Different kinds of rashes in babies
Baby Rash: Causes, Types, Treatments, Prevention
There are many types of rashes that affect various parts of a baby’s body.
These rashes are typically very treatable. While they may be uncomfortable, they aren’t cause for alarm. Rashes are rarely an emergency.
Sometimes, infant rashes can indicate a more serious illness. We’ll discuss different types of baby rashes, how to treat them, and when to call a doctor.
Babies have very new skin and developing immune systems. Their skin is sensitive and susceptible to many sources of irritation or infection. Causes of rashes in babies include:
- heat
- allergies
- friction
- dampness
- chemicals
- fragrances
- fabrics
Even their own feces can irritate a baby’s skin and cause a rash. Viral and bacterial infections can also cause rashes.
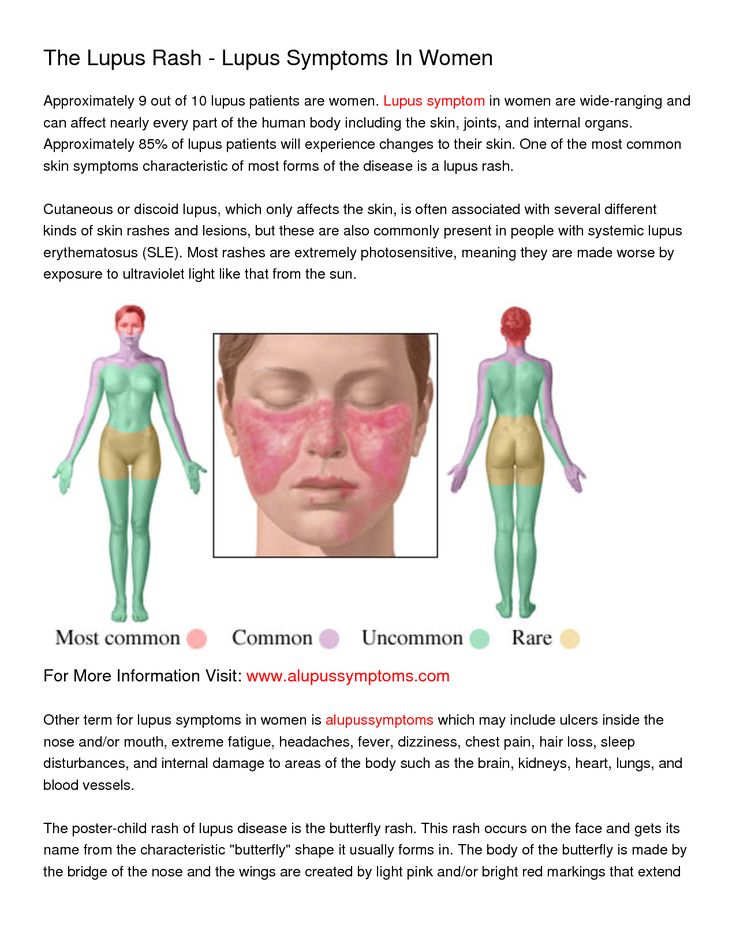
Depending on the cause of the rash, almost any part of your baby’s body can be affected:
- face
- neck
- trunk
- arms
- legs
- hands
- feet
- diaper area
- skin folds
Some of the most common types of infant skin rashes include:
- baby acne, which usually appears on the face
- cradle cap
- diaper rash, which is caused by wetness or the acidity of a baby’s urine and feces
- drool rash, which happens when drool irritates the skin around the mouth or on the chest
- eczema, most commonly found on the face, behind the knees, and on the arms
- fifth disease, which is a “slapped cheek” rash that may be accompanied by fever, fatigue, and sore throat
- hand, foot, and mouth disease
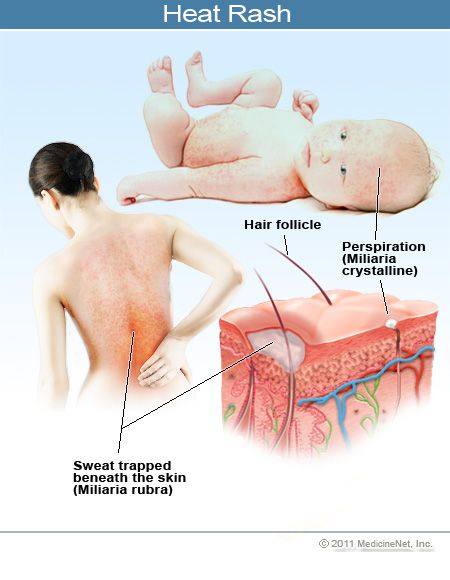
- heat rash, usually found in areas covered by clothes, such as armpits, neck, chest, arms, torso, and legs and is caused by overheating
- hives
- impetigo
- infectious rashes, such as measles, chickenpox, scarlet fever, and roseola
- miliamolluscum contagiosum
- thrush
Seek medical advice for a feverBring your child to a doctor if they’re experiencing a rash with a fever.
![]()
Diaper rash treatment
Diaper rash is one of the most common baby rashes. A diaper holds warmth and moisture close to the skin, and urine and feces may be acidic and very irritating to the skin. The best remedies for diaper rash include:
- frequent diaper changes
- wiping with a soft, wet cloth instead of pre-packaged wipes that contain alcohol and chemicals
- using a barrier cream, typically containing zinc oxide, which shouldn’t be wiped off of the skin with each diaper change or it can cause more irritation
- decreasing acidic foods, such as citrus and tomatoes, in your baby’s diet
- washing your hands before and after diaper changes so the rash doesn’t become infected
Eczema treatment
Eczema is another very common childhood rash. If you have a family history of eczema or sensitive skin, your baby is likely to be more prone to eczema.
It may be caused by allergies or skin sensitivities to food, laundry detergent, types of fabric, or other irritants. Helpful treatments for eczema include:
Helpful treatments for eczema include:
- keeping the area clean and dry
- over-the-counter creams and ointments
- oatmeal baths
- determining if there’s an allergy and eliminating the allergen
- working with a pediatric dermatologist to identify your baby’s triggers and how to best treat their eczema
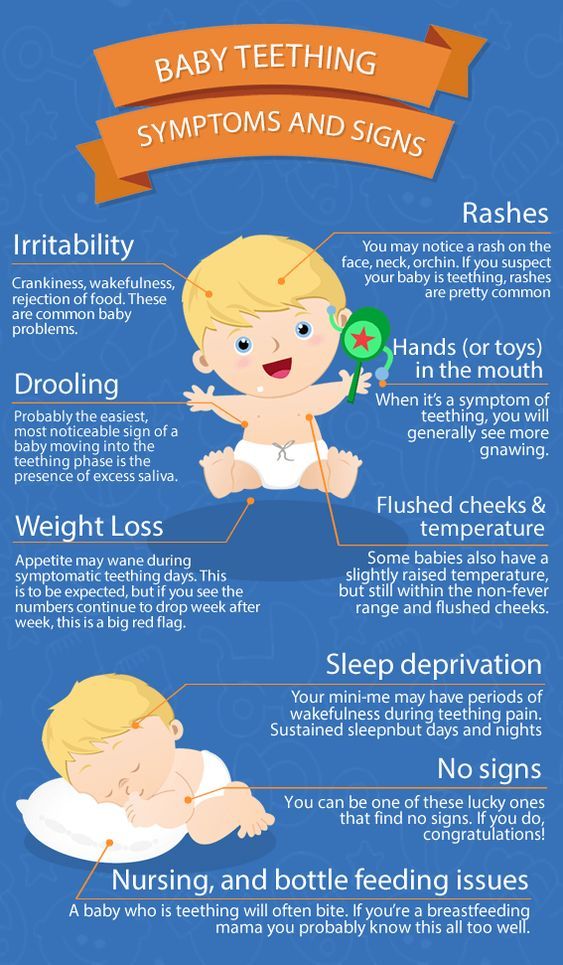
Drool rash treatment
Drool rash and general facial rash is very common in babies. They’re developing salivary glands and teething, so it’s not uncommon for them to have drool on their face much of the time. Pacifier use, food particles, teeth growing in, and frequent face-wiping may also irritate the skin.
Drool rash typically resolves on its own in a matter of weeks, but there are some ways to help:
- pat — don’t scrub — your baby’s face to dry
- clean with warm water but avoid using soap on the face
- have your baby wear a drool bib so their shirt doesn’t become soaked
- be gentle when cleaning food off of the face
- avoid fragranced lotions on the face
- minimize pacifier use when possible
Some rashes, such as baby acne, go away by themselves in a matter of weeks or months. You shouldn’t use adult acne medication to treat baby acne.
You shouldn’t use adult acne medication to treat baby acne.
Cradle cap can be treated with topical oil, such as coconut oil, gentle scrubbing with a cradle cap brush, and washing your baby’s head.
Infectious rashes such as thrush, measles, chickenpox, roseola, and scarlet fever should be evaluated by a pediatrician for the best treatment. These rashes are typically accompanied by a fever and other symptoms. They may require antibiotics or antiviral medication, or they may resolve on their own.
Fever
If your baby develops a rash accompanied by a fever or following a fever, it’s best to call your pediatrician. The cause may be infectious and you should have your child evaluated by a doctor.
Learn more about signs of fevers and low temperatures in babies, and what to do.
Rash for a week
If your baby has a rash that persists for more than a week, doesn’t respond to home remedies, or is causing your baby pain or irritation, you should call your doctor.
Rash spreads
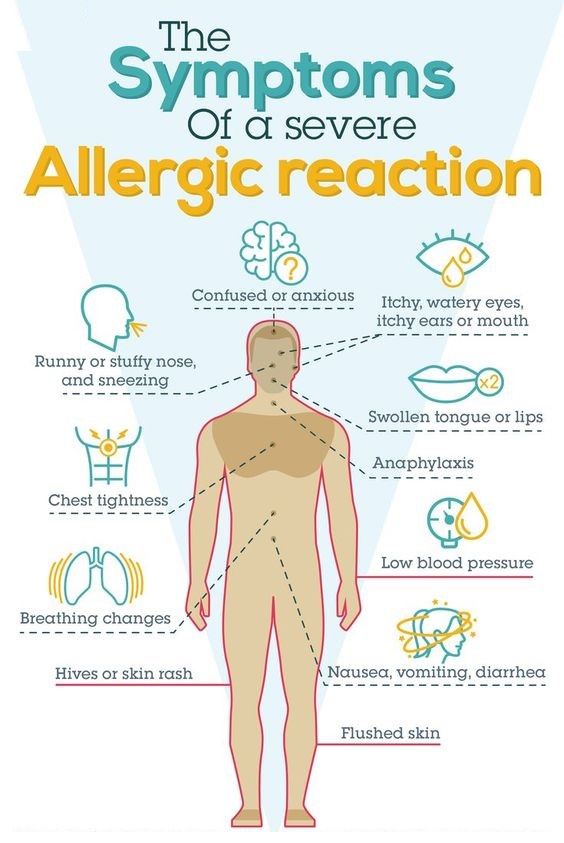
If your baby develops widespread hives, especially around the mouth, or develops hives accompanied by coughing, vomiting, wheezing, or other respiratory symptoms you should go to the emergency room. This may be a sign of a very serious allergic reaction called anaphylaxis.
