How to cure an earache for child
What's the Best Ear Infection Treatment for Kids?
Five tips to help relieve ear infection symptoms at home
Five tips to help relieve ear infection symptoms at home
If your little one is cranky, unusually fussy and tugging at his or her ear or is feverish and having difficulty sleeping, chances are it may be due to an ear infection.
Ear infections in children often go away on their own or in some cases with antibiotic treatment. The challenge for many parents is knowing what to do, what to watch for and when to call their pediatrician.
Five out of six children experience an ear infection by the time they are 3 years old, according to the National Institutes of Health. The odds are that your child will have an ear infection before kindergarten.
What causes an ear infection?
Ear infections can be caused by either bacteria or a virus, often following a cold. The common cold can cause the middle ear to become inflamed and fluid to build up behind the eardrum. The Eustachian tube, which connects the ears, nose and throat, can also become swollen.
“Children are more susceptible to ear infections than adults because they have shorter and narrower Eustachian tubes, and it is easier for germs to reach the middle ear and for fluid to get trapped there,” says Kara Hutton, MD, a pediatrician at Scripps Clinic Rancho Bernardo. “Babies and children also have weaker immune systems, so it is more difficult for their bodies to fight an infection.”
The onset of ear infections is often on day three of a cold. Ear infections peak at age 6 months to 2 years, and are a common problem until age 8, according to the American Academy of Pediatrics.
What is the best treatment for ear infection?
Some ear infections require antibiotic treatment, but many can get better without this medicine.
If you suspect your child has an ear infection, your pediatrician can diagnose it and determine the appropriate treatment.
“Common ear infections often do not require antibiotics, except in severe cases or in infants younger than six months,” says Dr. Hutton. “Many ear infections will resolve on their own within a week.”
Hutton. “Many ear infections will resolve on their own within a week.”
For mild cases, your doctor might recommend watchful waiting to give your child’s immune system time to fight off the infection or delayed antibiotic prescribing, which gives you time to see if your child is still sick before filling it.
Five tips for ear infection treatment at home
Even when antibiotics are prescribed, they won’t take effect for 24 to 48 hours. Your child need not suffer needlessly. There are simple, effective ways to reduce your child’s discomfort and pain during an ear infection.
1. Fever and pain medicine: based it on age, consult with doctor
Over-the-counter medications can help reduce pain and fever in your child. Based it on age and weight and consult with your pediatrician if necessary.
Read labels and instructions carefully when giving fever-reducing medications. “It’s very important to follow instructions and give the appropriate dosage according to your child’s weight and age,” says Dr. Hutton.
Hutton.
- For children younger than 6 months, give only acetaminophen, such as Tylenol.
- For children older than 6 months, you may give also give an ibuprofen product, such as Advil, for fever and pain.
- Infants younger than 3 months old who have a fever need immediate medical attention even if they appear well and show no other signs of being ill.
- Do not give aspirin to children because it can cause Reye’s syndrome, a rare but very serious illness that harms the liver and brain, according to the Centers for Disease Control and Prevention (CDC).
2. Place a cold pack or warm compress over your child’s ear
Put a cold wet washcloth on the outer ear for 20 minutes to help with pain until the pain medicine starts to work.
Some children prefer a warm compress to help alleviate pain. Use a warm washcloth and apply until it becomes cool. “Make sure that the compress is only warm, not hot,” says Dr. Hutton.
3. Keep child hydrated
Make sure to keep your child well hydrated. Give lots of cold fluids.
Give lots of cold fluids.
4. Elevate your child’s head
“Keeping your child’s head elevated can ease some of the pressure,” says Dr. Hutton.
If your child is older than 2 and no longer sleeps in a crib, use a pillow, but never use a pillow with an infant. You can keep an infant upright in a car seat to alleviate pressure.
5. Watch for ear discharge
Pus discharge can be normal with an ear infection. Most often, this heals after the ear infection is treated. Wipe the discharge away. Careful not to plug the ear with cotton as retained pus can cause an infection of the lining of the ear canal.
