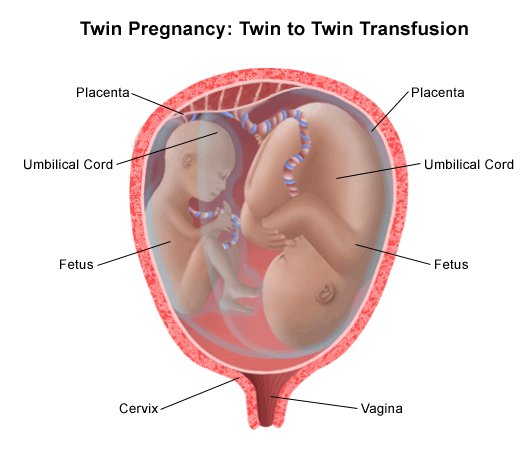
Umbilical cord with twins
Cord Blood & Tissue Banking for Twins
You’re having twins! Whether you see it as double the fun or biting off more than you can chew, you definitely will have your hands full. You know you have to double up on the diapers and double the food, but do you also have to double the cord blood and cord tissue that you bank, too?
Let’s get some basic questions out of the way:
Cryo-Cell siblings including a pair of twins
-
Does each twin have an umbilical cord?
It doesn’t matter if they are identical or fraternal; all twins, triplets, et cetera, et cetera, have their own umbilical cords. This means that, no matter what, there will be cord blood and cord tissue that can be (SPOILER: and should be) collected and preserved for each twin. -
Then, does each twin have its own placenta and its own source of cord blood?
Fraternal twins will always have their own placentas. In some rare cases, identical twins will, too; however, with identical twins, it comes down to when the egg splits to form the two embryos.If it splits within a few days from conception, as normal, they will form two separate placentas. If the split does not happen until 4–10 days—or later, they will share a single placenta. Identical twins make up a small proportion of twins, with the majority of them having separate placentas.
-
Is there still enough cord blood for two collections?
Cryo-Cell twins Julianna and Victoria
The body is an amazing thing. When pregnant, it produces 40%–50% more blood to provide nutrients to the baby. Even twins who share a single placenta and who may not be sharing the blood evenly will in most instances have enough cord blood to get two collections.
Why bank the cord blood from twins—fraternal or identical
As fraternal twins start as two separate eggs, they do not share an identical genetic makeup. This means that some genetic disorders that cord blood treats could affect one fraternal twin but not the other. As with other siblings, fraternal twins are more likely to be a suitable match, allowing one fraternal twin's cord blood to be used to treat the other twin who has a genetic disorder.
Cryo-Cell twins Landis and Laura
Identical twins come from the same egg and start with identical genomes, but remember that the environment can have an effect on if and how these genes are turned on and off because of something called epigenetics. Changes and mutations caused by the environment can affect many traits including disorders and even the HLA markers that determine the level of compatibility for the identical twins. One study estimated there to be an average of 359 genetic differences between the blood of identical twins alone. This means, just as with fraternal twins, twin A could form a genetic disorder that twin B does not have. It is also possible that twin 1 may not be as close of a match to twin 2 and vice versa. In the end, it is always a good idea for each twin—even identical twins—to have his or her own cord blood stored.
For either fraternal or identical twins, it is also a good idea to store as much cord blood as you can, making multiple doses available to better safeguard the whole family.
Proof in the numbers
We decided to look into the recovery rate for twins ourselves and see if and how volume and viability could be affected. As twins represent approx. three out of 100 births (i.e., 3 percent), we pulled data from our last 300 multiple births and our last 10,000 single births. Comparing the median results, we did receive 10 percent less cord blood in multi-birth collections than single-birth collections, but multiple-birth collections still had nearly 4 times more cells and nearly 8 times more CD34+ stem cells post-processing than the minimums we require.
In other words, even with twins, we were able to capture more than enough stem cells for a transfusion for each baby. We also found that our total post viability and CD34+ (stem cell) viability were a superlative 94 percent and 99 percent, respectively. This means, in addition to having a large number of stem and immune system cells, these cells were thriving and ready to aid the healing process.
What about the cord tissue?
It is also a good idea to store as much cord tissue as you can. Storing each twin's cord tissue will make multiple doses available, and with so much promise for treatment of diseases once believed to be untreatable, the need for cord tissue’s stem cells could rise dramatically in the future.
Storing each twin's cord tissue will make multiple doses available, and with so much promise for treatment of diseases once believed to be untreatable, the need for cord tissue’s stem cells could rise dramatically in the future.
Learn about Our Twins' Discount
Monochorionic Twins
What are monochorionic twins?
