How does postpartum depression affect child development
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.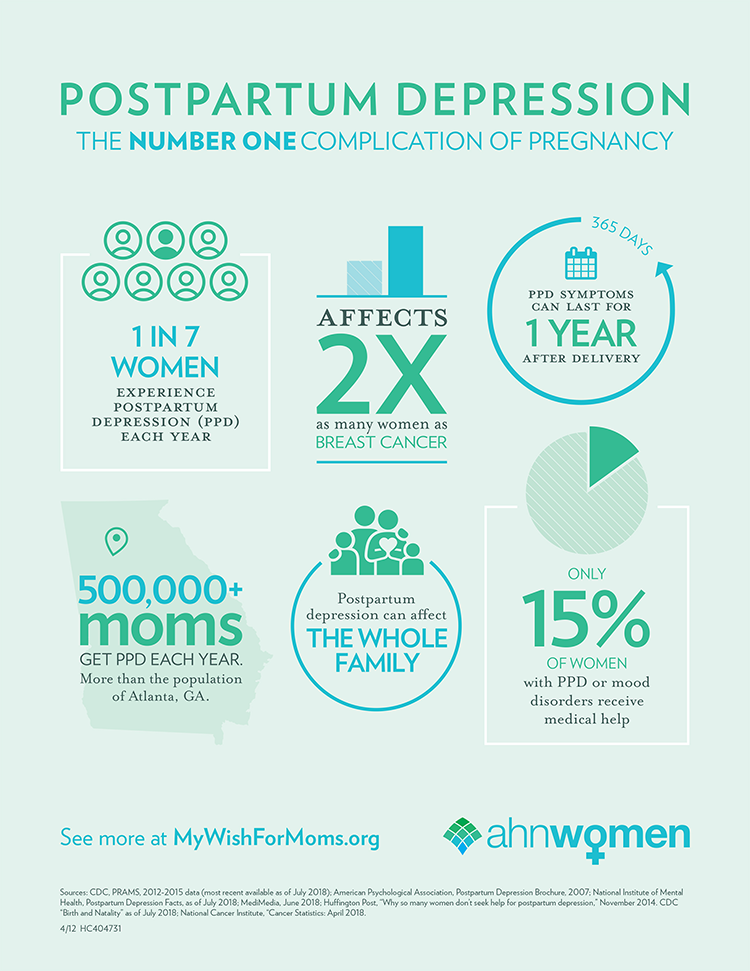 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery.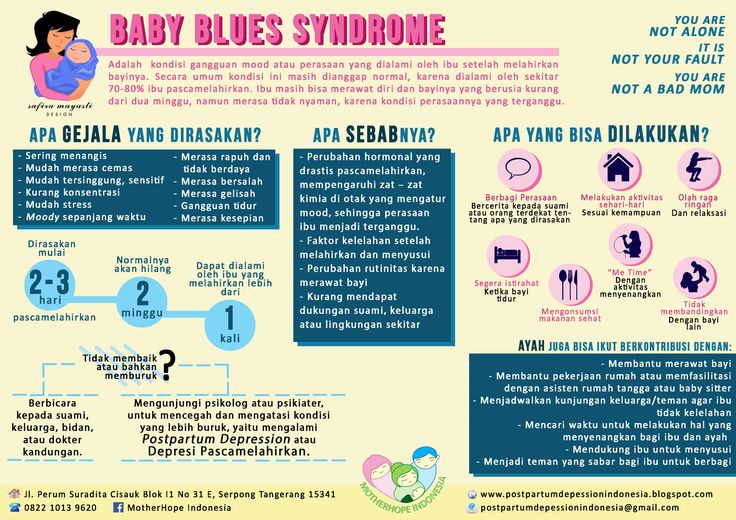 Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.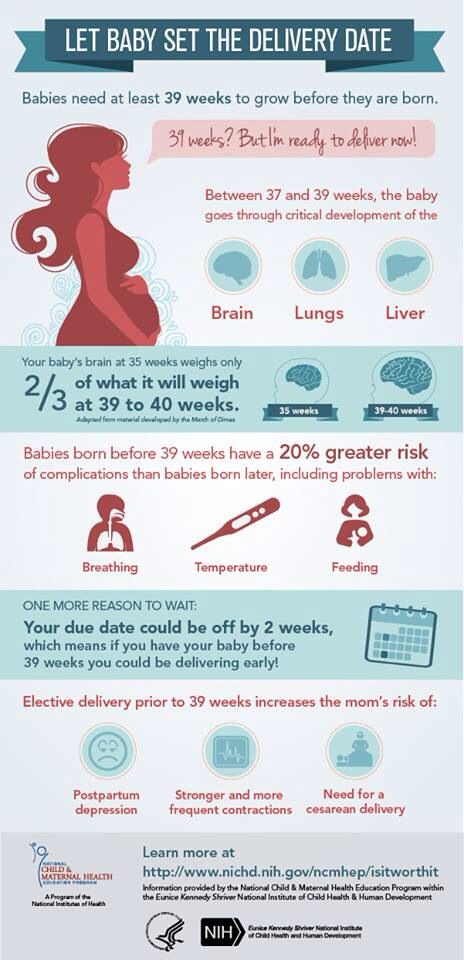
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Postpartum depression – nakedheart.online
What is postpartum depression – is it a diagnosis, a disease that needs to be treated?
