Week long migraine
Status Migrainosus: Symptoms, Treatment, Prevention
Written by Eric Metcalf, MPH
Medically Reviewed by Jennifer Robinson, MD on August 12, 2022
In this Article
- Symptoms
- Treatment
- Migraine Prevention
Migraines are a type of headache that tend to cause other symptoms, too, such as nausea and vision problems. They can last for a few hours to a few days. But a migraine that lasts for more than 72 hours is called status migrainosus. To treat it, you may need to go to the hospital to get help relieving the pain and dehydration from vomiting.
A typical migraine can sometimes turn into status migrainosus if:
- You don’t get treatment early enough after the attack starts.
- You don’t get the right treatment.
- You use too much headache medicine.
Symptoms
The warning signs of status migrainosus are similar to those of a typical migraine. Along with pain in your head, you might also feel:
- Sensation of sparkling lights or other vision changes (aura)
- Nausea and vomiting
- Trouble thinking clearly
Because the condition lasts for at least 3 days, you’re also at risk for dehydration and sleep loss because of prolonged vomiting and pain.
Treatment
If you have to go to an emergency room or stay in the hospital because of status migrainosus, doctors may need to treat other problems the migraine causes as well as the migraine itself.
In the hospital, doctors may give you drugs through an IV to control pain. They'll treat dehydration by giving you fluids through an IV.
Drugs that stop vomiting include:
- chlorpromazine
- metoclopramide (Metozolv, Reglan)
- prochlorperazine (Compro, Procomp)
A common medicine for halting status migrainosus is dihydroergotamine (DHE-45, Migranal). You can take it as a nasal spray or through a shot. Another drug, sumatriptan (Imitrex, Onzetra, Sumavel DosePro, Zecuity), comes as a shot, nasal spray, pill, or skin patch. Valproate, given by vein, can also be used.
People with certain medical problems should avoid these medicines though.
The corticosteroids dexamethasone (Dexamethasone Intensol, Dexpak) and prednisolone can also relieve status migrainosus.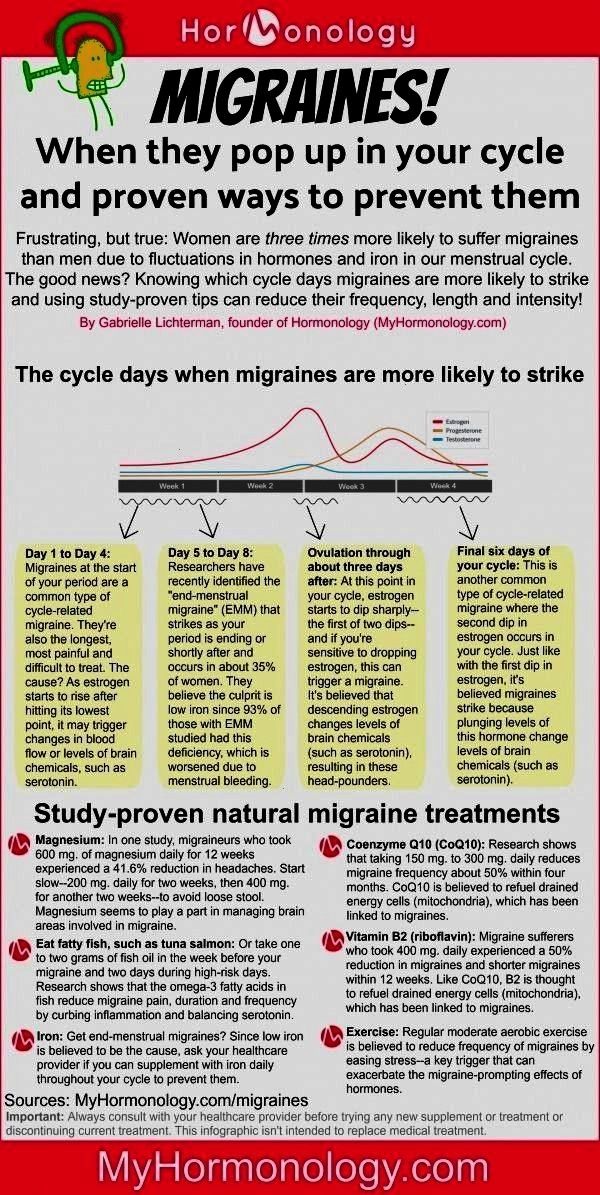
Migraine Prevention
If you don’t respond to other treatments and you have 4 or more migraine days a month, your doctor may suggest preventive medicines. You take these regularly to reduce the severity or frequency of the headaches. These include seizure medicines, blood pressure medicines (like beta blockers and calcium channel blockers), and some antidepressants. CGRP inhibitors are a new class of preventive medicine that your doctor may recommend if other medicines don’t help.