Emergency signs
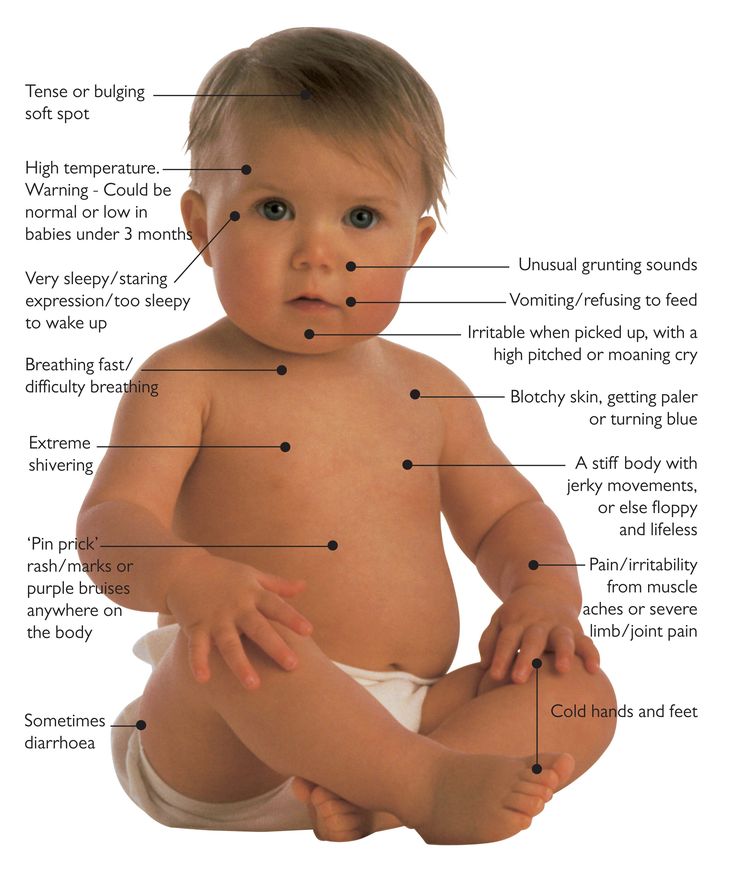
A rash accompanied by a very high fever, a stiff neck, sensitivity to light, neurological changes, or uncontrollable shaking may be caused by meningitis and is considered a medical emergency.
While rashes in babies are very common, there are some steps you can take to help prevent a rash. Preventive steps that some people try include:
- frequent diaper changes
- keeping skin clean and dry
- using irritant-free laundry detergent or detergent specially formulated for babies
- dressing your baby in breathable fabrics, such as cotton
- dressing your baby appropriately for the weather to avoid overheating
- keeping track of any skin reactions to foods so you can avoid trigger foods
- keeping your child up-to-date on vaccinations
- not letting strangers or anyone with symptoms of illness kiss your baby
- using lotions, shampoos, and soaps specifically designed for a baby’s sensitive skin
It can be alarming when your baby develops a rash, especially if they seem to be sick, itchy, or uncomfortable.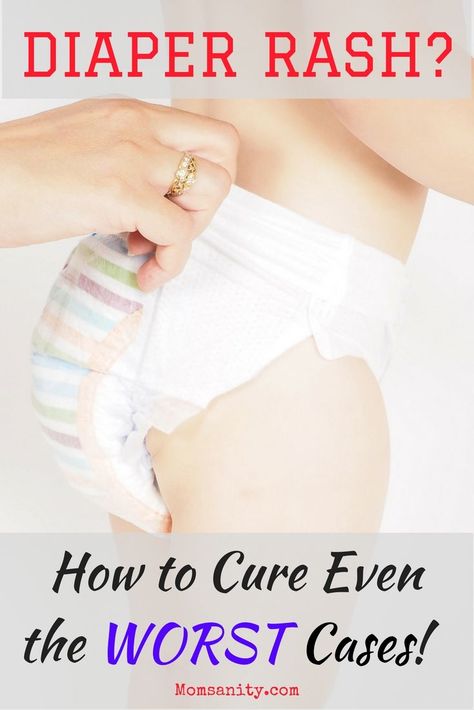 It can also be difficult to determine the cause of the rash.
It can also be difficult to determine the cause of the rash.
The good news is that rashes tend to be very treatable and aren’t usually serious. Many are even preventable and can be managed at home.
If you’re concerned about your child’s rash, or the rash is accompanied by a fever, call your pediatrician. They can help determine what is causing your baby’s rash and how to treat it.
17 Most Common Types of Baby Rashes (With Pictures)
Are small red bumps popping up on your baby’s body? There are many possible reasons for baby rashes, so it can be difficult to know what causes them.
Chances are, it’s something completely harmless that will resolve itself within a few days. But it’s still important to keep an eye on any rashes that pop up on your little one.
Our medical team will give you the lowdown on the 17 most common types of baby rashes to help you identify those bumps and set your mind at ease.
Table of Contents
- 1.
 Baby Acne
Baby Acne - 2. Cradle Cap
- 3. Erythema Toxicum Neonatorum (ETN)
- 4. Atopic Eczema
- 5. Hives
- 6. Diaper Rash
- 7. Milia
- 8. Impetigo
- 9. Fifth Disease
- 10. Hand, Foot, and Mouth Disease
- 11. Measles
- 12. Miliaria
- 13. Scabies
- 14. Ringworm
- 15. Meningitis
- 16. Chickenpox
- 17. Molluscum Contagiosum
- When to Worry About a Rash
- Make a Rash Decision
1. Baby Acne
This rash is nothing to worry about. Most babies have experienced it. It usually shows up within the first couple of weeks of a baby’s life and can last from several days to several months (1).
Causes
Doctors are still not entirely sure why some babies develop acne. But it may be caused by the maternal hormones your baby is exposed to in the womb.
Symptoms
Baby acne is distinguished by tiny red or white pimples on a baby’s cheeks, nose, forehead, and chin.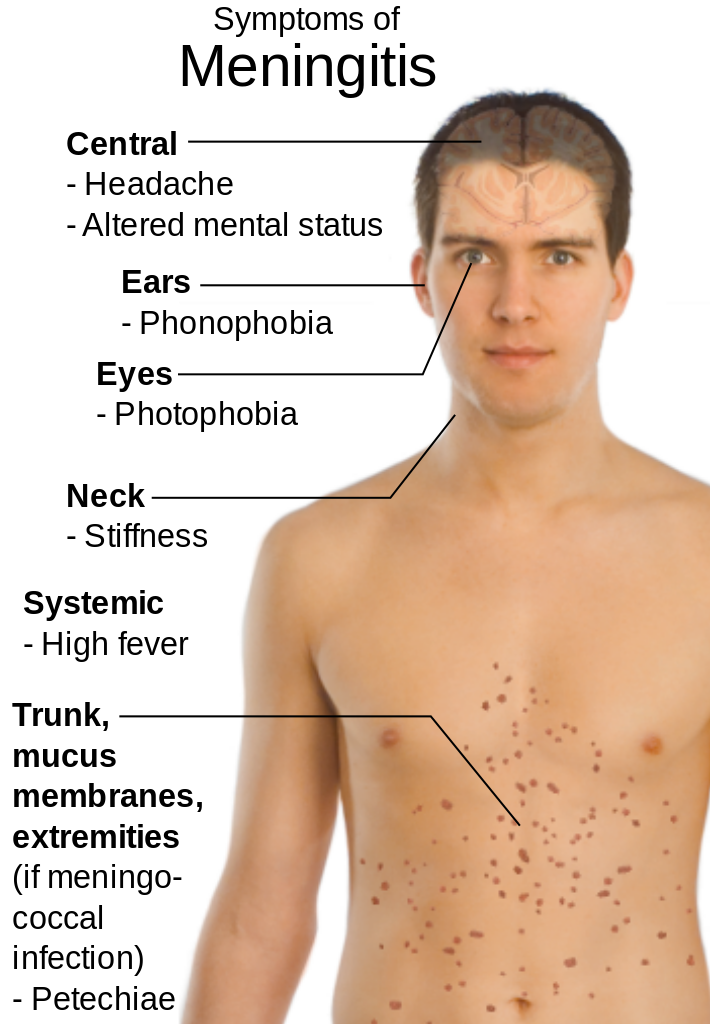 Basically, they look like a tiny teenager going through puberty.
Basically, they look like a tiny teenager going through puberty.
Treatment
The best way to get rid of baby pimples is to keep your baby’s skin clean. Gently wipe the area using soft materials like cotton balls or gentle washcloths.
Moisturizing the skin is essential, so try a mild baby lotion or baby oil. But don’t use too much since this could block the pores and worsen the acne. Most baby acne goes away on its own.
Your baby may need treatment for moderate to severe acne to prevent scarring. Never buy any over-the-counter acne treatment creams intended for teens or adults. These are not safe for newborns. Consult your pediatrician to find the appropriate treatment for the baby acne.
If the acne does not go away on its own, or if it worsens despite treatment, talk to your doctor immediately. Your baby may have a hormonal imbalance issue or other causes of rashes that would warrant a medical exam.
2. Cradle Cap
Cradle cap is easy to recognize and common in newborns. It results in greasy yellow or brown scales at the top of the baby’s head. In some cases, it will move down to the face or neck.
It usually develops within the first two or three months. Cradle cap is not contagious (2).
Causes
Nobody is 100% sure what causes cradle cap. However, it is linked to two common factors:
- Fungus: Some babies react to Malassezia, a fungus naturally found on the skin.
- High sebum levels in the affected area: Sebum is an oily substance consisting of fat, keratin, and cellular debris.
Symptoms
Cradle cap won’t cause fever or discomfort for your baby. However, it can cause large flakes to develop. As the scales fall off, you might notice a few hair strands following.
The skin around the scales can become red, and you might notice a smell in severe cases. I find it similar to the aroma of unwashed hair.
I find it similar to the aroma of unwashed hair.
Treatment
Cradle cap will often clear up on its own within a few weeks, although you can help to get rid of it faster. Treating cradle cap is relatively easy:
- Wash your baby’s hair: Using a mild shampoo, lather your baby’s head, and let the shampoo sit for a minute. Then brush the hair with a soft brush before rinsing.
- Apply baby oil: Baby oil or coconut oil will loosen the scales. Brush your baby’s hair with a soft brush to remove loose flakes.
- Soak overnight: Apply Vaseline, olive oil, coconut oil, or vegetable oil, and let it soak overnight. The following morning, wash your baby’s hair with a mild shampoo and rinse.
- Steroid cream and antifungal shampoo: In more severe cases, your physician may prescribe a low-potency steroid and antifungal cream to alleviate cradle cap.
There are special cradle cap shampoos available. These soften the scales quickly, making them easy to remove. The shampoo also prevents new scales from forming.
These soften the scales quickly, making them easy to remove. The shampoo also prevents new scales from forming.
You should never pick at the scales, although I know it can be very tempting. Removing them from the scalp in this way could result in an infection.
3. Erythema Toxicum Neonatorum (ETN)
ETN is a widespread rash that occurs within the first few days of a newborn’s life. It’s most common in full-term babies.
ETN appears as blotchy red bumps that can sometimes look pale and raised due to fluid buildup. If the fluid looks like pus, this can indicate an infection. But in most cases, it’s only a bodily fluid (3).
Causes
The cause of ETN is unknown but is thought to be related to immune system development.
Symptoms
ETN symptoms include a red rash with bumps that sometimes look white or yellow. It shouldn’t cause any discomfort or fever.
It shouldn’t cause any discomfort or fever.
This rash most commonly appears on the baby’s chest, neck, and face. It can develop anywhere except the palms and soles.
Treatment
There is no treatment necessary. However, if it becomes more severe, you should consult your doctor for advice.
4. Atopic Eczema
Eczema can be extremely uncomfortable as the affected area becomes red, itchy, and even cracked.
It could be a long-term, chronic condition that requires extensive treatment. However, it often clears over time as your little one grows (4).
Causes
Atopic eczema can be passed down by your parents. If you suffer from it or have previously, your newborn might also develop the condition.
If your baby is born with an increased risk, keep them away from specific triggers such as these:
- Soaps and detergents: Don’t use scented detergents or soaps. Make sure all soap residue is rinsed off your baby after a bath.
- Allergens: These could be cold, dry weather or a humid environment. Even dust mites, fur, pollen, mold, heat, sweat, and certain foods can cause an allergy.
- Certain fabrics: Wool and synthetic materials are known to trigger eczema.
Symptoms
The affected area will become red, dry, itchy, cracked, and sore. This could result in bleeding skin and inflammation, and secondary infections may occur.
The areas of skin affected might become darker or lighter after eczema has cleared, although this is only temporary.
Treatment
Keeping the skin hydrated is the best way to avoid a rash. Moisturizers, steroids, or eczema creams can help alleviate this. Consult your pediatrician for creams or ointments to help ease the symptoms.
Covering up the area with bandages might be necessary in some instances. However, damaging the skin could cause more eczema.
You may want to consider putting mittens on your baby. Newborns aren’t coordinated enough to scratch, but they might do some accidental damage. I had some great sleepsuits with integrated foldover mitts and found these worked much better than the loose mittens, which quickly fell off.
Newborns aren’t coordinated enough to scratch, but they might do some accidental damage. I had some great sleepsuits with integrated foldover mitts and found these worked much better than the loose mittens, which quickly fell off.
5. Hives
People of all ages can develop hives. The rash features red raised patches or bright red spots.