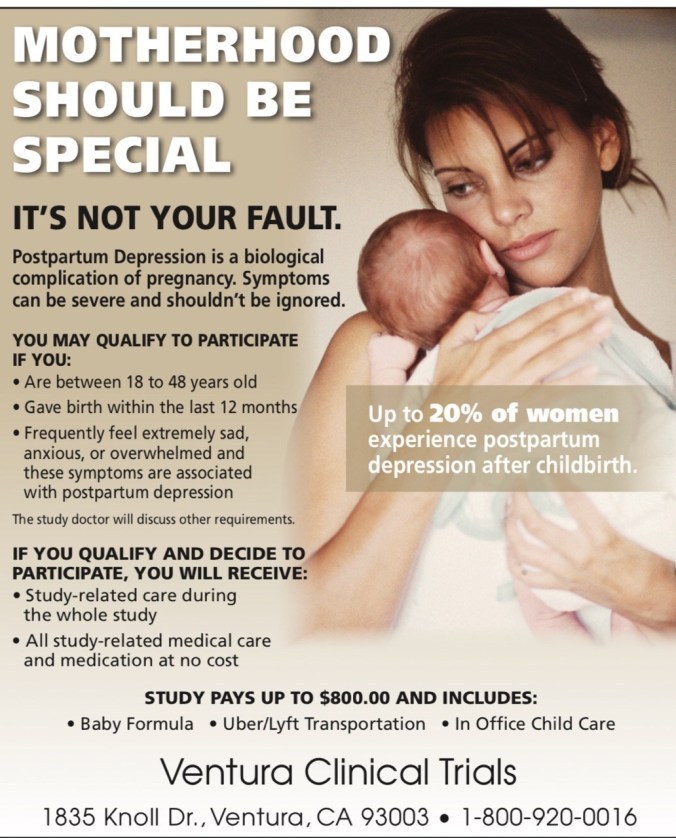
Postpartum depression is a clinical diagnosis associated with the fact that a lot of things change with the birth of a child. Scientific studies suggest that its prevalence is from 10 to 15%, which is quite a lot. At the same time, there is another condition: “baby blues”, or “sad mom syndrome”. This is just a condition, not a diagnosis. It is experienced, according to various sources, from 60 to 80% of mothers.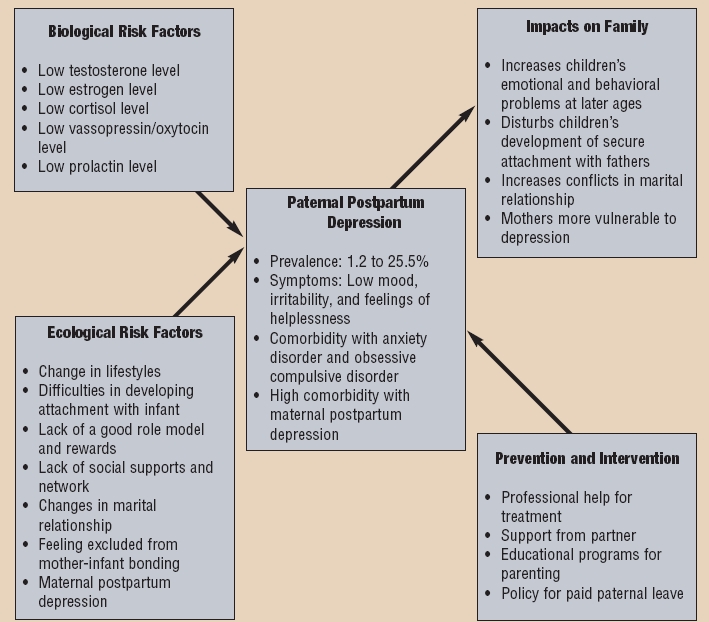 It is associated with low mood, fatigue, tearfulness, it appears quite quickly after childbirth (on the third or fourth day), but it goes away just as quickly, does not require special help, if it does not develop into depression. The main thing is to know that this is not the woman’s fault, you need to take it calmly, you need support, you need to be all together. This is part of the normal process of bringing a new person into the world.
