2 year old no fever vomiting
Why Is My Child Throwing Up With No Fever? Nausea and Vomiting, Age 11 and Younger
Written by WebMD Editorial Contributors
In this Article
- Stomach Flu
- Food Allergy
- Food Poisoning
- Intestinal Obstruction
- Concussion
- Medications
- Motion Sickness
- Migraines
- Stress
Throwing up is no fun for kids. But it can worry you, too. A kid who’s vomiting but doesn’t have a fever could be dealing with any number of things. Knowing what else to look for can help you narrow down the reasons for your child’s upset stomach --and get their the treatment they need.
Stomach Flu
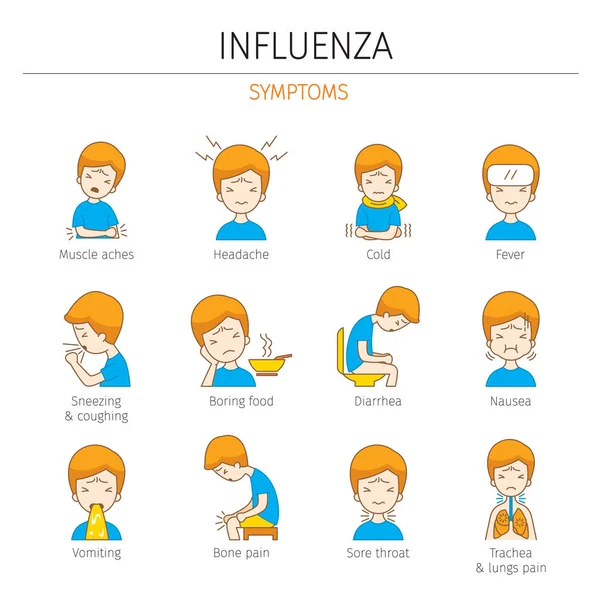
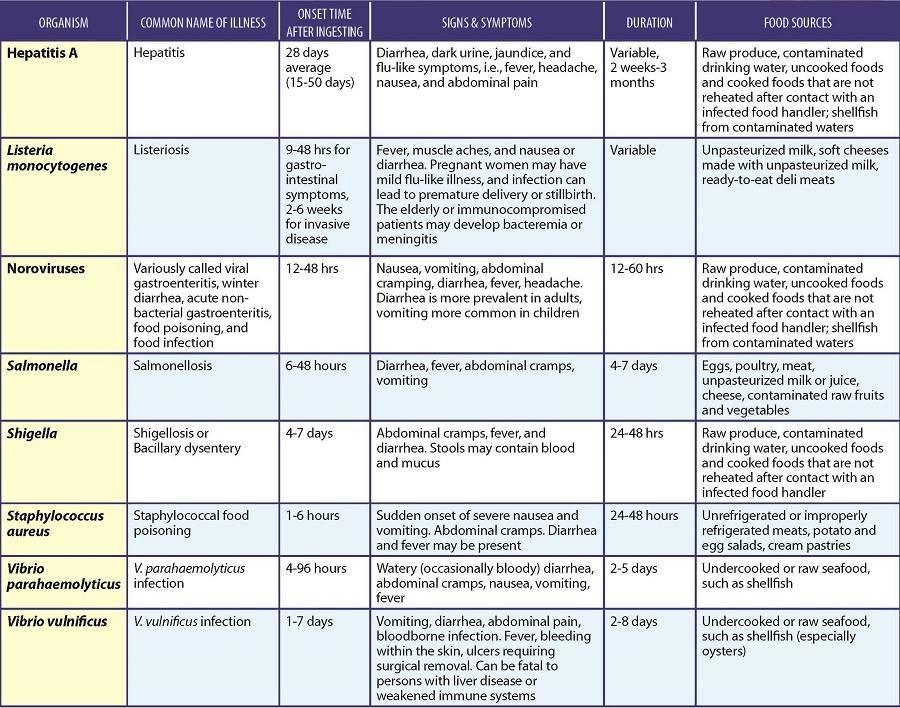
This isn’t the same as influenza (the flu). It’s the term people use when they’re talking about an illness called gastroenteritis. Most of the time, gastroenteritis is caused by a virus like rotavirus or norovirus. But you can also get it from bacteria like E. coli or salmonella. Although norovirus can sometimes cause a low-grade fever, you can also have it with no fever at all.
Norovirus is contagious like all viruses. If your child has it, they got it in one of three ways:
- They came into contact with someone who has it.
- They ate food that had the virus in it.
- They touched a surface with the virus on it, then touched their mouth or nose before washing their hands.
Symptoms start 12–48 hours after your child gets the virus. Along with throwing up, they’ll probably also have diarrhea, nausea, and stomach cramps.
Most kids get better within 1 to 3 days, but symptoms may last 7-10 days longer.
Food Allergy
Sometimes throwing up is a sign your child is allergic to food they’ve eaten. Throwing up may be their only symptom, but there could also be others, like trouble breathing, hives, repetitive cough, wheezing, or trouble swallowing. Nine out of 10 allergic reactions are linked to the following foods:
- Peanuts
- Tree nuts (almonds or walnuts, for example)
- Fish
- Shellfish (shrimp, for example)
- Eggs
- Milk
- Wheat
- Soy
Very young babies who try milk, soy, certain grains, and some other solid foods for the first time are at risk for something called “food protein-induced enterocolitis syndrome” (FPIES). It shows up 2 to 6 hours after they eat and makes them throw up many times. They may also have bloody diarrhea or stools flecked with blood. Take your child to the doctor right away if you suspect they have FPIES.
It shows up 2 to 6 hours after they eat and makes them throw up many times. They may also have bloody diarrhea or stools flecked with blood. Take your child to the doctor right away if you suspect they have FPIES.
Food Poisoning
Anytime germs hitch a ride on food your kids eat, there’s a chance they could get a food-borne illness (food poisoning). Some of the bacteria that usually hide in food are:
- Salmonella
- Listeria
- Campylobacter
- E. coli
You can get food poisoning from almost any food, especially if it hasn’t been cooked or stored correctly. The most common culprits are:
- Meat
- Poultry
- Eggs
- Shellfish
- Unwashed vegetables, like lettuce
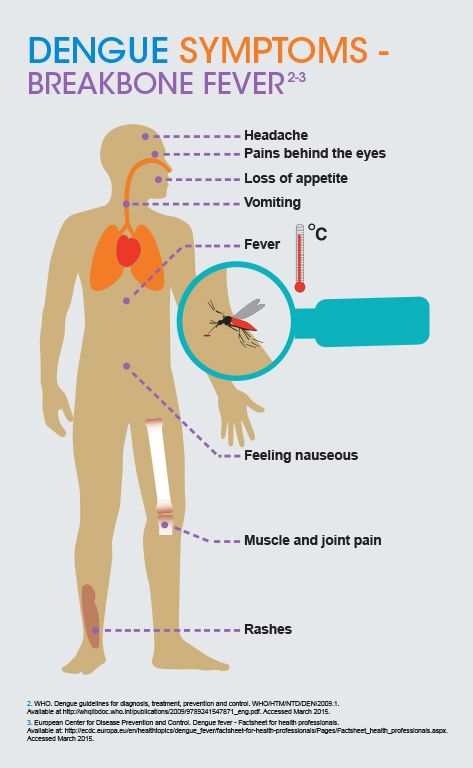
Your child might start throwing up within a couple of hours of eating contaminated food. Sometimes it can take a day or two for symptoms to show up. Usually, your child will also have nausea, watery diarrhea, and stomach pain.
