Can i still breastfeed with cracked nipples
Breastfeeding with Sore Nipples - La Leche League International
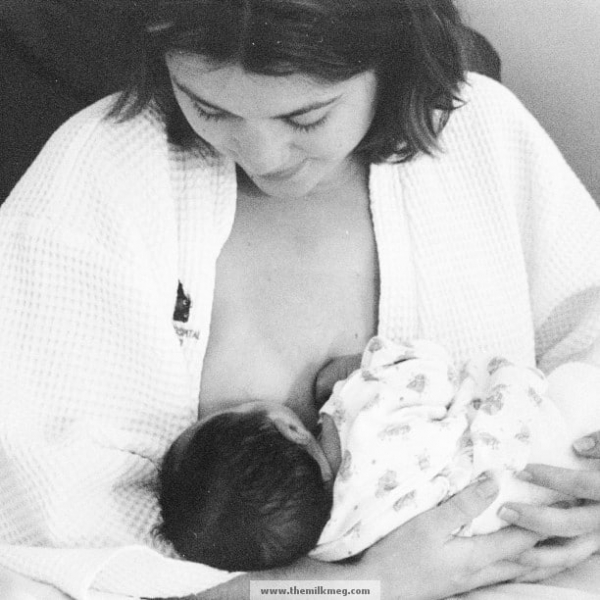
Breastfeeding is something only you can do for your baby. It should be a pleasant experience for both of you. A healthy, full-term baby is likely to know instinctively what to do at the breast. In the first three to five days after birth, if you experience nipple soreness beyond a slight tenderness when your baby latches on, it may be a sign that something isn’t right with the baby’s latch, position, or suck. An adjustment to the latch or positioning can help you and your baby to be more comfortable. With proper positioning and latch-on techniques, you can expect little or no nipple soreness. Correcting poor positioning or latch-on can often alleviate sore, cracked nipples and allow healing to begin.
If nipple pain worsens after the early days of breastfeeding your nipple pain may be due to other causes like thrush, bacterial infection, or tongue-tie. Contact a La Leche League Leader for help if you need further assistance to improve your sore nipples.
Learn to recognize your baby’s early feeding cues so you have time to get in a good position and comfortable before he becomes desperately hungry. Early cues include opening his mouth and moving his head side-to-side—known as the rooting reflex—or sucking on hands or fingers. Don’t wait for baby to cry to let you know he is hungry. Crying is a very late hunger cue.
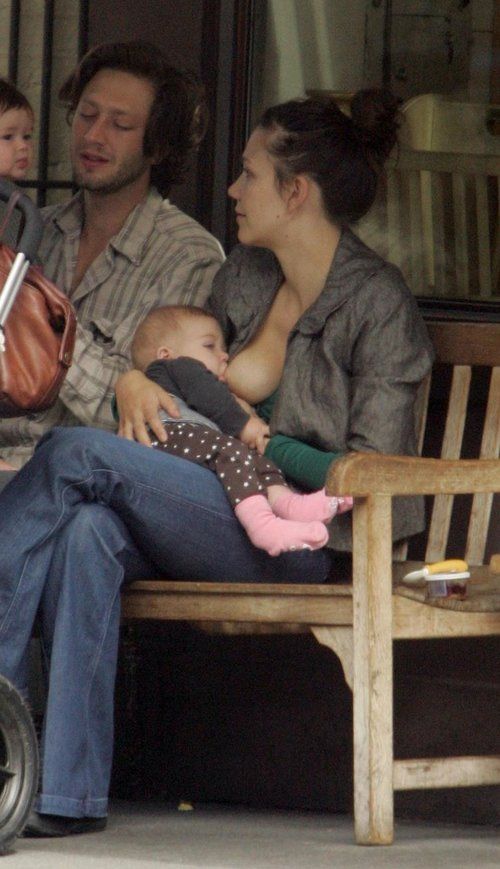
Adjusting the position can improve breastfeeding pain. If you have pain, try different positions such as laid-back, football or cradle position.
Laid-back position- Position yourself comfortably in bed, on the couch or in a recliner with back support, pillows to also support your head, shoulders, arms. Since you’re leaning back, your baby can rest on you in any position you like.
- If you are seated, support your feet with a footrest or a telephone book.
- Let your baby’s whole front touch your whole front.
 His mouth and nose should be facing your nipple. Let your baby’s cheek rest somewhere near your bare breast.
His mouth and nose should be facing your nipple. Let your baby’s cheek rest somewhere near your bare breast. - Rub your nipple on baby’s upper lip to encourage baby to open wide. Bring your baby close. Have his chin touch your breast first, and then his nose will touch your breast.
- Position baby close to you, with his hips flexed, so that he does not have to turn his head to reach your breast. Baby’s feet need to feel supported by your body so they don’t dangle in the air.
- Use one hand to support your breast, if needed, and the other to support baby’s thigh or bottom.
- If you are feeling pain, detach baby gently by using your finger to touch the corner of baby’s mouth and try again.