It is associated with low mood, fatigue, tearfulness, it appears quite quickly after childbirth (on the third or fourth day), but it goes away just as quickly, does not require special help, if it does not develop into depression. The main thing is to know that this is not the woman’s fault, you need to take it calmly, you need support, you need to be all together. This is part of the normal process of bringing a new person into the world.
How can you tell if it's depression or just "sad mommy syndrome" for the time being?
This condition lasts from two to four weeks, then it passes, and the woman returns to her normal mood, functioning, etc. Depression is usually put after the third or fourth week, this is a protracted long-term condition.
What are the symptoms of depression? What should mom pay attention to?
Feeling of sadness, low mood, lack of pleasure and loss of interest in what used to interest. Very little energy, chronic fatigue, difficulty sleeping.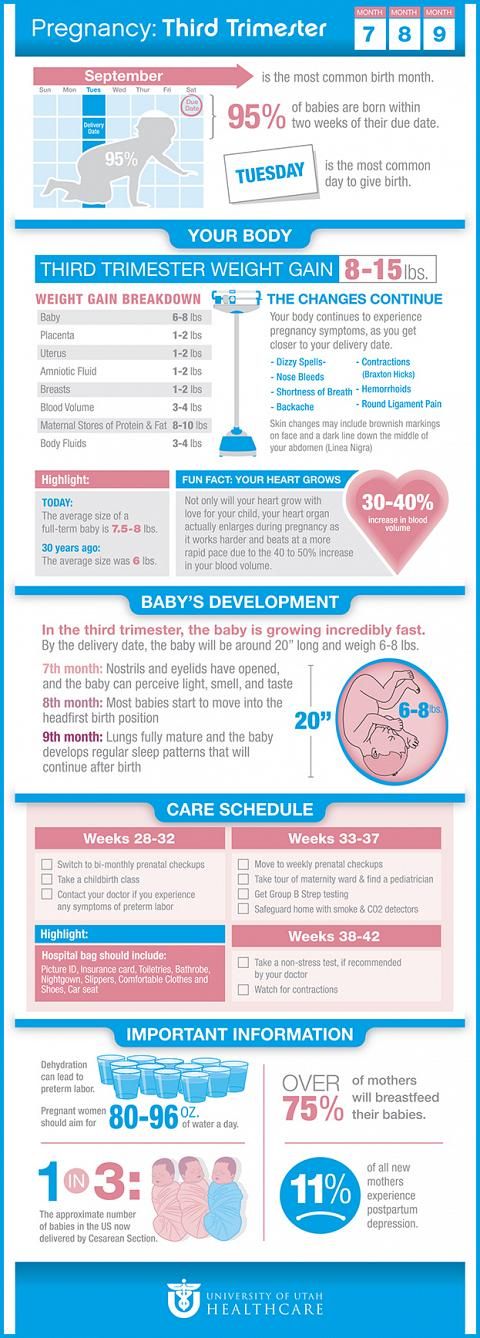 There are difficulties in caring for a child. There are difficulties with concentration, with making decisions, and a lot of negative, frightening thoughts.
There are difficulties in caring for a child. There are difficulties with concentration, with making decisions, and a lot of negative, frightening thoughts.
How does it happen that the father or the adoptive parents develop depression?
