Signs and symptoms of blighted ovum
Blighted Ovum (Anembryonic Pregnancy): Causes & Symptoms
Overview
A blighted ovum is when the gestational sac containing the embryo is empty.What is a blighted ovum?
A blighted ovum (also called an anembryonic pregnancy) is a type of early miscarriage that occurs when a fertilized egg implants into the uterus but does not develop into an embryo. The embryo will stop growing, but the gestational sac (where the embryo would develop) continues to grow. The placenta and empty gestational sac will release pregnancy hormones — even without an embryo present. This causes you to have early symptoms of pregnancy or even have a positive pregnancy test. Sometimes it occurs so early in pregnancy that you don't know you're pregnant.
When does a blighted ovum happen?
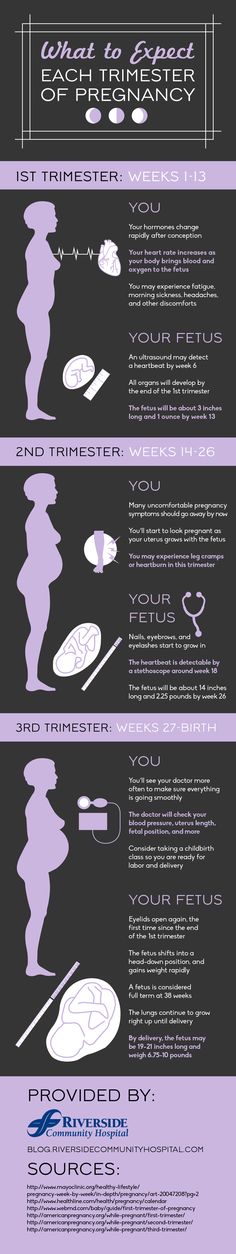
A blighted ovum causes an early miscarriage in the first trimester of pregnancy. During fetal development, a fertilized egg turns into a blastocyte. At around four weeks of pregnancy, this blastocyte implants in the wall of the uterus and develops into an embryo. When you have a blighted ovum, the gestational sac that would hold the embryo continues to grow, even without an embryo present. The following can occur:
- A blighted ovum happens so early in pregnancy, that you never realize you are pregnant.
- You have a positive pregnancy test and signs of pregnancy only to discover a blighted ovum at your first ultrasound.
- You have a positive pregnancy test and signs of pregnancy but then experience a miscarriage.
How common is a blighted ovum pregnancy?
A blighted ovum is the number one cause of first trimester miscarriages.
Symptoms and Causes
What are the symptoms of a blighted ovum?
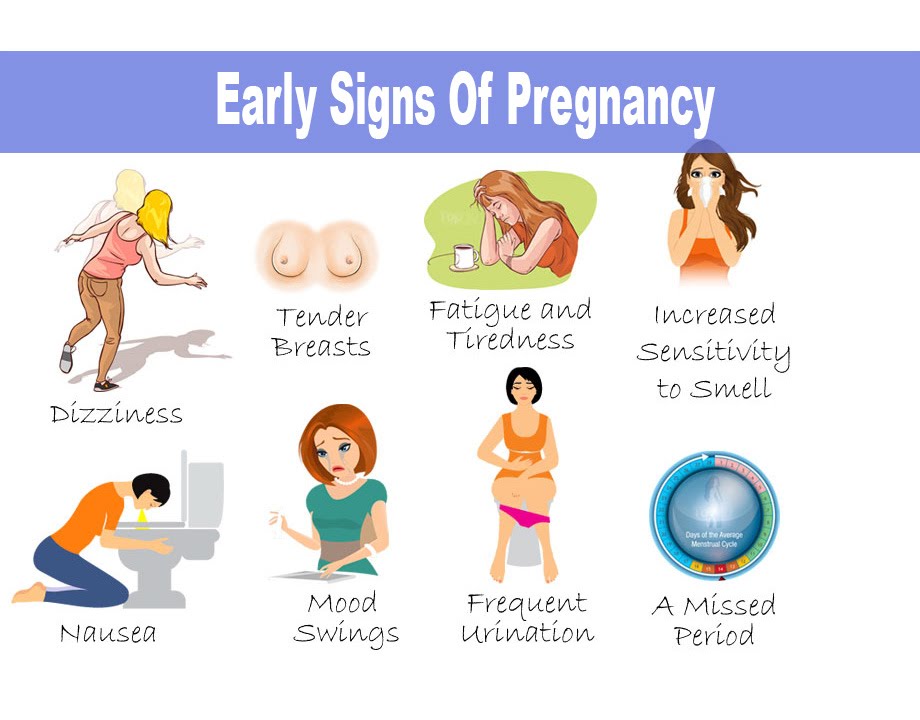
A blighted ovum can occur so early in pregnancy that you never knew you were pregnant. In other cases, you may experience signs of pregnancy such as a missed menstrual period or a positive pregnancy test. You can have symptoms of early pregnancy, such as breast tenderness and morning sickness.
Other times your symptoms will resemble those of a miscarriage:
- Vaginal bleeding: Spotting (light bleeding), bleeding or passing light gray tissue or blood clots.
- Cramping: Mild to moderate cramping in your pelvic and abdominal region.
