Urinary infections pregnancy
Urinary Tract Infection In Pregnancy - StatPearls
Patricia J. Habak; Robert P. Griggs, Jr.
Author Information and Affiliations
Last Update: July 5, 2022.
Continuing Education Activity
Urinary tract infections (UTIs) are frequently encountered in pregnant women. Pyelonephritis is the most common serious medical condition seen in pregnancy and may present similarly and may even result from inadequate treatment of urinary tract infections. Thus, it is crucial for providers to be able to distinguish normal versus abnormal findings of both the urinary tract and kidneys, evaluate abnormalities, and treat disease. Fortunately, urinary tract infections in pregnancy are usually easy to treat and respond well to treatment. This activity reviews the evaluation and management of urinary tract infection in pregnancy and highlights the role of interprofessional team members in collaborating to provide well-coordinated care and enhance outcomes for affected patients.
Objectives:
Identify the etiology of urinary tract infections pregnancy.
Explain how to diagnose urinary tract infections in pregnant patients.
Summarize the treatment options available for urinary tract infections in pregnant patients.
Review interprofessional team strategies for improving care and outcomes in pregnant patients with urinary tract infections.
Access free multiple choice questions on this topic.
Introduction
Urinary tract infections (UTIs) are frequently encountered in pregnant women. Pyelonephritis is the most common serious medical condition seen in pregnancy. Thus, it is crucial for providers of obstetric care to be knowledgeable about normal findings of the urinary tract, evaluation of abnormalities, and treatment of disease. Fortunately, UTIs in pregnancy are most often easily treated with excellent outcomes. Rarely, pregnancies complicated by pyelonephritis will lead to significant maternal and fetal morbidity.
Changes of the urinary tract and immunologic changes of pregnancy predispose women to urinary tract infection. Physiologic changes of the urinary tract include dilation of the ureter and renal calyces; this occurs due to progesterone-related smooth muscle relaxation and ureteral compression from the gravid uterus. Ureteral dilation may be marked. Decreased bladder capacity commonly results in urinary frequency. Vesicoureteral reflux may be seen. These changes increase the risk of urinary tract infections.
Etiology
During pregnancy, urinary tract changes predispose women to infection. Ureteral dilation is seen due to compression of the ureters from the gravid uterus. Hormonal effects of progesterone also may cause smooth muscle relaxation leading to dilation and urinary stasis, and vesicoureteral reflux increases. The organisms which cause UTI in pregnancy are the same uropathogens seen in non-pregnant individuals. As in non-pregnant patients, these uropathogens have proteins found on the cell-surface which enhance bacterial adhesion leading to increased virulence. Urinary catheterization, frequently performed during labor, may introduce bacteria leading to UTI. In the postpartum period, changes in bladder sensitivity and bladder overdistention may predispose to UTI.
Urinary catheterization, frequently performed during labor, may introduce bacteria leading to UTI. In the postpartum period, changes in bladder sensitivity and bladder overdistention may predispose to UTI.
Pregnancy is a state of relative immunocompromise. This immunocompromise may be another cause for the increased frequency of UTIs seen in pregnancy.
Epidemiology
The most significant factor predisposing women to UTI in pregnancy is asymptomatic bacteriuria (ASB). ASB is defined as more than 100,000 organisms/mL on a clean catch urinalysis obtained from an asymptomatic patient. If asymptomatic bacteriuria is untreated in pregnancy, the rate of subsequent UTI is approximately 25%.[1] Due to both to the high rate and potential seriousness of pyelonephritis, it is recommended that all pregnant women be screened for ASB at the first prenatal visit. This is most often done with a clean catch urine culture. Treatment of ASB decreases the rate of clinical infection to 3% to 4%.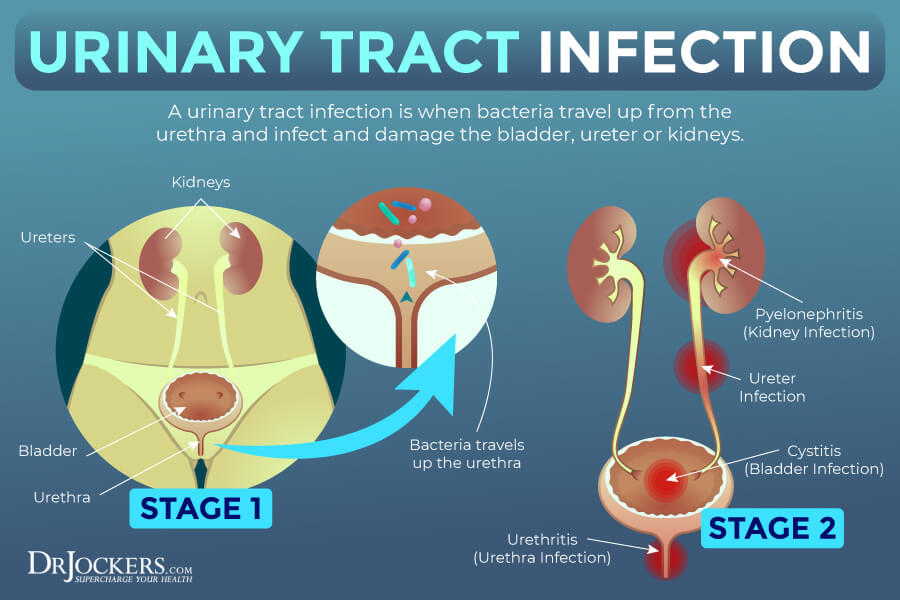
The rate of asymptomatic bacteriuria in non-pregnant women is 5% to 6% which compares similarly to estimated rates in pregnancy of 2% to 7%. ASB is seen more frequently in parous women and women of low socioeconomic status. Women who are carriers for sickle cell trait also have a higher incidence of ASB.[1]
UTIs are a common cause of serious infection in pregnant women. In one study, 3.5% of antepartum admissions were due to UTI.[2] Pyelonephritis is the most common cause of septic shock in pregnant women. Risk factors for UTIs in pregnancy include low socioeconomic status, young age, and nulliparity. As with ASB some patients may be predisposed to infection and may report a history of having had ASB, cystitis or pyelonephritis in the past. Pyelonephritis is more often right-sided however may be bilateral in up to 25% of cases.
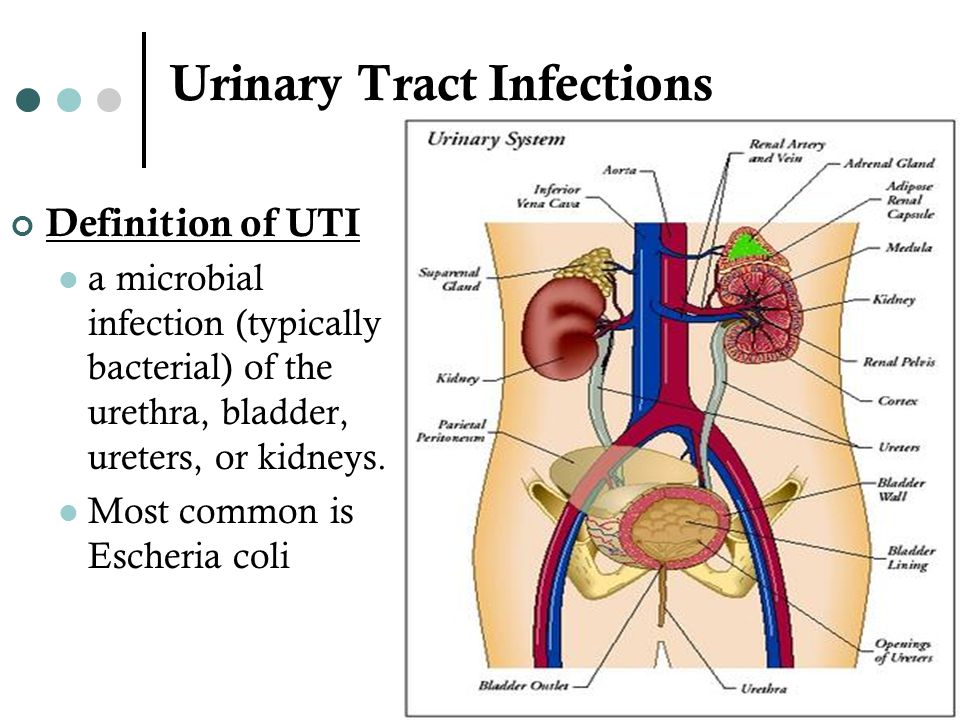
Pathophysiology
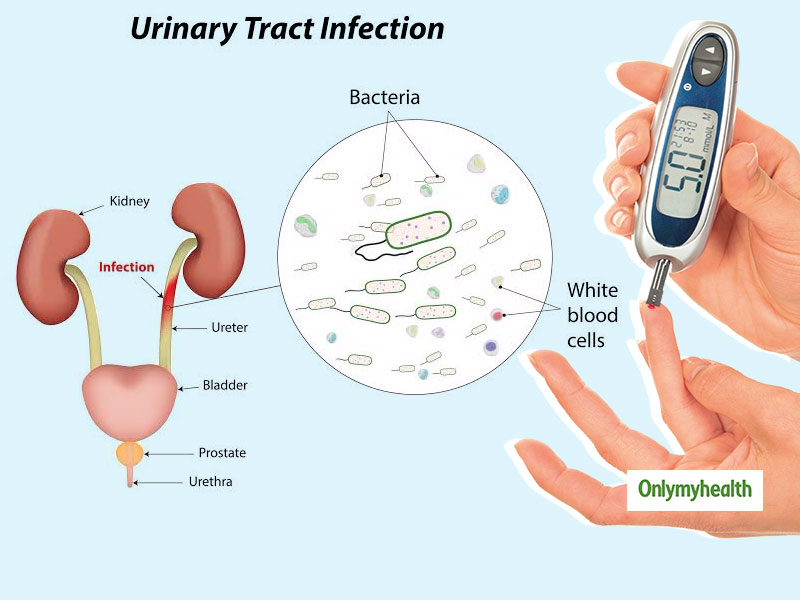
Organisms causing UTI in pregnancy are the same uropathogens which commonly cause UTI in non-pregnant patients. Escherichia coli is the most common organism isolated.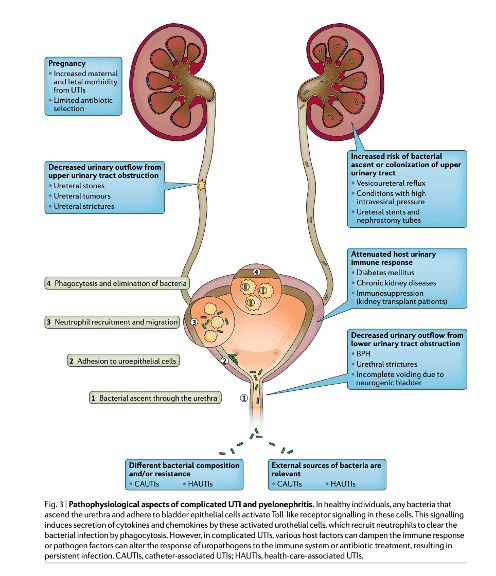 An 18-year retrospective analysis found E. coli to be the causative agent in 82.5% of cases of pyelonephritis in pregnant patients.[3] Other bacteria which may be seen include Klebsiella pneumoniae, Staphylococcus, Streptococcus, Proteus, and Enterococcus species.
