Hormone headaches during pregnancy
Headaches during pregnancy | Pregnancy Birth and Baby
Headaches during pregnancy | Pregnancy Birth and Baby beginning of content9-minute read
Listen
If you have a severe headache during pregnancy that is not usual for you, seek medical help immediately.
Key facts
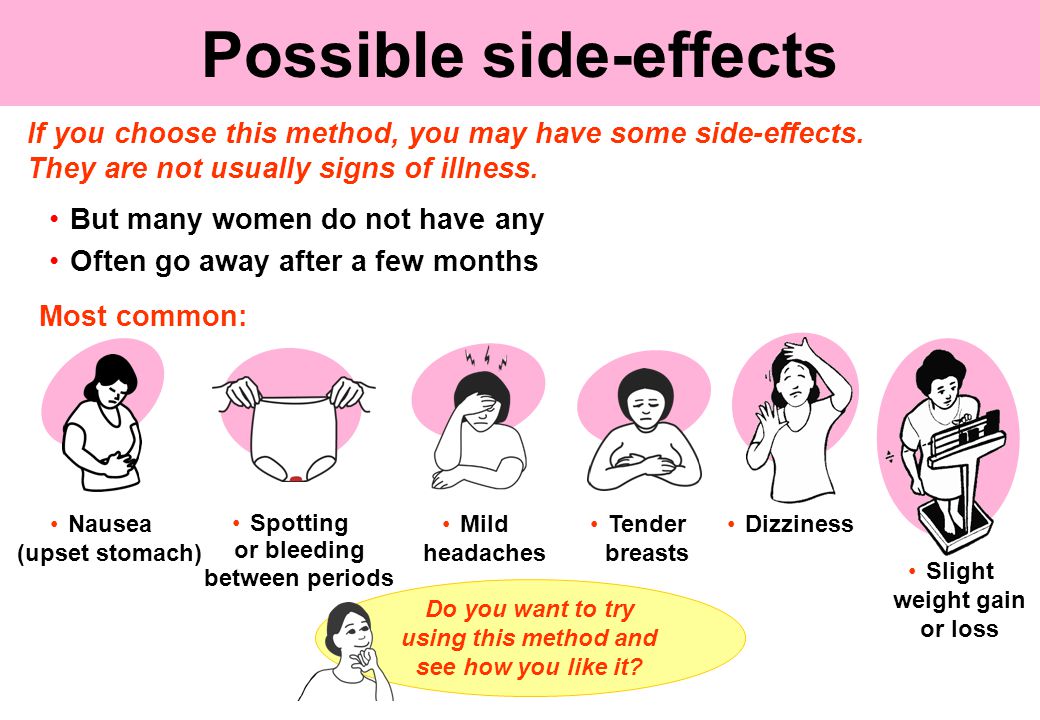
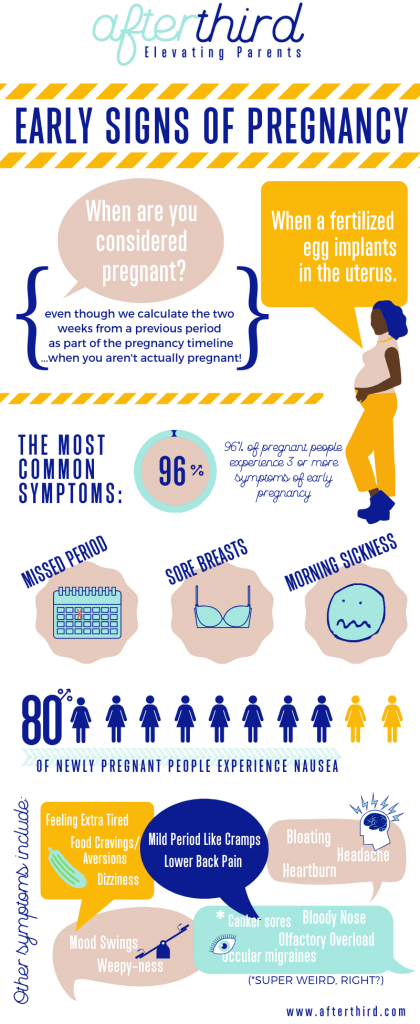
- It’s common to get mild headaches in the first few months of pregnancy because of hormonal changes.
- If you usually suffer from migraines, they may get better, worse, change or stay the same when you’re pregnant.
- Headaches during pregnancy may be triggered by poor sleep, stress, dehydration, low blood sugar or eye strain.
- If your headache doesn’t settle with simple measures (for example, rest and rehydration), you can take paracetamol.
- A headache after 20 weeks can be a sign of pre-eclampsia, which is a serious pregnancy condition that needs medical attention – see your doctor or midwife.
Does pregnancy cause headaches?
Many people get mild headaches when they are pregnant. Headaches can often be triggered by a change in hormones. They are more common in the first few months of pregnancy.
If you usually suffer from migraines, you might notice a change when you’re pregnant. There’s a good chance that your migraines will improve after the first trimester. This may be because your oestrogen level starts to stabilise. However, some people don’t notice a change, or may get worse migraines during pregnancy. You also might notice different changes from one pregnancy to the next.
Headaches can develop for many different reasons — it’s not always because of pregnancy hormones.
Why else might I get headaches during pregnancy?
Besides hormonal changes, there are many triggers that cause headaches in general, but might occur more often when you’re pregnant, such as:
- not getting enough sleep
- withdrawal from caffeine — such as in coffee, tea or cola drinks
- low blood sugar from not eating regularly
- dehydration
- feeling stressed, anxious or depressed
- eye strain — especially as your eye muscles relax during pregnancy
Many of these triggers can cause tension headaches, which are very common. The pain is usually mild and on both sides of your head.