When to call your doctor
Pediatricians recommend calling your doctor if:
- Fever lasts more than two days on antibiotics
- Ear pain becomes severe or crying becomes nonstop
- Ear pain lasts more than three days on antibiotics
- Ear discharge is not better after three days on antibiotics
- Your child becomes worse
Talk with your pediatrician if your child suffers recurrent ear infections, especially if you have a family history of allergies and asthma
Preventing ear infections
While you can’t fend off every germ, there are steps you can take to reduce the risk of an ear infection, including by:
- Breastfeeding your infant to pass along immunities
- Avoiding secondhand smoke
- Washing your hands
- Keeping immunizations up to date
How They Work & When They Fall Out
Written by WebMD Editorial Contributors
What Are Ear Tubes?
Ear tubes are very small metal or plastic tubes a doctor inserts in your child’s ears to help reduce the number of ear infections by allowings fluid or pus to drain. Other names for them include tympanostomy tubes, ventilation tubes, myringotomy tubes or pressure equalization tubes.
Other names for them include tympanostomy tubes, ventilation tubes, myringotomy tubes or pressure equalization tubes.
They’re like a section of a really tiny drinking straw. They’re round, hollow, and usually made of metal or plastic.
Your doctor makes a small opening in the eardrum and puts in the tube to let air into the middle ear.
Almost all children have at least one ear infection by the time they’re 5. But if they occur over and over or your child has hearing loss because of fluid build-up, your doctor might suggest ear tubes.
If other treatments aren’t working, they can provide relief for your child. They also prevent long-term hearing problems.
Chronic Ear Infections
These happen when viruses or bacteria collect in the middle ear, the space right behind the eardrum. Children get more ear infections than adults because their bodies are still developing.
In kids, the parts of the ear that drain fluid, the Eustachian tubes, are smaller and almost level to the ground. That means they don’t drain as well even when a young one is healthy.
That means they don’t drain as well even when a young one is healthy.
When the Eustachian tubes swell or fill with mucus, perhaps during a cold, it’s even worse. It creates just the right conditions for bacteria to thrive, which can lead to infection. And for some kids, it just happens more often.
During an infection, fluid builds up in the middle ear. That creates pressure and pain. It also explains the following signs and symptoms:
- Fluid coming from the ear
- Hard time sleeping
- More fussiness or crying than normal, especially when lying down
- Seeming clumsy or having trouble with balance
- Tugging at an ear
When to Treat Chronic Ear Infections
Your doctor might take a wait-and-see approach. Often, a typical infection goes away on its own, especially if it’s from a virus. Sometimes your child needs antibiotics to kill infections caused by bacteria.
But some kids just get a lot of ear infections and sometimes they don’t clear up very easily. Usually, it doesn’t cause long-term problems, but frequent ones can lead to:
Usually, it doesn’t cause long-term problems, but frequent ones can lead to:
- Delays in learning speech and developing social skills
- Hearing loss
- Infection that spreads to other parts of the head
- Tears, or holes, in the eardrum
Treating Ear Problems with Ear Tubes
Whether your child needs tubes depends on their history with infections. Your doctor might suggest tubes if your child gets a lot of them, meaning:
- Three or more in 6 months
- Four or more in a year
Most commonly, kids get tubes because of:
- Trapped fluid behind the eardrum
- Long-term infections that antibiotics haven’t helped
- Fluid buildup that causes hearing loss, even if there’s no infection
- Persistent ear infection that results in tearing or a hole in the eardrum
How Ear Tubes Work
Ears have natural ventilation through your eustachian tubes -- narrow tubes that run from your middle ear to high in the back of your throat. The side of the tube in your throat opens and closes in order to:
The side of the tube in your throat opens and closes in order to:
- Stabilize air pressure
- Refresh the air in your ear
- Drain fluid
When swelling or mucus keeps natural ventilation from working, ear tubes act as a small window for your ear. They provide an alternative way to help air flow into and out of the ear, which keeps pressure even and helps the ear drain better.
With better airflow, fluid won’t build up and bacteria won’t have such a friendly home.
If your child has hearing loss from fluid buildup, it goes away as soon as the tubes are in. For delays in development, you’ll likely see improvement in the weeks and months ahead.