- This is a good position for a mother who has had a Cesarean birth, as it keeps the baby away from the incision.
- Baby’s is to your side on the same side you are breastfeeding and under your arm. Support your baby’s head in your hand and his back along your arm beside you.

- Support your breast with a “C” hold.
- Have baby facing the nipple, with his mouth at nipple height. Use pillows to bring the baby to the correct height.
- Your baby’s legs and feet are tucked under your arm with his hips flexed and his legs resting along side your back rest so the soles of his feet are pointed toward the ceiling. (This keeps him from being able to push against your chair.)
- Make sure you are relaxed and comfortable as your baby feeds. Lean back in your chair, supporting your back with a bed pillow turned vertically if needed. Don’t lean forward and hunch over your baby. Raise your feet off the floor, using an ottoman or even a phone book. Breathe deeply and be sure to relax and drop your shoulders.
- Position your baby on his side, with his whole body facing yours and angled so his chest is securely against your abdomen. Baby should not have to turn his head to nurse.
- Cradle baby in the arm on the same side as the breast he will be nursing from.
 If you’re breastfeeding on the right breast, baby’s head will rest on your right forearm near your elbow, his nose at the level of your nipple, and his head tilted slightly back. He is supported by your forearm with your hand holding his bottom or thigh.
If you’re breastfeeding on the right breast, baby’s head will rest on your right forearm near your elbow, his nose at the level of your nipple, and his head tilted slightly back. He is supported by your forearm with your hand holding his bottom or thigh. - Support your breast with your other hand well back from the nipple and baby’s mouth, keeping your fingers positioned either above or below or on either side of the breast.
- Bring your baby to the breast. Trigger his natural response to open his mouth wide by touching his lips lightly with your nipple. Light, repeated tapping or brushing triggers a wide-open mouth.
- As you bring baby to the breast with his head slightly tilted back, his chin will press into the breast first. More of your breast will be covered with his lower jaw.
- Aim your nipple toward the roof of baby’s mouth and gently bring him onto the breast as he latches on.
- When baby is latched well, his chin should be pressed into the breast, and his nose slightly away from it.

- If you leave the hand supporting the breast in place, be sure you do not press down with your thumb, which can pull your nipple to the front of baby’s mouth. If you remove the supporting hand from your breast, make sure baby has enough head control to keep him well latched. If your breasts are large, it can be helpful to put a small rolled-up towel beneath them for support.
- This position is a variation of the cradle position, called the cross-cradle position.
- For this position, your baby is supported on a pillow across your lap to help raise him to your nipple level.
- Pillows should also support both elbows so your arms don’t hold the weight of the baby; they will tire before the feeding is finished.
- If you are preparing to breastfeed on the left breast, your left hand supports that breast in a “U” hold.
- You support your baby with the fingers of your right hand. Do this by gently placing your hand behind your baby’s ears and neck with your thumb and index finger behind each ear.

- Your baby’s neck rests in the web between the thumb, index finger and palm of your hand, forming a “second neck” for baby. The palm of your hand is placed between his shoulder blades.
- As you prepare to latch on your baby, be sure his mouth is very close to your nipple from the start. When baby opens his mouth wide, you push with the palm of your hand from between the shoulder blades. His mouth will be covering at least a half-inch from the base of your nipple.
If baby is not latched on well or if it hurts, remove him from the breast by inserting your finger into the side of his mouth and try again.
Look at your nipple after breastfeeding, if it looks blanched or pinched, review the latch and positioning tips to see if you can find adjustments to make. The nipple should look the same way it did before breastfeeding, neither pinched nor blanched.
If nipple soreness persists, contact a La Leche League Leader for help. Mild soreness, if left untreated, can lead to more pain.
You may also find this post about Positioning useful.
Causes of Sore NipplesImproper latch-on occurs when baby does not grasp enough breast tissue or his tongue is positioned improperly. Baby must be able to compress your breast tissue with your nipple positioned deep in his mouth. First, check baby’s body position. Be sure that he opens his mouth very wide, like a yawn, before you offer your breast, checking to see that his tongue is cupped and forward in his mouth. His lower lip should not be tucked in—it should be fanned outward on the breast. If you gently pull down the corner of the baby’s mouth while he is nursing, you should see the underside of his tongue, which should extend over his lower gum line, cupping the breast
Sometimes babies latch deeply, but slide down the nipple during the feed—watch for more distance between his nose and your breast. If this happens, break the suction and re-latch your baby, being sure that he is well supported.
Tongue-tie can also cause sore nipples. When baby cries, can you see if his tongue is able to reach past his lower lip? If baby’s tongue appears heart-shaped, it could be a short or restricted frenulum (tongue-tie) that prevents a good latch-on. Contact a La Leche League Leader if your baby does not seem to be latching on well.
