Itchy eyes during pregnancy
Pregnancy rhinitis | Pregnancy Birth and Baby
Pregnancy rhinitis | Pregnancy Birth and Baby beginning of content5-minute read
Listen
If you have unexplained breathing problems, see your doctor as soon as possible. If your breathing problems are very bad and come on quickly, call triple zero (000) for an ambulance.
What is pregnancy rhinitis?
Pregnancy rhinitis usually involves a stuffy nose, itchy eyes, and post-nasal drip. These symptoms seem to come out of nowhere during pregnancy. While it's not a life-threatening medical condition, pregnancy rhinitis can be bothersome. There are things you can do to find some relief.
What are the symptoms pregnancy rhinitis?
Symptoms of pregnancy rhinitis are like those of allergic rhinitis (hay fever). These include:
- a runny or congested nose
- sneezing
- itchy eyes
- watery eyes
While it might feel like you are getting a cold, pregnancy rhinitis is not associated with bacterial or viral infection. This means it is not contagious.
CHECK YOUR SYMPTOMS — If you are feeling unwell and not sure what to do next, check your symptoms using the healthdirect Symptom Checker tool.
What causes pregnancy rhinitis?
Rhinitis is an inflammation of the lining of your nose.
People who are affected by allergies may also experience similar symptoms during pregnancy. In these circumstances, symptoms are triggered by one or more allergens. These allergens may be seasonal, such as:
- pollens
- fungi
- moulds
Or they can be perennial (year-round) such as:
- dust mites
- pets
- cockroaches
Rhinitis in pregnancy may also have a non-allergic origin. It's not known exactly why rhinitis occurs more frequently in pregnancy. Some research suggests that factors such as hormones increase the likelihood of rhinitis during pregnancy.
It's not known exactly why rhinitis occurs more frequently in pregnancy. Some research suggests that factors such as hormones increase the likelihood of rhinitis during pregnancy.
Smoking is also associated with pregnancy rhinitis. It's never too late for future parents to quit smoking.
How is pregnancy rhinitis diagnosed?
Pregnancy rhinitis should be distinguished from other conditions such as infections. Your doctor can do this during a routine visit.
You may have a breathing problem if:
- you feel you can't get enough air through both your nose and mouth
- you are breathless
- you feel like you're being suffocated
- your chest feels very tight
- you are needing more of your usual asthma or lung medications
If you have unexplained breathing problems, see your doctor as soon as possible. If your breathing problems are very bad and come on quickly, call triple zero (000) for an ambulance.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How long will my symptoms last?
While pregnancy rhinitis can occur at any time during your pregnancy, it is most common during the first trimester.
Symptoms may last for at least 6 weeks. The good news is they usually disappear within 2 weeks of your baby's birth.
How is pregnancy rhinitis treated?
Your pregnancy rhinitis may be triggered by a known allergen. If this is the case, you can try and avoid or limit your exposure to the allergen.
Nasal irrigation is a drug-free technique to clear out air-borne allergens and mucus from blocked nostrils.
Using salt water (saline) nasal sprays can provide relief and is a good solution during pregnancy.
Persistent symptoms are managed individually. If you have itchy-watery eyes, there are certain eye drops that are approved for use during pregnancy. Similarly, specific medicated nasal sprays and antihistamines can be used.
Similarly, specific medicated nasal sprays and antihistamines can be used.
However, always check with your doctor or pharmacist before taking any medicine while pregnant.
Is there an impact on my unborn baby?
There are insufficient studies to fully understand the impact of pregnancy rhinitis on the growth and development of unborn babies.
However, any condition that reduces your quality of life has the potential to affect your baby. This includes the quality of your sleep during pregnancy.
If you are concerned about your sleep or breathing during pregnancy, speak to your doctor. They can help you find the best way to clear your breathing passages and improve your sleep.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Auris Nasus Larynx (Medical Management of rhinitis in pregnancy), American Journal of Rhinology & Allergy (Redefining Pregnancy-induced Rhinitis), International Journal of Chemistry, Mathematics and Physics (Chronic Rhinosinusitis and Its Impact on Pregnancy), South Eastern Sydney Local health District/The Royal Hospital for Women (Hay Fever in Pregnancy and Breastfeeding), The Royal Women’s Hospital (Medicines in Pregnancy), Australasian Society of Clinical Immunology and Allergy (ASCIA) (Allergic Rhinitis Clinical Update)Learn more here about the development and quality assurance of healthdirect content.![]()
Last reviewed: July 2022
Back To Top
Related pages
- Medicines during pregnancy
- Cold and flu during pregnancy and breastfeeding
- Allergies: controlling your environment
- Airborne allergies
- Allergies and hay fever during pregnancy
Need more information?