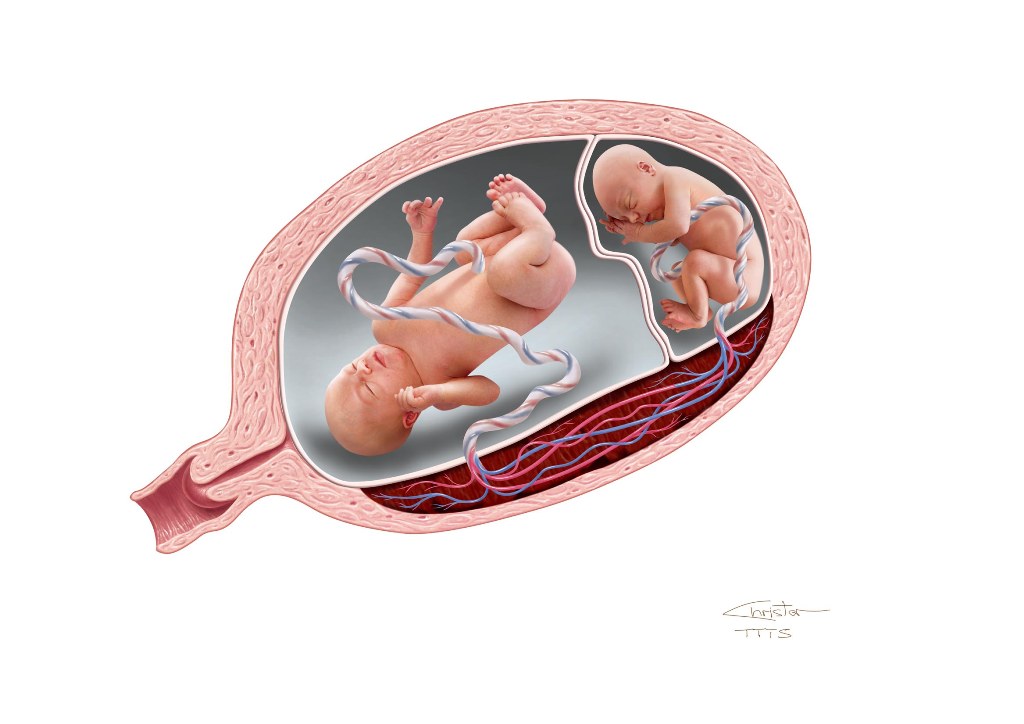
A single placenta normally supports a single fetus. When the situation arises in which two fetuses have to share a single placenta, complications may sometimes develop. Identical twins that share a single placenta are called monochorionic twins (MC). “Chorion” is the Latin root that refers to the placenta, while the word “amnion” refers to the sac, or “membranes” that surround each fetus. While fraternal twins (2 eggs and 2 sperm) are always surrounded in their own sacs and have their own individual placentas, 70% of identical twins may end up sharing a single placenta. Only 1% of identical twins share both a single placenta and a single sac, and this poses significant risk.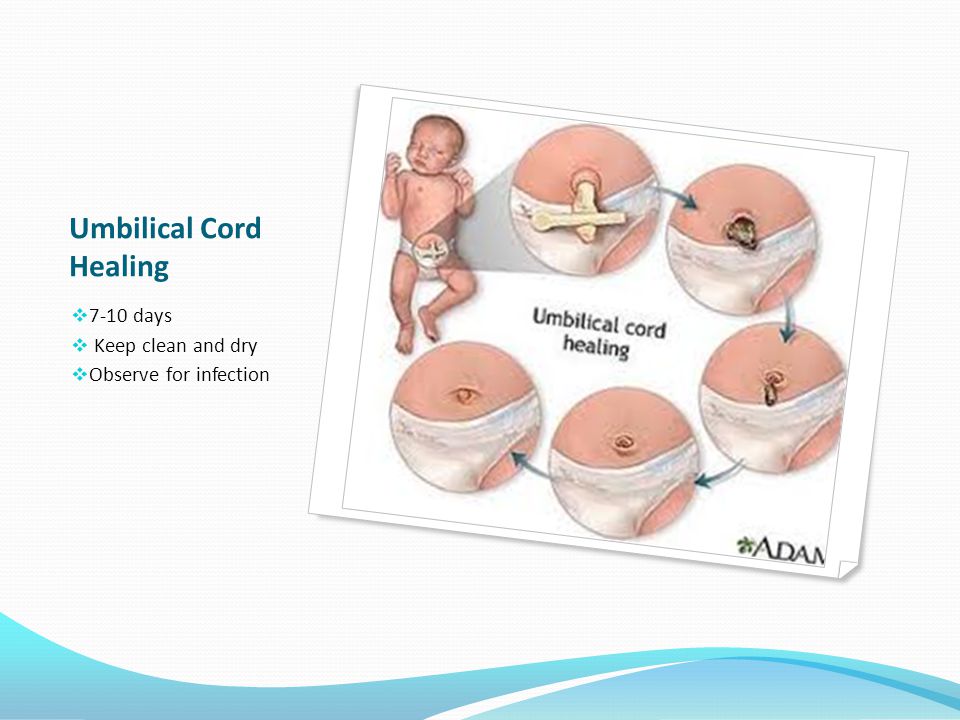
When two fetuses share one placenta, their umbilical cords may implant anywhere – there is no set or predictable pattern – and depending on where they implant, one fetus may get less of a ‘share’ of the placenta than it’s co-twin, resulting in less blood flow and nutrition to one fetus, with more to the other (unequal placental sharing). As a result, although identical twins usually share the same genetic material, they may actually grow differently. Like the roots of a tree, the blood vessels that run from each implanted cord may connect with each other beneath the surface, as there is nothing separating them within a single placenta. Depending on which types of vessels connect to which, one fetus may transfuse blood to the other. We will discuss each of these complications, their risks, and potential treatments, below.
- Watch Video (in Mandarin)
- Watch Video (in Spanish)
The following recommendations are meant for both patients and their providers as guidance during a pregnancy with monochorionic twins.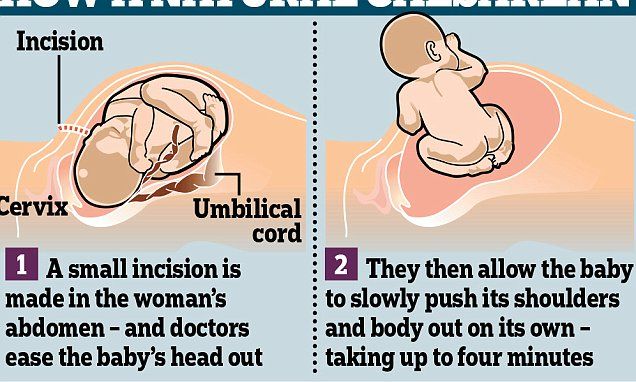 For questions and referrals please call us at 1-800-RX-FETUS.
For questions and referrals please call us at 1-800-RX-FETUS.
You can also download and print this information with our Monochorionic Twins Recommendations PDF brochure.