Ear Tube Surgery
Before your child’s surgery, you will likely get instructions from the hospital. Children who need to be given something to sleep will have to fast, or go without eating, for a certain number of hours before the surgery. Your child won’t be able to eat anything and can drink only certain liquids.
Check with your doctor to make sure you know:
- How long your child has to fast
- What liquids are OK
- If your child can take any medicine beforehand
Your doctor also will want to know about:
- Any medicine your child takes
- Problems that your child or anyone in your family has with drugs used for anesthesia (which make you unconscious so you won’t feel pain)
- Your child’s drug allergies
For adults getting ear tubes, your doctor may have similar questions.
Children, like some adults, will have concerns about what’s happening. To help them get ready for surgery, you may want to:
- Ask questions so they can talk about their feelings and you can make sure they're not confused about anything.
- Be specific about how the surgery will help, such as, “Your ear will feel so much better!”
- Talk ahead of time about going to the hospital. A good general rule is to talk 2 days ahead of time for a 2-year-old, 3 days for a 3-year-old, and so on.

- Let them pick a toy or blanket to take to the hospital.
- Remind them you’ll be there the whole time.
As you talk with children, it’s best to avoid certain phrases. If you say “put you to sleep,” that may remind them of a pet that’s been put down. Instead, you could talk about how a special doctor has medicine to help them sleep really well. The words “cut” or “make a hole” may make a child think of pain. Instead, you can say “make a small opening.”
On the day of the surgery, the first step for younger children is to get medicine so they’ll sleep through the procedure. The main reason is to make sure your child doesn’t move during the procedure.
You’ll take your youngster to a hospital or outpatient surgery center, and doctors will keep a close eye on their heart rate, oxygen, and blood pressure to make sure everything’s going well.
Older children and adults can have the surgery while they’re awake. For them, it can be done in the doctor’s office.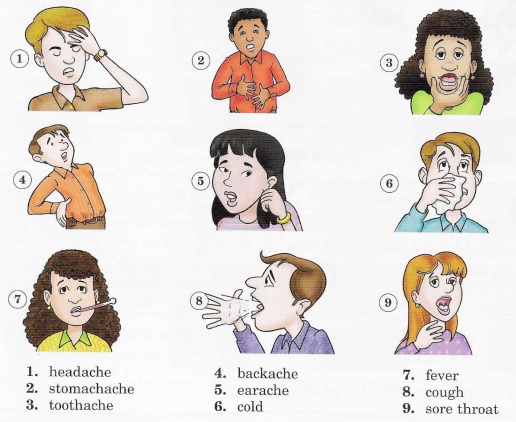
Ear tube surgery takes only about 15 minutes. During it, the surgeon:
- Makes a tiny cut in the eardrum with a scalpel or laser
- Removes fluids from the middle ear with suction
- Puts the tube into the hole in the eardrum
After it’s over, your child will go to a recovery room so nurses and doctors can be sure there were no problems. If all is well, you should be able to take your child home within a few hours.
Surgery and anesthesia can make kids groggy and possibly nauseated for the rest of the day. They should be back to normal after 24 hours.
Your doctor will schedule a follow-up appointment 2 to 4 weeks after the surgery to see if the tubes are in the right place and working well.
Risks of Ear Tube Surgery
Ear tube surgery is a safe procedure and doesn’t pose much serious risk. However, your child could have:
- Bleeding or infection
- Scars or weakness in the eardrum
- Tubes that fall out
- Drainage of ear fluid that doesn’t stop
- Blockages in the tubes from blood or mucus
- Eardrums that don’t close after tubes are removed
Some children have problems after being under anesthesia, and may have:
- An allergic reaction
- Trouble breathing
- Heart irregularities
- Nausea or vomiting
During recovery, talk to the doctor if your child has:
- Yellow, brown, or bloody ear discharge for more than a week
- Pain
- Hearing problems
- Balance problems
Ear Tube Surgery Recovery
Children who have been given anesthesia take some time to fully wake up.
They may be groggy, fussy, or a little queasy in the first 24 hours, but after that, they should be back to normal. You can usually take them home a few hours after the surgery.
Your child can go home right away if they weren’t given any anesthesia. The same is true for adults who get tubes.