Allergic rhinitis - symptoms, causes and treatment - MyDr.com.au
Rhinitis means inflammation of the lining of the nose. Allergic rhinitis means that this inflammation is caused by an allergy.
Read more on myDr website
Allergic rhinitis (hay fever)? - Australasian Society of Clinical Immunology and Allergy (ASCIA)
Allergic rhinitis (commonly known as hay fever) affects around 18% of people in Australia and New Zealand. It can affect children and adults.
It can affect children and adults.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Allergic Rhinitis (hayfever) - Allergy & Anaphylaxis Australia
Allergic rhinitis (hay fever) is one of the most common allergic conditions affecting 1 in 5 people in Australia. It is caused by the body’s immune system reacting to common allergens in the environment such as pollen, house dust mite, moulds and animal danders (skin cells and fur).
Read more on Allergy and Anaphylaxis Australia website
Hay Fever (Allergic Rhinitis) - Australasian Society of Clinical Immunology and Allergy (ASCIA)
The Australasian Society of Clinical Immunology and Allergy (ASCIA) is the peak professional body of clinical immunology and allergy in Australia and New Zealand. ASCIA promotes and advances the study and knowledge of immune and allergic diseases, including asthma.
ASCIA promotes and advances the study and knowledge of immune and allergic diseases, including asthma.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Immunotherapy for Allergic Rhinitis (Hay Fever) - Allergy & Anaphylaxis Australia
Allergen Immunotherapy (AIT) has been used for over 100 years and is a proven treatment providing long-term relief for hay fever. The aim of AIT is to help people react less to their trigger allergen/s that cause symptoms (such as grass pollen/house dust mite). This means having no/less symptoms and a better quality of life.
Read more on Allergy and Anaphylaxis Australia website
Pollen - a trigger for hay fever - National Asthma Council Australia
Plant pollen is well known as a trigger for seasonal allergic rhinitis (hay fever) and seasonal allergic conjunctivitis.
Read more on National Asthma Council Australia website
Hay Fever & Asthma | Hay Fever-related Asthma Causes & Symptoms - Asthma Australia
Hay fever is a common allergy, also known as allergic rhinitis, that can also trigger asthma flare-ups. Learn more about hay fever-related asthma & symptoms here.
Read more on Asthma Australia website
Other Allergic Conditions - Allergy & Anaphylaxis Australia
Other Allergic Conditions included: Urticaria (Hives), Eczema (Atopic Dermatitis), Allergic Conjunctivitis, Allergic Rhinitis (hayfever), Sinusitis
Read more on Allergy and Anaphylaxis Australia website
Thunderstorm asthma - Australasian Society of Clinical Immunology and Allergy (ASCIA)
It seems reasonable to think that rain would relieve allergic rhinitis (hay fever) and asthma triggered by pollen, by washing pollen out of the air. However, rain from some thunderstorms can make some people's symptoms worse. Epidemics of thunderstorm asthma in Australia have occurred in Melbourne and Wagga Wagga.
However, rain from some thunderstorms can make some people's symptoms worse. Epidemics of thunderstorm asthma in Australia have occurred in Melbourne and Wagga Wagga.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Allergy Treatments - Australasian Society of Clinical Immunology and Allergy (ASCIA)
The Australasian Society of Clinical Immunology and Allergy (ASCIA) is the peak professional body of clinical immunology and allergy in Australia and New Zealand. ASCIA promotes and advances the study and knowledge of immune and allergic diseases, including asthma.
Read more on ASCIA – Australasian Society of Clinical Immunology and Allergy website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Dry eyes during pregnancy: Symptoms, causes, treatments
If the eyes do not produce enough tears or cannot maintain a healthy moisture layer, a person may have dry eye syndrome. People may experience dry eyes during pregnancy due to fluctuating hormone levels.
The overall rate of dry eyes is higher during pregnancy. Doctors do not fully understand what causes this phenomenon, but hormonal shifts may make it more difficult for the eyes to produce enough tears. Dry eyes in pregnancy can be uncomfortable, but several treatments can help.