Complications Unique to Monochorionic Twins
- Unequal placental sharing
- Selective intrauterine growth restriction (S-IUGR) in one fetus
- TTTS - clinically defined as a deepest vertical pocket of > 8 cm in one twin and > 2 cm in in the other twin, simultaneously; TTTS can be seen overlapping with growth discordance, but these are separate diagnoses with different pathophysiologies
- Twin anemia polycythemia sequence (TAPS)
- Non-TTTS amniotic fluid discordance
- Discordant anomalies
- TRAP Sequence
Components of UCSF Evaluation
- Level II anatomic survey for (discordant) fetal anomalies
- Special attention paid to cord insertion locations and vascular mapping
- Fetal echocardiography for structural and functional integrity
- Fetal brain MRI > 22 weeks when indicated and appropriate
Potential Surgical Procedures
- Selective fetoscopic laser ablation
- Radiofrequency ablation (RFA) for cord occlusion
Timeframe for Referrals to UCSF
We welcome your call at any time to discuss your findings and obtain guidance about timing for referral and level of urgency 1-800-RX-FETUS.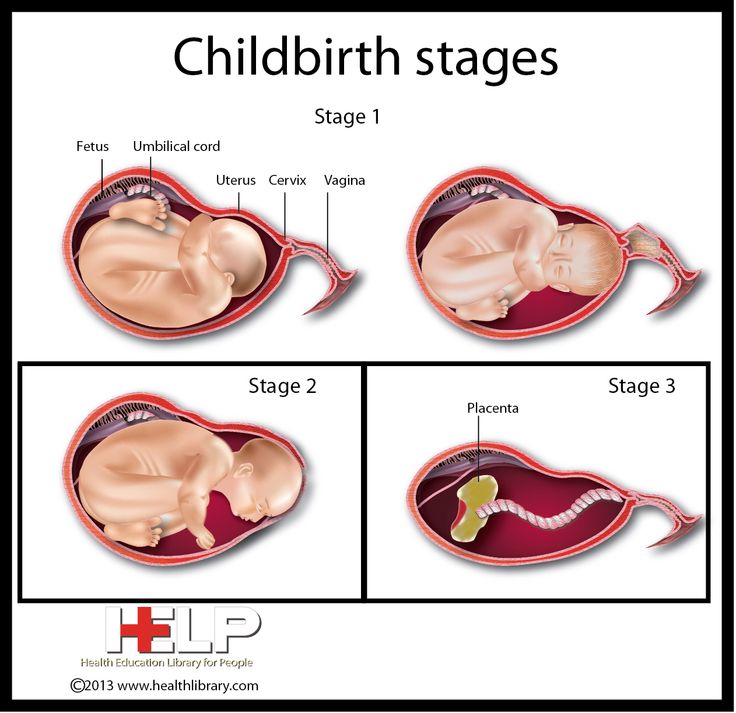
Consider Referral
- Significant amniotic fluid discordance
- Significant growth discordance (>20 percent)
- Isolated abnormal Doppler results
- Suspected discordant anomaly
Unless there is a lethal anomaly, if possible refer prior to 24 weeks to retain the option of RFA.
We encourage you to call our center to discuss your findings if you have concerns at 1-800-RX-FETUS
Call for Timely Referral (need to see patient within 1 week)
- Concurrent DVPs >8 cm and >2 cm, with normally sized bladder visualized and normal umbilical arterial (UA) Doppler results.
Call for Urgent Referral (need to see patient within a couple days)
- Concurrent DVPs >8 cm and >2 cm and either no visible donor twin bladder, abnormal UA Doppler results, suspected recipient cardiomyopathy or hydrops.
What is Needed For Referral
Patients referred to UCSF for an evaluation should have the following faxed to 415-502-0660:
-
Demographic information
-
A copy of the front/back of their health insurance card
-
All obstetric/maternal-fetal medicine (OB/MFM) medical records
-
If insurance authorization is required, for proper codes please download the Monochorionic Evaluation Codes.

-
Afterwards, call 1-800-RX-FETUS or 1-800-793-3887 to discuss your patient and complete the referral process.
What is the umbilical cord and how is it useful.
The umbilical cord is a connecting spirally twisted cord in placental mammals from the embryo to the placenta, which during intrauterine development is the physiological and genetic part of the fetus. It consists of one vein, through which arterial blood rich in oxygen and nutrients moves along the mother-fetus path, and two arteries for the outflow of “waste” venous blood along the fetus-mother path, although it happens 1 out of 100 when there is 1 umbilical artery in the umbilical cord , but this is extremely rare. The vein and arteries, in turn, are surrounded and protected by Wharton's jelly - a jelly-like intercellular substance of the connective tissue of the umbilical cord, thanks to which flexibility and plasticity are maintained, which prevents mechanical damage to the vessels. In full-term babies, the umbilical cord is 50-70 cm long, 1.5-2 cm in diameter, but there is a possibility that the umbilical cord can be short, about 30-40 cm. Both short less than 40 cm and long more than 70 cm can be unsafe for the life of the baby.
In full-term babies, the umbilical cord is 50-70 cm long, 1.5-2 cm in diameter, but there is a possibility that the umbilical cord can be short, about 30-40 cm. Both short less than 40 cm and long more than 70 cm can be unsafe for the life of the baby.
The umbilical cord is attached at one end to the abdominal wall of the fetus, and at the other to the placenta, (the place of attachment after the umbilical residue falls off, a scar is formed - the navel.) but if twins (triplets, etc. d :-)) are fraternal, then each placenta is different, and identical twins have one.
Human umbilical cord cutting can be served in a different time period and depends on specific factors. One of them is due to 5-20 whilins after birth. Since during natural childbirth, approximately 200 ml of blood remains in the placenta, which must return through the connection of the umbilical cord back to the baby after the birth and fill the small body with the right amount of oxygen and nutrients, this all happens because when the baby is born, it literally “reduces” by giving this amount of blood into the placenta through the umbilical cord, squeezing through the narrow birth canal and therefore it takes time to return.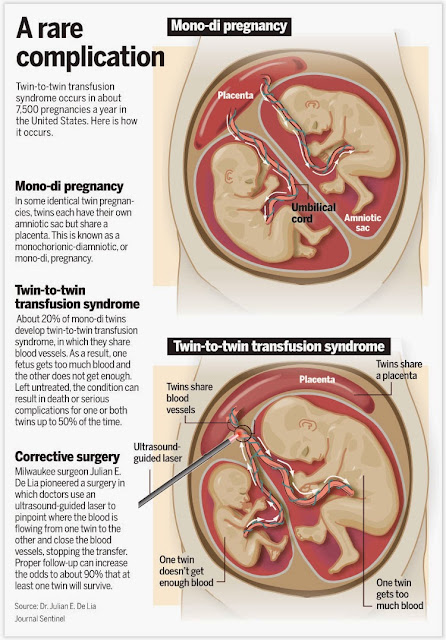 And as soon as the pulsation of blood in the umbilical cord is barely noticeable, it is clamped with umbilical clamps in two arms and cut ...... ..
And as soon as the pulsation of blood in the umbilical cord is barely noticeable, it is clamped with umbilical clamps in two arms and cut ...... ..
- One of the cases when the umbilical cord of a newborn needs to be cut immediately after exiting the birth canal in order to avoid possible complications is called Rh conflict. In short, this happens when the mother is Rh-negative and the father is Rh-positive, then there is a possibility that that the baby will also be Rh positive, which will lead to Rh conflict during pregnancy. (The painting of this particular case deserves a separate article.)
- Another case where the umbilical cord is cut immediately is a multiple pregnancy. This must be done so that the baby, who is born different, does not get tangled in the umbilical cord of the firstborn.
