Vulvar swelling in pregnancy
How to Ease Vaginal Swelling During Pregnancy
Swelling is a common side effect of pregnancy, especially when it comes to your feet and hands. But there’s one area that can also swell during pregnancy that doesn’t get a lot of attention: Your vagina. If you notice you have a swollen vagina during pregnancy, know you’re not the only woman going through this! Still, we’re guessing you might have questions about why this is happening. Here’s what you need to know, plus how to minimize the swelling and ease any discomfort.
In this article:
Symptoms of vaginal swelling during pregnancy
What causes vaginal swelling during pregnancy?
How to reduce vaginal swelling during pregnancy
How to prevent vaginal swelling during pregnancy
Symptoms of Vaginal Swelling During Pregnancy
Every woman and every pregnancy is different—which means the symptoms of vaginal swelling during pregnancy can differ from person to person. In general, though, you might experience the following:
• Noticeable swelling. You’re probably familiar on at least some level with what your vulva and vaginal area usually feels like. If it’s swollen, it can feel noticeably bigger or puffier, says Frederick Friedman, Jr., MD, associate professor of obstetrics, gynecology and reproductive science at the Icahn School of Medicine at Mount Sinai in New York City. “There may just be a general feeling of swelling or fullness in the vaginal area,” adds Julie Lamppa, APRN, CNM, a certified nurse midwife at Mayo Clinic, which can lead to overall discomfort.
• Bumps. Some women who experience vaginal swelling during pregnancy can have varicose veins surface in their vulvar area, which can cause swelling and a bumpy feel down there, Lamppa says.
• Itchiness. This isn’t the case for every woman, but itchiness can sometimes accompany vaginal swelling, Lamppa says.
What Causes Vaginal Swelling During Pregnancy?
There are several reasons why you might develop vaginal swelling in pregnancy. Here are some of the most common ones:
Here are some of the most common ones:
• An increase in blood volume. Your blood volume increases during pregnancy to help support the growing baby. As your uterus grows, there’s also an increase in pressure of the blood vessels in your pelvis, Lamppa explains. The combination of these two things can lead to swelling.
• Varicose veins in your vulva. Varicose veins are swollen, bumpy veins that develop when valves let blood pool in one spot or flow backward. Just like you can develop varicose veins in your legs, you can also develop these in your vulva during pregnancy, Lamppa says. “These aren’t dangerous, but they can be alarming to women when they suddenly show up.”
• A yeast infection. Yeast infections are common among moms-to-be, and they can also lead to a swollen vagina during pregnancy, Friedman says. “The inflammation that results from the infection can cause more swelling,” he explains.
• Excess fluid. Excess fluid can get trapped in your body’s tissues during pregnancy, and that can cause swelling down there, Friedman says.
Excess fluid can get trapped in your body’s tissues during pregnancy, and that can cause swelling down there, Friedman says.
How to Reduce Vaginal Swelling During Pregnancy
If you suspect that your vaginal swelling is due to excess fluid, compression or support stockings might help. “There are products on the market that you can buy that give vulvar support,” Lamppa says. (Just check in with your doctor first to make sure it’s okay for you to use.)
For direct relief, Lamppa recommends applying a cool pack directly to your vulva. That should help with discomfort as well as cut down on some of the swelling.
If you’re experiencing vaginal swelling along with symptoms of a yeast infection—such as an itchy vaginal area during pregnancy, accompanied by white vaginal discharge—Lamppa recommends seeing your doctor for an evaluation. If they determine that you do, in fact, have a yeast infection, your care provider will likely recommend that you use an over-the-counter cream.
How to Prevent Vaginal Swelling During Pregnancy
Sorry, but there isn’t a ton you can do to lower the odds you’ll experience vaginal swelling during pregnancy, given that it’s a normal side effect of being pregnant, Lamppa says. However, doing your best to avoid sitting or standing for long periods of time may be helpful, Friedman suggests.
While it’s pretty common, it’s a good idea to flag any vaginal swelling during pregnancy for your care provider so they can help pinpoint the cause and get you sweet relief ASAP.
Updated January 2020
Expert bios:
Frederick Friedman, Jr., MD, is an associate professor of obstetrics, gynecology and reproductive science at the Icahn School of Medicine at Mount Sinai. He also serves as director for both the division of obstetrics and the division of generalists in the department of obstetrics, gynecology and reproductive science at the Mount Sinai Health System, and maintains a clinical practice in general obstetrics and gynecology.
Julie Lamppa, APRN, CNM, is a certified nurse midwife and medical editor at Mayo Clinic, and maintains a midwifery practice in Rochester, New York.
*Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances. *
Plus, more from The Bump:
Swelling in Pregnancy: Why It Happens and How to Deal
How Your Vaginal Discharge Can Change During Pregnancy
10 Surprising Pregnancy Symptoms No One Warned You About
Spontaneous Massive Vulvar Edema in Pregnancy: A Case Report
On this page
AbstractIntroductionCase ReportDiscussionConclusionConsentConflicts of InterestReferencesCopyrightRelated Articles
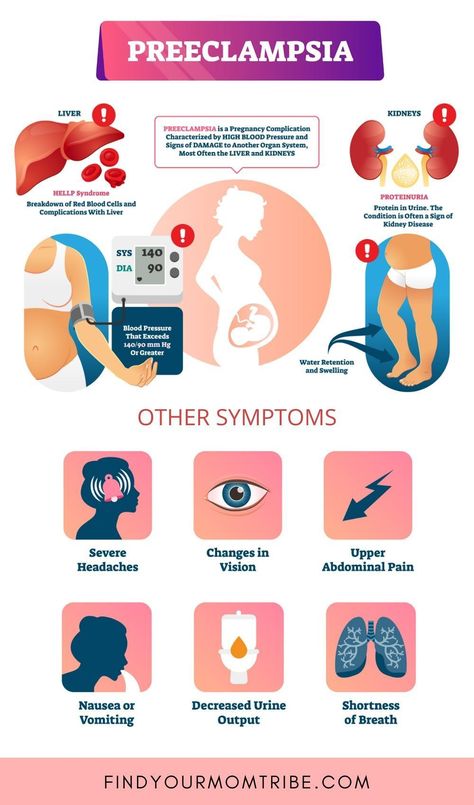
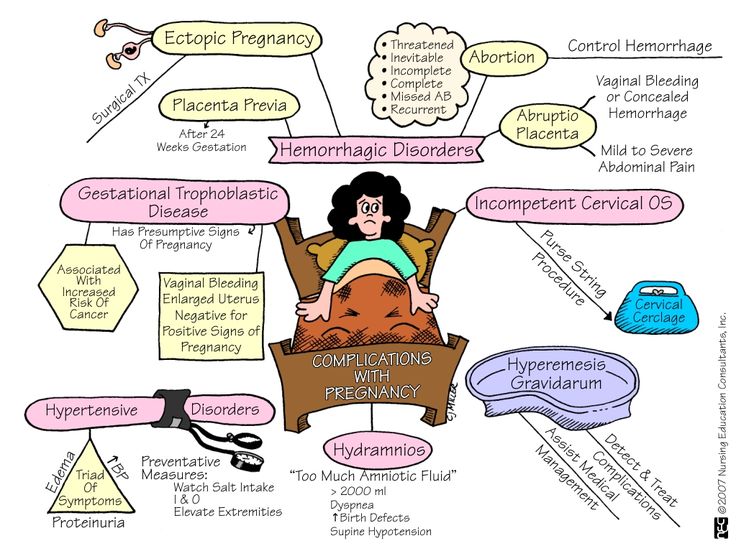
Spontaneous massive vulvar edema in pregnancy is unusual and a cause for concern. This condition should be taken seriously since it might be caused by some conditions such as preeclampsia, diabetes, vulvovaginitis, severe anemia, and neoplasms. We report a case of massive vulvar edema in a 15-year-old primigravida following tocolysis therapy at 33 weeks of gestation. Other causes of vulvar edema were excluded. The vulvar edema appeared spontaneously after tocolysis and rapidly increased in size, associated with severe vulvar pains. The vulvar edema resolved progressively with antibiotics, corticoids, and analgesics. The patient delivered by spontaneous vaginal delivery a term live newborn with an unremarkable postpartum period. The aim of this report is to alert clinicians that conservative attempts could be considered for vulvar edema complicating tocolysis.
