Second trimester warning signs
The Second Trimester of Pregnancy: Complications
The Second Trimester of Pregnancy: ComplicationsMedically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By April Kahn on December 3, 2018
Overview
The second trimester is often when people feel their best during pregnancy. Nausea and vomiting usually resolve, the risk of miscarriage has dropped, and the aches and pains of the ninth month are far away.
Even so, there are a few complications that can occur. Read on to learn what to watch for and how to prevent complications from occurring in the first place.
Bleeding
Although a miscarriage is much less common in the second trimester, it can still occur. Vaginal bleeding is usually the first warning sign. Miscarriages in the second trimester (before 20 weeks) may be caused by several different factors, which can include:
- Uterine septum. A wall, or septum, inside the uterus divides it into two separate parts.
- Incompetent cervix. When the cervix opens too soon, causing early birth.
- Autoimmune diseases. Examples include lupus or scleroderma. These diseases can occur when your immune system attacks healthy cells.
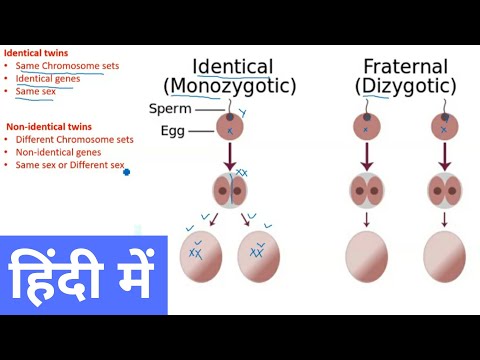
- Chromosomal abnormalities of the fetus. This is when something is wrong with the baby’s chromosomes, which are cells that are made up of DNA.
Other causes of bleeding in the second trimester include:
- early labor
- problems with the placenta, such as placenta previa (placenta covering the cervix)
- placental abruption (placenta separating from the uterus)
These problems are more common in the third trimester, but they can also occur late in the second trimester.
If you have have Rh-negative blood, get an injection of immunoglobulin (RhoGAM) if you experience bleeding during pregnancy.
Immunoglobulin is an antibody. An antibody is a protein your immune system produces that recognizes and fights harmful substances, such as bacteria and viruses.
Getting a shot of immunoglobulin will help prevent the development of Rh antibodies, which will attack the fetus if it has an Rh-positive blood type.
You may feel scared if you experience vaginal bleeding, but it’s important to remember that not all bleeding means pregnancy loss.
Seek immediate care if you’re bleeding in pregnancy, but try to stay calm while the doctor understands why you’re bleeding. You may be put on bed rest until the bleeding stops.
Preterm labor
When labor occurs before the 38th week of pregnancy, it’s considered preterm. Various conditions may cause preterm labor, such as:
- bladder infection
- smoking
- chronic health condition, like diabetes or kidney disease
Risk factors for preterm labor include:
- a previous preterm birth
- twin pregnancies
- multiple pregnancies
- extra amniotic fluid (the fluid surrounding the fetus)
- infection of the amniotic fluid or amniotic membranes
Symptoms
The signs and symptoms of preterm labor may be subtle. They can include:
They can include:
- vaginal pressure
- low back pain
- frequent urination
- diarrhea
- increased vaginal discharge
- tightness in the lower abdomen
In other cases, the symptoms of preterm labor are more obvious, such as:
- painful contractions
- leakage of fluid from the vagina
- vaginal bleeding
Call your doctor if you have these symptoms and are worried about being in labor. Depending on your symptoms, your doctor may tell you to go to the hospital right away.
Treatment
Each additional day you don’t go into preterm labor offers a chance for fewer complications when the baby is born. Several medications can be helpful in stopping preterm labor. These include:
- magnesium sulfate
- corticosteroids
- tocolytics
If preterm labor can’t be stopped, your doctor will give you a steroid medication. Doing so helps develop the baby’s lungs and reduces the severity of lung disease. It’s most effective two days after the first dose, so your doctor will try to prevent delivery for at least two days.
It’s most effective two days after the first dose, so your doctor will try to prevent delivery for at least two days.
Preterm premature rupture of membranes (PPROM)
It’s normal for your membranes to rupture (break) during labor. People often refer to it as “your water breaking.”