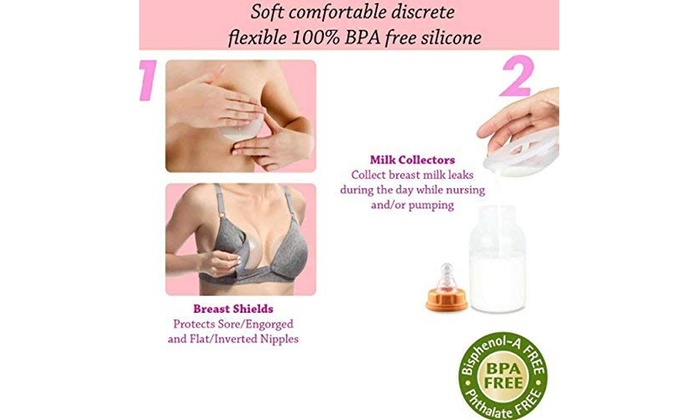
Flat or inverted nipples can make it difficult for baby to grasp your breast in his mouth and properly latch on. With proper latch-on, your baby’s sucking can effectively draw out flat or inverted nipples. Gentle pumping or special exercises are sometimes recommended to draw the nipple out. If you received IV fluids for several hours during the birth process, this can be a cause of edema (swelling) in the breast and nipple. Reverse Pressure Softening can help create a softer nipple/areola that baby can grasp. Reverse Pressure Softening involves using gentle finger pressure around the base of the nipple. This temporarily moves some of the swelling slightly backward and upward into the breast. This technique is also helpful in preventing sore nipples if your breasts become engorged (swollen and uncomfortable) when your milk supply comes in several days after birth, making it difficult for baby to latch on comfortably.
This technique is also helpful in preventing sore nipples if your breasts become engorged (swollen and uncomfortable) when your milk supply comes in several days after birth, making it difficult for baby to latch on comfortably.
Removing baby from the breast without breaking the suction first can be painful and cause damage to sensitive breast tissue. If baby is latched on and sucking well, he will end the feeding himself by letting go of the breast or releasing the nipple as he falls asleep. Allowing baby to determine the end of the feeding will ensure that he is getting the right balance of foremilk at the beginning of the feed, which is more watery and quenches baby’s thirst, and hindmilk at the end of the feed, which is creamy milk that is higher in calories and satisfies baby’s hunger. If you decide to take baby off the breast before he is finished, you can break the suction by pressing down on your breast near baby’s mouth, pulling down on baby’s chin, or inserting your finger into the corner of baby’s mouth.
Personal care practices may lead to nipple soreness. Avoid bras that are too tight and put pressure on your nipples. Be vigilant about thorough rinsing of nursing bras to be sure any laundry detergent residue is removed. Soap, shampoo, body wash, and alcohol can dry your nipples. Take care when applying cologne, deodorant, hair spray, or powder near your nipples. When bathing, rinsing breasts with clear water is all that is needed to keep your breasts and nipples clean.
When your nipples are sore you can gently apply your own milk or an emollient that is safe for the baby to ingest, such as HPA® Lanolin. Either of these can be very soothing. Contact a La Leche League Leader for suggestions.
Be aware that more than one cause can be contributing to nipple soreness at the same time. Avoid limiting the length of nursing sessions, a practice that is mistakenly thought of as a way to avoid sore nipples. Instead, aim to coordinate optimal positioning with careful personal care practices, and contact a La Leche League Leader for helpful tips.
While the cause of sore nipples is being determined and corrected, continued breastfeeding is important. When baby is latched on well with your nipple deep in his mouth, the nipple is protected from further damage. You may want to try one or more of these comfort measures while the cause of your sore nipples are being corrected.
Vary nursing positions—cradle hold, cross cradle hold, football (clutch) hold, and lying down—in order to vary the position of baby’s mouth on your breast. (For information on various nursing positions, contact an LLL Leader for assistance.)
Begin to nurse on the least sore side until the letdown occurs, then gently switch baby to the other breast, paying careful attention to good positioning and latch-on. Some mothers use relaxation breathing until their milk lets down.
Express a little milk or colostrum onto your nipples after nursing. In many cultures, human milk’s antibacterial properties are used to treat skin irritations. However, this is not recommended when soreness is due to thrush, which is a yeast infection of the nipples.
However, this is not recommended when soreness is due to thrush, which is a yeast infection of the nipples.
When your nipples are sore, apply some of your own milk on your nipples. Your milk has healing properties to relieve soreness. Also, a small pea-sized portion of ultrapure modified lanolin, such as HPA® Lanolin, between clean fingertips and apply to the nipple and areola. Gently pat it on: do not rub it in. It does not need to be removed before feedings. This provides a moisture barrier that will slow down the loss of internal moisture, which is vital to healthy, supple skin, eases discomfort, and promotes healing without scab formation. This process is known as “moist wound healing.” Gel pads may provide relief from soreness and promote healing.
Lanolin or gel pads are not recommended if you have a yeast infection.
If the pressure of your clothing or your bra causes further discomfort for your nipples, apply ultrapure lanolin after feedings to help soothe, protect, and heal nipples, then use breast shells with large openings.