An 18-year retrospective analysis found E. coli to be the causative agent in 82.5% of cases of pyelonephritis in pregnant patients.[3] Other bacteria which may be seen include Klebsiella pneumoniae, Staphylococcus, Streptococcus, Proteus, and Enterococcus species.
History and Physical
Patients with asymptomatic bacteriuria have no symptoms; thus, it is important to screen for the disease. These patients may have a history of frequent UTI or may have experienced ASB in a prior pregnancy.
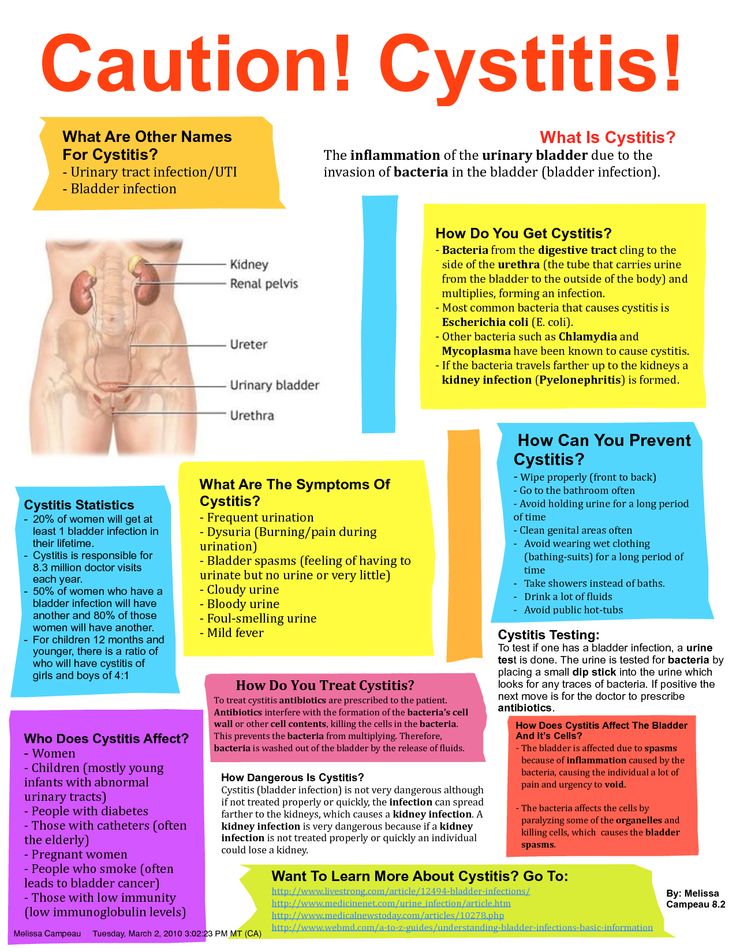
Cystitis presents with the same symptoms seen in non-pregnant individuals. Symptoms may include pain or burning with urination (dysuria), urinary frequency or urinary urgency. Suprapubic pain and tenderness may be noted.
Likewise, patients with pyelonephritis exhibit symptoms seen in non-pregnant patients with the same disease. Symptoms may include flank pain, fever, and chills. Non-specific symptoms such as malaise, anorexia, nausea, and vomiting may be reported thus the differential diagnosis on initial presentation is often broad. Differential diagnosis includes acute intraabdominal processes such as appendicitis, cholecystitis, and pancreatitis as well as pregnancy complications including preterm labor and placental abruption. Patients may report contractions or contractions may be seen with uterine monitoring. This uterine activity often is due to smooth muscle irritability caused by infection. Patients should be assessed, and if cervical dilation is not found, treatment is typically not needed for preterm labor. Patients should be monitored closely however as preterm labor may develop.
Differential diagnosis includes acute intraabdominal processes such as appendicitis, cholecystitis, and pancreatitis as well as pregnancy complications including preterm labor and placental abruption. Patients may report contractions or contractions may be seen with uterine monitoring. This uterine activity often is due to smooth muscle irritability caused by infection. Patients should be assessed, and if cervical dilation is not found, treatment is typically not needed for preterm labor. Patients should be monitored closely however as preterm labor may develop.
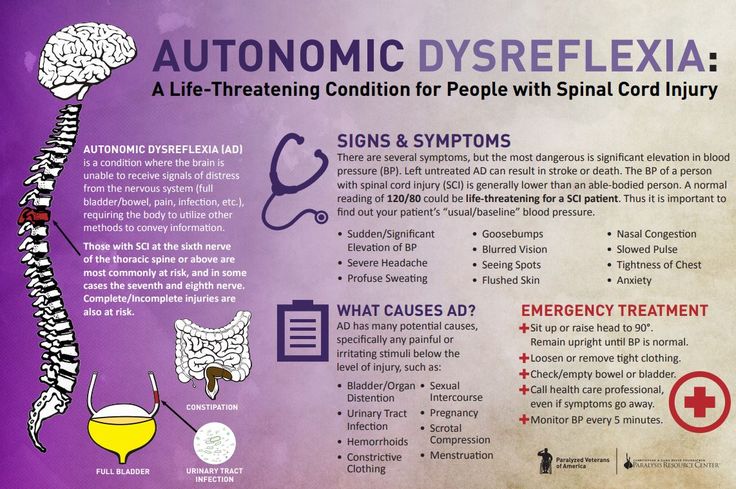
Signs and symptoms of sepsis may be present. These include tachycardia and hypotension. Such patients require prompt evaluation and interventions.
A full physical examination should be performed with special attention to vital signs and exam of the heart and lungs. An abdominal exam may reveal tenderness, and costovertebral tenderness is usually able to be elicited. A genitourinary (GU) exam should be performed to assess for cervical infection and assess cervical dilation on admission.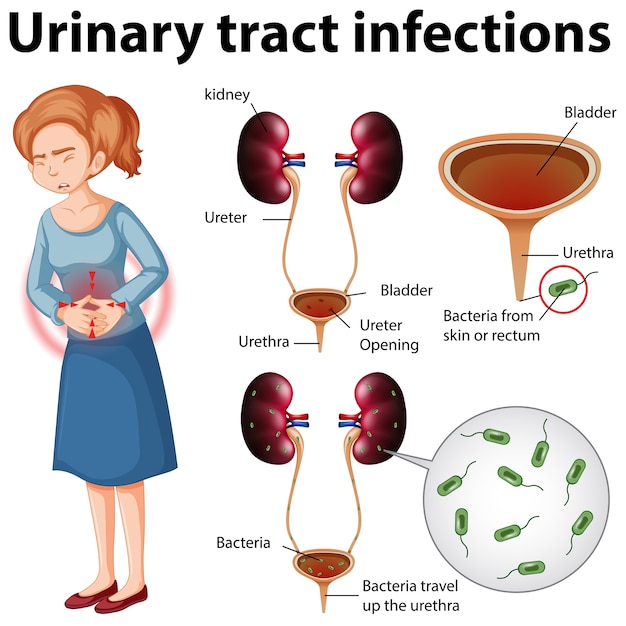 Even when pregnancy complications are not a concern initially, it is still reasonable to evaluate if contractions or other abnormalities occur during hospitalization.
Even when pregnancy complications are not a concern initially, it is still reasonable to evaluate if contractions or other abnormalities occur during hospitalization.
Evaluation
Evaluation will include urinalysis and clean catch urine culture. In the collection of urinary specimens in pregnancy a few considerations are noteworthy. Patients who are well hydrated may excrete dilute urine rendering some assessed parameters to be less accurate. Hematuria may be seen as a result of contamination, particularly when specimens are collected from laboring or postpartum patients. Due to reduced reabsorption of protein, small amounts of protein may normally be excreted. Contamination, as may occur with mucous discharge, may also contribute to the presence of proteinaceous material in the urine of pregnant women.
Laboratory analysis should include complete blood count (CBC), electrolytes and serum creatine. Tailored studies should be included as appropriate to exclude other causes of patient symptoms, for example, amylase and lipase if pancreatitis is being considered as a diagnosis. If there is a concern for sepsis lactic acid and blood cultures should be obtained. All cultures should be obtained as soon as possible and before starting antibiotic therapy.
If there is a concern for sepsis lactic acid and blood cultures should be obtained. All cultures should be obtained as soon as possible and before starting antibiotic therapy.
When the fetus is viable, fetal heart rate and contraction monitoring should occur. Consideration should be given to obtaining cervical and GBS cultures on admission if pregnancy-related complications develop. Infrequently, renal ultrasound may be indicated to assess for a possible renal abscess.
