Heavy bleeding after birth
Postpartum hemorrhage | March of Dimes
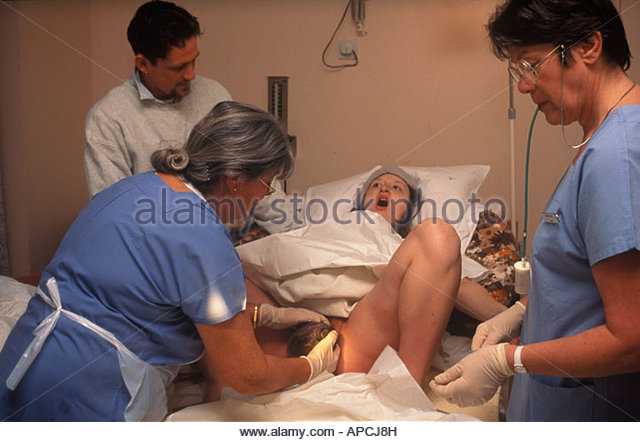
Postpartum hemorrhage (also called PPH) is a serious but rare condition when a woman has heavy bleeding after giving birth.
If you think you’re having PPH, call your health care provider or 911 immediately.
You may have PPH if you have heavy bleeding from the vagina that doesn’t slow or stop, blurred vision or chills, or if you feel weak or like you’re going to faint.
You’re more likely to have PPH if you’ve had it in the past or if you have certain medical conditions, especially conditions that affect the uterus (womb) or the placenta or conditions that affect how your blood clots.
Postpartum hemorrhage (also called PPH) is when a woman has heavy bleeding after giving birth. It’s a serious but rare condition. It usually happens within 1 day of giving birth, but it can happen up to 12 weeks after having a baby. About 1 to 5 in 100 women who have a baby (1 to 5 percent) have PPH.
It’s normal to lose some blood after giving birth. Women usually lose about half a quart (500 milliliters) during vaginal birth or about 1 quart (1,000 milliliters) after a cesarean birth (also called c-section). A c-section is surgery in which your baby is born through a cut that your doctor makes in your belly and uterus (womb). With PPH, you can lose much more blood, which is what makes it a dangerous condition. PPH can cause a severe drop in blood pressure. If not treated quickly, this can lead to shock and death. Shock is when your body organs don’t get enough blood flow.
When does PPH happen?
After your baby is delivered, the uterus normally contracts to push out the placenta. The contractions then help put pressure on bleeding vessels where the placenta was attached in your uterus. The placenta grows in your uterus and supplies the baby with food and oxygen through the umbilical cord. If the contractions are not strong enough, the vessels bleed more.:max_bytes(150000):strip_icc()/hemorrhage-in-miscarriage-meaning-2371523-FINAL-f2ab04cab1cc491e964a45e682f93da5.png) It can also happen if small pieces of the placenta stay attached.
It can also happen if small pieces of the placenta stay attached.
How do you know if you have PPH?
You may have PPH if you have any of these signs or symptoms. If you do, call your health care provider or 911 right away:
- Heavy bleeding from the vagina that doesn’t slow or stop
- Drop in blood pressure or signs of shock. Signs of low blood pressure and shock include blurry vision; having chills, clammy skin or a really fast heartbeat; feeling confused, dizzy, sleepy or weak; or feeling like you’re going to faint.
- Nausea (feeling sick to your stomach) or throwing up
- Pale skin
- Swelling and pain around the vagina or perineum. The perineum is the area between the vagina and rectum.
Are some women more likely than others to have PPH?
Yes. Things that make you more likely than others to have PPH are called risk factors. Having a risk factor doesn’t mean for sure that you will have PPH, but it may increase your chances.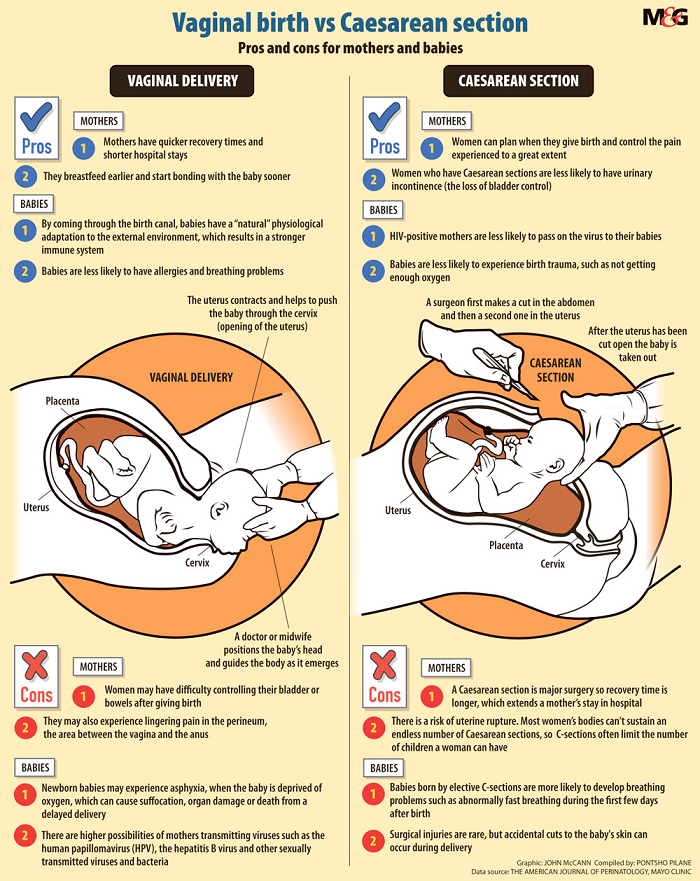 PPH usually happens without warning. But talk to your health care provider about what you can do to help reduce your risk for having PPH.
PPH usually happens without warning. But talk to your health care provider about what you can do to help reduce your risk for having PPH.
You’re more likely than other women to have PPH if you’ve had it before. This is called having a history of PPH. Asian and Hispanic women also are more likely than others to have PPH.
Several medical conditions are risk factors for PPH. You may be more likely than other women to have PPH if you have any of these conditions:
Conditions that affect the uterus
- Uterine atony. This is the most common cause of PPH. It happens when the muscles in your uterus don’t contract (tighten) well after birth. Uterine contractions after birth help stop bleeding from the place in the uterus where the placenta breaks away. You may have uterine atony if your uterus is stretched or enlarged (also called distended) from giving birth to twins or a large baby (more than 8 pounds, 13 ounces). It also can happen if you’ve already had several children, you’re in labor for a long time or you have too much amniotic fluid.
 Amniotic fluid is the fluid that surrounds your baby in the womb.
Amniotic fluid is the fluid that surrounds your baby in the womb. - Uterine inversion. This is a rare condition when the uterus turns inside out after birth.
- Uterine rupture. This is when the uterus tears during labor. It happens rarely. It may happen if you have a scar in the uterus from having a c-section in the past or if you’ve had other kinds of surgery on the uterus.
Conditions that affect the placenta
- Placental abruption. This is when the placenta separates early from the wall of the uterus before birth. It can separate partially or completely.