In most cases, sore or cracked nipples are no longer painful once good positioning and latch on are achieved. It is rarely necessary to discontinue breastfeeding. The many benefits to both baby and mother make continuing to breastfeed worthwhile.
It is not typically recommended any more that mothers dry sore nipples with a hair dryer or use a sun lamp. These practices have been shown to dehydrate skin further and cause additional damage to tender nipple tissue.
Sore, cracked or bleeding nipples
Sore, cracked or bleeding nipples | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Sore, cracked or bleeding nipples are common. Some mothers have such trouble with them that they stop breastfeeding early.
As a new mother, you may find it could take a few days or weeks to adapt to the strong suck of a healthy baby on your breasts.
It is normal for your breasts to become more sensitive in the first weeks after you have given birth. They may sting, burn, ache or feel tender. Over time, the discomfort and sensitivity should resolve.
If you have sore nipples, it may be that your baby isn’t attaching properly to your breast. This pain usually lasts about half a minute while baby first draws your nipple into their mouth.
Try to make sure your baby’s mouth is attached correctly for suckling from the very first breastfeed.
If you do not correct your baby’s latch, your nipples could be damaged, which causes problems like mastitis (infections).
How to get baby to attach to your breast correctly
- Make sure you are sitting or lying comfortably. Position your baby’s chest against your chest, with their mouth and nose facing your nipple.
- If you are lying down, let your baby’s cheek rest against your breast. If you are sitting up, lift your breast slightly so it does not press on your baby’s chin.

- Position your baby so the first contact point is their chin on your areola — the coloured area around your nipple.
- Bring your baby’s head to your breast, not the breast to baby’s head. Support your baby to move to where they are trying to go — towards your nipple.
- Ensure the nipple and much (or all) of the areola and some surrounding breast are in your baby’s mouth.
After a few rapid gulps, your baby should start to suck and swallow in a regular rhythm. Once you have got the hang of it, breastfeeding can be enjoyable and should not be painful.
How to manage sore nipples
Before putting baby to the breast
Wash your hands and sit in a comfortable position and try to relax. Apply a warm washer to the breast and gently massage or express to help milk flow. Express some milk to soften the areola to lubricate the nipple.
At the breast
Poor attachment is a key cause of sore nipples. Make sure the way your baby latches to your breast is correct. If you are not sure, ask for help from a health professional.
If you are not sure, ask for help from a health professional.
If the attachment feels uncomfortable after 30 seconds, break your baby’s suction by putting your finger in the corner of their mouth. Take your baby off and let them re-latch to your breast. Try different feeding positions. If your nipples are tender, limit your baby’s comfort sucking.
After the breastfeed
Check your nipples for redness and misshapen appearance. Wipe your breasts with clean water and let them dry. It can help to leave your bra off for a while and allow your nipples to air. Make sure your bra fits.
When expressing milk, make sure that the suction on your breast pump is not too strong. If the pain in your nipples increases after the first week, talk to a health professional.
Finding the cause of cracked or bleeding nipples
You will need to work out the source of your nipple problems. The first thing to do is to check if your baby is latching on correctly. You may need to ask a health professional for assistance. They can also check your baby for problems with their lips and tongue and whether you have medical problems like dermatitis or nipple infection. If you use a nipple shield, make sure it is the correct size and if you’re using a breast pump, make sure you’re doing it properly.
They can also check your baby for problems with their lips and tongue and whether you have medical problems like dermatitis or nipple infection. If you use a nipple shield, make sure it is the correct size and if you’re using a breast pump, make sure you’re doing it properly.
How to treat cracked or bleeding nipples
There are a number of things you can do to treat cracked or bleeding nipples.
- Look after your nipples: wash your nipples with water after every feed and clean and sterilise your nipple shield after each feed.
- If you can, continue breastfeeding (it is quite safe for baby to feed on a bleeding nipple). But if it’s too painful, you may need to take your baby off the breast for 24 to 48 hours, rest the nipple and feed your baby expressed breast milk. Gradually reintroduce the breast after resting for a short time and take special care with positioning and attachment.
- If you’re going to take pain-relieving medication, talk to your doctor or pharmacist.
 Many household remedies are ineffective or harmful.
Many household remedies are ineffective or harmful.
The Australian Breastfeeding Association has more tips on treating sore or cracked nipples.
If you need further help or are experiencing prolonged abnormal breast pain, contact your doctor, lactation consultant, breast feeding counsellor, child health nurse or Pregnancy Birth and Baby on 1800 882 436.
Sources:
Australian Breastfeeding Association (Sore/cracked nipples), Australian Breastfeeding Association (Mastitis), Australian Breastfeeding Association (Attachment to the breast), Raising Children Network (Breastfeeding attachment techniques), Tresillian (Breastfeeding 0-3 months)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: December 2020
Back To Top
Related pages
- Expressing and storing breast milk
- Breastfeeding your baby
Need more information?