It’s possible for food poisoning to cause fever, but it’s common for it to cause throwing up with no fever, too. Symptoms can last anywhere from a couple of hours to several days.
Symptoms can last anywhere from a couple of hours to several days.
Intestinal Obstruction
In newborns, it can be hard to tell whether they're throwing up or spitting up. Vomit usually comes out with more force than spit-up. Spit-up also tends to be linked to feeding and usually occurs shortly afterwards. Your doctor can help you figure out which one you’re dealing with.
Forceful throwing up in babies is rare, but when it happens, it can be a sign of a blockage in your baby’s intestines. It’s also possible that your little one could have what doctors call “pyloric stenosis.” That means their stomach is too narrow for food to pass through. Both of these are serious problems you should see a doctor about right away.
Concussion
Kids hit their heads a lot -- especially when they’re learning to walk or if they play sports. Anytime your child gets a head injury, it’s important to watch for signs of a concussion. Throwing up is one of these signs. Others include:
- Losing consciousness
- Headache
- Blurred vision
- Trouble walking
- Confusion
- Slurred speech
- Trouble waking up
Throwing up and other symptoms may not show up until 24 to 72 hours after your child hits their head.
Seek medical attention immediately if vomiting occurs after your child sustains a head injury.
Medications
If your child takes certain medications on an empty stomach, it can make them throw up. Sometimes, vomiting is a sign you’ve given your child too much of certain medications. The most common meds that cause this are:
- Codeine
- Erythromycin
- Some birth control pills
- Some asthma medications, like theophylline
- Iron
- Acetaminophen
- Ibuprofen
Motion Sickness
When your child’s brain gets mixed signals about how they're moving, it can make them feel sick enough to vomit. For example, some kids might feel sick just watching a movie -- their eyes see motion, but their body doesn’t feel motion. Carsickness is common in kids who are too small to see out the car window.
Motion sickness usually starts with a tummy ache or a queasy feeling. Some kids may also sweat, lose their appetite, and not want to eat.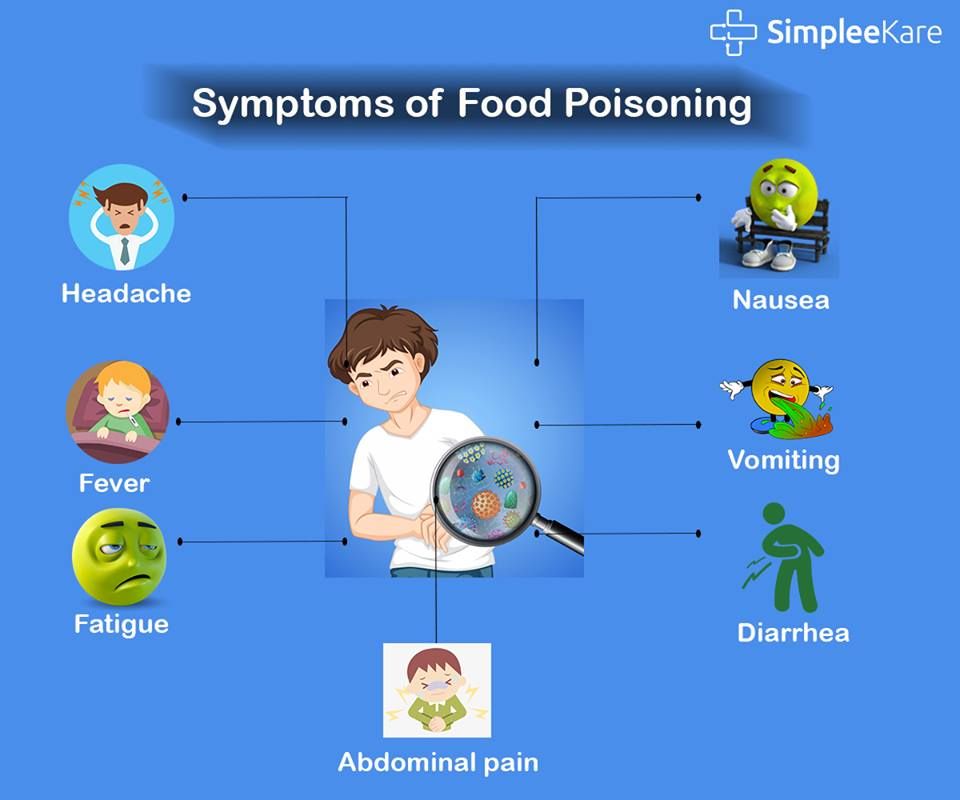 Eventually, throwing up starts. It’s a genetic condition. Your child is more likely to have motion sickness if one of their parents did.
Eventually, throwing up starts. It’s a genetic condition. Your child is more likely to have motion sickness if one of their parents did.
Migraines
About 10% of school-age children deal with migraines. These headaches can happen in kids as young as 18 months old. They cause head pain, but it’s also common for a migraine to make your child throw up. In addition, your child may have:
- Dizziness
- Nausea
- Sensitivity to touch, sound, and odors
Experts aren’t clear what causes migraines. It could be caused by something your child is around a lot. It’s also genetic: If one parent has migraines, your child has a 50% chance of getting them. If both their parents have migraines, their chance of getting them goes up to 75%.
if your child has a headache, fever, and vomiting, consult their doctor.
Stress
It’s true -- some kids throw up when they’re stressed. It may be because some other health problem, such as an ear infection, is bothering them. Or your child might throw up after crying for a long time. A good way to tell if the throwing up is stress-related is if it happens only once or twice and they don't have any other symptoms like stomach pain or diarrhea.
Or your child might throw up after crying for a long time. A good way to tell if the throwing up is stress-related is if it happens only once or twice and they don't have any other symptoms like stomach pain or diarrhea.
Children's Health Guide
- The Basics
- Childhood Symptoms
- Common Problems
- Chronic Conditions
First Aid Information for Skin Rashes in Children
Written by WebMD Editorial Contributors
In this Article
- Chickenpox (varicella)
- Measles
- Rubella (German measles)
- Scarlet fever (Scarlatina)
- Fifth disease
- Roseola Infantum
- Coxsackieviruses and other enteroviruses
- Impetigo
- Fungal and Parasitic Rashes
- Rashes in the Newborn
Many childhood diseases have bacterial or viral causes and may come with a rash. As study continues and more and more vaccines become available, these diseases become less of a threat to your child's long-term health. However, a rash of any kind should be taken seriously and may require a trip to the doctor's office for evaluation.
However, a rash of any kind should be taken seriously and may require a trip to the doctor's office for evaluation.
Chickenpox (varicella)
A virus called varicella-zoster causes chickenpox, a very contagious disease. Although it is rarely a serious disease to otherwise healthy children, the symptoms last about 2 weeks and can make the child very uncomfortable. In addition, chickenpox can be a serious illness in people with weak immune systems, such as newborns, people on chemotherapy for cancer, people taking steroids, pregnant women, the elderly, or those with HIV. A safe and effective vaccine is now available to children aged 1 year or older to prevent chickenpox. It takes up to 21 days to develop chickenpox after being exposed to the virus by inhaling infected droplets from coughs or sneezes or by coming in direct contact with the lesions on an infected person with chickenpox or from someone with shingles.