- Placenta accreta, placenta increta or placenta percreta. These conditions happen when the placenta grows into the wall of the uterus too deeply and cannot separate.
- Placenta previa. This is when the placenta lies very low in the uterus and covers all or part of the cervix.
 The cervix is the opening to the uterus that sits at the top of the vagina.
The cervix is the opening to the uterus that sits at the top of the vagina. - Retained placenta. This happens if you don’t pass the placenta within 30 to 60 minutes after you give birth. Even if you pass the placenta soon after birth, your provider checks the placenta to make sure it’s not missing any tissue. If tissue is missing and is not removed from the uterus right away, it may cause bleeding.
Conditions during labor and birth
- Having a c-section
- Getting general anesthesia. This is medicine that puts you to sleep so you don’t feel pain during surgery. If you have an emergency c-section, you may need general anesthesia.
- Taking medicines to induce labor. Providers often use a medicine called Pitocin to induce labor. Pitocin is the man-made form of oxytocin, a hormone your body makes to start contractions.

- Taking medicines to stop contractions during preterm labor. If you have preterm labor, your provider may give you medicines called tocolytics to slow or stop contractions.
- Tearing (also called lacerations). This may happen if the tissues in your vagina or cervix are cut or torn during birth. The cervix is the opening to the uterus that sits at the top of the vagina. You may have tearing if you give birth to a large baby, your baby is born through the birth canal too quickly or you have an episiotomy that tears. An episiotomy is a cut made at the opening of the vagina to help let the baby out. Tearing also can happen if your provider uses tools, like forceps or a vacuum, to help move your baby through the birth canal during birth. Forceps look like big tongs. A vacuum is a soft plastic cup that attaches to your baby’s head. It uses suction to gently pull your baby as you push during birth.
- Having quick labor or being in labor a long time.
 Labor is different for every woman. If you’re giving birth for the first time, labor usually takes about 14 hours. If you’ve given birth before, it usually takes about 6 hours. Augmented labor may also increase risk of PPH. Augmentation of labor means medications or other means are used to make more contractions of the uterus during labor.
Labor is different for every woman. If you’re giving birth for the first time, labor usually takes about 14 hours. If you’ve given birth before, it usually takes about 6 hours. Augmented labor may also increase risk of PPH. Augmentation of labor means medications or other means are used to make more contractions of the uterus during labor.
Other conditions
- Blood conditions, like von Willebrand disease or disseminated intravascular coagulation (also called DIC). These conditions can increase your risk of forming a hematoma. A hematoma happens when a blood vessel breaks causing a blood clot to form in tissue, an organ or another part of the body. After giving birth, some women develop a hematoma in the vaginal area or the vulva (the female genitalia outside of the body). Von Willebrand’s disease is a bleeding disorder that makes it hard for a person to stop bleeding. DIC causes blood clots to form in small blood vessels and can lead to serious bleeding.
 Certain pregnancy and childbirth complications (like placenta accreta), surgery, sepsis (blood infection) and cancer can cause DIC.
Certain pregnancy and childbirth complications (like placenta accreta), surgery, sepsis (blood infection) and cancer can cause DIC. - Infection, like chorioamnionitis. This is an infection of the placenta and amniotic fluid.
- Intrahepatic cholestasis of pregnancy (also called ICP). This is the most common liver condition that happens during pregnancy.
- Obesity. Being obese means you have an excess amount of body fat. If you’re obese, your body mass index (also called BMI) is 30 or higher. BMI is a measure of body fat based on your height and weight. To find out your BMI, go to www.cdc.gov/bmi.
- Preeclampsia or gestational hypertension. These are types of high blood pressure that only pregnant women can get. Preeclampsia is a condition that can happen after the 20th week of pregnancy or right after pregnancy. It’s when a pregnant woman has high blood pressure and signs that some of her organs, like her kidneys and liver, may not be working properly.
 Signs of preeclampsia include having protein in the urine, changes in vision and severe headache. Gestational hypertension is high blood pressure that starts after 20 weeks of pregnancy and goes away after you give birth. Some women with gestational hypertension have preeclampsia later in pregnancy.
Signs of preeclampsia include having protein in the urine, changes in vision and severe headache. Gestational hypertension is high blood pressure that starts after 20 weeks of pregnancy and goes away after you give birth. Some women with gestational hypertension have preeclampsia later in pregnancy.
How is PPH tested for and treated?
Your provider may use these tests to see if you have PPH or try to find the cause for PPH:
- Blood tests called clotting factors tests or factor assays
- Hematocrit. This is a blood test that checks the percent of your blood (called whole blood) that’s made up of red blood cells. Bleeding can cause a low hematocrit.
- Blood loss measurement. To see how much blood you’ve lost, your provider may weigh or count the number of pads and sponges used to soak up the blood.
- Pelvic exam. Your provider checks your vagina, uterus and cervix.

- Physical exam. Your provider checks your pulse and blood pressure.
- Ultrasound. Your provider can use ultrasound to check for problems with the placenta or uterus. Ultrasound is a test that uses sound waves and a computer screen to make a picture of your baby inside the womb or your pelvic organs.
Treatment depends on what’s causing your bleeding. It may include:
- Getting fluids, medicine (like Pitocin) or having a blood transfusion (having new blood put into your body). You get these treatments through a needle into your vein (also called intravenous or IV), or you may get some directly in the uterus.
- Having surgery, like a hysterectomy or a laparotomy. A hysterectomy is when your provider removes your uterus. You usually only need a hysterectomy if other treatments don’t work. A laparotomy is when your provider opens your belly to check for the source of bleeding and stops the bleeding.

- Massaging the uterus by hand. Your provider can massage the uterus to help it contract, lessen bleeding and help the body pass blood clots. Your provider may also give you medications like oxytocin to make the uterus contract and lessen bleeding.
- Getting oxygen by wearing an oxygen mask
- Removing any remaining pieces of the placenta from the uterus, packing the uterus with gauze, a special balloon or sponges, or using medical tools or stitches to help stop bleeding from blood vessels.
- Embolization of the blood vessels that supply the uterus. In this procedure, a provider uses special tests to find the bleeding blood vessel and injects material into the vessel to stop the bleeding. It’s used in special cases and may prevent you from needing a hysterectomy.
- Taking extra iron supplements along with a prenatal vitamin may also help. Your provider may recommend this depending on how much blood was lost.

See also: Maternal death
Last reviewed March 2020
What's Normal, What's Not, Causes, Treatment
Written by Paige Fowler
In this Article
- What's Normal
- When to Call Your Doctor
- What Causes It?
- How It's Treated
If you have a vaginal delivery or Cesarean section, you’ll have vaginal bleeding and discharge after birth. This is known as lochia. It’s how your body gets rid of the extra blood and tissue in your uterus that helped your baby grow.
Bleeding is heaviest the first few days after your baby is born. But if heavy bleeding continues after that, you may need to call your doctor.