Your doctor will talk to you about next steps. If everything goes as expected, this might mean a follow-up in 2 to 4 weeks, a hearing test, or ear drops to limit fluid coming from the ears.
If you see yellow, brown, or bloody fluid from the ear for more than a week after surgery, tell your doctor. You’ll also want to check with them if your loved one has ear pain, hearing problems, or trouble with balance.
Some ear tubes are for the short-term. They go in for 6 to 18 months and usually fall out on their own. Others are designed to stay in for longer. They may fall out on their own or might need to be taken out by a doctor.
Once the tubes are out, the opening in the eardrum usually closes on its own. If it doesn’t, your doctor may do a procedure to fix it.
If it doesn’t, your doctor may do a procedure to fix it.
what to do, first aid, how to treat
Most often, earaches begin suddenly - at night, on holidays or during rest, so they take the family by surprise. The problem can be caused by various internal and external factors. Most often, it is not possible to immediately determine the cause of pain in the ear, you have to act intuitively, rely on the help of a doctor or call an ambulance. It is important for parents to understand how to alleviate the condition of the baby. Learn how to competently and without harm to health to help a child if his ear hurts.
What you need to know about ear pain in children
| Functions of the human ear | The ear is a complex organ. They allow us not only to hear speech, sounds, but also help us navigate in space, maintain coordination of movements, determine where sounds come from, activate the cerebral cortex and brain centers. |
| How often do children get otitis media | By the age of 7, 95% of children suffer from acute otitis media at least once (1). More than 50% of cases occur in children under 5 years of age (2). More than 50% of cases occur in children under 5 years of age (2). |
| Otitis in children of the first year of life | Acute otitis media is a common disease in children of the first year of life, and in newborns it occurs 2 times more often than in older infants, and with a higher frequency in boys than in girls. In 31% of cases in newborns and in 26.5% of infants, acute otitis media occurs latently (that is, imperceptibly) (3). |
| Signs of ear pain in babies | At an early age it is difficult for a child to explain what is bothering him. When the ear hurts, the baby touches, rubs it and even pats it in annoyance. He lies on his side, where he hurts, cannot sleep, cries, is naughty, becomes lethargic and loses his appetite. |
| What not to do if your child has an earache | To avoid harm, never remove the wax plug with sharp objects or an ear stick. It is forbidden to rinse the ears with large amounts of water with a syringe and use antibiotics without consulting a doctor. If there is a discharge, you can not use ear drops and apply warm compresses to the sore spot. If there is a discharge, you can not use ear drops and apply warm compresses to the sore spot. |
How to understand that a child's ear hurts
- Recognizing the problem can be difficult, especially if the child is too young to tell his parents what is bothering him. Older children usually report sharp pains themselves. - The easiest way to determine the pain in the baby's ear is to lightly press on the tragus. This is a small cartilaginous protrusion on the outer ear, in front of the pinna. In case of pain, the child will definitely respond, advises Daniil Karpichev, lecturer in medical disciplines at the Cherepovets Medical College. N. M. Amosova .
Why a child may have an earache
Ear pain usually occurs at night, since the horizontal position promotes infection in the Eustachian tube and middle ear cavity. First of all, you need to find out the reason why the child has an earache. Consider the possible options.
Infections and anatomy
Most children experience ear infections at an early age. According to Russian scientists, more than 35% of babies already in the first year of life suffer from acute otitis media 1-2 times, and by the age of 3 years this diagnosis usually appears in the medical records of 71% of children (2).
The causes of the disease are the anatomical features of the location of the Eustachian tube. In babies, it is wide and short, so the infection easily gets from the nasopharynx into the Eustachian tube, and then into the middle ear cavity. In addition, when breastfeeding, milk can be thrown into the Eustachian tube. To avoid this, after feeding, the baby should be held upright for some time.
Foreign body in the ear
While playing, children can put buttons, small sweets, parts of the designer, beads, seeds, peas, pieces of cotton wool into the external auditory meatus. In more rare cases, ENT doctors find insects in the child's ear: ticks, cockroaches, bedbugs and flies. It most often occurs between the ages of 2 and 5.
It most often occurs between the ages of 2 and 5.