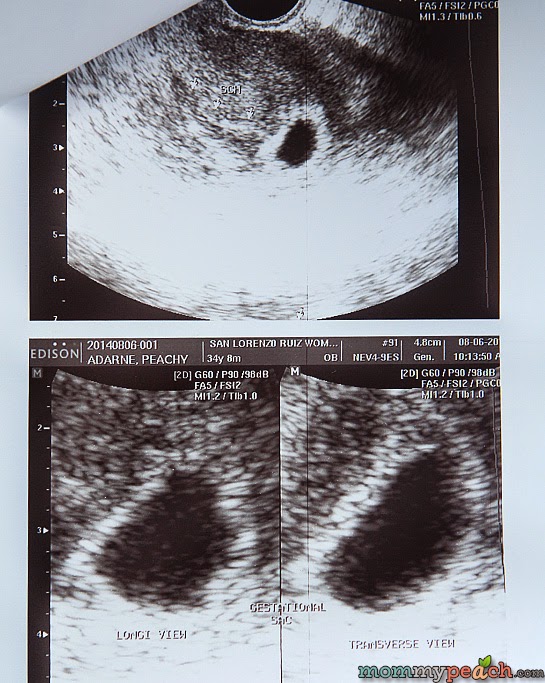
The only way to confirm a blighted ovum is through an ultrasound. It will show a gestational sac that is missing an embryo inside.
What causes a blighted ovum?
A blighted ovum is usually caused by chromosomal or genetic problems during cell division. During conception, the egg will begin to divide shortly after being fertilized by sperm. Around ten days later, the cells have formed an embryo. With a blighted ovum, the embryo never forms or stops growing after it’s formed.
How does a blighted ovum miscarriage start?
A blighted ovum miscarriage will cause vaginal bleeding and abdominal cramping. A miscarriage usually feels more intense than your regular menstrual period. You can take an over-the-counter medicine like acetaminophen to relieve cramping. Avoid lifting anything heavy or any strenuous exercise as it can increase your bleeding. You may experience spotting for several weeks after a miscarriage.
Diagnosis and Tests
How is a blighted ovum diagnosed?
Your healthcare provider will diagnose a blighted ovum using transvaginal ultrasound. This happens in the first trimester, usually between seven and nine weeks of pregnancy. An embryo should be visible at this time in pregnancy. With a blighted ovum, the gestational sac will be empty.
- You will lie back on an exam table and place your feet in stirrups like you do for a pelvic exam. Your healthcare provider will put an ultrasound wand into your vagina to see the contents of your uterus.
- A blighted ovum will appear as an empty sac — almost like a bubble.
A blighted ovum is when the gestational sac containing the embryo is empty.
People are often unaware that they have a blighted ovum. This is because your placenta continues to give off hormones, making your body think you are pregnant. This is also why you can still have symptoms of pregnancy, including a positive pregnancy test.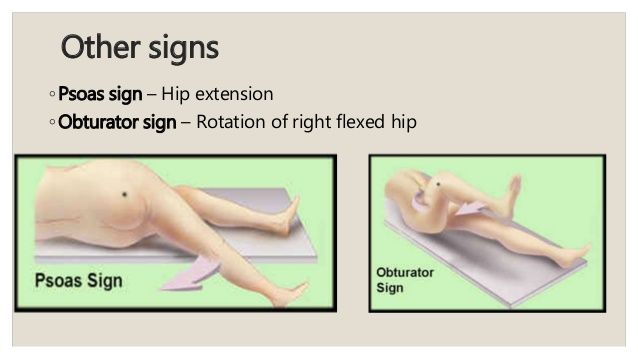
If you’ve already experienced bleeding or signs of a miscarriage, your healthcare provider will use ultrasound to look at the contents of your uterus to diagnose a blighted ovum.
Some healthcare providers will collect a series of blood samples that check the levels of hCG (human chorionic gonadotropin) in your body. HCG is known as the pregnancy hormone because it's only produced if you are pregnant. The level of hCG in your blood increases rapidly in early pregnancy and reaches its peak around weeks eight to ten. If it's not rising quickly, it can indicate a miscarriage or other complication. Your provider may decide to test your hCG levels over the course of several days to evaluate how your hCG levels are rising. This can be an effective tool for diagnosing blighted ovum.
Management and Treatment
How is a blighted ovum treated?
For some people, there may be no treatment needed, because your body passes the embryo through your vagina (a miscarriage). If your body does not miscarry the embryo, there are other options to remove the contents of your uterus. Your healthcare provider will talk you through possible treatments:
If your body does not miscarry the embryo, there are other options to remove the contents of your uterus. Your healthcare provider will talk you through possible treatments:
- Dilation & Curettage (D&C): This is a surgical procedure to remove the contents of your uterus. Your healthcare provider will dilate, or open, the cervix and use medical tools and suction to remove the pregnancy tissues from your uterus. This is done under sedation or general anesthesia.
- Natural miscarriage: If it's safe, you may be able to watch and wait to see if your body eventually releases the pregnancy tissues. It can sometimes take days or weeks for this to start. Your healthcare provider will let you know if this is an option for you. You will experience cramping, abdominal pain and bleeding once the miscarriage begins.
- Medication-induced miscarriage: You may be given a medication called misoprostol to trigger your body to miscarry.
 This moves the process along and eliminates the time waiting for a miscarriage to start on its own. You will have cramping, abdominal pain and bleeding within 30 minutes to ten hours of taking the medication.
This moves the process along and eliminates the time waiting for a miscarriage to start on its own. You will have cramping, abdominal pain and bleeding within 30 minutes to ten hours of taking the medication.
A follow-up appointment is usually scheduled four to six weeks after a miscarriage or D&C. You may be given another ultrasound to confirm the uterus is empty. Your healthcare provider will check for signs of infection and make sure there were no complications.
