What are braxton hicks in pregnancy
Braxton Hicks contractions | Pregnancy Birth and Baby
Braxton Hicks contractions | Pregnancy Birth and Baby beginning of content4-minute read
Listen
If you feel tightening or cramping in your abdomen during your pregnancy, you may be having Braxton Hicks contractions. This is normal and not a sign that you’re ready to give birth.
Braxton Hicks contractions are sometimes called ‘false’ or ‘practice’ contractions.
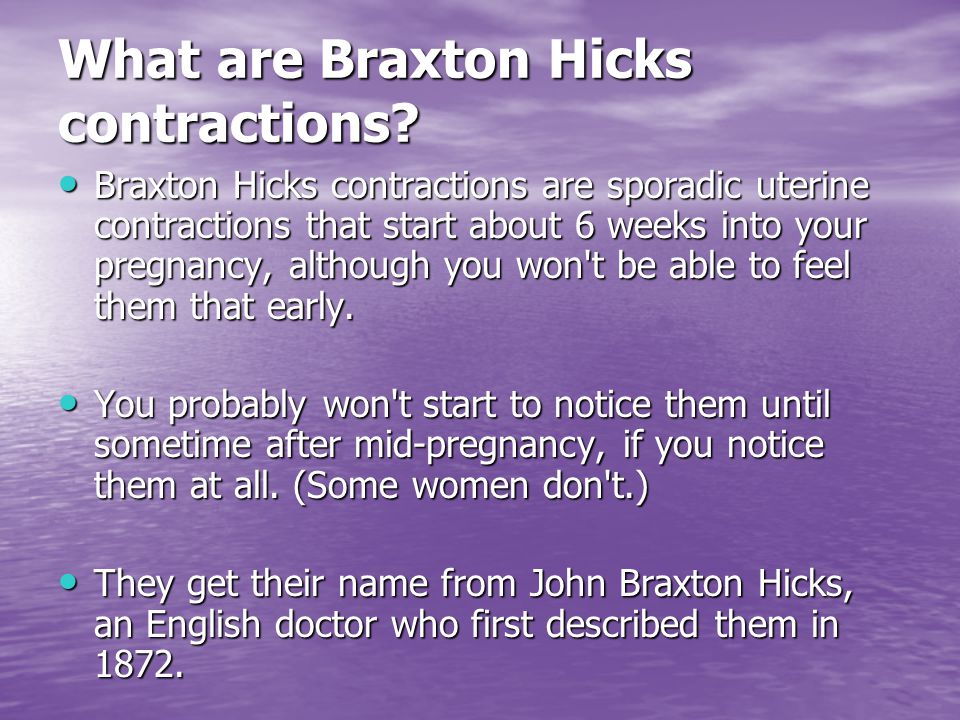
What are Braxton Hicks contractions?
Braxton Hicks contractions are a tightening in your abdomen that comes and goes. They are contractions of your uterus in preparation for giving birth. They tone the muscles in your uterus and may also help prepare the cervix for birth.
Braxton Hicks contractions don’t cause labour and aren’t a sign that labour is beginning.
If you’re not sure whether what you’re experiencing is Braxton Hicks contractions or actual labour, contact your doctor or midwife. They will be able to tell by doing a vaginal examination — if there are no signs that your cervix is changing, it is not labour.
What do they feel like?
Braxton Hicks contractions feel like muscles tightening across your belly, and if you put your hands on your belly when the contractions happen, you can probably feel your uterus becoming hard.
The contractions come irregularly and usually last for about 30 seconds. While they can be uncomfortable, they usually aren’t painful.
If the pain or discomfort of your contractions eases off, they’re probably Braxton Hicks contractions.
When do you get them?
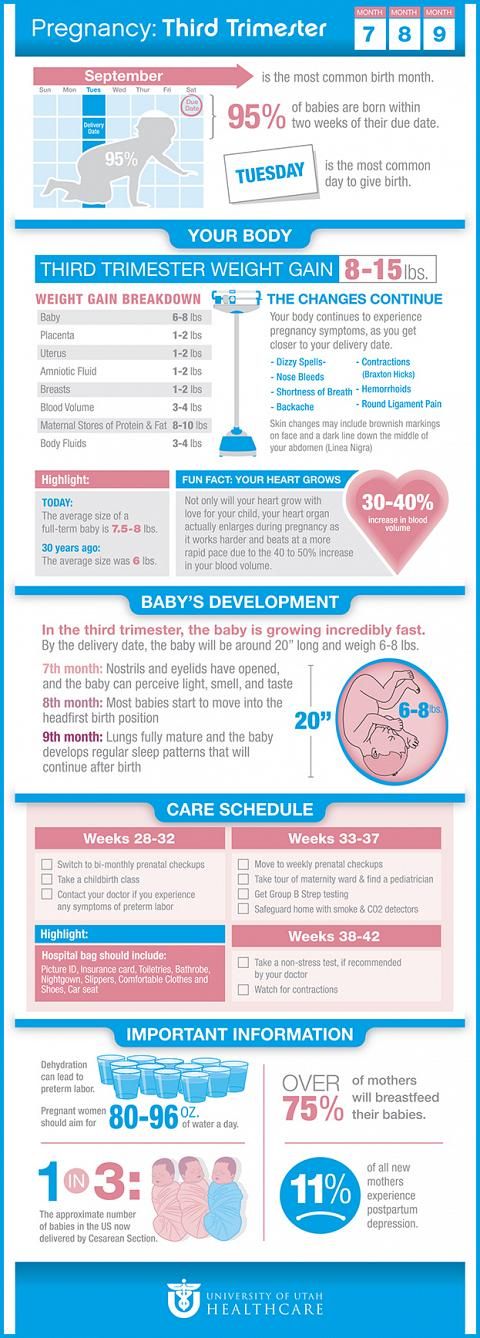
Braxton Hicks contractions occur from early in your pregnancy but you may not feel them until the second trimester. If this is your first pregnancy, you might start to feel them from about 16 weeks. In later pregnancies, you may feel Braxton Hicks contractions more often, or earlier. Some women won’t feel them at all.
