, N. (Updated 2011 May 1). Congenital rubella. MedlinePlus Medical Encyclopedia [On-line information]. Available online at http://www.nlm.nih.gov/medlineplus/ency/article/001658.htm through http://www.nlm.nih.gov. Accessed October 2011.
Kaneshiro, N. (Updated 2011 January 24). Rubella. MedlinePlus Medical Encyclopedia [On-line information]. Available online at http://www.nlm.nih.gov/medlineplus/ency/article/001574.htm through http://www.nlm.nih.gov. Accessed October 2011.
Litwin, C. (Updated 2010 October). Rubella Virus. ARUP Consult [On-line information]. Available online at http://www.arupconsult.com/Topics/RubellaVirus.html?client_ID=LTD through http://www.arupconsult.com. Accessed October 2011.
ARUP Consult [On-line information]. Available online at http://www.arupconsult.com/Topics/RubellaVirus.html?client_ID=LTD through http://www.arupconsult.com. Accessed October 2011.
P Strebel, P. et. al. (2010 December 3). Progress Toward Control of Rubella and Prevention of Congenital Rubella Syndrome — Worldwide, 2009. Medscape Today News from Morbidity & Mortality Weekly Report. 2010;59(40):1307-1310 [On-line information]. Available online at http://www.medscape.com/viewarticle/730825 through http://www.medscape.com. Accessed October 2011.
Ezike, E. and Ang, J. (Updated 2011 October 3). Pediatric Rubella. Medscape Reference [On-line information]. Available online at http://emedicine.medscape.com/article/968523-overview#showall through http://emedicine.medscape.com. Accessed October 2011.
Pagana, K. D. & Pagana, T. J. (© 2011). Mosby's Diagnostic and Laboratory Test Reference 10th Edition: Mosby, Inc., Saint Louis, MO. Pp 852-853.
(February 18, 2011) Centers for Disease Control and Prevention.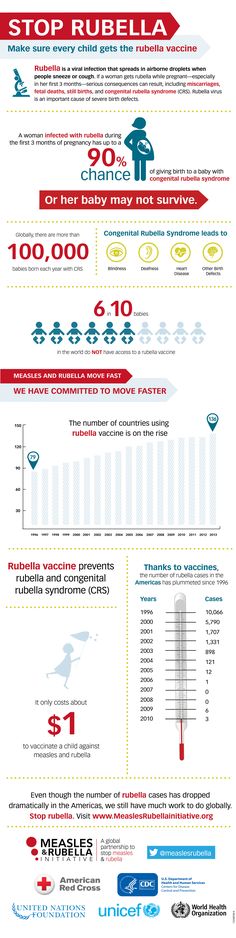 FastStats, Measles Morbidity. Available online at http://www.cdc.gov/nchs/fastats/measles.htm through http://www.cdc.gov. Accessed October 2011.
FastStats, Measles Morbidity. Available online at http://www.cdc.gov/nchs/fastats/measles.htm through http://www.cdc.gov. Accessed October 2011.
Rubella and pregnancy | March of Dimes
Rubella is an infection that causes mild flu-like symptoms and a rash.
Vaccines usually given in childhood prevent you from getting the infection
Up to half of people infected with rubella don’t have any symptoms but still can spread it to others.
You can get rubella from an infected person who coughs or sneezes, or by sharing food or drinks with someone who is infected.
Rubella can cause serious problems for your baby if you get infected while pregnant, especially during the first three months of pregnancy.
Rubella, also called German measles, is an infection that causes mild flu-like symptoms and a rash. Up to half of people infected with rubella don’t have any symptoms and may not even know they’re infected but still spread it to other people.
If you get infected during pregnancy, rubella can cause serious problems for your baby. Infection causes the most severe damage when the pregnant person is infected early in their pregnancy, especially in the first 12 weeks (3 months)..
Rubella has been nearly eliminated in the United States because of the routine vaccination of children. Vaccination protects a person against rubella for life. But people who were never vaccinated as children can get infected. You can be vaccinated as an adult when you are not pregnant.
Between 2005 and 2011, 67 cases of rubella were reported in this country. This is up from the previous period—2001 to 2004—when only 5 cases were reported. Vaccination is the best way to prevent infection. Today less than 10 people in the United States are reported to have rubella and it is usually associated with travel and not being vaccinated.
Rubella is common in many other countries. Travelers can bring it into the United States, or you can get it when traveling outside the country.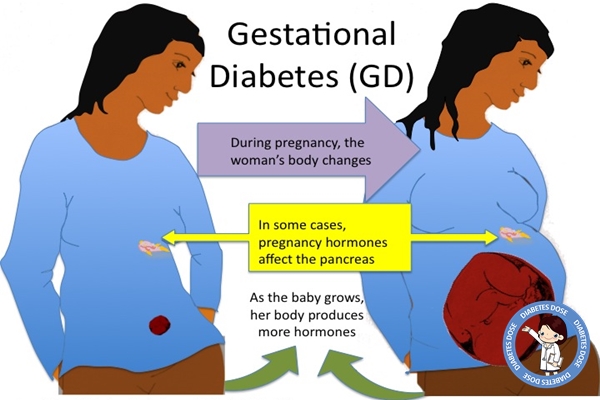
It’s important to get vaccinated for rubella. Talk to your health care provider to make sure you’re protected against it. A blood test can provide you with information about your immunity to rubella
What are the signs and symptoms of rubella?