Nipple infections | Australian Breastfeeding Association
About 10% of breastfeeding mothers experience nipple/breast pain (not associated with breast redness or fever) that is often described as one or more of the following: ‘burning’, ‘stabbing’, ‘knife-like’, ‘shooting’, ’sharp’. It is possible that such pain is caused by a nipple infection, especially when baby is attaching well to the breast, it is beyond the first week and other causes of nipple pain/trauma have been ruled out (e.g. tongue tie). This article provides information about the causes and symptoms of nipple infection.
It is possible that such pain is caused by a nipple infection, especially when baby is attaching well to the breast, it is beyond the first week and other causes of nipple pain/trauma have been ruled out (e.g. tongue tie). This article provides information about the causes and symptoms of nipple infection.
Read more on Australian Breastfeeding Association website
Sore/cracked nipples | Australian Breastfeeding Association
Mothers are often surprised to find breastfeeding feels more awkward, complicated or painful than they were prepared for. Breastfeeding is a learned skill for mothers. Like with learning any new skill, it can take some time to get the hang of breastfeeding. Sometimes breastfeeding feels difficult because mothers have been given traditional advice to position their babies in a way that feels uncomfortable. Uncomfortable breastfeeding positions can cause your baby to squash the nipple as they feed.
Read more on Australian Breastfeeding Association website
Vasospasm | Australian Breastfeeding Association
Vasospasm happens when blood vessels tighten and go into spasm, so that blood does not flow normally. Mothers with vasospasm of the nipple feel sharp pain, burning or stinging in the nipple. It is usually accompanied by sudden whitening of the nipple, followed by a colour change from red to blue.There are two main causes of nipple vasospasm.It can be a response of the nipple to trauma, if the baby is not attached to the breast well. In this case, it tends to occur following breastfeeds. Attention to how your baby attaches can help resolve this problem.
Read more on Australian Breastfeeding Association website
Breastfeeding – mastitis and other nipple and breast problems - Better Health Channel
Mastitis affects some breastfeeding women and may be caused by blocked milk ducts or a bacterial infection.
Read more on Better Health Channel website
Breastfeeding | Sydney Children's Hospitals Network
Breastfeeding is not always easy and you may have trouble breastfeeding your baby
Read more on Sydney Children's Hospitals Network website
Breastfeeding Advice For Newborn Babies | Tresillian
When establishing breastfeeding good positioning and attachment are key. Here are some tips from Tresillian to help your breastfeed your newborn.
Read more on Tresillian website
Vasospasm and breastfeeding
Vasospasm affects the flow of milk from the nipple and can be a painful condition for women breastfeeding. Learn about vasospasm and how to relieve the pain.
Read more on Pregnancy, Birth & Baby website
Attachment to the breast | Australian Breastfeeding Association
A baby who attaches well to the breast can help prevent many breastfeeding problems. The well-attached baby causes no nipple pain and drains the breast well. This helps ensure a good milk supply so the baby grows well. In this article you can find out how to attach your baby well using different techniques and holds, including baby-led attachment, the cradle hold, the underarm (football) hold and lying down.
Read more on Australian Breastfeeding Association website
Breast milk expressing - MyDr.com.au
There are a number of reasons why a breast feeding mother might wish to express milk rather than feeding the baby directly from the breast.
Read more on myDr website
Breastfeeding
Breastfeeding is learnt over the first weeks and months of your child’s life. It is a unique and special experience for families as no two mothers or babies are the same.
Read more on Karitane website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Cracked nipples in nursing mothers, methods of their treatment and prevention
08.10.2020 Reading time: 5 min 82324
Content:
- Causes of cracked nipples
- Risk of cracked nipples
- How to feed a baby with cracked nipples
- Is it necessary to stop breastfeeding with fissures
- How to organize the process of breastfeeding with cracks
- How to treat cracked nipples
- Prevention of cracked nipples
Breastfeeding a baby is an exciting and joyful process, but, alas, it does not always go smoothly. Approximately 10-15% of nursing mothers experience the problem of cracked nipples. They can occur from the first days of feeding, cause pain, discomfort, interfere. This problem requires a timely solution: you should not feed through force, it is better to take care of treatment in a timely manner. Neglecting the problem can make it worse.
Approximately 10-15% of nursing mothers experience the problem of cracked nipples. They can occur from the first days of feeding, cause pain, discomfort, interfere. This problem requires a timely solution: you should not feed through force, it is better to take care of treatment in a timely manner. Neglecting the problem can make it worse.
Causes of cracked nipples
Cracks are easy to identify: they look like small wounds, scratches or tears in the skin in the nipple area. Sometimes injuries to the skin of the breast occur for reasons unrelated to the behavior of the mother and baby, but breastfeeding errors are much more common. They are often allowed by primiparas, who do not have experience and sufficient baggage of information. Although WHO recommends that physicians provide adequate information to patients both before and immediately after delivery [1], mothers can still face challenges.