What's Normal
Your blood will be bright red, and you may see some clots for the first few days after you give birth. They shouldn’t be bigger than a quarter. You’ll have to wear a hospital-grade pad at first. But you should be able to go back to a regular pad later.
You might bleed a little more when you bring your baby home.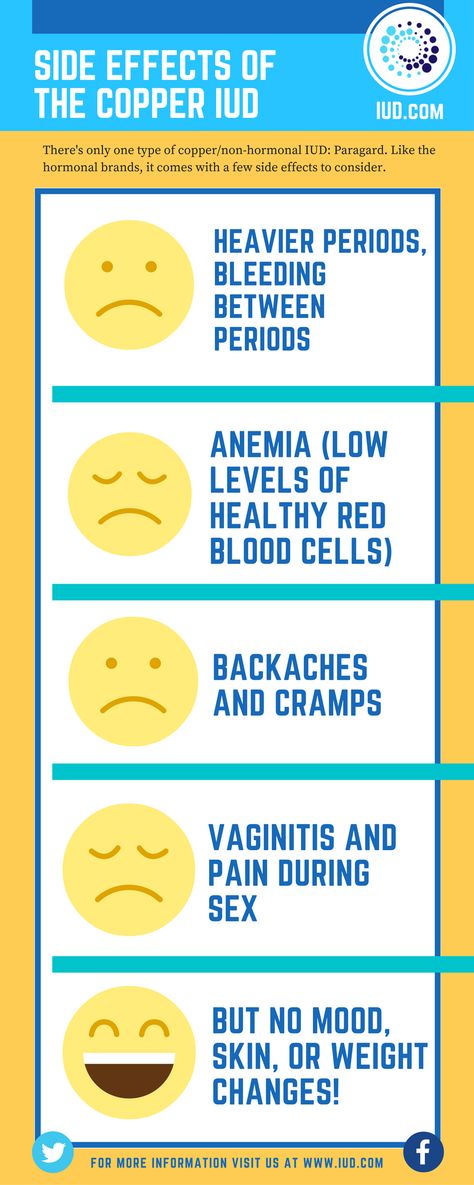 This may be because you’re moving around a lot. If this happens, try to stay off your feet and rest a little.
This may be because you’re moving around a lot. If this happens, try to stay off your feet and rest a little.
It’s also normal to sometimes feel a gush of blood when you stand. This is because of the way your vagina is shaped. The blood collects in a cup-like area while you’re sitting or lying down. When you stand, it comes out.
After about 10 days, you should see less blood. You may have light bleeding or spotting for up to 6 weeks after delivery. You can only use sanitary pads during this time. Tampons could lead to an infection.
When to Call Your Doctor
Heavy bleeding after giving birth is called postpartum hemorrhage. It affects up to 5% of women who give birth. It’s most likely to happen the first 24 hours after delivery. But it can happen anytime within the first 12 weeks after your baby is born.
Postpartum hemorrhage is serious. It can cause a big drop in your blood pressure. If the pressure gets too low, your organs won’t get enough blood. This is shock, and it can cause death. That’s why it’s important to get medical help right away.
That’s why it’s important to get medical help right away.
Tell your doctor or call 911 if you have any of these symptoms or signs:
- Bright red bleeding beyond the third day after birth
- Blood clots bigger than a plum
- Bleeding that soaks more than one sanitary pad an hour and doesn’t slow down or stop
- Blurred vision
- Chills
- Clammy skin
- Rapid heartbeat
- Dizziness
- Weakness
- Nausea
- Faint feeling
What Causes It?
Certain things can raise your chance of postpartum hemorrhage. You’re at higher risk if you’ve had it before. For unknown reasons, Asian and Hispanic women are more likely to have it.
The most common cause of postpartum hemorrhage is something called uterine atony. Normally, the uterus squeezes after delivery to stop bleeding where the placenta was. The placenta is an organ that grows in your uterus during pregnancy and nourishes your baby. With uterine atony, the uterus doesn’t contract as well as it should. This can cause heavy bleeding after you give birth.
This can cause heavy bleeding after you give birth.
You may be more likely to have this if you:
- Give birth to more than one child at a time (twins, for example)
- Have a baby bigger than 8 pounds 13 ounces
- Are in labor for a long time
- Have given birth several times before
Other conditions can raise your risk for postpartum hemorrhage. These include:
- Uterine rupture -- when the uterus tears during labor
- Cesarean section -- your risk for postpartum hemorrhage is higher compared with a vaginal delivery
- Tears in the vagina or cervix during delivery
- General anesthesia -- this may be used if you have a Cesarean section
- Oxytocin (Pitocin) -- a medicine that makes you go into labor
- Preeclampsia -- high blood pressure and protein in your urine that develops during pregnancy
- Obesity
- Issues that affect the placenta
How It's Treated
There are many different treatments for postpartum hemorrhage. The cause of your bleeding will help your doctor decide what may be best for you.
The cause of your bleeding will help your doctor decide what may be best for you.
They could:
- Give you medicine to help your uterus contract
- Massage your uterus
- Remove pieces of the placenta still in your uterus
- Perform a laparotomy -- surgery to open your abdomen to find out the cause of bleeding and stop it
- Give you a blood transfusion -- blood is given to you through a tube that goes in a vein to help replace blood you've lost
- Perform a hysterectomy -- surgical removal of the uterus
- Give you a shot of a special medicine to stop the bleeding
- Have a radiologist do what's called a uterine artery embolization, which limits blood flow to your uterus
- Use something called a Bakri balloon that's inflated inside your uterus and adds pressure to help slow the bleeding
Complications after childbirth - causes and consequences
- Increased discharge
- Retention of part of the placenta in the uterine cavity
- Changes in the blood coagulation system
- Disorder of uterine muscle contraction
- Inflammatory process in the vagina or uterus
- Vaginal candidiasis (thrush)
- Postpartum endometritis
- Laktostasis and mastitis
- Postpartum pyelonephritis
- Venous thrombosis
- Discomfort in the area of postoperative sutures
- Urinary incontinence, feces, uterine prolapse
- Hemorrhoids
After giving birth, a woman often thinks that all worries and anxieties are behind her. But, alas, sometimes the first, happiest days or weeks of the life together of mother and baby can be overshadowed by various complications. In what cases are postpartum changes normal, and when should you see a doctor?
But, alas, sometimes the first, happiest days or weeks of the life together of mother and baby can be overshadowed by various complications. In what cases are postpartum changes normal, and when should you see a doctor?
Labor ends after the third stage of labor, that is, after the birth of the placenta. Following this, the uterus immediately significantly decreases in size, becomes spherical, its cavity is filled with blood clots; the bottom of the uterus at this moment is located approximately in the middle between the womb and the navel. The early postpartum period lasts for 2 hours and during this time the woman is in the maternity ward. Then comes the late postpartum period. This period lasts 6-8 weeks. During this time, there is a reverse development (involution) of all organs and systems that have undergone changes due to pregnancy and childbirth. The exception is the mammary glands, whose function reaches its peak precisely in the postpartum period. The most pronounced involutional changes occur in the genital organs, especially in the uterus. The rate of involutional changes is most pronounced in the first 8-12 days. The uterus and cervix are significantly reduced in size. After the birth of the placenta, a large wound surface remains in the uterus, which takes about 4-6 weeks to heal. During this period, the placental site in the uterus bleeds, spotting - lochia - in the first days is bloody in nature, gradually their color changes from red to reddish-brown, brownish, by the 4th week the discharge almost stops and soon disappear completely. In women who have undergone a cesarean section, everything happens more slowly, because, due to the presence of a suture on the uterus, it contracts worse. Their total amount of spotting during the postpartum period is 500-1500 ml.