- Symptoms
- The symptoms of chickenpox often begins with a very itchy rash, which first appears on the scalp, chest, back and face then spreads to the rest of the body.
- The rash begins as an area of redness with a small, superficial blister in the center. The blister eventually ruptures with some possible drainage, and the lesion will then form a crust.
- Other associated symptoms include fever, malaise, sore throat, and red eyes. Fever and malaise may precede the rash in some cases.
- The symptoms of chickenpox often begins with a very itchy rash, which first appears on the scalp, chest, back and face then spreads to the rest of the body.
- Treatment
- The virus is spread primarily from the mucous membranes of the nose and mouth of the child, but the rash itself is also contagious. The child remains contagious and cannot go to school or daycare until the last lesion has appeared and is fully crusted over.
- No therapy treats chickenpox once it has begun, but your doctor can provide prescriptions and advice to help with the discomfort and the itching.
- Never give aspirin to a child in general but especially one with chickenpox. A deadly disease called Reye's syndrome has been associated with children taking aspirin, especially if they have chickenpox. Be sure to check the contents of any other over-the-counter medications for aspirin or salicylates because these are often found mixed with over-the-counter cold medications.
- Chickenpox can occasionally affect the cornea, the clear front portion of the eye. If your child develops chickenpox on the tip of the nose it is usually a precursor to having the eyes infected. See your doctor immediately.
- See a doctor immediately also if your child develops lesions in the genital regions internally or inside of the mouth.
Measles
A paramyxovirus causes the measles. A safe and effective vaccine is available to prevent this disease, but outbreaks in people who have not been adequately vaccinated still happen.
- Symptoms
- The disease usually begins with nasal congestion, eye redness, swelling and tearing, cough, lethargy, and high fever.
- On the third or fourth day of the illness, the child will develop a red rash on the face, which spreads rapidly and lasts about 7 days.
- Another rash consisting of white spots inside the mouth, may also develop.
- Treatment
- Once the disease begins, no medication treats measles.
 However, your doctor may offer treatments to care for cough, eye symptoms, and fever. Aspirin products cannot be used as they can cause a life-threatening condition called Reye's syndrome.
However, your doctor may offer treatments to care for cough, eye symptoms, and fever. Aspirin products cannot be used as they can cause a life-threatening condition called Reye's syndrome. - Some children develop secondary bacterial infections of the middle ear, sinuses, lung and neck lymph nodes. These can be treated with antibiotics.
- Children who have measles appear quite ill and are miserable, but the illness usually gets better without lasting ill effects within 7-10 days after symptoms started.
- You can prevent your child from getting measles by making sure they receive the recommended vaccinations. The measles vaccine is part of the MMR (measles-mumps-rubella) vaccine given at age 12-15 months and repeated at age 4-6 years.
- Once the disease begins, no medication treats measles.
Rubella (German measles)
Rubella is a much milder disease in children that's also caused by a virus (rubivirus). Symptoms may begin 14-21 days after exposure to the virus. If contracted in the womb, rubella is a much more serious disease, causing deafness, heart abnormalities, eye problems, retardation, and other conditions in the newborn.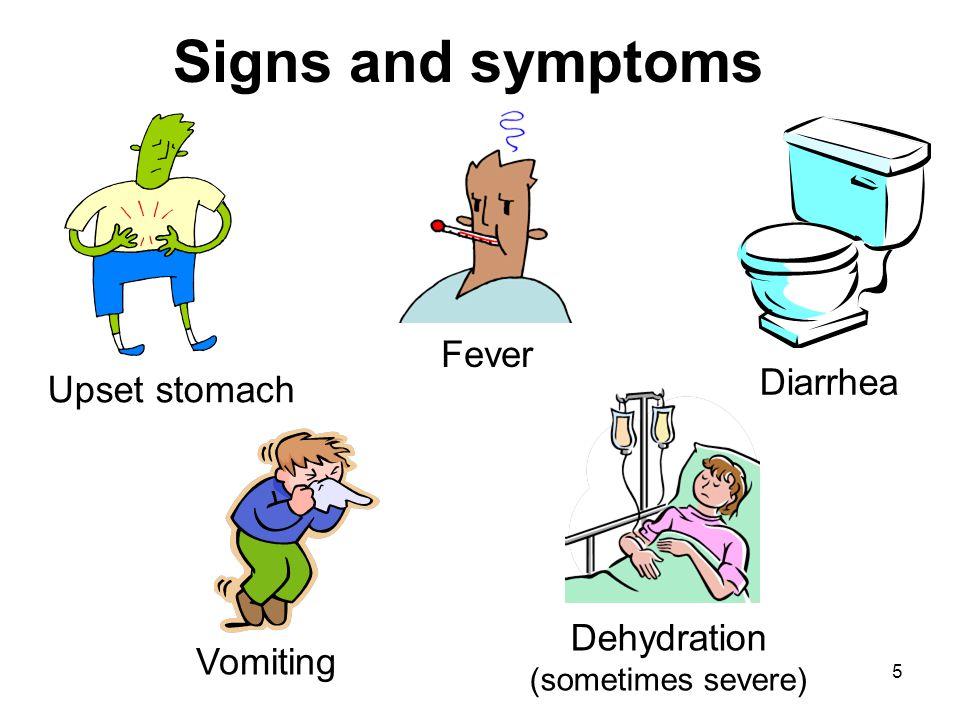
- Symptoms in children
- Rubella begins with a pink/red rash on the face then spreads to the rest of the body and gets better in about 4 days.
- Your child does not appear to be very ill but may develop swollen lymph nodes in the neck, especially behind the ears.
- Prevention
- Rubella is also easily prevented with an effective vaccine (the MMR).
- Rubella can be very serious to an unborn child if the mother develops rubella early in her pregnancy. All women of childbearing age should have their immune status verified.
Scarlet fever (Scarlatina)
Scarlet fever is strep throat with a rash. The throat infection is caused by streptococcal bacteria. It is most commonly seen in school-aged children in the winter and early spring, but it can occur in individuals of any age and in any season. It is very contagious, especially from saliva transmission. The risk of transmission can be decreased with good hand washing.
The rash is not serious, but serious complications can occur from the underlying strep throat infection. The most worrisome of these is rheumatic fever, a serious disease that can damage the heart valves and cause long-term heart disease.
- Symptoms
- The child's symptoms begin with sore throat (which can be mild), fever, headache, abdominal pain, and swollen glands in the neck.
- After 1-2 days of these symptoms, the child develops a rash on the body that is red like sunburn and has a sandpaper texture. The skin folds in the neck, armpits, elbows, groin and knees are usually a deeper red color compared to the overall rash. After 7-14 days, the rash sloughs off and peeling is usually present.
- The face may look very flushed, but the skin around the mouth appears normal or pale.
- The tongue can look like a strawberry- red with bumps.
- Treatment
- Streptococcal bacteria can be treated with antibiotics.
- Have your child seen by your doctor immediately if you suspect he or she has strep throat or scarlet fever.

- Your child will require a full course of antibiotics, which should be completed even if your child is feeling better before he or she completes the course.
- Your child may return to school 24 hours after starting the antibiotics if the fever has resolved and he or she is feeling better.