Treatment / Management
ASB and acute cystitis are treated with antibiotic therapy. Antibiotic choice can be tailored based on organism sensitivities when available from urine culture results. One-day antibiotic courses are not recommended in pregnancy, although 3-day courses are effective.[4] Antibiotics commonly used include amoxicillin, ampicillin, cephalosporins, nitrofurantoin, and trimethoprim-sulfamethoxazole. Fluoroquinolones are not recommended as a first-line treatment in pregnancy due to conflicting studies regarding teratogenicity.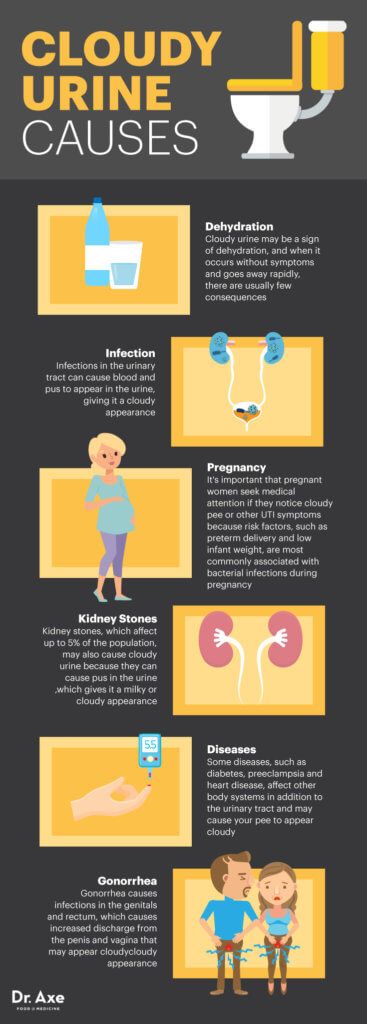 Short courses are unlikely to be harmful to the fetus, and thus, it is reasonable to use this class of drugs with resistant or recurrent infections.
Short courses are unlikely to be harmful to the fetus, and thus, it is reasonable to use this class of drugs with resistant or recurrent infections.
Recently evidence has developed suggesting a link between the use of sulfa derivatives and nitrofurantoin and congenital disabilities when these medications are prescribed in the first trimester. These studies have had limitations; however, it is currently recommended to avoid the use of these medications in the first trimester when alternatives are available.[5] Because the potential consequences of untreated UTI in pregnancy are significant, it is reasonable to use these medications when needed as the benefit strongly outweighs the risk of use. Additional cautions exist with respect to these 2 classes of antibiotics. Patients with G6P deficiency should not be prescribed sulfa derivatives or nitrofurantoin as these medications can precipitate hemolysis. In the late third trimester, trimethoprim-sulfamethoxazole should be avoided due to the potential risk for development of kernicterus in the infant following delivery.
If Group B Streptococcus (GBS) is noted on urine culture, patients should receive intravenous (IV) antibiotic therapy at the time of delivery in addition to indicated treatment for ASB or UTI. This is to prevent the development of early-onset GBS sepsis which may occur in the infants of women who are colonized with GBS.
Pyelonephritis in pregnancy is a serious condition usually requiring hospitalization. Once an evaluation has been completed, treatment consists primarily of directed antibiotic therapy and IV fluids to maintain adequate urine output. Fever should be treated with a cooling blanket and acetaminophen as needed. Commonly, second or third generation cephalosporins are used for initial treatment. Ampicillin and gentamicin or other broad-spectrum antibiotics are alternatives. Patients should be monitored closely for the development of worsening sepsis.
Differential Diagnosis
Differential diagnosis includes acute intraabdominal disease such as appendicitis, pancreatitis, or cholecystitis as well as pregnancy-related complications such as preterm labor, chorioamnionitis, or placental abruption.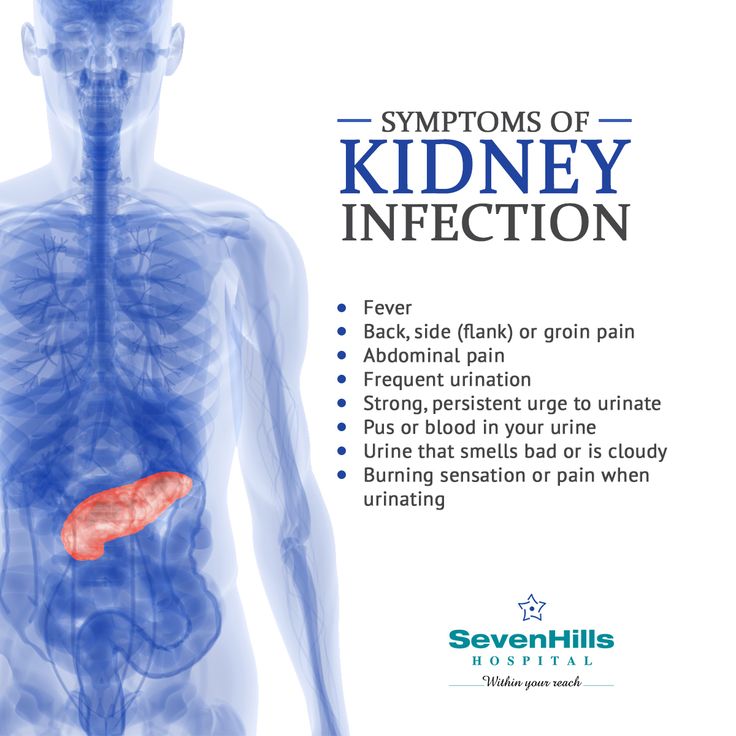
Complications
Patients with pyelonephritis are at risk for several significant complications.
Sepsis may worsen resulting in hypotension, tachycardia, and decreased urine output. ICU admission may be required.
Pulmonary complications are not uncommon, occurring in up to 10% of pregnant patients undergoing treatment for pyelonephritis.[4] This is due to endotoxin-mediated alveolar damage and may manifest as pulmonary edema or acute respiratory distress syndrome (ARDS). Urine output and oxygen status should be monitored closely, and patients may require ICU admission for respiratory support.
Endotoxin release may lead to anemia, this typically resolves spontaneously following treatment. This is the most common complication seen with pyelonephritis occurring in up to 25% of patients.[3]
Endotoxin release may also cause uterine contractions and patients should be monitored for preterm labor; patients should be treated for preterm labor when indicated.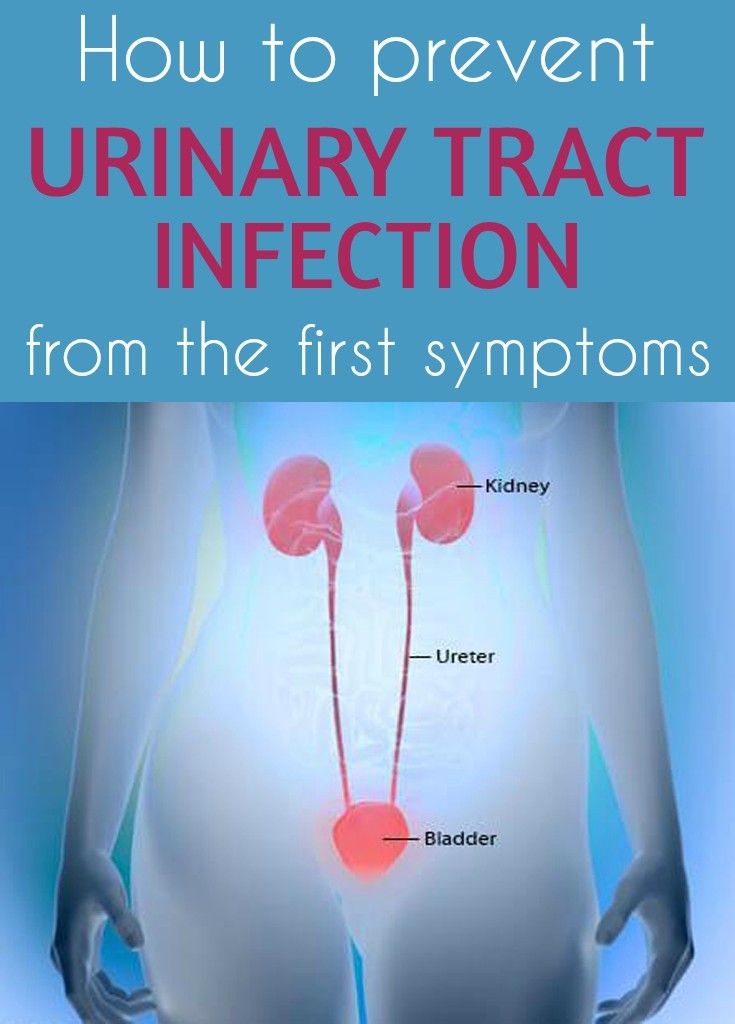 Caution should be exercised in use of tocolytic therapy as the risk of pulmonary edema is increased in the setting of UTI.
Caution should be exercised in use of tocolytic therapy as the risk of pulmonary edema is increased in the setting of UTI.
A small number of patients may experience persistent infection. In these cases, consideration should be given to urinary obstruction or renal abscess. Antibiotic choice should be re-evaluated and culture results reviewed.
Deterrence and Patient Education
After 2 to 4 weeks following completion of treatment, urine culture should be obtained to assure that reinfection has not occurred.
Suppressive antibiotic therapy, usually with nitrofurantoin once daily, is commonly recommended especially in cases where patients have had prior UTI. This is typically continued thru pregnancy and the early postpartum period.
Enhancing Healthcare Team Outcomes
Interprofessional collaboration is crucial in the management of these ill patients. With the administration of antibiotics patients may show initial worsening due to the release of endotoxin, however, most patients improve within 72 hours. Long-term complications such as renal damage are rare.
Long-term complications such as renal damage are rare.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Gilstrap LC, Ramin SM. Urinary tract infections during pregnancy. Obstet Gynecol Clin North Am. 2001 Sep;28(3):581-91. [PubMed: 11512502]
- 2.
Gazmararian JA, Petersen R, Jamieson DJ, Schild L, Adams MM, Deshpande AD, Franks AL. Hospitalizations during pregnancy among managed care enrollees. Obstet Gynecol. 2002 Jul;100(1):94-100. [PubMed: 12100809]
- 3.