What are the complications of a blighted ovum?
Complications of a blighted ovum are uncommon, but the possible complications could include:
- Excessive bleeding or hemorrhage.
- Infection.
- Scarring (from the D&C procedure).
- Tears in the uterus (from the D&C procedure).
How long does it take to recover from a blighted ovum?
Recovering from a blighted ovum miscarriage or D&C can last from one or two weeks to a month. Cramping generally lasts up to a week, but bleeding can last several weeks. Your bleeding should get lighter until it stops completely.
Your bleeding should get lighter until it stops completely.
You can resume normal activities when you feel comfortable. Bleeding can increase with strenuous activity or exercise. Hormones may remain in your body and delay your menstrual cycle. Most people will get their period within four to six weeks after a blighted ovum.
It may take longer to recover emotionally from a blighted ovum miscarriage. You may have feelings of sadness, anger or confusion. It’s OK to take time to grieve. Ask your friends and family for support.
Prevention
Can a blighted ovum be prevented?
A blighted ovum can’t be prevented. Some couples may want to do genetic testing on the tissue inside the uterus. This checks for underlying causes of your miscarriage and can be helpful to couples who have experienced multiple pregnancy losses.
Outlook / Prognosis
How soon after a blighted ovum can I get pregnant again?
Most healthcare providers recommend having one or two regular menstrual cycles before trying to conceive again after any type of miscarriage.
What are my chances of having another blighted ovum?
Your chances of having another blighted ovum are low. Most people go on to have healthy, full-term pregnancies. If you experience more than one blighted ovum, your healthcare provider may suggest testing to determine if there is an underlying cause.
Living With
When should I see my healthcare provider?
Call your healthcare provider right away if you have any of these symptoms:
- Excessive bleeding from your vagina.
- Dizziness or fainting.
- Fever that does not go away.
- Symptoms that get worse over time.
- Severe pain that isn’t helped with pain medicine.
When should I go to the ER?
Go to the nearest ER If you experience heavy vaginal bleeding — more than two pads per hour for two consecutive hours — or have symptoms of anemia like dizziness, palpitations or paleness.
What questions should I ask my doctor?
Losing a pregnancy is upsetting and confusing.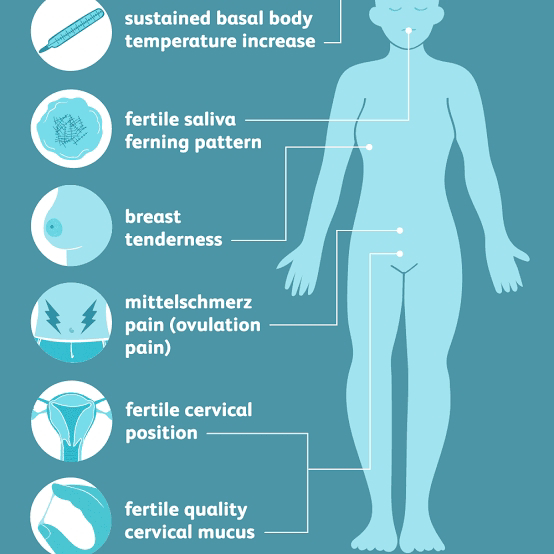 Do not be embarrassed to ask any questions you have. It's completely normal to have questions and feel emotional during this time. Some questions you may ask are:
Do not be embarrassed to ask any questions you have. It's completely normal to have questions and feel emotional during this time. Some questions you may ask are:
- Can I let my body miscarry or should I take medication to induce a miscarriage?
- What are the risks of miscarriage?
- Do I have to have a D&C?
- What are the risks of a D&C?
- How long can I expect to bleed or have cramping?
- Is there any indication this will happen again?
- When can I start trying to conceive?
- Do I need to come back for another ultrasound?
Frequently Asked Questions
Is a blighted ovum considered a miscarriage?
Yes, a blighted ovum is a miscarriage. A miscarriage is a loss of pregnancy before 20 weeks. A blighted ovum is considered an early miscarriage because it occurs before 13 weeks of pregnancy.
How long can you carry a blighted ovum?
The amount of time you can carry a blighted ovum varies. Your placenta will continue to grow and release hormones without an embryo. For some people, a miscarriage can occur within a few days or weeks. Others may still believe they are pregnant only to discover a blighted ovum at their first ultrasound.
Your placenta will continue to grow and release hormones without an embryo. For some people, a miscarriage can occur within a few days or weeks. Others may still believe they are pregnant only to discover a blighted ovum at their first ultrasound.
Can a blighted ovum turn into a baby?
No, an empty gestational sac will not turn into an embryo. The formation of the embryo occurs within two weeks of conception. By the time the gestational sac is formed, the cells should have already formed the embryo. Your healthcare provider will be able to examine your gestational sac to confirm that no embryo has developed.
Do hCG levels rise with blighted ovum?
Yes, most of the time hCG levels will rise, giving you a positive pregnancy test and symptoms of pregnancy. This is because the placenta continues to give off hCG even if an embryo is not present. The hormone hCG is sometimes called the pregnancy hormone because it is only produced if you are pregnant.
Is a blighted ovum more common with IVF?
A blighted ovum is not more common with IVF (In Vitro Fertilization). Your chances of having a blighted ovum with IVF treatment are about the same as they would be with a natural conception.
Your chances of having a blighted ovum with IVF treatment are about the same as they would be with a natural conception.
