Spina bifida and pregnancy
A Pregnant Woman with Spina Bifida: Need for a Multidisciplinary Labor Plan
Introduction
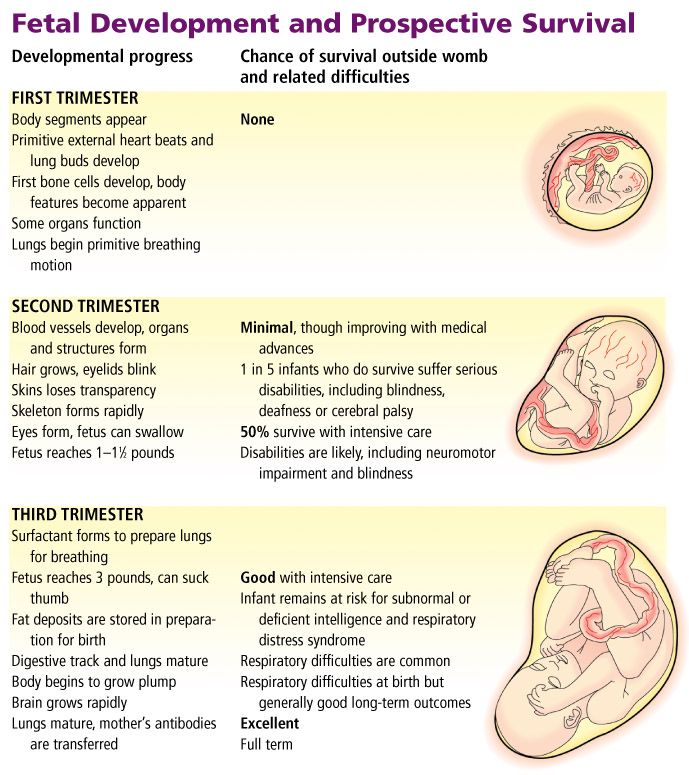
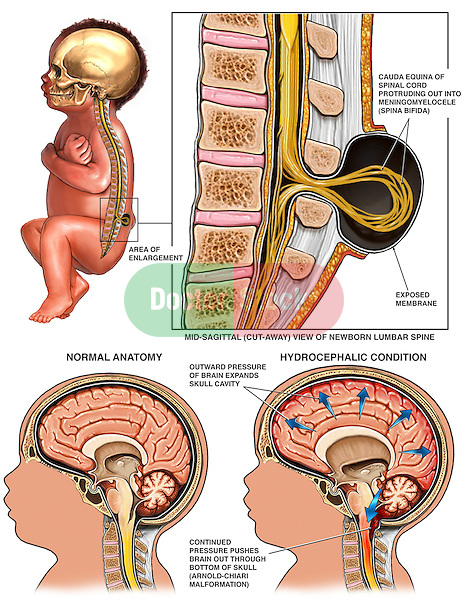
Spina bifida is caused by the failure of the neural tube to close during the first month of embryonic development. There are three main types: spina bifida occulta, meningocele, and myelomeningocele. In spina bifida occulta, the outer part of the vertebrae is not completely closed. The splits in the vertebrae are so small that the spinal cord does not protrude. A meningocele involves a defect in bony closure, which allows the meninges to herniate between the vertebrae. This is a closed spinal dysraphism where the skin is intact, but the underlying spinal cord and associated structures are abnormal. In the patient presented, there was an associated lipomatous mass. Last, in individuals who have a myelomeningocele, the unfused portion of the spinal column allows the spinal cord elements to protrude through the opening. This is an open spinal dysraphism where the malformed spinal cord segment and meninges are not covered by skin.
A tethered cord is defined as an abnormal attachment of the spinal cord to its surrounding tissues. This can occur because of abnormalities in the development in the end of the spinal cord, such as a thickened filum terminale or because of surgery for the spinal dysraphism. The radiologic diagnosis requires a low-lying conus medullaris and a thickened (more than 2 mm) filum terminale. This is distinct from the tethered cord syndrome, which refers to the neurologic symptoms such patients may display. The symptoms typically may include pain, which may be worse with exercise or flexion, lower extremity weakness, and sensory loss and bladder dysfunction (1). Patients with spina bifida often have other associated anomalies of the neural tube particularly Chiari II malformations. This malformation is characterized by cerebellar hypoplasia and caudal displacement of the lower brainstem into the upper cervical canal through the foramen magnum. This leads to impairment of cerebrospinal fluid flow causing hydrocephalus.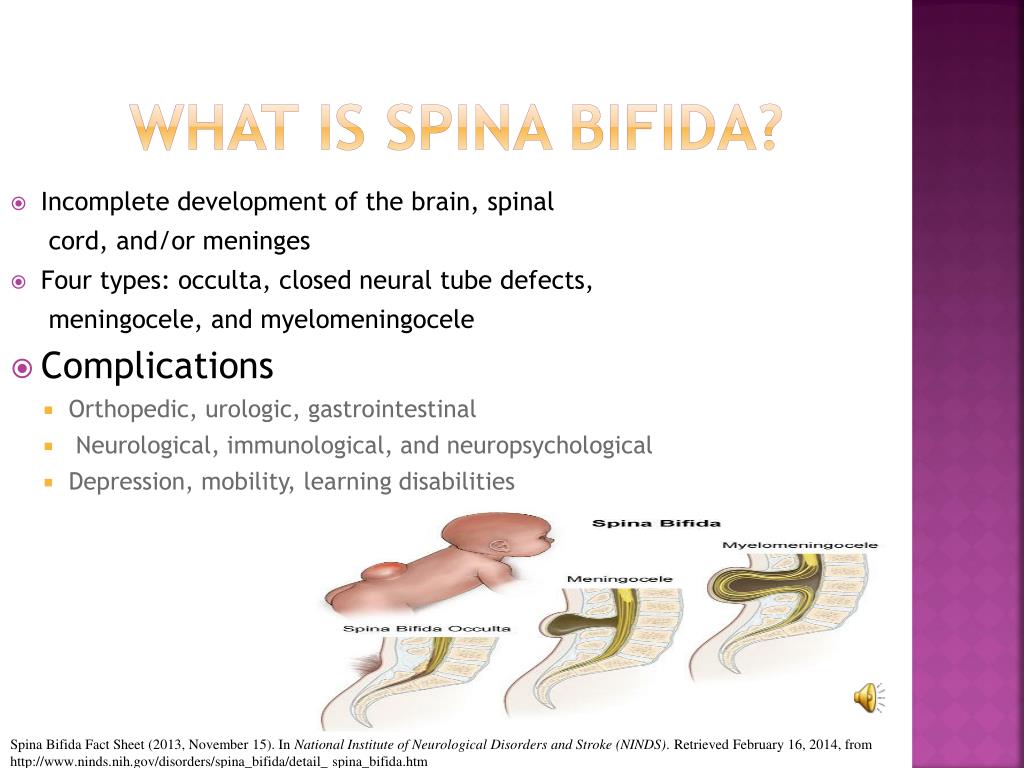 Chiari II malformations occur in more than 90% of infants with myelomeningocele. Other frequent anomalies include cortical dysplasias and abnormalities involving the corpus callosum and thalami (2).