The pain is usually mild and on both sides of your head.
Some of these triggers can cause migraines, which are more severe and mostly occur on one side of your head. If you have migraines, you might also feel sick or vomit and be sensitive to light or sound.
Pre-eclampsia
If you start getting frequent headaches after 20 weeks of pregnancy, this could be a sign of a more serious pregnancy condition called pre-eclampsia. Pre-eclampsia is when you have high blood pressure that affects your kidneys and sometimes other parts of your body. If you have a pre-eclampsia headache, you may find that simple pain-relieving medicines like paracetamol don’t help.
It’s very important to tell your doctor or midwife if you are getting headaches in the second half of pregnancy, or if your headaches are very severe.
If you have a severe headache during pregnancy, call your doctor or midwife. It could be something more serious.
Health conditions
Just like when you’re not pregnant, a headache can sometimes be a sign of other health conditions, including:
- infections, such as an ear infection or flu
- sinusitis
- problems with your teeth
- an aneurysm or stroke
What can I do to treat a headache when I’m pregnant?
If you have a headache, you could try:
- having a nap, or resting with your eyes closed
- drinking water
- having something to eat
- putting a cold or heat pack on your forehead or the back of your neck
- asking someone to give you a gentle neck massage
If you need to take medicine for pain relief, paracetamol is safe during pregnancy. Pain-relieving medicines can actually cause headaches if you take them too often, so don’t take paracetamol more than 3 times a week.
Pain-relieving medicines can actually cause headaches if you take them too often, so don’t take paracetamol more than 3 times a week.
When you’re pregnant, avoid anti-inflammatories such as ibuprofen or aspirin and medicines that contain caffeine.
What can I do to prevent headaches during pregnancy?
If you find you are getting mild headaches often, it’s a good idea to:
- getting more sleep
- drink at least 8 cups of water a day
- go to pregnancy yoga classes or do some other type of exercise
- learn relaxation or stress management techniques
- don't go more than 4 hours without eating
- avoid processed foods
- see an optometrist for an eye check
What can I do if I suffer from migraines during pregnancy?
If you suffer from migraines, try to avoid things that may trigger migraines for you. People have different triggers for migraines, so it’s important to learn what your personal triggers are.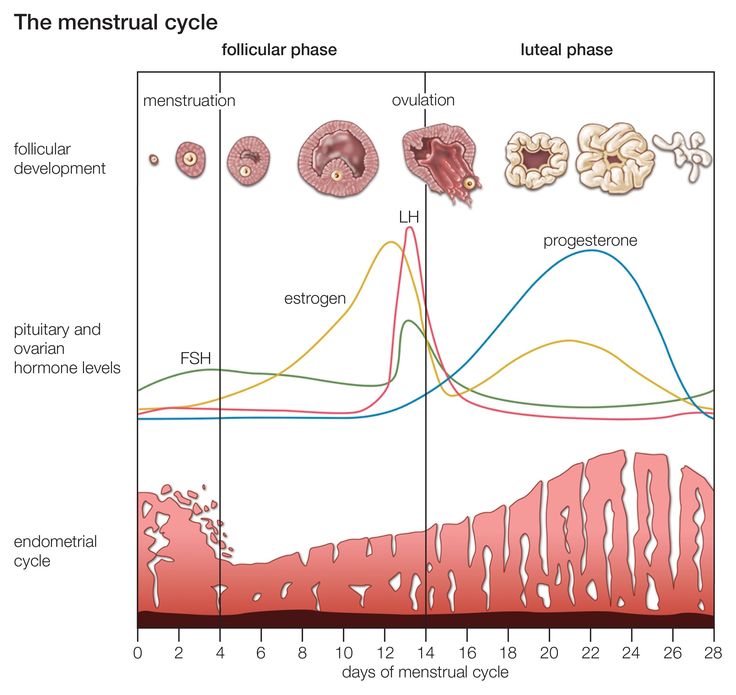 Keep a headache diary, and see if your triggers include:
Keep a headache diary, and see if your triggers include:
- specific foods such as chocolate, or food additives such as caffeine or MSG
- bright or flickering lights, strong smells and loud sounds
- not enough sleep, or too much sleep
- skipping meals
- computer or movie screens
- strenuous exercise
- emotional triggers such as arguments or stress
Check with your doctor, pharmacist or midwife before you take a medicine for your migraine, to make sure it’s safe during pregnancy.
Paracetamol is the safest option for pain relief. If paracetamol doesn’t help and you need something stronger, ask your doctor about if you can take codeine. Try not to take codeine often, as you could become dependent on it and your baby could have withdrawal symptoms after they are born.
Most triptans (migraine medicines) are not considered safe in pregnancy. If you don’t get relief from paracetamol and codeine, you may be able to take sumatriptan occasionally. This medicine is available from a pharmacist and requires a prescription. Speak with your doctor or pharmacist before using it to help you understand the risks and the benefits of this medicine during pregnancy.
This medicine is available from a pharmacist and requires a prescription. Speak with your doctor or pharmacist before using it to help you understand the risks and the benefits of this medicine during pregnancy.
You can take metoclopramide if you suffer from nausea or vomiting with migraines.
Acupuncture can help treat migraines. Talk to your doctor or midwife first to check it’s safe for you. Make sure to tell your acupuncturist that you’re pregnant, so they can avoid certain points that shouldn’t be used in pregnancy.