The rate of involutional changes is most pronounced in the first 8-12 days. The uterus and cervix are significantly reduced in size. After the birth of the placenta, a large wound surface remains in the uterus, which takes about 4-6 weeks to heal. During this period, the placental site in the uterus bleeds, spotting - lochia - in the first days is bloody in nature, gradually their color changes from red to reddish-brown, brownish, by the 4th week the discharge almost stops and soon disappear completely. In women who have undergone a cesarean section, everything happens more slowly, because, due to the presence of a suture on the uterus, it contracts worse. Their total amount of spotting during the postpartum period is 500-1500 ml.
What complications can occur after childbirth
You should consult a gynecologist in the following cases:
Increased amount of discharge
discharge does not stop for a long time, large blood clots appeared. When bleeding occurs, you need to contact an obstetrician-gynecologist, preferably at the maternity hospital where the birth took place. If the bleeding is very heavy (several pads are required within an hour), you do not need to go to the hospital yourself, you need to call an ambulance.
If the bleeding is very heavy (several pads are required within an hour), you do not need to go to the hospital yourself, you need to call an ambulance.
Retention of part of the placenta in the uterine cavity
The most common cause of late postpartum hemorrhage (that is, those that occur later than 2 hours after birth) is the retention of a part of the placenta in the uterine cavity. The diagnosis in this case is confirmed by ultrasound. To remove the remnants of the placenta, the walls of the uterus are scraped under general intravenous anesthesia with mandatory subsequent antibiotic therapy to prevent infectious complications.
Changes in the blood coagulation system
In rare cases, the causes of bleeding may be changes in the blood coagulation system of a hereditary or acquired nature, blood diseases. In these cases, complex drug therapy is required.
Violation of contraction of the muscles of the uterus
Development of bleeding associated with impaired contraction of the muscles of the uterus is possible. This is the so-called hypotonic bleeding. In the subsequent period, the hypotonic state of the uterus can be caused by its overstretching due to polyhydramnios, multiple pregnancies, large fetuses, and underdevelopment of the uterus. A decrease in the contractility of the uterus is also caused by changes in its very wall (fibroids, the consequences of inflammatory processes, frequent abortions). These bleeding most often occur in the first hours after childbirth and require active treatment with medications, and in severe cases, surgery.
This is the so-called hypotonic bleeding. In the subsequent period, the hypotonic state of the uterus can be caused by its overstretching due to polyhydramnios, multiple pregnancies, large fetuses, and underdevelopment of the uterus. A decrease in the contractility of the uterus is also caused by changes in its very wall (fibroids, the consequences of inflammatory processes, frequent abortions). These bleeding most often occur in the first hours after childbirth and require active treatment with medications, and in severe cases, surgery.
A sharp, unexpected cessation of spotting should also alert the woman and requires urgent medical attention. In this case, the outflow of blood from the uterus may be disturbed, that is, lochia accumulate in the cavity and the so-called lochiometer develops. Blood clots are a good breeding ground for bacteria, so if the lochiometer is not treated in time, bacteria enter the uterine cavity and endometritis develops - inflammation of the uterine mucosa. After a caesarean section, a lochiometer occurs more often than after a vaginal delivery. Treatment consists in prescribing drugs that reduce the uterus, while using antispasmodics to relax the cervix and restore the outflow of lochia. In some cases, it is necessary to resort to vacuum aspiration of the contents of the uterus under general intravenous anesthesia and mandatory follow-up antibiotic therapy.
After a caesarean section, a lochiometer occurs more often than after a vaginal delivery. Treatment consists in prescribing drugs that reduce the uterus, while using antispasmodics to relax the cervix and restore the outflow of lochia. In some cases, it is necessary to resort to vacuum aspiration of the contents of the uterus under general intravenous anesthesia and mandatory follow-up antibiotic therapy.
Learn more about the services:
- Ultrasound of the pelvic organs
Inflammatory process in the vagina or uterus
The discharge has acquired an unpleasant odor. This may indicate the development of an inflammatory process in the vagina or in the uterus. In the postpartum period, there was a significant increase in the composition of most groups of bacteria, including bacteroids, Escherichia coli, streptococci, staphylococci. Potentially, all of these species can be the cause of postpartum infectious diseases. A common problem for women after childbirth is the development of bacterial vaginosis.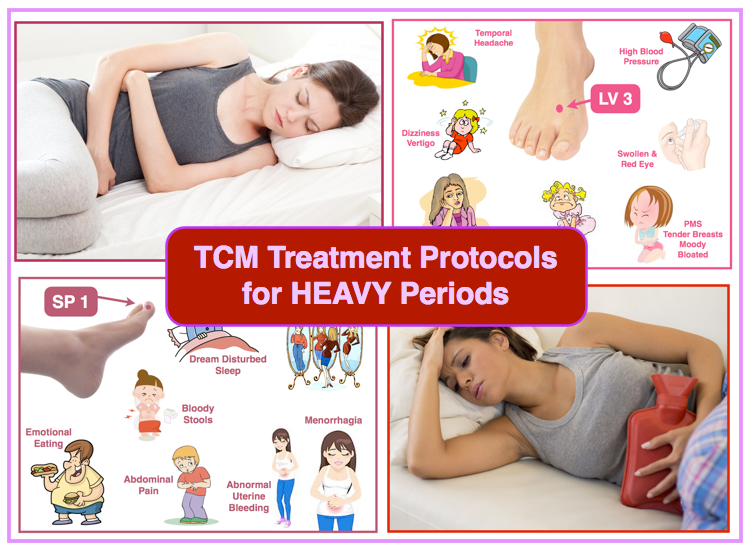 Bacterial vaginosis is a pathology of the vaginal ecosystem caused by the increased growth of predominantly anaerobic bacteria (that is, those that grow in an oxygen-free environment) that actively proliferate in the postpartum period in the woman's vagina and can be pathogens in postpartum endometritis or suppuration of the sutures of the vagina and cervix. Diagnosis of bacterial vaginosis is based on measuring the acidity of the vagina and detecting in a smear on the flora specific for this disease "key cells" (these are cells of the vaginal mucosa covered with anaerobic bacteria). Treatment of bacterial vaginosis in the postpartum period is carried out with local preparations.