This occurs when the amniotic sac surrounding the baby breaks, allowing the amniotic fluid to flow out. That bag protects the baby from bacteria. Once it’s broken, there’s a concern of the baby getting an infection.
While your water is supposed to break when you go into labor, it can cause serious problems for your baby when it happens too early. This is called preterm premature rupture of membranes (PPROM).
The exact cause of PPROM isn’t always clear. In many cases, though, the source of the problem is an infection of the membranes.
PPROM in the second trimester is a big concern, as it can lead to a preterm delivery. Infants born between the 24th and 28th weeks of pregnancy are at the greatest risk for developing serious long-term medical problems, particularly lung disease.
The good news is that with the appropriate intensive care nursery services, most preterm infants tend to do very well.
Treatment
Treatment for PPROM varies. It can often include:
- hospitalization
- antibiotics
- steroids, such as betamethasone
- medications that can stop labor, such as terbutaline
If there are signs of an infection, labor may be induced to avoid serious complications. Antibiotics will be started to prevent infection.
Many babies are born within two days of rupture, and most will deliver within a week. In rare cases, especially with a slow leak, the amniotic sac can reseal itself. Preterm labor can be avoided, and the baby is born closer to their due date.
Cervical incompetence (cervical insufficiency)
The cervix is a tissue that connects the vagina and the uterus. Sometimes, the cervix is unable to withstand the pressure of the growing uterus during pregnancy. The increased pressure can weaken the cervix and cause it to open before the ninth month.
This condition is known as cervical incompetence, or cervical insufficiency. While it’s an uncommon condition, it can cause serious complications.
The opening and thinning of the cervix eventually leads to the rupture of membranes and delivery of a very premature fetus. This usually occurs around the 20th week of pregnancy. Since the fetus is too premature to survive outside the uterus at that point, the pregnancy often can’t be saved.
Women are at a higher risk for cervical incompetence if they’ve had:
- a previous cervical trauma, such as a tear during delivery
- a cervical cone biopsy
- other operation on the cervix
Symptoms
Unlike preterm labor, cervical incompetence typically doesn’t cause pain or contractions. There may be vaginal bleeding or discharge.
Treatment
Treatment for cervical incompetence is limited. An emergency cerclage (stitch around the cervix) is a possibility if the membranes haven’t ruptured yet. The risk of rupturing the membranes is higher if the cervix is very dilated (wide). Extended bed rest is necessary after the placement of a cerclage.
The risk of rupturing the membranes is higher if the cervix is very dilated (wide). Extended bed rest is necessary after the placement of a cerclage.
In other cases, when the membranes have already ruptured and the fetus is old enough to survive, your doctor will likely induce labor.
Prevention
You can prevent cervical incompetence. If you have a history of it, you can receive a cerclage with future pregnancies at about 14 weeks. This will lower, but not eliminate, the risk of having a preterm delivery and losing the baby.
Preeclampsia
Preeclampsia occurs when you develop:
- high blood pressure
- proteinuria (a large amount of protein in the urine)
- excessive edema (swelling)
Preeclampsia affects every system in the body, including the placenta.
The placenta is responsible for providing nutrients to the baby. Though preeclampsia typically occurs during the third trimester for first-time pregnancies, some people develop preeclampsia during the second trimester.
Before making a diagnosis, your doctor will evaluate you for other conditions that may be confused with preeclampsia, such as lupus (which causes inflammation throughout the body) and epilepsy (a seizure disorder).
Your doctor will also evaluate you for conditions that can increase the likelihood of developing early preeclampsia, such as blood clotting disorders and molar pregnancy. That’s a noncancerous tumor that forms in the uterus.
Symptoms
Symptoms of preeclampsia include rapid swelling of your legs, hands, or face. Call your doctor right away if you experience this type of swelling or any of the following symptoms:
- headache that doesn’t go away after taking acetaminophen (Tylenol)
- loss of vision
- “floaters” in your eye (specks or spots in your vision)
- severe pain on your right side or in your stomach area
- easy bruising
Injury
You’re more prone to injury during pregnancy. Your center of gravity changes when you’re pregnant, which means it’s easier to lose your balance.
In the bathroom, be careful when stepping into the shower or tub. You may want to add nonskid surfaces to your shower so you don’t slip. Consider adding grab bars or rails in your shower, too. Also check your house for other hazards that could cause you to fall.