This condition should be taken seriously since it might be caused by some conditions such as preeclampsia, diabetes, vulvovaginitis, severe anemia, and neoplasms. We report a case of massive vulvar edema in a 15-year-old primigravida following tocolysis therapy at 33 weeks of gestation. Other causes of vulvar edema were excluded. The vulvar edema appeared spontaneously after tocolysis and rapidly increased in size, associated with severe vulvar pains. The vulvar edema resolved progressively with antibiotics, corticoids, and analgesics. The patient delivered by spontaneous vaginal delivery a term live newborn with an unremarkable postpartum period. The aim of this report is to alert clinicians that conservative attempts could be considered for vulvar edema complicating tocolysis.
1. Introduction
Spontaneous massive vulvar edema is uncommon during pregnancy with management challenges and significant patient discomfort especially pain and difficulty in ambulation [1]. In literature, the cases of the massive vulvar edema have been described associated with multiple pregnancy, diabetes, hypoproteinemia, preeclampsia, tocolytic therapy, vulvovaginitis, and severe anemia [1–4]. But very rarely is the occurrence after tocolytic therapy.
But very rarely is the occurrence after tocolytic therapy.
Vulvar edema has also been reported to result from infections, neoplasms, congenital lymphatic anomalies, trauma, inflammatory, and metabolic disorders [4, 5]. Vulvar edema should also be considered as in important marker for seropositive syphilis in pregnancy as reported in a study among pregnant Mozambican women [6].
In this report we describe a case of spontaneous massive vulvar edema following tocolytic therapy in a 15-year-old primigravida child who presented at 33 weeks of gestation with preterm labor.
2. Case Report
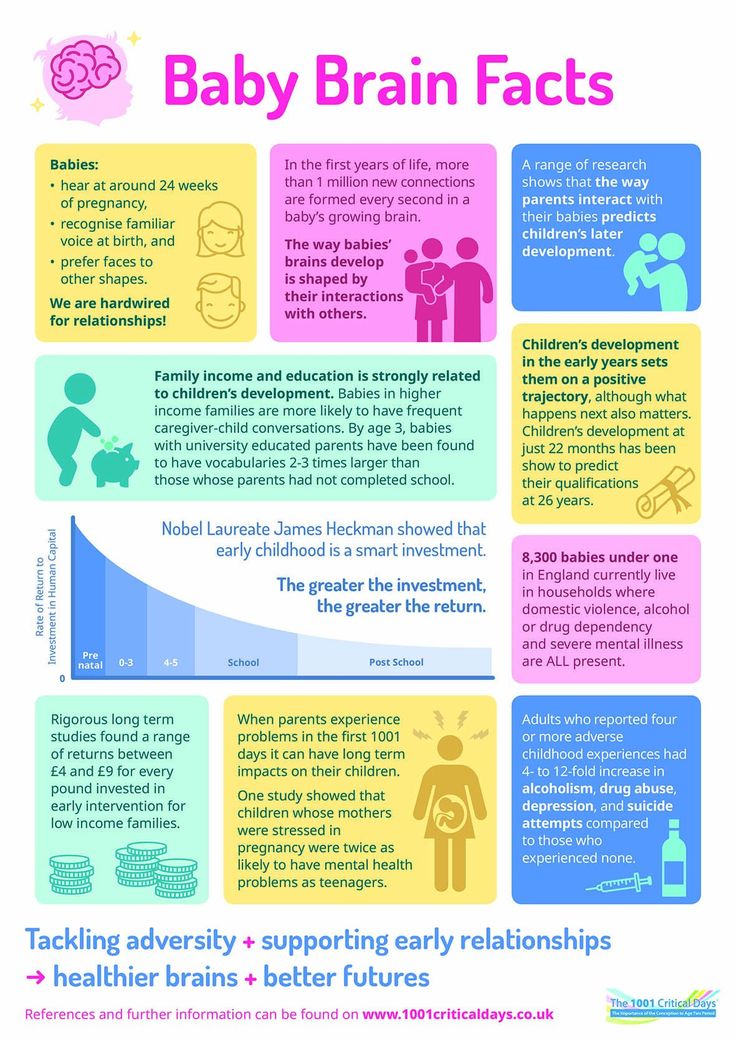
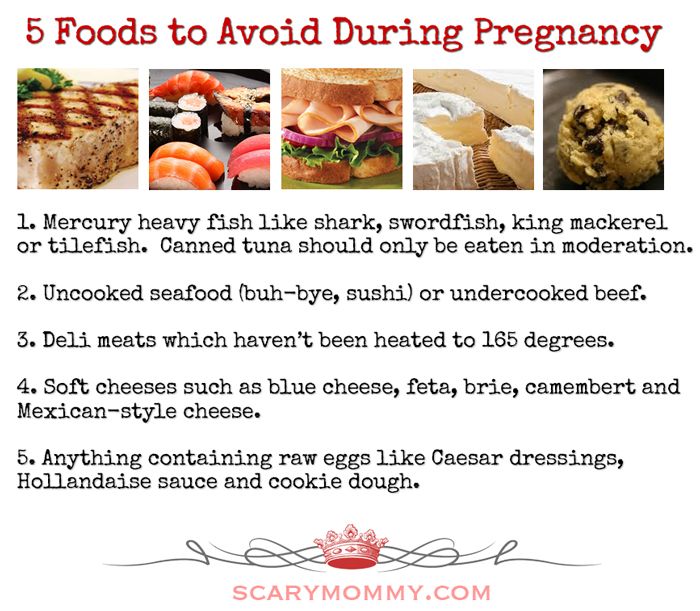
A 15-year-old primigravida was admitted at gestational age of 33 weeks and 3 days by ultrasound scan with complaint of intermittent lower abdominal pain with no per vaginal bleeding. Her prenatal care was done regularly in our hospital and the routine prenatal tests (hemoglobin level, syphilis, human immunodeficiency virus serologies, bacteriuria, glucosuria, and proteinuria by urine test strips) were unremarkable and she was of blood group O Rhesus positive. Her blood pressure was in normal range for her three visits. There was no history of urinary tract infection, preeclampsia, or diabetes. There was no reported drug or food allergy. Of note is that her pregnancy was the consequence of rape.
Her blood pressure was in normal range for her three visits. There was no history of urinary tract infection, preeclampsia, or diabetes. There was no reported drug or food allergy. Of note is that her pregnancy was the consequence of rape.
On admission, her general condition was normal, with a height of 143 cm and weight of 52 kgs.