Some women won’t feel them at all.
In late pregnancy, you may experience Braxton Hicks contractions more often — perhaps as much as every 10 to 20 minutes. This is a sign that you are preparing for labour — known as prelabour.
How are Braxton Hicks contractions different from labour pain?
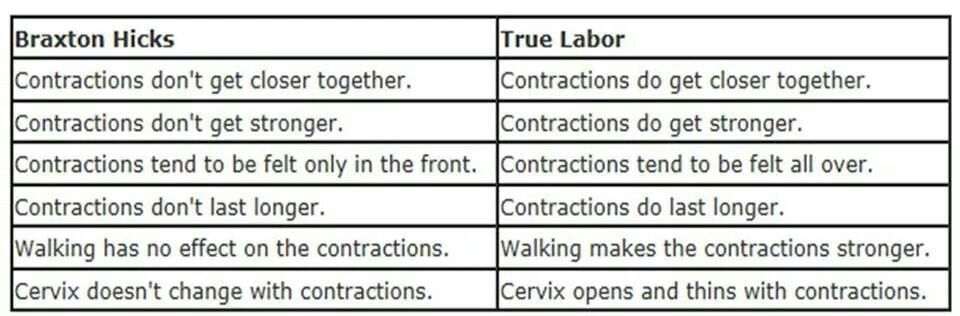
There are some differences between Braxton Hicks contractions and true labour contractions that will help your doctor or midwife decide whether you are in labour:
Braxton Hicks contractions:
- don’t result in your cervix thinning and opening
- usually last for about 30 seconds
- can be uncomfortable, but usually aren’t painful
- come and go at irregular times
- usually occur no more than once or twice an hour (until late in the pregnancy), a few times a day
- usually stop if you change position or activity or go for a walk
- usually go if you have a warm bath or shower
Real labour contractions:
- result in your cervix thinning and opening
- last 30 to 70 seconds
- become very regular
- get closer together
- last longer as time goes by
- get stronger or come more often when you walk
- get stronger over time
Should I call my doctor or midwife?
If you are less than 37 weeks pregnant, contractions can be a sign of premature labour. Contact your doctor or midwife immediately if:
Contact your doctor or midwife immediately if:
- you feel pain, pressure or discomfort in your pelvis, abdomen or lower back
- the contractions become stronger, closer together and more regular
- there is fluid leaking or gushing from your vagina
If you are full-term, you may choose to wait until a bit later in your labour, depending on what you have arranged with your doctor or midwife. If your waters break, or your contractions are strong and 5 minutes apart, it’s time to go to the hospital.
As any stage of pregnancy, you should contact your doctor or midwife immediately if you:
- you have persistent pain in your abdomen
- you have vaginal bleeding
- you notice your baby’s movements have slowed or stopped
- you feel very unwell
If you are in doubt, don’t hesitate to call your doctor or midwife for advice.
How can I ease the discomfort?
Braxton Hicks contractions are normal and don’t need treatment.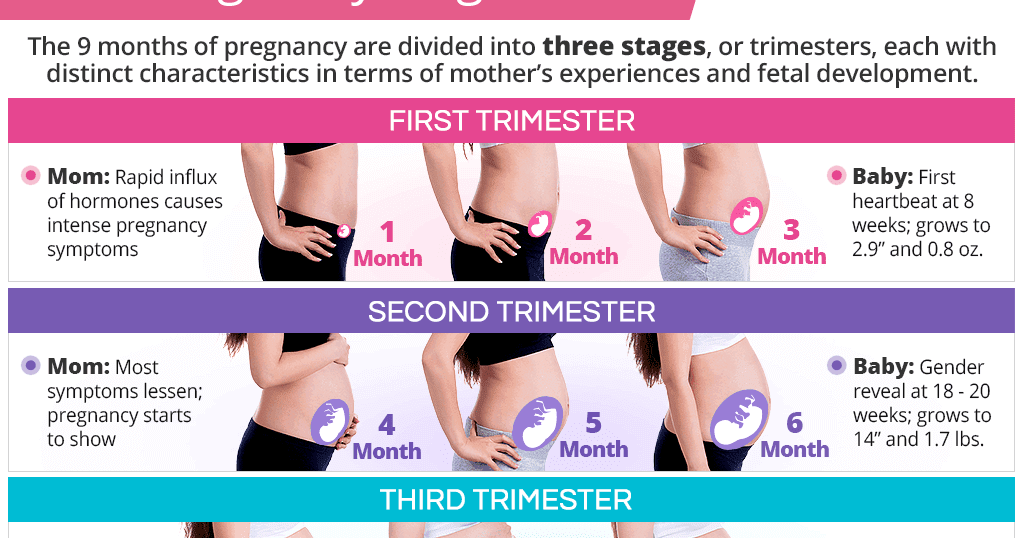 But if you feel uncomfortable, you can try:
But if you feel uncomfortable, you can try:
- lying down
- taking a walk
- relaxing in a warm bath
- having a massage
It may help to practise your breathing exercises during your Braxton Hicks contractions.
Sources:
Raising Children Network (23 weeks pregnant), RANZCOG (Labour and birth), Elsevier Patient Education (Braxton Hicks Contractions)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Health professionals involved in your pregnancy
- Giving birth - stages of labour
- Premature baby
Need more information?
Pregnancy at week 22
By week 22, some parts of your baby’s body are fully formed, while some women experience Braxton Hicks contractions about now.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 35
You'll probably be having lots of Braxton Hicks contractions by now. It's your body's way of preparing for the birth. They should stop if you move position.
Read more on Pregnancy, Birth & Baby website
Giving birth - contractions
Contractions are when the muscles in your uterus tighten and then relax. They occur throughout the later stages of your pregnancy.