Fifth disease
Fifth disease, also known as erythema infectiosum or "slapped cheeks" disease, is caused by a virus (parvovirus B19) spread via respiratory secretions such as coughs, sneezes, saliva, or nasal mucus. This disease tends to occur in the winter and spring but can happen year-round.
- Symptoms
- The child initially feels ill and tired; then a rash appears. The rash is characterized by bright red cheeks (the symptom inspiring the name slapped cheeks disease). The rash is warm, nontender, and sometimes itchy.
- In 1-2 days a lacy rash spreads throughout the body. The rash appears to fade when the skin is cool, but with a warm bath or with activity, the rash becomes more pronounced.
 Once the rash appears, the child is no longer contagious.
Once the rash appears, the child is no longer contagious.
- Treatment
- Fifth disease is not serious in otherwise healthy children but can pose a serious problem for children with sickle cell anemia, leukemia, or AIDS.
- The disease can also cause problems in the unborn fetus of pregnant women.
- Because the child is contagious only before the rash appears, children who develop the rash are free to return to day care or school.
Roseola Infantum
Roseola is also called exanthem subitum and is a common childhood illness caused by the human herpesvirus 6 or 7. The disease usually occurs in children younger than 4 years.
- Symptoms
- The symptoms are a high, spiking fever for typically 3-4 days followed by the onset of a rash.
- The rash is small, pink, flat, or slightly raised lesions that appear on the trunk and spread to the neck and arms, and sometimes then to the face and legs.
- The rash appears after the fevers begins to abate.
 This illness is many times referred to as “fever, fever, fever...rash”.
This illness is many times referred to as “fever, fever, fever...rash”.
- Treatment
- Despite the worrisome fever, the disease is not harmful and gets better without specific therapy. Fever can be managed with acetaminophen or ibuprofen.
- The fever, especially if it rises rapidly, may result in a “febrile” seizure in susceptible children. Consult your health care provider if you have any concerns about a seizure.
Coxsackieviruses and other enteroviruses
The enteroviruses, including the coxsackieviruses, are a very common cause of fever and rash in children. Two typical diseases caused by coxsackieviruses are hand-foot-and-mouth disease and herpangina. Coxsackievirus infections are more common in the summer and autumn.
- Symptoms
- In hand-foot-and-mouth disease, the children develop fever and rash. The rash includes blisters to the mouth and tongue and to the hands and the feet.
- Herpangina (not caused by a “herpes” virus) causes a fever, sore throat, and painful blisters or ulcers on the back of the mouth that cause difficulty swallowing.
 Children may also have loss of appetite, abdominal pain, headaches, and joint pain.
Children may also have loss of appetite, abdominal pain, headaches, and joint pain.
- Treatment
- No specific treatment is available except acetaminophen (Tylenol) or ibuprofen (Advil) for fever. Aspirin and aspirin-like products should ALWAYS be avoided in children as it can cause a life-threatening condition called Reye's syndrome.
- Make sure the child is well hydrated since pain in the mouth and throat can lead to less liquid intake and dehydration.
- The diseases are not harmful but can be prevented with good hand washing and not eating off someone else's plate or sharing straws.
Impetigo
Impetigo is a superficial skin infection with streptococcal or staphylococcal bacteria. It is often found around the nose and mouth but can occur anywhere. The rash is more common in the warmer months. It can also include infection of skin that has been damaged.
- Symptoms
- Impetigo begins as small superficial blisters that rupture leaving red, open patches of skin.

- Often a honey-colored crust forms over this rash.
- The rash is sometimes itchy.
- Impetigo is also highly contagious. A child can spread the infection to other parts of their own body or to other people.
- Impetigo begins as small superficial blisters that rupture leaving red, open patches of skin.
- Treatment
- This infection of the skin is easily treated with topical or oral antibiotics and washing the skin with antibacterial soap.
- Your child usually is no longer contagious after 2-3 days of therapy, and the rash begins to heal in 3-5 days.
- If the rash does not show signs of healing by the third day of treatment, or if it continues to spread while on therapy, your child needs to be seen by your doctor.
- When the impetigo occurs in conjunction with poison ivy or scabies, your child may benefit from an anti-itch medication while the antibiotics are taking effect.
Fungal and Parasitic Rashes
Because children often share many things and are less likely to take cleanliness precautions than adults, parasites and fungal infections can spread quickly through a day care or your child's class at school. Pay attention to any prolonged itching or hair loss your child might experience.
Pay attention to any prolonged itching or hair loss your child might experience.
Scabies
Scabies is an itchy rash that is often worsened with bathing or at night. It is caused by a mite, a very small insect (Sarcoptes scabiei) that burrows beneath the top layer of skin. It is spread by close bodily contact such as sleeping together or sharing of clothing. It can also be sexually transmitted. Mites can survive for several days in clothes, bedding, and dust.
- Symptoms
- The rash starts about 2 weeks after your child has come into contact with the mite.
- The itchy rash of scabies tends to be found between the fingers, in the armpits, and on the inner wrists and arms. It tends to spare the head, palms, and soles except in infants and with severe infestations.
- Sometimes you can see the wavy pattern where the mite has burrowed.
- Treatment
- To prevent scabies, good hygiene, frequent hand washing, and not sharing clothing with friends is important.

- If your child has an itchy rash that lasts for more than 2-3 days, he or she should be checked by a doctor.
- Prescription medications are available to kill the mites and to decrease the allergic skin reactions of swelling and itch.
- Once anyone in the family is diagnosed with scabies, everyone in the home should be treated for mite infestation.
- All clothing and bedding must be washed in hot water and the mattresses vacuumed.
- To prevent scabies, good hygiene, frequent hand washing, and not sharing clothing with friends is important.
Ringworm
Ringworm is a local infection of the skin with a fungus, usually Microsporum canis, Microsporum audouinii, orTrichophyton tonsurans. Doctors refer to these infections as "tinea" with several forms such as tinea corporis (ringworm on the body) and tinea capitis (ringworm of the scalp). Although the 2 are caused by the same organisms, they are treated differently. Ringworm can be caught from friends (exchanging combs, brushes, or hats) or from household pets. If you think your child may have ringworm, you should see your doctor.
- Symptoms
- With tinea corporis, the lesion starts as a red, slightly scaly, oval that gets bigger over time.
- The rash may be slightly itchy.
- The center of the rash may clear and appear to be normal skin.
- Tinea capitis usually starts with a round to oval area on the scalp with hair loss
- Sometimes, the area of the scalp will swell and may ooze. This is called a kerion and is a reaction of the body to the tinea fungus.
- Tinea capitis may also present as normal-to-severe dandruff with hairless patches on the scalp.
- Treatment
- Tinea corporis can easily be treated with topical medications available from your doctor.
- Unfortunately, it can be easily spread among family members and friends, making multiple unwanted return visits.
- Good hygiene combined with appropriate therapy can break this cycle.
- If complications such as a secondary bacterial skin infection occurs,or there is no improvement after four weeks, call your doctor.

- Tinea capitis requires an oral medication from your doctor.
Athlete's Foot
Athlete's foot (tinea pedis) is also caused by a fungal infection of the skin.
- Symptoms
- A very itchy rash between the toes is usually caused by athlete's foot.