When should I see a doctor?
See your doctor or midwife if you have symptoms of pre-eclampsia, including:
- a headache that doesn’t get better with paracetamol
- severe pain below your ribs
- heartburn that doesn’t disappear after taking antacids
- sudden swelling in your face, hands or feet
- blurred vision
Headaches can sometimes be a sign of other serious health conditions. Contact your doctor straightaway if you have:
- a sudden severe headache
- a change in your usual headaches
- your first-ever migraine
- a headache together with fever, neck stiffness, sensitivity of your eyes to light, drowsiness or weakness of your arm or leg
- a recent head injury
CHECK YOUR SYMPTOMS — If you are feeling unwell and not sure what to do next, check your symptoms using the healthdirect Symptom Checker tool.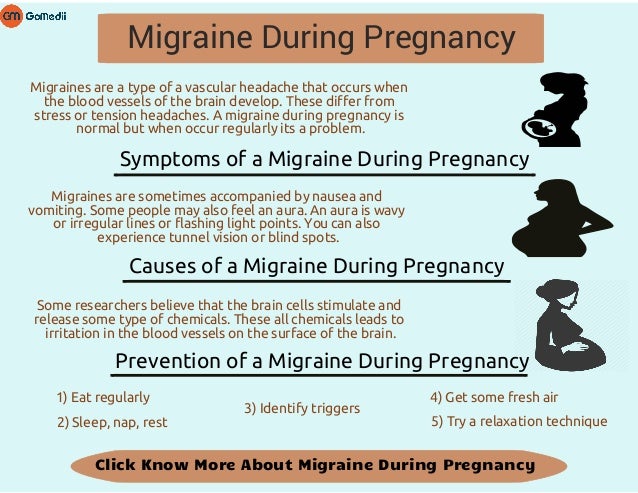
- Speak with your doctor or midwife, particularly if you have any concerns about pre-eclampsia.
- For more information about headaches, visit Migraine and Headache Australia.
- For more information about medicines you can take during pregnancy, talk to your doctor or pharmacist.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Tommy’s (Headaches in pregnancy – should I be worried?), NSW Government (Having a baby), Migraine & Headache Australia (Adults and headache), Migraine & Headache Australia (Migraine), Migraine & Headache Australia (Headache triggers), Migraine & Headache Australia (Headache treatment – no absolute cure), Migraine & Headache Australia (What is headache?), Migraine & Headache Australia (Tension headache), RANZCOG (Pre-eclampsia and high blood pressure in pregnancy), Royal Women's Hospital (Medicines in pregnancy), NSW Health (Migraine in pregnancy and breastfeeding), RANZCOG (Q&A: severe headache in the third trimester), Migraine & Headache Australia (Self-Care & Trigger Management)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Common discomforts during pregnancy
Need more information?
Treatment of Headache - Migraine & Headache Australia
There is no absolute cure for headache, but many effective treatments exist which can prevent and treat different headache types.
Read more on Migraine and Headache Australia website
Common discomforts during pregnancy
Your body has a great deal to do during pregnancy. Sometimes the changes taking place will cause irritation or discomfort, and on occasions they may seem quite alarming.
Read more on Pregnancy, Birth & Baby website
Adults and Headache - Headache Australia
Studies confirm that tension-type headache and migraine are more common in women while cluster headache, a rare form of headache, is more common in men.
Read more on Migraine and Headache Australia website
Tension-type Headache - Migraine & Headache Australia
Tension-type headache is one of the most common everyday headaches. It causes a dull, non-throbbing pain and can be caused by stress.
Read more on Migraine and Headache Australia website
Migraine Management Tips - Headache Australia
It’s important to be organized and informed about your migraine attacks and how they impact your life. Here are some migraine management tips to assist.
Read more on Migraine and Headache Australia website
Six ways to manage migraine without drugs | The George Institute for Global Health
We’ve all heard of the crushing headache pain that comes with migraine but did you know that one in every seven people experience them, three in every four people with migraine are females, and migraine is the number one cause of disability in young people? With so many people affected worldwide, you’d think modern medicine would have developed a solution by now but unfortunately there’s still no definite cure for migraine.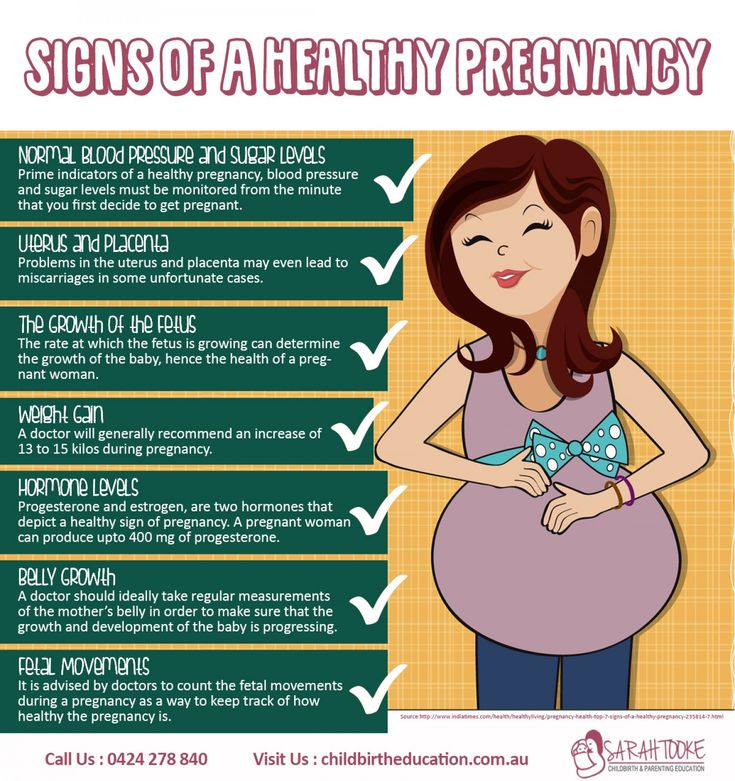
Read more on The George Institute for Global Health website
Stress and pregnancy
Stress is a normal response to major life changes but you can reduce pregnancy-related stress. Learn more about causes and strategies to help.