Read more on Pregnancy, Birth & Baby website
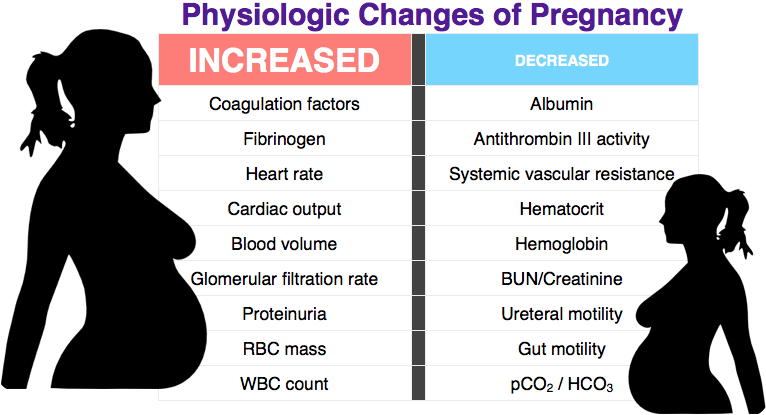
What happens to your body in childbirth
During childbirth, your body's hormones, ligaments and muscles, as well as the shape of your pelvis, all work together to bring your baby safely into the world.
Read more on Pregnancy, Birth & Baby website
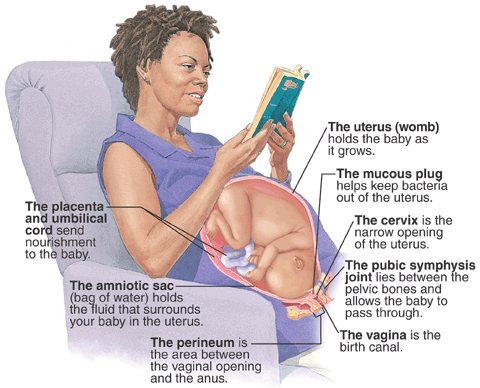
Anatomy of pregnancy and birth - uterus
The uterus is your growing baby’s home during pregnancy. Learn how the uterus works, nurtures your baby and how it changes while you are pregnant.
Read more on Pregnancy, Birth & Baby website
Preterm labour - MyDr.com.au
Going into labour before your 37th week of pregnancy is called preterm labour, or premature labour. Find out what it means for you and your baby.
Read more on myDr website
38 weeks pregnant | Raising Children Network
38 weeks pregnant? In this pregnancy week by week guide, find out how your baby is growing, how your body is changing and how to look after yourself.
Read more on raisingchildren.net.au website
26 weeks pregnant | Raising Children Network
26 weeks pregnant? In this pregnancy week by week guide, find out how your baby is growing, how your body is changing and how to look after yourself.
Read more on raisingchildren.net.au website
Giving birth - early signs of labour
You can know the early signs of labour, even if you cannot predict when your labour will begin. Find out also what to do if something appears to be wrong.
Read more on Pregnancy, Birth & Baby website
Anatomy of pregnancy and birth
From conception to giving birth, a woman's body goes through many physical changes. Learn what happens to your body during pregnancy and labour.
Learn what happens to your body during pregnancy and labour.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Braxton Hicks Contractions - StatPearls
Deborah A. Raines; Danielle B. Cooper.
Raines; Danielle B. Cooper.
Author Information and Affiliations
Last Update: August 8, 2022.
Continuing Education Activity
Braxton-Hicks contractions, also known as prodromal or false labor pains, are contractions of the uterus that typically are not felt until the second or third trimester of the pregnancy. Braxton-Hicks contractions are the body's way of preparing for true labor, but they do not indicate that labor has begun. Because many pregnant patients have not been educated about Braxton-Hicks contractions, they often seek care and undergo unnecessary evaluation for these contractions. This activity reviews the evaluation and management of patients with Braxton-Hicks contractions and highlights the role of the interprofessional team in educating the patient about the condition.
Objectives:
Describe the etiology of Braxton-Hicks contractions.
Review the presentation of a patient with Braxton-Hicks contractions.
Explain how to evaluate a patient with Braxton-Hicks contractions.
Employ strategies to improve interprofessional communication, which will improve outcomes in patients with Braxton-Hicks contractions.
Access free multiple choice questions on this topic.
Introduction
Braxton Hicks contractions are sporadic contractions and relaxation of the uterine muscle. Sometimes, they are referred to as prodromal or “false labor" pains. It is believed they start around 6 weeks gestation but usually are not felt until the second or third trimester of the pregnancy. Braxton Hicks contractions are the body's way of preparing for true labor, but they do not indicate that labor has begun or is going to start.