- Treatment
- Although athlete's foot can be treated with over-the-counter medications, other causes of rash can appear similar. It is best to have your child checked by the doctor if you suspect athlete's foot.
Rashes in the Newborn
When you first bring your baby home from the hospital, every little bump or red patch causes alarm. It is normal for your baby to have some skin rashes. Diaper rash and cradle cap are par for the course with newborns. If you suspect that your child has more than a simple skin irritation, it is best to see a doctor.
Milia
- Symptoms
- Small yellow to white dots on the nose, cheeks and chin occur in healthy newborns.
- Small cysts or milia of the gums or roof of the mouth are called Epstein's pearls
- Small yellow to white dots on the nose, cheeks and chin occur in healthy newborns.
- Treatment
- Milia go away by themselves and require no therapy.
- These dots are not contagious.
Seborrheic Dermatitis (Cradle Cap)
- Symptoms
- Cradle cap is a greasy, scaly, red, bumpy rash that can occur on the scalp, behind the ears, in the armpits, and the diaper area.
- Treatment
- This rash is not harmful and can be easily treated by your doctor. No emergency care is required.
Infantile Acne
Infantile acne is a disorder that will go away on its own and that occurs primarily in male babies in the first 6 weeks of life. Although treatment is not required, you can discuss options with your doctor.
Erythema Toxicum
This rash has a scary name but should really be called "the normal newborn rash" because it occurs in about half of all newborns.
- Symptoms
- The rash starts with small blisters on a red base.
- Sometimes only the blotchy red base shows, and sometimes the blisters have a white or yellow material inside.
- The rash starts the second or third day of life and usually gets better in 1-2 weeks.
- The rash starts with small blisters on a red base.
- Treatment
- The rash is not serious, is not contagious, and does not require treatment.
- The rash can look similar to other types of rash, so see your doctor with any questions or concerns.
Miliaria (Prickly Heat)
This rash includes small, clear blisters usually on the nose. It is caused by the production of sweat in a warm environment and plugged sweat glands. This rash is more common when the child is dressed too warmly. It gets better on its own.
Candidal Rash (Yeast Infection)
This diaper rash is a fungal or yeast infection of the skin by Candida albicans. This is the same organism that causes thrush, the white plaques in the mouth of infants. The combination of the moist diaper environment and the presence of C albicans in the normal gastrointestinal tract of children causes a candidal rash.
- Symptoms
- An intensely red, raised rash with discreet borders is found. The borders may have a ring of fine scales.
- Surrounding the main area of rash there may be smaller lesions, called satellite lesions, which are characteristic of candidal diaper rashes.
- The rash tends to involve the creases and folds because of the warm, moist environment.
- Treatment
- This rash is easily treated by medications available from your doctor, but it tends to recur. Your doctor will want to check for thrush as well.
Seborrheic Dermatitis
A greasy, scaly, red diaper rash, seborrheic dermatitis tends to occur in the creases and folds just as in candidal rashes. Unlike candidal rashes, the rash is usually not intensely red or scaly but instead is usually moist and greasy in appearance. This rash is not harmful and can be easily treated by your doctor.
Irritant Diaper Rash
The effects of urine and feces on the sensitive skin of the newborn cause this rash. The creases and folds are spared in this rash, unlike seborrhea or candidal diaper rash.
The creases and folds are spared in this rash, unlike seborrhea or candidal diaper rash.
- Treatment
- To prevent diaper rash, change soiled or wet diapers as soon as possible.
- Make sure that baby clothing is well rinsed, and do not use fabric softeners because this may irritate delicate skin.
- Many doctors suggest allowing the bottom to go bare for several hours a day, especially to help heal a diaper rash.
- Topical ointments with zinc oxide or Vaseline also provide a barrier and may help with healing of a diaper rash.
Children's Health Guide
- The Basics
- Childhood Symptoms
- Common Problems
- Chronic Conditions
reasons, what to do, how to stop
The gag reflex is one of the protective reactions of the body, it is not always a sign of any disease. Vomiting helps the body get rid of toxins. Signals about the need to empty the stomach can come from various organs - the stomach, intestines, kidneys, liver, vestibular apparatus. These signals are sent to the vomiting center in the brain, which gives the command to empty the stomach.
These signals are sent to the vomiting center in the brain, which gives the command to empty the stomach.
Types of vomiting in a child
Vomiting can occur under various circumstances, such as traumatic brain injury, poisoning, motion sickness. In some cases, repeated vomiting occurs, sometimes it is accompanied by dizziness, fainting and loss of consciousness, abdominal pain and diarrhea.
| Vomiting of bile | Most often occurs with acute pancreatitis. Initially, it consists of the contents of the stomach, then bile is mixed with the main mass. By volume, vomiting is quite significant, because of this, the body can quickly fall into a state of dehydration. Traces of bile also appear with intussusception (obstruction) of the intestine. In addition to vomiting, in this case, there is episodic pain with spasms. |
| Vomiting of blood | Severe vomiting of blood may occur due to chemical burns. For example, when a child swallows acid, alkali and other caustic or poisonous substances. In this case, he needs urgent medical attention. Vomiting with blood also occurs with bleeding from the dilated veins of the esophagus in children with cirrhosis of the liver, as well as with a stomach or duodenal ulcer. All of these conditions need to be treated promptly. In this case, he needs urgent medical attention. Vomiting with blood also occurs with bleeding from the dilated veins of the esophagus in children with cirrhosis of the liver, as well as with a stomach or duodenal ulcer. All of these conditions need to be treated promptly. |
| Yellow or green vomit | This vomit has a bitter taste, which means that there are traces of bile in the mass. Perhaps there are problems with the functioning of the liver, gallbladder, or vomiting - a consequence of taking an excessive amount of fatty foods. The rotten smell of vomit indicates stagnation of food in the stomach. |
| Vomiting with mucus | Occurs in acute and chronic gastritis, food allergies (gastrointestinal form) and bronchitis. Usually, children under 3 years of age swallow sputum, with a fit of coughing, vomiting may begin with an admixture of mucus or sputum. |
Causes of vomiting in a child
If vomiting is not accompanied by fever, then the most likely cause of its occurrence may be disorders of the gastrointestinal tract, food poisoning (expired or poor-quality food, chemicals), intoxication after taking the medicine , dysbacteriosis.
Consider some possible causes.
Pylorospasm or pyloric spasm
Gastric spasm, which most often occurs in newborns due to the underdevelopment of the nervous system. Vomiting may be profuse. Such a child is usually restless, poorly gaining weight. Pylorospasm should not be confused with regurgitation, which is most often observed when the stomach is full of food.
Intestinal obstruction
Accompanied by severe pain, bloating, spasms, blood in the stool. Intestinal obstruction in children is most often associated with worms or intussusception, which is the introduction of a section of the intestine into a segment of an adjacent section of the intestine. The vomit may contain bile.
Vomiting may be accompanied by anti-peristaltic bowel movements, which may contribute to the entry of intestinal contents into the stomach (2).
Inflammatory diseases of the gastrointestinal tract (acute gastritis, gastroduodenitis, pancreatitis, cholecystitis)
These diseases can occur in violation of the diet, abuse of fried, smoked, fatty foods. In these cases, vomiting is often accompanied by diarrhea, abdominal pain, loss of appetite, and bloating. An increase in temperature is usually not observed, but in some cases it can reach 37°C.