Rubella is usually mild, with flu-like symptoms followed by a pink or light red rash. The rash usually starts on the face, then spreads to the rest of the body. The rash lasts about 3 days. Other symptoms include:
- Low-grade fever (102 F/38.9 C or lower)
- Headache
- Loss of appetite
- Runny nose
- Sore throat
- Cough
- Red eyes or pink eye (conjunctivitis)
- Swollen glands in the neck or behind the ears
- Muscle aches or joint pain
Up to 7 in 10 (70 percent) teenage and adult women who get rubella develop arthritis. Arthritis is swelling and pain in your joints. Women who are infected with rubella may feel arthritis in their fingers, wrists and knees. This complication is rare in men or children who get rubella. In rare cases, rubella can cause serious problems, including brain infections and bleeding problems.
This complication is rare in men or children who get rubella. In rare cases, rubella can cause serious problems, including brain infections and bleeding problems.
Some people have no symptoms so you may not know that you or they have rubella.
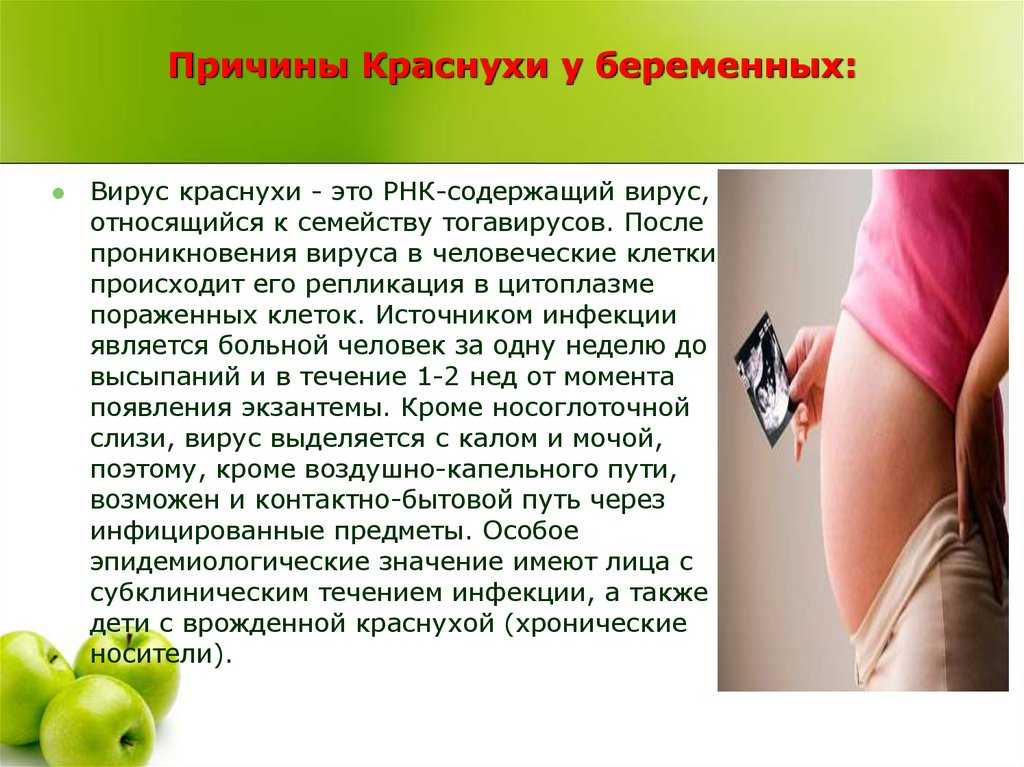
What causes rubella?
Rubella is caused by a virus (a tiny organism that can make you sick). It is not caused by the same virus that causes measles. It’s very contagious. It spreads through the air when an infected person coughs or sneezes, or by sharing food or drinks with someone who is infected. It also can be passed to a baby from a pregnant person who is infected.
A person with rubella may spread the disease to other people up to 1 week before they notice a rash. Infected people can continue to spread the disease up to 7 days after getting a rash.
People infected with rubella should tell their friends, family, and the people they work with if they have rubella. If your child has rubella, it’s important to tell their school or daycare provider. Telling others helps prevent the spread of rubella to even more people.
Telling others helps prevent the spread of rubella to even more people.
What problems can rubella cause during pregnancy?
Rubella can be serious for the baby, especially during the first 3months. Having rubella during pregnancy increases the risk of:
- Congenital rubella syndrome (CRS) – This is a condition that happens when a pregnant person passes rubella to their baby during pregnancy. It may cause your baby to be born with one or more birth defects, including heart problems, vision problems, deafness, intellectual disability, low birthweight, bone marrow problems, and liver and spleen damage. There is no cure for CRS. However, from 2005 to 2018, only 15 babies were diagnosed with CRS in the U.S., according to the Centers for Disease Control and Prevention (CDC).
- Miscarriage – This is when a baby dies before 20 weeks of pregnancy.
- Stillbirth – This is when a baby dies after 20 weeks of pregnancy.
- Preterm – This is birth that happens before 37 weeks of pregnancy
Can you pass rubella to your baby during pregnancy?