Hives can appear anywhere on the body. They’re often extremely itchy and are sometimes accompanied by a stinging or burning sensation (5).
Causes
When hives occur, it is because the body has been in contact with a trigger. This could be allergens, such as certain foods, pollen, latex, medications, or insect bites. Infections can also trigger hives.
The trigger causes the body to release histamines. These carry white blood cells to the affected area, which will repair the damage and eliminate the intruder (the trigger). The histamines cause swelling, redness, and itchiness.
Symptoms
The rash will be made up of swollen, red welts of different sizes.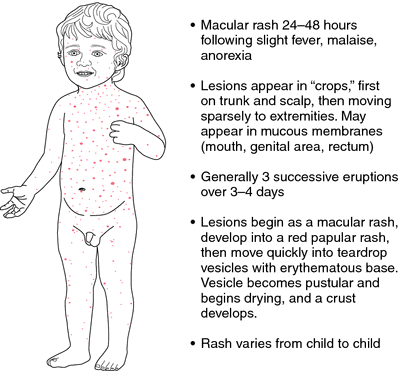 They will be well-defined with a pale center and red surrounding it (similar to mosquito bites but usually bigger).
They will be well-defined with a pale center and red surrounding it (similar to mosquito bites but usually bigger).
Hives can easily spread across the skin in different areas. They can last a few hours, days, or, on rare occasions, weeks.
Treatment
Antihistamines, such as Benadryl, are the best treatment for hives. However, you should never give your baby any medication without consulting a pediatrician first.
If your baby doesn’t seem too bothered by the rash and the size of it isn’t concerning, don’t worry. It should ease and disappear within a day or two.
You can always try different methods to ease the irritation. Wet a washcloth in water, similar to the temperature of a bath, and gently apply it to the affected area.
6. Diaper Rash
A diaper rash is something nearly all parents have to deal with at some point in their child’s life. The rash can be mild, with only a few red spots in one area. More severe rashes will look red and tender (6).
Causes
The leading cause of a diaper rash is prolonged exposure to urine or poop. Here are some other possible causes:
- Disposable diapers: These can sometimes contain chemicals or fragrances which might be causing the reaction.
- Fungal or yeast infection: Bacterias thrive in warm, moist environments, so they often cause rashes in the folds within the diaper area.
- Food: As your baby starts to have solid foods, their stools will change. Acidic foods are known to cause diaper rash in some babies.
- Antibiotics: These will increase the chance of a yeast infection.
Symptoms
The diaper area will be red, a little swollen, and warm to the touch. The rash can spread to the baby’s thighs, stomach, and back.
Some babies will seem troubled by it and uncomfortable during diaper changes. Older children may be holding themselves because it’s painful to pee.
Treatment and Prevention
A diaper rash can be difficult to deal with. But don’t worry, there are many effective ways to treat and prevent it:
But don’t worry, there are many effective ways to treat and prevent it:
- Keep the area dry and clean: Change your baby’s diaper frequently. Gently pat the area dry — never rub!
- Apply ointment or cream: Diaper rash ointments or creams will treat the area and create a barrier on the skin to protect it.
- Loosen the diaper: A good tip is to use a bigger diaper, as this allows for more airflow. You can even leave your baby without the diaper, but make sure to waterproof the surrounding area, particularly if you have a boy!
Cloth diapers are a great option and good for the environment. They need more work since you have to wash them. But they eliminate all the possible chemicals and harsh edges on disposable diapers.
My little one loves cloth diapers as they are softer than disposables. Just remember to wash them in fragrance-free detergent, and never use fabric softeners or dryer sheets.
7.
 Milia
MiliaMilia is common among newborn babies. It looks like tiny white spots that usually form around a baby’s nose (7).
Causes
Milia is entirely harmless. It is the result of the baby’s pores being blocked by dead skin cells.
Symptoms
Small white bumps will appear on a baby’s face and sometimes even on the limbs or the upper body. They can also appear on the roof of the baby’s mouth or on their gums, looking like little teeth coming through. The spots shouldn’t be itchy or painful.
Treatment
The spots will usually clear up on their own within the first four weeks after birth. Never try to squeeze them.
8. Impetigo
Impetigo is a highly contagious infection that causes blisters and sores. Babies and adults can get it, though it’s most common in young children aged 2 to 6 years old. For newborns, it can be dangerous.
The sores and blisters grow quickly and then burst, leaving golden, crusty patches. These may grow and spread to other parts of the body. The patches can also be itchy and painful (8).
These may grow and spread to other parts of the body. The patches can also be itchy and painful (8).
Causes
The rash occurs when bacteria enters the skin — this could be through a cut or a sore. If someone with impetigo comes into contact with your baby, there is a high risk of it being passed on.
Symptoms
Impetigo usually starts as a cluster of red blisters. These will grow, burst, ooze, and then spread. The rash is itchy, which increases the spreading.
The skin in the affected area will be red, and the lymph nodes may also become swollen.
Treatment
Mild cases of impetigo won’t require much treatment. By keeping the area clean, it should clear itself up.
A pediatrician might prescribe antibiotics to help your baby’s body fight off the bacteria. Depending on the child’s age, this could be given orally or as a cream.
Trim your baby’s nails and keep them clean to prevent the bacteria from spreading. Wash the scabs gently, twice a day, using warm water and soap.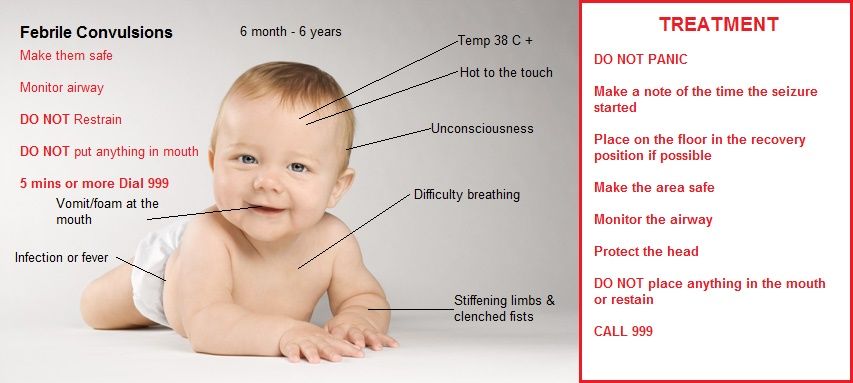 Dry with a towel that is only used for your baby.
Dry with a towel that is only used for your baby.
9. Fifth Disease
Fifth disease, also known as slapped cheek syndrome or parvovirus B19, takes its unique name from how it looks. Any guesses on what it looks like?
It starts as small red patches on the child’s cheeks. It is most common in preschoolers, but babies can also contract the virus, and pregnant mothers can pass it on to their babies.
It’s highly contagious but not harmful. After recovery, most people develop an immunity to the virus (9).
Causes
The cause of fifth disease is the same as most other viruses. If your baby is in contact with another person carrying the virus, they are at risk.
Symptoms
Apart from the red cheeks, there are a few other symptoms you might notice:
- Fever before the rash appears.
- Stuffy or runny nose.
- Sore throat.
- Upset stomach.
- Headache.
- Fatigue.
- Anemia (lack of red blood cells).
The rash can be itchy and will start on the face, but it can also appear on the arms, legs, and buttocks.
Treatment
You should treat fifth disease like any other cold. Your child will need rest and lots of fluids. However, you should always see your pediatrician when a rash occurs. Though harmless, it’s best to rule out other diseases. In rare instances when anemia becomes severe, further medical interventions such as blood transfusion may be warranted.
10. Hand, Foot, and Mouth Disease
Hand, foot, and mouth disease (HFMD) is another widespread viral disease most common in those under 5 years of age.
The child will begin to develop sores around and inside the mouth. You might find them on the tongue, back of the mouth, or inside of the cheeks (10).
Causes
HFMD is due to the infection commonly caused by a coxsackie virus and is highly contagious. It will spread through sneezes, coughs, stool, and fluid from sores and blisters.
Like any other viral infection, children often pass it on to each other.
Symptoms
There are a few symptoms you might notice before the rash begins. These include the following:
- Fever.
- Loss of appetite.
- Sore throat.
- Fatigue.
After the fever starts, usually within a few days, the first sores or blisters will appear on the hands, feet, or mouth.
These can be extremely painful. Older children will surely complain, while younger children and babies will seem super irritated (because they can’t complain).
Sometimes, the rash appears on the buttocks as well.
Treatment
Mild cases only need observation. Make sure to check your baby’s temperature often. They should drink and eat plenty to give the body strength. However, more severe cases require doctor visits and hospitalization.
Your baby might be miserable, so comfort them as much as possible. Treat them with cold drinks or ice cream, which can ease the discomfort.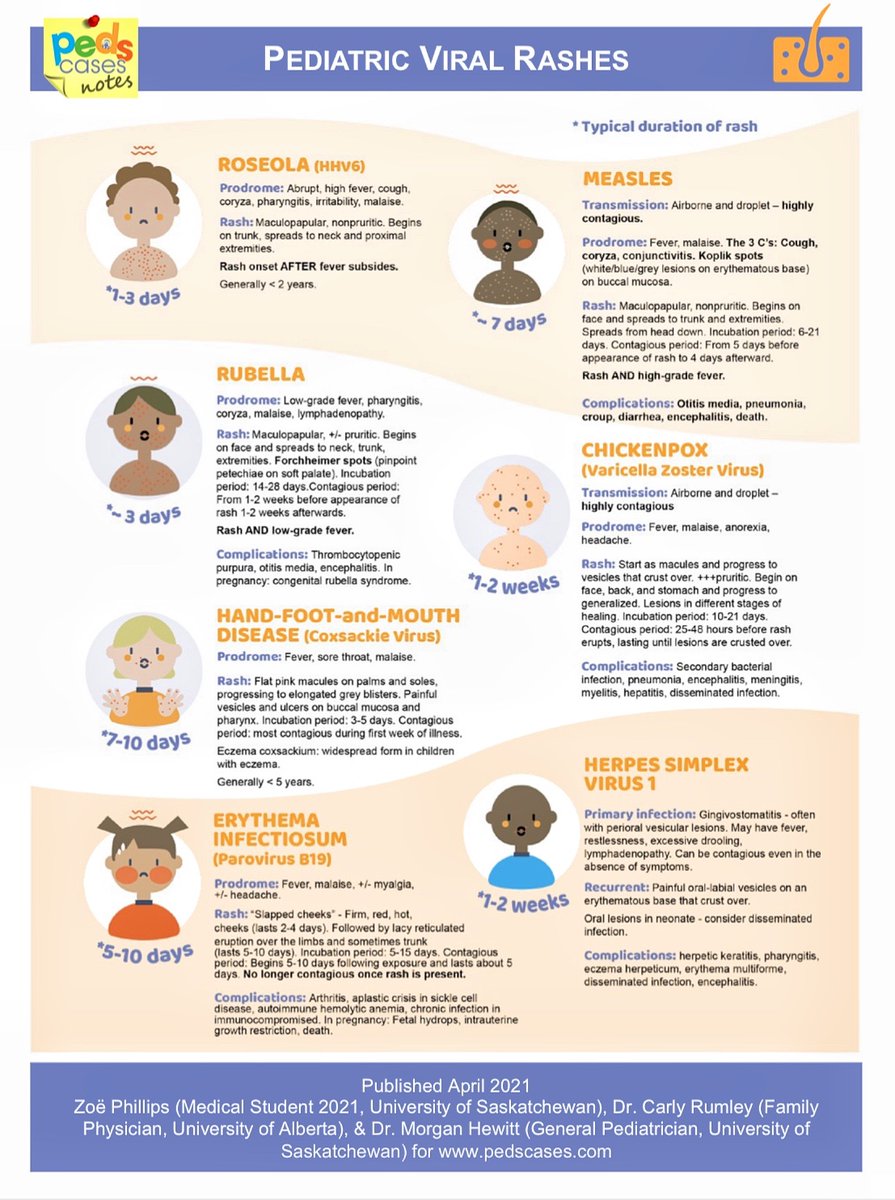 Never give salty, spicy, or acidic foods.
Never give salty, spicy, or acidic foods.