In a caesarean section, the fetus is removed at the head or pelvic end (along the inguinal fold or pedicle) with the fetus in the pelvic position, the cord is immediately cut between the clamps, and the baby is handed over to the midwife and neonatologist.
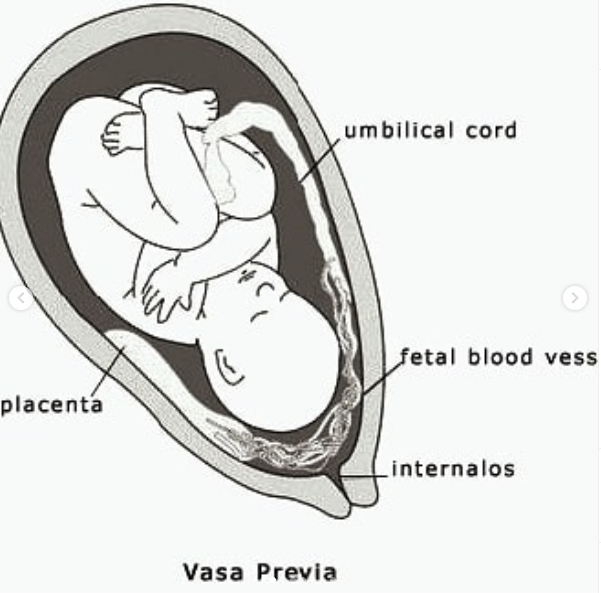
 After the baby is removed, the placenta is removed. It is important to note that it is the umbilical cord that can be the cause of a caesarean plant; Let's name two of them:
After the baby is removed, the placenta is removed. It is important to note that it is the umbilical cord that can be the cause of a caesarean plant; Let's name two of them: - is a prolapsed umbilical cord in which the umbilical cord is pinched and the baby cannot receive oxygen. The risk to the fetus in case of cord prolapse is the cessation of blood flow in the placenta-fetus system, followed by fetal hypoxia
- entanglement of the umbilical cord around the neck, torso, legs, arms. Especially dangerous is the tight entanglement around the neck. The entanglement of the umbilical cord during childbirth leads to stretching of the umbilical cord, narrows the lumen of the umbilical vessels, and to fetal asphyxia. This also creates a shortening of the umbilical cord, slows down the progress of the fetus through the birth canal, and can even cause premature detachment of the placenta.
You should know: the moment at which the umbilical cord is cut is extremely important, because immediately after childbirth a certain amount of blood, which is about 200 ml, goes back to the placenta (we wrote about this above), resulting in a decrease in blood pressure and hemoglobin level.
 Therefore, the expectant mother should ask the doctor about this in advance. Also, delaying the cutting of the umbilical cord may be beneficial for preterm infants, as keeping the umbilical cord reduces the neonate's need for blood transfusions.
Therefore, the expectant mother should ask the doctor about this in advance. Also, delaying the cutting of the umbilical cord may be beneficial for preterm infants, as keeping the umbilical cord reduces the neonate's need for blood transfusions. Interesting to know:
The umbilical cord does not have pain receptors, so cutting it is painless and not noticeable to either mother or baby.
stem cells can be taken from cord blood, which, in short, have the ability to restore or replace damaged cells.
After reading this article, in any case, you need to consult a doctor, and do not act on your own. After all, the article was written for the general development.
Be always healthy and don't get sick.
Your Baby Service.
Read also: "Proper care of the baby's umbilical cord in the first month after birth"
Multiple pregnancy fetus. Multiple pregnancy occurs in 0.
 4 - 1.6% of all pregnancies. Recently, there has been an obvious trend towards an increase in the incidence of such pregnancies due to the active use of assisted reproduction technologies, including in vitro fertilization (IVF).
4 - 1.6% of all pregnancies. Recently, there has been an obvious trend towards an increase in the incidence of such pregnancies due to the active use of assisted reproduction technologies, including in vitro fertilization (IVF). Types of multiple pregnancies
Children born in multiple pregnancies are called TWINS. There are two main types of twins: monozygotic (identical, homologous, identical, similar) and dizygotic (fraternal, heterologous, different). African countries have the highest twin birth rate, Europe and the USA have an average rate, and Asian countries have a low rate.
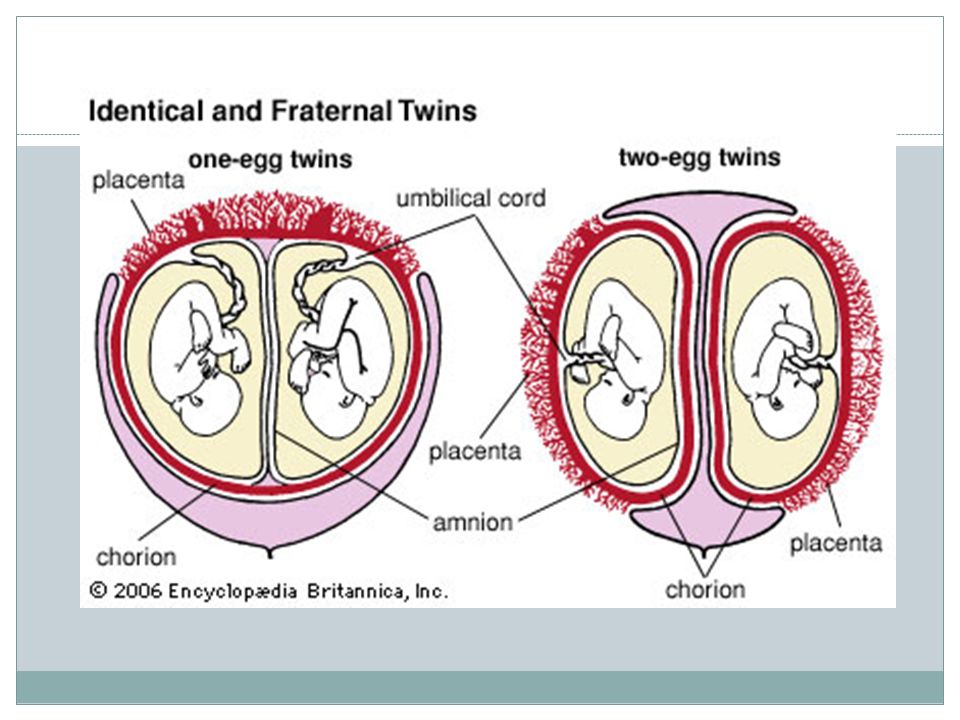