Yes. The best way to protect your baby is to make sure you’re immune to rubella. Immune means being protected from an infection. If you’re immune to an infection, it means you can’t get the infection.
The best way to protect your baby is to make sure you’re immune to rubella. Immune means being protected from an infection. If you’re immune to an infection, it means you can’t get the infection.
You are probably immune to rubella because you were vaccinated as a child or you had the illness during childhood. A blood test can tell if you’re immune to rubella. If you’re thinking about getting pregnant and aren’t sure if you’re immune, talk to your health care provider about getting a blood test. If you were not born in the United States or came as an adult you may not be vaccinated against rubella. Ask your health care provider to do a blood test to see if you are immune to rubella.
If you’re not immune to rubella, here’s what you can do to help protect your baby:
Before pregnancy. Get the measles, mumps and rubella (MMR) vaccine. Wait 1 month before trying to get pregnant after getting the shot.
During pregnancy. You can be tested at a prenatal visit to make sure you’re immune to rubella. If you’re not immune, the MMR vaccine isn’t recommended during pregnancy. But there are things you can do to help prevent getting infected with rubella:
If you’re not immune, the MMR vaccine isn’t recommended during pregnancy. But there are things you can do to help prevent getting infected with rubella:
- Stay away from anyone who has the infection.
- Tell your health care provider right away if you’ve been in contact with someone who is sick and may have rubella.
After pregnancy. Get the MMR vaccination after you give birth. It is safe to get the MMR vaccine while nursing. Being protected from the infection means you can’t pass it to your baby before they get their own MMR vaccination at about 12 months. It also prevents you from passing rubella to your baby during a future pregnancy.
What are the chances of passing rubella to your baby during pregnancy?
You’re more likely to pass rubella to your baby the earlier you become infected during pregnancy. For example:
- If you get rubella in the first 12 weeks of pregnancy, your baby has an 8 to 9 in 10 chance (85 percent) of getting infected.
 This is a very high chance.
This is a very high chance. - If you get rubella at 13 to 16 weeks of pregnancy, your baby has a 1 in 2 chance (50 percent) of being infected.
- If you get rubella at the end of your second trimester or later, your baby has a 1 in 4 chance (25 percent) of getting infected.
If you have rubella during pregnancy, your baby’s provider will carefully monitor your baby after birth to find any problems early.
How is rubella treated?
There is no specific medicine to treat rubella. In many cases, the symptoms of the disease are mild. Staying in bed (bed rest), drinking fluids and taking medicines to reduce fever can help.
Pregnant people with rubella may be treated with acetaminophen to relieve their symptoms. In more serious cases, treatment may include blood transfusion or steroids. A blood transfusion is when you have new blood put into your body. Steroids are synthetic hormones that treat inflammation.
Contact your health care provider if you are pregnant and think you have rubella or have been exposed to the disease.
Last reviewed: August 2021
See also: Your baby’s vaccinations, Vaccinations and pregnancy
Questions about rubella during pregnancy: page 1
My husband was vaccinated against rubella, a month later she became pregnant. Could this affect the child? Doctors of medical clinics "Art-Med" answer questions about the danger of rubella for pregnant women.
Ask a Question
At the age of 20 I was vaccinated against rubella (I know this for sure), at 29 I became pregnant, but during the tests, rubella antibodies were not found. Pregnancy and childbirth proceeded normally (I took care of my health), now I am 31 years old, we are thinking about a second child. Do I need to be vaccinated? And will it be effective?
You can repeat the blood test for rubella antibodies, because the previous test was taken during pregnancy. In the absence of the desired level of Ig G, it makes sense to get vaccinated before pregnancy.
With rubella IgG (+) 2.187 / 0.239 can pregnancy be planned?
You can plan pregnancy
Pregnancy occurred 1.5 months after the measles and rubella vaccine, are there any risks for the baby? I re-read the entire Internet, somewhere they write that it is necessary to protect themselves for 1 month, somewhere - 3 months.
After vaccination, pregnancy planning is recommended after 3-6 months. You need a face-to-face consultation with a geneticist to assess your individual risk.
Last Wednesday, on the 18th, I was in contact with a child (talked for several hours), who had a fever on the 20th, and today there were spots behind the ears, on the face, and swollen lymph nodes (rubella). According to her mother's theory, they got infected on the 12th when they went to the children's clinic to get a DPT shot. As a child, I didn’t suffer from any childhood diseases, in the first trimester and during pregnancy I never had TORCH infections (because there were no and no reagents in the LCD), i.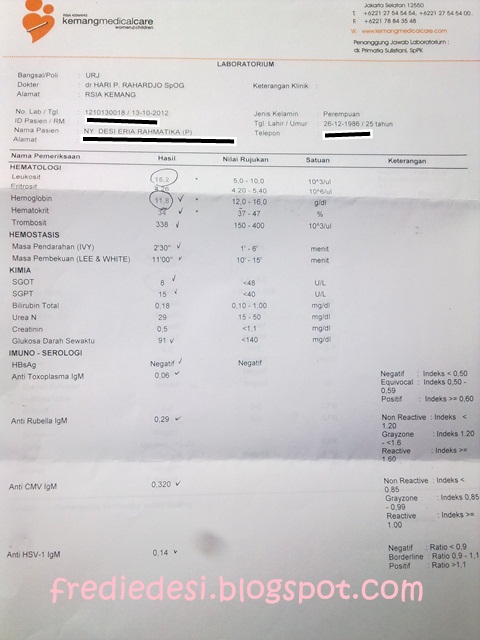 e. I don’t know if I have antibodies to the disease. How to proceed? To hand over on antibodies IgG and IgM tomorrow on an empty stomach or in two weeks? Or is it better tomorrow and again in two weeks? Maybe it makes sense to inject immunoglobulin? I don't want to call my gynecologist, I'm afraid he'll send me to an infectious diseases clinic. My due date is now 27-28 weeks. I also found my vaccination calendar, judging by it, I was vaccinated for the last time in 2009year. Today is the 23rd.