Outlook
If you’re experiencing any of the symptoms described in this article, contact your doctor. They’ll be able to determine the cause and get you started on the right treatment — which means a happy and healthy pregnancy for you!
Last medically reviewed on December 3, 2018
- Parenthood
- Pregnancy
- 2nd Trimester
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Get the full 40 weeks of pregnancy. (n.d.).
health5mom.org/wp-content/uploads/2015/03/Go-The-Full-40-Implementation-Toolkit_2015-1.pdf - March of Dimes. (2015). Cervical insufficiency and short cervix.
marchofdimes.org/complications/cervical-insufficiency-and-short-cervix.aspx - March of Dimes. (2017). Miscarriage.
marchofdimes.org/complications/miscarriage.aspx - Mayo Clinic Staff. (2018). Preeclampsia.
mayoclinic.org/diseases-conditions/preeclampsia/basics/definition/con-20031644 - Moldenhauer J. S. (2018). Premature rupture of membranes (PROM).
merckmanuals.com/professional/gynecology-and-obstetrics/abnormalities-and-complications-of-labor-and-delivery/premature-rupture-of-membranes-prom - Rundell K, et al. (2017). Preterm labor: Prevention and management.
aafp.org/afp/2017/0315/p366.html - WomensHealth.gov. (2018). Pregnancy complications.

womenshealth.gov/pregnancy/youre-pregnant-now-what/pregnancy-complications
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Dec 3, 2018
Written By
April Kahn
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By April Kahn on December 3, 2018
related stories
The Second Trimester: Constipation, Gas, and Heartburn
The Importance of Checkups in the Second Trimester
The Second Trimester of Pregnancy: Changes in Skin, Vision, and Gums
Pain, Bleeding, and Discharge: When Should You Worry?
Stroke Risk Factors and Prevention
Read this next
The Second Trimester: Constipation, Gas, and Heartburn
Medically reviewed by Debra Sullivan, Ph.
 D., MSN, R.N., CNE, COI
D., MSN, R.N., CNE, COIYou may experience digestive issues, such as constipation or gas, during the second trimester of pregnancy. Learn techniques that can help.
READ MORE
The Importance of Checkups in the Second Trimester
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Here’s what you need to know about checkups and tests during your second trimester.
READ MORE
The Second Trimester of Pregnancy: Changes in Skin, Vision, and Gums
Medically reviewed by Janine Kelbach, RNC-OB
You may notice changes in your skin, vision, and gums. Most of these changes are only temporary and will go away after pregnancy.
READ MORE
Pain, Bleeding, and Discharge: When Should You Worry?
Medically reviewed by Debra Rose Wilson, Ph.
 D., MSN, R.N., IBCLC, AHN-BC, CHT
D., MSN, R.N., IBCLC, AHN-BC, CHTDuring the second trimester, pain, bleeding, and vaginal discharge are normal symptoms. In some cases, however, these symptoms may be a sign of a…
READ MORE
Stroke Risk Factors and Prevention
Medically reviewed by Seunggu Han, M.D.
A stroke occurs when blood flow is blocked to a part of the brain. Brain cells become deprived of oxygen and begin to die. As brain cells die, people…
READ MORE
Can Ectopic Pregnancy Be Diagnosed With Ultrasound?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Ectopic pregnancy is a serious condition that requires accurate and swift diagnosis. Ultrasound for ectopic pregnancy diagnosis is just one tool your…
READ MORE
Is It Safe to Consume Flaxseeds During Pregnancy?
Given the inconclusive and conflicting stances about eating flaxseeds during pregnancy, it might be better to err on the side of caution.
READ MORE
Pregnancy After Miscarriage: Answers to Your Questions
Medically reviewed by Amanda Kallen, MD
Getting pregnant after a miscarriage can be an emotional experience, filled with joy but also anxiety and guilt. Learn more about pregnancy after…
READ MORE
What Is a Nurse Midwife and How to Tell If They Are Right for You
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
A nurse midwife is a nurse with education, training, and certification to provide prenatal, delivery, and women's care.