A note from Cleveland Clinic
Losing a pregnancy is difficult. If you are struggling after a miscarriage, speak with your healthcare provider so they can recommend support groups or counselors. Finding support may help you get through this hard time. Most people who have had a blighted ovum will go on to have a healthy pregnancy.
Blighted Ovum (Anembryonic Pregnancy): Causes & Symptoms
Overview
A blighted ovum is when the gestational sac containing the embryo is empty.What is a blighted ovum?
A blighted ovum (also called an anembryonic pregnancy) is a type of early miscarriage that occurs when a fertilized egg implants into the uterus but does not develop into an embryo. The embryo will stop growing, but the gestational sac (where the embryo would develop) continues to grow. The placenta and empty gestational sac will release pregnancy hormones — even without an embryo present. This causes you to have early symptoms of pregnancy or even have a positive pregnancy test. Sometimes it occurs so early in pregnancy that you don't know you're pregnant.
This causes you to have early symptoms of pregnancy or even have a positive pregnancy test. Sometimes it occurs so early in pregnancy that you don't know you're pregnant.
When does a blighted ovum happen?
A blighted ovum causes an early miscarriage in the first trimester of pregnancy. During fetal development, a fertilized egg turns into a blastocyte. At around four weeks of pregnancy, this blastocyte implants in the wall of the uterus and develops into an embryo. When you have a blighted ovum, the gestational sac that would hold the embryo continues to grow, even without an embryo present. The following can occur:
- A blighted ovum happens so early in pregnancy, that you never realize you are pregnant.
- You have a positive pregnancy test and signs of pregnancy only to discover a blighted ovum at your first ultrasound.
- You have a positive pregnancy test and signs of pregnancy but then experience a miscarriage.
How common is a blighted ovum pregnancy?
A blighted ovum is the number one cause of first trimester miscarriages.
Symptoms and Causes
What are the symptoms of a blighted ovum?
A blighted ovum can occur so early in pregnancy that you never knew you were pregnant. In other cases, you may experience signs of pregnancy such as a missed menstrual period or a positive pregnancy test. You can have symptoms of early pregnancy, such as breast tenderness and morning sickness.
Other times your symptoms will resemble those of a miscarriage:
- Vaginal bleeding: Spotting (light bleeding), bleeding or passing light gray tissue or blood clots.
- Cramping: Mild to moderate cramping in your pelvic and abdominal region.
The only way to confirm a blighted ovum is through an ultrasound. It will show a gestational sac that is missing an embryo inside.
What causes a blighted ovum?
A blighted ovum is usually caused by chromosomal or genetic problems during cell division. During conception, the egg will begin to divide shortly after being fertilized by sperm. Around ten days later, the cells have formed an embryo. With a blighted ovum, the embryo never forms or stops growing after it’s formed.
Around ten days later, the cells have formed an embryo. With a blighted ovum, the embryo never forms or stops growing after it’s formed.
How does a blighted ovum miscarriage start?
A blighted ovum miscarriage will cause vaginal bleeding and abdominal cramping. A miscarriage usually feels more intense than your regular menstrual period. You can take an over-the-counter medicine like acetaminophen to relieve cramping. Avoid lifting anything heavy or any strenuous exercise as it can increase your bleeding. You may experience spotting for several weeks after a miscarriage.
Diagnosis and Tests
How is a blighted ovum diagnosed?
Your healthcare provider will diagnose a blighted ovum using transvaginal ultrasound. This happens in the first trimester, usually between seven and nine weeks of pregnancy. An embryo should be visible at this time in pregnancy. With a blighted ovum, the gestational sac will be empty.
- You will lie back on an exam table and place your feet in stirrups like you do for a pelvic exam.
 Your healthcare provider will put an ultrasound wand into your vagina to see the contents of your uterus.
Your healthcare provider will put an ultrasound wand into your vagina to see the contents of your uterus. - A blighted ovum will appear as an empty sac — almost like a bubble.
A blighted ovum is when the gestational sac containing the embryo is empty.
People are often unaware that they have a blighted ovum. This is because your placenta continues to give off hormones, making your body think you are pregnant. This is also why you can still have symptoms of pregnancy, including a positive pregnancy test.
If you’ve already experienced bleeding or signs of a miscarriage, your healthcare provider will use ultrasound to look at the contents of your uterus to diagnose a blighted ovum.
Some healthcare providers will collect a series of blood samples that check the levels of hCG (human chorionic gonadotropin) in your body. HCG is known as the pregnancy hormone because it's only produced if you are pregnant. The level of hCG in your blood increases rapidly in early pregnancy and reaches its peak around weeks eight to ten. If it's not rising quickly, it can indicate a miscarriage or other complication. Your provider may decide to test your hCG levels over the course of several days to evaluate how your hCG levels are rising. This can be an effective tool for diagnosing blighted ovum.
If it's not rising quickly, it can indicate a miscarriage or other complication. Your provider may decide to test your hCG levels over the course of several days to evaluate how your hCG levels are rising. This can be an effective tool for diagnosing blighted ovum.
Management and Treatment
How is a blighted ovum treated?
For some people, there may be no treatment needed, because your body passes the embryo through your vagina (a miscarriage). If your body does not miscarry the embryo, there are other options to remove the contents of your uterus. Your healthcare provider will talk you through possible treatments:
- Dilation & Curettage (D&C): This is a surgical procedure to remove the contents of your uterus. Your healthcare provider will dilate, or open, the cervix and use medical tools and suction to remove the pregnancy tissues from your uterus. This is done under sedation or general anesthesia.