Bacterial vaginosis is a pathology of the vaginal ecosystem caused by the increased growth of predominantly anaerobic bacteria (that is, those that grow in an oxygen-free environment) that actively proliferate in the postpartum period in the woman's vagina and can be pathogens in postpartum endometritis or suppuration of the sutures of the vagina and cervix. Diagnosis of bacterial vaginosis is based on measuring the acidity of the vagina and detecting in a smear on the flora specific for this disease "key cells" (these are cells of the vaginal mucosa covered with anaerobic bacteria). Treatment of bacterial vaginosis in the postpartum period is carried out with local preparations.
Vaginal candidiasis (thrush)
The appearance of curdled discharge, itching, burning in the genital area, redness indicates the development of vaginal candidiasis (thrush). The risk of this complication increases with antibiotics. Diagnosis is based on the detection of a large number of yeast-like fungi in a smear on the flora.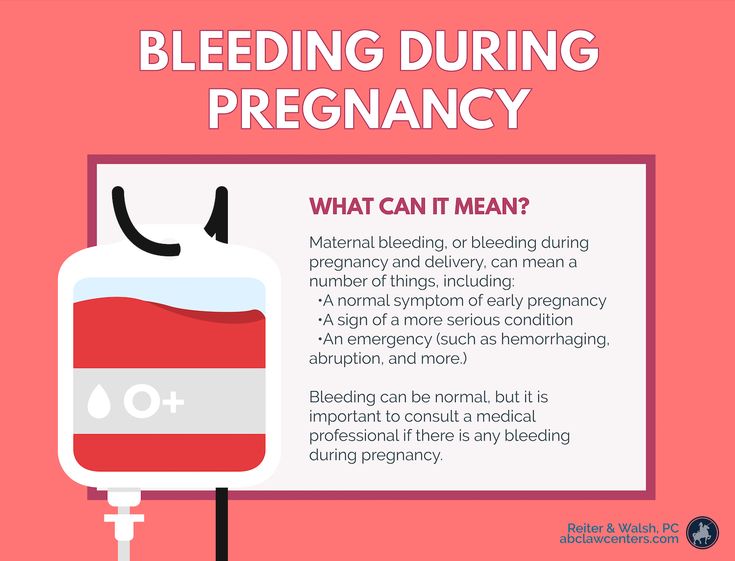 For treatment, local preparations are used in the form of vaginal suppositories or tablets.
For treatment, local preparations are used in the form of vaginal suppositories or tablets.
Postpartum endometritis
Purulent discharge, lower abdominal pain, fever. These symptoms may indicate the development of a serious complication - postpartum endometritis (inflammation of the inner lining of the uterus). Most often, endometritis occurs in patients after cesarean section, manual examination of the postpartum uterus, manual separation of the placenta and removal of the placenta (if independent separation of the placenta is difficult due to a violation of the contractile function of the uterus), with a long anhydrous interval (more than 12 hours from the moment of amniotic fluid outflow to the birth of a baby), in women admitted to childbirth with inflammatory diseases of the genital tract (for example, against the background of sexually transmitted infections), in patients with a large number of abortions in the past. The classic form of endometritis occurs on days 1-5.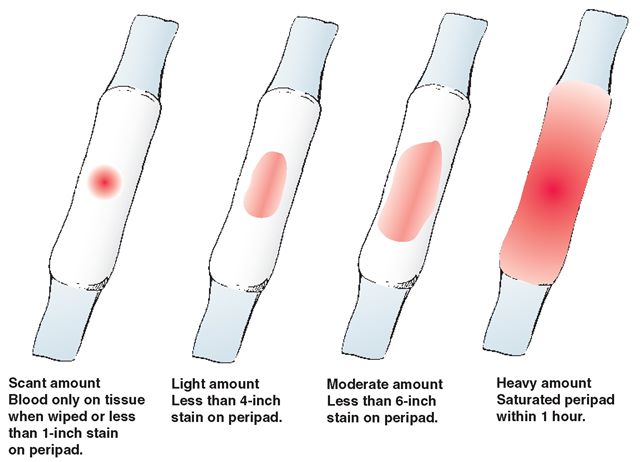 Body temperature rises to 38-39degrees, heart rate increases to 80-100 beats per minute. They note depression of the general condition, chills, dryness and hyperemia of the skin, soreness of the body of the uterus, purulent discharge with a smell. The erased form appears on the 5-7th day, develops sluggishly. The temperature does not exceed 38 degrees, there is no chill. Endometritis after caesarean section always proceeds in a severe form.
Body temperature rises to 38-39degrees, heart rate increases to 80-100 beats per minute. They note depression of the general condition, chills, dryness and hyperemia of the skin, soreness of the body of the uterus, purulent discharge with a smell. The erased form appears on the 5-7th day, develops sluggishly. The temperature does not exceed 38 degrees, there is no chill. Endometritis after caesarean section always proceeds in a severe form.
An ultrasound examination of the uterus and a complete blood count, which reveal signs of inflammation, help the doctor make a diagnosis. Treatment of endometritis should be started as early as possible. It is carried out in a hospital. Assign bed rest, with acute endometritis cold on the lower abdomen. Postpartum endomeritis is necessarily treated with antibiotics, along with them, agents that reduce the uterus are used. Currently, in many clinics and maternity hospitals, the uterine cavity is washed with cooled solutions of antiseptics. In severe cases, an intravenous infusion of saline solutions is required to improve blood circulation, relieve symptoms of intoxication.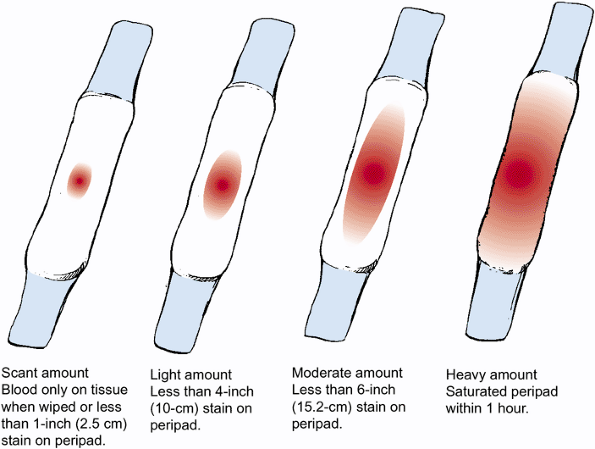
In case of untimely treatment, there is a very high risk of spreading the inflammatory process to the entire uterus, small pelvis, the development of sepsis (the appearance of infectious agents in the blood), up to the death of the patient.
Laktostasis and mastitis
In the postpartum period, there may be pain in the mammary glands, a feeling of fullness, an increase in body temperature. When these symptoms appear, you should definitely consult a doctor - an obstetrician-gynecologist in a antenatal clinic or a surgeon.
Possible causes of pain in the mammary glands and the accompanying fever are lactostasis and mastitis.