Read more on Pregnancy, Birth & Baby website
Mumps and pregnancy
Find out about mumps and its symptoms, how it spreads, how to manage it at home, and how to avoid mumps if you’re planning a pregnancy.
Read more on Pregnancy, Birth & Baby website
Toxaemia of pregnancy (pre-eclampsia) - MyDr.com.au
Pre-eclampsia, also known as pre-eclamptic toxaemia, or just toxaemia, occurs in pregnancy, causing problems for the baby and mother.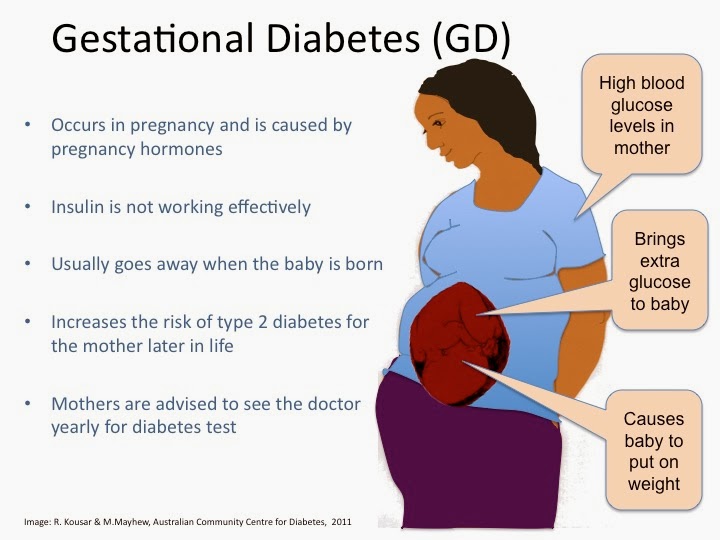
Read more on myDr website
Experiences of pregnancy - Healthtalk Australia
The parents we spoke with found pregnancy life-changing and exciting, and described at length its physical and emotional dimensions.
Read more on Healthtalk Australia website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.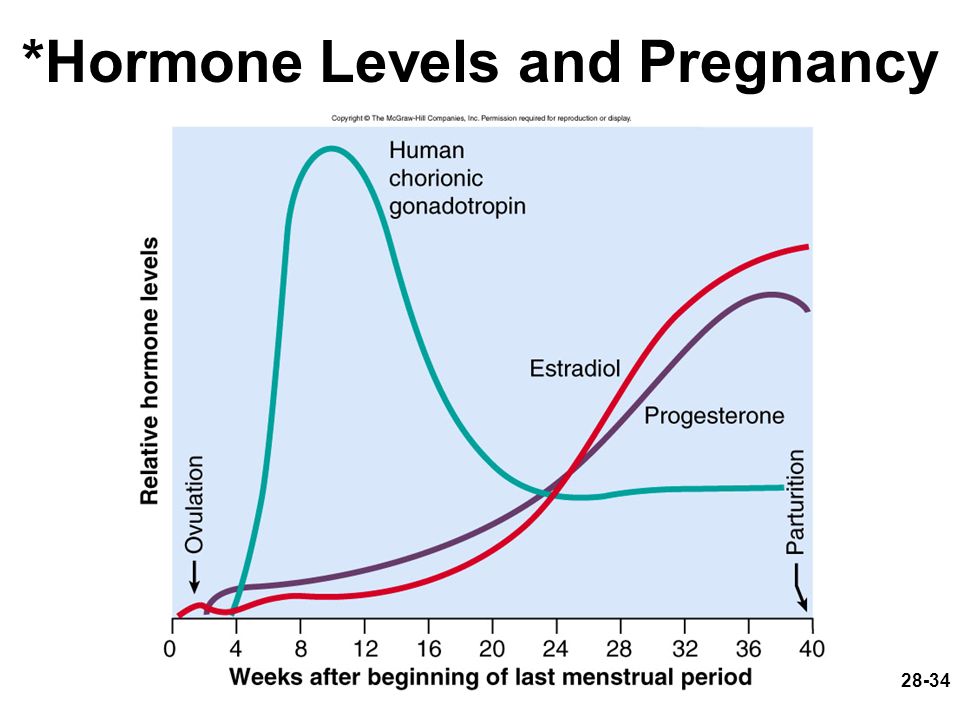
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care.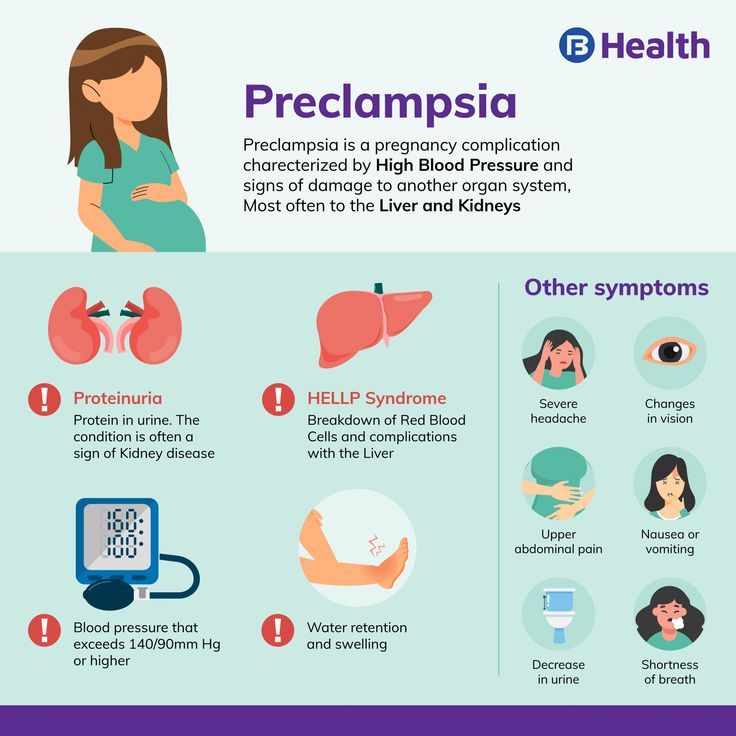 If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Migraine and pregnancy - PubMed
Review
. 1994;64:77-81.