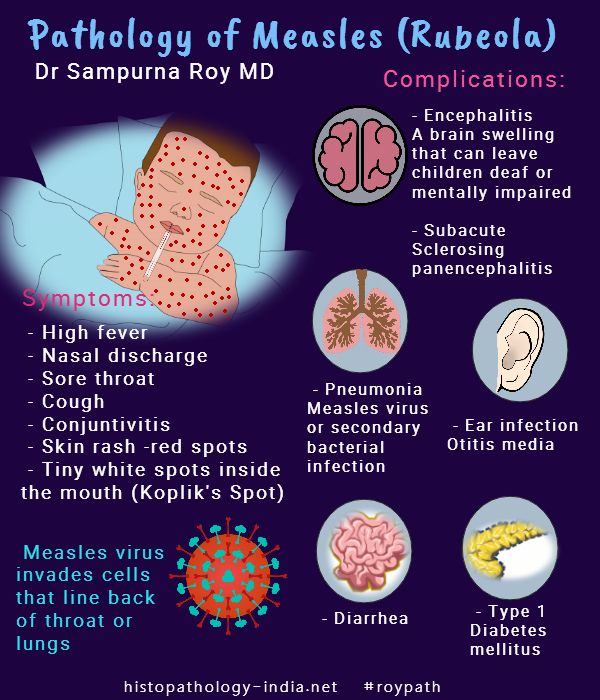
11. Measles
Measles is another viral infection similar to fifth disease. It starts as small red bumps with white dots inside the cheeks, followed by a fever.
A rash will quickly appear and spread from the face down the back and torso, making its way to the arms and legs.
The rash will look like red patches at first, but it will soon develop into itchy raised bumps. Measles is most likely to occur in unvaccinated children (11).
Causes
Measles is highly contagious and is caused by a virus called paramyxovirus. When a person carrying the virus sneezes or coughs, the virus will spread. The droplets containing the virus stay active for up to two hours outside the body.
The United States was considered measles-free in the year 2000. But it has been appearing again mainly because some parents choose not to vaccinate their children (12).
Symptoms
As the first few bumps begin appearing, you might also notice these symptoms:
- Red and runny nose.
- Low energy levels.
- Loss of appetite.
- Nausea and vomiting.
- Diarrhea.
- Swollen lymph nodes.
Treatment
It is critical you contact a doctor immediately if you suspect your child has measles.
Once confirmed, it is crucial to keep your child away from others to prevent the disease from spreading.
Some studies have demonstrated that vitamin A and antiviral agent ribavirin can play roles in the recovery process (13).
Ensure your little one is as comfortable as possible and watch closely for signs of a fever. Measles can cause the temperature to rise to 105 degrees Fahrenheit, which is dangerous.
Talk with your doctor if your child hasn’t been vaccinated yet and is exposed to the virus. They can give an immune globulin injection, which may prevent or ease the symptoms.
The MMR vaccine is usually scheduled at the age of 12 to 15 months, with a booster vaccine at 4 to 6 years.
12. Miliaria
Miliaria, also called sweat rash, prickly heat, or heat rash, usually occurs if your baby has been sweating excessively. It normally occurs in hot, humid conditions (14).
It normally occurs in hot, humid conditions (14).
Causes
If you live in a hot environment, your baby might sweat quite a lot. The sweat glands can become blocked, resulting in a rash. This can also happen if your baby is dressed too warmly or if they are in an overly hot room, such as a room with a fireplace that has been burning all day.
Symptoms
The rash looks like tiny red bumps or blisters, as sweat is trapped under the skin. There will be a lack of sweat in the affected area, and your baby will experience a prickly feeling.
Treatment
Miliaria doesn’t require any treatment since it usually goes away on its own once your baby cools down. Moving your baby to a cooler environment helps. If the rash takes a little longer to clear, your pediatrician might recommend a cream or ointment.
13. Scabies
Scabies is an infestation of the skin. People of all ages can become infected. A baby with scabies will develop small, red spots all over the body (15).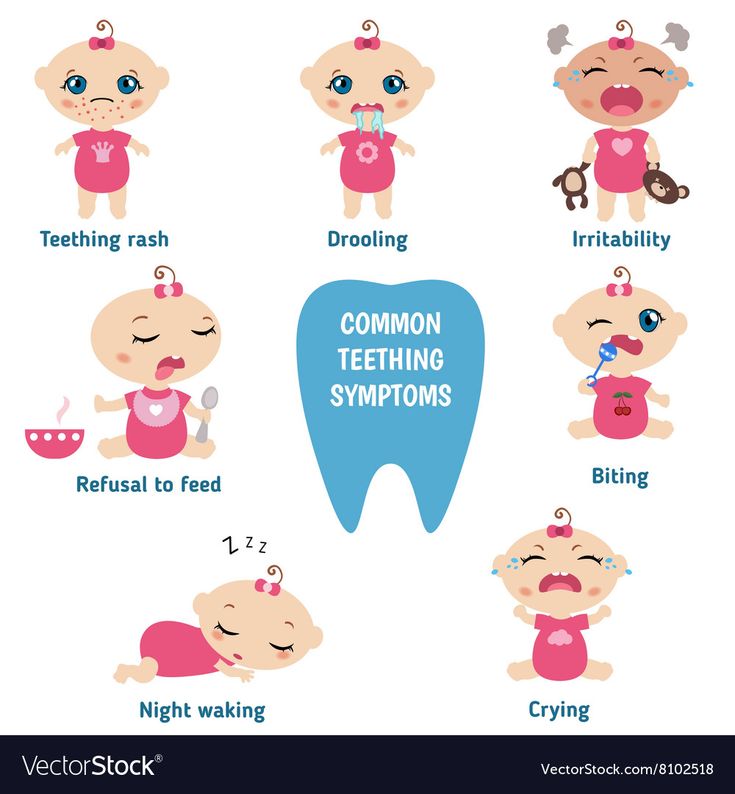
Causes
Scabies is caused by tiny parasitic mites which burrow into the skin. (Eww!) It most often makes its way to your baby with the help of friends or other family members.
Symptoms
The rash will feature little bumps that can form a line. There will be extreme itchiness that is worse at night with potential sores and crusty areas. Scabies usually occurs on hands and arms but can develop anywhere on a baby’s skin.
Treatment
It’s necessary to contact your doctor and obtain treatment that will kill the mites. However, it’s not enough to only treat your child; it’s crucial to treat everyone who might also be infected. Some people choose to treat the whole house.
14. Ringworm
Ringworm is a common fungal infection. It causes a unique red rash in the form of a ring. Ringworm can develop anywhere on the body.
In babies, it is most often seen on the scalp, feet, and groin area (16).
Causes
Ringworm is actually caused by fungi — not a worm! It spreads as people come into contact with others who are infected — humans or animals.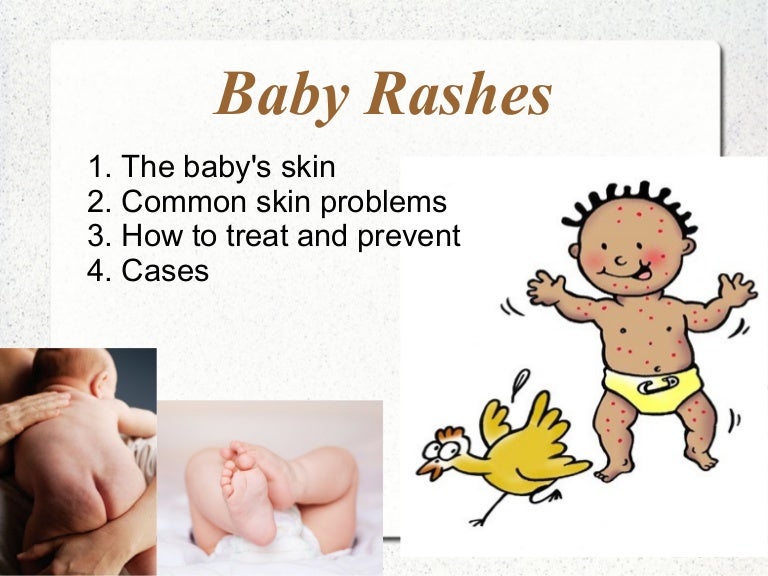 The fungi may also be present on bedsheets, towels, and even combs.
The fungi may also be present on bedsheets, towels, and even combs.
Symptoms
The rash will have round patches that are red or silver. It may be dry, scaly, itchy, and swollen. You might also notice blister-like lesions or some hair loss if the rash appears on the scalp.
Treatment
An antifungal cream, gel, or spray is an effective method. It’s essential to finish the whole course of treatment to make sure the infection is completely cleared.
15. Meningitis
Meningitis is a severe condition that affects the protective membranes surrounding the spinal cord and brain.
While meningitis can affect anyone, it’s most common in babies and children. The infection should be treated immediately. It could develop into life-threatening blood poisoning, called septicemia, which can lead to permanent brain and nerve damage.
Vaccines are available to protect against some forms of meningitis (17).
Causes
A viral or bacterial infection can cause meningitis.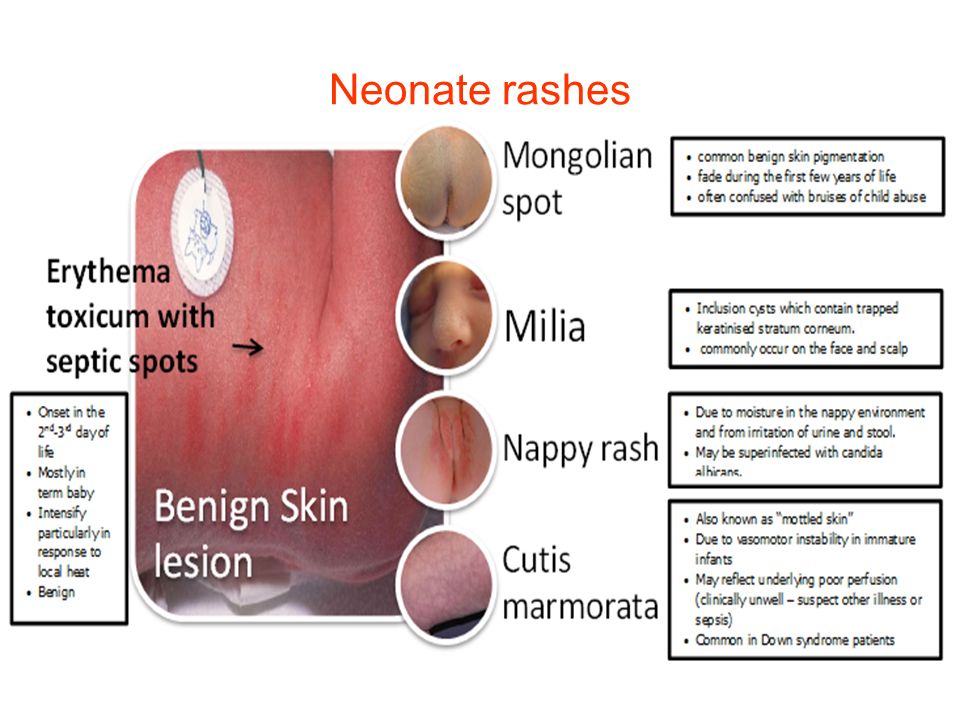 Viral infections are the most common cause, including the following :
Viral infections are the most common cause, including the following :
- Enteroviruses.
- Influenza.
- Herpes simplex viruses.
- Varicella-zoster virus.
- Measles and mumps.
- Haemophilus influenza type b (Hib).
- Group B Streptococcus.
- E. coli.
- Streptococcus pneumoniae.
- Listeria monocytogenes.
- Neisseria meningitis.
Symptoms
A patchy rash with lots of small red spots gathered in one area is the first sign. One way to tell if it’s a meningitis rash is by pressing a glass over it. If the rash doesn’t fade, it could be meningitis.
These are some other symptoms of meningitis:
- Fever of 100.4 degrees Fahrenheit or above.
- Lack of energy or extreme sleepiness.
- Rapid breathing.
- Cold hands and feet.
- Pale skin.
- A stiff neck and body.
- Swelling of the fontanelle (the soft spot on a baby’s head).
- Drowsiness or unresponsiveness.
- Seizures.
- Refusing to feed.
- Not wanting to be picked up.
- Unusual high-pitched cry.
- Shivering.
Treatment
If there are any signs of meningitis, it is vital you get your baby to a hospital immediately. This is a medical emergency.
Antibiotics may be given and fluids to treat dehydration. Some cases require steroid medication to reduce swelling around the brain.