She was afebrile, not pale with no general edema, having no jaundice and her blood pressure was 100/60 mmHg and her pulse rate was 82 bpm. The abdominal examination revealed a gravid uterus with fundal length of 28 cm, longitudinal lie, and cephalic presentation. Fetal heart rate was normal with uterine contractions. On pelvic examination, vulva and vagina were normal. The cervix was firm, posterior, and long admitting a tip of finger. Fingers were stained with whitish discharge. The diagnosis of threatened preterm labor and urinary tract infection was made and the patient was treated by tocolysis therapy with intravenous salbutamol 1,5 mg in 500 ml dextrose 5% at the rate of 7 drops per minute, intravenous ampicillin 1 g two times a day, and intramuscular diclofenac 75 mg two times a day.
Investigations found her hemoglobin at 10.5 g/dl, while on other laboratory examination, urinalysis and vaginal swab were unremarkable.
On day 3, she was improving with no lower abdominal pain and the tocolysis was stopped.
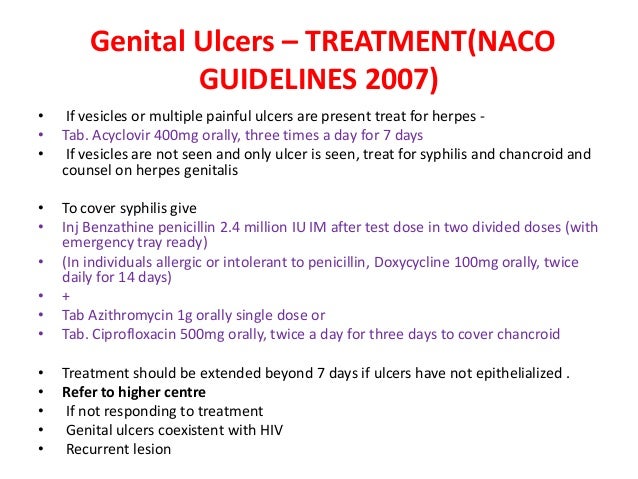
However, on day 4, she complained of vulvar edema. Her blood pressure was 110/80 mmHg, fetal heart rate in normal range with no palpable uterine contractions. On pelvic examination, the vulva was edematous and the diagnosis of vulvitis was suggested. Intravenous gentamycin 80 mg two times a day and oral metronidazole 500 mg three times a day were added on her treatment for 5 days, plus oral ibuprofen 400 mg two times a day as intramuscular diclofenac was already stopped.
On day 6, the swelling was getting worst despite the treatment and the patient had persistent vulvar pain with difficulty in ambulation and dysuria (Figure 1). Her vital signs were in normal range. Some laboratory tests were requested (the white blood cells were 4,400/mm3, the albuminuria was negative, and the random blood sugar was 82,4 mg/dl) and an obstetrical ultrasound scan revealed a single live, intrauterine fetus at 33 weeks and 6 days. The patient was then treated with intravenous ceftriaxone 1 g two times a day for 7 days, dexamethasone 12 mg once a day for 5 days, and diclofenac suppositories 100 mg two times a day for 3 days as she was in severe pain and ibuprofen was stopped. A urinary catheter was inserted with difficultly due to the edema, to allow easy drainage and the urine output was in the normal range (Figure 2).
The patient was then treated with intravenous ceftriaxone 1 g two times a day for 7 days, dexamethasone 12 mg once a day for 5 days, and diclofenac suppositories 100 mg two times a day for 3 days as she was in severe pain and ibuprofen was stopped. A urinary catheter was inserted with difficultly due to the edema, to allow easy drainage and the urine output was in the normal range (Figure 2).
Under the above treatment, she progressively improved and on day 10, the patient was doing well without swelling of the vulva (Figure 3) and the urinary catheter was removed. She was kept on ward until the onset of labor at term and for close monitoring.
She delivered at 39 weeks and 3 days by spontaneous vaginal delivery a live newborn boy, with weight of 2360 g and Apgar score of 9 at the first minute and 10 at the fifth minute.
3. Discussion
In this report we described a case of massive vulvar edema following tocolysis of preterm labor.
The vulvar edema is an extremely rare complication of pregnancy. In literature, cases of the massive vulvar edema have been described associated with multiple pregnancy, diabetes, hypoproteinemia, preeclampsia, tocolytic therapy, vulvovaginitis, and severe anemia [1–4]. But very rarely is the occurrence after tocolytic therapy. For this case, it is still a hypothesis that the edema might have occurred due to the salbutamol therapy. Other studies have shown the same [5, 7, 8]. However, there is a need for further studies to confirm and explain the mechanism behind tocolysis to get vulvar edema.
In literature, cases of the massive vulvar edema have been described associated with multiple pregnancy, diabetes, hypoproteinemia, preeclampsia, tocolytic therapy, vulvovaginitis, and severe anemia [1–4]. But very rarely is the occurrence after tocolytic therapy. For this case, it is still a hypothesis that the edema might have occurred due to the salbutamol therapy. Other studies have shown the same [5, 7, 8]. However, there is a need for further studies to confirm and explain the mechanism behind tocolysis to get vulvar edema.
With edema, one might have thought of hypoproteinaemia as the cause. But this was excluded clinically by the good general condition on admission, with good nutritional status without pedal, lower limb, or generalized edema.
There is no standard way of managing threatened preterm labor. The tocolysis protocol varies from a setting to another and due to the available drugs. Brittain et al. managed their patient with a combination tocolysis with intravenous ritodrine and magnesium sulfate; Trice L et al. used magnesium sulfate, nifedipine, and terbutaline and in a case report by Awwad JT et al., vulvar edema occurred in a twin gestation while on intravenous magnesium sulfate tocolysis. However our patient was managed with only salbutamol.
used magnesium sulfate, nifedipine, and terbutaline and in a case report by Awwad JT et al., vulvar edema occurred in a twin gestation while on intravenous magnesium sulfate tocolysis. However our patient was managed with only salbutamol.
As for the management, there is no standard way of managing this condition, as there were only few cases reported in the literature [5, 7, 8]. Some manage surgically by incision and drainage or puncturing the edema or by mechanical drainage [9, 10], while others prefer conservative management [11]. Moreover, it is important to find the cause, as management is best influenced by the cause of edema [2]. Some authors report that in most cases, vulvar edema resolves spontaneously after delivery [1]. For this particular case, since patients with vulvar edema might be considered as at high risk, close monitoring was instituted as stipulated by other authors [12], and this could explain the reason that we kept our patient until the delivery. Also, since the diagnosis of threatened preterm labor and urinary tract infection was the first impression diagnosis on admission, the patient was managed by tocolysis (intravenous salbutamol according to our local protocol) and antibiotics (Intravenous ampicillin) as the laboratory tests were going on.
A trial of triple intravenous antibiotics and local skin care proved ineffective in a study by Brittain et al. 1991. But our patient was only managed on the triple antibiotics, corticoids, and analgesics.
Finally, there is no fatality in most reported cases of vulvar edema after tocolysis. Trice L et al., 1996, reported two cases of tocolysis-induced vulvar edema with no fatality and resolved after repositioning the patient in one case and after cesarean section in the other.
4. Conclusion
Treatment of vulvar edema is necessary, since it may be alarming to the patient, painful, and uncomfortable and may cause occlusion of the vulva openings. The patient with vulvar edema merits special attention, identification, and treatment of the associated factors is vital to its management.
Consent
An informed consent was obtained from the patient for this publication.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
O. O. Owa, A. A. Aderoba, and A. L. Akintan, “Spontaneous massive vulva swelling in pregnancy: a case report,” Tropical Journal of Obstetrics and Gynaecology, vol. 32, no. 2, pp. 157–160, 2015.