Dizygotic (fraternal) twins are more common (in 66-75% of all twins). The birth rate of dizygotic twins varies from 4 to 50 per 1000 births. Dizygotic twins occur when two separate eggs are fertilized. The maturation of two or more eggs can occur both in one ovary and in two. The predisposition to develop dizygotic twins may be maternally inherited. Dizygotic twins can be either same-sex or opposite-sex, they look like each other like ordinary brothers and sisters.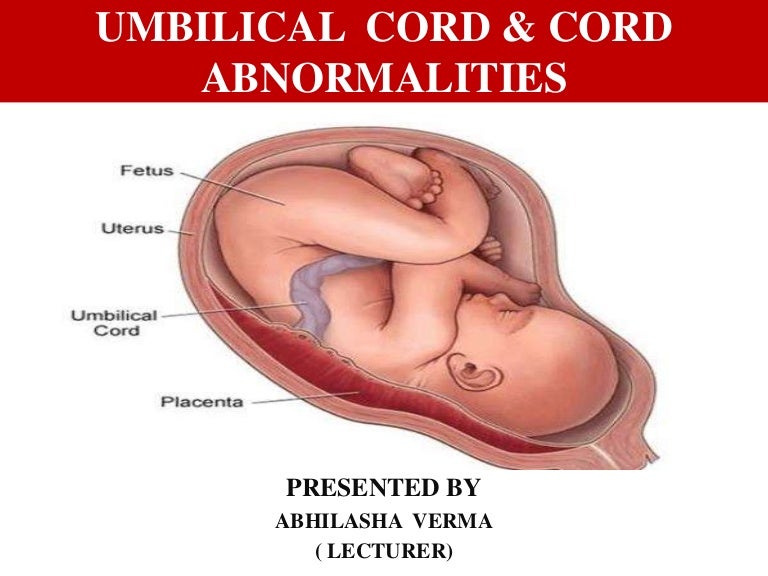 With fraternal twins, two placentas are always formed, which can be very close, even touching, but they can always be separated. Two fruit spaces (i.e., fetal bladders or two “houses”) are separated from each other by a septum consisting of two chorionic and two amniotic membranes. Such twins are called dizygotic dichorionic diamniotic twins.
With fraternal twins, two placentas are always formed, which can be very close, even touching, but they can always be separated. Two fruit spaces (i.e., fetal bladders or two “houses”) are separated from each other by a septum consisting of two chorionic and two amniotic membranes. Such twins are called dizygotic dichorionic diamniotic twins.
Monozygotic (identical) twins are formed as a result of the separation of one fetal egg at various stages of its development. The frequency of birth of monozygotic twins is 3-5 per 1000 births. The division of a fertilized egg into two equal parts can occur as a result of a delay in implantation (immersion of the embryo in the uterine mucosa) and oxygen deficiency, as well as due to a violation of the acidity and ionic composition of the medium, exposure to toxic and other factors. The emergence of monozygotic twins is also associated with the fertilization of an egg that had two or more nuclei. If the separation of the fetal egg occurs in the first 3 days after fertilization, then monozygotic twins have two placentas and two amniotic cavities, and are called monozygotic diamniotic dichoriones (Fig. A). If the division of the ovum occurs between 4 - 8 days after fertilization, then two embryos will form, each in a separate amniotic sac. Two amniotic sacs will be surrounded by a common chorionic membrane with one placenta for two. Such twins are called monozygotic diamniotic monochorionic twins (Fig. B). If division occurs by 9- 10th day after fertilization, then two embryos are formed with a common amniotic sac and placenta. Such twins are called monozygotic monoamniotic monochorionic (Fig. B) If the egg is separated at a later date on the 13th - 15th day after conception, the separation will be incomplete, which will lead to the appearance of conjoined (undivided, Siamese) twins. This type is quite rare, approximately 1 observation in 1500 multiple pregnancies or 1: 50,000 - 100,000 newborns. Monozygotic twins are always the same sex, have the same blood type, have the same eye color, hair, skin texture of the fingers, and are very similar to each other.
A). If the division of the ovum occurs between 4 - 8 days after fertilization, then two embryos will form, each in a separate amniotic sac. Two amniotic sacs will be surrounded by a common chorionic membrane with one placenta for two. Such twins are called monozygotic diamniotic monochorionic twins (Fig. B). If division occurs by 9- 10th day after fertilization, then two embryos are formed with a common amniotic sac and placenta. Such twins are called monozygotic monoamniotic monochorionic (Fig. B) If the egg is separated at a later date on the 13th - 15th day after conception, the separation will be incomplete, which will lead to the appearance of conjoined (undivided, Siamese) twins. This type is quite rare, approximately 1 observation in 1500 multiple pregnancies or 1: 50,000 - 100,000 newborns. Monozygotic twins are always the same sex, have the same blood type, have the same eye color, hair, skin texture of the fingers, and are very similar to each other.
Twin births occur once in 87 births, triplets - once in 87 2 (6400) twins, quadruples - once in 87 3 (51200) triplets, etc.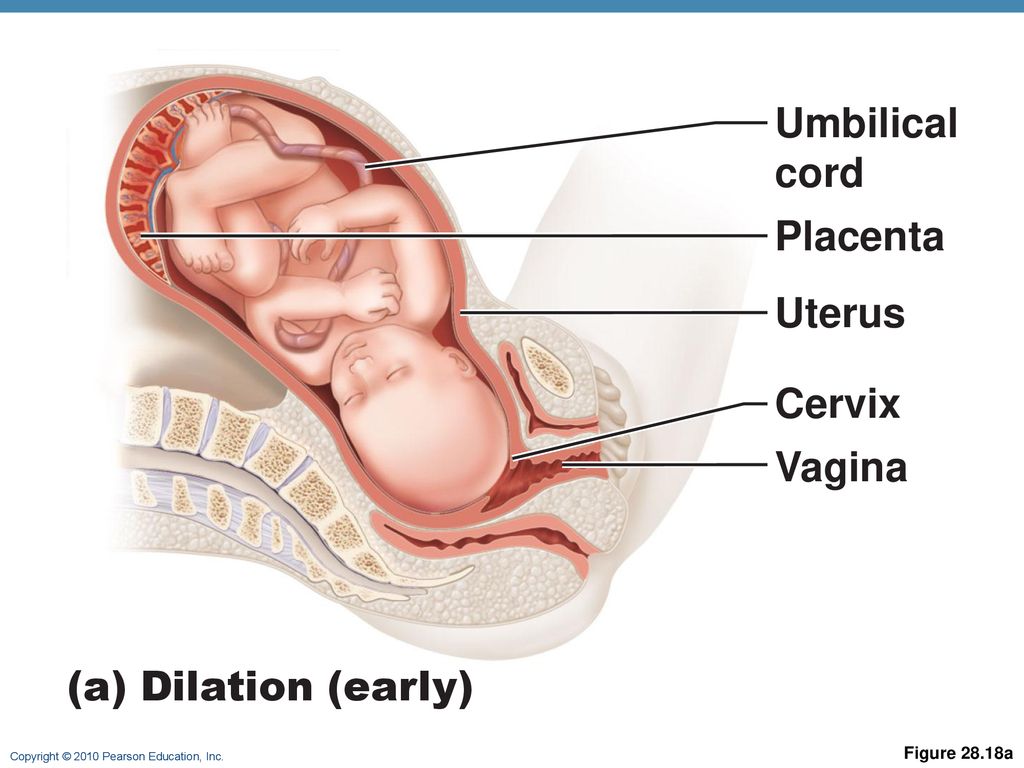 (according to the Gallin formula). The origin of triplets, quadruplets, and more twins varies. So, triplets can be formed from three separate eggs, from two or one egg. They can be monozygotic and heterozygous. Quadruples can also be identical and fraternal.