Chiari II malformations occur in more than 90% of infants with myelomeningocele. Other frequent anomalies include cortical dysplasias and abnormalities involving the corpus callosum and thalami (2).
Case
A 34-year-old lady G1 P0, 35 weeks pregnant who had a history of surgery for spina bifida and a tethered cord was sent for neurologic evaluation to define both obstetric risks and safety of neuraxial anesthesia. She had a lipomeningocele operated on at 3 months of age. At age 10, she developed a tethered cord syndrome, which required surgery. Unfortunately, due to progressive neurologic symptoms, she required a second untethering procedure. Her neurologic impairments included weakness in legs, distal more than proximal, distal lower extremity numbness, and urinary incontinence. She required braces and crutches to walk and needed to self-catheterize.
Pertinent Findings on Neurologic Examination
Her right leg was shorter than the left with a smaller right foot.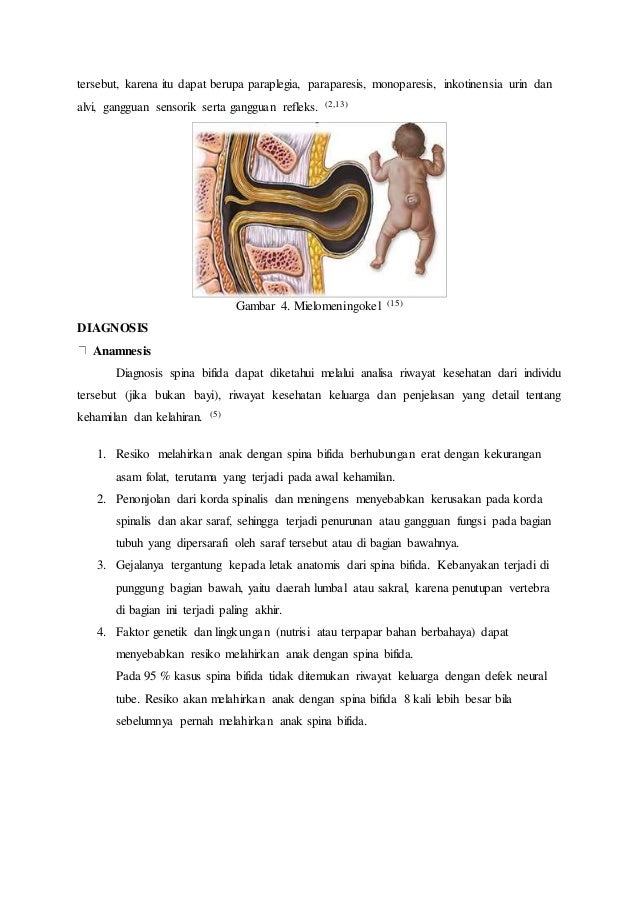 She had bilateral pes cavus deformities and hammer toes. Lower extremity strength: 4/5 hip flexors on the left, 4-/5 on the right, full hip adductors, abductors were 4/5 bilaterally. She had full knee flexion and extension strength. She has no movement of either foot with distal atrophy. Reflexes: 1+ right knee jerk, no left knee jerk, absent ankle jerks. Toes were mute. Sensation showed diminished pinprick right greater than left in an L5-S1 distribution. She could transfer from her wheelchair.
She had bilateral pes cavus deformities and hammer toes. Lower extremity strength: 4/5 hip flexors on the left, 4-/5 on the right, full hip adductors, abductors were 4/5 bilaterally. She had full knee flexion and extension strength. She has no movement of either foot with distal atrophy. Reflexes: 1+ right knee jerk, no left knee jerk, absent ankle jerks. Toes were mute. Sensation showed diminished pinprick right greater than left in an L5-S1 distribution. She could transfer from her wheelchair.
Lumbar MRI showed cord dysraphism from L4-L5 with a lipomeningocele. There were surgical changes at L3-L5. Neural elements were present to the sacrum. See Figure 1; obstetrical anesthesia was also consulted. After review of her imaging and joint consultation, the patient was offered epidural anesthesia with the plan to perform the procedure above the level of her previous surgeries. It was explained that due to her prior surgeries that the block might not be as effective and technically difficult.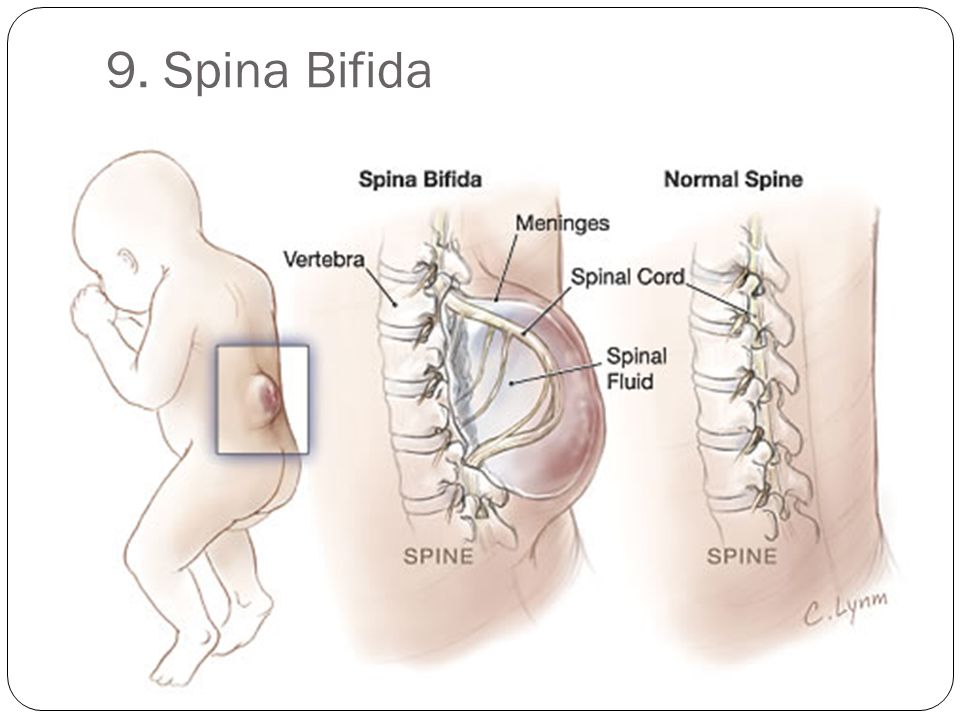 In addition, she understood that it was likely given her significant lower extremity weakness that she would require a caesarian delivery.