e. I don’t know if I have antibodies to the disease. How to proceed? To hand over on antibodies IgG and IgM tomorrow on an empty stomach or in two weeks? Or is it better tomorrow and again in two weeks? Maybe it makes sense to inject immunoglobulin? I don't want to call my gynecologist, I'm afraid he'll send me to an infectious diseases clinic. My due date is now 27-28 weeks. I also found my vaccination calendar, judging by it, I was vaccinated for the last time in 2009year. Today is the 23rd.
We recommend that you take a blood test for IgM immunoglobulin against rubella without fail. After that, based on the results of the analysis, decide the issue with the attending physician (gynecologist) about further treatment practice.
At the age of 13 I was vaccinated against rubella, I did not get rubella. I am now 27 years old and pregnant (10 weeks). She passed the tests and according to the results, she allegedly had recently been ill with rubella (lgM antibodies were detected, lgG 173, 100% highly avid antibodies).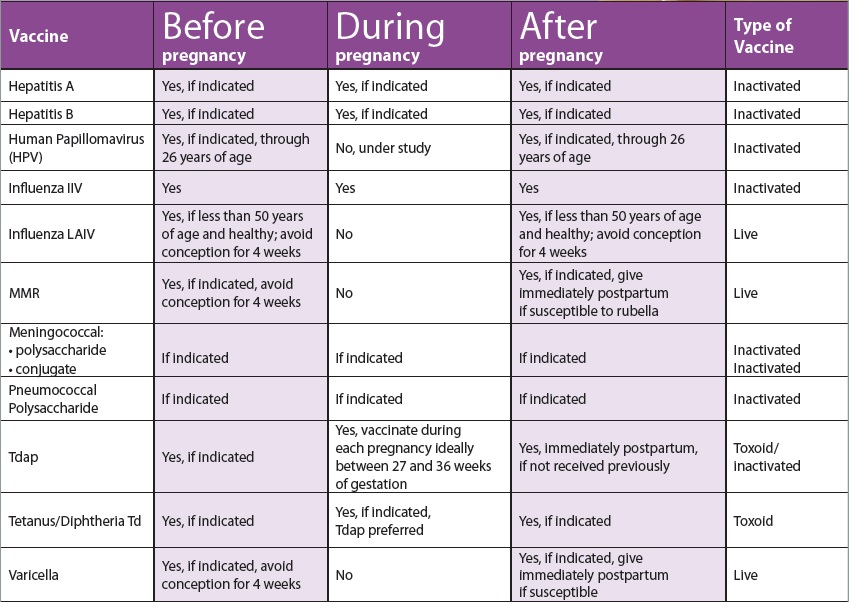 What is the risk to the fetus?
What is the risk to the fetus?
You need to contact an in-person consultation with an infectious disease specialist. At 11-13 weeks, I screening is recommended (ultrasound + biochemical study), based on the results of which possible risks can be assessed.
I was vaccinated with Priorix (measles, rubella, mumps) on November 13th. December 20th I find out I'm pregnant. The doctor said you can not 3 months at least. How to be, how it can affect the fetus?
16 weeks pregnant. I didn't get rubella and didn't get vaccinated. I donated blood at the antenatal clinic. The result of the analysis: rubella igM-neg, igG-pos (1.81,) up to 0.03. As a result, do I have immunity or not?
You are tested positive for rubella. Most likely, you once came into contact with the virus and the immune system reacted, but there were no clinical manifestations.
