How to break up phlegm in child
9 methods of congestion relief in toddlers including home remedies
A few simple home remedies, such as using a humidifier, can provide congestion relief for toddlers. In most cases, the common cold causes congestion, but other causes include allergies.
Colds can be a miserable experience for toddlers, and unfortunately, according to the Centers for Disease Control and Prevention (CDC), colds are common in young children. Because colds are viruses, antibiotics do not have any effect. In most cases, colds eventually go away on their own.
In this article, we discuss nine ways to treat congestions in toddlers, causes of congestion, and when to see a doctor.
Share on PinterestInhaling steam, using a humidifier, and drinking fluids are home remedies that may provide congestion relief for toddlers.There is a range of home remedies that can provide congestion relief for toddlers:
1. Steam inhalation
A warm, steamy room can help loosen thick mucus and make it easier for a child to breathe. Try giving a child a warm bath before bed. Then take the child out of the tub, turn the shower up to its hottest setting, and close the door.
Allow the steam to fill the room while sitting with the child. The room should not be so hot that breathing is difficult.
2. Humidifier
A humidifier, especially a cool mist one, keeps the air moist. This can help ease a dry cough and may reduce congestion, particularly at night. Try putting a humidifier in the child’s room.
Make sure the child is not alone with the humidifier and does not treat it as a toy. Keep the humidifier clean, since mold can easily grow in wet spaces.
3. Bulb suction
Very young children may struggle more with congestion because they cannot clear their nose. Try using a bulb suction device to gently clear the child’s nose. If the child resists or says suctioning hurts, try another treatment.
4. Saline nasal sprays
Saline nasal sprays can help soothe an irritated nose.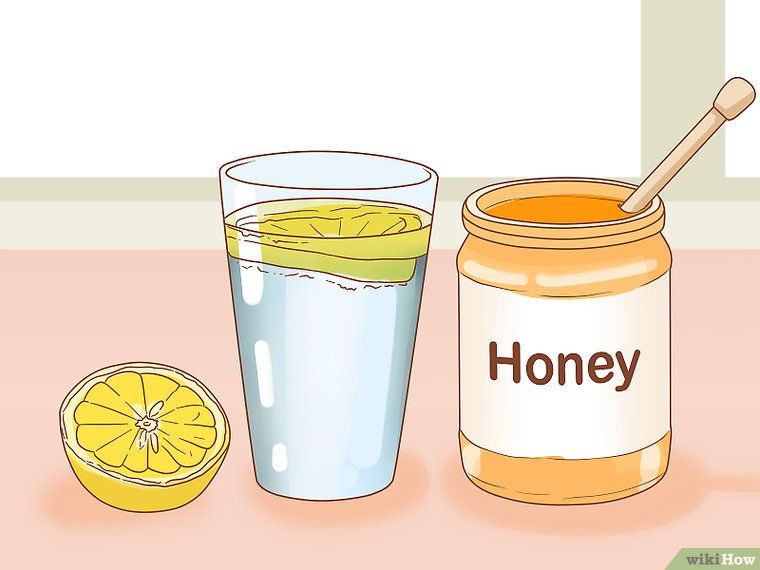 They may also help loosen up thick mucus. Most stores sell over-the-counter (OTC) solutions. Parents can also make their own by combining half a teaspoon of table salt with 1 cup of warm water.
They may also help loosen up thick mucus. Most stores sell over-the-counter (OTC) solutions. Parents can also make their own by combining half a teaspoon of table salt with 1 cup of warm water.
Gently spray into the child’s nose, or show the child how to do it themselves. For more relief, try spraying the nose and then suctioning the nose with a bulb syringe. Parents may also find that saline nasal sprays offer more relief after a child spends time in a steamy room.
5. Chicken soup
Chicken soup is more than just a folk remedy. It may ease congestion by reducing inflammation. Some research suggested that chicken soup may ease inflammation in the upper respiratory tract, which could alleviate cold congestion symptoms.
Additionally, chicken soup can help a child remain hydrated and encourage them to keep eating when they do not feel well.
6. OTC pain relievers
OTC pain relievers, such as acetaminophen and ibuprofen, will not relieve congestion, but they may help with other symptoms, such as congestion-related pain in the face, or a fever. Ask a doctor before using these medications in very young children.