1994;64:77-81.
K M Welch 1
Affiliations
Affiliation
- 1 Department of Neurology, Henry Ford Hospital, Detroit, MI.
- PMID: 8291477
Review
K M Welch. Adv Neurol. 1994.
. 1994;64:77-81.
Author
K M Welch 1
Affiliation
- 1 Department of Neurology, Henry Ford Hospital, Detroit, MI.
- PMID: 8291477
Abstract
PIP: Female hormones are linked to migraine. Women who have had menstrual migraine and migraine onset at menarche tend to experience no migraine during pregnancy. Not all migraines improve during pregnancy, however. Some women experience migraine for the first time during pregnancy. Migraine developing during pregnancy may indicate an underlying structural or functional disorder, e.g., cerebral aneurysms. Headaches caused by cerebral arteriovenous malformations often present as migraine with aura. Cerebral venous thrombosis (common during pregnancy and the puerperium) may manifest with migraine-like visual disturbance and headache. Idiopathic intracranial hypertension or intracranial hypertension secondary to cerebral venous thrombosis or coincidental brain mass can manifest as a continuous and increasing headache. Physicians need to intensively evaluate such cases to achieve an accurate diagnosis. Spinal procedures linked to delivery can cause a low pressure headache. Oral contraceptive use is linked to migraine. Decreasing estrogen levels appear to precipitate migraine.
Women who have had menstrual migraine and migraine onset at menarche tend to experience no migraine during pregnancy. Not all migraines improve during pregnancy, however. Some women experience migraine for the first time during pregnancy. Migraine developing during pregnancy may indicate an underlying structural or functional disorder, e.g., cerebral aneurysms. Headaches caused by cerebral arteriovenous malformations often present as migraine with aura. Cerebral venous thrombosis (common during pregnancy and the puerperium) may manifest with migraine-like visual disturbance and headache. Idiopathic intracranial hypertension or intracranial hypertension secondary to cerebral venous thrombosis or coincidental brain mass can manifest as a continuous and increasing headache. Physicians need to intensively evaluate such cases to achieve an accurate diagnosis. Spinal procedures linked to delivery can cause a low pressure headache. Oral contraceptive use is linked to migraine. Decreasing estrogen levels appear to precipitate migraine. Estradiol and progesterone therapy for menstrual migraine maintains high estrogen levels during the menstrual epoch, which generally prevents migraine. High but stable estrogen levels prevent migraine. Thus, migraines who do not suffer from migraine during pregnancy benefit from high estrogen levels. Pregnant women with migraine should not take drugs unless the frequency and severity of migraine is life threatening to the mother or fetus. Acetaminophen can be used to relieve pain. Meperidine suppositories can relieve severe pain. Pregnant women should not use aspirin, nonsteroidal anti-inflammatory drugs, or vasoconstrictors. Fluid replacement and acceptable antiemetic drugs can treat dehydration and vomiting. Behavioral modification, identification, and elimination of foods that trigger attacks, magnesium supplementation, and low doses of propranolol 3-4 times/day in severe cases may prevent migraine in pregnant women.
Estradiol and progesterone therapy for menstrual migraine maintains high estrogen levels during the menstrual epoch, which generally prevents migraine. High but stable estrogen levels prevent migraine. Thus, migraines who do not suffer from migraine during pregnancy benefit from high estrogen levels. Pregnant women with migraine should not take drugs unless the frequency and severity of migraine is life threatening to the mother or fetus. Acetaminophen can be used to relieve pain. Meperidine suppositories can relieve severe pain. Pregnant women should not use aspirin, nonsteroidal anti-inflammatory drugs, or vasoconstrictors. Fluid replacement and acceptable antiemetic drugs can treat dehydration and vomiting. Behavioral modification, identification, and elimination of foods that trigger attacks, magnesium supplementation, and low doses of propranolol 3-4 times/day in severe cases may prevent migraine in pregnant women.
Similar articles
-
The role of sex hormones in headache.
Silberstein SD. Silberstein SD. Neurology. 1992 Mar;42(3 Suppl 2):37-42. Neurology. 1992. PMID: 1557190 Review.
-
Sex hormones and headache.