READ MORE
Your 6-Week Ultrasound: What to Expect
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
We'll tell you all about the 6-week ultrasound, including why your doctor may have ordered it, what the risks are, and what it means if no heartbeat…
READ MORE
The Second Trimester of Pregnancy: Complications
The Second Trimester of Pregnancy: ComplicationsMedically reviewed by Debra Rose Wilson, Ph. D., MSN, R.N., IBCLC, AHN-BC, CHT — By April Kahn on December 3, 2018
D., MSN, R.N., IBCLC, AHN-BC, CHT — By April Kahn on December 3, 2018
Overview
The second trimester is often when people feel their best during pregnancy. Nausea and vomiting usually resolve, the risk of miscarriage has dropped, and the aches and pains of the ninth month are far away.
Even so, there are a few complications that can occur. Read on to learn what to watch for and how to prevent complications from occurring in the first place.
Bleeding
Although a miscarriage is much less common in the second trimester, it can still occur. Vaginal bleeding is usually the first warning sign. Miscarriages in the second trimester (before 20 weeks) may be caused by several different factors, which can include:
- Uterine septum. A wall, or septum, inside the uterus divides it into two separate parts.
- Incompetent cervix. When the cervix opens too soon, causing early birth.
- Autoimmune diseases.
Examples include lupus or scleroderma. These diseases can occur when your immune system attacks healthy cells.
- Chromosomal abnormalities of the fetus. This is when something is wrong with the baby’s chromosomes, which are cells that are made up of DNA.
Other causes of bleeding in the second trimester include:
- early labor
- problems with the placenta, such as placenta previa (placenta covering the cervix)
- placental abruption (placenta separating from the uterus)
These problems are more common in the third trimester, but they can also occur late in the second trimester.
If you have have Rh-negative blood, get an injection of immunoglobulin (RhoGAM) if you experience bleeding during pregnancy.
Immunoglobulin is an antibody. An antibody is a protein your immune system produces that recognizes and fights harmful substances, such as bacteria and viruses.
Getting a shot of immunoglobulin will help prevent the development of Rh antibodies, which will attack the fetus if it has an Rh-positive blood type.
You may feel scared if you experience vaginal bleeding, but it’s important to remember that not all bleeding means pregnancy loss.
Seek immediate care if you’re bleeding in pregnancy, but try to stay calm while the doctor understands why you’re bleeding. You may be put on bed rest until the bleeding stops.
Preterm labor
When labor occurs before the 38th week of pregnancy, it’s considered preterm. Various conditions may cause preterm labor, such as:
- bladder infection
- smoking
- chronic health condition, like diabetes or kidney disease
Risk factors for preterm labor include:
- a previous preterm birth
- twin pregnancies
- multiple pregnancies
- extra amniotic fluid (the fluid surrounding the fetus)
- infection of the amniotic fluid or amniotic membranes
Symptoms
The signs and symptoms of preterm labor may be subtle. They can include:
- vaginal pressure
- low back pain
- frequent urination
- diarrhea
- increased vaginal discharge
- tightness in the lower abdomen
In other cases, the symptoms of preterm labor are more obvious, such as:
- painful contractions
- leakage of fluid from the vagina
- vaginal bleeding
Call your doctor if you have these symptoms and are worried about being in labor. Depending on your symptoms, your doctor may tell you to go to the hospital right away.
Treatment
Each additional day you don’t go into preterm labor offers a chance for fewer complications when the baby is born. Several medications can be helpful in stopping preterm labor. These include:
- magnesium sulfate
- corticosteroids
- tocolytics
If preterm labor can’t be stopped, your doctor will give you a steroid medication. Doing so helps develop the baby’s lungs and reduces the severity of lung disease. It’s most effective two days after the first dose, so your doctor will try to prevent delivery for at least two days.
Preterm premature rupture of membranes (PPROM)
It’s normal for your membranes to rupture (break) during labor. People often refer to it as “your water breaking.”
This occurs when the amniotic sac surrounding the baby breaks, allowing the amniotic fluid to flow out. That bag protects the baby from bacteria. Once it’s broken, there’s a concern of the baby getting an infection.
Once it’s broken, there’s a concern of the baby getting an infection.
While your water is supposed to break when you go into labor, it can cause serious problems for your baby when it happens too early. This is called preterm premature rupture of membranes (PPROM).
The exact cause of PPROM isn’t always clear. In many cases, though, the source of the problem is an infection of the membranes.