Research shows that depression is not only related to hormones, because it affects adoptive parents too. The child is simply taken into the family, and this causes the onset of postpartum depression. That is, the hormonal background affects, but the appearance of a new member in the family is very important in itself. Since the adoptive parents are described as depressed, and not all adoptive parents take babies in the first days of life, we can talk about the adoptive parent's depression, even when he takes a three-five-year-old child. This is a huge event in the life of a family, when the structure of the family changes suddenly and at once. It affects our hormonal state and brain chemistry.
How terrible is this depression for a child?
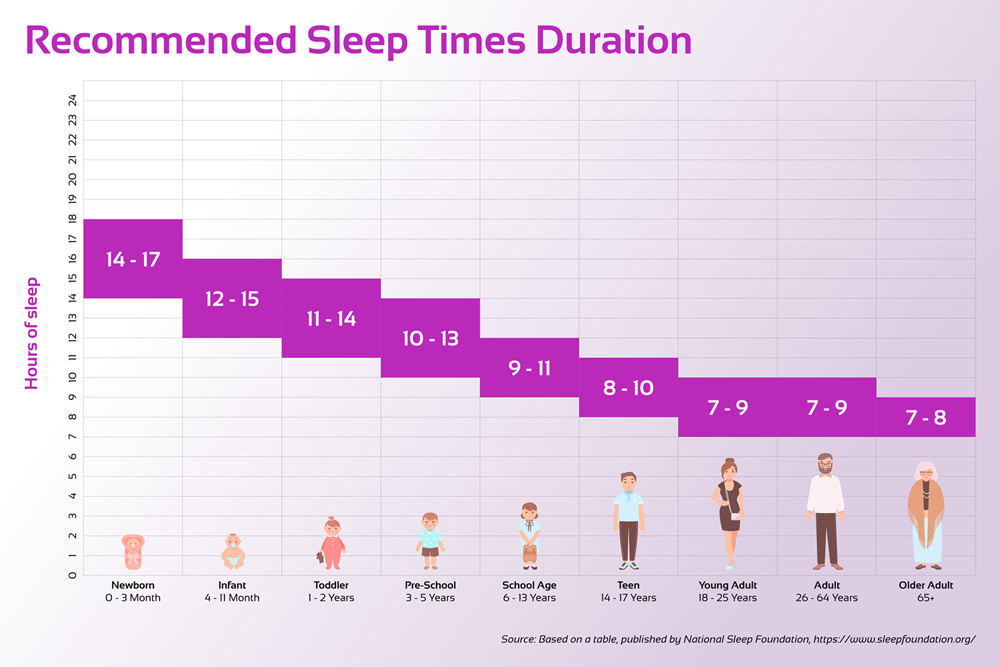
Depression correlates with future difficulties in raising a child.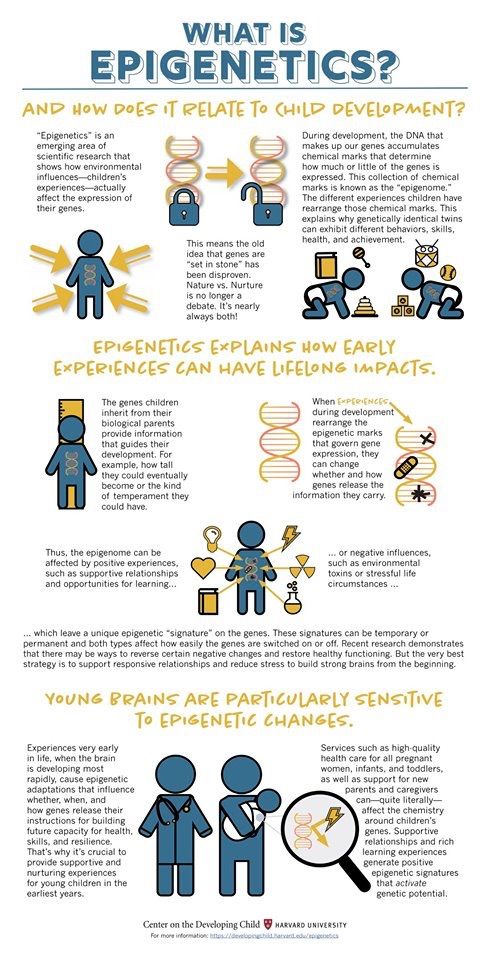 The child may develop eating disorders, sleep disorders, delayed speech development, etc. In general, depression affects the bonding between parent and child. This occurs because the normal attachment cycle is disrupted. When a person is depressed, it is harder for them to respond to the child's signals. And in the first weeks after birth, a child experiences a huge need for his signals to be answered. From this, basic security is formed, on which all mental development is further built. And of course, if parents experience postpartum depression, it is more difficult for them to respond to the signals of the child, because they feel tired or exhausted, too sleepy, more irritable. This is an important point when existing resources must come together to help the child. But, if the mother is left alone and experiences extensive symptoms of depression, this can negatively affect the development of the child in the future.