This article discusses the symptoms and causes of dry eyes in pregnancy. It also explains the home remedies and medical treatments that people can use to manage this condition.
It also explains the home remedies and medical treatments that people can use to manage this condition.
A note about sex and gender
Sex and gender exist on spectrums. This article will use the terms “male,” “female,” or both to refer to sex assigned at birth. Click here to learn more.
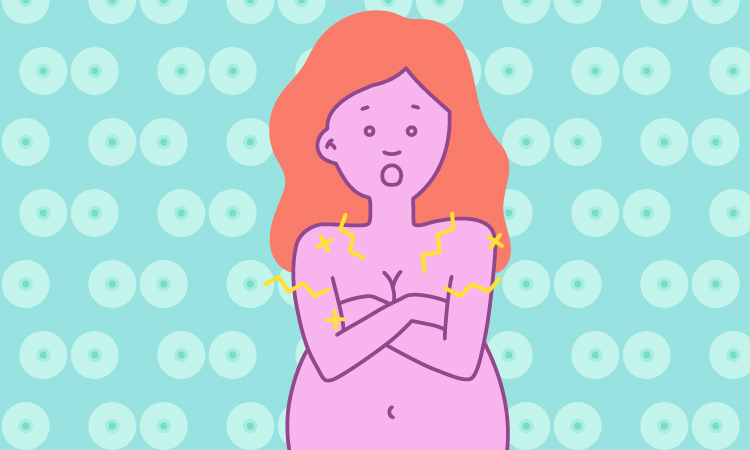
An individual may notice the following dry eye symptoms:
- eyes that feel dry, itchy, or uncomfortable
- feeling the need to blink frequently
- sensitivity to light
- watery eyes
- dried mucus or stringy fluid in the corners of the eyes
- red eyes
- trouble putting in or taking out contact lenses, in those who wear them
- changes in vision
- a sensation of the eyes feeling tired or droopy
- feeling as though something is in the eyes
Researchers do not yet fully understand why pregnant people commonly experience dry eyes, but several studies support this finding. For example, a 2019 study of 134 pregnant people in Nigeria found that dry eyes peaked in the third trimester, with the lowest rates at 6 weeks postpartum.
Females are more likely than males to have dry eyes, especially when hormonal changes occur, such as during pregnancy or menopause or when taking some forms of birth control.
Males have higher levels of hormones called androgens, which include testosterone. These hormones may protect them from dry eyes because they support tear production from the lacrimal glands. Although females also have these sex hormones, their levels are lower, which might explain why they have higher rates of dry eyes than males.
Androgens alone cannot explain dry eyes during pregnancy, as these hormones usually increase during pregnancy. For example, testosterone levels rise by about 70% during pregnancy.
However, the levels of estradiol — a hormone present in higher levels in most females — also increase with pregnancy. Estradiol may counteract the protective effects of androgens by suppressing genes that help with tear production. This action might explain why more people experience dry eyes as their pregnancy progresses.
Aside from hormone fluctuations, various other health conditions and lifestyle factors can cause dry eyes. People should, therefore, see a doctor for an evaluation. Other potential causes of dry eyes include:
- allergies
- vitamin A deficiency
- spending prolonged periods using computer or phone screens
- autoimmune diseases, such as lupus
- medications, such as antihistamines and nonsteroidal anti-inflammatory drugs
People may find that skin issues such as rosacea and eczema cause dry eyes. These skin conditions may worsen during pregnancy and further compound the problem of hormone-associated dry eyes.
Some home remedies and lifestyle adjustments may help ease symptoms of dry eyes. People can try:
- drinking plenty of water to prevent dehydration
- using a humidifier to prevent the air from becoming too dry
- applying over-the-counter artificial tears
- taking a fatty acid supplement, such as fish oil or an omega-3 supplement
- wearing sunglasses outside to minimize sun damage to the eyes
- trying warm compresses or eyelid massage
- avoiding fans or heaters near the face, which can further dry the eyes
People should also avoid using potential irritants, such as certain lotions and creams, around the eyes.:strip_icc():format(jpeg)/kly-media-production/medias/2785562/original/028627600_1556001360-shutterstock_1019963743.jpg) If an individual uses several products, they can try eliminating one product at a time and logging their symptoms. For example, a person might find that their eyes only become dry when using a specific brand of mascara.
If an individual uses several products, they can try eliminating one product at a time and logging their symptoms. For example, a person might find that their eyes only become dry when using a specific brand of mascara.