View at:
Google Scholar
A. N. Massinde, N. Ngwalida, and B. Gumodoka, “Massive vulval oedema in multiple pregnancies at Bugando Medical Centre: Case reports,” Tanzania Journal of Health Research, vol. 13, no. 2, 2011.
View at:
Google Scholar
H. El Fazazi, Y. Benabdejlil, M. Achenani et al., “Isolated massive vulval edema in pregnancy: A case report,” International Journal of Innovation and Applied Studies, vol. 7, no. 2, p. 631, 2014.
View at:
Google Scholar
P. K. Saha, “Massive vulval edema in pregnancy,” The Internet Journal of Gynecology and Obstetrics, vol.
 6, no. 2, 2007.
6, no. 2, 2007.View at:
Google Scholar
J. T. Awwad, A. M. Khalil, N. K. Aswad, F. J. Suidan, and K. S. Karam, “Labial edema in pregnancy: A case report,” Journal of Reproductive Medicine, vol. 39, no. 11, pp. 921-922, 1994.
View at:
Google Scholar
S. Bergström, “Vulvar oedema among pregnant mozambican women,” Gynecologic and Obstetric Investigation, vol. 34, no. 2, pp. 73–75, 1992.
View at:
Publisher Site | Google Scholar
C. Brittain, J. W. Carlson, D. L. Gehlbach, and A. W. Robertson, “A case report of massive vulvar edema during tocolysis for preterm labor,” American Journal of Obstetrics & Gynecology, vol. 165, no. 2, pp. 420–422, 1991.
View at:
Publisher Site | Google Scholar
L.
 Trice, H. Bennert, and P. G. Stubblefield, “Massive vulvar edema complicating tocolysis in a patient with twins. A case report,” The Journal of Reproductive Medicine, vol. 41, no. 2, pp. 121–124, 1996.
Trice, H. Bennert, and P. G. Stubblefield, “Massive vulvar edema complicating tocolysis in a patient with twins. A case report,” The Journal of Reproductive Medicine, vol. 41, no. 2, pp. 121–124, 1996.View at:
Google Scholar
T. Radomański, R. Sikorski, and E. Baszak, “Vulvar edema in pregnancy,” Ginekologia Polska, vol. 69, no. 12, pp. 1067–1070, 1998.
View at:
Google Scholar
O. Deren, I. Bildirici, and A. Al, “Massive vulvar edema complicating a diabetic pregnancy,” European Journal of Obstetrics & Gynecology and Reproductive Biology, vol. 93, no. 2, pp. 209–211, 2000.
View at:
Publisher Site | Google Scholar
J. S. Lindsey and J. E. DeVente, “Surgical Management of Massive Labial Edema in a Gravid Preeclamptic Diabetic,” Case Reports in Obstetrics and Gynecology, 2014.

View at:
Google Scholar
A. Daponte, H. Skentou, K. D. Dimopoulos, A. Kallitsaris, and I. E. Messinis, “Massive vulvar edema in a woman with preeclampsia: a case report,” Obstetrics, Gynaecology and Reproductive Medicine, vol. 52, no. 11, pp. 1067–1069, 2007.
View at:
Google Scholar
Copyright
Copyright © 2018 Olivier Mulisya et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
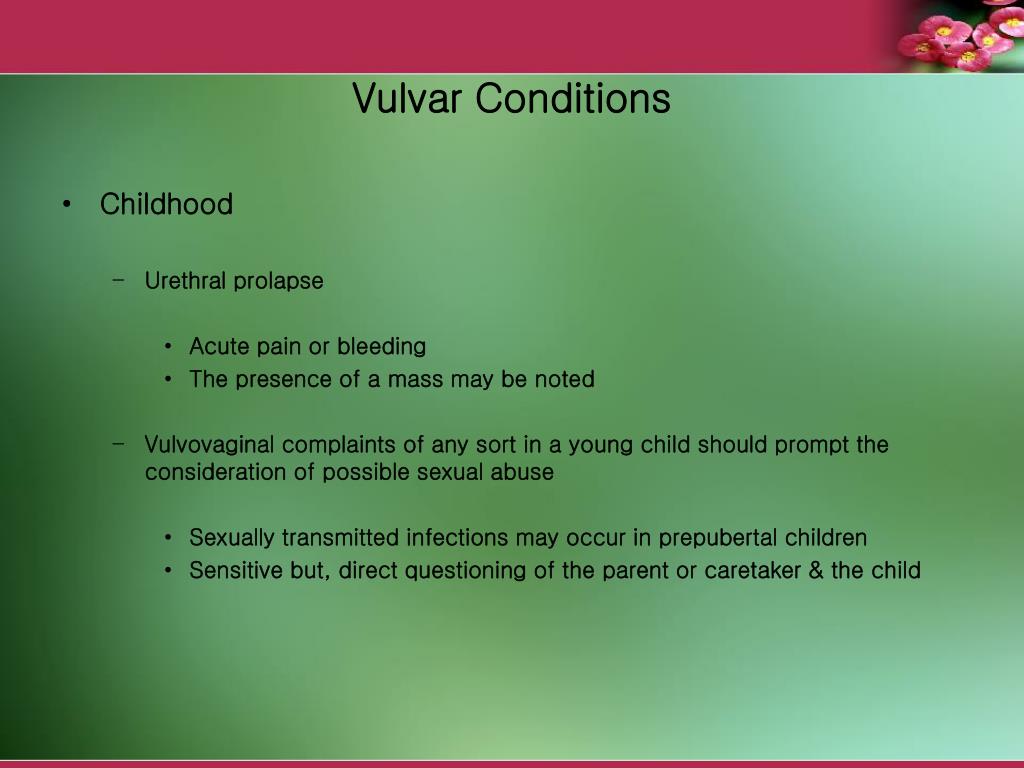
Neoplasms of the vulva - description, causes, symptoms, diagnosis and treatment
Neoplasms of the vulva - tumors of a benign and malignant nature in the area of the external female genital organs. A tumor occurs when the process of cell differentiation is disturbed. A healthy immune system identifies these cells and destroys them. With a weakened immune system, they begin to grow and multiply, not obeying the body.
A healthy immune system identifies these cells and destroys them. With a weakened immune system, they begin to grow and multiply, not obeying the body.