Braxton Hicks contractions are a normal part of pregnancy. They may be uncomfortable, but they are not painful. Women describe Braxton Hicks contractions as feeling like mild menstrual cramps or a tightening in a specific area of the abdomen that comes and goes. [1][2][3]
[1][2][3]
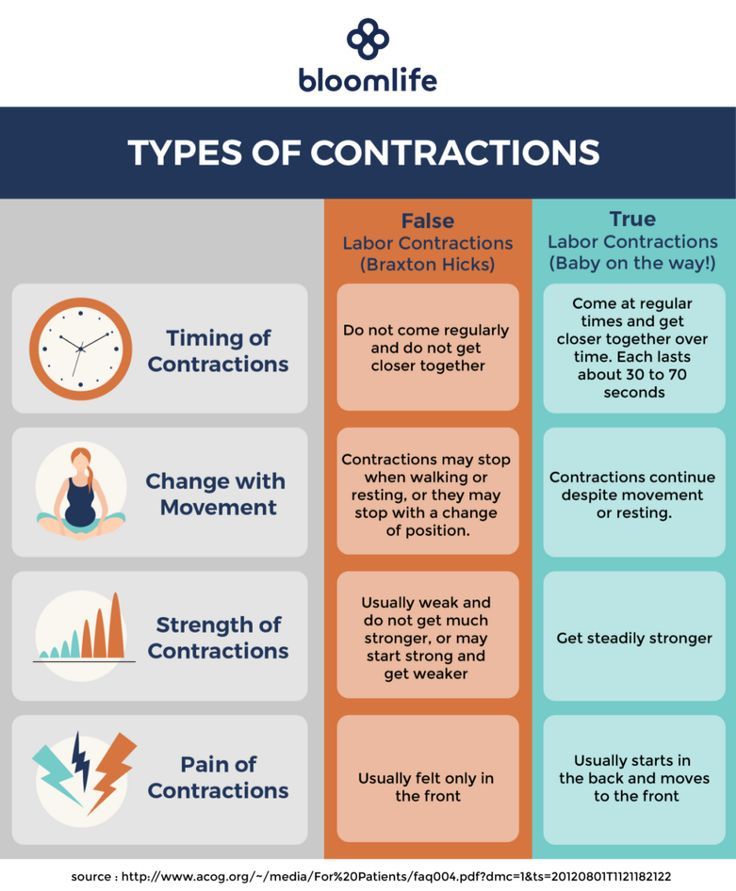
Braxton Hicks contractions can be differentiated from the contractions of true labor. Braxton Hicks contractions are irregular in duration and intensity, occur infrequently, are unpredictable and non-rhythmic, and are more uncomfortable than painful. Unlike true labor contractions, Braxton Hicks contractions do not increase in frequency, duration, or intensity. Also, they lessen and then disappear, only to reappear at some time in the future. Braxton Hicks contractions tend to increase in frequency and intensity near the end of the pregnancy. Women often mistake Braxton Hicks contractions for true labor. However, unlike true labor contractions, Braxton Hicks contractions do not cause dilatation of the cervix and do not culminate in birth.
Etiology
Braxton Hicks contractions are caused when the muscle fibers in the uterus tighten and relax. The exact etiology of Braxton Hicks contractions is unknown. However, there are known circumstances that trigger Braxton Hicks contractions including when the woman is very active, when the bladder is full, following sexual activity, and when the woman is dehydrated. A commonality among all these triggers is the potential for stress to the fetus, and the need for increased blood flow to the placenta to provide fetal oxygenation.[4][5][6]
A commonality among all these triggers is the potential for stress to the fetus, and the need for increased blood flow to the placenta to provide fetal oxygenation.[4][5][6]
Epidemiology
Braxton Hicks contractions are present in all pregnancies. However, each woman's experience is different. Most women become aware of Braxton Hicks contractions in the third trimester, and some women are aware of them as early as the second trimester. Sometimes Braxton Hick contractions occurring near the end of the third trimester of pregnancy are mistaken as the onset of true labor. It is not unusual, especially in a first pregnancy, for a woman to think she is in labor only to be told it is Braxton Hicks contractions and not true labor.
Pathophysiology
Braxton Hicks contractions are thought to play a role in toning the uterine muscle in preparation for the birth process. Sometimes Braxton Hicks contractions are referred to as "practice for labor." Braxton Hicks contractions do not result in dilation of the cervix but may have a role in cervical softening.
The intermittent contraction of the uterine muscle may also play a role in promoting blood flow to the placenta. Oxygen-rich blood fills the intervillous spaces of the uterus where the pressure is relatively low. The presence of Braxton Hicks contractions causes the blood to flow up to the chorionic plate on the fetal side of the placenta. From there the oxygen-rich blood enters the fetal circulation.
History and Physical
When assessing a woman for the presence of Braxton Hicks contractions, there are some key questions to ask. Her response to these questions will assist the healthcare provider to differentiate Braxton Hicks contractions and true labor contractions.[7][8][9]
How often are the contractions? Braxton Hicks contractions are irregular and do not get closer together over time. True labor contractions come at regular intervals, and as time goes on, they get closer together and stronger.
How long are the contractions? Braxton Hicks contractions are unpredictable.
 They may last less than 30 seconds or up to 2 minutes. True labor contractions last between 30 to less than 90 seconds and become longer over time.
They may last less than 30 seconds or up to 2 minutes. True labor contractions last between 30 to less than 90 seconds and become longer over time.How strong are the contractions? Braxton Hicks contractions are usually weak and either stay the same or become weaker and then disappear. True labor contractions get stronger over time.
Where are the contractions felt? Braxton Hicks contractions are often only felt in the front of the abdomen or one specific area. True labor contractions start in the midback and wrap around the abdomen towards the midline.
Do the contractions change with movement? Braxton Hicks contractions may stop with a change in activity level or as the woman changes position. If she can sleep through the contraction, it is a Braxton Hicks contraction. True labor contractions continue and may even become stronger with movement or position change.
During the physical assessment, the provider may palpate an area of tightening or a "spasm" of the uterine muscle, but the presence of a uterine contraction in the uterine fundus is not palpable. The woman will be assessed for the presence of uterine bleeding or rupture of the amniotic membrane. An examination of the cervix reveals no change in effacement or dilatation as a result of the Braxton Hicks contractions.
The woman will be assessed for the presence of uterine bleeding or rupture of the amniotic membrane. An examination of the cervix reveals no change in effacement or dilatation as a result of the Braxton Hicks contractions.
Evaluation
There are no laboratory or radiographic tests to diagnose Braxton Hicks contractions. Evaluation of the presence of Braxton Hicks contractions is based on an assessment of the pregnant woman's abdomen, specifically palpating the contractions.