Wing DA, Fassett MJ, Getahun D. Acute pyelonephritis in pregnancy: an 18-year retrospective analysis. Am J Obstet Gynecol. 2014 Mar;210(3):219.e1-6. [PubMed: 24100227]
- 4.
Sheffield JS, Cunningham FG. Urinary tract infection in women. Obstet Gynecol. 2005 Nov;106(5 Pt 1):1085-92. [PubMed: 16260529]
- 5.
Committee Opinion No.
 717: Sulfonamides, Nitrofurantoin, and Risk of Birth Defects. Obstet Gynecol. 2017 Sep;130(3):e150-e152. [PubMed: 28832488]
717: Sulfonamides, Nitrofurantoin, and Risk of Birth Defects. Obstet Gynecol. 2017 Sep;130(3):e150-e152. [PubMed: 28832488]
Urinary Tract Infections (UTI) During Pregnancy
Written by WebMD Editorial Contributors
Medically Reviewed by Nivin Todd, MD on September 04, 2022
In this Article
- UTI Symptoms
- Why Are UTIs More Common During Pregnancy?
- UTI Diagnosis
- UTI Treatment During Pregnancy
- UTI Complications During Pregnancy
- UTI Prevention
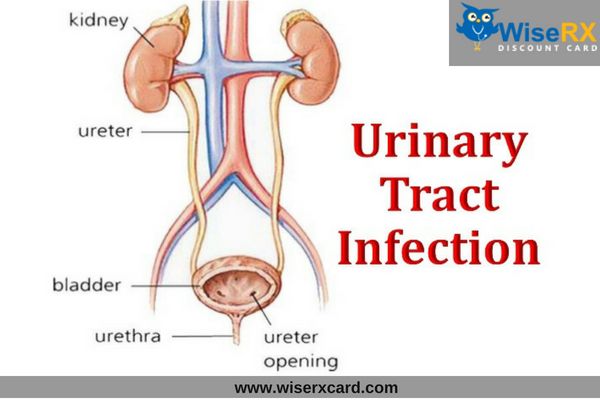
A urinary tract infection (UTI) is an infection of some part of your body's urinary system, which includes your:
- Kidneys
- Ureters (tubes that carries urine from your kidneys to your bladder)
- Bladder
- Urethra (a short tube that carries urine from your bladder to outside your body)
Bacteria cause most UTIs. Anyone can get one, but they're most common in women, and they can be extra concerning if you're pregnant.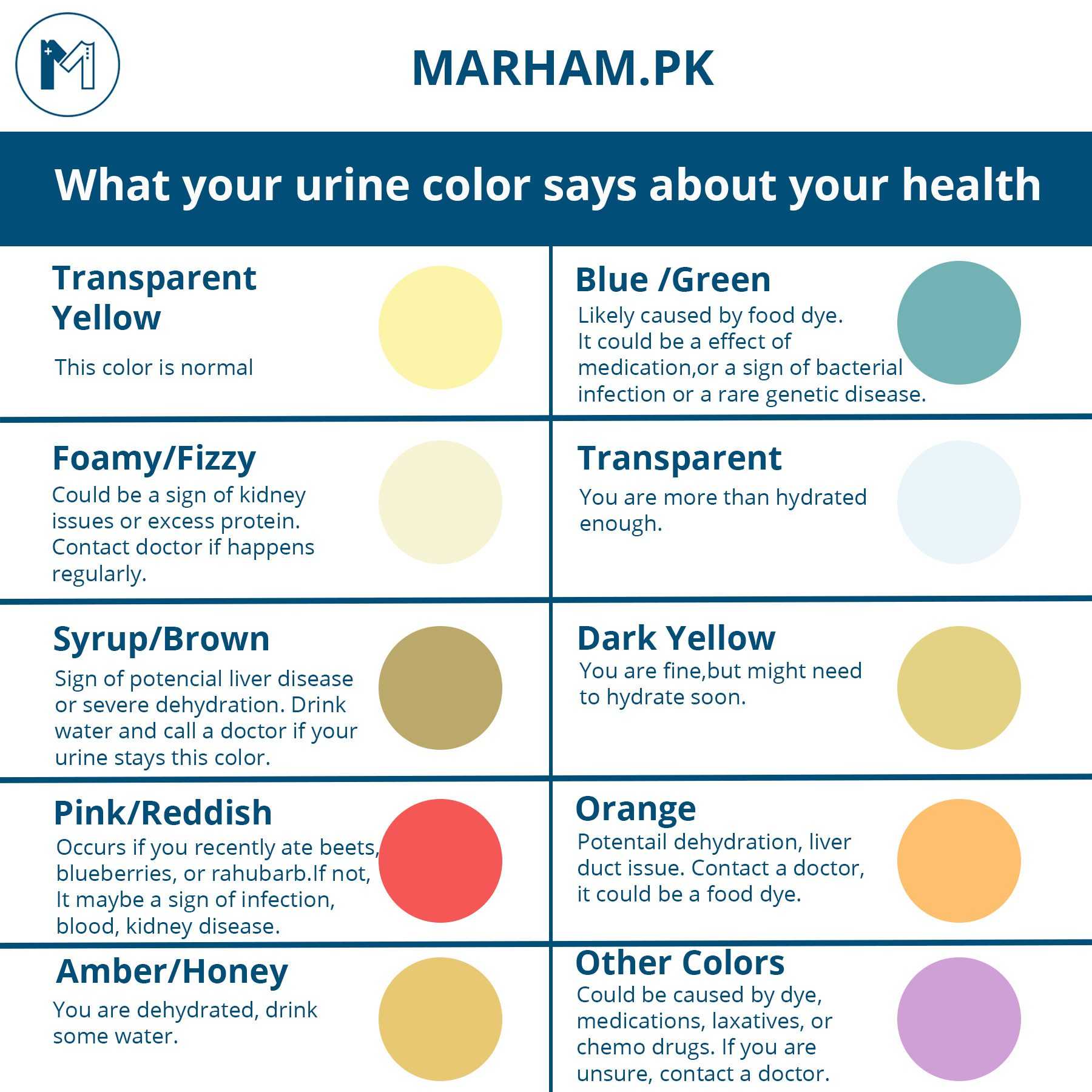
If you think you might have a UTI, tell your doctor. With proper care, you and your baby should be fine.
Usually, these infections are in the bladder and urethra. But sometimes they can lead to kidney infections. If they do, UTIs may lead to preterm labor (giving birth too early) and low birth weight.
UTI Symptoms
If you have a UTI, you may have:
- An urgent need to pee, or peeing more often
- Trouble with peeing
- A burning sensation or cramps in your lower back or lower belly
- A burning feeling when you pee
- Urine that looks cloudy or has an odor
- Blood in your pee, which can turn it red, bright pink, or cola-colored
If you have a kidney infection, you may have:
- Fever
- Nausea
- Vomiting
- Upper back pain, often on just one side
If you have symptoms of a kidney infection, see your doctor right away. Without treatment, the infection can spread into your bloodstream and cause life-threatening conditions.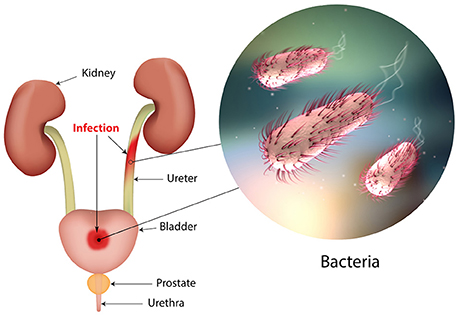
Why Are UTIs More Common During Pregnancy?
Hormones are one reason. In pregnancy, they cause changes in the urinary tract, and that makes women more likely to get infections. Changes in hormones can also lead to vesicoureteral reflux, a condition in which your pee flows back up from your bladder to your kidneys. This can cause UTIs.
When you’re pregnant, your pee has more sugar, protein, and hormones in it. These changes also put you at higher risk for a UTI.
Because you’re pregnant, your growing uterus presses on your bladder. That makes it hard for you to let out all the urine in your bladder. Leftover urine can be a source of infection.
Other causes of UTIs include:
Escherichia coli and other bacteria from your poop. E. Coli is the most common cause of UTIs and can move from your rectum to your urethra if you don’t wipe from front to back.
Sexual activity. Fingers, your partner’s penis, or devices can move bacteria near your vagina into your urethra.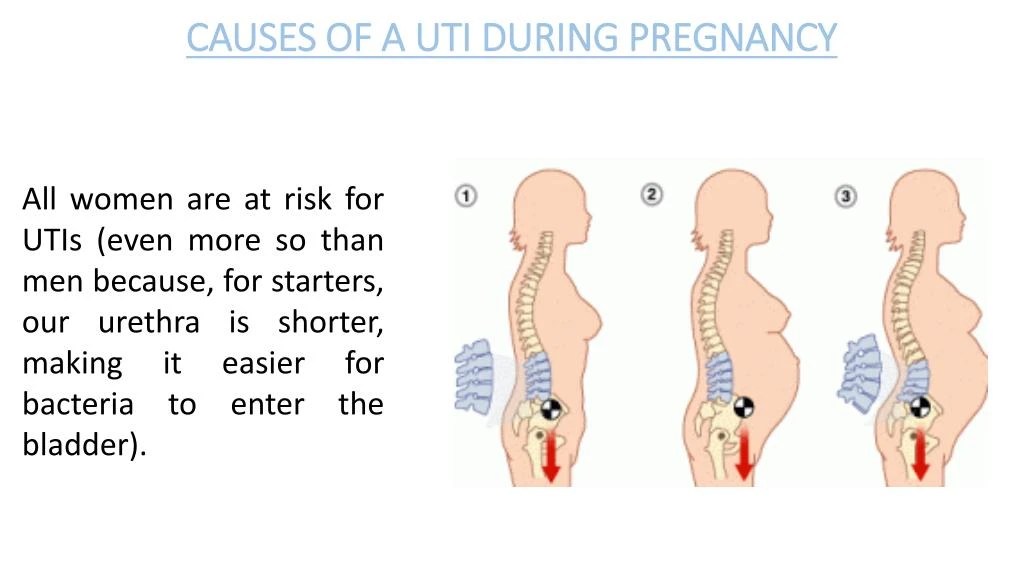
Group B streptococcus. Many women have this bacteria in their colon and vagina. It can cause UTIs and women can pass it to their newborns. Your doctor will test you for this bacteria around weeks 36 to 37 of pregnancy. If you’re positive for group B strep, your doctor will give you IV antibiotics during labor.