Ask a doctor before using these medications in very young children.
According to the American Academy of Pediatrics (AAP), in most cases, ibuprofen is safe for children over 6 months, and acetaminophen is safe for children of all ages. Aspirin is not safe for children.
Parents should choose a formula for children and follow the weight-based dosing instructions. If a child younger than 3 months old has a fever, call a pediatrician.
7. Plenty of fluids
Water and other fluids may help thin out mucus, making it easier for a child to cough it up. Fluids can also help prevent dehydration if a child has a fever.
Offer a child plenty of water when they are sick. Toddlers may be more willing to drink from a cup that features characters they like or from a silly straw.
8. Changing sleeping position
Congestion often worsens at night. One reason is that the sinuses cannot drain as easily when a person is lying down. Some children may also feel thirsty at night if they are congested and sleep with their mouths open.
Children may prefer sleeping with their heads elevated on a few pillows to ease the symptoms of congestion. Other children may enjoy sleeping in an even more upright position in a recliner.
9. Keeping the air clean
Parents who smoke should not smoke around children, and should not take the child to visit places where there may be smoke.
Although harder to control, air pollution can have a significant impact on children’s health. According to the American Lung Association, children living in areas with cleaner air display fewer respiratory symptoms, such as phlegm, congestion, and coughing.
Parents should not give toddlers OTC decongestants.
The Food and Drug Administration (FDA) advise against using decongestants in children under the age of 2 and recommend not using decongestants containing codeine or hydrocodone in anyone under 18.
The AAP emphasize that decongestants offer little or no benefit to children under the age of 4 and may have serious side effects.
Several studies of decongestants in toddlers and young children have found that these drugs offer no more relief than a placebo.
Antibiotics cannot cure a common cold but may help with other infections that can cause congestion, such as a sinus infection. However, sinus infections that require antibiotic treatment are rare in toddlers.
Colds in toddlers may improve in a few days, with congestion lasting longer. If a child’s symptoms worsen, they develop a fever, or their congestion does not improve, see a doctor for treatment.
Sometimes, a person may be unable to tell the difference between colds and other illnesses. Most infections that cause cold-like symptoms are contagious, so parents or caregivers should practice frequent handwashing and other hygiene measures to control the spread of all infections.
Some other potential causes of congestion include:
- Allergies: Allergies may also cause itchy, watery eyes, and do not usually cause a fever.

- Flu: The flu causes cold-like symptoms, though the symptoms tend to be more severe, and a child may be very sick for many days.
- Bacterial infections: A bacterial sinus infection can cause congestion; this could happen after a cold.
- Structural abnormalities: Sometimes, a child has a problem with the structure of their respiratory system. They might have a deviated septum or enlarged adenoids. Children who always seem congested should see a doctor.
Learn more about how cold symptoms present in toddlers here.
See a doctor if:
- A child seems very sick or does not get better within a few days with home remedies.
- A child has a very high fever.
- A child appears lethargic or confused.
- A baby younger than 3 months has a fever.
Most colds go away on their own within 7–10 days, though some symptoms may linger longer than this. If the infection does not go away, see a doctor as the toddler may have an allergy or a bacterial infection, such as a sinus infection.
The best way to prevent colds and most other illnesses is with diligent hygiene. This is difficult for toddlers, especially in daycare settings, where they have close contact with other children. Some strategies to prevent the spread of colds include:
- Practicing regular handwashing before meals and after using the bathroom. Make handwashing a fun ritual.
- Not sending a child who is unwell to school or daycare and not allowing people to visit who are sick.
- Teaching children to cover their cough by coughing into an elbow.
- Disinfecting frequently used surfaces, such as doorknobs, countertops, sink handles, and toilet flushers.
The average toddler gets a lot of colds — as many as 8–10 per year before they turn 2 years old. Parents can experiment with home remedies until they find something that works and that a child is willing to try. Consult a pediatrician for more advice about home remedies that may ease the specific symptoms a child gets.
Home Remedies, Meds, Tips, and More
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Certain remedies, such as staying hydrated, using a humidifer, and taking over-the-counter decongestants can all help ease excess phlegm in your throat or chest.
Phlegm is that thick, sticky stuff that hangs around in the back of your throat when you’re sick. At least that’s when most people notice it. But did you know that you have this mucus all the time?