Incorrect nipple latch. Doctors say it's a common cause of damage. Until now, many people believe that the capture of the nipple by a child during feeding is simple, and are perplexed when faced with the need to learn. The fact is that it is difficult to properly capture the breast for a baby, although he has a sucking reflex almost immediately. If breastfeeding is incorrect, only the tip of the nipple will be in the mouth of the baby, which will roll freely in the mouth during feeding. In an attempt to fix the chest, the baby will try to grab it with his gums, inadvertently injuring. You can understand that this is a problem by several signs:
Until now, many people believe that the capture of the nipple by a child during feeding is simple, and are perplexed when faced with the need to learn. The fact is that it is difficult to properly capture the breast for a baby, although he has a sucking reflex almost immediately. If breastfeeding is incorrect, only the tip of the nipple will be in the mouth of the baby, which will roll freely in the mouth during feeding. In an attempt to fix the chest, the baby will try to grab it with his gums, inadvertently injuring. You can understand that this is a problem by several signs:
- the child causes pain to the mother while feeding;
- baby does not fully grasp the areola during suckling.
Incorrect grip leads to the fact that after 2-3 feedings, microtraumas will appear on the surface of the nipple, which can subsequently turn into deep cracks.
Incorrect pumping. This problem is usually encountered by mothers who pump irregularly, for example, only in situations when they need to go somewhere. They lack experience to form a habit. If pumping is done manually, you do not need to press on the entire nipple: this is a common mistake that leads to microtrauma and damage.
They lack experience to form a habit. If pumping is done manually, you do not need to press on the entire nipple: this is a common mistake that leads to microtrauma and damage.
Interfering with feeding. It happens that the mother mistakenly believes that the child has already eaten, and tries to wean him from the breast. The baby continues to eat and reflexively begins to grab the nipple, which leads to his injuries. So that weaning does not cause discomfort to the mother and does not lead to the appearance of cracks, you need to do this only when the baby is sure to eat, fall asleep and release the breast on his own. If, for some reason, the mother urgently needs to stop feeding, you can gently insert a finger into the baby's mouth, and only then remove the breast.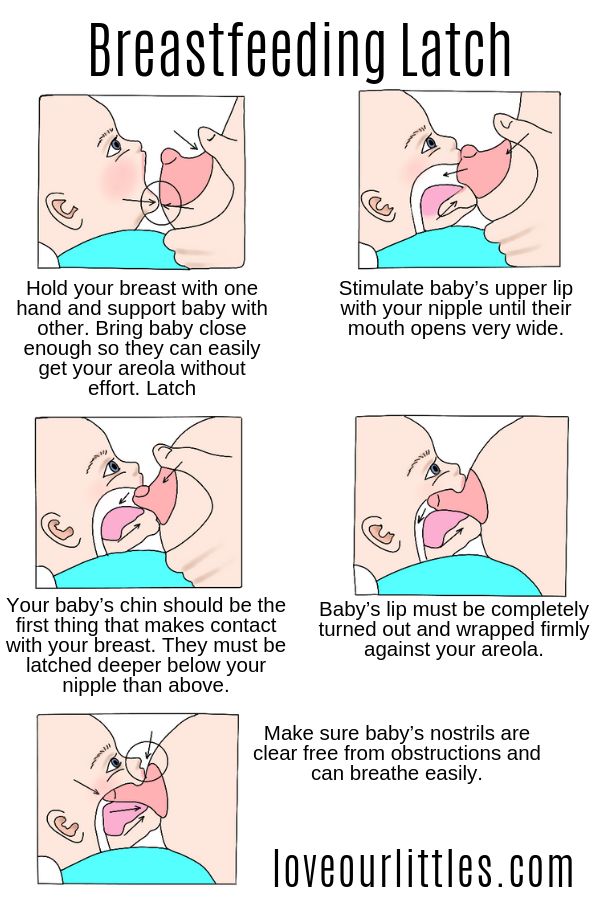 This will help avoid injury. Also, do not abuse pacifiers: a baby accustomed to them squeezes the chest more.
This will help avoid injury. Also, do not abuse pacifiers: a baby accustomed to them squeezes the chest more.
Improper care of the skin of the mammary glands. Neglect of hygiene or, conversely, an excess of drying care products can also cause cracks. Soap, cosmetics, which contain alcohol - all this dries the skin, and overdried skin is easier to injure. Some people think that it is necessary to wash the breast with soap before each feeding. This is not so: daily hygiene procedures are enough. Improper care may also include:
- wearing underwear that is too tight or hard in unsuitable fabrics, underwired bras;
- use of powders and other laundry detergents that may cause allergies.
Cracks can also occur due to leaking milk residues. They are recommended to be removed. If a baby develops thrush in his mouth, this can also harm the sensitive skin of the chest - you need to carefully monitor the condition of the baby.
Skin diseases. Cracked nipples are often associated with other diseases, both infectious and non-infectious. For example, allergies or thrush can increase the risk of injury. In addition, diseases can develop against the background of cracks: injured skin is more vulnerable to infections. If you find signs of any illness, contact your doctor immediately. The specialist will prescribe treatment and give advice on what to do with feeding further, depending on the situation.