Treatment in the hospital can take anywhere from a few days to several weeks. Your baby might also need some aftercare once home again.
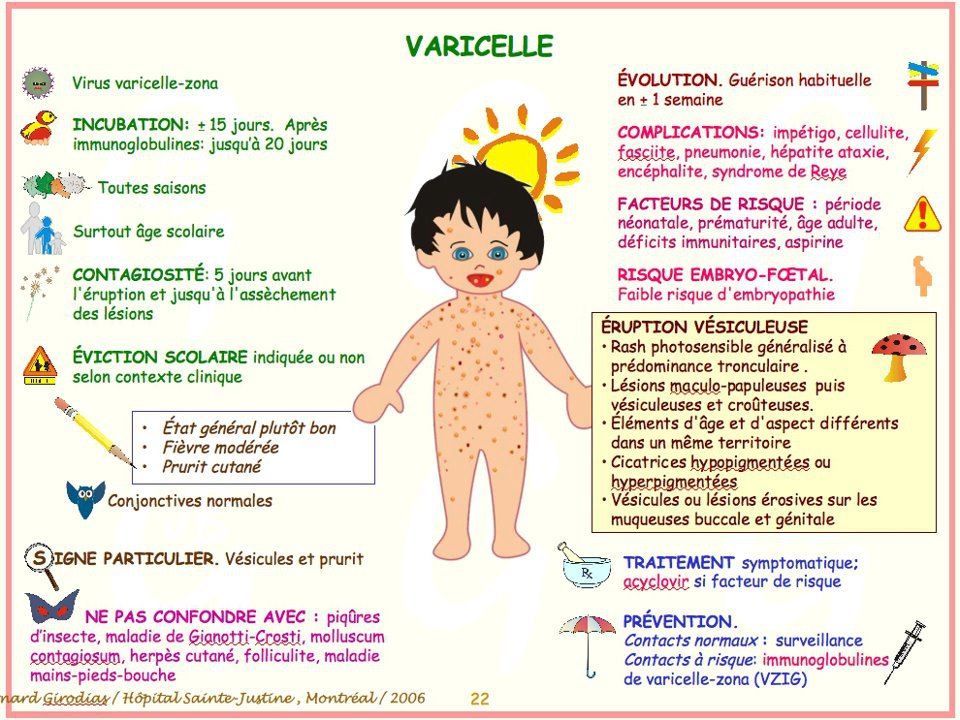
16. Chickenpox
Chickenpox is a rash due to the varicella-zoster virus (VZV) infection. The baby may first show flu-like symptoms before developing a rash, which appears as red, itchy spots over the body.
Babies are especially susceptible to chickenpox infection because they cannot get immunization until the age of one year old. Fortunately, the incidence of chickenpox has declined by 90% since 1995 with the introduction of the varicella vaccine.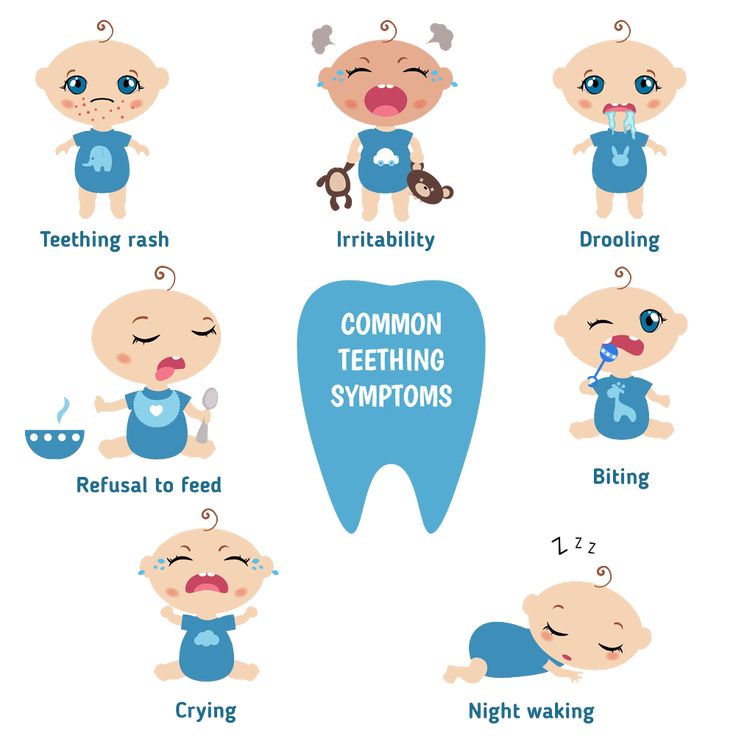 Since the prevalence of chickenpox decreased drastically in the general population, there are fewer carriers who can pass the disease on to infants, a phenomenon called “herd immunity” (18).
Since the prevalence of chickenpox decreased drastically in the general population, there are fewer carriers who can pass the disease on to infants, a phenomenon called “herd immunity” (18).
Causes
VZV infection occurs through viral transmission similar to that of measles. When a person coughs or sneezes, the air droplets containing the virus can spread to unvaccinated babies, leading to chickenpox. Transmission can also occur through physical contact with those who have a chickenpox rash. Vertical transmission can also occur when an infected pregnant mother transmits the virus directly to the fetus.
Symptoms
Flu-like symptoms can occur in infants infected with chickenpox days before the development of the rash. The flu-like symptoms include:
- Fever.
- Cough.
- Poor feeding.
- Fussiness.
- Fatigue.
- Sleepiness.
The rash starts at the torso and the head, then spreads to limbs over several days.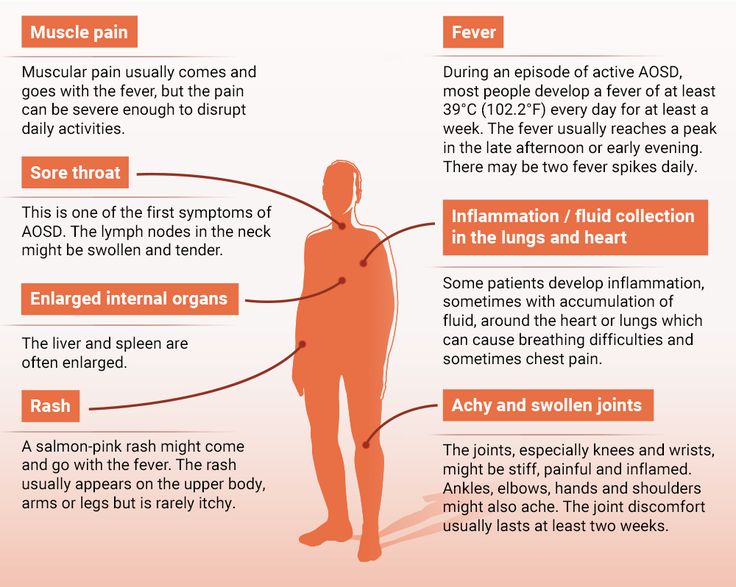 The rash starts as itchy, red bumps, which later become fluid-filled blisters. The blisters burst to become open sores that scab over and heal. This whole process can last from five days to two weeks.
The rash starts as itchy, red bumps, which later become fluid-filled blisters. The blisters burst to become open sores that scab over and heal. This whole process can last from five days to two weeks.
Treatment
You should notify your pediatrician immediately if you suspect your baby has a chickenpox infection, even if the symptoms are mild. You should also let your physician know right away if your baby develops any of the following symptoms:
- High fever.
- Rash on the eyelid or around the eyes.
- Stiff neck.
- Vomiting.
- Severe cough.
- Difficulty breathing.
- Extreme sleepiness or difficulty waking up.
- Rash that has become warm and swollen.
Treatment of chickenpox is usually supportive. However, in more severe cases of chickenpox, or if a baby is born with chickenpox (congenital chickenpox) due to an infected mother, the physician may prescribe an antiviral agent called acyclovir.
To prevent chickenpox from infecting an unvaccinated baby, avoid contact with anyone who is infected with chickenpox.
17. Molluscum Contagiosum
Molluscum contagiosum is another viral infection that causes rashes in babies. The rashes consist of small pink bumps with indented centers. Molluscum contagiosum can occur anywhere on a baby’s body, but it is most commonly found on the head, neck, torso, and armpits.
Causes
The rash is caused by an infection with the molluscum contagiosum virus (MCV). Babies can get molluscum contagiosum rashes in a couple of ways, such as direct skin-to-skin contact with someone who has molluscum contagiosum or contact with objects, such as toys or towels, that have MCV on them.
Most of the time, the only symptom of MCV infection is the rash. The rash appears like pink, skin-colored dome-shaped bumps with central indentations. They can appear anywhere on the body except the palms of the hands, the soles of the feet, and very rarely on the oral mucosa. The bumps can occur in isolations or in groups.
Treatment
Treatment is optional, especially in immunocompetent infants and children, since MCV rashes usually go away on their own within 18 months.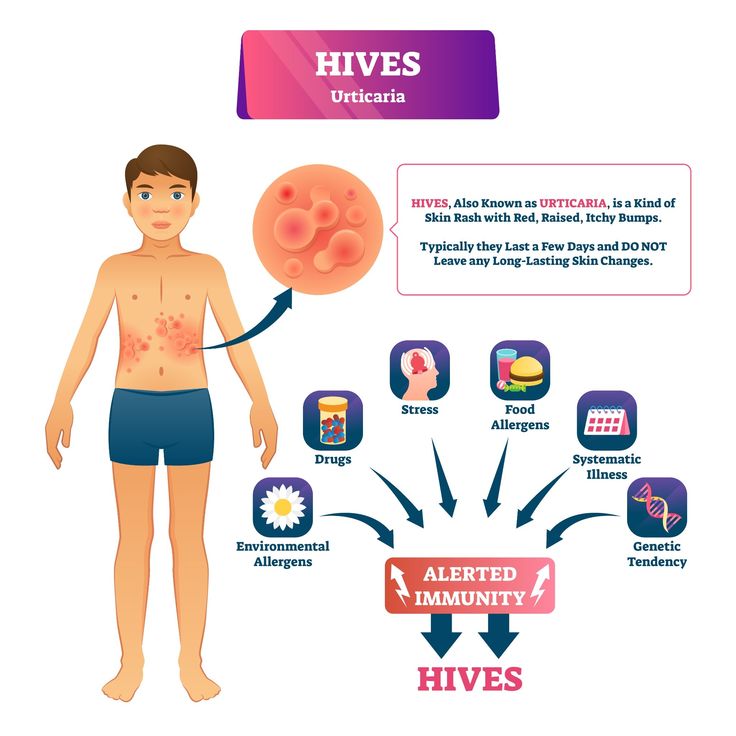 Some doctors may use a variety of methods such as freezing the bumps (cryotherapy), removal via sharp instruments (curettage), or application of wart removing chemicals or creams. However, many doctors prefer not to use these methods because they can cause burns and skin scarring.
Some doctors may use a variety of methods such as freezing the bumps (cryotherapy), removal via sharp instruments (curettage), or application of wart removing chemicals or creams. However, many doctors prefer not to use these methods because they can cause burns and skin scarring.
Since molluscum contagiosum can spread from one part of the body to another through contact, it is wise to cover up the areas of rash with small, watertight bandages. Caretakers should also wash their hands often to prevent the spread of the MCV.
When to Worry About a Rash
Babies have sensitive skin, so even the most minor thing can cause a reaction.
Most rashes are harmless and will improve or disappear within a few days. Always contact your pediatrician if a rash looks suspicious or is accompanied by a fever.
Rashes can sometimes be caused by an allergic reaction. With this comes the risk of anaphylactic shock.
These are some of the symptoms of a severe allergic reaction:
- Difficulty breathing.
- Hard for baby to feed or swallow.
- Baby is lethargic.
- Vomiting.
- Increased heart rate.
- Any swelling in the face, around the mouth or throat (19).
Make a Rash Decision
Always take good care of your baby’s precious skin. Don’t bathe your child too frequently using soap. Instead, choose a gentle cleaning product that is unperfumed and moisturizing. End the bath with a lotion or oil massage — this is when you can get a good look at your child’s skin and spot anything out of the ordinary.
Most rashes that appear in newborns are harmless. ETN, baby acne, and heat rash are the most common.
Knowing what to look for should help to ease your mind or let you know when to take action. If you’re ever unsure of a rash and what could be causing it, don’t hesitate to contact your child’s pediatrician.