PPROM in the second trimester is a big concern, as it can lead to a preterm delivery. Infants born between the 24th and 28th weeks of pregnancy are at the greatest risk for developing serious long-term medical problems, particularly lung disease.
The good news is that with the appropriate intensive care nursery services, most preterm infants tend to do very well.
Treatment
Treatment for PPROM varies. It can often include:
- hospitalization
- antibiotics
- steroids, such as betamethasone
- medications that can stop labor, such as terbutaline
If there are signs of an infection, labor may be induced to avoid serious complications. Antibiotics will be started to prevent infection.
Antibiotics will be started to prevent infection.
Many babies are born within two days of rupture, and most will deliver within a week. In rare cases, especially with a slow leak, the amniotic sac can reseal itself. Preterm labor can be avoided, and the baby is born closer to their due date.
Cervical incompetence (cervical insufficiency)
The cervix is a tissue that connects the vagina and the uterus. Sometimes, the cervix is unable to withstand the pressure of the growing uterus during pregnancy. The increased pressure can weaken the cervix and cause it to open before the ninth month.
This condition is known as cervical incompetence, or cervical insufficiency. While it’s an uncommon condition, it can cause serious complications.
The opening and thinning of the cervix eventually leads to the rupture of membranes and delivery of a very premature fetus. This usually occurs around the 20th week of pregnancy. Since the fetus is too premature to survive outside the uterus at that point, the pregnancy often can’t be saved.
Women are at a higher risk for cervical incompetence if they’ve had:
- a previous cervical trauma, such as a tear during delivery
- a cervical cone biopsy
- other operation on the cervix
Symptoms
Unlike preterm labor, cervical incompetence typically doesn’t cause pain or contractions. There may be vaginal bleeding or discharge.
Treatment
Treatment for cervical incompetence is limited. An emergency cerclage (stitch around the cervix) is a possibility if the membranes haven’t ruptured yet. The risk of rupturing the membranes is higher if the cervix is very dilated (wide). Extended bed rest is necessary after the placement of a cerclage.
In other cases, when the membranes have already ruptured and the fetus is old enough to survive, your doctor will likely induce labor.
Prevention
You can prevent cervical incompetence. If you have a history of it, you can receive a cerclage with future pregnancies at about 14 weeks. This will lower, but not eliminate, the risk of having a preterm delivery and losing the baby.
This will lower, but not eliminate, the risk of having a preterm delivery and losing the baby.
Preeclampsia
Preeclampsia occurs when you develop:
- high blood pressure
- proteinuria (a large amount of protein in the urine)
- excessive edema (swelling)
Preeclampsia affects every system in the body, including the placenta.
The placenta is responsible for providing nutrients to the baby. Though preeclampsia typically occurs during the third trimester for first-time pregnancies, some people develop preeclampsia during the second trimester.
Before making a diagnosis, your doctor will evaluate you for other conditions that may be confused with preeclampsia, such as lupus (which causes inflammation throughout the body) and epilepsy (a seizure disorder).
Your doctor will also evaluate you for conditions that can increase the likelihood of developing early preeclampsia, such as blood clotting disorders and molar pregnancy. That’s a noncancerous tumor that forms in the uterus.
That’s a noncancerous tumor that forms in the uterus.
Symptoms
Symptoms of preeclampsia include rapid swelling of your legs, hands, or face. Call your doctor right away if you experience this type of swelling or any of the following symptoms:
- headache that doesn’t go away after taking acetaminophen (Tylenol)
- loss of vision
- “floaters” in your eye (specks or spots in your vision)
- severe pain on your right side or in your stomach area
- easy bruising
Injury
You’re more prone to injury during pregnancy. Your center of gravity changes when you’re pregnant, which means it’s easier to lose your balance.
In the bathroom, be careful when stepping into the shower or tub. You may want to add nonskid surfaces to your shower so you don’t slip. Consider adding grab bars or rails in your shower, too. Also check your house for other hazards that could cause you to fall.
Outlook
If you’re experiencing any of the symptoms described in this article, contact your doctor. They’ll be able to determine the cause and get you started on the right treatment — which means a happy and healthy pregnancy for you!
They’ll be able to determine the cause and get you started on the right treatment — which means a happy and healthy pregnancy for you!