Vomiting 10-15 minutes after eating is observed in functional dyspepsia, acute gastritis, tumor process of the cardiac part of the stomach. In some forms of gastritis, blood may be present in the vomit.
With gastroduodenitis, prolonged constipation may be replaced by diarrhea. In acute pancreatitis, the nature of vomiting attracts attention: it is repeated, plentiful. In this case, the contents of the stomach are first released, followed by bile and the contents of the duodenum. Such vomiting threatens with dehydration of the child's body. Vomiting in acute cholecystitis is usually not accompanied by diarrhea. The child, as a rule, is disturbed by pain in the right hypochondrium, bitterness in the mouth. Vomiting of food eaten the day before and even 1-2 days before its occurrence is characteristic of pyloric stenosis (1).
The child, as a rule, is disturbed by pain in the right hypochondrium, bitterness in the mouth. Vomiting of food eaten the day before and even 1-2 days before its occurrence is characteristic of pyloric stenosis (1).
Risk groups for the formation of functional disorders of the gastrointestinal tract in the first year of life:
- children born prematurely, morphofunctionally immature,
- children who did not receive breast milk at the first feeding,
- children who received total parenteral (through injection) nutrition ( 3).
Foreign body in the esophagus
Because children often put things in their mouths, a foreign body in the esophagus can cause vomiting. If a foreign body damages the mucous membrane of the esophagus or stomach, an admixture of blood may be detected in the vomit.
Food poisoning
Vomiting is common with food poisoning, such as expired or poor quality food, unwashed fruits and vegetables. In such cases, vomiting may be accompanied by diarrhea, sometimes the temperature rises.
Dysbacteriosis
Violation of the intestinal microflora due to prolonged use of antibiotics is often accompanied by vomiting and diarrhea. It is important to carefully consider the intake of such drugs, since they are detrimental not only to pathogenic microbes, but also to normal microflora.
Other diseases
Vomiting may also develop in diseases not related to the gastrointestinal tract, such as:
- traumatic brain injury, such as concussion or brain contusion;
- psychogenic trauma - can be provoked by stress, anxiety, emotional upheavals;
- disorders of the vestibular apparatus;
- metabolic diseases (diabetes mellitus, lactose intolerance, etc.).
What to do and how to stop vomiting in a child
First of all, you need to call a doctor. Before his arrival, the child should be given plenty of fluids - warm, slightly salted or mineral water without gas.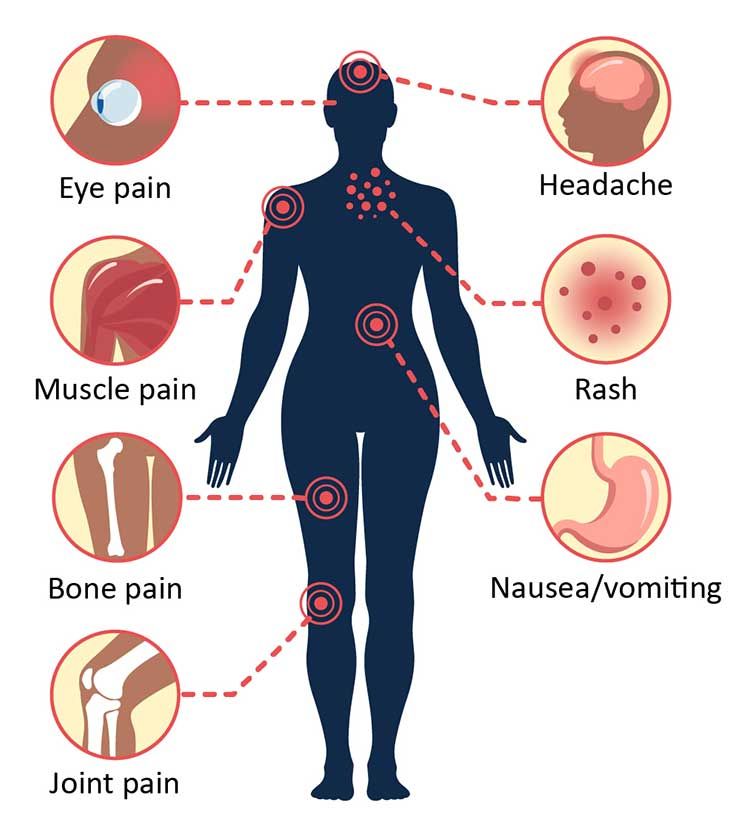 You can try herbal decoctions, for example, from chamomile, mint, etc. This will unload the digestive tract, help remove toxins and replenish fluid loss.
You can try herbal decoctions, for example, from chamomile, mint, etc. This will unload the digestive tract, help remove toxins and replenish fluid loss.
During an attack of vomiting, it is important to ensure that the child is in a position that facilitates the discharge of vomit and does not choke. For this, the baby needs to be turned on its side and held in a semi-vertical position. After vomiting, it is necessary to rinse the mouth and free from vomit. You do not need to give your child any drugs or do a gastric lavage. Only a doctor can give appropriate appointments, having established the causes of vomiting.
— Depending on the cause of the vomiting, there are several ways to stop it before the doctor arrives. Parents of a child should not be given antiemetic drugs, since vomiting most often has a protective function, says pediatrician Svetlana Ivanchenko . - To replace the lost fluid, parents can start drinking a solution to restore fluid and electrolyte balance, as well as give tea with lemon for children over 3 years old. Doctors do not recommend bottled "baby" water for drinking a child with vomiting, because. this can further worsen the water and electrolyte composition of the blood in the body. In addition, current fluid losses with loose stools and vomiting are taken into account: for each episode of diarrhea / vomiting, an additional 100-200 ml of fluid is given.
Doctors do not recommend bottled "baby" water for drinking a child with vomiting, because. this can further worsen the water and electrolyte composition of the blood in the body. In addition, current fluid losses with loose stools and vomiting are taken into account: for each episode of diarrhea / vomiting, an additional 100-200 ml of fluid is given.
The child should be calmed down and placed in a cool, quiet place. Put a cool damp cloth on your forehead, stroke your stomach without pressure in a clockwise direction. You should pay attention to the frequency and volume of urination in a child.
Thirst increases in the child, dry skin and mucous membranes appear. But with increasing dehydration, the child becomes lethargic, stops urinating, thirst disappears, the skin loses turgor (elasticity), and the eyes “sink”. In this case, there is no time to waste, it is necessary to call a doctor and hospitalize the child.