Foreign bodies cause discomfort and pain. With a long stay in the ear canal, complications can develop. It is not worth taking out a foreign body on your own - even if it is visible. It is better to trust a specialist who has everything necessary for the procedure.
Trauma to the ear or pinna
Mechanical trauma to the ear is a common problem in children. A child may experience pain after a burn or an insect bite, such as a bee. During sports training and games, with a strong blow, the ear may swell, sometimes blood appears from the ear canal. If this happens, close the ear canal with a sterile bandage or cotton, apply a bandage and go with the child to the emergency room.
Hypothermia
Hypothermia during windy weather can sometimes lead to ear pain. The people say about it "blown away".
Water in the ear
It happens that when swimming in a pool, river, sea or in the shower, water gets into the ear. If moisture has reached the middle ear, the child feels backache and congestion. Older children can be taught to hop on one or two legs by tilting their head towards the blocked ear. With kids who still do not know how to jump or do not understand how to do it, they act differently. An adult puts his hand to the blocked ear of the child, presses it with force, and then abruptly removes it. The air flow destroys the water plug.
If moisture has reached the middle ear, the child feels backache and congestion. Older children can be taught to hop on one or two legs by tilting their head towards the blocked ear. With kids who still do not know how to jump or do not understand how to do it, they act differently. An adult puts his hand to the blocked ear of the child, presses it with force, and then abruptly removes it. The air flow destroys the water plug.
Large buildup of earwax
Wax plug is a common problem in children. The fact that it exists is indicated by the absence of reactions to sounds, tinnitus, a feeling of congestion, coughing and other signs. The child may often rub his ear. It is better to solve the problem not at home, but with the help of a doctor.
Side effect of an infectious disease
Angina, laryngitis, pharyngitis, SARS can lead to complications in the form of ear pain. As a rule, discomfort disappears after the child gets rid of the underlying disease.
Ear canal abscess
The ear canals, like the skin in general, have their own hair follicles. If for some reason the hair follicle becomes inflamed, ear pain appears.
If for some reason the hair follicle becomes inflamed, ear pain appears.
What to do if your child's ear hurts: first aid at home
First aid can be provided at home, but then the child must be shown to a pediatrician or ENT doctor. After the examination, the doctor will give recommendations and prescribe the necessary drugs. Further treatment can take place on an outpatient basis, and with the development of complications of otitis media - in a hospital. If you called an ambulance, you should not give medicines and carry out any manipulations on your own. The doctor will examine the child, ascertain the symptoms and give recommendations.
If there is a temperature
If the temperature rises to 38°C or more, antipyretics based on ibuprofen or paracetamol can be given. These medicines also relieve ear pain. With severe unbearable pain, drops help (for example, Otipax, Otinum), but they can be instilled when there is no purulent discharge.
If there is no temperature
Seat the child. In an upright position, the mucus will more easily come out of the Eustachian tube, and the pain in the ear will decrease. If the nose is blocked, free it from mucus and drip vasoconstrictor drops.
In an upright position, the mucus will more easily come out of the Eustachian tube, and the pain in the ear will decrease. If the nose is blocked, free it from mucus and drip vasoconstrictor drops.
In the absence of purulent compartments, you can apply an alcohol compress to the ear: moisten gauze with alcohol, wrap around the ear, cover with wax paper and a layer of cotton. Wrap a scarf or scarf on top and leave for several hours.
Prevention of ear pain in children
Physicians cite regular viral infections, nearby adults smoking, infections in day care centers and family history of acute otitis media as risk factors (2). What can be done to avoid ear pain in children? Protect babies from hypothermia, infectious diseases, strengthen immunity. Kids need to be taught to play carefully with small objects, to explain that pencils, brushes, toothpicks, and other objects should not be put into their ears - anything that can cause injury to the auricles and eardrums. Do not let children swim without a rubber cap.
Do not let children swim without a rubber cap.
These are the basic rules for preventing injuries and otitis media. When it comes to health, it's better to be over-indulgent than under-indulgent.