Last medically reviewed on December 3, 2018
- Parenthood
- Pregnancy
- 2nd Trimester
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Get the full 40 weeks of pregnancy. (n.d.).
health5mom.org/wp-content/uploads/2015/03/Go-The-Full-40-Implementation-Toolkit_2015-1.pdf - March of Dimes. (2015). Cervical insufficiency and short cervix.
marchofdimes.org/complications/cervical-insufficiency-and-short-cervix.aspx - March of Dimes. (2017). Miscarriage.

marchofdimes.org/complications/miscarriage.aspx - Mayo Clinic Staff. (2018). Preeclampsia.
mayoclinic.org/diseases-conditions/preeclampsia/basics/definition/con-20031644 - Moldenhauer J. S. (2018). Premature rupture of membranes (PROM).
merckmanuals.com/professional/gynecology-and-obstetrics/abnormalities-and-complications-of-labor-and-delivery/premature-rupture-of-membranes-prom - Rundell K, et al. (2017). Preterm labor: Prevention and management.
aafp.org/afp/2017/0315/p366.html - WomensHealth.gov. (2018). Pregnancy complications.
womenshealth.gov/pregnancy/youre-pregnant-now-what/pregnancy-complications
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Dec 3, 2018
Written By
April Kahn
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Share this article
Medically reviewed by Debra Rose Wilson, Ph. D., MSN, R.N., IBCLC, AHN-BC, CHT — By April Kahn on December 3, 2018
D., MSN, R.N., IBCLC, AHN-BC, CHT — By April Kahn on December 3, 2018
related stories
The Second Trimester: Constipation, Gas, and Heartburn
The Importance of Checkups in the Second Trimester
The Second Trimester of Pregnancy: Changes in Skin, Vision, and Gums
Pain, Bleeding, and Discharge: When Should You Worry?
Stroke Risk Factors and Prevention
Read this next
The Second Trimester: Constipation, Gas, and Heartburn
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
You may experience digestive issues, such as constipation or gas, during the second trimester of pregnancy. Learn techniques that can help.
READ MORE
The Importance of Checkups in the Second Trimester
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Here’s what you need to know about checkups and tests during your second trimester.

READ MORE
The Second Trimester of Pregnancy: Changes in Skin, Vision, and Gums
Medically reviewed by Janine Kelbach, RNC-OB
You may notice changes in your skin, vision, and gums. Most of these changes are only temporary and will go away after pregnancy.
READ MORE
Pain, Bleeding, and Discharge: When Should You Worry?
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
During the second trimester, pain, bleeding, and vaginal discharge are normal symptoms. In some cases, however, these symptoms may be a sign of a…
READ MORE
Stroke Risk Factors and Prevention
Medically reviewed by Seunggu Han, M.D.
A stroke occurs when blood flow is blocked to a part of the brain. Brain cells become deprived of oxygen and begin to die.
 As brain cells die, people…
As brain cells die, people…READ MORE
Can Ectopic Pregnancy Be Diagnosed With Ultrasound?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Ectopic pregnancy is a serious condition that requires accurate and swift diagnosis. Ultrasound for ectopic pregnancy diagnosis is just one tool your…
READ MORE
Is It Safe to Consume Flaxseeds During Pregnancy?
Given the inconclusive and conflicting stances about eating flaxseeds during pregnancy, it might be better to err on the side of caution.
READ MORE
Pregnancy After Miscarriage: Answers to Your Questions
Medically reviewed by Amanda Kallen, MD
Getting pregnant after a miscarriage can be an emotional experience, filled with joy but also anxiety and guilt. Learn more about pregnancy after…
READ MORE
What Is a Nurse Midwife and How to Tell If They Are Right for You
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
A nurse midwife is a nurse with education, training, and certification to provide prenatal, delivery, and women's care.

READ MORE
Your 6-Week Ultrasound: What to Expect
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
We'll tell you all about the 6-week ultrasound, including why your doctor may have ordered it, what the risks are, and what it means if no heartbeat…
READ MORE
Warning signs during pregnancy - CGP on REM city polyclinic No. 11
We discuss the most pressing issues of pregnancy management in the classroom at the Young Mother's School and invite our women to an active constructive dialogue.
Schools are held in the format of an interactive conversation, we invite you to ask questions to the doctor, get comprehensive advice on planning and managing pregnancy, contraception and women's health. Our obstetrician-gynecologists are ready to do everything possible for a comfortable pregnancy, however, we hardly get feedback from our women.