Feedback: Was This Article Helpful?
Thank You For Your Feedback!
Thank You For Your Feedback!
What Did You Like?
What Went Wrong?
Skin rash in children: analyze the causes
Features of children's skin
The skin, like most other organs and systems, gradually develops until puberty.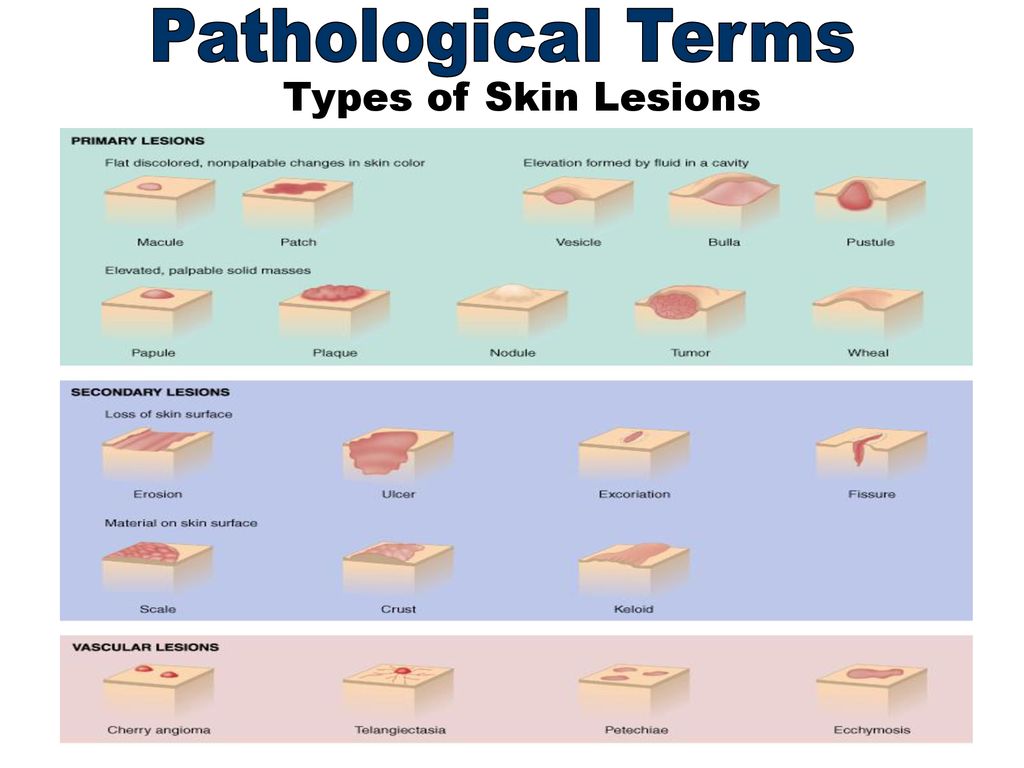 In a child, it is functionally and structurally more sensitive to external influences and allergic reactions. At the same time, the sweat and sebaceous glands do not yet work properly, which is associated with insufficient development of skin innervation.
In a child, it is functionally and structurally more sensitive to external influences and allergic reactions. At the same time, the sweat and sebaceous glands do not yet work properly, which is associated with insufficient development of skin innervation.
At the same time, the skin from birth takes an active part in metabolism and respiration due to the many superficially located vessels. Because of this, skin diseases often greatly affect the general condition of the child.
Types of rash in children
Skin rash caused by a particular disease usually has its own characteristics. The most common types of rashes include:
- Papules. These are volumetric formations of a small size (up to 10 mm), which rise above the skin. The main color is red and pink. Occurs with lichen planus, roseola infantum, atopic dermatitis, etc.
- Vesicles. They are bubbles up to 5 mm in diameter, filled with a cloudy liquid. After opening, erosion is often left behind.
 May be a sign of chickenpox and other herpes infections.
May be a sign of chickenpox and other herpes infections. - Petechiae. A purplish skin eruption that does not go away with pressure. Its elements do not exceed 3 mm in diameter, do not rise above the skin and are not felt to the touch. As a rule, they indicate meningococcal infection, vascular damage (vasculitis), platelet deficiency.
- Erosion. This is a skin defect that does not penetrate deeper than the epidermis. It has the appearance of a rounded, somewhat in-depth formation of red color with a weeping surface.
- Peel. A secondary element formed by the drying of secretions from vesicles, erosions, or blood. Solid, has a dark red, brown color.
- Macula or spot. This is an area of discoloration that is on the same level as adjacent areas of the skin. It can be both an independent element in rubella, measles, roseola, and a residual phenomenon after papules, vesicles or erosions.
- Wheals or urticaria. A rounded element of a rash of pale pink, red or purple-white color, the size of which varies from 1-2 mm to tens of centimeters.
 Leaves no secondary elements behind. Meet with allergic reactions, urticaria.
Leaves no secondary elements behind. Meet with allergic reactions, urticaria. - Lichenification. These are areas of excessive thickening of the skin with increased skin pattern. Often a secondary element.
Diseases that cause skin rashes in children
Baby skin rashes can indicate various diseases, most often infections and allergic reactions.
Roseola infantum
Roseola infantum or sudden exanthema is a childhood infectious disease that occurs when infected with human herpesviruses type 6 or 7. Most often observed between the ages of 6 months and 2 years.
Sudden exanthema is accompanied by an increase in body temperature up to 39-40°C, which persists for 3-5 days, after which a bright red maculopapular rash appears on the child's skin. It occurs on the surface of the chest and abdomen, spreading throughout the body (Fig. 1). The elements of the rash, as a rule, are not felt by the fingers, but sometimes they can be raised. They disappear when the skin is stretched or when the glass of a glass is pressed on them.
They disappear when the skin is stretched or when the glass of a glass is pressed on them.
In roseola infantum there may be white rings around some elements of the rash. Often the rash is limited only to the trunk and, not having time to reach the face and limbs, disappears. The rash does not cause discomfort or itching, but children usually become sharply capricious and "unbearable" during this time; the rash lasts from several hours to several days, and then disappears, leaving no pigmentation or peeling. An excerpt from the book by Sergei Butriy “Child health: a modern approach. how to learn to cope with illness and your own panic.
Roseola infantum should be treated symptomatically, preferably with antipyretics and plenty of fluids. In immunodeficiency states (HIV infection, congenital disorders of the immune system), antiherpetic drugs are additionally prescribed.
Figure 1. Rash in roseola infantum. Source: WikipediaNo matter how hard baby roseola flows, it is perfectly safe.
Complications are extremely rare and are usually limited to febrile convulsions. An excerpt from the book by Sergei Butriy “Child health: a modern approach. how to learn to cope with illness and your own panic.
Enteroviral exanthems: chicken pox and enteroviral pharyngitis
The viral pemphigus, also known as turkish varicella, is caused by enterovirus 71 (EV-71). Enteroviral pharyngitis is caused by Coxsackie A16, B2, B5 viruses. They occur mainly among children under the age of 10 years, infection often occurs during holidays in southern countries.
The primary signs of pathologies are pain in the mouth and throat, because of which the child refuses to eat and does not even swallow saliva, but spits it out. Then the body temperature rises to 39°C. The fever persists for about 4 days and is accompanied by nausea and vomiting, loss of appetite and excessive irritability. With enteroviral pharyngitis, small white sores usually occur only on the palatine arches (Fig.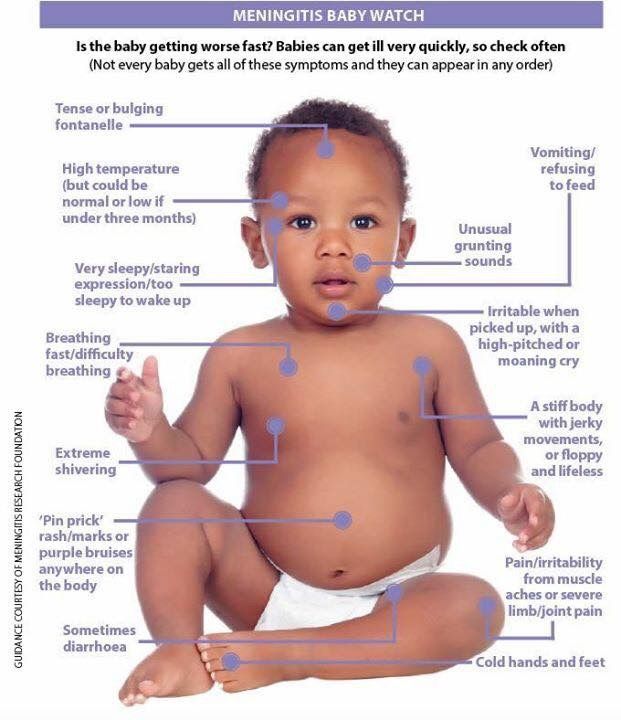 2), but Turkish chickenpox is a rash throughout the mouth, including the tongue, around the mouth, on the palms and feet. The rash on the skin may resemble chickenpox - red spots or blisters.
2), but Turkish chickenpox is a rash throughout the mouth, including the tongue, around the mouth, on the palms and feet. The rash on the skin may resemble chickenpox - red spots or blisters.
Symptomatic treatment:
- Oral hygiene and rinsing with antiseptic solutions.
- Non-steroidal anti-inflammatory drugs (NSAIDs) that help control pain while lowering body temperature.
- Plentiful warm fluids to prevent dehydration, cold drinks and ice cream may be given (these are more easily tolerated by sick children).
- Diet with the exception of mechanically hard, sour and salty foods.
- Enteroviral exanthems are self-limiting, the disease usually recedes after 3-7 days. However, the condition of the child during the illness must be monitored in order to consult a doctor in time in case of complications. The most common are dehydration and secondary bacterial infections.
 In the latter case, abscesses, yellow crusts appear on the skin, the skin swells. Rarely enterovirus infection leads to serous meningitis.
In the latter case, abscesses, yellow crusts appear on the skin, the skin swells. Rarely enterovirus infection leads to serous meningitis.
Chickenpox
Chickenpox or chickenpox is an infectious disease caused by the human herpesvirus type 3 (Varicella Zoster). People of any age get sick with it, but mostly it is children 5-9years.
The main symptom is skin rashes that have a certain sequence of development. Small pink spots appear first, quickly transforming into papules, and then into vesicles (Fig. 3) with reddening around. After a couple of days, they open or dry out, forming crusts of dark red, brown color on their surface. A characteristic feature is severe itching.
Figure 3. Development of a skin rash in chickenpox. Source: SlideToDoc
The total period of rashes lasts from 2 to 9days. At the same time, the general condition practically does not suffer, but fever may occur.
There are no drugs that can completely eliminate the virus, so the treatment tactics are aimed at eliminating the symptoms and normalizing the child's condition:
- Bed rest in the presence of fever.
- Treatment of elements of the rash with a solution of manganese, methylene blue or brilliant green (brilliant green).
- Antihistamines for itching.
- Antipyretics.
- Taking regular warm showers without using a washcloth or brush.
Complications of chickenpox occur against the background of suppression of the body's immune system. These include: inflammation of the lungs (pneumonia), lesions of the nervous system (neuralgia, meningitis, encephalitis, damage to the facial nerve), eyes (keratitis, conjunctivitis, uveitis), etc.
Important ! For the prevention of chickenpox, especially for adults, against the background of a weakened immune system and a high risk of complications, vaccination is recommended. It can also be carried out as an emergency prophylaxis up to 2 days from the moment of contact with a sick person.
Measles
Measles is a viral infectious disease. Often it occurs in unvaccinated children from 2 to 5 years and older.
Measles debuts with a sharp rise in temperature to 39-40°C, dry cough, runny nose, headache, hoarseness. Characteristic features are swelling and redness of the eyelids, pharynx and red spots in the sky. On the 2-3rd day of development, a symptom specific to measles occurs - Filatov-Belsky-Koplik spots. These are white spots with a red border, observed on the inner surface of the cheeks near the molars. On the 4-5th day from the appearance of the first signs of the disease, these spots disappear, and they are replaced by a skin rash.
The primary localization of measles papular rash is the outer surface of the elbow, knees, fingers. Further, it spreads throughout the body (Fig. 4). The elements of the rash are surrounded by red spots and tend to merge with each other. After 4 days from the moment they appear, the child's condition returns to normal, and the elements of the rash become darker and peel off. Residual effects and pigmentation disappear after 7-10 days.