UTI Diagnosis
You’ll take a urine test. Your doctor will test it for bacteria and red and white blood cells. A urine culture may also be checked. It shows what kind of bacteria are in the urine.
UTI Treatment During Pregnancy
You’ll take antibiotics for 3 to 7 days or as your doctor recommends. If your infection makes you feel uncomfortable, your doctor will probably start your treatment before you get your urine test results.
Your symptoms should go away in 3 days. Take all of your medication on schedule anyway. Don’t stop it early, even if your symptoms fade.
Many common antibiotics -- amoxicillin, erythromycin, and penicillin, for example -- are considered safe for pregnant women. Your doctor wouldn’t prescribe others, such as ciprofloxacin (Cipro), sulfamethoxazole, tetracycline, or trimethoprim (Primsol, Proloprim, Trimpex), that can affect your baby’s development.
Your doctor wouldn’t prescribe others, such as ciprofloxacin (Cipro), sulfamethoxazole, tetracycline, or trimethoprim (Primsol, Proloprim, Trimpex), that can affect your baby’s development.
UTI Complications During Pregnancy
Pyelonephritis is a UTI that affects the kidneys. If you’re pregnant it can cause:
- Preterm labor
- Severe infection
- Adult respiratory distress syndrome
- Anemia
- Long-term infection
UTI Prevention
To try to avoid getting a UTI:
- Drink at least eight glasses of water a day.
- Wipe yourself from front to back when you go to the bathroom.
- Empty your bladder shortly before and after sex.
- If you need a lubricant when you have sex, choose a water-based one.
- Don't douche.
- Avoid strong feminine deodorants or soaps that cause irritation.
- Wash your genital area with warm water before sex.
- Wear cotton underwear.
- Take showers instead of baths.
- Don’t wear pants that are too tight.
- Pee often.
- Avoid alcohol, citrus juices, spicy food, and caffeinated drinks, which can irritate your bladder.
Urinary tract infections vs pregnancy: treatment and prevention
Summary. Urinary tract infections are one of the most common complications in pregnant women, which can lead to serious consequences not only for the expectant mother, but also for the child. When managing pregnant women with diseases of the urinary system, it is extremely important to choose the right and, most importantly, safe therapeutic tactics. What drugs are safe during pregnancy? What obstetric and therapeutic tactics are most effective for kidney diseases in pregnant women? What diagnostic methods are best used for asymptomatic bacteriuria, acute cystitis and pyelonephritis? Professor 9 spoke about this in her speech0003 Olga Grishchenko , Head of the Department of Perinatology, Obstetrics and Gynecology of the Kharkov Medical Academy of Postgraduate Education during the training workshop for gynecologists "Actual Guidelines of Gynecology, Reproductology, Obstetrics", held on March 29, 2019 in Kharkov. The event was organized by the MedExpert Group of Companies together with the National Medical University named after A.A. Bogomolets and National Medical Academy of Postgraduate Education named after P.L. Shupyk.
The event was organized by the MedExpert Group of Companies together with the National Medical University named after A.A. Bogomolets and National Medical Academy of Postgraduate Education named after P.L. Shupyk.
Urgency of the problem
Urinary tract infections (UTIs) are the most common bacterial infections in outpatient practice, they take the 2nd place, second only to respiratory tract infections. According to statistics, 50% of women in the world have an episode of UTI at least once in their lives, of which 25–40% experience a relapse of the disease within 6–12 months. Every year, about 10% of women develop acute cystitis, and pyelonephritis remains the leading cause of hospitalization during pregnancy for non-obstetric indications.
In the presence of UTI in pregnant women, the risk of preterm labor and rupture of amniotic fluid, chorioamnionitis increases, premature or functionally immature children are born, and the level of perinatal mortality increases.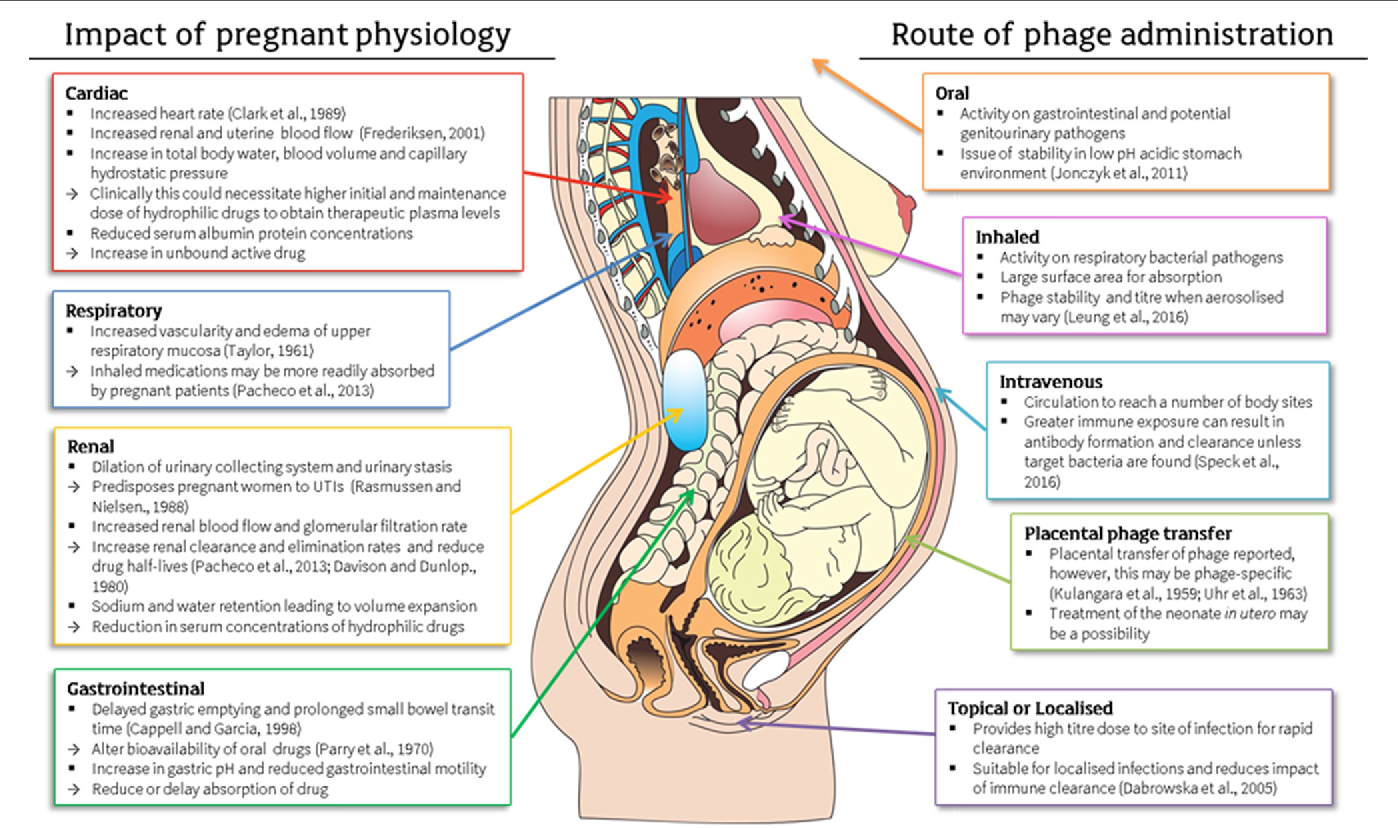
In the structure of UTI, asymptomatic bacteriuria is observed in 4-9.5% of pregnant women, acute pyelonephritis - in 12-25%, chronic pyelonephritis - in 33%, glomerulonephritis, urolithiasis - in 0.1-0.2%.
Risk factors and pregnancy
As a rule, infections, self-medication or improper treatment, asymptomatic bacteriuria, frequent UTIs in combination with inflammatory diseases (colpitis), lifestyle and nutrition can affect the occurrence of pathology of the urinary system.