(according to the Gallin formula). The origin of triplets, quadruplets, and more twins varies. So, triplets can be formed from three separate eggs, from two or one egg. They can be monozygotic and heterozygous. Quadruples can also be identical and fraternal.
Features of the course of multiple pregnancy
In case of multiple pregnancy, the woman's body is subject to increased requirements. All organs and systems function with great tension. In connection with the displacement of the diaphragm by the enlarged uterus, the activity of the heart becomes difficult, shortness of breath, fatigue occur. Enlargement of the uterus, especially towards the end of pregnancy, leads to compression of the internal organs, which is manifested by impaired bowel function, frequent urination, and heartburn. Almost 4-5 times more often there is the development of preeclampsia, which is characterized by an earlier onset, a protracted and more severe clinical course, often combined with acute pyelonephritis of pregnant women.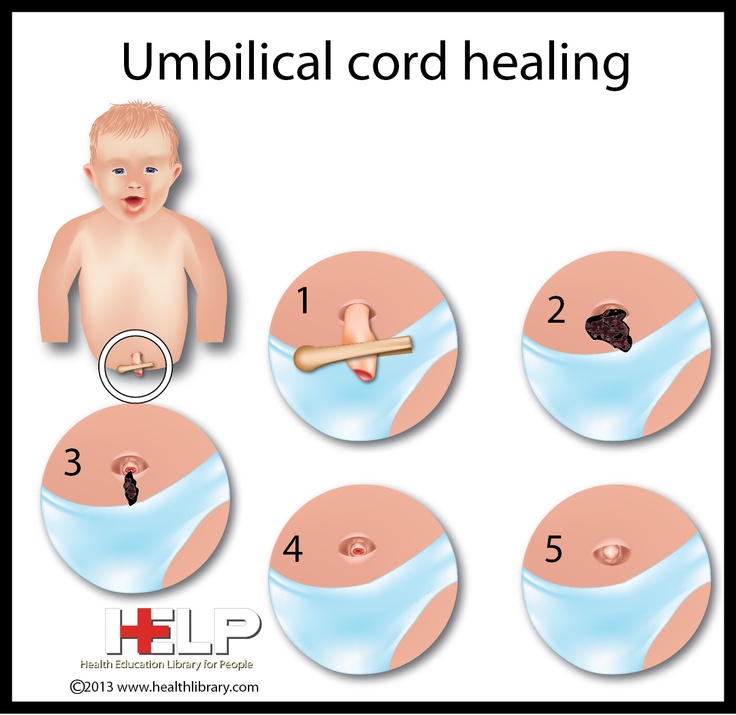 Due to the increased need and consumption of iron, iron deficiency anemia often develops in pregnant women. Significantly more often than with a singleton pregnancy, complications such as bleeding during pregnancy and childbirth, anomalies in labor, and a low location of the placenta are observed. Often, with multiple pregnancies, abnormal positions of the fetus occur. One of the most common complications in multiple pregnancy is its premature termination. Preterm birth is observed in 25-50% of cases of such pregnancies.
Due to the increased need and consumption of iron, iron deficiency anemia often develops in pregnant women. Significantly more often than with a singleton pregnancy, complications such as bleeding during pregnancy and childbirth, anomalies in labor, and a low location of the placenta are observed. Often, with multiple pregnancies, abnormal positions of the fetus occur. One of the most common complications in multiple pregnancy is its premature termination. Preterm birth is observed in 25-50% of cases of such pregnancies.
The development of term twins is normal in most cases. However, their body weight is usually less (by 10% or more) than in singleton pregnancies. With twins, the weight of children at birth less than 2500 g is observed in 40-60%. The low weight of twins is most often due to insufficiency of the uteroplacental system, which is not able to adequately provide several fetuses with nutrients, trace elements and oxygen. The consequence of this is a delay in the development of the fetus, which is a common occurrence in multiple pregnancies.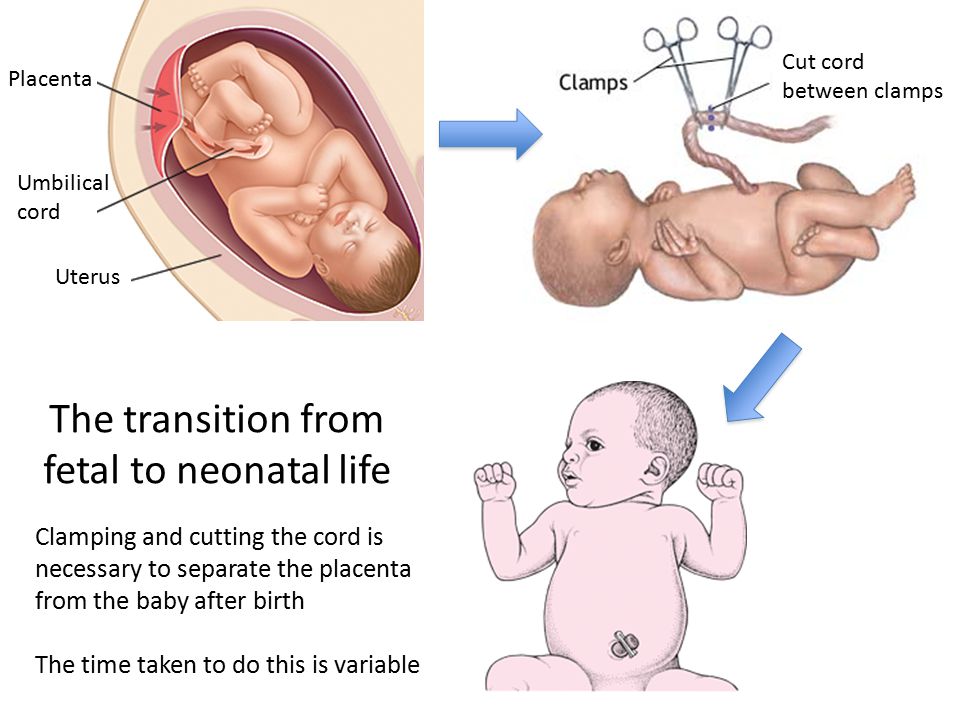 The mass of twins, respectively, decreases in proportion to their number (triplets, quadruplets, etc.).