Pregnancy 11 weeks. I got vaccinated against rubella ten years ago.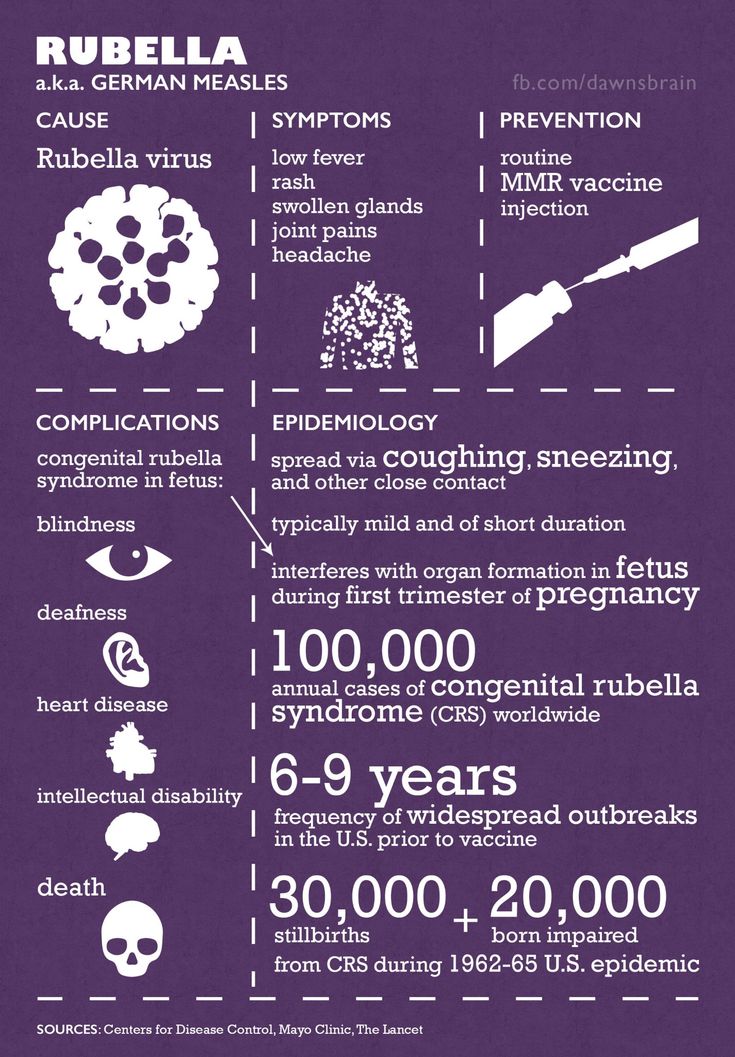 When planning pregnancy, I took an analysis for antibodies: IgM is doubtful, IgG is positive. Planning a pregnancy was allowed. But for a period of 11 weeks, the tests showed: IgM positive, IgG positive. Sent to retake. In two laboratories, different results: in one IgM is questionable, in the other IgM is positive. There are no symptoms and never have been. No contact with patients. Could I be re-infected 10 years after the vaccination? I'm 28 years old.
When planning pregnancy, I took an analysis for antibodies: IgM is doubtful, IgG is positive. Planning a pregnancy was allowed. But for a period of 11 weeks, the tests showed: IgM positive, IgG positive. Sent to retake. In two laboratories, different results: in one IgM is questionable, in the other IgM is positive. There are no symptoms and never have been. No contact with patients. Could I be re-infected 10 years after the vaccination? I'm 28 years old.
Questionable IgM results occur intermittently during pregnancy. To clarify the issue of infection, it is necessary to determine the avidity index of IgG antibodies to cytomegalovirus. But in any case, in the absence of clinical manifestations of the disease, the risk of fetal pathology is low.
Fourth pregnancy at 18 weeks positive for igM 5.7 and igG 28. All three previous pregnancies were igM negative at high igG (132 - 6 years ago, 48 - 4 years ago, 34 - 2 years ago). Clinically, I did not feel the manifestations of the disease and I can tell at what period of fetal development this happened. How can you comment on the situation? The pediatrician claims that there was an infection, the gynecologist refers to some properties of the blood. I am 30 years old.
How can you comment on the situation? The pediatrician claims that there was an infection, the gynecologist refers to some properties of the blood. I am 30 years old.
In your situation, we recommend that you conduct an additional examination and consult with an infectious disease specialist.
Second pregnancy, 16 weeks. Test results: igg positive and igm positive (without any numbers, values). I didn't have any rubella symptoms. The doctor only noticed at 30 weeks. Two years ago I had my first pregnancy and I remember 100% that the doctor then told me that I had rubella (according to test results) in childhood and that I have antibodies. What do the analyzes of this year mean? Is there a danger? Unfortunately, the doctor noticed such dubious results only 14 weeks after the test.
It is believed that after suffering from rubella, a person develops stable immunity for life. The "strength" of immunity is confirmed by a certain amount of specific antibodies in the blood.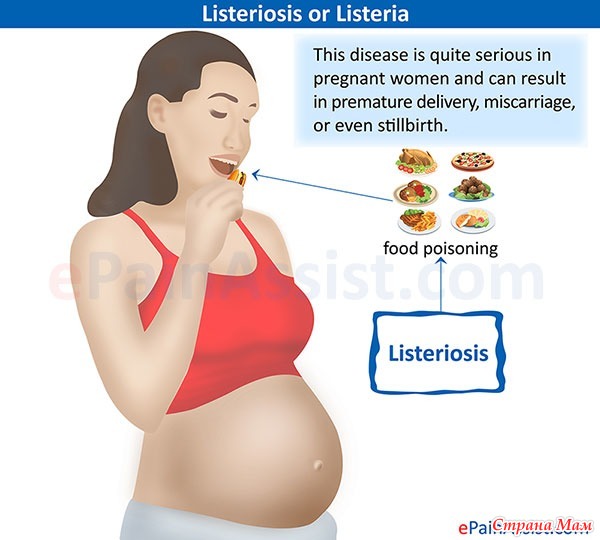
10 weeks of pregnancy, high levels of G,M antibodies were found during blood test for rubella. She retaken the test, but there are no results yet, she has been vaccinated against rubella and there are no signs of the disease. Can the result be wrong?
If you have been vaccinated against rubella, the result may be erroneous depending on the timing of the vaccination.