Expert comments
Daniil Karpichev, Lecturer in Medical Sciences, Cherepovets Medical College. NM Amosova:
— Pain in the ears is a fairly common symptom, most often occurs with acute respiratory viral infections (rhinitis, nasopharyngitis). Pain in the ears against the background of high temperature may indicate the onset of the inflammatory process - otitis media. There is otitis externa, internal, with purulent discharge from the ear and without it. With timely treatment, the prognosis of the course of the disease is favorable. If it is not possible to see a doctor right now and there is no discharge from the ear, you can use drops with anti-inflammatory and analgesic effects. If the temperature persists for more than 4 days with pain in the ear, you may need antibiotic therapy, so you should not postpone visiting a specialist.
Elizaveta Gammel, pediatrician, functional diagnostician:
- The outer ear is a canal that runs from the auricle to the entrance to the middle ear, tightly closed by the tympanic membrane. Inflammation in the outer ear, called "otitis externa", can occur after a microtrauma, such as a scratch, or after hypothermia. This happens after swimming in the pool, or if you jump out without a hat on a cold street. The pain in this case is not very pronounced, but noticeable. The ear itches unbearably, and if you touch it or, moreover, look inside, it causes a sharp increase in pain. Sometimes there is discharge from the ear.
The middle ear is an isolated chamber. From the "street" it is closed by a thin eardrum. However, to maintain optimal pressure inside, the middle ear cavity is connected to the nasal cavity and pharynx by a thin tube - the Eustachian tube. When the pressure in the middle ear changes, the person feels stuffy in the ears and hearing is reduced. This happens, for example, when taking off in an airplane, going up in a high-speed elevator, or when the atmospheric pressure changes before it rains.
This happens, for example, when taking off in an airplane, going up in a high-speed elevator, or when the atmospheric pressure changes before it rains.
In inflammation of the middle ear, the tympanic cavity is filled with mucus - exudate. The pressure in the tympanic cavity rises, affecting the ear nerve. The pain is unbearable, it is comparable to the pain experienced by a woman during childbirth. On examination, the specialist will see redness of the eardrum, its bulging, and sometimes rupture. He will also determine that behind the eardrum is just exudate or pus. Pain in otitis media is throbbing, sharp, aggravated by any sound.
There is also such a thing as tubo-otitis. This is when, due to swelling in the nose during a runny nose, the lower part of the Eustachian tube is blocked, and a vacuum is created in the middle ear. In this case, the tympanic membrane is retracted. With tubo-otitis, a person feels a slight itch in the ear or as if something is tickling inside. There is no pain in this.
There is no pain in this.
Lidocaine drops and pain relievers based on ibuprofen or paracetamol are used for any ear pain. The child should immediately be shown to a doctor: a pediatrician who owns otoscopy, or an ENT doctor, since the treatment of different types of otitis media depends on the cause.
Popular Questions and Answers
pediatrician of the branch of the Israeli clinic "Hadassah" in Skolkovo Maria Volkova answers readers' questions.
Can I give my child pain medication if he has an earache?
In case of acute pain, the child should definitely be given an anesthetic, since the pain syndrome during otitis media is quite intense. This can affect the general condition of the child: appetite, sleep, mood. It is better to choose drugs based on ibuprofen or paracetamol.
When should an ambulance be called?
"Red flag" for ear pain and a signal for urgent medical attention - a severe pain syndrome that is not stopped by painkillers. In addition, it is important to assess the general condition of the child - severe anxiety or severe weakness, fever, swelling in the ear, and the appearance of discharge from the ear.
In addition, it is important to assess the general condition of the child - severe anxiety or severe weakness, fever, swelling in the ear, and the appearance of discharge from the ear.
What should I do if my child's ear is blocked but does not hurt?
In this case, an examination by an ENT doctor is also necessary. Ear congestion can be a symptom of hearing loss that occurs with otitis media. It is necessary to explain to the child that you can not "blow your nose hard" and "pull the mucus into yourself", because this can increase ear congestion. It is also recommended to drip vasoconstrictor drops into the nose.
What should I do if my child has an earache due to a cold?
In case of pain in the ear with a cold, you should definitely consult a pediatrician or an ENT doctor, since otitis media can be external or internal - when inflammation occurs behind the eardrum. It will depend on what treatment the doctor prescribes.
What should I do if my child's ear hurts at night?