Mucous membranes make phlegm to protect and support your respiratory system. These membranes line your:
- mouth
- nose
- throat
- sinuses
- lungs
Mucus is sticky so it can trap dust, allergens, and viruses. When you’re healthy, the mucus is thin and less noticeable. When you’re sick or exposed to too many particles, the phlegm can get thick and become more noticeable as it traps these foreign substances.
Phlegm is a healthy part of your respiratory system, but if it’s making you uncomfortable, there are ways to thin it or reduce it.
Keep reading to learn about some natural remedies, over-the-counter (OTC) medicines, and when you may want to see your doctor.
Moisturizing the air around you can help keep mucus thin. You may have heard that steam can clear phlegm and congestion, but there isn’t a lot of scientific support for this idea.
Instead of steam, you can use a cool mist humidifier. You can run this humidifier safely all day long. You’ll just want to make sure you change the water each day and clean your humidifier according to the package instructions.
Drinking enough liquids, especially warm ones can help with mucus flow.
Water and other liquids can loosen your congestion by helping your mucus move. Try sipping liquids, like juice, clear broths, and soup. Other good liquid choices include decaffeinated tea, warm fruit juice, and lemon water.
Your drinks shouldn’t be the only thing that’s warm. You should be, too! Staying warm is an easy home remedy to soothe your respiratory system. That’s because you’re better able to fight off conditions that cause excess mucus (like the common cold) when you’re at a warmer body temperature.
You should be, too! Staying warm is an easy home remedy to soothe your respiratory system. That’s because you’re better able to fight off conditions that cause excess mucus (like the common cold) when you’re at a warmer body temperature.
Methods to stay warm include:
- warm showers
- wearing warmer clothing to fend off cold temperatures
- cuddling up in bed with an extra blanket
Try consuming foods and drinks that contain lemon, ginger, and garlic. A 2018 survey found these may help treat colds, coughs, and excess mucus, though there isn’t much research to back it up.
Spicy foods that contain capsaicin, such as cayenne or chili peppers, might also help temporarily clear sinuses and get mucus moving.
There’s some scientific evidence from 2016 that the following foods and supplements may help treat and reduce the risk of certain viral respiratory diseases:
- licorice root
- ginseng
- berries
- echinacea
- pomegranate
You might also be wondering about the classic many grab when they’re sick: chicken soup. Does it help get rid of phlegm too? Some research suggests yes.
Does it help get rid of phlegm too? Some research suggests yes.
Chicken soup might be good for treating colds and getting rid of excess mucus. This is because chicken soup slows neutrophils’ movement in your body. Neutrophils, a type of white blood cell, fight off infection. When moving slowly, they stay in the areas of your body where infection exists for longer.
Overall, more studies are needed to confirm the effects of these foods, but for most people, adding these ingredients to their diet is safe to try.
If you’re taking any prescription medications, ask your doctor before adding any new ingredients to your diet.
Gargling warm salt water may help clear phlegm in the back of your throat. It may even help soothe a sore throat.
When gargling salt water, follow these easy steps:
- Mix together a cup of water with 1/2 to 3/4 teaspoon of salt. Warm water works best, because it dissolves the salt more quickly. It’s also a good idea to use filtered or bottled water that doesn’t contain irritating chlorine.

- Sip a bit of the mixture and tilt your head back slightly.
- Let the mixture wash into your throat without drinking it.
- Gently blow air up from your lungs to gargle for 30 to 60 seconds, and then spit out the water.
- Repeat as needed.
If you don’t want to gargle salt water, there’s an easier, more effective alternative to thin phlegm: saline. Saline is a salt water solution you can use as a nasal spray or in a neti pot. It’s available over the counter and is a natural way to clear out the sinuses.
Research from 2018 supports the idea that mucus thins out after consistently using a saline solution for longer than a week.
Using eucalyptus essential oil may help reduce excess mucus in your chest. It works by loosening the mucus so you can cough it out more easily. At the same time, if you have a nagging cough, the eucalyptus may relieve it.
You can either inhale the vapor by using a diffuser or use a balm that contains this ingredient.
While research suggests there are health benefits, the FDA doesn’t monitor or regulate the purity or quality of essential oils. It’s important to talk with a healthcare professional before you begin using essential oils and be sure to research the quality of a brand’s products. Always do a patch test before trying a new essential oil.