How long after exposure to rubella can it be reliably determined by analysis whether I have been infected or not? Or symptoms of the disease occur earlier? I do not have antibodies and there is a suspicion that I may be pregnant (not sure yet, too early for tests). How can I check my status? What should I do if it turns out that I am infected?
Every living organism has an immune system that protects the body from the effects of foreign cells. The mechanism of immunity ensures the removal from the body of proteins that have been changed during illness, pathological process or life changes. The whole complex of immunological reactions supports individual homeostatic immunity in multicellular organisms. All cells of the immune system are divided into several types: antigen-recognizing, stromal and auxiliary. The most important is the first type of cells, which consist of lymphocytes - they carry receptors on their surface, with the help of which they bind to antigens (substances foreign to our body). The molecules responsible for the recognition and binding of antigens are called immunoglobulins. They are made up of glycoproteins. There is a classification of immunoglobulins with a specific designation: immunoglobulins - IgG, IgA, IgM, IgE, IgD, where Ig means globulin, and the letter is the class of immunoglobulin. All of them differ in amino acid composition, structure and functions. Consult an infectious disease specialist with the results of your tests.
The whole complex of immunological reactions supports individual homeostatic immunity in multicellular organisms. All cells of the immune system are divided into several types: antigen-recognizing, stromal and auxiliary. The most important is the first type of cells, which consist of lymphocytes - they carry receptors on their surface, with the help of which they bind to antigens (substances foreign to our body). The molecules responsible for the recognition and binding of antigens are called immunoglobulins. They are made up of glycoproteins. There is a classification of immunoglobulins with a specific designation: immunoglobulins - IgG, IgA, IgM, IgE, IgD, where Ig means globulin, and the letter is the class of immunoglobulin. All of them differ in amino acid composition, structure and functions. Consult an infectious disease specialist with the results of your tests.
Rubella vaccine was given as part of pregnancy planning on December 24 last year (VPK preparation, dose 0. 5). Positive IgM persisted for a long time, so planning was refrained from. The pregnancy came in July of this year. For a period of 5 weeks (7 months after vaccination), the results of the analysis of IgG - 81.08; IgM - 1.02 (weakly positive: 0.8 - 1.1). Why mentally prepare? Is there a possibility of the virus affecting the embryo?
5). Positive IgM persisted for a long time, so planning was refrained from. The pregnancy came in July of this year. For a period of 5 weeks (7 months after vaccination), the results of the analysis of IgG - 81.08; IgM - 1.02 (weakly positive: 0.8 - 1.1). Why mentally prepare? Is there a possibility of the virus affecting the embryo?
Immunoglobulin M (IgM) is produced by plasma B cells as an immune response to the appearance of antigens of foreign bacteria, viruses, fungi, parasites and other pathogens. When they enter the human blood, they are quickly identified by the immune system, and the synthesis of antibodies begins to destroy them as soon as possible. It is class M proteins that are responsible for the first response of the body to the onset of infectious processes and provide initial humoral immunity. The likelihood of the virus affecting the embryo is minimal.
6 weeks pregnant, wife became pregnant one and a half months after PRIORIX (GSK) 0. 5 ml, series: AMJRO002AA. We passed the tests and did an ultrasound, but the results will be only in a week, we are very worried. How safe is it to get pregnant in a month and a half? Will there be side effects and how much will this fact affect the health of the embryo?
5 ml, series: AMJRO002AA. We passed the tests and did an ultrasound, but the results will be only in a week, we are very worried. How safe is it to get pregnant in a month and a half? Will there be side effects and how much will this fact affect the health of the embryo?
The risk to the fetus is minimal. Do not worry.
3-4 weeks of pregnancy, I work as a consultant in a children's store, I dressed a 4-year-old girl who had rubella these days, there was direct contact. The vaccine was given to me 20 years ago. What is the danger to the fetus?
If you don't get sick (most likely), the risk to your unborn child is low.
8 weeks of pregnancy, when planning, the doctor insisted on a rubella vaccination Priorix (measles, rubella, mumps), made in Belgium, the vaccination was made on December 15th. The doctor said that it is not necessary to wait 3 months, the manufacturers are reinsured. I got pregnant in February, but on the Internet everyone writes that it is necessary to wait 3 months. What will happen to the fetus now? Can I leave the pregnancy?
There is no convincing evidence of an increased risk of fetal CM after vaccination against measles rubella, including. In this regard, there are no indications for termination of pregnancy.
I had rubella in my childhood, more than 20 years ago. Now antibodies lgG - 57.1, lg M - have been detected. Could this mean that the immunity is gone and I have been ill again in a latent form? Is it possible to plan a pregnancy?
Unlikely. Most likely - this is not a specific reaction. You can plan your pregnancy.
I was vaccinated against rubella at 4 weeks of pregnancy. Can a vaccine adversely affect a child's health?
Extremely unlikely.
Date of conception January 31st and rubella vaccination on February 1st. Can there be pathologies in a child due to this vaccination?
No, this will not lead to fetal pathology.
13 weeks pregnant, rubella test result: lgg 198.6, avidity 82.0. Re-analysis showed: lgg 810, avidity 99.lgm - not found. Third result: lgg 159.3, avidity 87.7 lgm - positive. During and before pregnancy, there were no symptoms of rubella. Did I get sick as a child or already during pregnancy? I am 21 years old.