Silberstein SD. Silberstein SD. Rev Neurol (Paris). 2000;156 Suppl 4:4S30-41. Rev Neurol (Paris). 2000. PMID: 11139745 Review.
-
Migraine associated with menstruation.
MacGregor A. MacGregor A. Funct Neurol. 2000;15 Suppl 3:143-53. Funct Neurol. 2000. PMID: 11200785 Review.
-
Women's issues of migraine in tertiary care.
Kelman L. Kelman L. Headache. 2004 Jan;44(1):2-7. doi: 10.
 1111/j.1526-4610.2004.04003.x. Headache. 2004. PMID: 14979877
1111/j.1526-4610.2004.04003.x. Headache. 2004. PMID: 14979877 -
Hormonal changes throughout life in women.
Zacur HA. Zacur HA. Headache. 2006 Oct;46 Suppl 2:S49-54. doi: 10.1111/j.1526-4610.2006.00554.x. Headache. 2006. PMID: 17044841 Review.
See all similar articles
Cited by
-
Cross sectional imaging of post partum headache and seizures.
Hiremath R, Mundaganur P, Sonwalkar P, N S V, G S N, P S. Hiremath R, et al. J Clin Diagn Res. 2014 Dec;8(12):RC01-5. doi: 10.7860/JCDR/2014/8783.5234. Epub 2014 Dec 5. J Clin Diagn Res. 2014. PMID: 25654004 Free PMC article.
Publication types
MeSH terms
Substances
Headache during pregnancy
Authors: A. Yu. Limanskaya, Yu.V. Davydova
01/19/2017
A.Yu. Limanskaya
Tension headache and migraine are the most common types of headaches (30-78% and 15% respectively). According to the WHO, primary headache is in general in 10th place among all conditions leading to disability, and in women, in 5th place. In 16% of patients, episodic tension-type headache becomes chronic. The economic loss in Western Europe and North America due to headache-related disability is estimated at $17-20 billion a year. To date, there is a trend towards an increase in the incidence of headache in young people.
Yu.V. Davydova
The International Headache Society defines migraine as a throbbing, unilateral headache associated with nausea, sensitivity to light, sound, and turning of the head.
In a broader sense, this pathology can be considered as a hereditary disease in which physiological changes (whether external, such as changes in weather conditions, or internal, such as changes in sleep patterns) often cause stereotypical attacks with migraine symptoms, as defined above. Migraine occurs three times more often in women than in men, with the highest rates in women during active childbearing age, peaking at 27% at age 41 years. To date, there is no evidence that migraine itself affects fertility or the course of pregnancy, but the quality of life in pregnant women with migraine is significantly reduced.
According to some researchers, migraine and tension-type headache in pregnant women are risk factors for the development of arterial hypertension and preterm birth (F. Facchinetti et al., 2009). Pregnancy can provoke the occurrence of diseases accompanied by headache (preeclampsia, thrombosis of the cerebral arteries, compression of the brain as a result of the presence of tumors). Relevant today is the rapid diagnosis of pathology and an adequate choice of therapeutic and obstetric tactics for the treatment of headache in pregnant women due to the great medical and social significance of the problem.
Antiphospholipid syndrome (APS) is defined by the presence of antiphospholipid antibodies (APLA) associated with an increased risk of thrombosis or recurrent spontaneous abortions. The most serious complications can occur in secondary APS against the background of inflammatory systemic autoimmune diseases. Studies conducted in neurological clinics have found that it is migraine, and not headache of all types, that is significantly associated with APLA in patients with systemic autoimmune pathology. However, in patients with systemic lupus erythematosus (SLE), headache is significantly associated with positive APLA titers. Also in this group, cerebral ischemic lesions were significantly more common.
During pregnancy, a woman may experience many health problems. For example, a headache during pregnancy occurs quite often, at different times of the day and for various reasons. Oddly enough, but a woman's frequent headache may be a sign of pregnancy, which she does not yet know about.
More than 80% of women sooner or later complain of a headache during pregnancy. Even if a woman was absolutely healthy before pregnancy, then during the bearing of a child she gets a headache. Sometimes it becomes so strong that it is difficult to endure. Headache can occur at any time during pregnancy, but it tends to be most common during the first and third trimesters.
There are factors that can cause headaches during pregnancy.
1. Hormonal changes: The state of the nervous system depends on the woman's hormonal status, that is, on the quantity and quality of hormones produced.
2. Hypotension during pregnancy is associated with the predominance of progesterone over other hormones; the vasodilating effect of progesterone leads to a decrease in blood pressure, cerebral hypoxia and, as a result, to headache.
3. Arterial hypertension and preeclampsia cause headache as a result of generalized vasospasm and circulatory disorders in the central nervous system.
4. Nutritional factors - cold food or eating foods containing tyramine and phenylamine (nitrogen compounds that can affect blood vessels) can cause headache attacks; pregnant women who are prone to migraine headache should be careful in consuming the following foods: chocolate, nuts, yogurt, chicken liver, avocados, citrus fruits, bananas, canned and pickled foods, Japanese cuisine, tea, coffee, cola, sausages, red wine, cheese.
5. Hunger headache occurs as a result of a decrease in blood glucose levels and impaired supply of nutrients to the brain.
6. Overweight.
7. Eye strain or prolonged forced stay in the same uncomfortable position.
8. Allergic reactions.
9. Dehydration of the body.
10. Exacerbation of chronic diseases - spine, especially osteochondrosis, due to increased load during pregnancy, static and dynamic loads often cause headaches; neurocirculatory asthenia as a cause of vasospasm and as a consequence of the appearance of a feeling of heaviness in the head, mood lability and headache.