Botox, though better known as a treatment for wrinkles, has also been approved by the FDA to prevent recurring migraines. Natural options such as magnesium may work but we need more research to know which of these treatments are effective.
There are a couple of devices designed to interrupt abnormal electrical activity in the brain associated with migraine. A device called SpringTMS or eNeura sTMS uses a technique called transcranial magnetic stimulation (TMS). Place it on the back of your head for about a minute for release of a pulse of magnetic energy. Similarly, Cefaly uses transcutaneous supraorbital nerve stimulation and is worn as a headband on the forehead and turned on daily for 20 minutes to prevent migraine from developing. There is also a noninvasive vagus nerve stimulator called gammaCore. When placed over the vagus nerve in the neck, it releases a mild electrical stimulation to the nerve's fibers to relieve pain.
Similarly, Cefaly uses transcutaneous supraorbital nerve stimulation and is worn as a headband on the forehead and turned on daily for 20 minutes to prevent migraine from developing. There is also a noninvasive vagus nerve stimulator called gammaCore. When placed over the vagus nerve in the neck, it releases a mild electrical stimulation to the nerve's fibers to relieve pain.
Migraine Headaches | Johns Hopkins Medicine
By far the most common type of headache we see in our practice, migraines are the most frequent cause of disabling, recurring headache pain.
-
What are the symptoms of a migraine?
-
How prevalent are migraines?
-
What triggers a migraine?
-
How are migraines diagnosed?
-
How are migraines treated?
Individual migraines are moderate to severe in intensity, often characterized by a throbbing or pounding feeling. Although they are frequently one-sided, they may occur anywhere on the head, neck and face — or all over. At their worst, they are typically associated with sensitivity to light, noise and/or smells. Nausea is one of the most common symptoms and it worsens with activity, which often results in patient disability. In many respects, migraines are much like alcohol-related hangovers.
Although they are frequently one-sided, they may occur anywhere on the head, neck and face — or all over. At their worst, they are typically associated with sensitivity to light, noise and/or smells. Nausea is one of the most common symptoms and it worsens with activity, which often results in patient disability. In many respects, migraines are much like alcohol-related hangovers.
Migraine pain can be felt in the face, where it may be mistaken for sinus headache — or in the neck, where it may be mistaken for arthritis or muscle spasm. Complicating the diagnosis of migraine is that the headaches may be accompanied by other "sinus like" symptoms, including watering eyes, nasal congestion and a sense of facial pressure. Most patients who think they have sinus headache in fact have migraines.
In up to 25 percent of patients, the migraine headache pain may be preceded by an aura, a temporary neurological syndrome that slowly progresses and then typically resolves just as the pain begins. While the most common type of migraine aura involves visual disturbances (flashing lights, zigzags, blind spots), many people experience numbness, confusion, trouble speaking, vertigo (spinning dizziness) and other strokelike neurological symptoms. Some patients may experience auras without headaches.
While the most common type of migraine aura involves visual disturbances (flashing lights, zigzags, blind spots), many people experience numbness, confusion, trouble speaking, vertigo (spinning dizziness) and other strokelike neurological symptoms. Some patients may experience auras without headaches.
Migraines are about three times more common in women than men, and may affect more than 12 percent of the U.S. adult population. Migraines often run in families, and can start as early as elementary school but most often in early adulthood. They often fade away later in life, but can strike at any time. The most common cause of recurring, disabling headache pain, migraines are also the most common underlying cause of disabling chronic, daily headache pain. While migraines are the No. 1 reason that patients see a neurologist, most cases are handled by primary care physicians.
Things that can make the headaches more likely to occur include:
Despite their dramatic symptoms, migraines are almost never due to an underlying problem that will show up on any testing, even on brain MRIs. Many experts do not recommend brain imaging at all, even in severe cases, as long as the patient's symptoms are typical for migraines and a thorough neurological examination is normal.