Figure 4.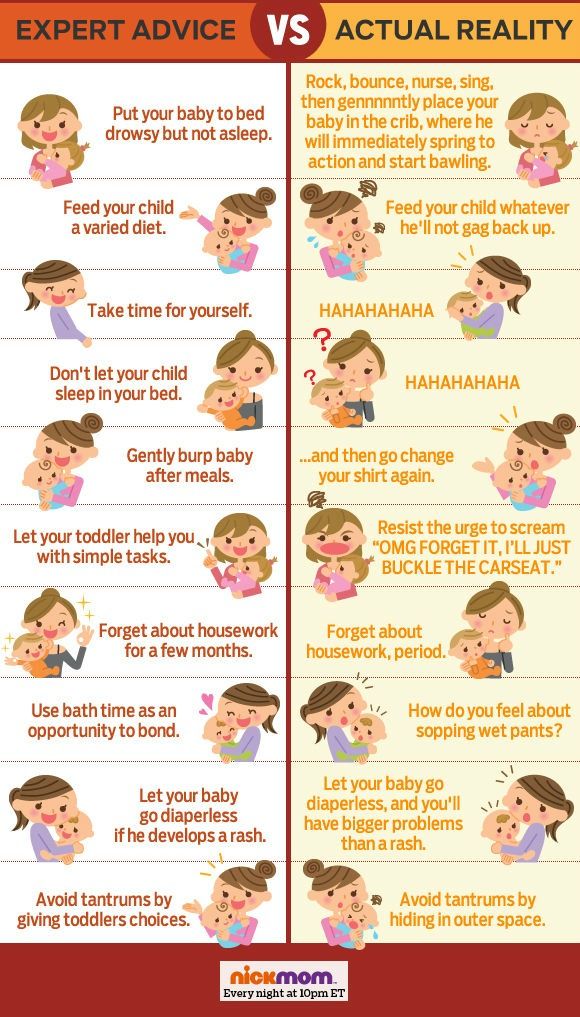 Skin rash in measles. Source: CDC
Skin rash in measles. Source: CDC
There is no specific treatment for measles; helping a child involves managing individual symptoms:
- NSAIDs to reduce body temperature.
- Expectorants for relief of coughs.
- Antiseptic mouth rinses.
- Topical treatment of rash elements with astringents or tea to relieve itching and soreness.
Measles is very dangerous. Possible complications of measles:
- Stenosis of the larynx - croup.
- Primary measles or secondary bacterial pneumonia.
- Inflammation of the respiratory tract - bronchitis, tracheitis, laryngitis, pharyngitis.
- Otitis media.
- Hepatitis.
- Encephalitis and subacute sclerosing panencephalitis.
Scarlet fever
Scarlet fever is a bacterial infection caused by group A beta-hemolytic streptococcus. Most cases occur in children between 3 and 7 years of age.
The first manifestation of scarlet fever is an intoxication syndrome - an increase in body temperature up to 38-39°C, headache, general weakness and loss of appetite. On the 2-4th day from the moment the first signs of the disease appear, one of the characteristic symptoms appears - "crimson tongue" (Fig. 5). It is manifested by pronounced graininess and bright red color of the surface. Angina also occurs - inflammation of the palatine tonsils.
On the 2-4th day from the moment the first signs of the disease appear, one of the characteristic symptoms appears - "crimson tongue" (Fig. 5). It is manifested by pronounced graininess and bright red color of the surface. Angina also occurs - inflammation of the palatine tonsils.
From the first days of scarlet fever, a characteristic red punctate rash appears, which does not disappear when pressed with glass, but becomes yellowish with effort. It is located on the flexion surfaces: the inner parts of the elbows, under the knees, in the inguinal pits, on the cheeks and sides of the body. It lasts up to 1 week, after which it disappears, leaving no pigmentation behind. A specific sign is the pallor of the nasolabial triangle.
Another characteristic feature of scarlet fever is the peeling of the skin that occurs after the rash has disappeared. At the same time, the skin "moves away" in whole layers in the area of the palms and feet, while in other areas - in small fragments.
Treatment is based on antibiotics from the penicillin group. Vitamin C and B vitamins, symptomatic preparations are used as adjuvants. Plentiful warm drink and bed rest are recommended. In severe cases, glucocorticosteroids and intravenous drip of glucose solutions and plasma substitutes are used.
The most common complications of scarlet fever: otitis media, sinusitis and frontal sinusitis (inflammation of the maxillary and frontal paranasal sinuses, respectively), cervical lymphadenitis (inflammation of the lymph nodes of the cervical region).
Rubella
Rubella is caused by Rubella virus. The majority of patients are children aged 3 to 9 years.
Rubella begins with an intoxication syndrome of moderate severity: fever up to 38-38.5°C, headache and increased fatigue, signs of pharyngitis and conjunctivitis, pronounced enlargement of the lymph nodes of the cervical and occipital region.
After 1.5-2 days from the onset of the disease, a skin rash appears in the form of spots, which spreads downward over several hours - appearing on the face, gradually moving to the trunk and limbs.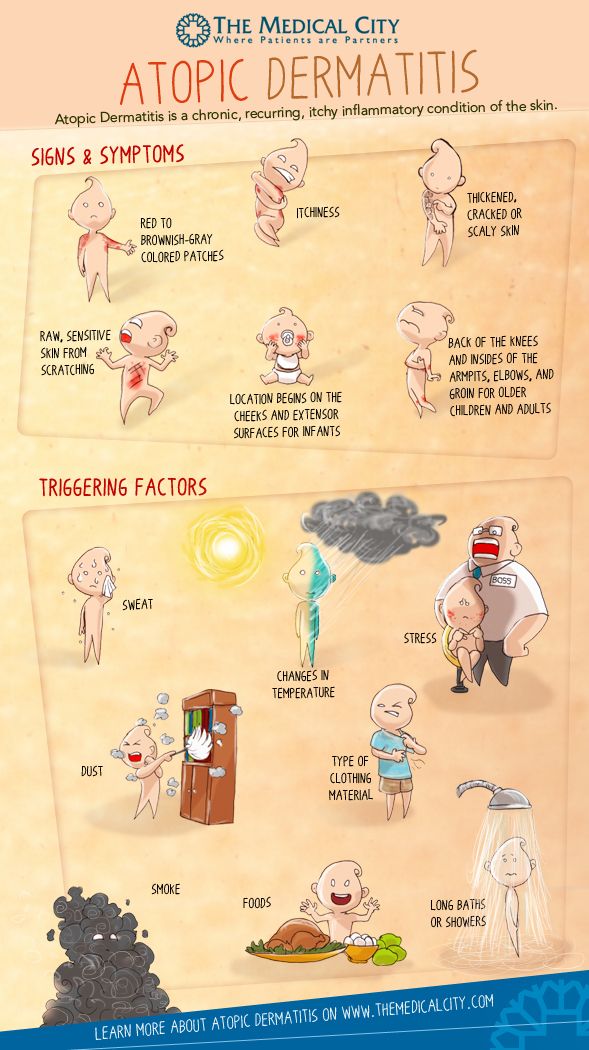 Outwardly, the rash initially resembles measles, then scarlet fever. Itching and peeling are absent, and the spots, unlike measles, do not merge with each other. The bulk of the spots are located on the buttocks and lower back, the outer surface of the elbows and knees. After 3-5 days, the rash disappears without a trace.
Outwardly, the rash initially resembles measles, then scarlet fever. Itching and peeling are absent, and the spots, unlike measles, do not merge with each other. The bulk of the spots are located on the buttocks and lower back, the outer surface of the elbows and knees. After 3-5 days, the rash disappears without a trace.
There is no specific treatment for rubella, and the main actions are aimed at eliminating individual symptoms of the disease. Complications are very rare, as a rule - against the background of disorders of the immune system. In such cases, the development of pneumonia, arthritis, otitis media is possible.
Important ! Rubella is especially dangerous for pregnant women, as it causes problems in the fetus, so when planning a pregnancy, all unvaccinated people should be vaccinated against this infection.
Urticaria
Urticaria or urticaria is a type of dermatitis caused by allergies. The disease is very common among both children and adults.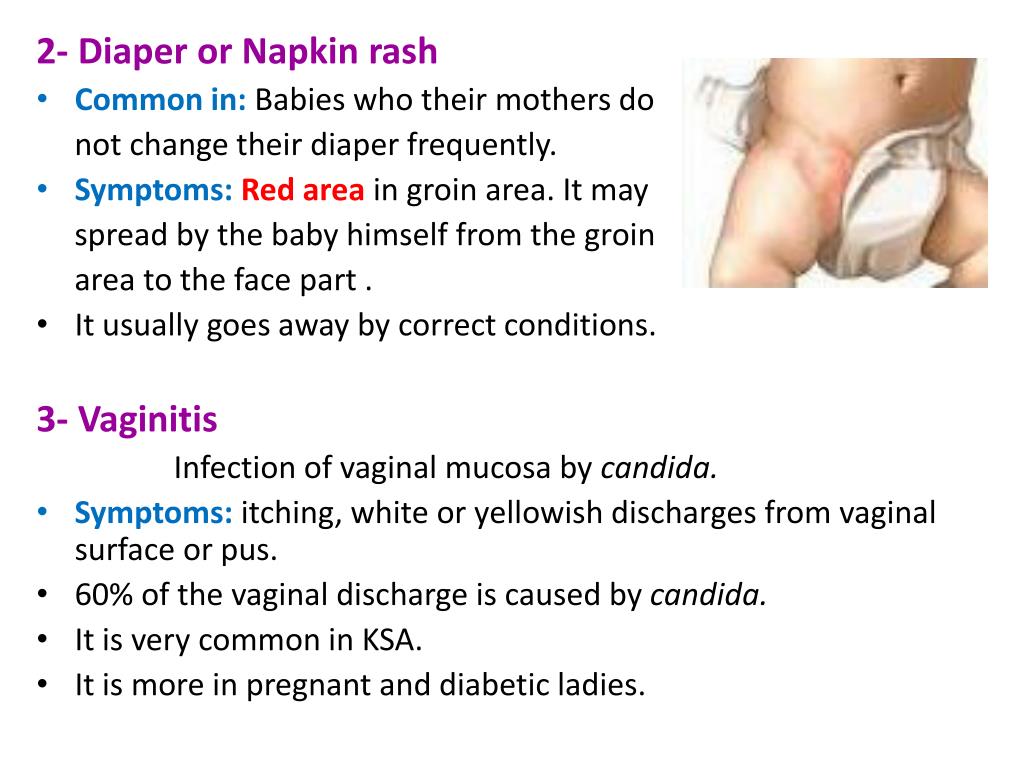 In total, about 20% of the adult population and 2-7% of children suffer from it.
In total, about 20% of the adult population and 2-7% of children suffer from it.
Medications (most often antibiotics), various foods, vaccines and physical influences: cold, sunlight, mechanical pressure can provoke the development of urticaria.
The leading symptom of the pathology is a skin rash in the form of dense red or pink vesicles or nodules 2-10 mm in diameter with clear edges, which become pale when pressed (Fig. 6). A characteristic feature is the sudden appearance and equally rapid disappearance of the elements of the rash without a trace, as well as severe itching.
Figure 6. Urticaria rash. Source: James Heilman, MD/Wikipedia
Treatment, depending on the form of the disease, is represented by antihistamines, histamine receptor blockers or glucocorticosteroids.