There are also OTC medicines you can use. Decongestants, for example, can cut down the mucus that flows from your nose. This mucus isn’t considered phlegm, but it can lead to chest congestion. Decongestants work by reducing swelling in your nose and opening up your airways.
You can find oral decongestants in the form of:
- tablets or capsules
- liquids or syrups
- flavored powders
There are also many decongestant nasal sprays on the market.
You can try products like guaifenesin (Mucinex) that thin mucus so it won’t sit in the back of your throat or your chest. This type of medication is called an expectorant, which means it helps you to expel mucus by thinning and loosening it.
This type of medication is called an expectorant, which means it helps you to expel mucus by thinning and loosening it.
This OTC treatment usually lasts for 12 hours, but you should follow the package instructions. There are children’s versions for kids ages 4 and older.
Chest rubs, like Vicks VapoRub, contain eucalyptus oil to ease coughs and potentially get rid of mucus. You can rub it onto your chest and neck up to three times each day. Younger children should not use Vicks at its full strength, but the company does make a baby-strength version.
If you have certain conditions or infections, your doctor may prescribe medications to treat the root cause of your symptoms. There are specific medications that can thin your mucus if you have a chronic lung condition, like cystic fibrosis.
Hypertonic saline is a treatment that’s inhaled through a nebulizer. It’s stronger than an OTC saline solution, which means it can sometimes be more effective. It works by increasing the amount of salt in your air passages.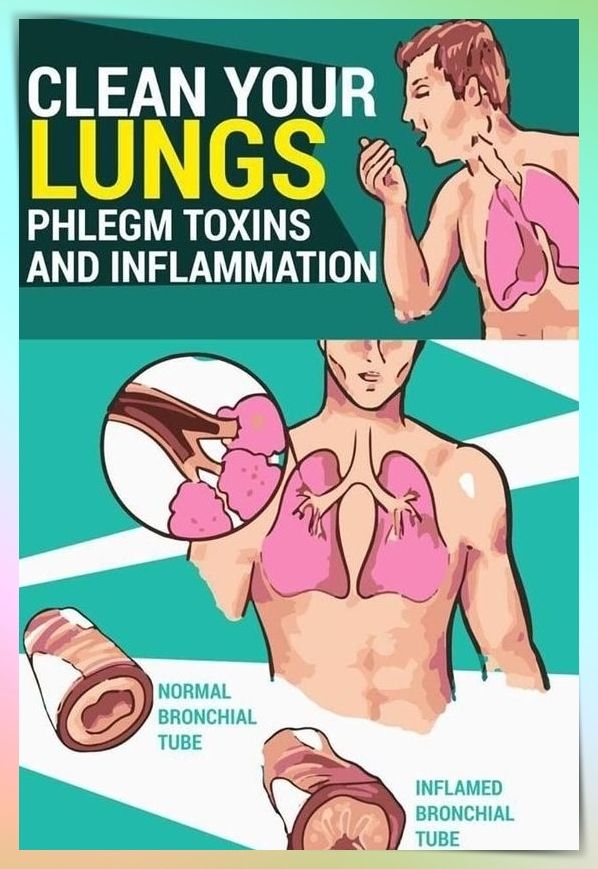 It comes in different strengths and can be used on people ages 6 and older.
It comes in different strengths and can be used on people ages 6 and older.
Hypertonic saline treatment only provides temporary relief and may cause some side effects, like:
- cough
- sore throat
- chest tightness
Dornase-Alfa (Pulmozyme) is a mucus-thinning medication often used by people with cystic fibrosis. You inhale it through a nebulizer. It’s also suitable for people ages 6 and up.
You may lose your voice or develop a rash while on this medication. Other side effects include:
- throat discomfort
- fever
- dizziness
- runny nose
Excess or thick phlegm from time to time is usually not a reason for concern. You may notice it in the morning because it’s accumulated and dried overnight. You may also notice phlegm more if you’re sick, have seasonal allergies, or if you’re dehydrated.