Doctors must determine the cause of dry eyes before they can treat them. If someone has an underlying illness, such as an autoimmune disease, a doctor may refer them to a specialist while offering prescription eye drops or other treatments.
Medical treatment options include:
- Prescription drops: A doctor might prescribe prescription-strength artificial tears or eye drops to reduce inflammation.
- Tear plugs: A doctor can fit removable tear plugs into the tear ducts, which help the tears remain in the eyes for longer.
- Steroids: Steroids can help treat some types of eye inflammation. A doctor may recommend using steroid creams on the eyelids or trying steroid eye drops.
- Moisture goggles: Wearing moisture goggles at night can help keep the eyes lubricated.
 A doctor may recommend using the goggles alongside eye drops or ointments.
A doctor may recommend using the goggles alongside eye drops or ointments. - Antibiotics: Some antibiotics have anti-inflammatory properties and may help relieve the symptoms of dry eyes. However, these treatments may not be suitable during pregnancy.
- Surgery: A doctor may recommend surgery if other treatments do not alleviate the symptoms. One option is to seal the tear ducts permanently, keeping tears in the eyes for longer. Another procedure, called tarsorrhaphy, sews parts of the upper and lower eyelids together to narrow the eye opening and reduce dryness. Skin grafts may also help.
For most people, dry eyes are a minor annoyance rather than a serious medical condition. People who notice dry eyes for the first time during pregnancy may find that their symptoms improve after delivery.
There is a lack of extensive research on how dry eyes may progress if someone does not treat the condition. For many people, dry eyes become a chronic condition that may improve or worsen at times. With home treatment, symptoms may improve. When they do not, a person may need more intensive medical care.
With home treatment, symptoms may improve. When they do not, a person may need more intensive medical care.
Pregnant people should talk with a doctor before trying home remedies, as some options may not be safe during pregnancy.
The hormone fluctuations that people experience during pregnancy can worsen dry eyes. Although seldom a serious condition, individuals may find dry eyes unpleasant and have difficulty with everyday tasks because of pain and irritation.
A range of treatments can help ease dry eye symptoms. However, pregnant people should exercise caution when using both prescription and over-the-counter medications for dry eyes. A doctor, optometrist, or ophthalmologist can advise pregnant individuals on which treatments are most suitable.
Read this article in Spanish.
Allergic rhinitis during pregnancy: description of the disease, causes, symptoms, cost of treatment in Moscow
Allergic rhinitis during pregnancy is not uncommon, as the woman's body begins to react more violently to any irritants due to the peculiarities of the hormonal background and some disturbances in the functioning of the nasal mucosa. Most often, before pregnancy, the woman did not have a negative reaction to substances that become irritants when carrying a child. The disease usually debuts abruptly and unexpectedly. Since the condition of a woman with such a phenomenon worsens, it is imperative that when rhinitis appears, it is necessary to seek medical help. It is strictly forbidden to treat the disease on your own due to the fact that serious harm to the fetus can be caused by errors in therapy. Any treatment should be coordinated with the gynecologist who is leading the pregnancy.
Most often, before pregnancy, the woman did not have a negative reaction to substances that become irritants when carrying a child. The disease usually debuts abruptly and unexpectedly. Since the condition of a woman with such a phenomenon worsens, it is imperative that when rhinitis appears, it is necessary to seek medical help. It is strictly forbidden to treat the disease on your own due to the fact that serious harm to the fetus can be caused by errors in therapy. Any treatment should be coordinated with the gynecologist who is leading the pregnancy.
Rhinitis of an allergic nature during pregnancy is primarily due to hormonal changes and features of the immune system. In this case, an unpleasant phenomenon can occur both from the very first day after conception, and after a few months of gestation. According to medical statistics, every third woman suffers from such a disorder during pregnancy. In most cases, after childbirth, rhinitis goes away, and what was an allergen again begins to be normally tolerated by the body. If allergic rhinitis develops during pregnancy, treatment should be mandatory.
If allergic rhinitis develops during pregnancy, treatment should be mandatory.
There is usually only one allergen during pregnancy. Intolerance to two or more substances, if it was not previously, is considered an exceptional phenomenon. The most harmless is an allergy to cold, in which rhinitis develops only on the street during the cold season and completely disappears indoors. This form of the disease is not so dangerous, as it is present sporadically and for a short time. With it, the risk of complications is extremely small, and it does not greatly disturb the general condition.