Ladies, Women's Health Schools are held every Thursday from 13.00 to 14.00.
First trimester warning signs that require medical attention:
- vomiting more than 8-10 times a day
- bleeding from the genital tract
- severe pain in the abdomen or side.
- The pain may be dull at first and then begins to increase.
Physiological changes during pregnancy that do not require special treatment:
- nausea
- change of taste
- appearance or darkening of pigment spots on the skin
- soreness of the mammary glands.
There are three trimesters during pregnancy. The first trimester corresponds to the first three months of pregnancy, the second - the period from 4 to 6 months of pregnancy,
Signs that require immediate medical attention in the second trimester of pregnancy:
- persistent or severe headache
- blurred vision or flickering of dark dots ("flies") before the eyes
- noticeable or sudden onset and rapidly increasing edema
- bleeding from the genital tract
- severe persistent abdominal pain
- persistent vomiting
- no fetal movement within 24 hours
- profuse watery vaginal discharge (amniotic fluid rupture)
You should know and seek immediate medical attention if you develop any of the following symptoms in the third trimester of pregnancy:
- bleeding from the genital tract
- profuse watery vaginal discharge (amniotic fluid discharge)
- persistent or severe headache
- blurred vision or flickering of dark dots ("flies") before the eyes
- fever up to 38C or more
- severe abdominal pain
- weakening or absence of fetal movements
- contractions at intervals of 5-10 minutes.

Signs that urgently need to seek medical attention in the postpartum period:
- profuse bleeding (you have to change several pads per hour), bright red or with clots
- purulent, foul-smelling discharge from the genital tract, severe pain in the lower abdomen
- increase in body temperature up to 38 C or more
- soreness, discharge in the area of the postoperative suture on the anterior abdominal wall or in the perineum
- engorgement, soreness, redness of the mammary glands.
#gynecologist #GP11 #obstetrician_gynecologist #health_school #pregnancy #pregnancy_alarm signs #symptoms
Second trimester of pregnancy (13 to 28 weeks)
The beginning of the second trimester is traditionally considered one of the calmest. Walk more. Walking is very helpful. Sit down to rest only when you are tired. Movement in the fresh air improves the supply of oxygen to the fetus, which is very necessary for its normal development.
Nausea disappears, appetite improves. Do not eat a lot of salty, refuse marinades, smoked meats, if you have not done this before. The increased need of the child's body for proteins and vitamins begins. The daily diet should include meat or fish (boiled or stewed), dairy products, especially cottage cheese, eggs. Do not forget about vegetables, fruits, greens. An excellent source of vitamin C is sauerkraut (rather than salted) cabbage. Salads from carrots, cabbage, beets, apples, green radish should be on your table every day.
At 17-20 weeks you will feel your baby's first kicks. From them you can determine how comfortable the baby feels. Intense tremors are a signal of lack of oxygen. Maybe you haven’t walked for a long time or, on the contrary, you are engaged in hard physical labor. Get out into the fresh air or lie down to rest and you will immediately feel how the child has calmed down.
But the lack of movement is an alarm. See a doctor immediately!
The fetal need for calcium sharply increases - intensive growth of the skeleton has begun. If you don't have enough free calcium in your body right now, you could lose your teeth. To prevent this from happening, start taking calcium supplements in consultation with your doctor.
If you don't have enough free calcium in your body right now, you could lose your teeth. To prevent this from happening, start taking calcium supplements in consultation with your doctor.
At this time, toxicosis of the second half of pregnancy may occur, the child suffers greatly from it. Therefore, if the doctor suggests hospitalization, do not refuse. Toxicosis can, if not be avoided, then at least reduce its manifestations. Be sure to follow your diet. Completely exclude salty, smoked, fried, spicy, canned food, chocolate. Do not eat a lot of grapes and drink fresh milk. Limit flour and rich products. As before, your diet should include boiled meat and fish, oatmeal and buckwheat porridge, vegetables and fruits
Periodically, once a week, check for fluid retention in the body. It is allowed to release liquid 200-300 ml less than what was drunk. If little urine is released, this is a signal of latent edema and the onset of toxicosis.
It is very good if you can measure your blood pressure at home.