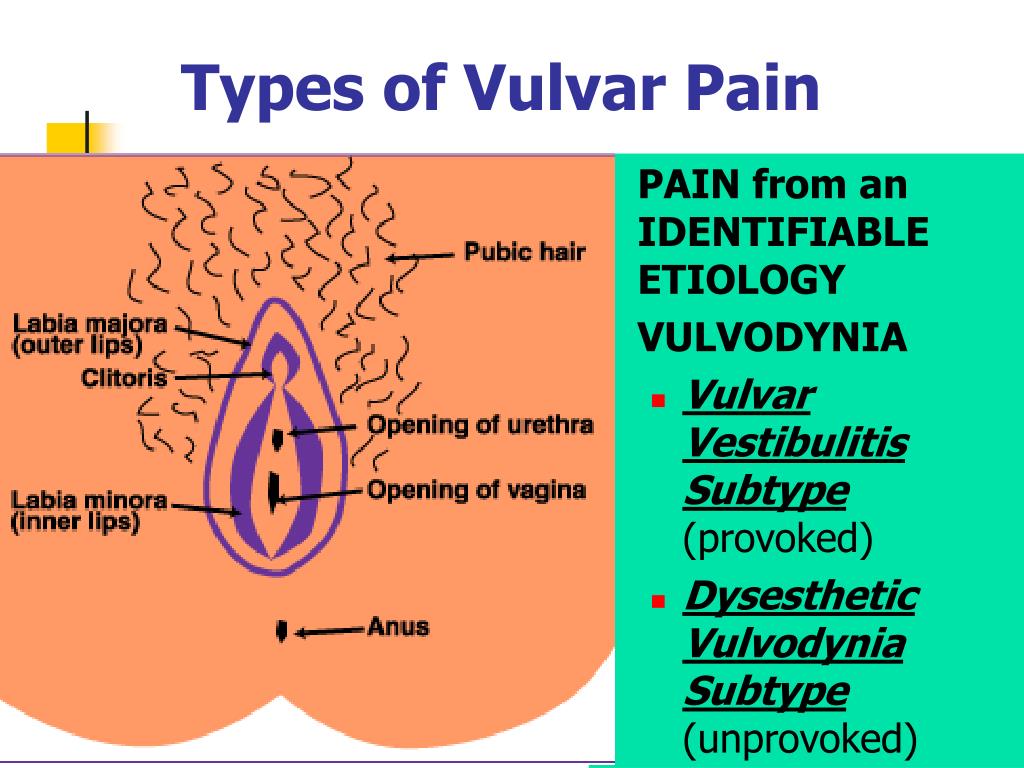
The vulva includes:
- pubic area;
- clitoris area;
- labia vulva and labia minora;
- entrance to the vagina.
Tumors of the vulva can spread:
- Posteriorly to the perineum, posterior labial commissure, rectum.
- Anteriorly - on the opening of the urethra, bladder.
- Up to the vagina, cervix, uterus. The boundary between the external and internal genital organs in girls is the hymen.
The function of the vulva is to participate in sexual intercourse. With tactile stimulation of the receptors of the vulva, the production of a secret that moisturizes the entrance to the vagina is stimulated.
Symptoms of neoplasms of the vulva
If a tumor process develops in the vulva, a woman may experience the following symptoms:
- pain;
- foreign body sensation;
- discomfort when moving, walking, during sexual intercourse;
- discharge with impurities of blood, pus;
- menstrual disorders;
- general weakness, temperature;
- enlarged inguinal lymph nodes;
- urination disorders - frequent painful urges, pathological impurities in the urine;
- pain in the perineum, defecation disorders.

It is desirable to detect the disease as early as possible. This will facilitate the treatment process, relieve unpleasant symptoms, and reduce the risk of complications. Therefore, at the first suspicious sensations from the reproductive system, it is necessary to consult a gynecologist.
Complications of vulvar tumors include:
- Anemia due to chronic blood loss.
- Problems with conception.
- Refusal of sexual activity due to pain on contact with the tissues of the external female genital organs.
- Degeneration of a benign tumor into a malignant one.
- Compression of neighboring organs - urethra, bladder, rectum.
Diagnosis
A woman is examined by a doctor in a gynecological chair. Assesses the size, shape, symmetry, color of the external genital organs, then proceeds to the examination of the vagina, cervix. Tumors of small sizes in the depth of tissues may not be visible during examination.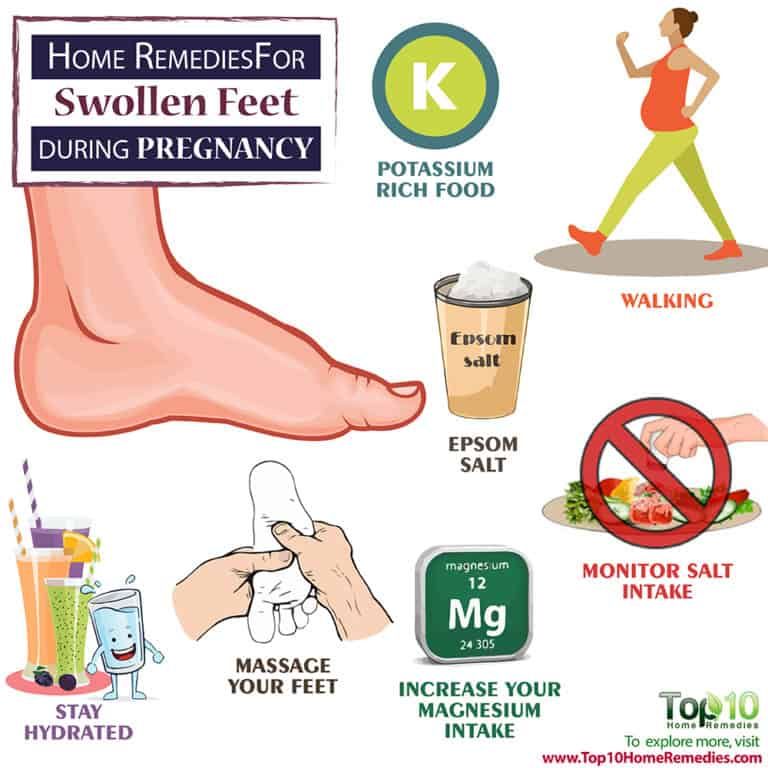 If they are from 1-2 cm, bulging of tissues in this place is noticeable. Skin color can be reddish, cyanotic, normal.
If they are from 1-2 cm, bulging of tissues in this place is noticeable. Skin color can be reddish, cyanotic, normal.
A colposcope is used for targeted examination. Applying a solution of acetic acid or toluidine blue to the skin of the external genital organs makes areas with neoplasms more visible against the background of healthy tissues.
Condylomas look like pointed dark pyramids, they are painless, soft to the touch, located one by one or in groups.
During palpation, the doctor specifies the consistency of the tumor (soft, dense), the boundaries, whether the focus is soldered to the surrounding tissues, pain. It also checks the regional lymph nodes. They can be enlarged, painful, dense.
They take smears for cytology, this will allow you to examine the tissues under a microscope and make an accurate diagnosis. Sometimes a piece of tissue is plucked from a suspicious area for histological examination.
To assess the condition of the internal genital organs, a vaginal examination, colposcopy, and transvaginal ultrasound are performed.
If necessary, additional research methods are prescribed:
- MRI, CT, X-ray of the pelvic organs.
- General analysis of blood, urine, biochemical study.
Due to the fact that the female genital organs are located near the rectum and bladder, with tumors of the vulva, the process often extends to neighboring organs. There may be disorders of urination, defecation, false and painful urges, pain in the perineum. To examine the bladder appoint:
- general and special urine tests;
- ultrasound;
- x-ray with contrast;
- endoscopic examination of the bladder.
To examine the intestine in detail, a woman is prescribed:
- Sigmoidoscopy - examination of the mucous membrane with an optical instrument.
- Proctologist's consultation, digital examination.
- X-ray with contrast.
Lymph nodes are assessed by ultrasound, MRI, CT, palpation. The PET scan method is good at detecting metastases. To detect metastases in the breast, it is enough to do a contrast mammogram.
To detect metastases in the breast, it is enough to do a contrast mammogram.
Types of benign diseases of the vulva
Benign tumors are neoplasms that are not aggressive towards neighboring cells and tissues. They grow by pushing away healthy tissues rather than invading them. They do not metastasize, do not affect the lymphatic system and other organs, do not spread throughout the body. The cells that make up a benign tumor do not differ much from normal ones.
However, this does not mean that they can be ignored and that they are not dangerous at all. Tumors can compress neighboring cells, cause ischemia, inflammation, and tissue necrosis. Some types of tumors can degenerate into malignant ones, so they need to be removed in a timely manner.