Daily fluid requirement per child's weight:
| 2-10 kg | 100 ml/kg |
| 10-20 kg per 10+5 kg each over 10 + 5 ml | |
| > 20 kg | 1500 ml + 20 ml/kg for every kg over 20 kg To stop vomiting if it occurs during feeding, you can hold the child in an upright position. Liquid food can be given no earlier than two hours after the end of vomiting. Liquid food can be given no earlier than two hours after the end of vomiting. After vomiting, a sparing diet and sufficient fluid intake should be followed. A child can be given cereals from rice, buckwheat, oatmeal, low-fat vegetable soups, baked apples, boiled vegetables, crackers, kissels. Prevention“To prevent vomiting, you need to follow some preventive measures,” says pediatrician Svetlana Ivanchenko. - Do not give your child fatty, fried foods, soda, foods that have expired or are suspected of their low quality. During the hot season, offer to drink more often, stay in the shade of trees, and not under the rays of the scorching sun. Timely pass medical examinations in the decreed terms. Then, at the slightest change in laboratory and instrumental studies, the doctor can pre-diagnose and prescribe preventive or therapeutic measures. Here are some more important rules:
Popular Questions and AnswersSvetlana Ivanchenko, pediatrician at MEDSI Clinic on Leninsky Prospekt, doctor of the first qualification category, answered popular questions. Vomiting in a child and stomach ache - what could be the reasons?Abdominal pain in a child is one of the most common symptoms. In infants, it is associated with colic and the accumulation of gases in the intestines. In children older than one year, it may occur due to food poisoning, acute inflammation of the gastrointestinal tract. If your child has a stomachache, seek medical attention. The doctor will diagnose, determine the cause of the pain, prescribe the most appropriate treatment. It is important to know that some diseases can be almost asymptomatic or atypical. Therefore, you should not prescribe treatment yourself, if pain occurs, you should immediately seek medical help. What does vomiting with diarrhea mean?Vomiting with diarrhea may be indicative of: • food poisoning with products that have expired or with violations of storage rules, preparation technologies, etc.; Vomiting without abdominal pain or other symptoms - what could be the cause? Vomiting in a child without fever and diarrhea is common. For parents, this condition causes serious concern, since they cannot find an explanation for what is happening. Here are some examples of such conditions. • Gastroesophageal reflux. Reflux is accompanied by the following symptoms: the child is restless, does not gain weight well, often hiccups, asthma attacks are possible. Also, children with gastroesophageal reflux are characterized by salivation and morning cough. If the pathology is not eliminated in a timely manner, then heartburn, belching, bouts of shortness of breath, night snoring, dysphagia will join in the future, and tooth enamel will suffer. In children under three months of age, reflux is a normal physiological phenomenon and is often accompanied by vomiting and regurgitation. This is due to the underdevelopment of the distal esophagus and the small volume of the stomach. Over time, regurgitation will occur less and less, and then it should stop altogether. • Pylorospasm is a disease that manifests itself as a spasm of the pyloric part of the stomach, which leads to problems with emptying it. • Pyloric stenosis is a condition that refers to congenital malformations of the muscular layer of the stomach and manifests itself in profuse vomiting. It usually occurs 20 minutes after feeding the baby. The vomit does not contain impurities and consists of undigested breast milk. Manifests (manifests) a pathological condition already on the 2nd-3rd day of the baby's life. In addition to vomiting, there is a sinking of the fontanel and weight loss, which is dangerous for infants. • Intestinal intussusception — a variant of intestinal obstruction, consists in the introduction of a section of the intestine into the lumen of an adjacent segment. The disease occurs in 90% of cases in infants, it is detected mainly at 5-7 months, although it can also develop in older children. • Diseases of the central nervous system. Diseases that affect the central nervous system are often accompanied by persistent vomiting, which is not associated with food intake. As a rule, cerebral vomiting occurs at the peak of the headache and does not bring relief to the child. The most common diseases of the central nervous system in infancy, accompanied by vomiting: cerebral ischemia and hydrocephalus. In children older than one year, these are brain tumors and increased intracranial pressure. In pathologies of the central nervous system, vomiting is rarely the only symptom of the disease. Most often there are such signs as: headaches, coordination disorders, visual disturbances, dizziness. • Psychogenic vomiting. Psychogenic vomiting occurs in a child after the age of three years. Provoking factors can be severe anxiety, fear, overexcitation and other emotional upheavals. Sometimes psychogenic vomiting is a way to attract attention, which is typical for children deprived of parental care. There may be other causes of vomiting: sunstroke, being in a stuffy room, motion sickness. Sources
What should I do if my child vomits without fever? – Provincial pharmaciesNausea and vomiting are protective reactions of the human body to various factors. Not always the cause of their occurrence will be a disease. The main purpose of the gag reflex is to rid the body of toxins. Our body signals the beginning of the process with the help of organs such as the kidneys, stomach, liver and vestibular apparatus. Vomiting occurs under various circumstances, for example, during poisoning, with traumatic brain injuries or motion sickness. The whole process is usually accompanied by abdominal pain, diarrhea, dizziness and mental confusion. Sometimes it comes down to fainting and loss of consciousness. In cases where vomiting occurs without elevated body temperature, the cause of its occurrence is considered to be a violation of the normal functioning of the digestive system. Experts from the network of pharmacies "Provincial Apteki" will tell you more about this topic. Why does the child vomit without fever?Child health is an important topic for any parent. Sometimes the baby may experience digestive disorders in the form of nausea and vomiting. Most often it is associated with diseases or various conditions of the gastrointestinal system. Here is some of them:
Child vomits without fever - what to do? When nausea and vomiting occur in a baby, it is better to seek medical help. During vomiting, it is recommended to monitor the position in which the child is located. It is important that the position of the body contributes to the discharge of vomit, while the baby should not choke in them. To do this, it is better to turn the child on its side and keep it in a semi-vertical position. After that, it is recommended to rinse the oral cavity and free it from vomit. Without the guidance of a specialist, it is better not to give the baby any medications or do a gastric lavage. Only a pediatrician or the attending physician can prescribe all medications. Usually with such a diagnosis, the pediatrician sends the child to a gastroenterologist. This specialist deals with the treatment of pathologies of the gastrointestinal tract. He prescribes a therapy strategy, a course of drug treatment and a diet. Even if the matter is not in the pathology of the gastrointestinal tract, then you still cannot do without a diet - it is required to restore the body. Sometimes vomiting without fever is a symptom of some diseases of the nervous system. In such cases, it is better to consult a neurologist. Sometimes this is a sign of psychosomatic illness. Then it is better to send the baby to a psychologist or psychotherapist. In this case, treatment will take a long time and require changes in the lifestyle of the child and other family members. Don't feed your baby when he's vomiting. It is better to wait a few hours to make sure that the process of indigestion is completed. Liquid food can be given to the child no earlier than two hours after the end of vomiting. After recovery, the child is better to feed on a special diet. It will normalize the work of the digestive system and all its organs. There are no secrets - proper nutrition and water balance. A child can be given cereals from rice, buckwheat, oatmeal, low-fat vegetable soups, baked apples, boiled vegetables, crackers, kissels. The child has a stomach ache and vomiting - measures to prevent such cases There is a list of preventive measures that will help avoid the return of the disease. First of all, follow the rules of personal hygiene - wash your baby's hands before each meal and after returning home from the street. You should also handle foods well before eating them - wash vegetables and fruits. It is important to pay attention to the quality of the dish and its shelf life. Limit the child's access to household chemicals and medicines, wean them from putting foreign objects in their mouths - toys and household items. If a child has an attack of vomiting, it is necessary to provide him with timely treatment. The same should be done with the appearance of pain and bloating in the abdomen, violation of the stool. Full list of recommendations:
It is always easier to prevent the onset of an ailment than to treat it. Following these simple rules of prevention will help to do this. What are the complications of vomiting and diarrhea in a child?We have already figured out what to do if the child has a stomachache and vomiting without fever. However, if timely treatment is ignored, complications can occur. The feature of vomiting without an increase in body temperature is not a disease, but only a symptom of it. |
 ;
; 
 As a result, the child periodically vomits. It is not abundant and is observed from the first days of life. Girls are more likely to suffer from the disease.