Treatment / Management
By the midpoint of pregnancy, the woman and provider should discuss what the woman may experience during the remainder of the pregnancy. Braxton Hicks contractions are one of the normal events a woman may experience. Teaching her about Braxton Hicks contractions will help her to be informed and to decrease her anxiety if they occur.[10][11][12]
There is no medical treatment for Braxton Hicks contractions. However, taking action to change the situation that triggered the Braxton Hicks contractions is warranted. Some actions to ease Braxton Hicks contractions include:
Some actions to ease Braxton Hicks contractions include:
Changing position or activity level: if the woman has been very active, lie down; if the woman has been sitting for an extended time, go for a walk.
Relaxing: take a warm bath, get a massage, read a book, listen to music, or take a nap.
Drinking water to rehydrate.
If these actions do not lessen the Braxton Hicks contractions or if the contractions continue and are becoming more frequent or more intense, the patient's healthcare provider should be contacted.
Also, if any of the following are present the healthcare provider should be contacted immediately:
Vaginal bleeding
Leaking of fluid from the vagina
Strong contractions every 5-minutes for an hour
Contractions that the woman is unable to "walk through"
A noticeable change in fetal movement, or if there are less than ten movements every 2 hours.
Differential Diagnosis
Amenorrhea
Ascites
Full bladder
Hematometra
Nausea
Ovarian cysts
Pseudocyesis
Uterine fibroids
Vomiting
Pearls and Other Issues
In addition to Braxton Hicks contractions, there are other causes of abdominal pain during pregnancy. Some normal reasons for abdominal pain during pregnancy, in addition to Braxton Hicks contractions and true labor contractions, include:
Round ligament pain or a sharp, jabbing feeling felt in the lower abdomen or groin area on one or both sides.
Higher levels of progesterone can cause excess gas during pregnancy.
Constipation may be a source of abdominal pain.
Circumstances in which abdominal pain is a sign of a serious condition that requires immediate medical attention include:
Ectopic pregnancy.

Placental abruption. A key symptom of placental abruption is intense and constant pain that causes the uterus to become hard for an extended period without relief.
Urinary tract infection symptoms include pain and discomfort in the lower abdomen as well as burning with urination.
Preeclampsia is a condition of pregnancy occurring after 20-weeks gestation and characterized by high blood pressure and protein in the urine. Upper abdominal pain, usually under the ribs on the right side, can be present in preeclampsia.
If a woman is unsure if she is experiencing Braxton Hicks contractions or another condition, a discussion with a healthcare provider is needed. The healthcare provider may recommend a visit to the office setting or labor and delivery for an examination by a healthcare professional to determine the cause of the abdominal pain.
Enhancing Healthcare Team Outcomes
Braxton hicks contractions are fairly common and it is important for the emergency department physician labor & delivery nurse and nurse practitioner to be aware that this is not true labor.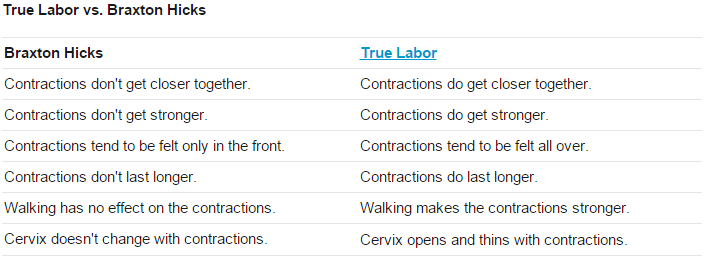 If there is any doubt, the obstetrician should be consulted. However, at the same time, the onus is on the healthcare workers to rule out true labor. Other organic disorders like appendicitis, urinary tract infection or cholecystitis must also be ruled out. With the right education, patients with braxton hicks contraction will not needlessly rush to the ED every time they sense a contraction.
If there is any doubt, the obstetrician should be consulted. However, at the same time, the onus is on the healthcare workers to rule out true labor. Other organic disorders like appendicitis, urinary tract infection or cholecystitis must also be ruled out. With the right education, patients with braxton hicks contraction will not needlessly rush to the ED every time they sense a contraction.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Hanghøj S. When it hurts I think: Now the baby dies. Risk perceptions of physical activity during pregnancy. Women Birth. 2013 Sep;26(3):190-4. [PubMed: 23711581]
- 2.
MacKinnon K, McIntyre M. From Braxton Hicks to preterm labour: the constitution of risk in pregnancy. Can J Nurs Res. 2006 Jun;38(2):56-72. [PubMed: 16871850]
- 3.
Dunn PM. John Braxton Hicks (1823-97) and painless uterine contractions.
 Arch Dis Child Fetal Neonatal Ed. 1999 Sep;81(2):F157-8. [PMC free article: PMC1720982] [PubMed: 10448189]
Arch Dis Child Fetal Neonatal Ed. 1999 Sep;81(2):F157-8. [PMC free article: PMC1720982] [PubMed: 10448189]- 4.
Lockwood CJ. The diagnosis of preterm labor and the prediction of preterm delivery. Clin Obstet Gynecol. 1995 Dec;38(4):675-87. [PubMed: 8616965]
- 5.
Arduini D, Rizzo G, Rinaldo D, Capponi A, Fittipaldi G, Giannini F, Romanini C. Effects of Braxton-Hicks contractions on fetal heart rate variations in normal and growth-retarded fetuses. Gynecol Obstet Invest. 1994;38(3):177-82. [PubMed: 8001871]
- 6.
Kofinas AD, Simon NV, Clay D, King K. Functional asymmetry of the human myometrium documented by color and pulsed-wave Doppler ultrasonographic evaluation of uterine arcuate arteries during Braxton Hicks contractions. Am J Obstet Gynecol. 1993 Jan;168(1 Pt 1):184-8. [PubMed: 8420324]
- 7.
Lockwood CJ, Dudenhausen JW. New approaches to the prediction of preterm delivery. J Perinat Med. 1993;21(6):441-52.
 [PubMed: 8006770]
[PubMed: 8006770]- 8.