- Natural miscarriage: If it's safe, you may be able to watch and wait to see if your body eventually releases the pregnancy tissues.
 It can sometimes take days or weeks for this to start. Your healthcare provider will let you know if this is an option for you. You will experience cramping, abdominal pain and bleeding once the miscarriage begins.
It can sometimes take days or weeks for this to start. Your healthcare provider will let you know if this is an option for you. You will experience cramping, abdominal pain and bleeding once the miscarriage begins. - Medication-induced miscarriage: You may be given a medication called misoprostol to trigger your body to miscarry. This moves the process along and eliminates the time waiting for a miscarriage to start on its own. You will have cramping, abdominal pain and bleeding within 30 minutes to ten hours of taking the medication.
A follow-up appointment is usually scheduled four to six weeks after a miscarriage or D&C. You may be given another ultrasound to confirm the uterus is empty. Your healthcare provider will check for signs of infection and make sure there were no complications.
What are the complications of a blighted ovum?
Complications of a blighted ovum are uncommon, but the possible complications could include:
- Excessive bleeding or hemorrhage.

- Infection.
- Scarring (from the D&C procedure).
- Tears in the uterus (from the D&C procedure).
How long does it take to recover from a blighted ovum?
Recovering from a blighted ovum miscarriage or D&C can last from one or two weeks to a month. Cramping generally lasts up to a week, but bleeding can last several weeks. Your bleeding should get lighter until it stops completely.
You can resume normal activities when you feel comfortable. Bleeding can increase with strenuous activity or exercise. Hormones may remain in your body and delay your menstrual cycle. Most people will get their period within four to six weeks after a blighted ovum.
It may take longer to recover emotionally from a blighted ovum miscarriage. You may have feelings of sadness, anger or confusion. It’s OK to take time to grieve. Ask your friends and family for support.
Prevention
Can a blighted ovum be prevented?
A blighted ovum can’t be prevented. Some couples may want to do genetic testing on the tissue inside the uterus. This checks for underlying causes of your miscarriage and can be helpful to couples who have experienced multiple pregnancy losses.
Some couples may want to do genetic testing on the tissue inside the uterus. This checks for underlying causes of your miscarriage and can be helpful to couples who have experienced multiple pregnancy losses.
Outlook / Prognosis
How soon after a blighted ovum can I get pregnant again?
Most healthcare providers recommend having one or two regular menstrual cycles before trying to conceive again after any type of miscarriage.
What are my chances of having another blighted ovum?
Your chances of having another blighted ovum are low. Most people go on to have healthy, full-term pregnancies. If you experience more than one blighted ovum, your healthcare provider may suggest testing to determine if there is an underlying cause.
Living With
When should I see my healthcare provider?
Call your healthcare provider right away if you have any of these symptoms:
- Excessive bleeding from your vagina.
- Dizziness or fainting.

- Fever that does not go away.
- Symptoms that get worse over time.
- Severe pain that isn’t helped with pain medicine.
When should I go to the ER?
Go to the nearest ER If you experience heavy vaginal bleeding — more than two pads per hour for two consecutive hours — or have symptoms of anemia like dizziness, palpitations or paleness.
What questions should I ask my doctor?
Losing a pregnancy is upsetting and confusing. Do not be embarrassed to ask any questions you have. It's completely normal to have questions and feel emotional during this time. Some questions you may ask are:
- Can I let my body miscarry or should I take medication to induce a miscarriage?
- What are the risks of miscarriage?
- Do I have to have a D&C?
- What are the risks of a D&C?
- How long can I expect to bleed or have cramping?
- Is there any indication this will happen again?
- When can I start trying to conceive?
- Do I need to come back for another ultrasound?
Frequently Asked Questions
Is a blighted ovum considered a miscarriage?
Yes, a blighted ovum is a miscarriage. A miscarriage is a loss of pregnancy before 20 weeks. A blighted ovum is considered an early miscarriage because it occurs before 13 weeks of pregnancy.
A miscarriage is a loss of pregnancy before 20 weeks. A blighted ovum is considered an early miscarriage because it occurs before 13 weeks of pregnancy.
How long can you carry a blighted ovum?
The amount of time you can carry a blighted ovum varies. Your placenta will continue to grow and release hormones without an embryo. For some people, a miscarriage can occur within a few days or weeks. Others may still believe they are pregnant only to discover a blighted ovum at their first ultrasound.
Can a blighted ovum turn into a baby?
No, an empty gestational sac will not turn into an embryo. The formation of the embryo occurs within two weeks of conception. By the time the gestational sac is formed, the cells should have already formed the embryo. Your healthcare provider will be able to examine your gestational sac to confirm that no embryo has developed.
Do hCG levels rise with blighted ovum?
Yes, most of the time hCG levels will rise, giving you a positive pregnancy test and symptoms of pregnancy. This is because the placenta continues to give off hCG even if an embryo is not present. The hormone hCG is sometimes called the pregnancy hormone because it is only produced if you are pregnant.
This is because the placenta continues to give off hCG even if an embryo is not present. The hormone hCG is sometimes called the pregnancy hormone because it is only produced if you are pregnant.
Is a blighted ovum more common with IVF?
A blighted ovum is not more common with IVF (In Vitro Fertilization). Your chances of having a blighted ovum with IVF treatment are about the same as they would be with a natural conception.