Many experts do not recommend brain imaging at all, even in severe cases, as long as the patient's symptoms are typical for migraines and a thorough neurological examination is normal.
There are extremely rare families that have migraines as a result of a single genetic mutation in one of four known genes that can lead to the condition called familial hemiplegic migraine. There are no genetic tests for the vast majority of patients. Because the condition cannot be diagnosed by scan or blood test, the diagnosis is "clinical" — made by an experienced physician.
Migraines that are severe, frequent or accompanied by neurological symptoms are best treated preventively, usually with a combination of dietary modification, lifestyle changes, vitamins and daily prescription medications. Most of our best preventive medications are often used for other medical purposes as well; the majority are blood pressure drugs, antidepressants or epilepsy medications. Individual headache attacks are best treated early, often with one or more of the following types of medications: triptans, nonsteroidal anti-inflammatory drugs (NSAIDs), anti-emetics (anti-nausea), and sometimes narcotics or steroids.
Migraines typically last a few hours to a couple of days and respond well to specific treatments. However, in some patients, the migraine is particularly severe and long-lasting — and may even become chronic, occurring continuously for weeks, months or even years. If improperly managed or left untreated, intermittent migraines may essentially transform into a chronic daily headache, with continuous and smoldering symptoms that periodically erupt into a "full-blown" migraine. This condition is extremely difficult to treat.
Other patients may develop increasingly frequent headaches as a result of overusing their short-acting headache medications. See medication overuse headache. While they are considered primary headaches, meaning they have no known underlying cause, migraines are associated with an increased risk of stroke, brain scarring as seen on MRI scans, a heart defect called a patent foramen ovale (PFO) and other medical conditions.
At the Johns Hopkins Headache Center, located at the Johns Hopkins Bayview Medical center, we have expert physical therapists, nutritionists and psychologists who work closely with our neurologists to help manage patients with frequent migraines. Biofeedback and relaxation techniques are available to complement our standard medical treatments.
Biofeedback and relaxation techniques are available to complement our standard medical treatments.
How do neurologists explain the phenomenon — TsM Zdravitsa
Marina Aleksandrovna, how often do such complaints occur in practice?
- I encounter this phenomenon from time to time, it is very clearly reflected in the "headache diary" kept by the patient. Occasionally occurring "weekend migraine" can transform into more frequent attacks, and vice versa, during the treatment of chronic migraine, when the patient takes control of his disease, we observe intermittent "weekend" attacks.
How can this phenomenon be explained?
– This mysterious phenomenon has been haunting the minds of physicians for a long time. Scientists conducted an observation, and during the study it was found that 30% of migraine attacks occurred at the end of the working week on Friday, while 50% of migraine attacks were recorded on Saturday, on Sunday - 30%. A significant decrease in the number of attacks was noted by patients in the middle of the week (Wednesday, Thursday).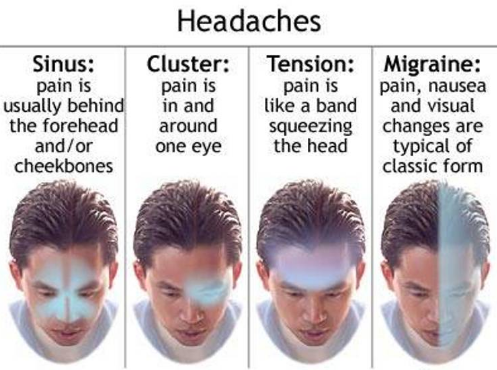
What does it depend on? There are several points of view. First of all, this phenomenon is associated with a violation of the regime, because we can afford a lot on weekends. We can not sleep for a day, doing some business. Sleep deprivation causes headaches. But, and the most interesting thing is that it is excessive sleep on weekends that is accompanied by more severe migraine attacks.
Does it mean that “sleeping on weekends” is harmful?
– Yes, it is a mistake to think that “sleeping on the weekends” is good. Most living organisms, including you and me, have autonomously regulated complexes of endogenous time programs that are synchronized with the 24-hour cycle of light and dark. These internal endogenous rhythms are called circadian rhythms (from Latin circa - about and dias - day), they are triggered by mechanisms that are metaphorically called "biological clocks".