In addition, she understood that it was likely given her significant lower extremity weakness that she would require a caesarian delivery.
Figure 1. Axial and sagittal T2 lumbar MRI showing postsurgical changes from L3-L5 with neural elements present to the sacrum with an associated syrinx.
She presented at 39 weeks in labor. Epidural anesthesia was successfully placed at T12-L1 using ultrasound guidance. Due to failure to progress, the patient had a caesarian delivery. The epidural anesthesia provided good analgesia. A healthy baby girl was delivered.
Discussion
Obstetric Concerns
Fertility is felt to be normal in these women. However, there are no studies looking at fertility in this group of women specifically, so the best information is that extrapolated from studies of women with spinal cord injury (3). In one series of 17 women (14 had a myelomeningocele, 3 had a meningocele), antenatal complications occurred in 14/17 patients.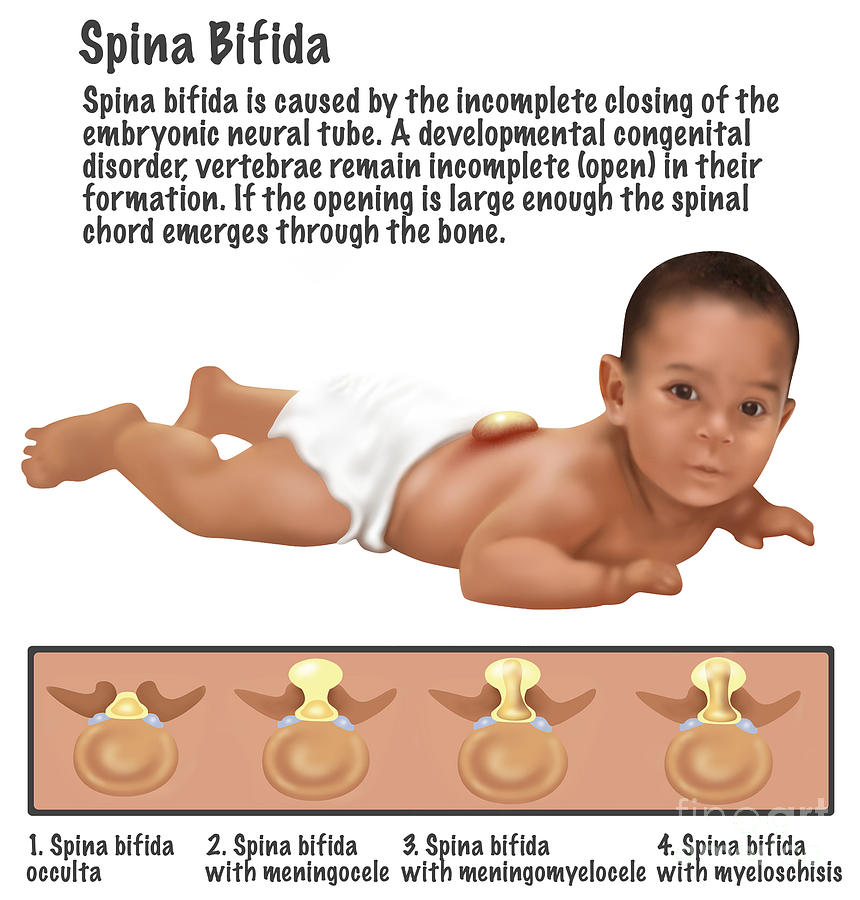 Antenatal admissions were less frequent in women who could ambulate independently as compared with those who were wheelchair dependent. The most frequent complications related to spinal bifida include urinary tract infections, stoma complications, decubitus ulcers, and worsening back pain. Severe thoracic scoliosis in the setting of pregnancy can contribute to restrictive lung disease. Many of these women may have undergone urologic procedures to improve their bladder function. This may complicate performing a caesarian delivery due to the abnormal and complex anatomy. These women also had obstetric complications with a higher frequency of hypertension and preeclampsia. Nearly half of these women required caesarian delivery; this was especially common in women who were wheelchair dependent (4).
Antenatal admissions were less frequent in women who could ambulate independently as compared with those who were wheelchair dependent. The most frequent complications related to spinal bifida include urinary tract infections, stoma complications, decubitus ulcers, and worsening back pain. Severe thoracic scoliosis in the setting of pregnancy can contribute to restrictive lung disease. Many of these women may have undergone urologic procedures to improve their bladder function. This may complicate performing a caesarian delivery due to the abnormal and complex anatomy. These women also had obstetric complications with a higher frequency of hypertension and preeclampsia. Nearly half of these women required caesarian delivery; this was especially common in women who were wheelchair dependent (4).
Neuraxial Anesthesia
There are several case reports in the literature of using epidural or combined spinal and epidural anesthesia in women who had prior surgery for their spina bifida. The complications encountered are related to the altered anatomy. These include difficulty locating the epidural space, an asymmetric block likely related to scarring, dural punctures, and the need for multiple operator attempts to place the anesthesia (5). However, reports of permanent neurologic injury after neuraxial anesthesia in such patients are rare (6).
The complications encountered are related to the altered anatomy. These include difficulty locating the epidural space, an asymmetric block likely related to scarring, dural punctures, and the need for multiple operator attempts to place the anesthesia (5). However, reports of permanent neurologic injury after neuraxial anesthesia in such patients are rare (6).