Rhoads GG, McNellis DC, Kessel SS. Home monitoring of uterine contractility. Summary of a workshop sponsored by the National Institute of Child Health and Human Development and the Bureau of Maternal and Child Health and Resources Development, Bethesda, Maryland, March 29 and 30, 1989. Am J Obstet Gynecol. 1991 Jul;165(1):2-6. [PubMed: 1677235]
- 9.
Oosterhof H, Dijkstra K, Aarnoudse JG. Fetal Doppler velocimetry in the internal carotid and umbilical artery during Braxton Hicks' contractions. Early Hum Dev. 1992 Aug;30(1):33-40. [PubMed: 1396288]
- 10.
Oosterhof H, Dijkstra K, Aarnoudse JG. Uteroplacental Doppler velocimetry during Braxton Hicks' contractions. Gynecol Obstet Invest. 1992;34(3):155-8. [PubMed: 1427416]
- 11.
Bower S, Campbell S, Vyas S, McGirr C. Braxton-Hicks contractions can alter uteroplacental perfusion. Ultrasound Obstet Gynecol. 1991 Jan 01;1(1):46-9. [PubMed: 12797102]
- 12.

Hill WC, Lambertz EL. Let's get rid of the term "Braxton Hicks contractions". Obstet Gynecol. 1990 Apr;75(4):709-10. [PubMed: 2314790]
Braxton-Hicks contractions or false labor contractions are irregular contractions and relaxation of the muscles of the uterus as a way of preparing for true labor. They are thought to start around 6 weeks of gestation but are not usually felt until the 2nd or 3rd trimester.
False contractions are a normal part of pregnancy. They may be uncomfortable, but not painful. Women describe them as a feeling that feels like mild menstrual cramps or tightness in a specific area of the abdomen that quickly resolves.
They are also irregular in duration and intensity, occur infrequently, are unpredictable and not rhythmic, and are more uncomfortable than painful.
Braxton Hicks contractions tend to increase in frequency and intensity towards the end of pregnancy. Women often mistake Braxton Hicks contractions for real labor. However, unlike real contractions, they do not dilate the cervix and result in the birth of a baby.
Women often mistake Braxton Hicks contractions for real labor. However, unlike real contractions, they do not dilate the cervix and result in the birth of a baby.
Braxton Hicks contractions occur when the muscle fibers of the uterus contract and relax. The exact etiology of Braxton Hicks contractions is unknown. However, there are circumstances that can cause them:
- when the woman is very active,
- when the bladder is full,
- after sexual activity,
- when the woman is dehydrated.
Common among all these circumstances is the potential stress on the fetus and the need for increased blood flow to the placenta to provide oxygen to the fetus.
- Change position or activity level: if you were very active, lie down; if you have been sitting for a long time, go for a walk.
- Relax: take a warm bath, massage, read a book, listen to music or take a nap.
If you have Braxton Hicks contractions or if they continue and become more frequent and intense, you should see your doctor.
When assessing for Braxton Hicks contractions, there are a few key questions to ask yourself. We have prepared for you a table with questions, the answers to which will help you understand what kind of contractions you have:
| Braxton Higgs contractions | Real labor pains | |
|---|---|---|
| How often do contractions occur? | Irregular and do not increase over time. | Occurs at regular intervals and gets stronger over time. |
| How long do contractions last? | Unpredictable. They can last less than 30 seconds or up to 2 minutes. | Lasts 30 to 90 seconds and gets longer over time. |
| How strong are the contractions? | Usually weak and either stay the same or get weaker and then disappear. | Increase over time. |
| Where do contractions feel? | Often only felt in the front of the abdomen or in one specific area. | Begin in the middle of the back and wrap around the belly towards the midline. |
| Do abbreviations change with movement? | May stop if activity level changes or if woman's position changes. | Continue and may even get worse with movement or change of position. |
Back to article list
False contractions. What are false contractions?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
False contractions are irregular uterine contractions that cause pain but no cervical dilatation. Occur in late pregnancy, more often after the 20th week. The main manifestations: cramping pains in the lower abdomen or in the lumbar region without a clear periodicity. Methods for diagnosing this condition are cardiotocography, examination of the cervix in mirrors with the determination of its degree of maturity, ultrasound of the genitals with an assessment of uterine blood flow. Specific treatment depends on the duration of pregnancy and the causes of this condition.
Methods for diagnosing this condition are cardiotocography, examination of the cervix in mirrors with the determination of its degree of maturity, ultrasound of the genitals with an assessment of uterine blood flow. Specific treatment depends on the duration of pregnancy and the causes of this condition.
ICD-10
O47 False contractions
- Causes
- Pathogenesis
- Symptoms of false contractions
- Diagnostics
- Treatment of false contractions
- Prognosis and prevention
- Prices for treatment
General
False contractions are otherwise called "training" or "Braxton-Hicks contractions" after the English doctor who first described this phenomenon. Back in 1872, he noted that many women feel such contractions long before the expected birth. This caused fear and confusion among women in connection with the timing of real childbirth, so J. Braxton Hicks began to warn pregnant women in advance about the possibility of such a phenomenon. False contractions normally occur in 33% of pregnant women. Multiparous women feel false contractions at an earlier date compared to primiparas.
Braxton Hicks began to warn pregnant women in advance about the possibility of such a phenomenon. False contractions normally occur in 33% of pregnant women. Multiparous women feel false contractions at an earlier date compared to primiparas.
false contractions
Causes
The contractile activity of the uterus depends on the work of the pituitary gland. In the later stages (from 37 weeks), the preparation of the body for future childbirth gradually begins, hormones that have contractile ability (oxytocin, cortisone-like substances) are released. Under their influence, contractions periodically occur in the myometrium. In early gestation, the causes of false contractions can be:
- Pathology of the pituitary and endocrine glands. An increased content of thyroid, adrenal, and posterior pituitary hormones in the blood can increase the readiness of muscle cells to contract. An increase in the level of prolactin provokes excessive formation of male steroid hormones in the female body, which can also lead to false contractions.