If uncomfortable phlegm becomes a regular occurrence, you might want to make an appointment with your doctor. There are several health conditions that may cause a buildup of phlegm, including:
- acid reflux
- allergies
- asthma
- cystic fibrosis (although this condition is usually diagnosed early in life)
- chronic bronchitis
- other lung diseases
Contact your doctor if your phlegm has been bothering you for a month or longer. Let your doctor know if you have other symptoms, like:
Let your doctor know if you have other symptoms, like:
- coughing up blood
- chest pain
- shortness of breath
- wheezing
It’s important to remember that the body produces mucus at all times. When you notice excess mucus, it’s typically a sign your body is fighting off a cold, allergies, or something more serious.
There are many medicines and remedies tailored to different severity levels and preferences. OTC medication and at-home remedies are great places to start.
While many home remedies don’t have a large body of research on their effectiveness, they typically aren’t harmful to most people. OTC saline solutions and medications, on the other hand, have been researched and found effective in many cases.
Severe cases of excess mucus can usually be treated with prescribed medication.
While excess mucus can often be treated at home, contact your doctor if:
- you’re concerned by how much phlegm you have
- the amount of phlegm has dramatically increased
- you have other symptoms that worry you
Read this article in Spanish.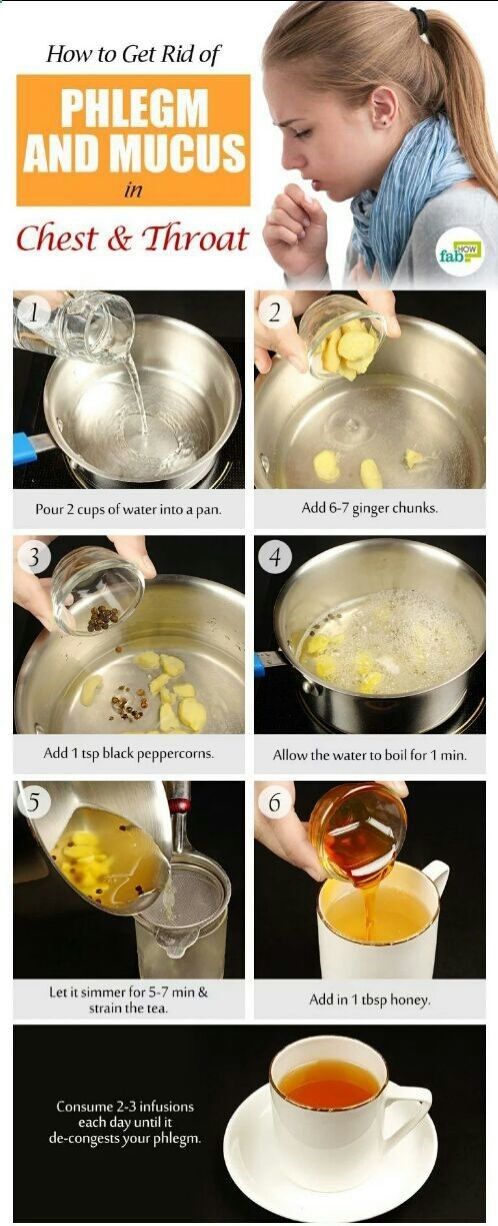
Cough in children - Oleksandrivska Family Clinic
Cough in children! Recommendations ...
Another cough... How often one hears such a complaint from the parents of their little patients to a pediatrician. At the same time, it is the frequency of occurrence of this symptom, and the variety of medicines in pharmacies aimed at ridding the baby of a painful cough, that leads many adults to believe that they can quite cope on their own, acting as the attending physician of their child. And the abundance of advertising and the sale of these drugs without prescription only exacerbates the situation.
So, what is a cough? What diseases of the child can he testify to? And why is it impossible to resort to self-treatment, motivating your choice of a drug with the fact that “they prescribed it for us last time and it helped”?
Cough - a sharp exhalation of air, reflexively relieving the mucous membrane of the respiratory tract from viscous sputum or foreign substances.
The most common symptom in various infections, up to 9They occupy 0% of the causes of coughing. So, coughing can occur when:
- respiratory tract infections (rhinitis, pharyngitis, tonsillitis, bronchitis, pneumonia…)
- and also, in diseases of the ENT organs (with otitis media, a reflex cough often develops, adenoiditis - inflammation of the nasopharyngeal tonsil)
- very specific cough with whooping cough
What other diseases can be accompanied by a cough?