Following surgery in patients, like the one presented, the epidural space is not going to be normal. In addition, even after a detethering procedure, the conus medullaris will likely still be in an abnormally low position (as in our patient). Scoliosis with or without associated corrective surgery can further complicate the spine anatomy. These factors make the ability to perform a safe and efficacious block difficult. Careful analysis of such a patient requires a careful pre-labor analgesic plan. The plan should include a detailed neurologic exam to establish baseline motor and sensory deficits as well as an obstetrical anesthesia consult.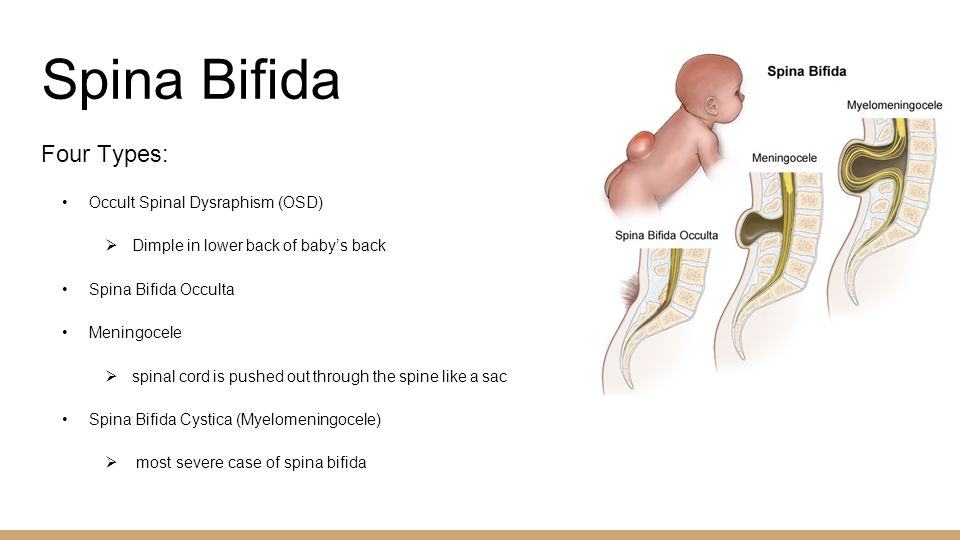 The consultants should then discuss the best patient care algorithm.
The consultants should then discuss the best patient care algorithm.
Imaging is important to look at the anatomy in detail, to locate the best level for neuraxial anesthesia. The most appropriate imaging modality is lumbar magnetic resonance imaging. The level where the cord is not too posteriorly located and the epidural space is likely to be normal is the area where a block should be attempted. Finally, a backup analgesic plan should be formulated in case the block is incomplete or unsuccessful.
Conclusion
1. Women with spina bifida have an increased risk of obstetric complications. The inability to ambulate is highly correlated with the need for a caesarian delivery.
2. Neuraxial anesthesia can be performed safely and effectively in women with spina bifida.
3. Consultations with neurology and obstetric anesthesia should occur to document a baseline neurologic exam and coordinate an appropriate pre-labor analgesic plan.
Ethics Statement
Written informed consent was obtained from the patient for the publication of this case report.
Author Contributions
The author confirms being the sole contributor of this work and approved it for publication.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Agaralla PK, Dunn IF, Scot RM, Smith ER. Tethered cord syndrome. Neurosurg Clin N Am (2007) 18:1–547.
Google Scholar
2. Gilbert JN, Jones KL, Rorke LB, Chernoff GF, James HE. Central nervous system anomalies associated with meningomyelocele, hydrocephalus, and the Arnold-Chiari malformation: reappraisal of theories regarding the pathogenesis of posterior neural tube closure defects. Neurosurgery (1986) 18(5):559–64. doi:10.1097/00006123-198605000-00008
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Jackson AB, Mott PK. Reproductive health care for women with spina bifida. Sci World J (2007) 7:1875–83. doi:10.1100/tsw.2007.304
Sci World J (2007) 7:1875–83. doi:10.1100/tsw.2007.304
CrossRef Full Text | Google Scholar
4. Arata M, Grover S, Dunne K, Bryan D. Pregnancy outcome and complications in women with spina bifida. J Reprod Med (2000) 43(9):743–8.
PubMed Abstract | Google Scholar
5. Murphy CJ, Stanley E, Kavanagh E, Lenane PE, McCaul CL. Spinal dysraphisms in the parturient: implications for perioperative anaesthetic care and labour analgesia. Int J Obstet Anesth (2015) 24:252–63. doi:10.1016/j.ijoa.2015.04.002
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Hebl JR, Horlocker TT, Schroeder DR. Neuraxial anesthesia and analgesia in patients with preexisting central nervous system disorders. Anesth Analg (2006) 103(1):223–8. doi:10.1213/01.ane.0000220896.56427.53
PubMed Abstract | CrossRef Full Text | Google Scholar
Pregnancy in women with Spina Bifida
Many women with spina bifida will have a safe and successful pregnancy, but you will probably need to plan more carefully than other women.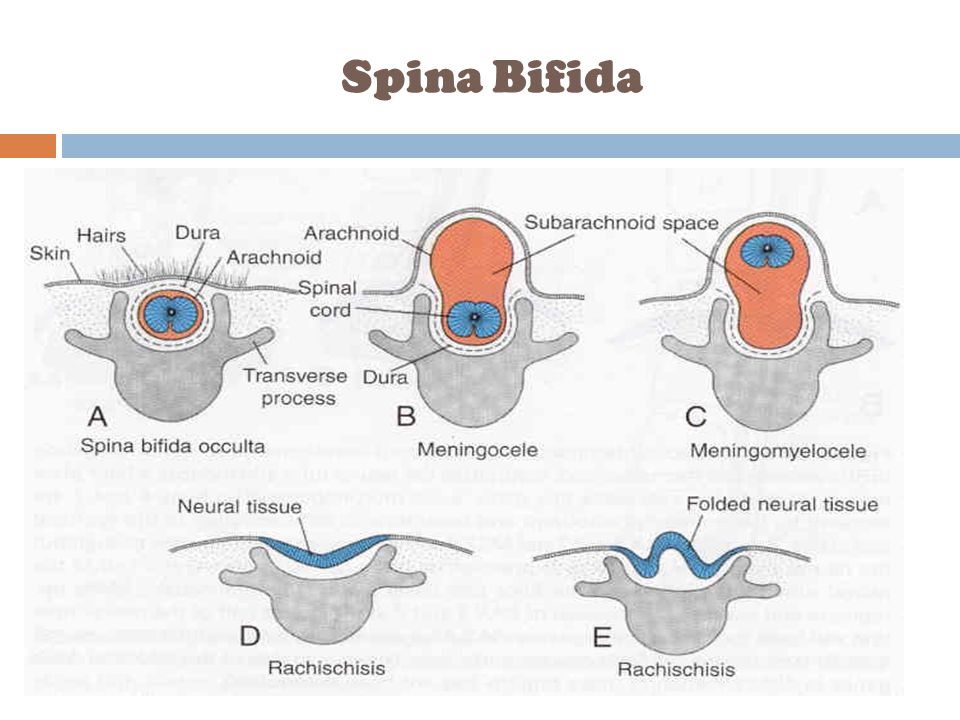 We hope this information will give you an idea of how to get ready, and what to expect, if you decide to try for a baby.