The child may develop eating disorders, sleep disorders, delayed speech development, etc. In general, depression affects the bonding between parent and child. This occurs because the normal attachment cycle is disrupted. When a person is depressed, it is harder for them to respond to the child's signals. And in the first weeks after birth, a child experiences a huge need for his signals to be answered. From this, basic security is formed, on which all mental development is further built. And of course, if parents experience postpartum depression, it is more difficult for them to respond to the signals of the child, because they feel tired or exhausted, too sleepy, more irritable. This is an important point when existing resources must come together to help the child. But, if the mother is left alone and experiences extensive symptoms of depression, this can negatively affect the development of the child in the future.
Postpartum depression: the brain and hormones
What causes postpartum depression? What about evolution and mammals? How do hormones affect depression? Can she pass by herself? How long does postpartum depression last? Does depression in a mother affect the child and the entire sphere of family relationships? Neuroscientist Vyacheslav Dubynin, professor at Moscow State University, who has been studying postpartum depression for more than 15 years, answers these and other questions.
Why does postpartum depression occur? It is generally accepted that a long-awaited child should become a source of positive emotions and happiness. So why do many parents experience completely different emotions instead of joy and love: fatigue, fear, anxiety, indifference?
Unfortunately, there is no single answer to this question. This does not mean that there are no answers at all. However, they are not so simple and require taking into account a whole range of factors. The most important of them: a sharp change in the hormonal state of the mother, stress during pregnancy, the initial depressive status of the woman's nervous system.
How is postpartum depression studied?
The professional community regularly discusses both common and unusual cases of PPD (abbreviation - from the English " postpartum depression ", postpartum depression). Psychologists, endocrinologists, neuroscientists are making great efforts to investigate and solve this problem.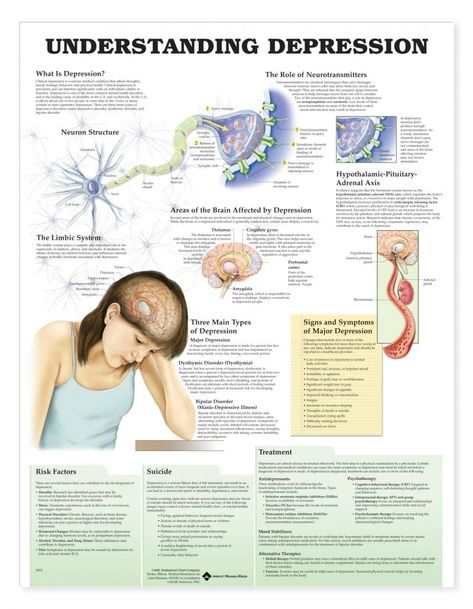 For example, in the laboratory of the Department of Physiology, Faculty of Biology, Moscow State University, many works are devoted to modeling and simulating postpartum depression in experimental animals.
For example, in the laboratory of the Department of Physiology, Faculty of Biology, Moscow State University, many works are devoted to modeling and simulating postpartum depression in experimental animals.
Postpartum depression is very common and affects more than just women. It may turn out to be news for someone: postpartum depression in men * also happens, albeit 2-3 times less often and usually in a less acute form, but this is a medical fact.
How has evolution affected parenthood?