- the leading place among them is bronchial asthma
- occurs in some helminthic infestations, such as ascariasis
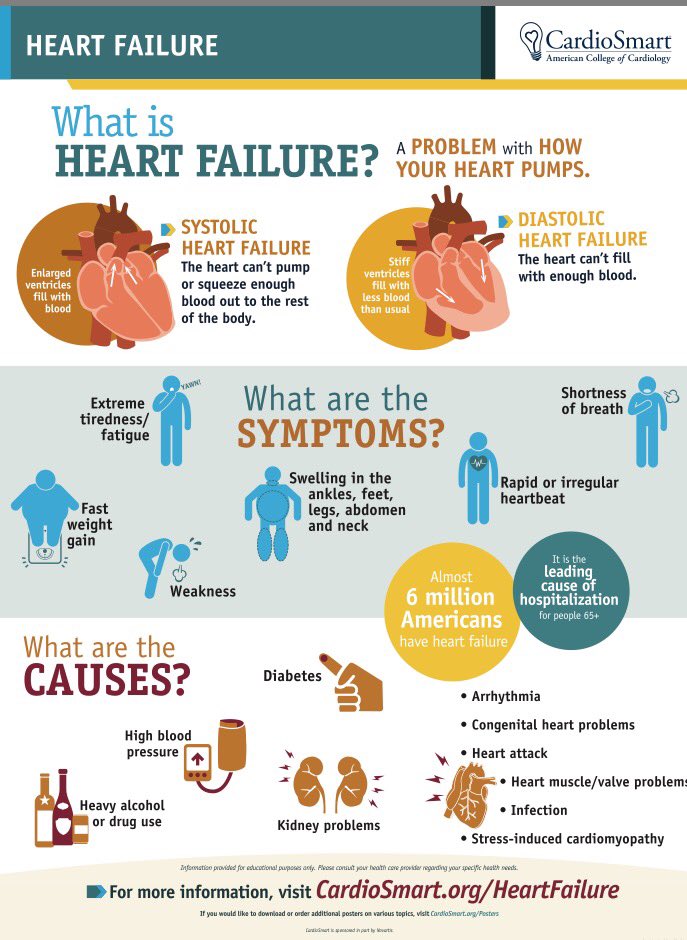
- Cough can be a sign of diseases not related to the bronchopulmonary system, so it can be a leading sign of gastroesophageal reflux disease, or heart defects that occur with signs of heart failure
- cough is a formidable symptom if a foreign body enters the respiratory tract
You can list the diseases indefinitely, it is important to understand that its treatment will also depend on determining the cause of the cough.
Almost each of the listed diseases has its own calling card in the form of a kind of cough, given the characteristics of which it is possible to establish the cause of its occurrence. For example, at:
- various acute infections of the upper respiratory tract - cough is frequent, superficial, accompanied by a rise in body temperature, profuse mucous discharge from the nose, sore throat.
- with obstructive bronchitis, as well as bronchial asthma - paroxysmal cough, accompanied by wheezing, shortness of breath and wheezing, which can be heard at a distance
- with stenosing laryngotracheitis - breathing is difficult, the cough becomes "barking", rough, the voice is hoarse, it may disappear completely
- with a foreign body in the respiratory tract - against the background of complete well-being, a paroxysmal cough suddenly appears, with a low sound at the beginning and a whistling high sound at the end. An indication that before the onset of such a cough the child played with small objects can help in the diagnosis.

- The hallmark of such an infectious disease as whooping cough is a paroxysmal cough, the tremors of which follow one after another, at the end of the attack there is a loud noisy breath. The face turns purple, may be accompanied by vomiting.
- with adenoiditis - cough, mostly in the morning or after sleep, against the background of significantly difficult nasal breathing, with profuse, mucopurulent discharge. The child breathes with an open mouth, in a dream - snores.
- cough in gastroesophageal reflux disease is associated with frequent regurgitation in the first year of life, later on with frequent vomiting, belching and abdominal pain.
So, the characteristics of a cough can tell a lot about the cause of its occurrence, but only a pediatrician can correctly assess the child's condition and determine the disease that led to the appearance of a cough. In what cases is a doctor's call obligatory and urgent?