A note from Cleveland Clinic
Losing a pregnancy is difficult. If you are struggling after a miscarriage, speak with your healthcare provider so they can recommend support groups or counselors. Finding support may help you get through this hard time. Most people who have had a blighted ovum will go on to have a healthy pregnancy.
symptoms, diagnosis, treatment of ovarian apoplexy - Department of Gynecology - State Hospital NCC No. 2 (CCH RAS)
Get a consultation with a gynecologist
or make an appointment
See all prices
+7 (499) 400-47-33
- Causes and mechanism of ovarian apoplexy
- Symptoms of ovarian apoplexy
- Diagnosis of ovarian apoplexy
- Treatment of ovarian apoplexy
Ovarian apoplexy is a hemorrhage in the ovary that can rupture the ovary and cause internal bleeding. Ovarian apoplexy is an acute, often life-threatening condition that requires immediate medical attention.
Ovarian apoplexy is an acute, often life-threatening condition that requires immediate medical attention.
Causes and mechanism of ovarian apoplexy
During the menstrual cycle, a follicle begins to develop in a woman's body, from which a formed egg will subsequently come out. In place of the follicle, the so-called "yellow body" appears - a formation that is involved in preparing for pregnancy. If pregnancy does not occur, the corpus luteum begins to reverse development and decreases. But in some cases this does not happen, the corpus luteum grows, its cysts may appear. Often the cause of ovarian apoplexy is a rupture of the corpus luteum or its cyst.
In healthy ovaries, apoplexy is not a frequent occurrence. As a rule, the walls of the ovaries and vessels are pathologically changed due to various inflammatory diseases and their consequences.
Violations of the integrity of the ovary can be provoked by physical activity, trauma (especially trauma to the abdomen), sexual intercourse, etc.
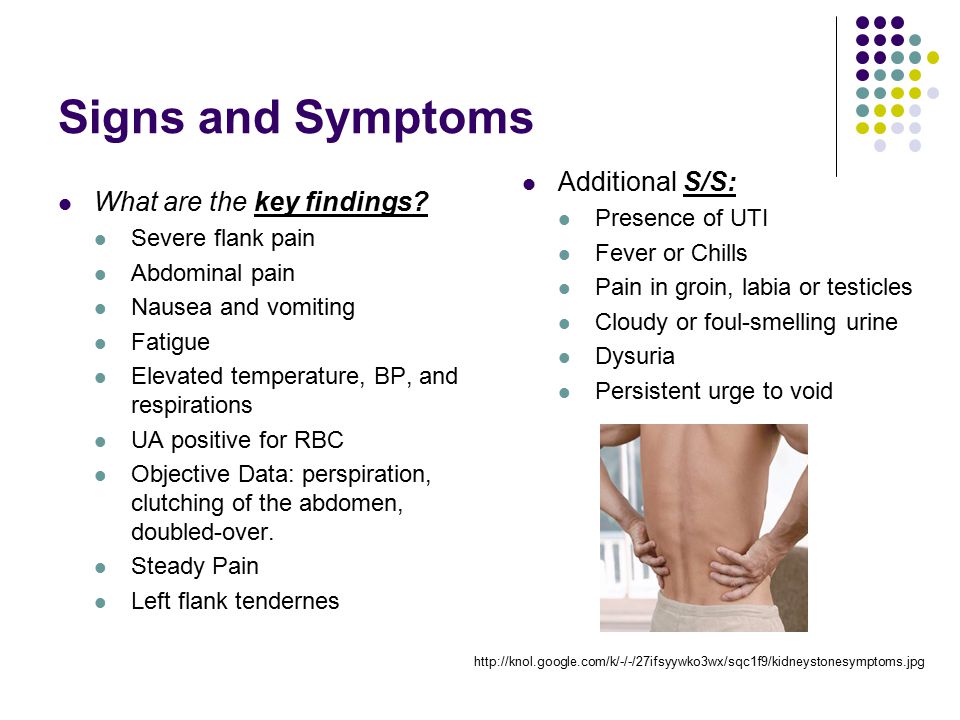
Symptoms of ovarian apoplexy
- Severe pain in the abdomen, usually in the lower abdomen; usually pain from the affected ovary
- Weakness, dizziness, chills
- Nausea
- Pale skin
- Fainting
All these symptoms are associated with internal bleeding, and if they occur, you should consult a doctor!
Diagnosis of ovarian apoplexy
Ovarian apoplexy gives symptoms, which in medicine is commonly called "acute abdomen". The doctor, conducting diagnostic measures, excludes pathologies such as appendicitis, ectopic pregnancy, etc. In most cases, to confirm ovarian apoplexy, the following are performed:
- Gynecological examination
- Blood test
- Ultrasound, which can see the presence of blood in the abdominal cavity, as well as the corpus luteum
- Laparoscopy (diagnostic) - examination of the abdominal cavity from the inside, through instruments with cameras inserted into small punctures on the abdomen.
 If necessary, diagnostic laparoscopy turns into a therapeutic one, and the doctor takes all the necessary measures to stop bleeding and restore the integrity of the ovary.
If necessary, diagnostic laparoscopy turns into a therapeutic one, and the doctor takes all the necessary measures to stop bleeding and restore the integrity of the ovary.
Treatment of ovarian apoplexy
The most effective, and often the only, method of treating ovarian apoplexy is surgical. In the vast majority of cases, the doctors of the gynecological department of the NCC No. 2 (CCH RAS) perform laparoscopy. The rupture of the ovary is sutured, when a cyst is found, its capsule is removed. Or coagulation of the site of rupture of the ovary is carried out. The consequences of bleeding into the abdominal cavity (blood clots), which could subsequently form adhesions, are eliminated. In extremely rare cases, when absolute indications are identified, doctors remove the ovary.