Parental behavior and maternal care programs ( maternal care, parental care ) appeared in the course of evolution not so long ago. For hundreds of millions of years, the main way to protect offspring was to keep fertilized eggs in a safe place. However, in warm-blooded animals, caring for offspring becomes an absolute necessity: without a mother and father, a chick or a baby mammal will definitely freeze, will not be able to properly feed itself and will die.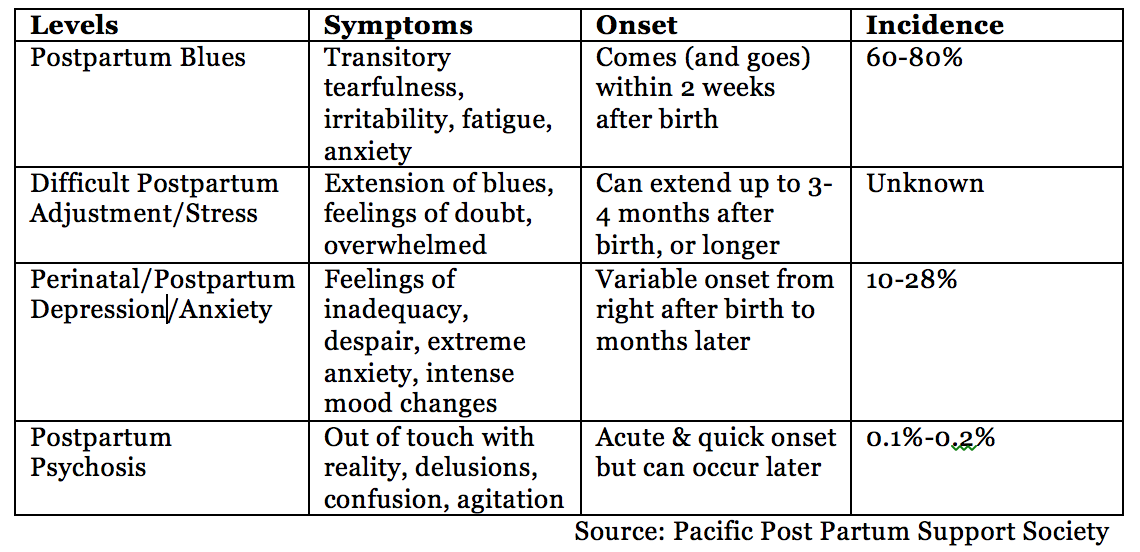
The mother's brain immediately after birth must competitively suppress motivations related to food, safety, protection of personal territory; suppress programs of laziness, which in neuroscience are called "power saving algorithms."
Imagine a mother rat: she lived for herself, lived - and suddenly naked, blind, helpless pink lumps are born. At this moment, her nervous system changes its activity very dramatically! The brain must understand: pink lumps are not food, not a danger, but an object of constant care, care, protection. This reformatting is usually quite fast and reliable. However, "very" does not mean "always". Most often, problems arise in relation to the "firstborn". The female can lose some of the newborns, feed them poorly, or even eat them altogether.
Thus, the symptoms of postpartum depression can be observed, provoked, investigated in animal experiments. And this is an important key to understanding what happens in the case of PPD in a woman's body.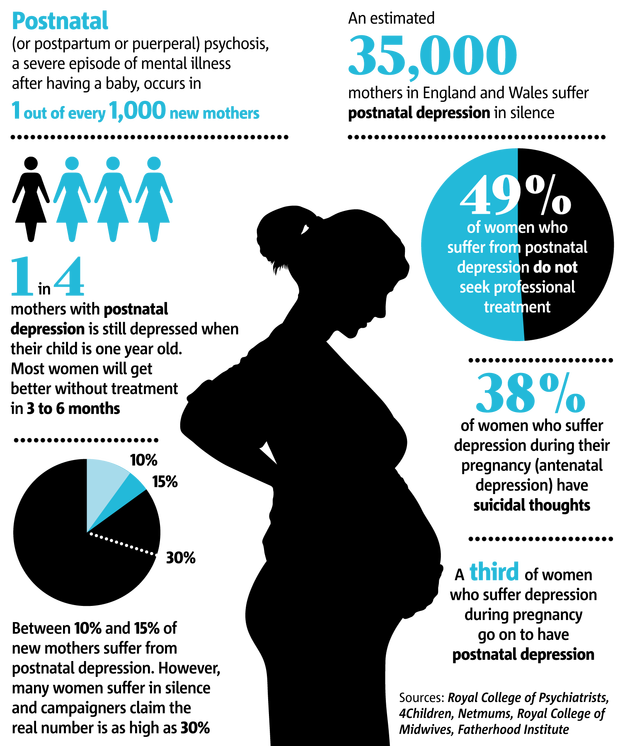
What changes in the body of a young mother?