- for cough accompanied by shortness of breath (rapid breathing, retraction of intercostal spaces)
- when combined with cough and fever in a child
- when a baby coughs in the first year of life
- if sputum is green or bloody
- for prolonged cough, lasting more than 10-14 days
- if the cough appeared suddenly, against the background of complete well-being (especially if the child played with small toys or ate shortly before it appeared)
It should be borne in mind that after examining the child and talking with the parents, the pediatrician may need additional research methods, starting with laboratory: a general blood test and tests to determine antibodies to a particular pathogen, swabs from the nose and throat for flora, sputum culture on the flora (to determine the exact diagnosis of respiratory infections).

In addition, it may be necessary to conduct a number of instrumental examination methods: spirography with the determination of the function of external respiration (to exclude bronchial asthma), ECG and ultrasound of the heart (to exclude heart defects), chest x-ray (to exclude pneumonia).
But now, the diagnosis is established, and the doctor prescribes treatment. Let's talk about the most prescribed groups of drugs, but let's start, as always, with regime moments.
- The regimen should be at home, but it is not necessary to limit the child in his physical activity, since movements stimulate sputum discharge and reduce the time of illness.
- Be sure to drink, increasing the amount of water the child usually drinks by 30% - 50%.
- Humidification is also a must! Achieved with the help of humidifiers. If you don’t have such a “miracle machine”, don’t worry, you can achieve the same effect with wet laundry (hang wet bedding on batteries).

- Postural drainage is recommended to facilitate expectoration of sputum. After inhalation, the child lies on his stomach, his head and chest are tilted slightly lower, an adult taps on the back of the child with his fingers (in children of the first year of life) or with the edge of his palm (in older children).
- And remember! After the child recovers from bronchitis or pneumonia, a course of chest massage is mandatory.
Drug treatment of cough is prescribed only if the cough significantly disturbs the child's condition and in any case begins with the elimination of the cause that caused it. Medicines can be prescribed for dry, paroxysmal, unproductive cough, which significantly changes the child's well-being for the worse. Most often, such a cough is caused by the presence of thick, viscous sputum and a violation of its removal from the bronchial mucosa. Therefore, the purpose of prescribing drugs in this case is to thin the sputum and facilitate its excretion.
That is, the efforts of the pediatrician will be aimed at transferring a dry cough into a productive (wet). Treatment of wet cough most often does not require the use of drug therapy. Exceptions are cases of intense wet cough, exhausting the child, accompanied by vomiting, sleep disturbance, or when there is a threat of aspiration.
By clicking on the button you can make an appointment with a specialist!
Now let's move on to the main medicines that can be prescribed by a pediatrician for diseases accompanied by a cough in a child:
- Perhaps one of the most effective cough suppressants is moisturizing the mucous membranes. It is achieved by inhalation with saline or in combination with another drug (as prescribed by a doctor). Moisturizing the mucosa leads to a decrease in its irritation, liquefaction of sputum and facilitates its removal. Inhalations can be carried out using various types of inhalers. Remember that inhalations using boiling water in children are not allowed! Currently, nebulizers are becoming increasingly popular, they are easy to use, are used in children from the first year of life, with their help, the medicinal substance in the form of an aerosol of small particles reaches the most distant parts of the bronchi.

- For coughs associated with respiratory infections of the upper respiratory tract, so-called enveloping agents have proven themselves well. These are various means for resorption in the oral cavity, teas, syrups, their use is aimed at the appearance of a protective layer of the drug components on the oral mucosa, as a result of which its irritation is reduced.
- Antitussives (tusuprex, libexin, synecode) are designed to suppress the cough center in the central nervous system. In children, their scope is very limited, mainly in cases of whooping cough, especially in children of the first years of life.
- Mucolytics (ACC, ambrohexal, carbocysteine) are designed to thin the sputum, practically without affecting its volume. They are used for dry, unproductive cough to convert it into a productive one, and to facilitate sputum discharge. They can be used not only as drugs used by mouth, but also for inhalation. It is important to remember that a drug such as ACC can increase bronchospasm, so it should not be used for obstructive bronchitis.