Conservative treatment of ovarian apoplexy, as a rule, is not carried out.
After surgery, patients can be prescribed physiotherapy procedures or other methods from the arsenal of rehabilitation medicine for the fastest possible recovery. Drug therapy is selected individually.
Drug therapy is selected individually.
Diagnosis of the cause of female infertility and treatment in gynecology at the polyclinic of the Literary Fund
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection?
- Rules for patients
- Online doctor's consultation
- to corporative clients
- Documentation
Conceiving a child is an urgent problem for many families. The program "Diagnosis of the causes of infertility", developed in the Polyclinic of the Litfond, allows you to effectively help couples to identify all the factors that led to infertility and solve this problem.
What are the causes of female infertility?
Often, hormonal imbalances are the cause of female infertility. This can lead to the absence of menstruation at all, or to the lack of maturation of the egg. In this case, violations can relate to both sex hormones and any others, for example, the thyroid gland, pancreas.
This can lead to the absence of menstruation at all, or to the lack of maturation of the egg. In this case, violations can relate to both sex hormones and any others, for example, the thyroid gland, pancreas.
The figure below shows the menstrual cycle, egg development, changes in the endometrium and changes in the hormonal background (for 4 hormones) in a healthy woman.
Hormonal causes of infertility
Hormonal causes of infertility can be caused by violations of the blood levels of such basic hormones as FSH (follicle stimulating hormone), LH (luteinizing hormone), prolactin, estradiol, progesterone, testosterone, DEA sulfate and others. As a rule, a comprehensive study of the hormonal status allows you to identify this cause and begin effective treatment of the identified disorder(s).
Problems with ovulation
If a woman does not have a regular menstrual cycle, or if the menstrual cycle is less than 21 days or more than 35 days, then there is a risk that the egg does not mature or is not viable.
At the same time, in almost half of the cases of the absence of ovulation, the ovaries do not produce mature follicles, from which eggs could then develop. Therefore, ovulation is impossible, mature eggs do not appear, there is nothing for spermatozoa to fertilize. This is the most common cause of female infertility.
The main purpose of examining women in this direction is to trace all stages of the formation, maturation and release of an egg ready for fertilization. An examination can reveal a violation at one of the stages or refute the presence of a violation in the maturation of the egg.
Ovarian dysfunction
Ovarian dysfunction (violation of the process of formation of a "young" egg [follicle]) in 20% of cases is the result of violations of hormone production in the hypothalamus-pituitary gland. If the activity of this system is disturbed, the corresponding signals do not enter the ovaries, and therefore the rhythmic production of hormones is disturbed. Luteinizing hormone (LH) and follicle stimulating hormone (FSH) are produced in too much or too little amounts, or their ratio is disturbed. Accordingly, the maturation of the follicle is disrupted, the egg either does not mature at all or is not viable.
Luteinizing hormone (LH) and follicle stimulating hormone (FSH) are produced in too much or too little amounts, or their ratio is disturbed. Accordingly, the maturation of the follicle is disrupted, the egg either does not mature at all or is not viable.
The easiest way to check the formation of follicles is an ultrasound examination (ultrasound) of the ovaries, which is performed on the seventh to ninth day of the menstrual cycle. At least a few follicles should form in one ovary.
Early menopause
Early menopause is rarely the cause of the lack of ovulation. The usual age of female menopause is 45-55 years, but in some women, egg reserves, for unclear reasons, are exhausted earlier, menstruation stops before 45 years. Many doctors are not inclined to consider this condition as the norm and talk about the ovarian function depletion syndrome. In some cases, this condition can be overcome with the help of hormonal treatment, physiotherapy, even the activation of sexual activity.
Polycystic ovaries
Polycystic ovaries are hormonal changes leading to the production of many dysfunctional (non-functional) follicles.
Among several follicles, one should mature - dominant, that is, superior in size to the rest and directly involved in ovulation. This happens closer to the middle of the menstrual cycle (on the 11-13th day). And this can be observed during an ultrasound examination. The untimeliness and inferiority of the maturation of the dominant follicle can be the cause of infertility. This infertility problem, called polycystic ovaries, is quite common.
Polycystic ovaries leads to both disturbances in hormone metabolism and changes in the ovaries. Outwardly, it is manifested by increased hair growth, menstrual irregularities or even amenorrhea, lack of ovulation, and infertility. In polycystic disease, the production of (FSH) is reduced, although the level of (LH), estrogen and testosterone is within the normal range or elevated. It is believed that low FSH levels cause permanent underdevelopment of the follicles produced by the ovaries, and therefore the absence of mature eggs. In this case, many follicular cysts up to 6-8 mm in size are formed, which can be easily seen using ultrasound (ultrasound). The affected ovary is usually enlarged by 2 times, its surface is covered with a smooth white capsule, through which even a mature egg cannot pass. This disease successfully gives in to effective and adequate treatment.
It is believed that low FSH levels cause permanent underdevelopment of the follicles produced by the ovaries, and therefore the absence of mature eggs. In this case, many follicular cysts up to 6-8 mm in size are formed, which can be easily seen using ultrasound (ultrasound). The affected ovary is usually enlarged by 2 times, its surface is covered with a smooth white capsule, through which even a mature egg cannot pass. This disease successfully gives in to effective and adequate treatment.