In case of severe pain at night, it is necessary to give an anesthetic drug orally, instill drops in the ear based on an anesthetic. Usually this medicine is based on lidocaine. It is not recommended to apply heat to the ear, on the contrary, it can increase inflammation and pain. In the morning you need an urgent examination by a doctor.
Usually this medicine is based on lidocaine. It is not recommended to apply heat to the ear, on the contrary, it can increase inflammation and pain. In the morning you need an urgent examination by a doctor.
References
- Kochetkov P. A., Kosyakov S. Ya., Lopatin A. S. Acute otitis media // Practical Pulmonology. 2005. No. 4. URL: https://cyberleninka.ru/article/n/ostryy-sredniy-otit/viewer
- Ryazantsev S. V., Alekseenko S. I. The choice of drug therapy for ear pain in a child // Medical Council. 2018. (20). pp.18-23. URL: https://doi.org/10.21518/2079-701X-2018-20-18-23
- Minasyan VS Features of diseases of the middle ear in newborns and infants // Abstract of the dissertation. Moscow. 2004. URL: https://medical-diss.com/medicina/osobennosti-zabolevaniy-srednego-uha-u-novorozhdennyh-i-detey-grudnogo-vozrasta
Ear inflammation in a child: how to prevent complications
Otitis is one of the most common diseases in childhood. According to international statistics, 98% of children suffer from ear inflammation at least once, 60% experience the disease twice. What is effective prevention and how otitis is treated, said the otorhinolaryngologist of the Morozov Children's Hospital, Candidate of Medical Sciences, holder of the status of "Moscow Doctor" Alexander Mikhailovich Ivanenko.
According to international statistics, 98% of children suffer from ear inflammation at least once, 60% experience the disease twice. What is effective prevention and how otitis is treated, said the otorhinolaryngologist of the Morozov Children's Hospital, Candidate of Medical Sciences, holder of the status of "Moscow Doctor" Alexander Mikhailovich Ivanenko.
Why does otitis occur?
Depending on the location of the inflammatory process, otitis media can be external, medial or internal. Otitis externa is caused by microbes and fungi, most often manifested by damage to the skin of the ear canal and boils in the auricle.
Acute otitis media is an acute inflammation of the mucous membrane of the middle ear cavity. It develops against the background of respiratory infections. Ear infection occurs through the auditory tube, when mucus from the nasopharynx enters the middle ear and viruses, bacteria, fungal flora freely penetrate from the nasopharynx through the mouth of the auditory tube into the tympanic cavity.
Due to anatomical features, the smaller the child, the shorter and wider the auditory tube connecting the ear cavity with the nasopharynx. Therefore, in an infant who spends most of his time lying down, and in a younger child who does not know how to clean his nose, mucus can flow at any time. In adolescent children, the auditory tube is a tortuous narrow tube, so the infection from the nasopharynx to the middle ear is less likely to pass.
Adenoid vegetations also contribute to the development of ear inflammation. This is an overgrowth of the nasopharyngeal tonsil, which is the main focus of bacterial infection in the nasopharynx.
How does the disease manifest itself?
The main symptom of otitis media is pain in the ear. Children under one year old, as a rule, refuse to eat, because sucking movements cause pain. Babies often touch their ears, rub them, and cry. You can suspect otitis media by pressing on the tragus of the child's auricle.
The key method for diagnosing otitis media is otoscopy - an examination by a doctor of the external auditory canal and eardrum using a special instrument.
How to treat otitis?
If the inflammatory process is at the initial stage, outpatient treatment is carried out. The therapy is selected by a pediatrician or an otorhinolaryngologist depending on the child's condition. Be sure to use vasoconstrictor drops in the nose.
If medical assistance is not provided in a timely manner, the inflammatory process turns into acute catarrhal otitis media, and then into acute purulent otitis media, characterized by the appearance of purulent discharge from the ear. In some cases, with inadequate outflow of contents or its absence, the child in the hospital undergoes paracentesis - an incision in the eardrum. The intervention is performed under anesthesia. Then medical conservative treatment continues.
Which preventive measures are most effective?
There is an opinion among many parents that otitis media can be prevented by “covering the ear with cotton wool in the street” or “putting a few hats on the child”.