- Expectorants work by reducing the viscosity of sputum while increasing its volume. These mainly include preparations based on medicinal herbs (marshmallow, elecampane, coltsfoot, wild rosemary, oregano, licorice). Remember that the natural composition of such products does not indicate their complete safety, and in children, especially in the first years of life, there is a high risk of developing allergic reactions. And the thermopsis herb enhances the gag and cough reflexes, which, combined with increased sputum volume, can lead to aspiration in young children.
- Bronchodilators (berodual, salbutamol) used to reduce the effects of bronchospasm, with obstructive bronchitis or bronchial asthma, inhaled or through a nebulizer
- Anti-inflammatory drugs - used to reduce inflammation of the respiratory mucosa. Of the funds in this group, "erespal" is recommended for use in children.
And many, many other drugs are produced by the pharmacological industry to relieve the symptom of a number of diseases, such as cough.
To understand all this diversity, and prescribe the necessary drug after clarifying the diagnosis, only an experienced pediatrician can. Do not self-medicate! Call Alexandrovskaya Family Clinic and we will help you cope with your child's cough!
Author: Kosolapov Alexander Nikolaevich
Head physician
Back to list
How to remove sputum from the lungs during an illness?
The most vulnerable organ in the period of coronavirus is our lungs. We tell you how to help them safely and quickly: remove phlegm, reduce inflammation and speed up recovery.
Vera Ermakova
Normally, the lungs are a self-cleaning system and are able to cope with the effects of pollution from the external environment. However, if we constantly expose ourselves to dangerous effects - for example, during active or passive smoking or inhaling polluted air - the lungs simply do not have time to remove dangerous mucus. The sputum that accumulates inside our respiratory organs attracts bacteria and other pathogenic microorganisms, which in turn can contribute to the development of various diseases, including very dangerous ones.
The sputum that accumulates inside our respiratory organs attracts bacteria and other pathogenic microorganisms, which in turn can contribute to the development of various diseases, including very dangerous ones.
If you or someone close to you smokes (and you constantly inhale cigarette smoke), live in a city with polluted air, or use toxic substances at work or at home, you may need to help your lungs. We tell you how you can clean the respiratory organs at home and make them healthier and more resilient.
Do not self-medicate! In our articles, we collect the latest scientific data and the opinions of authoritative health experts. But remember: only a doctor can diagnose and prescribe treatment.
Inhalation
Warming the lungs with warm (never hot!) steam can facilitate the separation of sputum and reduce inflammation in the tissues. What's more, inhaling water vapor brings immediate relief and helps people with respiratory problems breathe. But it is important to remember that inhalation is a temporary solution that does not replace full-fledged therapy.
But it is important to remember that inhalation is a temporary solution that does not replace full-fledged therapy.
Controlled Cough
Controlled Cough can help clear phlegm and mucus through the airways. Doctors especially recommend it to patients suffering from chronic obstructive pulmonary disease, however, in other diseases accompanied by sputum accumulation, it may be useful.
- Sit on a chair, back relaxed, both feet on the floor;
- Place your hands on your stomach;
- Inhale slowly through the nose;
- Exhale slowly, leaning forward, pressing your hands to your stomach;
- Cough two or three times while exhaling with your mouth open;
- Inhale slowly through the nose.
- After a short rest, the exercise can be repeated.
( See also: Pneumonia or SARS? 9 important differences)
Postural Drainage
These exercises are also suitable for those patients who develop breathing problems - shortness of breath, shortness of breath. Of course, in such cases, you should immediately call a doctor, but before he arrives, you can help yourself or a loved one with the help of the exercises below.
Of course, in such cases, you should immediately call a doctor, but before he arrives, you can help yourself or a loved one with the help of the exercises below.
Lying on your back:
- Lie on the floor or bed;
- Place pillows under the thighs so that the chest is lower than the thighs;
- Inhale slowly through your nose and exhale through your mouth. Each exhalation should take twice as long as the inhalation.
- Repeat for several minutes.
Lying on your side:
- Lie on your side with your head on your arm or pillow;
- Place pillows under your thighs;
- Inhale slowly through your nose and exhale through your mouth. Each exhalation should take twice as long as the inhalation.
- Repeat for a few minutes, then repeat on the other side.
Lying on stomach
- Place a pile of pillows on the floor;
- Lie on your stomach on pillows with your thighs higher than your chest;
- Place hands under head for support;
- Inhale slowly through your nose and exhale through your mouth.