We hope this information will give you an idea of how to get ready, and what to expect, if you decide to try for a baby.
As a general rule, if you or your partner has spina bifida or you have already had a child with spina bifida, you have a 1 in 25 chance of having another baby with the condition. You may wish to see a genetic counsellor to discuss the chances of a pregnancy being affected by spina bifida or another neural tube defect. Your GP can refer you to a genetic counsellor.
- Before and during pregnancy
- Preparing for birth
- Going home with your baby
Before and During Pregnancy
Before you start your other preparation, let the doctors involved in your care know about your plans, as your care may need to change before and throughout your pregnancy.
If you choose to try to lower the chance of your baby having spina bifida or anencephaly (a fatal condition where the baby’s brain doesn’t develop), you are advised to take 5mg of folic acid (available on prescription) for around 8 weeks before you start trying to conceive.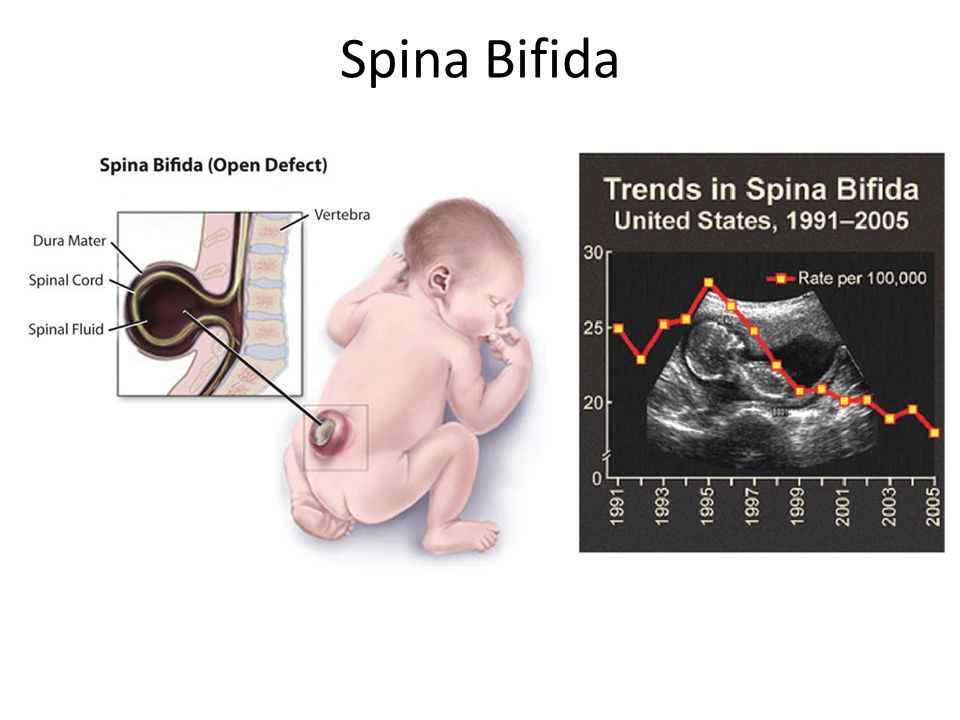 Shine also suggests you take vitamin B12, 2.5mcg for around 3 months before conceiving. This will be included in pre-pregnancy multivitamins, and will be especially important if you’re vegetarian or vegan.
Shine also suggests you take vitamin B12, 2.5mcg for around 3 months before conceiving. This will be included in pre-pregnancy multivitamins, and will be especially important if you’re vegetarian or vegan.
Epilepsy
If you take epilepsy medication, let your neurologist know. Some epilepsy medication, such as sodium valproate are associated with several health problems in babies, and you may be advised to change medication. This would need to be done gradually, under close supervision to make sure your epilepsy is well controlled, and this can take many months to do safely. Your medication dose may need to be changed during pregnancy,as your blood volume increases.
Weight
You are advised to be at a healthy weight before you start trying for a baby.
A BMI between 18.5 and 24.9 is considered healthy, which is around 9 stones for a woman of 5 feet 5 inches. Being under- or overweight can result in health problems for you and your baby, and it could take you much longer to fall pregnant.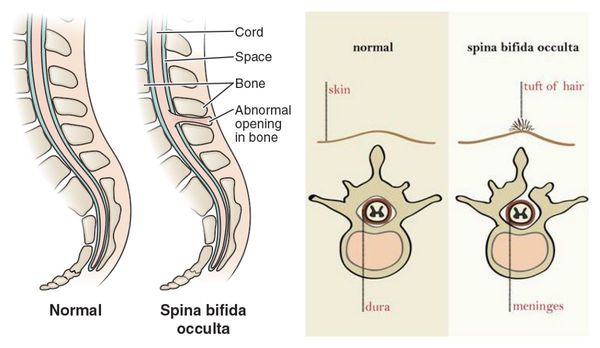
Kidneys
If you have any renal problems, you would need to take advice from your Urologist or Nephrologist to see whether pregnancy would be safe for you. As pregnancy goes along, your blood volume will increase about 30%, and all this extra blood needs ‘cleaning’ by the kidneys. If you’ve never had kidney problems, ask your GP for a blood test just to check everything is still OK.