Inflammatory process in the ovaries
The mature dominant follicle must break the ovarian membrane. With inflammation, the wall thickens significantly, respectively, the follicle cannot exit the ovary. This is another reason for infertility. Before you start trying to get pregnant, you need to analyze for the presence of hidden infections, including genital infections, because they most often cause a sluggish inflammatory process in the ovaries and affect both conception and the course of pregnancy.
Damage to fallopian tubes
Damage to the fallopian tubes - their complete obstruction, as well as altered tube mobility.
Released from the dominant follicle and ready for fertilization, the egg goes to the fallopian tubes and is there, waiting for the sperm. Naturally, if the patency of the tubes is broken, fertilization will be extremely difficult.
Most often, the pipes are damaged as a result of inflammation caused by sexually transmitted infections. At the same time, violations in the tubes can be very different - from damage to the cilia lining the tubes from the inside, to the formation of hydrosalpinx (accumulation of fluid in the fallopian tube, sealed as a result of inflammation).
Hysterosalpingography is used to determine the patency of the fallopian tubes. The essence of this method is that a contrast agent is injected into the uterine cavity, and under X-ray control, the movement of the contrast through the fallopian tubes and its penetration into the abdominal cavity is checked, there is also a sonohysterography method - checking the patency of the fallopian tubes using ultrasound.
Uterine disorders
Any formations that deform the uterine cavity act as an intrauterine device, preventing the egg from attaching to the endometrium. Such diseases include polyps of the uterine mucosa, uterine myoma, endometrioid formations, as well as congenital anomalies in the development of the uterus - a saddle, bicornuate uterus, a uterus with an incomplete septum, complete doubling of the uterus, and others.
Many diseases affect the quality of cervical mucus. If it is too thick, then the spermatozoa cannot overcome it. If the mucus is poisonous to sperm (by chemical composition or due to immune characteristics), then they will simply die.
True erosion of the cervix , as well as polyps of the cervical canal can cause infertility due to changes in mucus, and therefore require mandatory removal before infertility treatment.
Endometriosis
Normally, endometrial cells form the inner surface of the uterus, help the embryo to feed, and in the absence of pregnancy are involved in menstruation. With endometriosis, endometrial cells grow, forming something like polyps or deep "pockets" in the thickness of the uterus, they can penetrate into the fallopian tubes, ovaries, and even into the abdominal cavity. Endometriosis interferes with the maturation of the egg, interferes with the fusion of the egg and sperm, and also disrupts the attachment of the fertilized egg to the uterine wall.
With endometriosis, endometrial cells grow, forming something like polyps or deep "pockets" in the thickness of the uterus, they can penetrate into the fallopian tubes, ovaries, and even into the abdominal cavity. Endometriosis interferes with the maturation of the egg, interferes with the fusion of the egg and sperm, and also disrupts the attachment of the fertilized egg to the uterine wall.
Psychological reasons
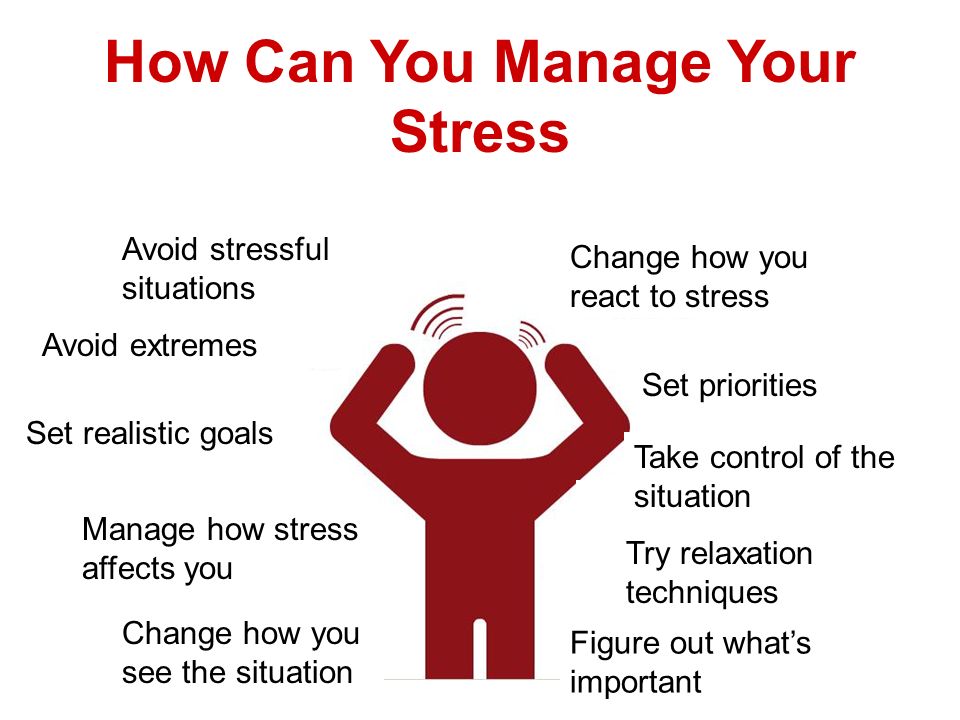
Psychological causes are also the cause of infertility. There are known conditions such as wartime amenorrhea, stress amenorrhea, even examination amenorrhea, when the functions of hormone-dependent organs are disrupted due to stress.
Psychological causes include idiopathic infertility (infertility of unknown origin). A woman (less often a man) subconsciously developed a negative attitude towards a possible pregnancy, and therefore the body itself automatically does not allow the processes leading to conception to take place.
If all the causes of infertility that have already been mentioned are absent in a married couple, then in this case, infertility treatment is not required.