If the neoplasm does not cause discomfort, is found by chance during examination, is small, slowly growing, and is monitored. If active growth begins, symptoms appear that interfere with the woman, it must be removed surgically.
Depending on what cells the tumor consists of, all benign neoplasms of the vulva are subdivided:
- Myoma - it develops from muscle tissue. If from smooth muscles, it is called leiomyoma, if from striated - rhabdomyoma. The tumor is similar to a mobile dense ball, it is more often found on the surface of the labia majora.
- Fibroma - consists of connective tissue fibers. The tumor is elastic to the touch, with clear contours, may have a stalk or is located in the depths of the tissues. The most common localization is the labia majora, the entrance to the vagina.
- Condylomas, papillomas - superficial formations from the stratification of epithelial cells. They have the appearance of a tubercle, often with papillary outgrowths on the surface. Human papillomatosis viruses (HPV) play an important role in their development. They have a high risk of malignancy, especially if the process spreads to the internal genital organs of a woman. The color often differs from the surrounding tissues - brown or whitish.
 The condyloma has a wide base, the papilloma has a narrow stalk that connects the tumor to the organ. Single formations are possible, but more often - multiple. They are located on the labia, at the entrance to the vagina, on the pubic area.
The condyloma has a wide base, the papilloma has a narrow stalk that connects the tumor to the organ. Single formations are possible, but more often - multiple. They are located on the labia, at the entrance to the vagina, on the pubic area. - Adenoma - consists of epithelial cells of the mucous membrane of the vulva.
- Angioma is a tumor of vascular tissue. There is a lymphangioma, it is soft, has a blue tint, consists of lymphatic vessels filled with fluid. A hemangioma is an overgrowth of small blood vessels. It can spread from the external genitalia into the vagina, to the cervix. Reddish or blue nodules protrude above the surface of the vulva, bleed heavily when injured.
- Lipoma, or wen. Not dangerous, soft to the touch, rounded. Found on the pubis, external labia.
- Myxoma - the formation has a capsule, inside it is filled with a yellowish liquid.
- Tumors from mixed tissues - fibrolipoma, fibromyoma (incorporates modified cells of connective and muscle tissue).
- Hydroadenoma - from the sweat glands in the vulva. Nodules are small, multiple, usually brown, pink or yellow. They are found on the pubis and in the area of the labia, often located symmetrically.
- Bartholin gland cyst - located in one of the labia, filled with fluid, painless.
Features of the treatment of benign tumors
Whether it is necessary to remove a benign tumor, the doctor decides. It depends on the age of the woman, the growth rate and type of tumor, the severity of symptoms. If you need to remove the formation, it is done within healthy tissues:
- If the tumor is on the leg, it is cut.
- If the skin or mucous membrane is cut deep in the tissues, the tumor is bluntly excised, the bleeding is stopped, the tissues are sutured.
After the operation, it is necessary to observe, change dressings with antiseptic ointments and solutions. Locally prescribed drugs that speed up healing. Sometimes oral or injectable antibiotics.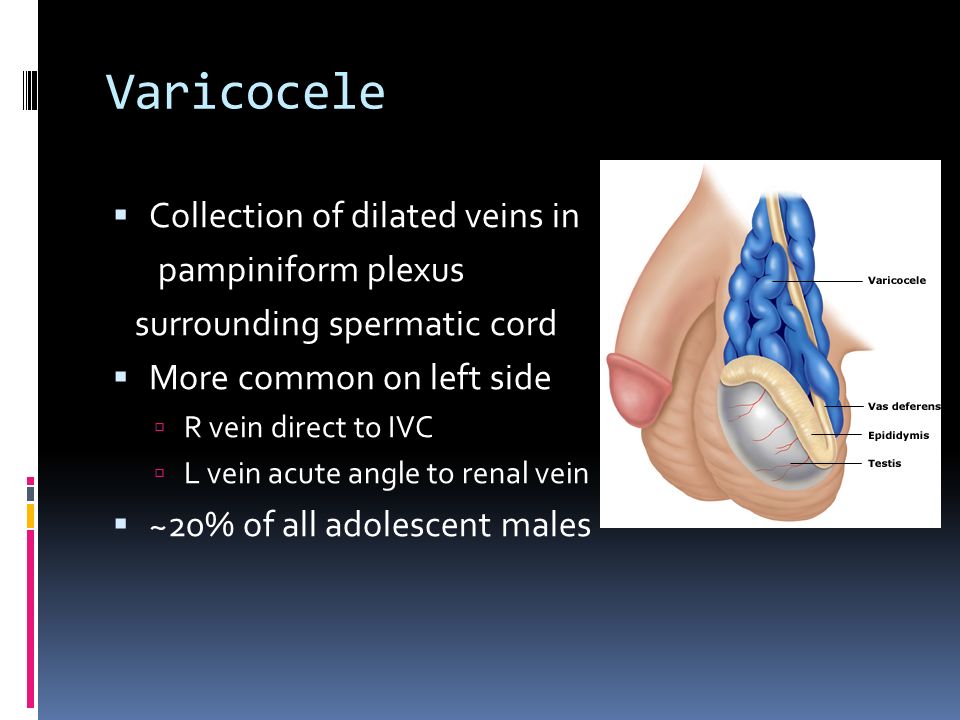
To remove superficial benign formations, not only a scalpel is used, but also more gentle methods:
- Cryodestruction - under the action of nitrogen, tumor cells are frozen, they die. The operation is used for warts, does not require anesthesia. It is easily tolerated by women.
- Radio wave therapy involves the separation of tissues by a directed stream of low frequency radio waves. The procedure does not cause pain, is not accompanied by bleeding. The tissues heal almost without scarring. The rehabilitation period is minimal, as is the risk of complications.
- Laser removal of neoplasms is also characterized by respect for healthy tissues. The condyloma cells are evaporated due to the high temperature that is created by the directed beam of light.
- Electrocoagulation - a more rough method, the tumor is affected by an electric current. Subsequently, a scar may remain in the treatment area, deforming the vulva.
- Plasma coagulation - evaporation of a tumor by exposure to a plasma discharge.
 As a rule, the scars are small, and the woman does not experience pain.
As a rule, the scars are small, and the woman does not experience pain. - Cauterization with chemically active substances, such as acids, solcoderm. The most commonly used nitric acid, it causes coagulation of tumor cells. There is no need to anesthetize, the tissues heal well without large scars.
- Sclerotherapy is used in the treatment of hemangiomas - a substance is introduced into the vessels, leading to tissue sclerosis, gluing and emptying of the vessels.
All these methods can be used if there are no signs of inflammation, malignancy in the tumor growth zone, the woman does not have a herpes infection of the genital organs, problems with blood clotting. After removal, the tissue is sent for histological examination. If at the same time malignant cells are detected, the treatment will be supplemented with chemotherapy or radiation exposure.