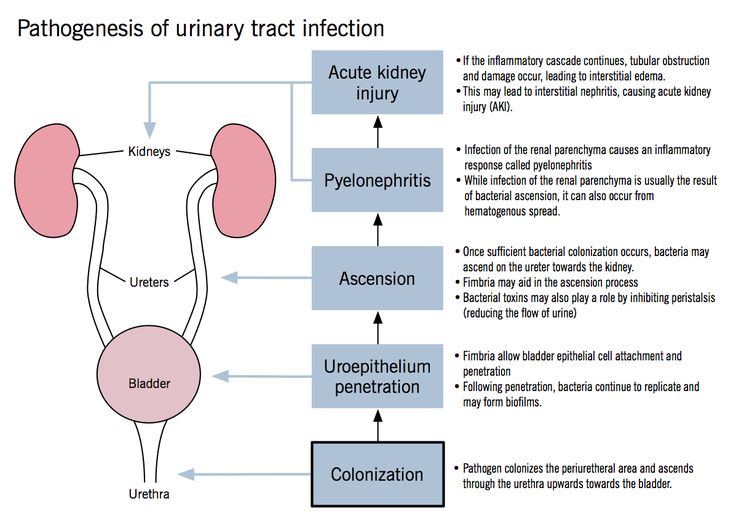
Bladder
If you have a urine infection (UTI) once you start trying, stop trying that month and use a condom until your next period, especially if you need to take trimethoprim. If you take prophylactic antibiotics to prevent UTIs, talk to your Urologist about whether it will be safe or advisable to stop. Trimethoprim is associated with birth conditions, including spina bifida. If you take medication for an overactive bladder, talk to your Urologist. Just before and during the first few months of pregnancy, you’ll usually be advised to stop your medicines.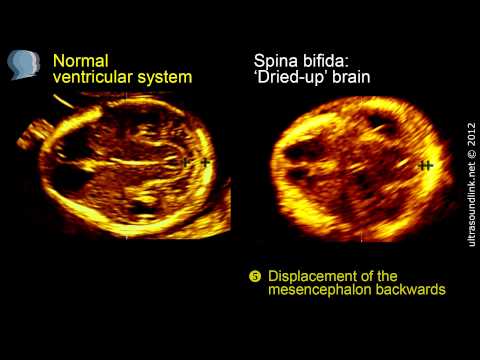 If you
If you
have an overactive bladder, you will probably find increased leakage, frequency and urgency of passing urine, especially as your pregnancy progresses. You may need to wear continence pads if you are leaking large amounts. For some of you, it could lead to reflux back to the kidneys, so you might need more regular scans to check. Some women find it gets much harder to catheterise in the last few months of pregnancy.
Ultrasound scans
Most scans give the best view of the baby when your bladder is full, as the full bladder ‘lifts’ the uterus above the pelvic bones. If you choose to have the ultrasound scans you’re offered, explain if you can’t fill your bladder very much. There’s no point drinking more water if it won’t improve the scan.
Bowels
Most women, with or without spina bifida, find they get more constipated during pregnancy. Increasing water intake, eating plenty of fruits, vegetables, and pulses (lentils, peas and beans) can help but you may need to take a laxative, even if you don’t usually need to, so check with your GP what would be best. Keep as active as you can to help things moving along.
Keep as active as you can to help things moving along.
Shunt
Many women with shunts have completely routine pregnancies, with no shunt complications at all. If you need a Caesarean delivery, make sure your Obstetric team know about your shunt. They might want to talk with a Neurosurgeon before your delivery
Back
If you have curvature of your lower spine, it can mean less space for your baby to grow, and you might need extra monitoring in the later months of your pregnancy. If you have a curvature of the top part of your back, it can make it harder for you to breathe, especially as the baby grows up under your ribs. Some women need to rest, and this may even include bed rest, in the last few months. Occasionally, it will be best to deliver your baby a little early.
Pelvis
Some women with spina bifida have changes to the shape of their pelvis which can mean a Caesarean would be safer than delivering vaginally.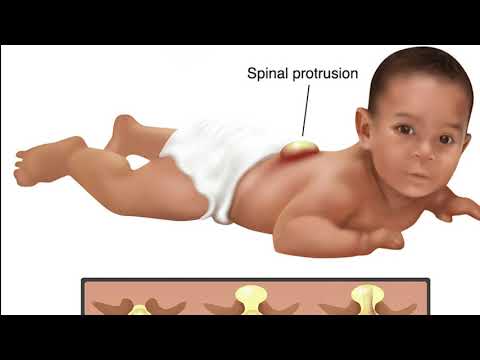 Your midwife should be able to advise you on this. You might want a scan at around 36 weeks, to check how big your baby is, and whether this affects your delivery plans. Very small as well as very large babies can be harder to deliver vaginally
Your midwife should be able to advise you on this. You might want a scan at around 36 weeks, to check how big your baby is, and whether this affects your delivery plans. Very small as well as very large babies can be harder to deliver vaginally
Balance
As your pregnancy progresses, you gain weight and your shape changes, balance may be a problem especially if you normally use calipars and or crutches. You may have to use a wheelchair for a period of time.
Pain
If you usually take pain medication, you will usually be advised to stop before and during the first few months of pregnancy at the least. This might be very difficult, and some medicines should be reduced slowly over several weeks to prevent withdrawal symptoms. Some women find warm baths and yoga techniques/mindfulness helpful, but often it’s a case of ‘getting through it’. You might have more pain, or new pain such as symphysis pubis dysfunction.