As a result, the child periodically vomits. It is not abundant and is observed from the first days of life. Girls are more likely to suffer from the disease. 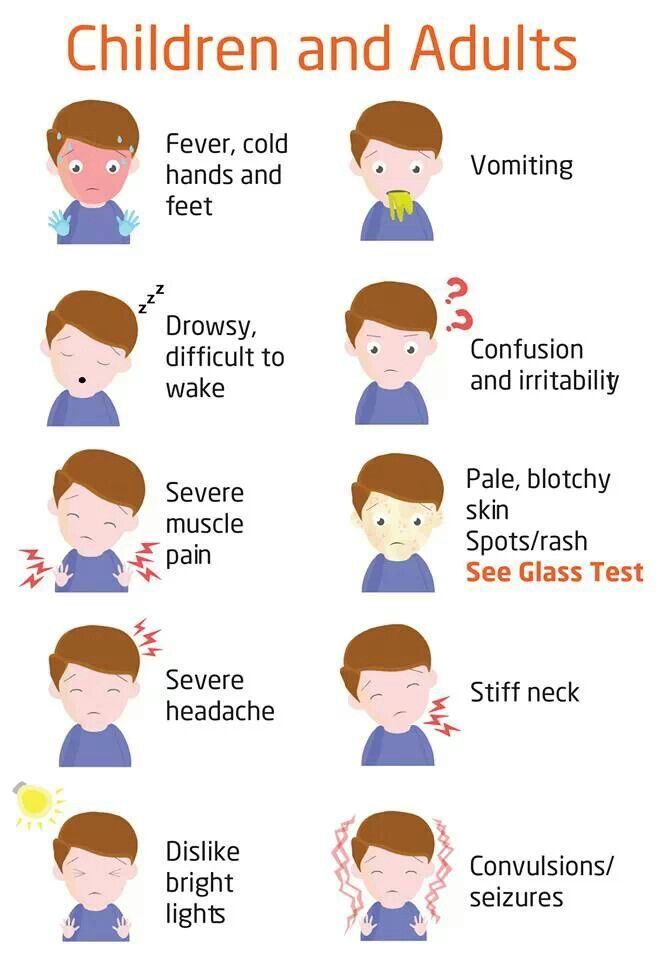

 Such beacons are caught by the vomiting center in the brain, which gives the command to empty the stomach.
Such beacons are caught by the vomiting center in the brain, which gives the command to empty the stomach.  Defecation is also disturbed, bloody discharge can be found in the stool. The disease in children appears due to worms or intestinal intussusception. It is the introduction of a section of the intestine into a segment of an adjacent section of the intestine. Sometimes bile comes out with vomiting
Defecation is also disturbed, bloody discharge can be found in the stool. The disease in children appears due to worms or intestinal intussusception. It is the introduction of a section of the intestine into a segment of an adjacent section of the intestine. Sometimes bile comes out with vomiting  Medicines kill not only pathogenic trace elements, but everything around. Therefore, it is important to observe the period set by the attending physician or indicated on the package of the drug.
Medicines kill not only pathogenic trace elements, but everything around. Therefore, it is important to observe the period set by the attending physician or indicated on the package of the drug.  Such diseases are diagnosed in violation of the diet, the abuse of fast food, fried and fatty foods or smoked meats. Then vomiting comes along with diarrhea, bloating and pain in the abdomen, loss of appetite and apathy. There is no increase in body temperature, but in some cases the mark on the thermometer can reach 37℃. With gastritis, blood is present in the vomit. With gastroduodenitis, the nature of the stool is changeable, prolonged constipation can be replaced by diarrhea. In acute pancreatitis, the nature of vomiting is noteworthy - it is repeated, plentiful. In this case, the contents of the stomach are first released, followed by bile and the contents of the duodenum. Such vomiting threatens with dehydration of the baby's body. Vomiting in a child with acute cholecystitis is usually not accompanied by diarrhea. The child is usually worried about pain in the right hypochondrium and bitterness in the mouth.
Such diseases are diagnosed in violation of the diet, the abuse of fast food, fried and fatty foods or smoked meats. Then vomiting comes along with diarrhea, bloating and pain in the abdomen, loss of appetite and apathy. There is no increase in body temperature, but in some cases the mark on the thermometer can reach 37℃. With gastritis, blood is present in the vomit. With gastroduodenitis, the nature of the stool is changeable, prolonged constipation can be replaced by diarrhea. In acute pancreatitis, the nature of vomiting is noteworthy - it is repeated, plentiful. In this case, the contents of the stomach are first released, followed by bile and the contents of the duodenum. Such vomiting threatens with dehydration of the baby's body. Vomiting in a child with acute cholecystitis is usually not accompanied by diarrhea. The child is usually worried about pain in the right hypochondrium and bitterness in the mouth.  Take him to the pediatrician, in special cases you need to call an ambulance. Before the arrival of the doctor, the child should be given plenty of fluids. Slightly warm slightly salted or still mineral water will do. To calm the microflora of the digestive system, herbal decoctions, for example, from mint or chamomile, are excellent. The liquid will unload the gastrointestinal tract, remove toxins and replenish the loss of water.
Take him to the pediatrician, in special cases you need to call an ambulance. Before the arrival of the doctor, the child should be given plenty of fluids. Slightly warm slightly salted or still mineral water will do. To calm the microflora of the digestive system, herbal decoctions, for example, from mint or chamomile, are excellent. The liquid will unload the gastrointestinal tract, remove toxins and replenish the loss of water. 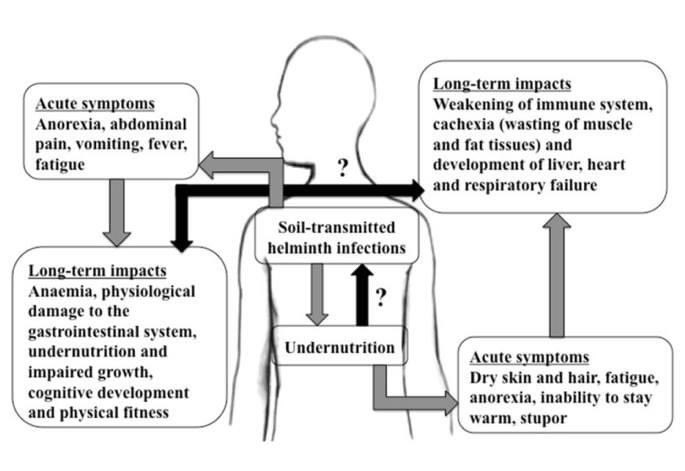 Self-medication sometimes does not contribute to recovery, but, on the contrary, directs this process in the opposite direction, causing complications. The doctor recommends all medications, taking into account the characteristics of the course of the disease and the child's body.
Self-medication sometimes does not contribute to recovery, but, on the contrary, directs this process in the opposite direction, causing complications. The doctor recommends all medications, taking into account the characteristics of the course of the disease and the child's body. 
 Limit your intake of unhealthy foods - fatty, fried and fast food. Cut down on sweets and pastries.
Limit your intake of unhealthy foods - fatty, fried and fast food. Cut down on sweets and pastries.  The kid should wash his hands before eating, use a personal towel and so on.
The kid should wash his hands before eating, use a personal towel and so on.