11. Occurrence of infectious and other diseases such as: meningitis, encephalitis, sinusitis, pyelonephritis, glomerulonephritis and certain ophthalmic pathologies; the characteristic manifestations of this headache are its intensity and the lack of effect of pain medications.
12. Stress factor. Lability of the nervous system, ups and downs in mood, excitement, psycho-emotional stress, depression - all this can cause a headache.
13. Changing weather conditions. During pregnancy, fluctuations in atmospheric pressure can lead to headaches.
14. Physical stimuli - flickering light, noise, strong odors.
15. Weekend headache. If you sleep longer than usual during the day, the cause of headache can be, for example, venous congestion.
16. Indoor climate: too dry or warm air, a lot of tobacco smoke.
The most common form of headache during pregnancy is migraine, which is accompanied by visual impairment, gastrointestinal disorders, nausea, vomiting, photoreaction, and various vestibular disorders.
In the United States, 28 million people aged 12 and older suffer from migraine, of which 21 million are women aged 25-55. In about 25% of families, one of its members suffers from migraine.
A feature of migraine pain is known to be severe, throbbing pain, predominantly hemicrania, often preceded by aura and marked photoreaction.
It is noteworthy that about 15% of women who have never experienced migraine before, first encounter it with the onset of pregnancy. On the other hand, there are cases when during pregnancy a woman completely stops migraine attacks. In this case, this is due to changes in hormonal status and the absence of ovulation and menstruation.
The occurrence of migraine in women under the influence of hormonal changes is possible throughout the entire menstrual cycle. The positive effect of pregnancy on migraine is observed in 55-90% of women during the gestation period, regardless of the type of migraine. The relief of headache symptoms during pregnancy and their possible worsening after childbirth is likely due to uniformly high and stable estrogen levels during pregnancy and their rapid decline after childbirth.
Another type of headache in pregnancy is tension headache. As a rule, it is characterized by medium intensity, unlike migraine, it often covers the entire head. The pain of tension squeezes the head like a hoop, or causes a pulling sensation; occurs mainly as a result of stress or overexertion.
- If a woman has frequent headaches before pregnancy, the risk of developing preeclampsia increases by 2. 4 times
- If a woman is diagnosed with migraine before pregnancy, the risk of developing preeclampsia increases by 3.5 times migraine attacks are observed in the early stages - the risk of developing preeclampsia increases 4 times
Pregnancy headache treatment
A pregnant woman needs medical advice when:
- headache has become almost constant, and has recently changed its character;
- headache in the morning and all day;
- pain is constantly localized in a certain area of the head;
- headache is accompanied by other symptoms - impaired vision, hearing, speech, motor functions, sensitivity, etc.;
- Pain accompanies high or low blood pressure.
Doctor's prescriptions depend on the underlying cause of the headache. Sometimes several factors influence at once, so it is difficult to make an accurate diagnosis. If the headache bothers you regularly, you should contact a neurologist for a specific examination.
Primary therapy during pregnancy - non-drug (relaxation, sleep, massage). For the treatment of acute migraine attacks, paracetamol (1000 mg) is considered the drug of choice, preferably in the form of suppositories. The table shows data on the possibility of using a number of drugs for the treatment of headache during pregnancy.
The risks associated with the use of aspirin (acetylsalicylic acid) and ibuprofen are considered relatively low if the drugs are taken episodically and removed in the last trimester.
Information on the safety of triptan treatment during pregnancy is available for only a few drugs in this group (sumatriptan, naratriptan and rizatriptan). According to information databases containing information on pregnancy outcomes in women who received these drugs, there were no facts indicating serious risks to the mother and fetus.
With some triptans (sumatriptan, zolmitriptan, naratriptan), there is currently a possibility of a small increase in preterm birth, so triptans are acceptable in severe migraine in exceptional cases. However, data on the use of triptans continues to accumulate and there is not yet sufficient evidence for the safety of the use of triptans during pregnancy.
Dihydroergotamine and ergotamine tartrate are contraindicated in pregnant women.
Headache definitely cannot be tolerated, it must be correctly diagnosed, differentiated and treated.
The American Academy of Neurology recommends a brain scan in the following cases (if pregnant, only MRI is recommended)
- if, in the presence of a headache, a neurological deficit occurs or any, even short-term, changes in the neurological status;
- if the headache has atypical manifestations and does not fit into the strict framework of establishing a diagnosis of migraine;
- if there is a proven immunodeficiency;
- a sudden severe headache in women for the first time.
- Number:
- Thematic issue "Gynecology, Obstetrics, Reproductology" No.
4 (24), chest 2016
05.02.2023 Obstetrics/Gynexologii Actual Problems of the Council of Councils of the Council of Practices
PID Tour Plenum “ASOSIAISIA AKUSHERIV-GINEKOLIVARIVA” TA HEARTICAL-POSTICIALY STRISTICS, GINECOLIA, SUNNED LIGHTS: NAMILARIA (PA. )", which was discussed on October 27-28 in an online format, the experts looked at the global problems of current gynecological practice, associated with genital ailments in the reproductive tract, planning and saving pregnancy. Key words: genital endometriosis, adenomyosis, spontaneous abortion, antepartum period, threat of pregnancy reversal, dienogest, micronization of progesterone. ...
05.02.2023 Obstetrics/gynecologyModern aspects of therapy for genitourinary menopausal syndrome
At the same time, the people of the people are inevitable at the nationwest, the process of old village, the lead to the Zbilhennya Kilkosti Assocyovani Izu Zakhvoryuvan, one of the Genitoinaric Menopausky syndrome, and the festivities of the erase of the ejacino of the erase ...