Click here for more information about pelvic pain in pregnancy
You might experience more back pain, as your posture changes and you’re carrying more weight, and for some of you, this will not go completely once you’ve had your baby
Preparing for Birth
Before Admission
You may wish to visit the maternity unit to have a look around where you will be giving birth.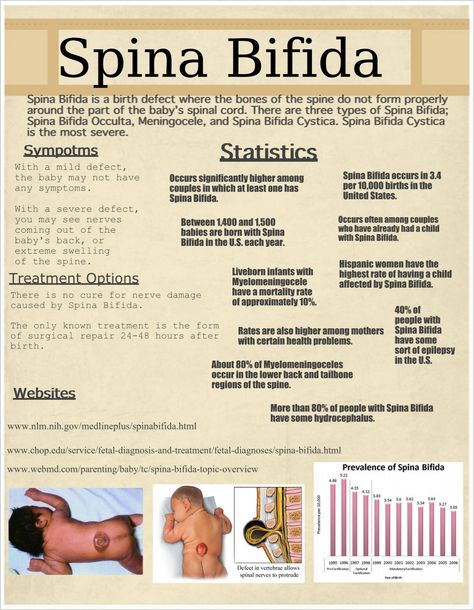 This will give you an opportunity to familiarise yourself with the facilities, discuss access issues and meet some of the members of staff. During this visit, make the staff aware of any additional equipment you may require such as a pressure relieving mattress, cushion, hoist or other transfer equipment.
This will give you an opportunity to familiarise yourself with the facilities, discuss access issues and meet some of the members of staff. During this visit, make the staff aware of any additional equipment you may require such as a pressure relieving mattress, cushion, hoist or other transfer equipment.
Planning for delivery
If your pelvis is narrow, or your abdomen muscles are not strong enough to push, a Caesarean might be a safer option than vaginal delivery. A Caesarean might also save damage to your pelvic floor, which might prevent bladder and bowel leakage later on. However, if possible, a vaginal delivery is the best start for your baby, and you will be able to return to your usual activities sooner than after a Caesarean. If it is decided that a vaginal delivery is best, you may need closer monitoring than other women. It can sometimes be hard to predict how the labour will go and how your spina bifida will affect it, and it’s important that assumptions aren’t made.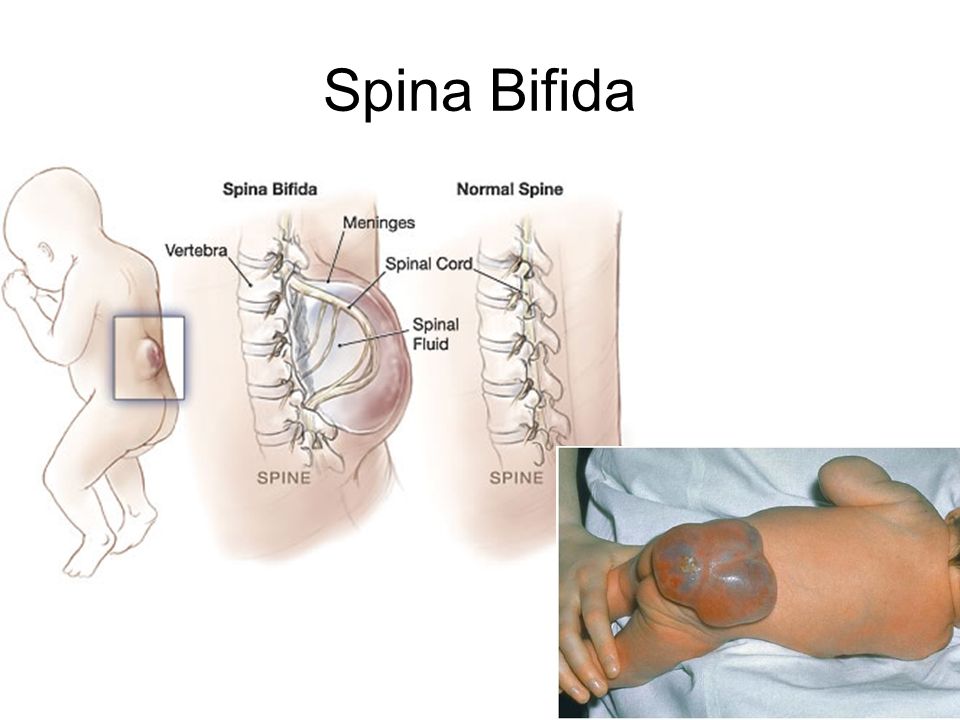
Occasionally, it may be possible for women with spina bifida to have spinal analgesia (injections into the back to block pain) but it varies from person to person, as the spina bifida lesion and shape of the bones often stop the analgesic from working. It’s a good idea to ask to talk with an anesthetist at your antenatal appointments well ahead of your delivery, to explore your options for pain relief. Professionals shouldn’t assume that because you have no skin sensation in certain areas, you won’t feel the pain of childbirth!
Going home with your baby
It’s a good idea to get as much in place before you go home, especially if you have a Caesarean, as this will mean driving and lifting would not be advised for several weeks. Cribs that attach to your bed can make it easier to tend to your baby without getting out of bed. Sometimes it is easier to leave your car seat in the car and lift your baby into a carry cot than trying to carry the car seat too.
If you use a wheelchair, you can purchase a lightweight pram that is easy to push, fold and attaches to your wheelchair.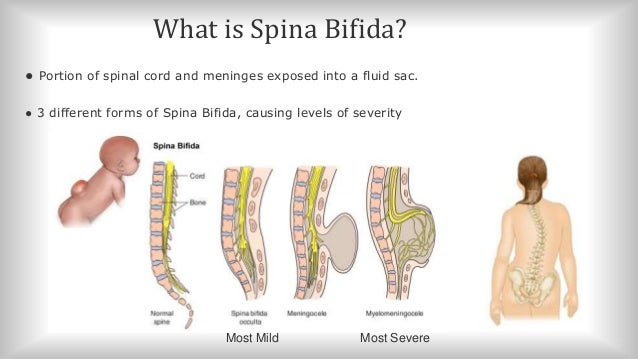 An occupational therapist will be able to advise you on suitable equipment to make it easier to care for your baby.
An occupational therapist will be able to advise you on suitable equipment to make it easier to care for your baby.
If anyone offers help, accept it in the spirit it’s meant, and give them something to do, especially the mundane chores like laundry. It will help you conserve your energy for your baby. It’s normal to feel exhausted in the early weeks, and it takes time for the hormones to settle. You might feel tearful or sensitive and feel offers of support imply you can’t cope. Mostly people just want to help. If the low mood or tearfulness last longer than a couple of weeks, let your Health Visitor or GP know.