Laktostasis (stagnation of milk in the gland), due to blockage of the excretory ducts. Most often, this condition develops when the baby is not properly attached to the chest, violation of the feeding regimen. Laktostasis often affects primiparous women. With the stagnation of milk, the mammary gland increases in volume, its dense enlarged lobules are determined. Body temperature can rise to 38-40 degrees. There is no redness of the skin and swelling of the gland tissue, which usually appear with inflammation. After decanting the mammary gland with lactostasis, the pain disappears, painless lobules with clear contours are small in size, and the body temperature decreases. If lactostasis is not eliminated within 3-4 days, mastitis (inflammation of the mammary gland) occurs, since when milk stagnates, the number of microbial cells in the milk ducts increases dramatically, milk is a good breeding ground for various bacteria, which contributes to the rapid progression of inflammation. With the development of mastitis, the body temperature constantly remains high, accompanied by chills. Symptoms of intoxication appear (general weakness, fatigue, headache). The patient is disturbed first by a feeling of heaviness, and then by pain in the mammary gland, which is accompanied by stagnation of milk. The mammary gland increases in volume, areas of redness are noted on the skin.
Body temperature can rise to 38-40 degrees. There is no redness of the skin and swelling of the gland tissue, which usually appear with inflammation. After decanting the mammary gland with lactostasis, the pain disappears, painless lobules with clear contours are small in size, and the body temperature decreases. If lactostasis is not eliminated within 3-4 days, mastitis (inflammation of the mammary gland) occurs, since when milk stagnates, the number of microbial cells in the milk ducts increases dramatically, milk is a good breeding ground for various bacteria, which contributes to the rapid progression of inflammation. With the development of mastitis, the body temperature constantly remains high, accompanied by chills. Symptoms of intoxication appear (general weakness, fatigue, headache). The patient is disturbed first by a feeling of heaviness, and then by pain in the mammary gland, which is accompanied by stagnation of milk. The mammary gland increases in volume, areas of redness are noted on the skin. Pumping milk is painful and does not bring relief, after pumping, dense painful areas remain, and a high body temperature persists. In severe cases, pus impurities can be determined in milk.
Pumping milk is painful and does not bring relief, after pumping, dense painful areas remain, and a high body temperature persists. In severe cases, pus impurities can be determined in milk.
To eliminate lactostasis, pumping, local anti-inflammatory ointments, and physiotherapy are used. Mastitis is treated with antibiotics. In some cases, lactation suppression and surgical treatment are required.
Postpartum pyelonephritis
Fever, pain in the back or side, painful urination. These symptoms may indicate the development of postpartum pyelonephritis, that is, inflammation of the kidneys. Critical periods for the development of postpartum pyelonephritis, doctors consider 4-6 and 12-14 days of the postpartum period. The development of the disease is associated with infection in the urinary tract from the genital tract. Most often, the disease develops in puerperas, in the urine of which a small amount of bacteria was found during pregnancy. An ultrasound examination of the kidneys and bladder and a urine test help the doctor make the diagnosis.
Treatment of pyelonephritis is mandatory with antibiotics.
Venous thrombosis
Pain in the legs, swelling, redness on the legs along the vein, increased pain when walking - these are symptoms of a serious pathology - venous thrombosis (formation of blood clots in the veins) and require an urgent visit to a surgeon or phlebologist. The most dangerous periods for the occurrence of thrombosis are considered 5-6 days after childbirth or cesarean section, less often thrombosis occurs 2-3 weeks after childbirth. The causes of thrombosis are changes in the blood coagulation system that occur during pregnancy and after childbirth. Physiologically, in the postpartum period, the activation of the coagulation system occurs. As the body tries to stop bleeding. At the same time, the tone of the vessels of the small pelvis and lower extremities is reduced, the veins have not yet had time to adapt to work in new conditions. These conditions trigger the mechanisms of thrombus formation.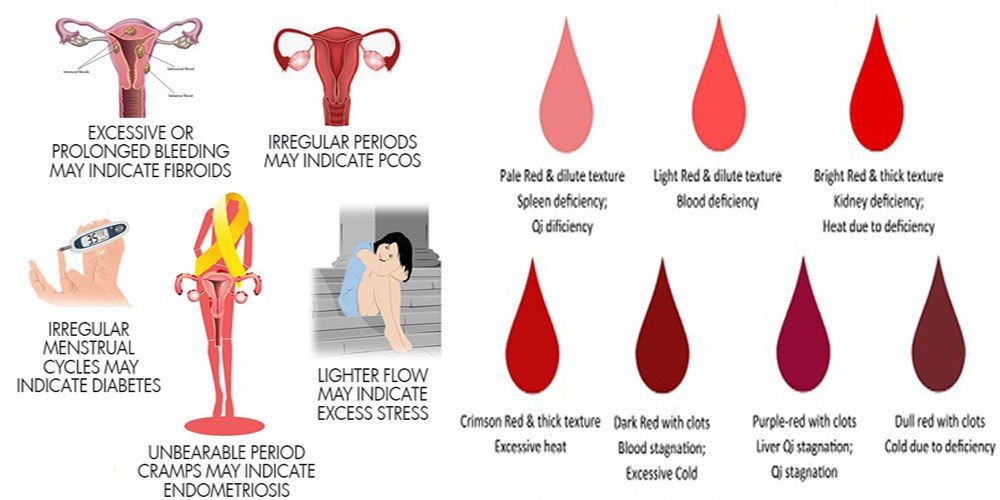 An important role in the development of postpartum venous thrombosis is also played by the hormonal background, which changes dramatically after the end of pregnancy.
An important role in the development of postpartum venous thrombosis is also played by the hormonal background, which changes dramatically after the end of pregnancy.
The risk of developing venous thrombosis is especially high in women with various pathologies of the blood coagulation system, which are detected even before pregnancy or during childbearing. There is a high probability of thromboembolic complications and in the presence of diseases of the cardiovascular system, overweight. The risk of thrombosis also increases in women in the age group after 40 years, in the presence of varicose veins of the lower extremities. The risk of thrombus formation is increased in women who have undergone a caesarean section. An ultrasound examination of the veins, with Dopplerography, that is, an assessment of blood flow in the vessels, helps the doctor in making a diagnosis. For the treatment of venous thrombosis, medications are used, wearing compression stockings.