Migraine during pregnancy: description of the disease, causes, symptoms, cost of treatment in Moscow
Migraine during pregnancy is a fairly common phenomenon that should not be ignored and treated. There are many reasons for the appearance of the problem during this period. After childbirth, the disease usually disappears completely. In the next pregnancy, there is a risk of recurrence of the violation, but it will not necessarily appear again. Since the pain negatively affects not only the condition of the woman, but also the child, it is necessary to take drugs to eliminate the attack, but only those that are allowed for pregnant women.
Migraine in pregnant women occurs not infrequently, since, in addition to hormonal changes in the body, there are also changes in the psycho-emotional state, which often also act as a trigger for the development of pathology. Depending on the duration of pregnancy, a woman's well-being may improve or worsen. The peak of migraines in most cases occurs in the first trimester of pregnancy, when a woman's body undergoes especially rapid hormonal changes. In the later stages, headaches may begin to disturb due to changes in the spine that appear against the background of a shift in the center of gravity.
Reasons
Migraine attacks during pregnancy are usually triggered by specific factors. Migraines during early pregnancy can be caused by the following reasons:
-
specific stresses for the body, which are associated with the process of implantation of the egg and the beginning of the development of the embryo;
-
a sharp change in hormonal levels;
-
dehydration due to changes in metabolic processes in the body and a woman's lack of attention to herself;
-
emergence of food intolerance against the background of early toxicosis.
Also, a number of women in the first trimester of pregnancy often experience migraine-provoking nervous strain due to constant concern about their condition, the development of the child and the upcoming birth.
In the second trimester, a woman has a significant improvement in her condition. The frequency of seizures is reduced, and because of the ability to use more drugs, they become less painful. The main provocateurs of the appearance of headaches in this period are the following factors:
-
physical overload - it occurs if a woman does not reduce physical activity, continuing to lead the same lifestyle as before pregnancy.
As a result, an attack occurs as a protest of the body against what is happening;
-
strong emotional experience;
-
abrupt weather changes - they affect a woman if she suffered from meteorological dependence before pregnancy;
-
inhalation of very sweet heavy odours.
In the third trimester of pregnancy, the intensity of migraine increases. Due to the ongoing changes in the spine, blood circulation begins to deteriorate to a large extent, due to which even a slight vascular spasm is enough for a migraine attack. The main reasons that can cause it are:
-
drinking a large amount of liquid at once - in order not to provoke an attack, you need to drink often, but little by little, thereby not causing a sharp influx of water into the blood;
-
staying in an uncomfortable position, which significantly worsens blood circulation in the lower extremities;
-
prolonged stay in the supine position, which also worsens blood circulation;
-
eating spicy or spicy foods;
-
great excitement or prolonged nervous tension.
Migraines may persist for some time after childbirth due to hormonal changes in the body. However, this phenomenon is not always the case and is considered the exception rather than the rule for migraine during pregnancy.
Is an aura possible
Migraine with aura occurs in pregnant women with the same frequency as the classical one. In a quarter of cases, a few minutes before an attack or a maximum of an hour before it, a woman develops previous neurological disorders. If they do not appear strongly, then the patient has time to take medications, thereby relieving an attack, or to return home. When the symptoms of the aura are strong, they can cause no less torment than the pain attack itself.
You can talk about the presence of an aura in a woman if any of the following symptoms are present before a migraine attack:
-
visual disturbances - with them, loss of visual fields, temporary loss of vision in one or both eyes, flickering flies before the eyes or flashes of light;
-
severe weakness - it can spread to the whole body, but more often it is felt only in the limbs of the side from which the head will hurt in the future.
The opposite side of the body suffers much less often;
-
tingling in the limbs and upper half of the body, even affecting the tongue and lips;
-
goosebumps;
-
complete loss or significant reduction in the sensation of limbs;
-
various speech disorders such as confusion or slurring.
Quite often, in pregnant women with migraine with aura, such a phenomenon is noted that if during this period the effect of the negative factor is eliminated, a further attack does not develop, even if medications are not taken. Because of this, in such a situation, a woman needs to fix as accurately as possible what caused the deterioration.
Is an attack dangerous for the fetus
Today, thanks to numerous studies, doctors have been able to find out whether a migraine attack affects the fetus. The unborn child is able to feel the emotions of the mother and her pain, which is why there is a negative change in his condition at the time of the attack. Also, against the background of pain, a spasm of the vessels supplying the placenta often occurs. As a result, the fetus begins to receive significantly less oxygen, which causes hypoxia in it, which, with frequent repetitions of migraine attacks, can cause mental development disorders against the background of brain damage.
Medicines prescribed for pregnant women must be taken during an attack without fail. They will not harm the child, as they do not penetrate the placental barrier and effectively relieve pain, eliminating its negative impact. It is unacceptable to prescribe such funds on your own, since mistakes can be too dangerous for the fetus. All drugs are correctly selected taking into account the duration of pregnancy only by a doctor.
Prophylaxis
Preventive measures against migraine during pregnancy greatly help to reduce the risk of this problem. Additionally, it will help improve well-being and a proper lifestyle. The main preventive measures during pregnancy include:
-
full sleep at least 9 hours a day;
-
taking light sedatives when nervous tension appears;
-
providing a comfortable temperature in the room;
-
drinking frequently and in small amounts;
-
eating food that does not cause a burning sensation in the mouth.