Sensitive skin. There is a situation when the baby is properly applied to the breast, but the nipples still crack and hurt. This may be due to the individual characteristics of the skin. If the skin is thin and sensitive, the mother usually knows about this in advance, but for reliability, you can consult a doctor. In such situations, the cracks are usually small and quickly heal, and the sensitivity gradually decreases. The longer a woman breastfeeds, the less discomfort she causes, until eventually it disappears completely. However, if the pain does not go away, this is a reason to consult a specialist.
However, if the pain does not go away, this is a reason to consult a specialist.
Vascular problems. After milk has been sucked out of the breast, a spasm may occur in it. Nipples at such moments become hard and tense, hurt and change color. It is important to remember that in the event of a spasm, the nipple becomes especially vulnerable, so the breast should be treated with care. Discomfort will soon pass: vasospasm does not last long. To alleviate the condition, you can put a damp, warm towel or heating pad on your chest.
Danger of cracked nipples
It may seem that microtrauma does not cause much harm to the mother, but this is not so. It is not worth neglecting them and feeding through force, ignoring pain. In fact, injured nipple skin is an open door for a variety of infections. If bacteria get into the crack, an inflammatory process may begin, which will subsequently pass to the entire mammary gland. Cracks can cause mastitis.
In addition, inflammation can lead to serious consequences: you will need to drink medicines and possibly stop breastfeeding. Therefore, if cracks appear on the nipples, you need to pay attention to this immediately, do not endure and do not think that pain is normal. Cracks are easier to manage when they are still shallow; the more severe the injury, the longer it will take to heal.
Therefore, if cracks appear on the nipples, you need to pay attention to this immediately, do not endure and do not think that pain is normal. Cracks are easier to manage when they are still shallow; the more severe the injury, the longer it will take to heal.
How to feed a baby with cracked nipples
By themselves, microtraumas are not a reason to stop breastfeeding, but sometimes the pain during feeding is so severe that the mother begins to think about it. In reality, this is not at all necessary: there are ways to continue breastfeeding your baby, even if cracks appear on the nipples. Breastfeeding is beneficial for both mother and baby. The baby receives all the substances he needs, the mother, in turn, releases the hormone oxytocin [2], which, among other things, contributes to the return to normal after childbirth.
Is it necessary to stop breastfeeding with fissures
No, this is completely optional if the cracks are not caused by an infection or have not become infected after they appeared. Of course, if the damage is deep, blood or ichor oozes from the injured nipple, you should not give it to the child. It is better to wait for complete healing. The same goes for inflammation, conditions in which the milk is contaminated or the baby can become infected through contact with the nipple. In such cases, you need to consult a doctor, consult with him about taking medication and the possibility of continuing to feed. You should not neglect a visit to the doctor, each case is individual and needs to be considered separately. If there is no infection or extensive damage, then there is no ban on feeding even if there are cracks. But there are ways to reduce the pain and reduce the risk of further injury to the breast.
Of course, if the damage is deep, blood or ichor oozes from the injured nipple, you should not give it to the child. It is better to wait for complete healing. The same goes for inflammation, conditions in which the milk is contaminated or the baby can become infected through contact with the nipple. In such cases, you need to consult a doctor, consult with him about taking medication and the possibility of continuing to feed. You should not neglect a visit to the doctor, each case is individual and needs to be considered separately. If there is no infection or extensive damage, then there is no ban on feeding even if there are cracks. But there are ways to reduce the pain and reduce the risk of further injury to the breast.
How to Organize Breastfeeding with Fissures
- Attach the baby correctly to the breast, correctly remove it from the baby's mouth after feeding and hold the baby during feeding. You can learn this with the help of informational materials or specialists: doctors or lactation consultants [3], who will teach you how to properly attach your baby to the breast.
 According to some reports, this can reduce the risk of cracks by 50%;
According to some reports, this can reduce the risk of cracks by 50%; - If only one breast is damaged, it is recommended not to feed it until the cracks have healed, and to use the second for the healing period.
- Special nipple covers for nursing can be used. They prevent the baby from squeezing the nipple and damaging the skin of the breast. There are also sanitary pads that are worn between feedings. Under them, you can apply a healing ointment.
- Feed the baby more often than usual. The more hungry the baby, the more intensively he sucks.
- It is recommended to start with a less damaged nipple: at the beginning of feeding, the baby sucks more actively.
- If the injury is severe, breastfeeding can be interrupted by expressing, then giving the baby the expressed milk. After wound healing, HB can be resumed.
How to treat cracked nipples
If the nipples are injured, treatment should be comprehensive. These are healing ointments and preparations containing vitamins: they are needed to strengthen and protect the skin. Overdried with soap or alcohol-containing products, the skin will need to be moisturized. The scheme in each case is individual and depends on the condition of the breast. You can consult with your doctor to better understand how to treat cracks in a particular case. Remember that drugs must be approved for use while breastfeeding.
These are healing ointments and preparations containing vitamins: they are needed to strengthen and protect the skin. Overdried with soap or alcohol-containing products, the skin will need to be moisturized. The scheme in each case is individual and depends on the condition of the breast. You can consult with your doctor to better understand how to treat cracks in a particular case. Remember that drugs must be approved for use while breastfeeding.