Complications occur in the absence of treatment and include angioedema, anaphylactic shock, heart and kidney damage in the form of myocarditis or glomerulonephritis, respectively.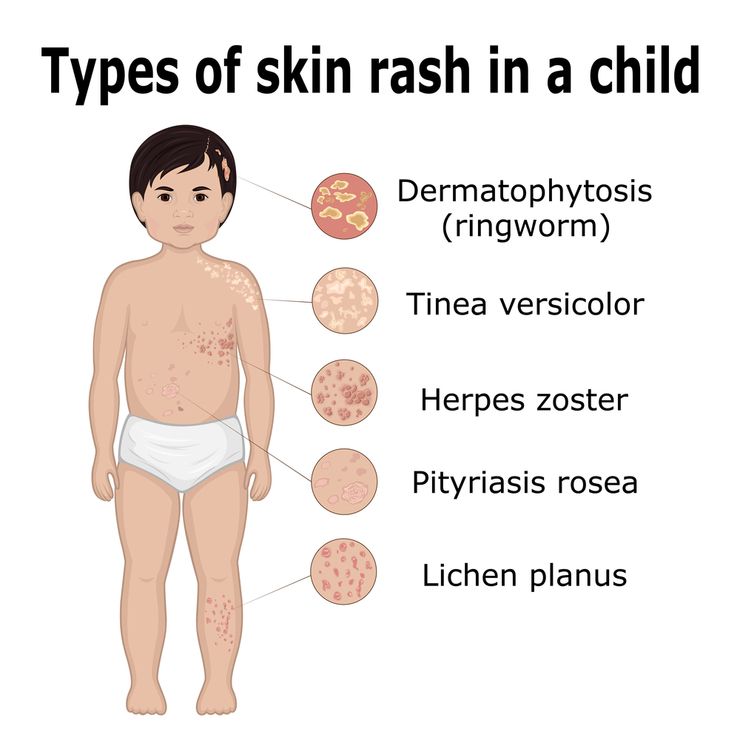
Lichen planus
Lichen planus is a chronic dermatitis of unknown origin. Most of the patients are people aged 30 to 60 years. However, about 5% of the total number of patients are children.
A typical form of the disease is accompanied by the appearance of gray-white papules up to 2 mm in diameter on the oral mucosa, namely: the inner surface of the cheeks behind the molars, on the lateral parts of the tongue and on the palate. Sometimes the rashes can merge, forming patterns.
In some patients, a rash also appears on the skin of the flexor surfaces of the limbs of the arms and legs, the inner thighs. It has the appearance of small papules of various shapes and pinkish-purple color with a shiny surface and a depression in the center.
Treatment includes diet with restriction of salt, smoked and fried foods, coarse food that irritates the mucous membranes. Glucocorticosteroids are prescribed as medical support.
Pityriasis rosea
Pityriasis rosea or Gibert's versicolor is a variant of a skin lesion whose cause has not been clearly identified.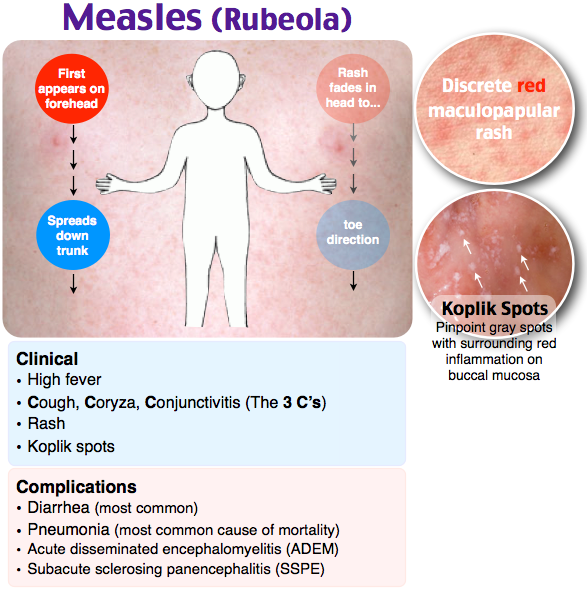 Exacerbations occur against the background of immune suppression - colds, hypothermia, chronic stress, etc. Most cases of this pathology are observed in people aged 20 to 40 years, as well as in adolescents.
Exacerbations occur against the background of immune suppression - colds, hypothermia, chronic stress, etc. Most cases of this pathology are observed in people aged 20 to 40 years, as well as in adolescents.
The disease begins with the formation of a primary scaly focus of pinkish or yellowish color from 1 to 10 cm in diameter with a clear rim. After 1-2 weeks, secondary plaques and smaller papules appear on the body and limbs - up to 2 cm (Fig. 7). Gradually, the elements of the rash turn pale, and the outer edge becomes rougher. The rash may be accompanied by itching, fever and other manifestations of the intoxication syndrome.
The disease tends to self-heal within 4-5 weeks. Treatment is mainly local in the form of ointments based on glucocorticosteroids, and antihistamines and NSAIDs are prescribed to combat itching and fever.
Figure 7. Skin rash with rosacea. Source: James Heilman, MD/Wikipedia
Atopic Dermatitis
Atopic dermatitis or eczema is a genetically determined inflammatory skin lesion of an autoimmune nature. Most often, children under 14 years of age living in large, industrial cities get sick.
Most often, children under 14 years of age living in large, industrial cities get sick.
Atopic dermatitis develops with a probability of 80% if both parents have a history of this pathology, and with a 50% probability if only one of them.
The first symptoms occur before the age of 2 years due to exposure to allergens, which can be food, plant pollen, dust and mold, cosmetics.
Typical symptoms are skin rashes, which vary depending on the stage of the disease. When exacerbated, red spots, papules and small vesicles appear, accompanied by severe itching. In infants, the typical site is the face, scalp, and neck. At an older age, the flexion surfaces of the limbs and the neck are affected. In the remission stage, they are replaced by foci of increased dryness of the skin, peeling and lichenification. During the year, on average, there are 2-4 exacerbations.
Ointments and creams based on glucocorticosteroids, calcineurin inhibitors, and zinc are used in the treatment.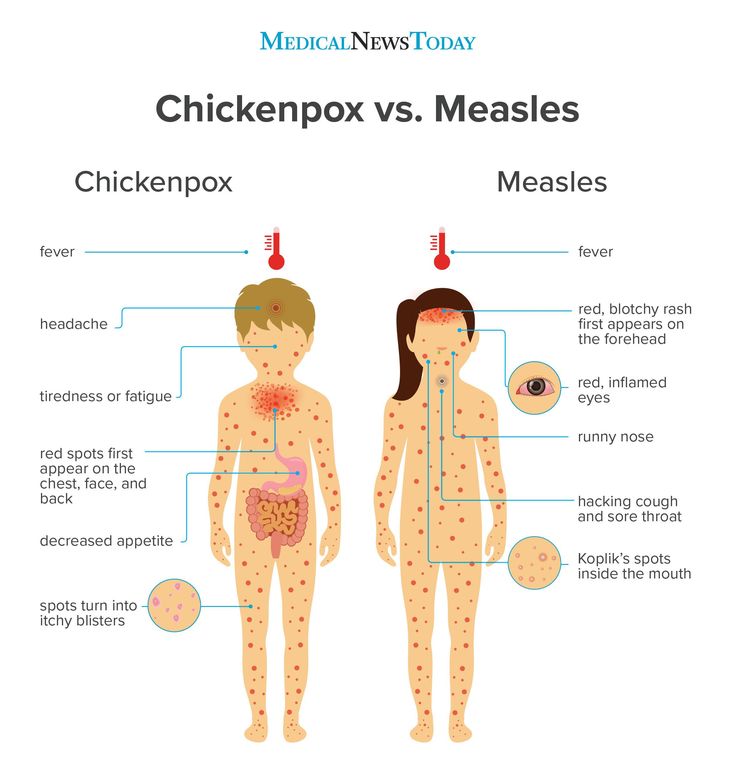 In severe cases, hormonal drugs are used in the form of tablets or intravenous injections. Antihistamines are also used to combat itching.
In severe cases, hormonal drugs are used in the form of tablets or intravenous injections. Antihistamines are also used to combat itching.
Infectious mononucleosis
Infectious mononucleosis is the result of infection with human herpesvirus type 4 (Epstein-Barr virus). It is believed that already before the age of 5, about 50% of children become infected with this virus, and its prevalence among adults reaches 95% of the population. Most often, clinical signs of pathology occur at the age of 14-18 years.
Typical symptoms of infectious mononucleosis include:
- General weakness and malaise.
- Sore throat and pain when swallowing
- Headache.
- Slight increase in body temperature.
- Sensation of aching in muscles and joints.
- Enlargement and soreness of the lymph nodes in the region of the lower jaw and neck.
Skin rash occurs in less than ¼ of patients. Most often, they occur on the 5th-10th day of the course of the disease against the background of the erroneously prescribed antibiotics ampicillin or amoxicillin.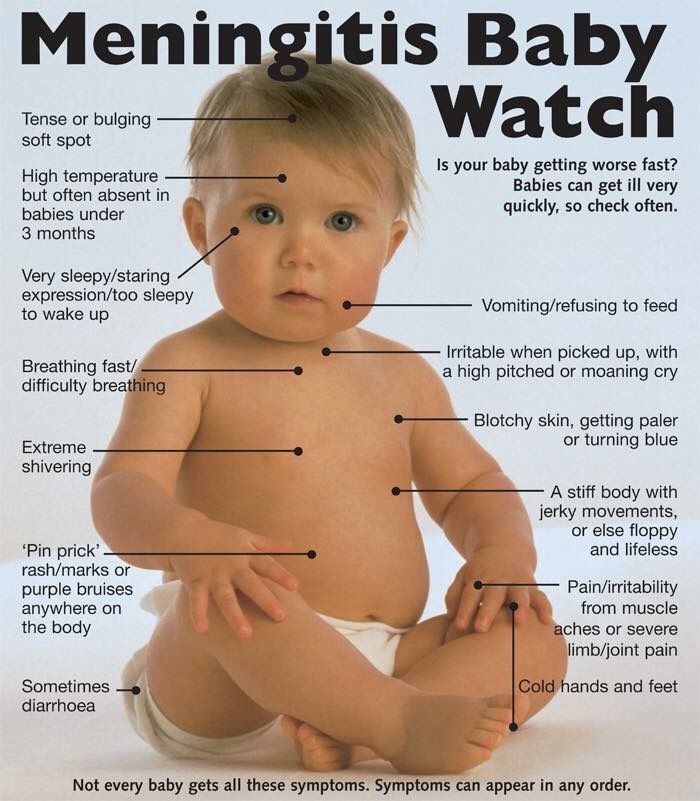 The rash is represented by spots and papules and is located in the face, trunk, thighs and shoulders. It is accompanied by swelling of the skin and itching, sometimes peeling. The rash disappears within 5-7 days.
The rash is represented by spots and papules and is located in the face, trunk, thighs and shoulders. It is accompanied by swelling of the skin and itching, sometimes peeling. The rash disappears within 5-7 days.
Since mononucleosis is of viral origin, antibiotic therapy is not used against it. Treatment of the disease involves the elimination of individual symptoms. In severe cases and with concomitant immunodeficiency, antiherpetic drugs are prescribed: ganciclovir, valaciclovir.
Prevention of rashes
In cases of infectious diseases, the only way to avoid rashes is to prevent infection, namely by limiting contact with sick people and practicing basic personal hygiene.
In case of allergic pathologies, it is important to exclude contact with triggers, and if this is not possible, take antihistamines or corticosteroids previously agreed with the attending physician in advance.
A series of recommendations to help avoid skin rashes of other origin for people with sensitive skin:
- Avoid direct skin contact with aggressive, irritating substances such as household chemicals.
- Limit skin exposure to sunlight, cold.
- Give preference to clothing and underwear made from natural fabrics.
- Avoid tight, uncomfortable clothing and mechanically rough objects such as washcloths.
- Use ointments or other skin care products recommended by a dermatologist or esthetician.
Conclusion
Skin rash is an important symptom of many diseases. She can tell you exactly what kind of disease you have to deal with. This, in turn, makes it possible to provide the right assistance before going to the doctor, avoiding mistakes or even coping with the problem on your own.
References
- Federal Clinical Guidelines. Dermatovenereology 2015. Skin diseases. Sexually transmitted infections. - 5th ed. revised and additional - M: Business Express, 2016. - 768 p.
- V.M. Kozin, Yu.V. Kozina, N.N. Yankovskaya "Dermatological diseases and sexually transmitted infections: Educational and methodological manual" - Vitebsk: VSMU, 2016.
 - 409 p.
- 409 p. - P.D. Walk. "Skin and venereal diseases: Textbook" - Grodno: Grodno State Medical University, 2003. - 182 p.
- Yu.V. Odinets, M.K. Biryukova “Atopic dermatitis, allergic rhinitis, urticaria in children: method. decree. for stud. and interns" - Kharkiv: KhNMU, 2015. - 52 p.
- S. A. Butriy “Child health: a modern approach. How to learn to cope with diseases and your own panic ”-“ Eksmo ”, 2018.
Rash in a child on body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and drugs! We will prescribe only what has proven effective and will help your child.