Pregnant women have an increased risk of diseases of the urogenital tract. A high level of progesterone leads to the development of hypotension, hypokinesia, dyskinesia of the ureters and pyelocaliceal system. In turn, the uterus compresses the ureter, high intra-abdominal pressure occurs, especially in primiparas. During pregnancy, the renal pelvis enlarges, the growing uterus squeezes the ureter more and more, the outflow of urine from the kidneys becomes difficult, the urine stagnates, bacteria multiply in it, and inflammation easily occurs.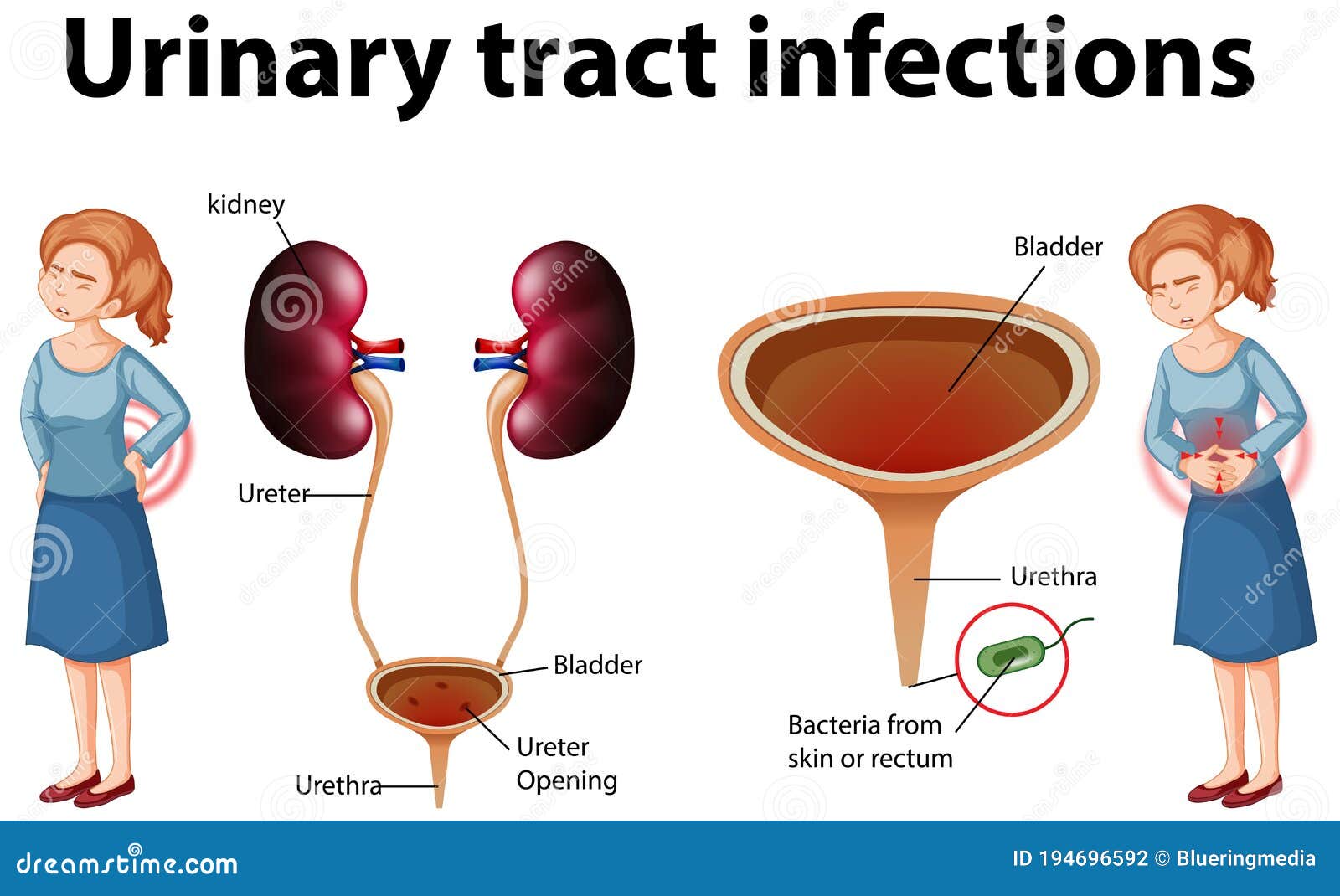
Infectious agents can enter the bladder by ascending (with inflammatory diseases of the urethra), descending (most often with tuberculous kidney damage), hematogenous (if there is a purulent focus in other parts of the body) and lymphogenic (with diseases of the genital organs) by.
Classification of UTIs in pregnant women
UTIs in pregnant women include asymptomatic bacteriuria, lower urinary tract infections (acute and recurrent cystitis) and upper urinary tract infections (acute pyelonephritis, chronic pyelonephritis in remission, exacerbation, latent course).
Cystitis in pregnancy: course, diagnosis
Cystitis is an inflammation of the bladder wall, one of the most common urological diseases, as a rule, its cause is an infection. Symptoms of cystitis in women are manifested in the form of frequent urination, cramps and pain when urinating, pulling sensations in the lower abdomen, weakness, fatigue, irritability, blood in the urine, cloudy urine, pus or yellow spots on the underwear.
Normally, urination is not accompanied by pain. In women, painful urination can be caused by diseases of the bladder, urethra, or vagina. So, pain in the bladder, as a rule, is felt in the area of the womb, it can increase during urination or, conversely, decrease when the bladder is empty. Urethral pain associated with urination is felt by the patient directly in the urethra and is usually aggravated by urination. Urine entering the vaginal opening can cause pain if it is inflamed. Inflammation of the urethra is most often characterized by a bacterial nature and requires additional examination and treatment.
Primary diagnosis of cystitis involves an examination by specialized specialists (urologist, nephrologist, gynecologist), as well as taking an anamnesis and establishing possible causes of the disease (hypothermia, unprotected intercourse, taking medications, the presence of concomitant diseases).
Laboratory tests include a urinalysis for Nechiporenko cultures (helps identify the pathogen), a general urinalysis (allows you to identify erythrocytes, leukocytes, protein in the urine; the urine itself may be cloudy with an admixture of blood or pus), a general blood test (allows you to identify a picture inflammatory process, it is possible to increase the erythrocyte sedimentation rate (ESR), leukocytosis).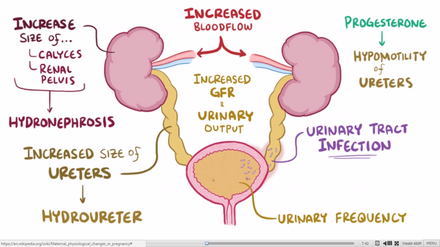 Among instrumental methods, ultrasound examination (ultrasound) of the bladder, ureteroscopy and cystoscopy (in case of violation of the passage of urine) are used.
Among instrumental methods, ultrasound examination (ultrasound) of the bladder, ureteroscopy and cystoscopy (in case of violation of the passage of urine) are used.
Asymptomatic bacteriuria during pregnancy
Asymptomatic bacteriuria during pregnancy is dangerous for both mother and fetus, against its background, 25% of women develop acute pyelonephritis. According to the World Health Organization, about 8% of women report asymptomatic bacteriuria, 15-57% of women with untreated asymptomatic bacteriuria develop symptoms of a UTI (acute cystitis or pyelonephritis). Therapy of this disease during pregnancy reduces the risk of developing acute UTIs, preterm birth, and low birth weight.
Diagnosis of asymptomatic bacteriuria can be established by detecting 10 5 CFU/ml of one bacterial strain or 10 2 CFU/ml of uropathogen Escherichia coli field of view in the absence of clinical manifestations of UTI.
It should be remembered that the risk of this pathology is most real from the 9th to the 17th week of pregnancy.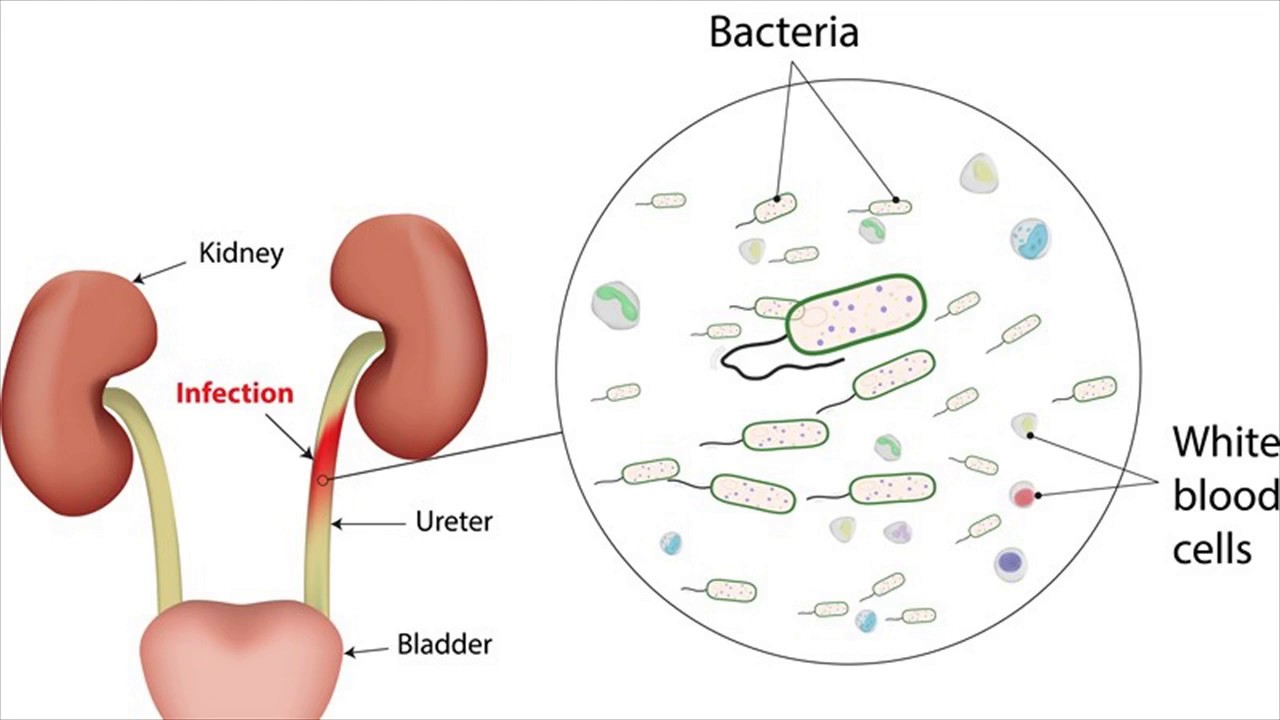 The only reliable method for diagnosing asymptomatic bacteriuria is the method of urine culture.
The only reliable method for diagnosing asymptomatic bacteriuria is the method of urine culture.
In accordance with Ukrainian and international guidelines for asymptomatic bacteriuria, oral antibiotic therapy with a single dose of fosfomycin trometamol is recommended.
Pyelonephritis: diagnosis
Pyelonephritis is an infectious and inflammatory disease of the kidneys of bacterial etiology with a primary and predominant lesion of the interstitium and tubular apparatus. The incidence of pyelonephritis during pregnancy reaches 33%, mortality - 3.5%, maternal mortality from kidney disease in the structure of extragenital pathology is 8-10%, the incidence of gestational pyelonephritis is 11.5%.
Primary pyelonephritis in pregnant women is difficult to treat, may be accompanied by fever, chills, nausea, vomiting, pain in the lumbar region, the appearance of pyuria, bacteriuria. As a rule, the right kidney is affected more often than the left one, with expansion of the pelvicalyceal system (according to ultrasound).