Basic preparations. There are several basic products that can help with cracks:
- ointments and creams based on dexpanthenol. This substance is used as a wound healing, at the same time it increases skin regeneration, moisturizes and strengthens. It is used for burns, wounds, ulcers. Well-known means - "Panthenol-D" or "Bepanten". Funds are sold in different forms;
- preparations containing zinc. Zinc has an anti-inflammatory and antibacterial effect, avoids the penetration of infection into wounds, but dries the skin;
- products with lanolin, which has a moisturizing effect.
 It is recommended to eliminate dry skin;
It is recommended to eliminate dry skin;
Folk remedies. If the cracks are still shallow, there is no inflammation or infection, you can use folk methods. They are also used for prevention. They should be used with caution: remember that some herbs may cause allergies or not be suitable in a particular case, and untested remedies can do harm. To avoid this risk, check in advance if the method is safe and use only those that will not cause harm. This is the milk itself, which, according to some reports, has a wound-healing effect. You can gently anoint the nipples with breast milk and be without underwear for a while.
Remember that this does not always work, and if the defeat is serious, this will not be enough. In the case of inflammation, extensive damage or infection, consult a doctor and use the drugs that he will prescribe.
Prevention of cracked nipples
It is much easier to prevent painful and interfering cracks than it is to treat them. To reduce the risk of them occurring, you can:
To reduce the risk of them occurring, you can:
- consult a doctor or use the services of a lactation consultant [3], who will teach you how to properly latch on. According to some reports, this can reduce the risk of cracks by 50%;
- start breast care in advance. Do not overdry it with soap or care products, and moisturizers, do not wear tight traumatic underwear;
- use hygienic liners and change them when wet, so that an excessively humid environment does not provoke cracks;
- do not neglect hygiene, but also do not wash your breasts too often. A daily shower will suffice.
World medical organizations, in particular the WHO, agree that breast milk is the best food for an infant [1]. Moreover, breastfeeding can also be beneficial for the mother [2]. Therefore, you should not turn off the process when cracks occur, unless there are serious reasons for this. You can get rid of pain and injuries, and then feeding will not cause discomfort to either the baby or his mother.
[1] WHO: Breastfeeding
[2] Carlos Gonzalez "The Gift of a Lifetime: A Guide to Breastfeeding"
[3] William and Martha Sears "Your Baby from Birth to 2 Years"
(0 ratings; article rating 0)
Cracked nipples | Medela
Amir, L.H. ABM Clinical Protocol #4: Mastitis, Revised March 2014. Breastfeed Med 9, 239–243 (2014). - Amir L.Kh., "AVM Clinical Protocol #4: Mastitis", revised March 2014 Brestfeed Med 9 (Breastfeeding Medicine) 239–243 (2014).
Jacobs, A. et al. S3-Guidelines for the Treatment of Inflammatory Breast Disease during the Lactation Period: AWMF Guidelines, Registry No. 015/071 (short version) AWMF Leitlinien-Register Nr. 015/071 (Kurzfassung). Geburtshilfe Frauenheilkd . 73, 1202–1208 (2013). - Jacobs, A. et al., "Guideline S -3 for the management of inflammatory breast disease during breastfeeding: AWMF Guideline , registration number 015/071 (abbreviated version)" Leitlinjen- Registration number 015/071 (Kurzfassung). Geburtschilde Frauenheilkd. 73, 1202–1208 (2013).
Geburtschilde Frauenheilkd. 73, 1202–1208 (2013).
American Academy of Pediatrics and The American College of Obstetricians and Gynecologists. Breastfeeding handbook for physicians 2006). - American Academy of Pediatrics and American College of Obstetrics and Gynecology. "Medical Guide to Breastfeeding", 2006.
Lawrence , R . A . & Lawrence , R . M . Breastfeeding : a guide for the medical profession ( Elsevier Mosby , Maryland Heights , MO , 2011). - Lawrence R. A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." (Publishing house Maryland Heights , Missouri, USA: Elsevier Mosby; 2011.)
A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." (Publishing house Maryland Heights , Missouri, USA: Elsevier Mosby; 2011.)
McClellan, H.L. et al. Infants of mothers with persistent nipple pain exert strong sucking vacuums. Paediatica 97, 1205–1209 (2008). — McClellan H.L. et al., "Babies of mothers suffering from persistent nipple pain create extremely high sucking vacuums." Pediatrics 97, 1205–1209 (2008).
McClellan, H.L. et al. Breastfeeding frequency, milk volume, and duration in mother-infant dyads with persistent nipple pain. Breastfeed Med 7, 275–281 (2012). — McClellan H.L. et al., "Breastfeeding frequency, milk quantity and duration of feedings in case of persistent maternal sore nipples", Brestfeed Med (Breastfeeding Medicine) 7, 275–281 (2012).
McClellan, H.L. et al. Nipple pain during breastfeeding with or without visible trauma.