Major irritants
Doctors were able to determine which irritants most often provoke allergic rhinitis. This greatly helps in the treatment of the disease, as it simplifies the process of determining the allergen, the effect of which should be minimized as much as possible.
Allergic rhinitis develops at the moment when an irritant enters the mucous membrane. Due to its presence, inflammation of the mucosa occurs and, as a result, its swelling. The body, in order to get rid of the allergen, begins to secrete a large amount of especially liquid mucus, which should wash it out. Due to the fact that the allergen is constantly supplied with air, it cannot be removed naturally. As a result, it is impossible to solve the problem of allergic rhinitis without drugs.
The body, in order to get rid of the allergen, begins to secrete a large amount of especially liquid mucus, which should wash it out. Due to the fact that the allergen is constantly supplied with air, it cannot be removed naturally. As a result, it is impossible to solve the problem of allergic rhinitis without drugs.
The main allergens that can cause problems in pregnant women are:
-
pollen of plants and their seeds - they are the cause of rhinitis in the warm season. With these irritants, health may remain unsatisfactory until the very end of the growing season of plants;
-
smoke from cigarettes or wood - such irritants usually begin to cause damage to health if a woman lives in an area with unfavorable environmental conditions;
-
Dust - it is not the dust itself that causes allergies, but the dust mites that live in it. Because of this, a negative reaction of the body also occurs when using down pillows and blankets, in which there are ideal conditions for the life of dust mites;
-
air fresheners and deodorants - they contain a large number of aggressive chemical components that can cause allergies even in non-pregnant women, and when carrying a child, they almost always provoke a runny nose;
-
animal hair and bird feathers - sometimes during pregnancy, an allergy to pets can develop, although there were no negative consequences from their stay in the house before.
 To solve the problem, the animal, which has become a source of irritants, must be isolated from the woman in another room until the birth of the child and minimize her contact with him.
To solve the problem, the animal, which has become a source of irritants, must be isolated from the woman in another room until the birth of the child and minimize her contact with him.
Whatever the cause of the disease, it is necessary to carry out treatment with the involvement of a specialist. Self-medication during pregnancy is extremely dangerous and can lead to irreversible negative consequences.
Quite often, before an allergic rhinitis occurs, a woman has a simple catarrhal rhinitis. During pregnancy, it is this form of the disease that often becomes the impetus for the development of a pathological process, in which something will no longer be tolerated by the body.
At what time is the disease especially dangerous
Depending on how pregnant a woman is, allergic rhinitis poses a greater or lesser danger. The most serious problem is the problem that occurs in the first trimester of pregnancy. At this moment, all systems and organs of the unborn child are laid, and with a lack of oxygen in the blood, especially severe congenital malformations or intrauterine death of the fetus can occur. When a woman in the first trimester does not pay attention to her well-being and does not treat allergic rhinitis, the risk of miscarriage increases many times due to respiratory failure at night. If allergic rhinitis is present in pregnant women, only a doctor will determine how to treat it.
When a woman in the first trimester does not pay attention to her well-being and does not treat allergic rhinitis, the risk of miscarriage increases many times due to respiratory failure at night. If allergic rhinitis is present in pregnant women, only a doctor will determine how to treat it.
In the second and third trimester, the lack of oxygen in the mother's blood also does not benefit the child. However, due to the enlarged belly, a woman can only sleep on her side (otherwise she is uncomfortable), respiratory disorders are not so strong and threaten deformities to a lesser extent. At the same time, if you do not start treatment, the symptoms of rhinitis will increase and nasal congestion will constantly disturb. This is already dangerous for the child and can even cause premature birth against the background of general hypoxia of the mother and fetus.
Forecast
In the event that attention was paid to allergic rhinitis in pregnant women in a timely manner, the prognosis is positive. The violation can be effectively dealt with with the help of drugs allowed during this period, and then the risk of harm to the mother and fetus when an allergy appears will be eliminated. The doctor, if necessary, will adjust the treatment and will be able to build it so that there are no negative side effects of therapy.
The violation can be effectively dealt with with the help of drugs allowed during this period, and then the risk of harm to the mother and fetus when an allergy appears will be eliminated. The doctor, if necessary, will adjust the treatment and will be able to build it so that there are no negative side effects of therapy.