By the time of the first birth, a young mother does not yet have the experience of caring for offspring, and her brain tries to find the right behavioral responses, based on innate knowledge and programs.
To start maternal behavior, serious hormonal changes are required, in which oxytocin and prolactin play a key activating role. In parallel, the effect of the so-called "hormonal withdrawal" develops, which to a large extent provokes PRD.
And it's not always the first birth; you can feel the clear signs of PPD on the second-third-fifth time.
What to do if postpartum depression occurs?
There are two good news.
First, the symptoms of postpartum depression can be controlled on a conscious level. To do this, it is very important to have information about the PRD itself, because whoever is warned is protected. The biggest problem is women's low awareness of postpartum depression.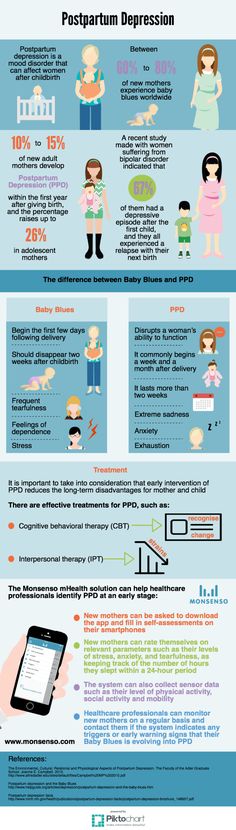 A young mother may perceive her depression as something unique, happening only to her and through her fault. And this is not so. World statistics show: within 4-6 weeks after the birth of a child, individual depressive symptoms are recorded in approximately 50% of mothers; serious depressive states - in 10-15%. **
A young mother may perceive her depression as something unique, happening only to her and through her fault. And this is not so. World statistics show: within 4-6 weeks after the birth of a child, individual depressive symptoms are recorded in approximately 50% of mothers; serious depressive states - in 10-15%. **
The second good news is that there are many ways to help a woman in this condition. Here it is important not to hide anything from relatives and friends, from doctors and psychologists. And then you will definitely receive the necessary support already at the very first symptoms of depression.
Can postpartum depression go away on its own?
The probability is very high. It is due to the compensatory action on the anterior hypothalamus of prolactin and oxytocin. These hormones are released into the blood not only during pregnancy and childbirth, but also during breastfeeding.
When a baby suckles the mother's breast, signals of mechanical stimulation of the nipple reach the pituitary gland. And the pituitary gland increases the secretion of prolactin so that there is more milk, as well as oxytocin, so that the ducts of the mammary glands contract more actively. At the same time, these hormones stimulate the centers of parental motivation, causing positive emotions. All this stabilizes the system called "mother-baby", allows you to turn child care into a long-term and positive process.
And the pituitary gland increases the secretion of prolactin so that there is more milk, as well as oxytocin, so that the ducts of the mammary glands contract more actively. At the same time, these hormones stimulate the centers of parental motivation, causing positive emotions. All this stabilizes the system called "mother-baby", allows you to turn child care into a long-term and positive process.
Mom's body gradually adapts to low concentrations of progesterone and estrogen, nervous processes normalize and life returns to its usual rhythm. Not only breastfeeding helps, but also constant interaction with the baby. The brain of an adult is arranged in such a way that the visual image of a baby, its smell, the sounds it makes at an innate, unconscious level “reach out” to the anterior hypothalamus. A state of tenderness develops, or, as they say now, the “mimimi effect”. Moreover, both in women and in men: after all, for the biological species Homo sapien s, it is characteristic that both parents take care of the offspring (“ biparental car e").
What to do if postpartum depression persists?
If the symptoms of PPD do not disappear and even intensify, turning not into postpartum, but into “normal” severe depression, you definitely cannot do without the help of specialists. However, there are cases when an attentive husband, observing the state of his wife, literally forcibly kicked her out on a week-long vacation - this allowed the young mother to break the vicious circle of accumulation of negative emotions and nervousness, return to normal life and positive interaction with the baby.
If postpartum depression lasts for a long time, more than one and a half to two months, it is absolutely necessary to contact doctors and psychotherapists. There is a well-established system of psychological support that will not leave you alone with the problem. You can seek help through children's clinics, antenatal clinics, through psychological assistance services.
In addition, there are modern, sparing medications, what exactly to use should be decided by the specialist after taking.