The mass of twins, respectively, decreases in proportion to their number (triplets, quadruplets, etc.).
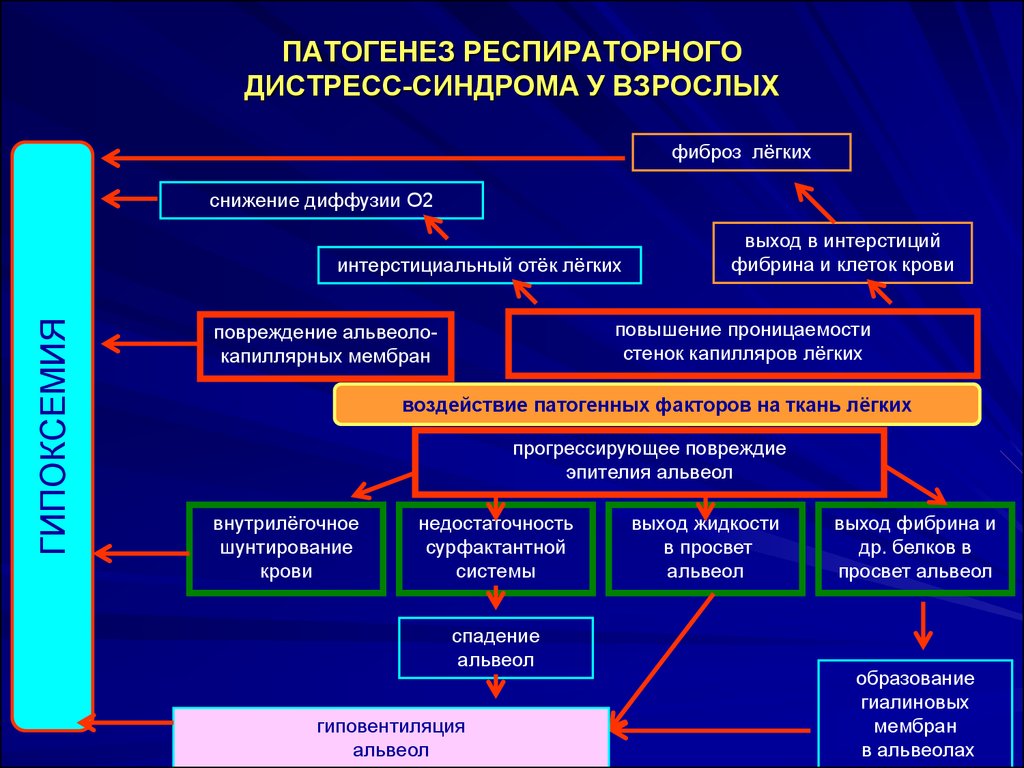
With monochorionic twins in the placenta, anastomoses are often formed between the vascular systems of the fetus, which can lead to a serious complication - the syndrome of feto-fetal transfusion. In this case, there is a redistribution of blood from one fetus to another, the so-called "stealing". The severity of feto-fetal transfusion (mild, moderate, severe) depends on the degree of redistribution of blood through the anastomoses, which vary in size, number and direction.
Diagnosis in multiple pregnancy
The most reliable method for diagnosing multiple pregnancies is ultrasound, which allows not only early diagnosis of multiple pregnancies, but also to determine the position and presentation of fetuses, localization, structure and number of placentas, the number of amniotic cavities, the volume of amniotic fluid, congenital malformations and antenatal fetal death, the state of the fetus from a functional point of view, the nature of the uteroplacental and fetal-placental blood flow.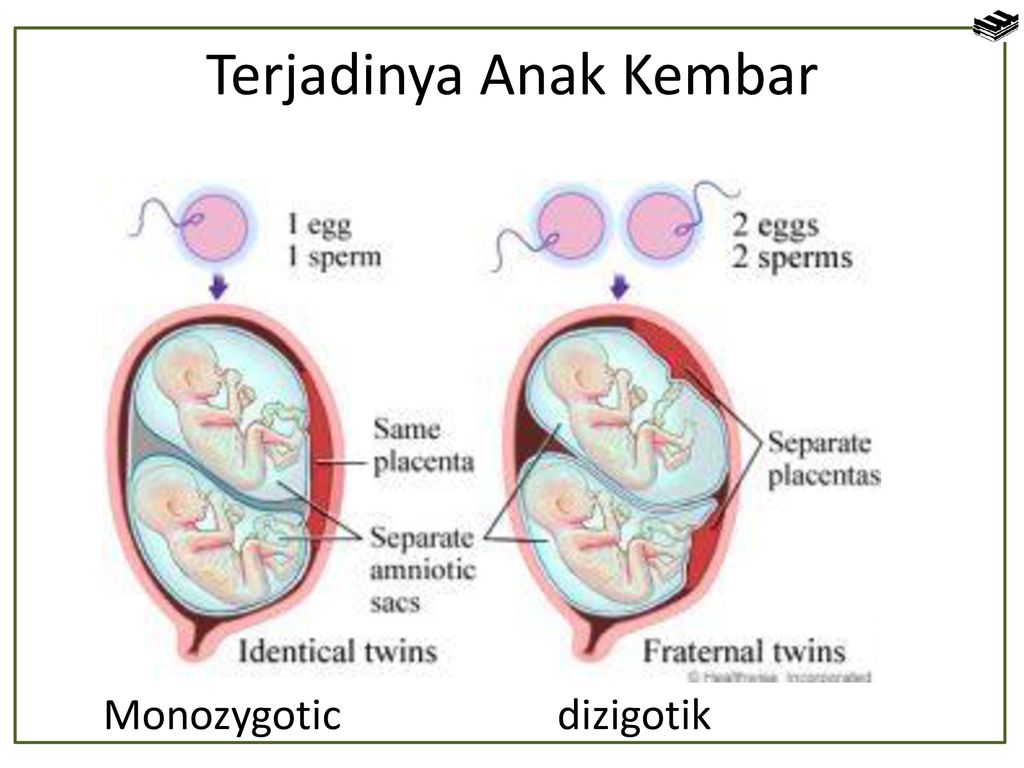
In multiple pregnancies, due to the higher risk of complications, ultrasound monitoring is performed more frequently than in singleton pregnancies. With dizygotic twins, about once every 3-4 weeks, with monozygotic twins - once every 2 weeks.