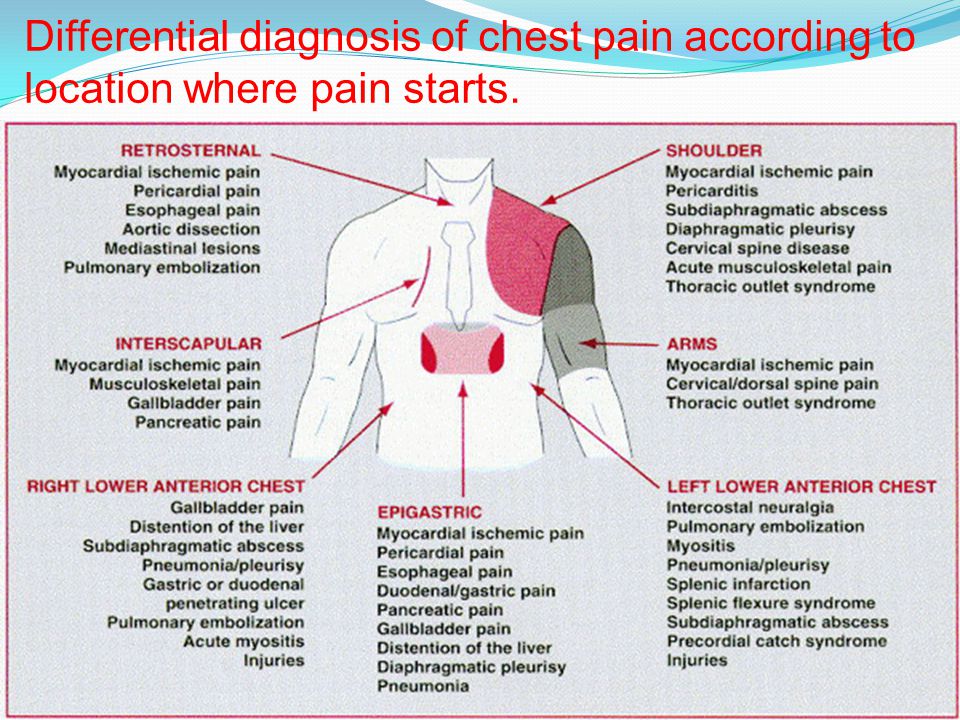
A severe complication of venous thrombosis is the detachment of part of the thrombus and its movement along the vascular bed. In this case, blood clots, entering the vessels of the lung or brain, cause strokes (impaired cerebral circulation) or pulmonary embolism (blockage of the pulmonary arteries by a thrombus). This serious complication appears as a sharp cough, shortness of breath, pain in the chest, hemoptysis may begin - the appearance of blood streaks in the sputum when coughing. In severe cases, the work of the heart is disrupted and death can occur.
In this case, blood clots, entering the vessels of the lung or brain, cause strokes (impaired cerebral circulation) or pulmonary embolism (blockage of the pulmonary arteries by a thrombus). This serious complication appears as a sharp cough, shortness of breath, pain in the chest, hemoptysis may begin - the appearance of blood streaks in the sputum when coughing. In severe cases, the work of the heart is disrupted and death can occur.
Unpleasant sensations in the area of postoperative sutures
Discomfort in the area of postoperative sutures after caesarean section or in the area of sutures on the perineum. Normally, after suturing vaginal tears, there may be slight pain for 1-2 days, but they quickly pass. Pain in the postoperative wound after cesarean section may be disturbing for 2 weeks, gradually decreasing. Feeling of heaviness, fullness, pain in the area of the postoperative wound may indicate the accumulation of hematoma (blood) in the area of the sutures. This usually happens in the first three days after childbirth and requires surgical treatment - removal of accumulated blood. Pain, burning, bleeding of the sutures, the appearance of discharge with an unpleasant odor, swelling in the area of the sutures, an increase in body temperature indicates the attachment of an infection and suppuration of the sutures. In these cases, you should also consult a doctor to treat the wound and decide on a further method of treatment.
This usually happens in the first three days after childbirth and requires surgical treatment - removal of accumulated blood. Pain, burning, bleeding of the sutures, the appearance of discharge with an unpleasant odor, swelling in the area of the sutures, an increase in body temperature indicates the attachment of an infection and suppuration of the sutures. In these cases, you should also consult a doctor to treat the wound and decide on a further method of treatment.
Urinary incontinence, feces, uterine prolapse
Violation of the physiological functions of the pelvic organs of varying degrees (bladder, rectum), which may appear as in the postpartum period - urinary incontinence, feces, uterine prolapse. The problem of genital prolapse occurs when the pelvic floor muscles have lost the ability to contract so much that individual organs or parts of them do not fall into the projection of the supporting apparatus. The most common cause of pelvic organ prolapse is trauma to the pelvic floor muscles during childbirth.
Hemorrhoids
Quite often, after childbirth, women are worried about the appearance of hemorrhoids - varicose veins of the rectum. The predisposing factor in this case is a significant increase in intra-abdominal pressure during pregnancy and during childbirth. In the case of hemorrhoids, formations appear in the anus, which can be painless, but most often - painful, bleeding and itchy. The appearance of intense pain in the anus, bloody discharge from the rectum are a reason to consult a doctor - a proctologist. Most often, uncomplicated forms of hemorrhoids are treated with local medications - creams and suppositories, in case of complications (nodule pinching, bleeding), surgical treatment is required.
In any case, if you experience any symptoms that cause concern, it is advisable to consult a doctor, because any complication is best prevented or treated at the very initial stage.
Causes of heavy periods after childbirth
Pregnancy and childbirth are a period of significant changes in a woman's life. These periods cause a real hormonal storm in the body, and often lead to changes in familiar areas such as the menstrual cycle.
These periods cause a real hormonal storm in the body, and often lead to changes in familiar areas such as the menstrual cycle.
Please remember that the body after childbirth requires special attention. Take care of yourself and in case of any doubt, consult a doctor.
First of all, let's talk about the difference between postpartum hemorrhage (lochia) and menstruation.
What are lochia?
Lochia should be distinguished from heavy first menstruation after childbirth. Lochia is profuse bleeding from the vagina that begins immediately after childbirth. During them, the vagina gets rid of the thick layer of endometrium formed during pregnancy. They are usually dark red in color and abound in blood clots. Lochia is NOT menstruation, they should be considered as a sign of recovery of the body after childbirth. Usually they last 24-36 days, ie. 3-5 weeks. Over time, they become less abundant and change color: they become pink or transparent. Despite the similarity with menstruation, they should be distinguished. During lochia, there are also cramps, as well as during menstruation, because the uterus contracts, returning to its normal size and getting rid of excess endometrium. Lochia differs from menstruation in that it becomes lighter over time, while menstrual blood tends to darken towards the end of the cycle.
Despite the similarity with menstruation, they should be distinguished. During lochia, there are also cramps, as well as during menstruation, because the uterus contracts, returning to its normal size and getting rid of excess endometrium. Lochia differs from menstruation in that it becomes lighter over time, while menstrual blood tends to darken towards the end of the cycle.
What to do when lochia comes?
Bleeding is usually very heavy at first, and in the hospital you will most likely need special gynecological pads or panties for adults. As soon as the bleeding subsides, you can start using the usual sanitary pads.
The body is weakened at this time, so it is especially important to monitor hygiene and change pads in time so as not to infect.
Do not use tampons unless your doctor tells you to. When the lochia is completely weakened and brightened, you can switch to daily pads and wait for the first menstruation after childbirth.
What to expect from menstruation after childbirth?
If you are not breastfeeding, your period is likely to start 1-3 months after giving birth, but if you are breastfeeding only, your period may not return for the entire period of breastfeeding. However, for many breastfeeding women, menstruation also returns after a couple of months. This is due to the hormone prolactin, which is responsible for the production of breast milk. It can suppress other sex hormones, thereby preventing ovulation and thus menstruation. But most often in women who are breastfeeding, the menstrual cycle is restored 6 months after childbirth.
If menstruation returned quickly, and the birth was vaginal (not caesarean section), then you should not use tampons for the first time, because the body is still recovering, and give preference gaskets.