- Uterine hypertonicity. The increased readiness of the myometrium for premature contractions can be caused by various factors. Both hormonal causes (reduced progesterone levels) and changes in the fetal-uterine blood flow (like hypoxia of the uterine muscles) play a role here.
- Underdevelopment of the neuro-receptor apparatus of the uterus. The ratio of the number of receptors for estrogen and progesterone is not constant and normally changes at different stages of pregnancy. A pathological increase in the number of estrogen receptors contributes to the occurrence of premature uterine contractions.
The risk group for the occurrence of false contractions in early pregnancy includes patients with preeclampsia, congenital anomalies of the reproductive apparatus and immune diseases. The development of false contractions is facilitated by overstretching of the uterus during multiple pregnancy or the presence of a postoperative scar. Very often, pathological contractile activity of the muscular layer of the uterus is observed with intrauterine infection and isthmic-cervical insufficiency.
Pathogenesis
In the last month of pregnancy, the contractile activity of the myometrium increases. The synthesis of biologically active substances and hormones that stimulate the tension of muscle fibers increases. The number of excitatory uterine contractions of nerve impulses increases. In the brain, a focus coordinating labor activity is formed - the “dominant of childbirth”.
Periodically occurring during this period, false contractions help maintain normal uterine tone and stimulate fetoplacental blood flow. The vessels of the placenta do not have their own muscle layer, periodic uterine contractions displace venous blood from them, which is replaced by arterial blood. Thus, the fetus receives more oxygen and nutrients.
false contractions
Symptoms of false contractions
False contractions are felt by a pregnant woman as an irregular tension in the lower abdomen.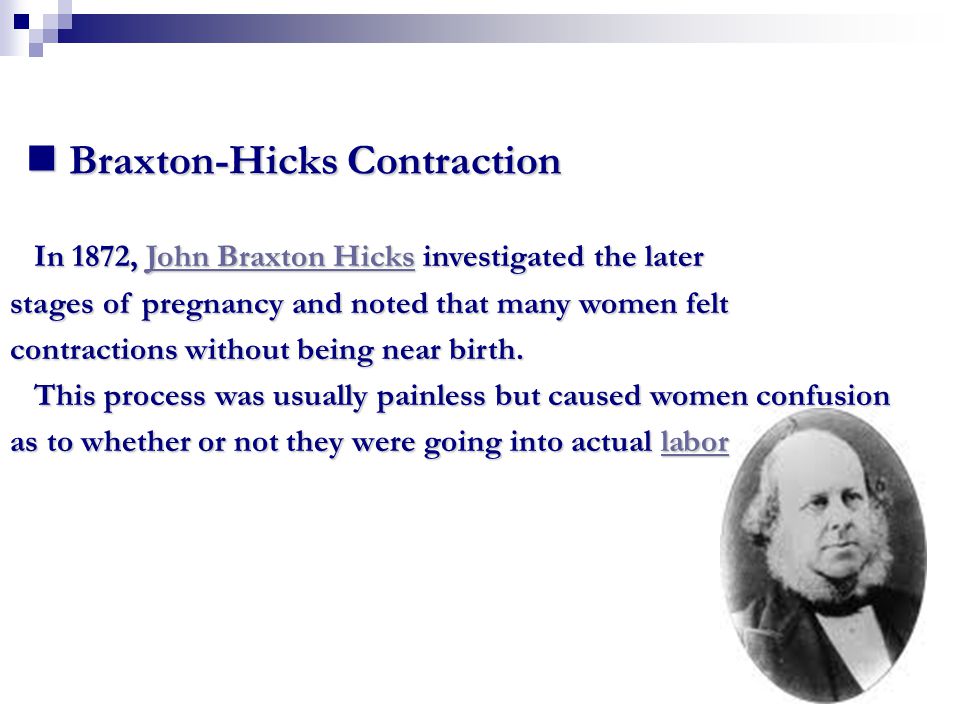 The sensations may resemble discomfort during menstruation. Pains of a pulling, aching nature can spread to the lumbar region, sometimes they are accompanied by a feeling of fullness in the genital area. The abdomen during the period of the fight becomes dense, rounded, "hardens". With a high pain threshold, Braxton-Hicks contractions may not be felt at all and may be detected by chance, for example, during a doctor's appointment.
The sensations may resemble discomfort during menstruation. Pains of a pulling, aching nature can spread to the lumbar region, sometimes they are accompanied by a feeling of fullness in the genital area. The abdomen during the period of the fight becomes dense, rounded, "hardens". With a high pain threshold, Braxton-Hicks contractions may not be felt at all and may be detected by chance, for example, during a doctor's appointment.
False contractions begin and end suddenly, they have no clear rhythm. Attacks often develop at night, when the pituitary gland increases the production of oxytocin. They are distinguished from true contractions by the fact that the force of contractions does not increase over time, and the intervals between contractions do not decrease. False contractions disappear with a change in position or cessation of physical activity. They may appear and end several times a day.