In acute pyelonephritis, the mandatory research methods are a general urinalysis (in 2 portions) 1 time in 7 days, a Nechiporenko urinalysis, a general and biochemical blood test, a bacteriological urinalysis, ultrasound of the kidneys and bladder, daily proteinuria, a biochemical blood test , blood pressure monitoring, urologist consultation. Additional research methods - computed tomography without contrast or excretory urogram, nuclear magnetic resonance imaging - are carried out exclusively for strict, sometimes vital, indications.
It should be remembered that dysuria in primary acute cystitis with a body temperature of 38 ° C and chills may indicate acute ascending pyelonephritis. A sharp dysuric syndrome is characteristic of the associated cystitis during exacerbation of chronic pyelonephritis. Urinary syndrome (proteinuria, leukocyturia, hematuria, etc.) may periodically disappear with a unilateral process and ureter occlusion; therefore, serial urine tests are necessary. The degree of leukocyturia does not always correspond to the severity of the inflammatory process. A single urine culture gives at least 20% false positive results. Bacteriuria appears and can be detected 2 days earlier than pyuria.
The degree of leukocyturia does not always correspond to the severity of the inflammatory process. A single urine culture gives at least 20% false positive results. Bacteriuria appears and can be detected 2 days earlier than pyuria.
Choice of drugs for the treatment of pregnant women with UTIs
There are certain requirements for antibiotics for the treatment of UTIs in pregnant women. In particular, they must be effective against most pathogenic pathogens, have the ability to create a high concentration in organs - foci of infection, have a long half-life sufficient to maintain a high concentration of the antibiotic in the blood, not have toxic and allergic effects, be well tolerated by patients, be harmless to mother and fetus.
It has been shown that for the treatment of pregnant women with acute cystitis, asymptomatic bacteriuria, acute pyelonephritis, it is advisable to use antibacterial uroseptics. In particular, fosfomycin trometamol has a bactericidal effect associated with blocking the bacterial enzyme involved in the synthesis of the cell wall, as well as an anti-adhesive effect (destroys the fimbria of Escherichia coli, preventing it from fixing on the wall of the urothelium and promoting leaching from the urinary tract). After a single dose of the drug, the therapeutic concentration is observed for 48 hours (this is enough to sterilize urine and recover).
After a single dose of the drug, the therapeutic concentration is observed for 48 hours (this is enough to sterilize urine and recover).
An alternative to antibiotics are phytoneering preparations with anti-adhesive and antibacterial activity, as well as anti-inflammatory, antispasmodic, nephroprotective properties.
Organization of care for pregnant women with UTI and prevention
Delivery of pregnant women with UTI (without obstetric pathology) is carried out through the natural birth canal, taking into account the obstetric situation.
There are degrees of risk of pyelonephritis:
- I degree - uncomplicated pyelonephritis that occurred during pregnancy;
- II degree - chronic uncomplicated pyelonephritis, noted before pregnancy;
- III degree - pyelonephritis with hypertension, azotemia, pyelonephritis of a single kidney.
They must be taken into account when managing pregnant women. So, at I-II degree of risk, pregnancy can be prolonged, but at III degree (creatinine> 265 μmol / l, glomerular filtration rate < 30 ml / min), pregnancy should be terminated.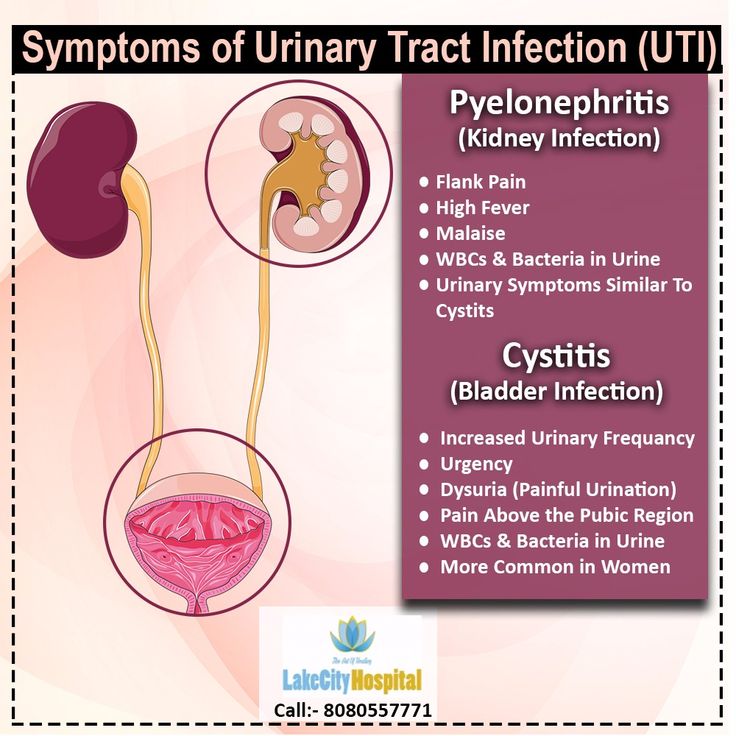
Prevention of UTIs in pregnant women should include sanitation of the vagina in case of violation of its microflora and other sources of infection (teeth, pharynx, etc.), normalization of bowel function, optimal water regime.
Subscribe to our Telegram channel, Viber community, Instagram, Facebook page, and Twitter to be the first to receive the latest and most relevant news from the world of medicine.
Marina Kolesnik,
photo of the author
Uncomplicated urinary tract infection in pregnant women. Modern ideas about treatment and prevention | #09/18
| This article outlines modern ideas about urinary tract infections in pregnant women. | |
#09/18 Keywords / keywords: Antibacterial therapy, Pregnancy, Asymptomatic bacteriuria, Urinary tract infection, Pyelonephritis, Uronefrologiya, Phyto-therapy, Cystitis, Infection
OB Poselyugina
Uncomplicated urinary tract infection in pregnant women. Modern views on treatment and prevention O. B. Poselyugina
In the article, modern views on urinary tract infection in pregnant women are presented. The features of antibacterial therapy depending on the localization of the infectious process in the urinary tract are revealed, the tactics of management of pregnant women according to clinical recommendations are given.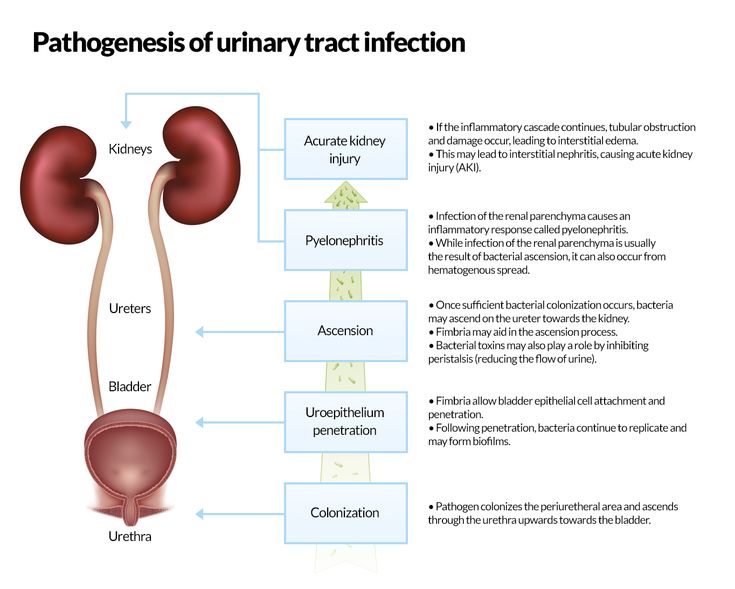 Phytotherapy and prevention in this disease are covered.
Phytotherapy and prevention in this disease are covered.
Urinary tract infections (UTIs) are one of the most common complications that can develop during pregnancy in women. Every year, the frequency of this pathology grows and ranges from 20% to 40% [2, 4, 7]. So, acute pyelonephritis of pregnant women occurs in about 10% of cases, including exacerbations of chronic pyelonephritis. At the same time, about 80% of exacerbations occur in the second trimester of pregnancy (at 22–28 weeks), less often in the third and first trimesters [1, 3, 7].
This is facilitated by both the well-known female anatomical features of the urethra (short urethra, close location of the rectum and genital tract), and the changes that occur in the body of a woman during pregnancy. During this period, women experience a change in the hormonal background associated with the development of hyperprogesteronemia. Against this background, dilatation of the pelvicalyceal system (PCS) and urinary tract develops.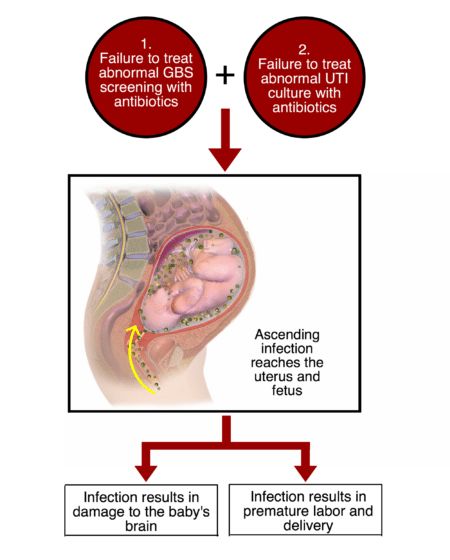 In addition, the pressure of the uterus on the urinary tract matters as the duration of pregnancy increases. In addition to the above development of gestational pyelonephritis, borderline and pathological variants of the course of pregnancy (polyhydramnios, multiple pregnancies, large fetuses) contribute [7].
In addition, the pressure of the uterus on the urinary tract matters as the duration of pregnancy increases. In addition to the above development of gestational pyelonephritis, borderline and pathological variants of the course of pregnancy (polyhydramnios, multiple pregnancies, large fetuses) contribute [7].
Thus, the problem of treatment and prevention of urinary tract infections is not only general medical, but also social.
The term UTI refers to an infection that is present in the urinary tract (UTI) but does not directly affect the kidneys. This concept combines all infectious and inflammatory diseases of the urinary system. The term "bacteriuria" indicates that bacteria are not only present in the urinary tract, but also actively multiply [2, 4].