Often after childbirth, the very nature of menstruation changes: in some women it becomes more abundant, and in others it is easier. Often, the cycle is unstable for some time, but eventually returns to normal. Unfortunately, there is no way to predict what changes await a woman after childbirth in this regard.
Often, the cycle is unstable for some time, but eventually returns to normal. Unfortunately, there is no way to predict what changes await a woman after childbirth in this regard.
Childbirth is a huge burden for the body, and it will take some time to recover. There is no gold standard for the postpartum recovery period; it is individual for each woman. If you are in any doubt, it is always best to consult a doctor.
Why do periods change after childbirth?
-
The uterus should return to normal size
-
Breastfeeding affects the cycle and hormones
-
Hormonal imbalance
How can menstruation change after childbirth?
-
Pain in the lower abdomen may become worse or vice versa less
-
Blood clots may appear
-
Unstable menstrual cycle
-
Abrupt onset and end of bleeding
-
More profuse periods
Why are the first periods after childbirth heavy and what is heavy menstruation?
Very often the very first periods after pregnancy and childbirth are more abundant than usual. Heavy periods - such periods when a woman has to use one pad or tampon per hour for several hours in a row (more than 80 ml of fluid per cycle) and / or which last more than 7 days, they are also called "menorrhagia". On the other hand, bleeding in women is different, and what is normal and normal for one is unusual and strange for another, so you should focus on what kind of menstruation is typical for you.
Heavy periods - such periods when a woman has to use one pad or tampon per hour for several hours in a row (more than 80 ml of fluid per cycle) and / or which last more than 7 days, they are also called "menorrhagia". On the other hand, bleeding in women is different, and what is normal and normal for one is unusual and strange for another, so you should focus on what kind of menstruation is typical for you.
Often, the first menstruation is characterized by increased soreness, because the mucous membrane of the uterus, even after childbirth, is still thicker than its usual state before menstruation.
Most likely, over time, everything will return to normal, but some discomfort is possible in the first months due to the amount of discharge. To avoid trouble with leakage during heavy periods with clots, you can use night panty liners Kotex Ultra Night. They quickly absorb even the heaviest of secretions thanks to their unique 3D center, while special elastic grooves along the pad give it flexibility and provide additional protection against back leaks.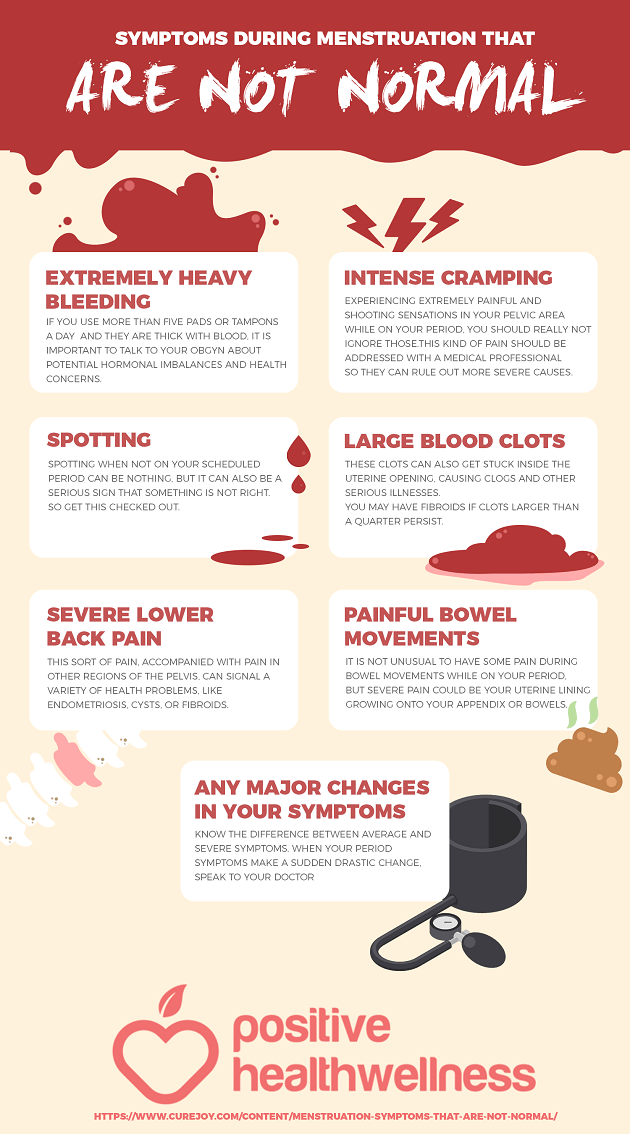 Adjustable inner layer adapts perfectly to body shape and posture. Suitable for this occasion Kotex Natural Night: They have the same benefits as Kotex Ultra Night, and are ideal for women with sensitive skin. You can buy these pads in stores and pharmacies, as well as order on the Internet.
Adjustable inner layer adapts perfectly to body shape and posture. Suitable for this occasion Kotex Natural Night: They have the same benefits as Kotex Ultra Night, and are ideal for women with sensitive skin. You can buy these pads in stores and pharmacies, as well as order on the Internet.
What symptoms should I look out for?
Although many cycle changes after childbirth are normal, some symptoms still require medical attention:
-
Sudden heat and high temperature
-
Very heavy periods (you have to change the pad with the maximum degree of absorption more than once an hour, such intense bleeding lasts more than 2 hours)
-
Menstruation lasts longer than 7 days
-
Breathing difficulties
-
Severe headaches
-
Very large blood clots (larger than a ping-pong ball)
-
Sharp, sharp pain at the onset of bleeding
Please remember that excessive bleeding can lead to anemia and weakness, women with heavy periods need to monitor the level of iron and ferritin in the blood.
What methods of correction of heavy periods can doctors suggest?
Unfortunately, sometimes heavy periods after childbirth do not return to normal and begin to interfere with normal life. In such cases, doctors can help you choose the right method for correcting this condition, depending on your state of health, the cause that causes them and personal preferences.
Here are some of them:
-
An intrauterine device is a small device containing the hormone progesterone that a doctor places inside the uterus.
-
Non-hormonal drugs - a doctor may suggest non-steroidal anti-inflammatory drugs and tranexamic acid drugs
-
Hormonal preparations such as combined oral contraceptives or progesterone tablets
-
Surgical operations correcting the cause of abnormal heavy periods (curettage of the uterine cavity, removal of fibrosis, etc.
 )
)
How can you help yourself at home if you have heavy periods?
Yes, there is little pleasure in heavy menstruation, especially if they are painful, but this does not mean that it is impossible to help yourself during this period.
-
Try using a heating pad. Heat can relieve acute cramps in the lower abdomen and reduce pain. This method works because the heat helps relax the muscles that cause uterine contractions. If you don't have a heating pad, you can pour warm water into an empty plastic bottle. Try not to pour too hot water or wrap a heating pad in a towel so as not to burn yourself.
-
At night you can use special Kotex night panties. Sleeping in them is much more comfortable than with a pad, they fit perfectly to the body in any position and protect against leaks from all sides. After all, after giving birth, most women have more important things to do than spend time worrying about stains on their underwear.