Diagnostics
The presence of Braxton-Hicks training contractions can be suspected already on the basis of the patient's complaints.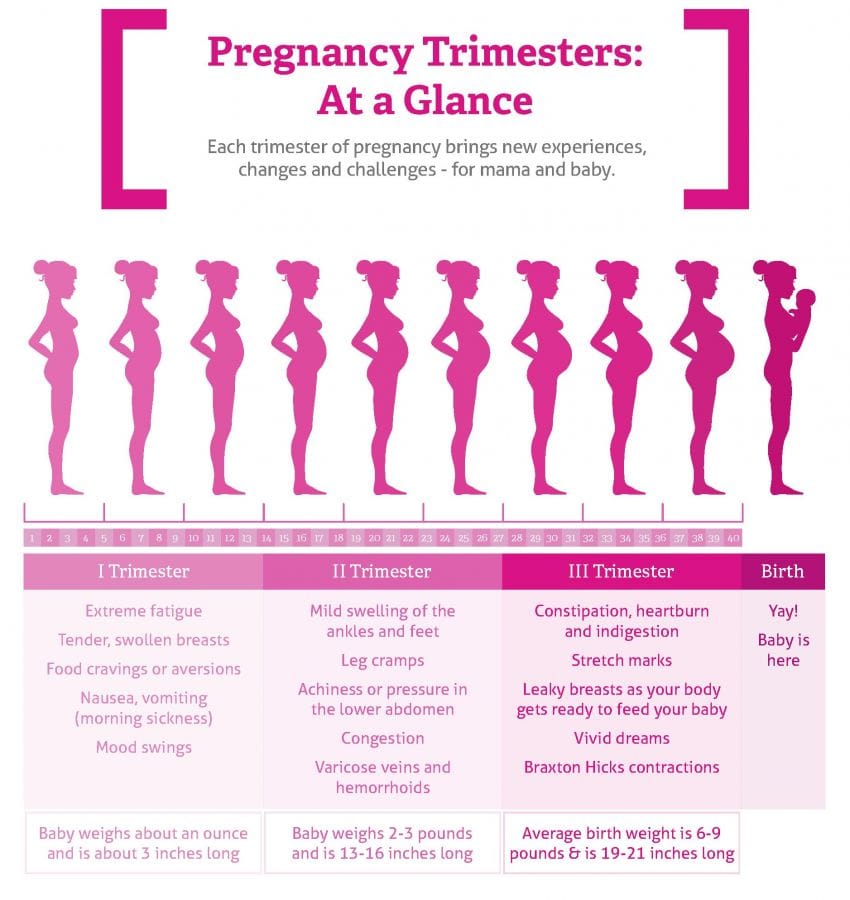 During the examination, the tone of the uterus is assessed, which often tenses in response to palpation. Be sure to conduct an examination in the mirrors to determine the degree of maturity of the cervix and its length. If it is shorter than 25 mm, then this is considered a risk of preterm labor and requires appropriate therapy (installation of a pessary, circling).
During the examination, the tone of the uterus is assessed, which often tenses in response to palpation. Be sure to conduct an examination in the mirrors to determine the degree of maturity of the cervix and its length. If it is shorter than 25 mm, then this is considered a risk of preterm labor and requires appropriate therapy (installation of a pessary, circling).
From the genital tract of a pregnant woman, a smear is taken for the flora, a nitrazine test is performed to exclude spotting, infection, or leakage of amniotic fluid. To assess the general condition of the expectant mother, laboratory tests are carried out, such as a general analysis of urine and blood, a biochemical study, an assessment of the excretory function of the kidneys (Zimnitsky's test). The patient consults a general practitioner, if necessary, a nephrologist and endocrinologist.
As special studies, methods for assessing the condition of the uterus and fetus are used. It is very important to examine the placenta for functional consistency, location and intensity of blood flow. For this, the following is carried out:
It is very important to examine the placenta for functional consistency, location and intensity of blood flow. For this, the following is carried out:
- Cardiotocography. At the same time, it allows you to track the contractile activity of the uterus, the presence of contractions and the state of the fetal heart activity. Based on the results, it can be decided whether the fetus suffers from a lack of oxygen during contractions.
- Ultrasound of fetal and uterine blood flow. During the study, anomalies of the vascular bed of the placenta, uterus, and fetus are revealed. Sometimes there is a premature "aging" of the placenta, because of this, the level of blood circulation decreases, hypoxic conditions may develop in the fetus or in the myometrium, which cause abnormal contractions.
Cardiotocography
Treatment of false contractions
Treatment tactics are selected depending on the gestational age at which false contractions occurred. Starting from 37 weeks of gestation, with normal tests, the treatment of false contractions is not carried out. From 22 to 37 weeks, therapy is primarily aimed at eliminating the cause that caused uterine contractions. With endocrine pathology, hormonal correction is prescribed, maintaining an adequate level of progesterone, as the main prolonging pregnancy hormone.
Starting from 37 weeks of gestation, with normal tests, the treatment of false contractions is not carried out. From 22 to 37 weeks, therapy is primarily aimed at eliminating the cause that caused uterine contractions. With endocrine pathology, hormonal correction is prescribed, maintaining an adequate level of progesterone, as the main prolonging pregnancy hormone.
With an increased tendency of the uterus to contractions, tocolytic (relaxing myometrium) therapy is performed. A proven remedy is magnesium sulfate (magnesia). When administered intravenously and intramuscularly, it has an anticonvulsant effect. In addition, the drug prevents fluid retention in the body of a pregnant woman and activates the fetal-uterine blood flow. Sometimes the introduction of a drug is used as a diagnostic test: false contractions stop at the same time, but it does not affect true contractions.
Selective beta-agonists (hexoprenaline), inhibitors of prostaglandin synthesis (indomethacin) and antispasmodics (drotaverine) are also used from tocolytics according to indications. For the prevention of intrauterine fetal hypoxia and circulatory disorders in the uterus and placenta, cytoprotectors and antiplatelet agents (pentoxifylline) are prescribed.
For the prevention of intrauterine fetal hypoxia and circulatory disorders in the uterus and placenta, cytoprotectors and antiplatelet agents (pentoxifylline) are prescribed.
Prognosis and prevention
False contractions do not lead to the onset of labor, so the prognosis for pregnancy is favorable. In most cases, false contractions are part of the normal process of preparing for childbirth. If they are caused by a complicated course of pregnancy, it is important to be examined in time and carry out adequate treatment. To prevent false contractions, a pregnant woman is advised to avoid excessive physical exertion and stressful situations. Also, for the coordinated work of the pituitary gland and endocrine glands, it is necessary to observe the daily regimen and good sleep.
You can share your medical history, what helped you in the treatment of false contractions.
Sources
- Problems of false contractions in modern obstetrics / Buzumova Zh.