An uncomplicated infection of the lower urinary tract is considered to be diseases in which patients have no structural or functional disorders of the urinary system and no severe comorbidities.
Asymptomatic bacteriuria (BB) is understood as the presence of two consecutive (with an interval of 24 hours) positive results of a bacteriological study of urine (> 100,000 CFU / ml) in women in which the same strain of the UTI pathogen was detected in the absence of clinical manifestations of the disease [2 , 4].
Determination and treatment of BD is most important in pregnant women, as it reduces the risk of developing pyelonephritis [4, 6, 7].
The incidence of BD in pregnant women in the population is about 6%, it is associated with the presence of pathogenic microorganisms in the periurethral region even before the upcoming pregnancy. This factor poses a risk of developing pyelonephritis during pregnancy, can lead to premature birth, anemia in women, and contribute to the development of preeclampsia [1, 7].
There are risk factors for the development of pyelonephritis during pregnancy, which include BD, not diagnosed before pregnancy, congenital malformations of the kidneys and urinary tract, reflux, chronic kidney disease.
The most common causative agent of uncomplicated UTI is uropathogenic Escherichia coli , which is detected in 85% of patients; less common are pathogens such as Staphylococcus saprophyticus , Proteus mirabilis , Enterococcus spp. , Klebsiella spp. and other representatives of the family Enterobacteriaceae [2–5]. The table presents the main criteria for diagnosing UTI in pregnant women.
, Klebsiella spp. and other representatives of the family Enterobacteriaceae [2–5]. The table presents the main criteria for diagnosing UTI in pregnant women.
Acute pyelonephritis in pregnant women is characterized, as a rule, by a sudden onset, with high body temperature with chills, intoxication, pain in the lumbar region or hypochondrium on the side of the lesion. In the absence of the effect of the therapy, it is necessary to exclude the complicated course of pyelonephritis - purulent forms of the disease (apostematous pyelonephritis, carbuncle of the kidney, paranephritis).
In addition, pyelonephritis in pregnant women can occur with blurred clinical symptoms, which can make it difficult to diagnose the disease [3, 7].
Treatment of uncomplicated UTIs in pregnant women, the choice of an antibacterial drug are of great importance not only for the health of the mother, but also for the fetus [1].
In pregnant women, regardless of the period, BD is subject to mandatory treatment [2, 6] with antibacterial drugs.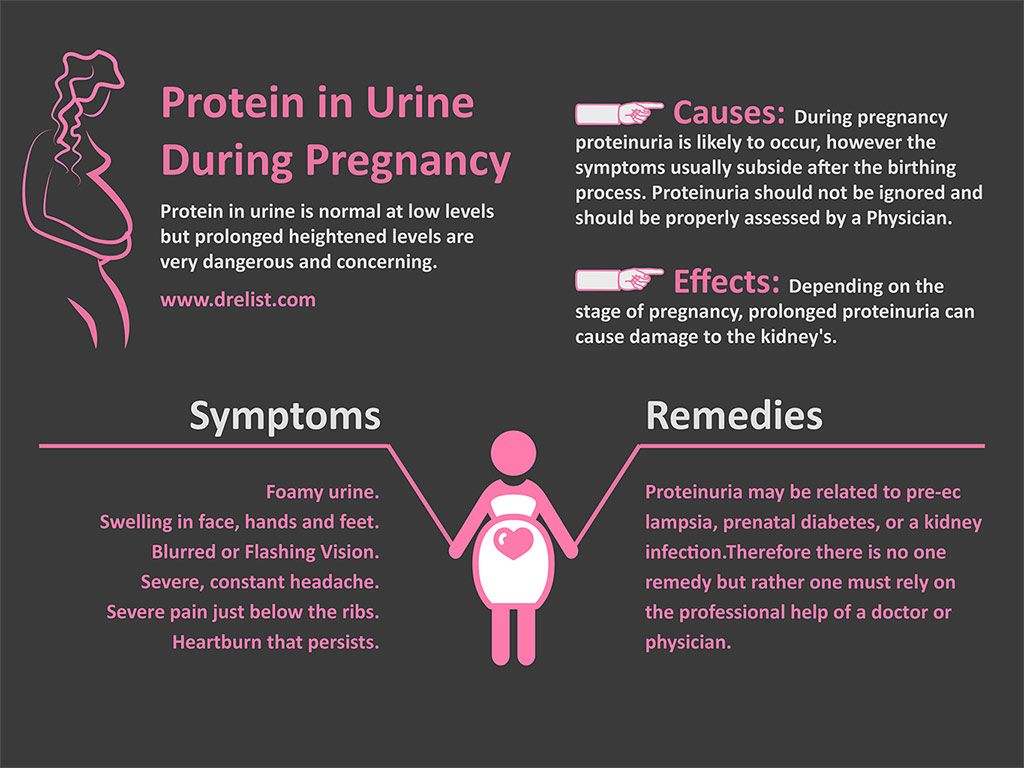
BB selectors:
- Fosfomycin trometamol orally 3.0 g once or
- Nitrofurantoin inside 0.1 g 2 times a day - 7 days.
Alternative therapy:
- Ceftibuten PO 0.4 g once a day for 3–7 days, or
- Cefixime 0.4 g orally once a day for 5–7 days, or
- Amoxicillin/clavulanate PO 0.625 g 3 times a day for 3–7 days.
For the treatment of acute cystitis in pregnant women, fosfomycin trometamol, beta-lactam antibiotics and nitrofurans are used, the average duration of treatment is 7 days, starting from the second trimester of pregnancy.
Treatment regimens for acute cystitis in pregnancy:
- Fosfomycin trometamol orally 3.0 g once, or
- Cefixime orally 0.4 g once a day for 7 days, or
- Ceftibuten orally 0.4 g once a day - 7 days, or
- Oral nitrofurantoin 0.
 1 g 2 times a day - 7 days, or
1 g 2 times a day - 7 days, or - Cefuroxime PO 0.25–0.5 g twice a day for 7 days, or
- Amoxicillin / clavulanate inside 0.625 g 3 times a day - 7 days.
In the treatment of acute pyelonephritis in pregnant women in the presence of a significant expansion of the upper urinary tract, it is recommended to install a self-retaining ureteral catheter (stent) or percutaneous puncture nephrostomy [2, 5, 6]. In acute pyelonephritis of pregnant women, the recommended duration of antibiotic therapy is 14 days:
Choices for acute pyelonephritis of pregnancy:
- Ceftibuten orally 0.4 g once a day, or
- Cefixime 0.4 g orally once a day, or
- Ceftriaxone IV or IM 1.0 once a day, or
- Aztreonam 2.0 IV 3 times a day.
Alternative therapy:
- Ertapenem IV, IM 1.0 g once a day, or
- Meropenem IV 1.
 0 g 3 times a day, or
0 g 3 times a day, or - Piperacillin/tazobactam IV 4.5 g 4 times a day.
The effectiveness of treatment is assessed by clinical and laboratory changes. In pregnant women, a bacteriological examination of urine is recommended 1-4 weeks after treatment and 1 time before delivery.
Such groups of antibacterial drugs as fluoroquinolones are not recommended for use during pregnancy, as they cause disturbances in the synthesis of fetal cartilage tissue. In the first half of pregnancy, tetracyclines, trimethoprim should not be used, and in the third - nitrofurantoin [1].
From herbal remedies, the use of Canephron N is effective and safe. It contains centaury herb, lovage root and rosemary leaves. Kanefron H has anti-inflammatory, antispasmodic, diuretic and nephroprotective effects. It is prescribed 2 tablets 3 times a day or 50 drops 3 times a day. After stopping the manifestations of UTI, it is recommended to continue taking Canephron N for prevention up to 1 month, it is possible to use it continuously for up to three months [2, 6].
With the prophylactic purpose of UTI, it is possible to use cranberry products (Monurel supplement), herbal uroseptics phytolysin (1 teaspoon 3-4 times a day - 2-6 weeks), the use of probiotics (vaginal applications of drugs containing lactobacilli, 1-2 times a day). week).
In general, the prognosis for treatment of uncomplicated UTI in pregnant women is favorable.
Taking into account the peculiarities of the course of uncomplicated UTI in pregnant women, knowledge of the modern characteristics of pathogens, approaches to diagnosis and treatment is of great importance not only for nephrologists and therapists, but also for doctors of other specialties.
Literature
- Mukhin N. A., Kozlovskaya L. V., Shilov E. M. , red. Rational pharmacotherapy in nephrology. Guide for practicing physicians. M.: Litter. 2006. 896 p.
- Perepanova T. S., Kozlov R. S., Rudnov V. A., Sinyakova L.
 A. Antimicrobial therapy and prevention of infections of the kidneys, urinary tract and male genital organs. Federal clinical guidelines. M., 2015. 72 p.
A. Antimicrobial therapy and prevention of infections of the kidneys, urinary tract and male genital organs. Federal clinical guidelines. M., 2015. 72 p. - Shilov E. M. , red. Nephrology: textbook for postgraduate education. Moscow: GEOTAR-Media. 2007. 688 p.
- Cormican M., Murphy A. W., Vellinga A. A. Interpreting asymptomatic bacteriuria // BMJ. 2011. 343: d4780. DOI: 10.1136.–bmg.d4780.
- Guidelines on urological, European Association of Urology, 2015. 88 p.
- Kunin C. M. Urinary tract infections: Detection, prevention, and management. 5th ed. Williams & Wilkins. 1997.34 p.
- Zinner S. H. Management of urinary tract infections in pregnancy: A review with comments on single therapy. Chemotherapy 36 (suppl 1). 1990. R. 50–52.
O. B. Poselyugina , doctor of medical sciences, professor
GBOU VPO TVGMU Ministry of Health of the Russian Federation , Tver
Contact information: poselubina@mail.
 The features of antibiotic therapy depending on the localization of the infectious process in the urinary tract are disclosed, the tactics of managing pregnant women are presented
The features of antibiotic therapy depending on the localization of the infectious process in the urinary tract are disclosed, the tactics of managing pregnant women are presented