Papillomas tend to recur. Therefore, after surgical removal, it is necessary to undergo a course of antiviral treatment.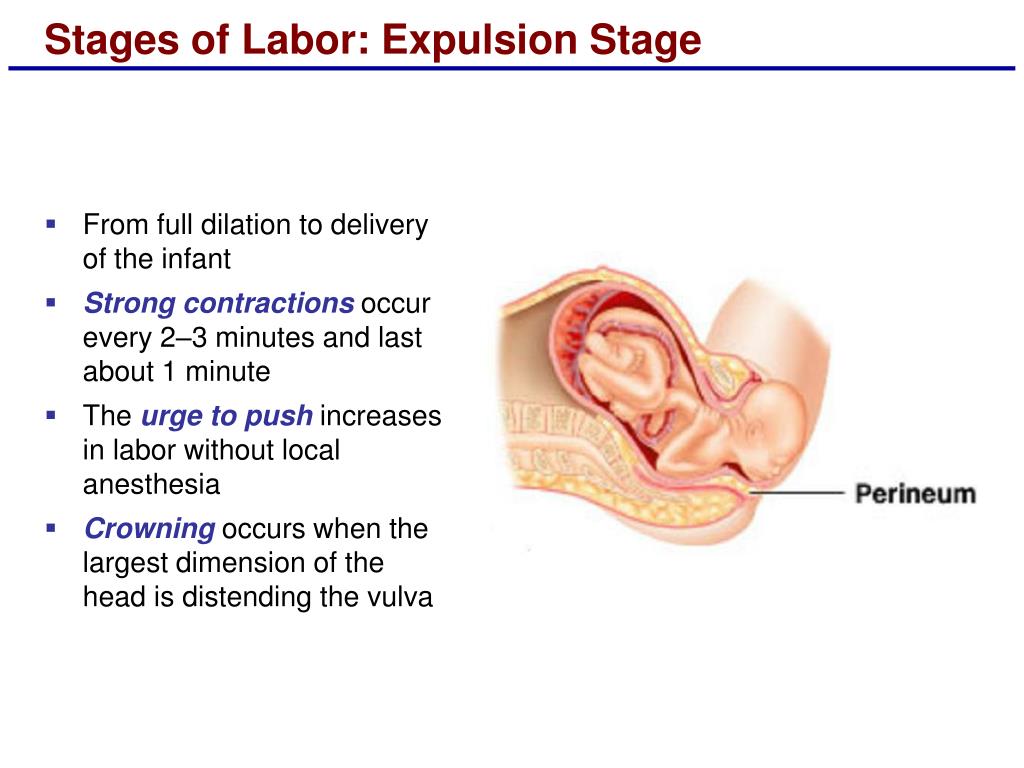
Types of malignant neoplasms of the vulva
Malignant diseases are more dangerous, but they can also be successfully cured if detected in the early stages. About 80% of all cases of vulvar cancer are diagnosed in women over 55 years of age. Types of malignant tumors of the external genital organs:
- Squamous cell carcinoma (90% of all cancers) is a malignant formation from epithelial cells. Often it is found in the thickness of the labia majora. At the same time, the woman complains of a feeling of a foreign body, irregular discharge with blood impurities. Burning, itching, pain are possible. The skin in the area of education changes color to red or cyanotic, there are ulcers, seals. Ulcers do not heal for a long time, have an unpleasant odor, bleeding occurs upon contact. Carcinoma is often preceded by a benign papilloma that grows from sweat or Bartholin gland cells.
- Melanoma - consists of pigment cells. Alertness should arise if the mole began to grow rapidly, its color and shape changed, redness appeared around it, swelling of the skin, itching, pain.
- Less common are sarcoma, Paget's cancer, basal cell carcinoma, adenocarcinoma.
How to treat malignant tumors?
The main methods of treatment of malignant neoplasms:
- Surgical - remove the focus and adjacent tissues so that no tumor cells remain in the body. If the lymph nodes are affected, they are also removed along with fiber. In the presence of metastases in other organs, the volume of the operation increases even more. Therefore, everyone is interested in identifying the disease at the earliest possible stages.
- Chemotherapy - prescribe cytostatics that inhibit the growth and division of cells in tumors. Often it is prescribed before or after surgery, which allows you to reduce the primary focus and reduce the risk of relapse.
- Radiation therapy - irradiation of tumor growth zones inhibits the development of a neoplasm, facilitates its surgical removal.
Depending on the histological structure of the tumor, these methods are combined to achieve the best effect.
In the development of malignant tumors of the external female genital organs, 4 stages are conventionally distinguished. This is necessary for choosing a treatment regimen:
- Precancer is a disease that often turns into a malignant tumor. Precancerous diseases include papilloma, genital warts (cause HPV), leukoplakia (increased keratinization of the epidermis), vulvar kraurosis (sclerosis and deformity, atrophic changes in the external female genital organs), intraepithelial neoplasia.
- The first is a focus up to 2 cm, located within the same anatomical zone.
- Second - the tumor captures more than 2 cm, but does not extend beyond the vulva.
- The third is characterized by spread to the lymph nodes, nearby organs - anus, urethra, vagina.
- Fourth - distant organs are involved in the tumor process, such as bones, liver, lungs, brain. Metastases can be indicated by bone pain, exhaustion, rapid weight loss, and an unhealthy skin tone.
In the early stages, it is possible to perform organ-preserving operations, while maintaining the appearance and shape of the vulva. If the tumor has invaded more tissue, part or all of the vulva may need to be removed. In such cases, a woman may be offered a reconstructive operation, after which the external genitalia will be formed from other soft tissues of the patient. This will allow her to lead a normal sex life, not to feel psychological discomfort.
If distant organs are affected, surgery may not always be possible. In advanced cases, palliative treatment is prescribed to alleviate the suffering of a woman. For pain, analgesics are prescribed orally or by injection. If the tumor spreads to the urethra, a urologist is involved in the operations, the rectum - a proctologist.
Measures to prevent vulvar neoplasms
It is not possible to prevent 100% of vulvar neoplasms. However, if you follow a number of rules, you can reduce the risk of developing a tumor:
- Treat acute and chronic diseases of the female reproductive system.
 Trichomonas, chlamydia, the causative agent of gonorrhea, fungi of the genus Candida, the herpes virus cause vulvitis, vulvovaginitis. Despite the chronic course, complaints may be practically absent. Without treatment, fibrotic changes in organs increase, their shape and function are disturbed, and local immunity is weakened.
Trichomonas, chlamydia, the causative agent of gonorrhea, fungi of the genus Candida, the herpes virus cause vulvitis, vulvovaginitis. Despite the chronic course, complaints may be practically absent. Without treatment, fibrotic changes in organs increase, their shape and function are disturbed, and local immunity is weakened. - Have sex with one partner. If you do not want to become pregnant, you need to use contraceptive methods so as not to resort to abortion.
- Visit a gynecologist once a year for preventive purposes. Even in the absence of symptoms, a tumor may be detected.
- A mobile lifestyle, walking, exercises will reduce the stagnation of blood in the small pelvis.
- HPV infection can be prevented by using a vaccine, contact methods of contraception, limiting the number of sexual partners. HIV weakens the body's immune defenses. Against the background of this disease, HPV infection occurs more easily. The virus penetrates into the cell nucleus, leads to changes in the genetic apparatus, causes the reproduction of atypical mutated cells.
 Thus, HPV leads to the development of not only vulvar cancer, but also cervical cancer, one of the most common pathologies in women.
Thus, HPV leads to the development of not only vulvar cancer, but also cervical cancer, one of the most common pathologies in women. - Refusal of bad habits - overeating, smoking, alcohol, sweets.
- Genital hygiene.
- Injury to the vulva should be avoided. More often this happens during rapid childbirth, during sports, during falls, during intimate relationships.
You can have an examination by a gynecologist at our clinic. Admission is by appointment. On the spot, you can pass all the necessary tests, do ultrasound, x-rays and apply other imaging methods. The older the woman, the higher the risk of developing cancer.