Many of the existing weekly patterns of cyclical changes are strictly related to the 5-6 day cycle of working and rest days. Relatively speaking, during the working week, the tone of the vascular wall, hormones, and other mechanisms that are regulated by the hypothalamus work in a regular cyclic rhythm.
Relatively speaking, during the working week, the tone of the vascular wall, hormones, and other mechanisms that are regulated by the hypothalamus work in a regular cyclic rhythm.
In case of failures of the regular habitual cyclicity, the mechanisms of homeostasis control are accordingly violated.
Scientists suggest that inadequate secretion of melatonin (the "sleep hubbub") contributes to the development of migraine attacks by weakening its direct analgesic effect or reducing the anti-inflammatory effect that it has.
In addition, a direct link between migraine and delayed sleep phase syndrome (SSPS) has been found through a mutation in the casein kinase-1-delta gene, which belongs to the group of clock genes. The study of the causes leading to the transformation of episodic migraine into chronic migraine showed that the presence of long-term sleep disorders and subjective dissatisfaction with night sleep are the most important factors in migraine chronicity.
How can the situation be improved?
– Good sleep is of great importance for the normal functioning of the nervous system, as well as for the whole organism. Sleep is the inhibition of the nervous system, necessary to save it from overexertion.
On average, a person should sleep 8 hours a day. To prevent "weekend headaches", it is important to stay on "sleep hygiene strategies" on the weekends as well. However, some people use the time allotted for sleep as a reserve for unfinished business, which triggers "failure mechanisms." Systematic lack of sleep negatively affects mental and physical activity, a person becomes aggressive, irritable and nervous.
In the study of the characteristics of the course of episodic and chronic migraine in 200 patients in 46.5% of cases, the regular occurrence of migraine attacks after a change in sleep patterns was revealed. The daily routine should be considered as a regulated factor of vital activity that affects the human body.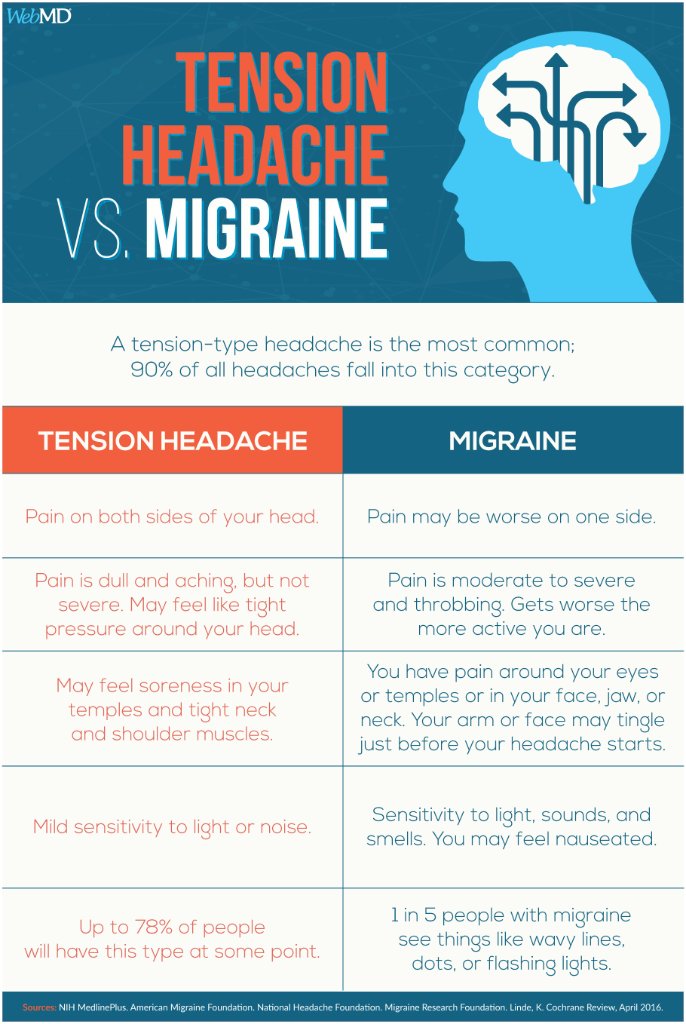
So, in the treatment of migraine, the first item in the recommendations to patients is far from drugs, but lifestyle correction. Often, adherence to the daily routine, diet, rejection of bad habits, a stable emotional background lead to a regression of headaches. For the doctor and effective treatment of headaches, the active participation of the patient himself in this matter is very important.