In addition, examinations and control of clinical tests are carried out with great care, and CTG is regularly recorded from 28 weeks of pregnancy.
Management of childbirth
Indications for caesarean section associated with multiple pregnancy are triplets (quadruple), the transverse position of both or one of the fetuses, breech presentation of both fetuses or the first of them, and not associated with multiple pregnancy - fetal hypoxia, anomalies labor activity, prolapse of the umbilical cord, extragenital pathology of the mother, severe gestosis, placenta previa and abruption, etc.
-
ECO
In the department of assisted reproductive technologies of the Maternity Hospital No.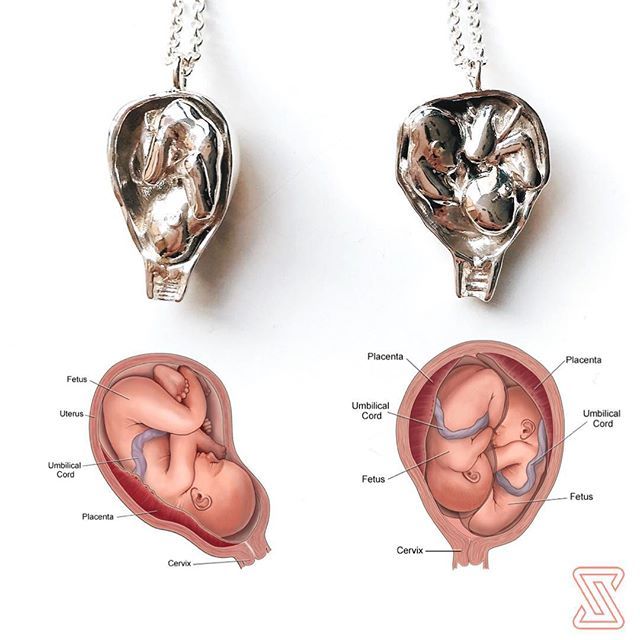 2
2
, IVF is performed at the expense of the Republican budget for couples
who have received a positive decision from the Minsk city or regional commissions to provide one free IVF attempt.
No drug supply problem. There is no waiting list.The largest number of children
The largest number of children born to one mother, according to official data, is 69. According to reports made in 1782, between 1725 and 1765. The wife of a Russian peasant Fyodor Vasiliev gave birth 27 times, giving birth to twins 16 times, triplets 7 times and 4 twins 4 times. Of these, only 2 children died in infancy.
The most prolific mother of our contemporaries is Leontina Albina (or Alvina) of San Antonio, Chile, who at 1943-81 years gave birth to 55 children. As a result of the first 5 pregnancies, she gave birth to triplets, and exclusively male.
Most birthed
The record 38 births are said to be Elizabeth Greenhillies Abbots-Langley, c.
 Hertfordshire, UK. She had 39 children - 32 daughters and 7 sons.
Hertfordshire, UK. She had 39 children - 32 daughters and 7 sons. The largest number of multiple births in one family
Maddalena Pomegranate from Italy (b. 1839) had triplets born 15 times.
There is also information about the birth on May 29, 1971 in Philadelphia, Pennsylvania, USA, and in May 1977 in Bagarhat, Bangladesh, 11 twins. In both cases, no child survived.Most fertile pregnancies
Dr. Gennaro Montanino, Rome, Italy, claimed to have removed, in July 1971, the embryos of 10 girls and 5 boys from the uterus of a 35-year-old woman who was 4 months pregnant. This unique case of 15-fertility was the result of infertility pills.
9 children - the largest number in one pregnancy - were born on June 13, 1971 by Geraldine Broadrick in Sydney, Australia. 5 boys and 4 girls were born: 2 boys were stillborn, and none of the rest survived more than 6 days.
The birth of 10 twins (2 boys and 8 girls) is known from reports from Spain (1924), China (1936) and Brazil (April 1946).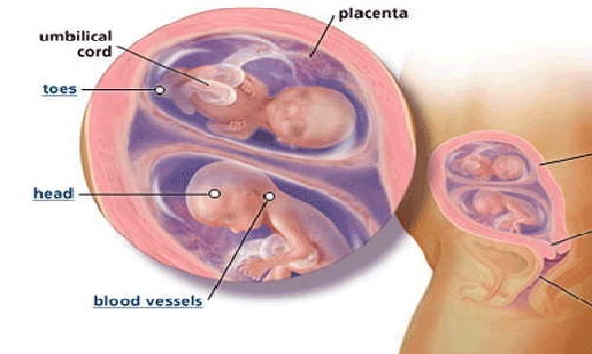
The father with many children
The largest father in the history of Russia is Yakov Kirillov, a peasant from the village of Vvedensky, who in 1755 was presented to the court in connection with this (he was then 60 years old). The first wife of a peasant gave birth to 57 children: 4 times four, 7 times three, 9once twice and 2 times once. The second wife gave birth to 15 children. Thus, Yakov Kirillov had 72 children from two wives.
Longest Birth Intervals for Multiple Pregnancies
Peggy Lynn of Huntington Pennsylvania, USA, gave birth to a girl, Hanna, on November 11, 1995, and the second of the twins, Erika, only 84 days later (February 2, 1996).
Siamese twins
United twins were called "Siamese" after Chang and Eng Bunkers were born fused in the sternum on May 11, 1811 in the Maeklong region of Siam (Thailand). They married Sarah and Adelaide Yates of pc. North Carolina, USA, and had 10 and 12 children, respectively.