If therapy is not started on time and severe fetal hypoxia is already present, then the prognosis is usually considered difficult, since this condition does not pass without a trace for the unborn child. Also, the prognosis will be unfavorable if the treatment was carried out on its own without the involvement of a specialist. In such a situation, there is a risk of serious consequences for the child, due to the fact that the mother used the wrong drugs.
Differences from colds
There are certain signs that even allow you to independently understand whether a cold or an allergic cause has a runny nose. The main distinguishing feature is that the snot in case of an allergic disorder is liquid, transparent, more like water. If the disease is cold, then the discharge becomes thick, green or yellow-green. They may also have a strong odor. In addition, with a cold, there is an increase in temperature, but not with an allergic one.
If the disease is cold, then the discharge becomes thick, green or yellow-green. They may also have a strong odor. In addition, with a cold, there is an increase in temperature, but not with an allergic one.
How to cure allergic rhinitis during pregnancy?
Allergic rhinitis develops as a specific response of the body to an allergen and is accompanied by swelling of the nasal mucosa, runny nose, sneezing, and watery eyes. During pregnancy, the situation is aggravated by the fact that it is rather problematic to treat allergic rhinitis during this period. Let's try to figure out what are the causes of the disease and what methods of treatment should be chosen so as not to harm the health of the woman and the unborn child?
What is the danger?
An additional load on the immune system, hormonal imbalance increases the risk of such terrible complications for a woman as Quincke's edema or anaphylactic shock. There is also a danger to the unborn child. Prolonged nasal breathing difficulties experienced by the mother due to nasopharyngeal edema can cause fetal hypoxia and intrauterine growth retardation. In addition, discomfort, poor health of a woman negatively affects the condition of the child.
In addition, discomfort, poor health of a woman negatively affects the condition of the child.
However, the greatest threat comes from improper treatment. Those drugs that have been successfully used before pregnancy can lead to impaired fetal development. Uncontrolled medication is especially dangerous in the first month of pregnancy, when the neural tube and other vital structures of the body are laid. Therefore, the treatment regimen for allergic rhinitis should be selected only by a doctor after a thorough examination of the woman.
Etiology
Allergic rhinitis is caused by the body's hypersensitivity to a provoking agent (allergen). The next contact with the latter triggers a chain of specific immune reactions with the release of substances that form inflammation in the nasal mucosa. Typical precipitating factors are:
- house dust microscopic mites;
- wool, down, pet excrement;
- moulds, especially during sporulation;
- some products;
- household chemicals, perfumery, certain medicines.
It should be noted that in pregnant women the content of estrogen, β-estradiol, growth hormone increases, which increase the reactivity of the immune system. Therefore, the intensity of seizures during gestation can increase significantly. However, a high concentration of estrogen disrupts vascular motility, causing vasomotor rhinitis during pregnancy. It develops in 20-30% of women and disappears after childbirth. Only a plasma test for the presence of class E immunoglobulins, which serve as markers of allergic reactions, can confirm or refute the allergic nature of the disease.
Symptoms
During an exacerbation of the disease, a woman is disturbed by difficulty in nasal breathing, runny nose, sneezing, itching in the nose and eyes, watery eyes, swelling of the eyelids. Allergic rhinitis in pregnant women is often accompanied by systemic manifestations of the disease:
- dizziness, weakness, hypotension;
- headache;
- sleep disorder;
- increased irritability.

Diagnosis
Examination is carried out by a general practitioner and an allergist-immunologist. When diagnosing, it is important to exclude a respiratory infection, vasomotor rhinitis, drug-induced rhinitis. For this purpose, blood and nasal mucus smears are tested for specific antibodies. For special indications, skin allergy tests are performed.
Treatment
Treatment of pregnant women with allergic rhinitis is aimed at eliminating the allergen and stopping the symptoms of the disease. In the first trimester, the main methods of therapy are nasal lavage with isotonic solutions and preventive measures aimed at limiting contact with the allergen (regular wet cleaning, airing, frequent bed linen changes, exclusion of potentially dangerous foods from the diet, isolation of pets).
Medicines
Drug therapy is used in severe cases, when the benefits of taking drugs significantly outweigh the risk of toxic effects on the fetus.
Nasal lavage
If the treatment of allergic rhinitis during pregnancy excludes the use of most drugs, the question arises - how to treat the disease? In such a situation, sanitation of the nasal cavities with saline solutions acquires an important therapeutic value.