Read more
Chronic migraine
What is chronic migraine?
Chronic migraine - a disease in which the head hurts 15 days a month or more. At the same time, attacks typical of migraine occur at least eight times a month . This is the description given by the III International Classification of Headaches.
How does chronic migraine occur?
Usually, before a person develops a chronic migraine, they have fewer attacks (episodic migraine). When the disease becomes chronic, the headache may lose its migraine features. It can become bilateral, compressive rather than pulsating. Concomitant symptoms become weaker - vomiting, photo and sound fear. However, although chronic migraine is less similar to classical migraine, it is also sensitive to specific anti-migraine drugs - triptans.
It can become bilateral, compressive rather than pulsating. Concomitant symptoms become weaker - vomiting, photo and sound fear. However, although chronic migraine is less similar to classical migraine, it is also sensitive to specific anti-migraine drugs - triptans.
Video
See allWhat is migraine and how to deal with it. Lecture by a neurologist-cephalologist.
Migraine. Problems of diagnosis and treatment. Lecture for neurologist Yulia Azimova
Why do we have a headache? How to treat a migraine? Neurologist Kirill Skorobogatykh
What is the problem with treating chronic migraine?
Up to 3-4% of people worldwide suffer from chronic daily or almost daily headache. The main cause of which is chronic migraine. However, it is usually difficult for doctors to diagnose it. They take it for chronic tension headache, believe that pain is caused by osteochondrosis or insufficient blood supply to the brain (which does not correspond to modern scientific ideas about the nature of migraine at all).
They take it for chronic tension headache, believe that pain is caused by osteochondrosis or insufficient blood supply to the brain (which does not correspond to modern scientific ideas about the nature of migraine at all).
What actually causes chronic migraine?
There have been large studies that have shown that the development of chronic migraine is affected by:
- overweight,
- depression, stress and/or anxiety,
- hypothyroidism,
- increased incidence of episodic migraine attacks.
One of the significant factors in the transition of migraine to chronic is also considered previous, even for many years, physical or emotional abuse.
However, whether this is a cause or a consequence of chronic migraine is still under discussion. What has been scientifically proven: at the initial stage of the development of chronic migraine, when rare attacks become more frequent, certain biochemical changes occur in the brain. The brain “learns” pain. If preventive treatment is started at this stage, chronic migraine can be prevented. If more than 6 months have passed since the onset of chronic migraine, the chances of success decrease. Therefore, it is important not to delay treatment.
The brain “learns” pain. If preventive treatment is started at this stage, chronic migraine can be prevented. If more than 6 months have passed since the onset of chronic migraine, the chances of success decrease. Therefore, it is important not to delay treatment.
What to do if you suspect that your migraine attacks have become more frequent?
- Start keeping a headache diary. For example @Migrebot in Telegram. You need to consider how many days per month you are "out of life" due to migraines, what medications, including over-the-counter medications, and how much you take, what events preceded the increase in attacks (head injury, started taking a new medication, etc.). ). Try to remember how many times a month your head hurt before
- Contact a specialist. Chronic migraine is much easier to prevent than to treat. Don't wait until it becomes daily!
- If you are taking opiate/opioid painkillers (codeine, hydrocodone, meperidine, tramadol, oxycodone) and medicines containing butalbital, you will need to stop or cut back on them.

If the headache has already become chronic
- do not tolerate headache, relieve attacks quickly and aggressively (take a sufficient dose of the drug at the beginning of an attack). At the same time, avoid taking the drug of the same class too often. Ask your doctor to advise you on several drugs of various pharmacological groups;
- actively use non-pharmacological methods of treatment;
- if you are overweight, try to get rid of it;
- Ask a specialist for help with co-morbidities, if any. It is necessary to treat depression, anxiety, sleep disorders.
Openness and honesty between doctor and patient is especially important in the treatment of chronic migraine. Thanks to partnerships, timely treatment of developing chronic migraine can give a wonderful result.
Literature:
- "International classification of headaches 2nd edition (full Russian version)" , 2006, 380 p.