You have high avidity, indicating a long-term (before pregnancy) infection, which could be asymptomatic.
On October 18, she was vaccinated against rubella, Igg was 0.2 - negative, no antibodies. The result of the analyzes from December 12: Igg - 35.4 (at 0.0 - 10.0), Img -1.08 (at 0.0 - 0.8). Is it possible to plan a pregnancy already or should I wait?
After vaccination, it is recommended to plan pregnancy after 3 months.
35-36 weeks of pregnancy, a 4-year-old daughter has rubella. What should I do? Is it dangerous?
The fetus has already formed, malformations will no longer occur.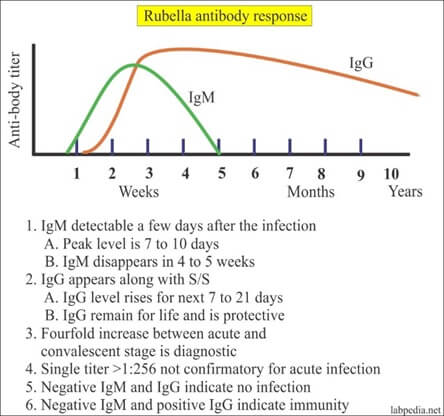 But if you get sick, it is possible that the fetus will have an intrauterine infection.
But if you get sick, it is possible that the fetus will have an intrauterine infection.
I was vaccinated against rubella in October and I got pregnant in November. Is it necessary to terminate the pregnancy?
You have no indications for termination of pregnancy due to vaccination.
2 - 3 weeks pregnant, 14 October vaccinated against rubella and tetanus, 21 October found out she was pregnant. Is there a risk to the fetus?
No risk to the fetus. Can keep pregnancy.
I was vaccinated with Priorix (measles, rubella, mumps) on April 24, the last test for rubella antibodies on September 17: Igm 1.7+, lgg 32.3++. Is it possible to plan a pregnancy? Does it make sense to get tested for rubella by PCR?
Three months after vaccination, pregnancy can be planned.
Pregnancy 3 weeks confirmed on 11 August. On May 28, she was vaccinated against rubella, a week later she had a rash, a temperature of 37. 2 and an increase in lymph nodes. All these symptoms disappeared within three days. I could not get pregnant for 3 years, so for the last month I did not use protection with my husband, as I was going to start an examination of the causes of infertility. Donated blood for the presence of rubella antibodies: IgM - 2.2 COI positive, IgG 33.7 IU / ml positive. How high is the risk of developing pathology in the fetus and is an abortion indicated in this case?
2 and an increase in lymph nodes. All these symptoms disappeared within three days. I could not get pregnant for 3 years, so for the last month I did not use protection with my husband, as I was going to start an examination of the causes of infertility. Donated blood for the presence of rubella antibodies: IgM - 2.2 COI positive, IgG 33.7 IU / ml positive. How high is the risk of developing pathology in the fetus and is an abortion indicated in this case?
Carry your pregnancy calmly. There is no cause for concern in this regard.
Was vaccinated against rubella, diphtheria, tetanus on the 11th day after ovulation, when the gestational age was 3 weeks. The first day of the last day of the cycle is June 6, the vaccine was given on June 30. The gynecologist insists on terminating the pregnancy, I did not find information that the rubella vaccine has a negative effect on the fetus and that the risk is theoretical, but since there are no studies, there is no reliable data. How to act in such a situation? What were your practical experiences?
How to act in such a situation? What were your practical experiences?
You have no indications for abortion. The risk to the fetus is minimal.
vaccinated against rubella on 1 June, not tested for rubella antibodies. June 18 test result: anti-Rubella IgG 145.4 U/ml (>=10 positive), IgM - negative. Is it possible to plan a pregnancy now? Or do I have to wait two months?
Test results indicate that your body is responding to the vaccine. You can plan your pregnancy.
I was vaccinated against rubella on March 4, I regularly monitor IgG and IgM levels, I take an analysis every three weeks. IgM is still "detected". How long can it remain in the blood and when can pregnancy be planned?
You can now easily plan a pregnancy. Depending on the characteristics of the immune system, a long-term increase in IgM is possible - it does not bother anyone.
5 weeks pregnant, a 6-year-old child brought measles rubella from kindergarten. As a child, I was vaccinated, according to the vaccination plan, and also had rubella myself. I feel fine, no breakouts. What about pregnancy? Is it dangerous to be with a rubella patient?
As a child, I was vaccinated, according to the vaccination plan, and also had rubella myself. I feel fine, no breakouts. What about pregnancy? Is it dangerous to be with a rubella patient?
It is the disease of the mother during pregnancy that is dangerous for the fetus, and not contact with the patient. It is advisable for you to do an analysis for rubella antibodies (immunoglobulins M and G) at intervals of 2 weeks.
Rubella during pregnancy - maternity hospital "Leleka"
What is rubella?
Rubella is an infectious disease that is accompanied by high fever and rashes on the skin, as well as chills, redness of the face, pain in the throat and in the lymph nodes. Rubella is classified as a childhood disease: this highly contagious virus most often affects children of preschool and primary school age. The infection is transmitted only from person to person by airborne droplets, the peak incidence occurs in the spring. Sometimes adults get sick too. Subject to the regimen, the disease is easily tolerated and does not cause complications.