Experienced doctors will help to identify the beginning problem in time. The staff is attentive to each patient. Treatment can be obtained in full, including surgery, if necessary, chemotherapy, radiation. The clinic widely uses sparing methods of treatment. After them, the recovery of a woman is faster, pain is not bothered. Whenever possible, organ-sparing operations are always chosen.
Whenever possible, organ-sparing operations are always chosen.
Author
Radlevich Natalya Vadimovna
obstetrician-gynecologist, ultrasound diagnostics
Doctor of the highest category, candidate of medical sciences
Experience 25 years
+7 (495) 032-15-21
COLPITIS IN PREGNANCY
During pregnancy, a woman, as a rule, takes special care of her health and reacts anxiously to every unusual symptom.
Unusual discharge and discomfort in the genital area are often the cause of the expectant mother's panic. Such a complex of symptoms most likely indicates the development of a pathological process, which in medicine is called vaginitis or colpitis. In pregnant women, this condition is noted especially often against the background of a decrease in immunity, hormonal changes in the body and high loads on all organs and systems of a woman.
Vaginitis during pregnancy is a good reason to immediately contact a gynecologist and start treating this dangerous pathology. Diagnose the disease and determine how to treat colpitis during pregnancy without harming the mother and baby, qualified gynecologists will prompt.
Symptoms of colpitis during pregnancy
First of all, it should be determined that vaginitis or colpitis is an inflammatory disease that involves the mucous membranes of the vagina. The inflamed walls of the vagina swell and undergo hyperemia. Also, single hemorrhages are noted on the surface of the vaginal tissues. If the inflammation does not spread beyond the vagina, the woman does not notice visual manifestations of the disease, while in some cases the pathological process affects the external genitalia. In this case, inflammation can be seen with the naked eye.
The characteristic signs of colpitis during pregnancy do not differ from the symptoms of a non-pregnant woman:
- itching and burning in the vaginal area - the inflammatory process irritates the delicate mucous membranes, which causes discomfort and sometimes pain in the vaginal walls;
- pain in the lower abdomen - this symptom is especially frightening for pregnant women, but it is not associated with uterine tone, as many assume, but with tissue inflammation;
- the appearance of specific discharge - the discharge during colpitis during pregnancy is very abundant and may have a different color and consistency. Most often, a woman visually notes a white curdled discharge, resembling a characteristic sign of thrush, but sometimes the vaginal discharge acquires a putrid odor and is greenish-yellow in color. This indicates the specific nature of the pathogen and requires immediate medical advice;
Most often, a woman visually notes a white curdled discharge, resembling a characteristic sign of thrush, but sometimes the vaginal discharge acquires a putrid odor and is greenish-yellow in color. This indicates the specific nature of the pathogen and requires immediate medical advice;
- swelling and redness of the genital organs - patients often notice hyperemia and swelling of the labia and clitoris, which become more sensitive and cause discomfort to the woman.
Acute vaginitis during pregnancy is accompanied by severe symptoms, which should make the patient seek professional help. This will help protect the child from possible negative consequences.
Causes and types of vaginitis during pregnancy
Inflammation of the mucous membranes of the vagina is usually of an infectious nature. This becomes possible due to vaginal dysbacteriosis, which often accompanies the period of pregnancy. Hormonal changes and high loads on all organs of the expectant mother cause a decrease in the body's defenses, which provokes an infectious and inflammatory process.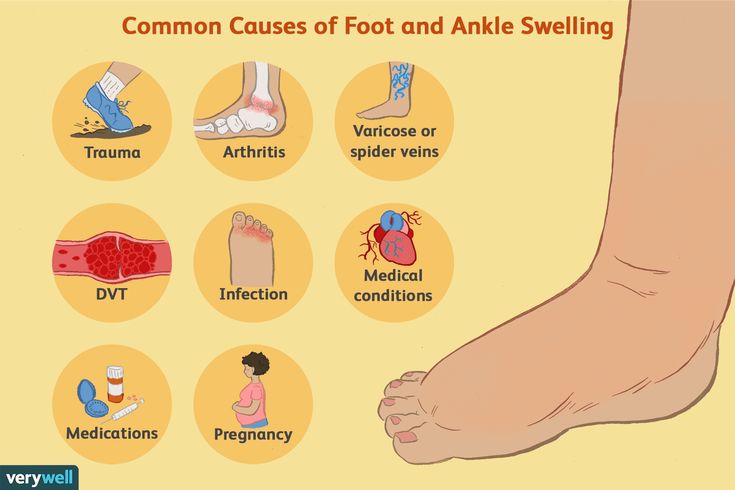 In this case, the causative agent of the pathology can act as a bacterial flora that has penetrated into the body from the outside during sexual intercourse or in the household way, and that makes up the normal microflora of the vagina. The most likely infectious agents of colpitis in pregnant women include streptococci, fungi of the genus Candida, E. coli, trichomonas, ureaplasma, mycoplasma, etc.
In this case, the causative agent of the pathology can act as a bacterial flora that has penetrated into the body from the outside during sexual intercourse or in the household way, and that makes up the normal microflora of the vagina. The most likely infectious agents of colpitis in pregnant women include streptococci, fungi of the genus Candida, E. coli, trichomonas, ureaplasma, mycoplasma, etc.
It is interesting that depending on the cause of the development of the disease, its symptoms and manifestations may differ:
- candidal colpitis - accompanied by abundant cheesy discharge and severe itching of the genital organs, which manifests itself even at rest;
- emphysematous colpitis - a very common type of vaginitis in pregnant women. Pathology is accompanied by the formation of small watery vesicles on the surface of the mucous membranes of the genital organs. This form of colpitis resolves on its own in 2-3 weeks after childbirth;
- Trichomonas colpitis is a very dangerous form of pathology that develops when Trichomonas enters the vaginal environment. Infection occurs during intercourse or when using personal hygiene items shared with the carrier (towel, washcloth, etc.). It is manifested by characteristic putrefactive secretions with a sharp unpleasant odor.
Infection occurs during intercourse or when using personal hygiene items shared with the carrier (towel, washcloth, etc.). It is manifested by characteristic putrefactive secretions with a sharp unpleasant odor.
Concomitant conditions for the development of colpitis in a pregnant woman, in addition to a decrease in immunity, may be allergic reactions, microtrauma of the vagina, non-observance of personal hygiene, the presence of chronic diseases.
Colpitis during pregnancy: consequences for the child
Inflammation of the mucous membranes of the vagina poses a threat not only to the health of the expectant mother, but also to the baby. The ascending route of infection can lead to pregnancy abnormalities such as polyhydramnios, premature birth, and infection of the amniotic fluid. Vaginitis is especially dangerous during childbirth, when the baby passes through an infected maternal birth canal. At at this moment there is a high probability of infection newborn.
Interestingly, colpitis after pregnancy can go away on its own, but this happens relatively rarely. The development of colpitis after childbirth is most often provoked by trauma to the vaginal membranes during delivery. In connection with this fact, doctors recommend abstaining from sexual activity for the first weeks after childbirth. Violating this prohibition, a woman increases the risk of developing colpitis after childbirth.
Treatment of colpitis during pregnancy
Diagnosis of the disease involves a standard gynecological examination and colposcopy. This research method makes it possible to visualize the surface of the mucous membrane of the walls of the vagina and assess their condition. During the examination, the doctor takes a smear for analysis. The study of biological material is carried out by bacterioscopic and bacteriological methods.
Treatment of colpitis in pregnant women requires a rational approach to prescribing antibiotics.