Rubella during pregnancy
During pregnancy, rubella is considered a dangerous disease. In the first trimester, the transferred rubella increases the risk of miscarriage up to 40%, fading of pregnancy and the birth of a dead child - by 20%, the death of a baby in the first year of life - 10% higher. The virus inhibits the process of cell division. During the period of intensive development of the fetus, laying and formation of internal organs, the action of the virus can critically affect the viability of the fetus, as well as the ability of its organs to fully perform their functions.
The most dangerous period is up to the 14th week of pregnancy, when all the main organs are laid in the fetus. If a pregnant woman becomes ill, the virus can pass through the placenta to the fetus and cause congenital rubella syndrome. This syndrome causes pathologies of development: from 3 to 11 weeks of pregnancy - the brain, 4-7 weeks - pathologies of the eyes and heart, 7-13 - hearing impairment; during the same period, rubella can lead to the appearance of a cleft lip, as well as other pathologies and deformities in the fetus, up to its complete non-viability. Most often, the "Gregg triad" develops (cataract - 75% of cases, heart disease - 50%, deafness - 50%). Unfortunately, after suffering rubella, auto-abortion often occurs, or premature birth, in which the fetus is born unviable.
Most often, the "Gregg triad" develops (cataract - 75% of cases, heart disease - 50%, deafness - 50%). Unfortunately, after suffering rubella, auto-abortion often occurs, or premature birth, in which the fetus is born unviable.
Congenital rubella syndrome
From about 16 weeks, the risk of dangerous pathologies due to congenital rubella syndrome decreases, the consequences of the disease are not so critical. But if a pregnant woman has been ill with rubella before 14 weeks, this is the official reason for artificial termination of pregnancy. A woman should remember that the decision to terminate a pregnancy is not made by the doctor, but by herself. In such a situation, the doctor can only advise and advise. If a woman hesitates in making a decision, a consultation with a gynecologist can help her.
A special fetal blood test will help determine if the rubella virus has been able to cross the placenta and pose risks to the fetus. In addition, it is recommended to prescribe an additional ultrasound diagnostic session in order to examine the development of the baby's vital organs and exclude the development of pathologies.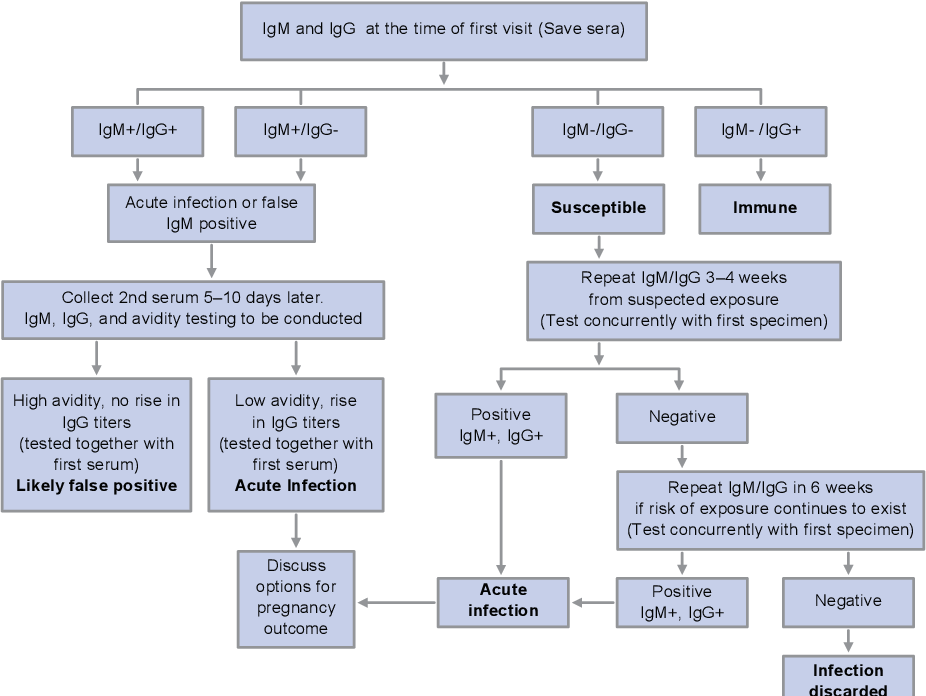
Another danger of rubella is that it can be asymptomatic in adults. Thus, a woman can get rubella without noticing it. If cases of rubella are recorded in the region, pregnant women are offered to undergo a special analysis for antibodies. The presence in the blood of a pregnant woman of a large number of antibodies to the causative agent of this disease will show whether the woman was sick.
Vaccination against rubella
Rubella is included in the list of diseases against which children in Ukraine are vaccinated at the age of one year. The incidence of rubella is low. If for some reason a pregnant woman has not been vaccinated against rubella, she should inform her doctor at the time of registration for pregnancy. However, even childhood vaccination does not provide 100% protection against the disease. Ideally, the rubella vaccine should be done additionally, a few months before the planned pregnancy. This is especially true for women who work in areas with an increased risk of disease - children's educational institutions, children's clinics, etc.