Most doctors recommend that women terminate a pregnancy if the fetus is diagnosed with spina bifida
Veltishcheva Evgenia Berdichevskaya, the most effective for the treatment of this pathology are high-tech intrauterine operations / Kirill Braga / RIA Novosti
Doctors in the regions do not sufficiently inform pregnant women about the possibility of intrauterine surgery in a fetus with spina bifida (spina bifida) and in most cases advise only termination of pregnancy, Experts of the Spina Bifida Foundation believe, referring to the appeal of patients to the Foundation.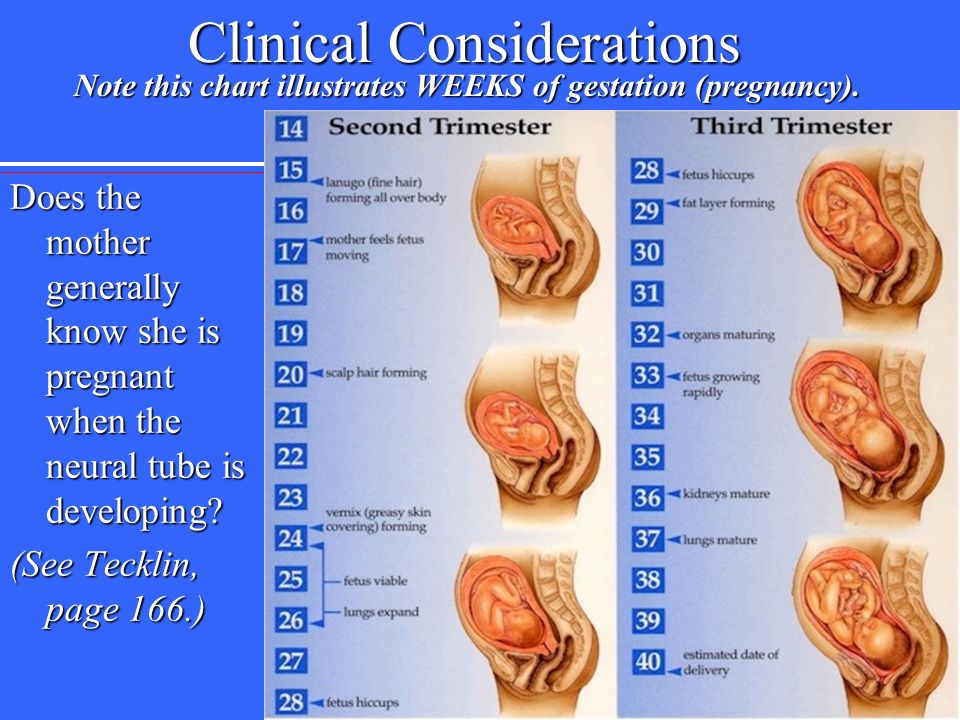 This is the only fund in Russia that maintains a register of those who have experienced such a disease.
This is the only fund in Russia that maintains a register of those who have experienced such a disease.
Spina bifida is a severe congenital defect of the spine that develops in the fetus in the womb. Every year in Russia, 1500-2000 children are born with spinal cord pathology, about 275 operations are performed immediately after the birth of a child. “The Foundation knows about 1,100 children across Russia, of which there are more than 200 orphans in orphanages in the Foundation’s registry,” Inna Inyushkina, founder of Spina Bifida, told Vedomosti. “About 20 new requests for help come in every month.” As explained by the neurophysiologist of the Department of Neurosurgery of the Institute of Pediatrics. Veltishcheva Evgenia Berdichevskaya, the most effective for the treatment of this pathology are high-tech intrauterine operations: they reduce the risk of a child's disability by a factor of three compared to operations after birth.
According to her, about 20 intrauterine surgeries are performed a year for spina bifida in Russia.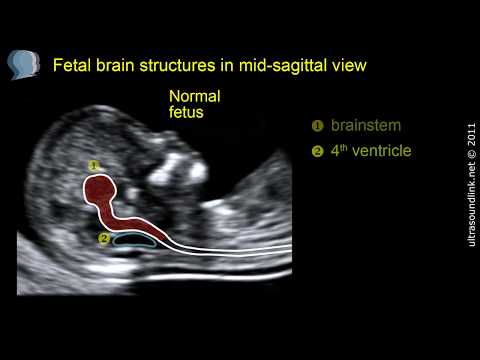 Such operations are actively performed in Russia by the Center for Obstetrics and Gynecology. Kulakov and the clinical hospital "Lapino", in other medical institutions "such operations are rare." In 2020, 10 pregnant women applied to the fund, of which only one of them underwent intrauterine surgery, in 2021 - 37 pregnant women, in the six months of 2022 - 70. Women who applied to the fund report that "doctors insisted on interrupting pregnancy”, “aggressively persuaded to have an abortion, did not explain anything about spina bifida”, “many doctors have not heard about fetal (intrauterine) operations”.
Such operations are actively performed in Russia by the Center for Obstetrics and Gynecology. Kulakov and the clinical hospital "Lapino", in other medical institutions "such operations are rare." In 2020, 10 pregnant women applied to the fund, of which only one of them underwent intrauterine surgery, in 2021 - 37 pregnant women, in the six months of 2022 - 70. Women who applied to the fund report that "doctors insisted on interrupting pregnancy”, “aggressively persuaded to have an abortion, did not explain anything about spina bifida”, “many doctors have not heard about fetal (intrauterine) operations”.
The Foundation also conducted a survey in which 62 parents of children with spina bifida from 43 Russian cities took part. 50% of the respondents found out about the diagnosis before 24 weeks of gestation - during the period when intrauterine surgery would be most successful, if detected at a later stage of pregnancy, surgery is possible after the birth of the child. But, as follows from the results of the survey, none of these patients was immediately informed by the attending physician about the possibility of intrauterine surgery.
At the same time, 9.5% of respondents received information from a doctor later, 28.6% found information on their own, and 43% did not receive information at all. All those who received information about the possibilities of intrauterine surgery decided to carry it out, "considering it as an opportunity to improve health, a chance that the child will be born healthy." 85.5% consider the level of information about the diagnosis and treatment options for spina bifida to be “insufficient” or “extremely low”.
Head of the fund's legal support project Elena Moryakina noted that almost 50% of the fund's beneficiaries found out about the diagnosis at the third screening. “But in accordance with the order on the procedure for providing medical care in the field of obstetrics and gynecology, the third screening is not mandatory. Screening at 30–34 weeks should be made mandatory, as early diagnosis of the disease opens up opportunities for surgery and can provide time to prepare for childbirth.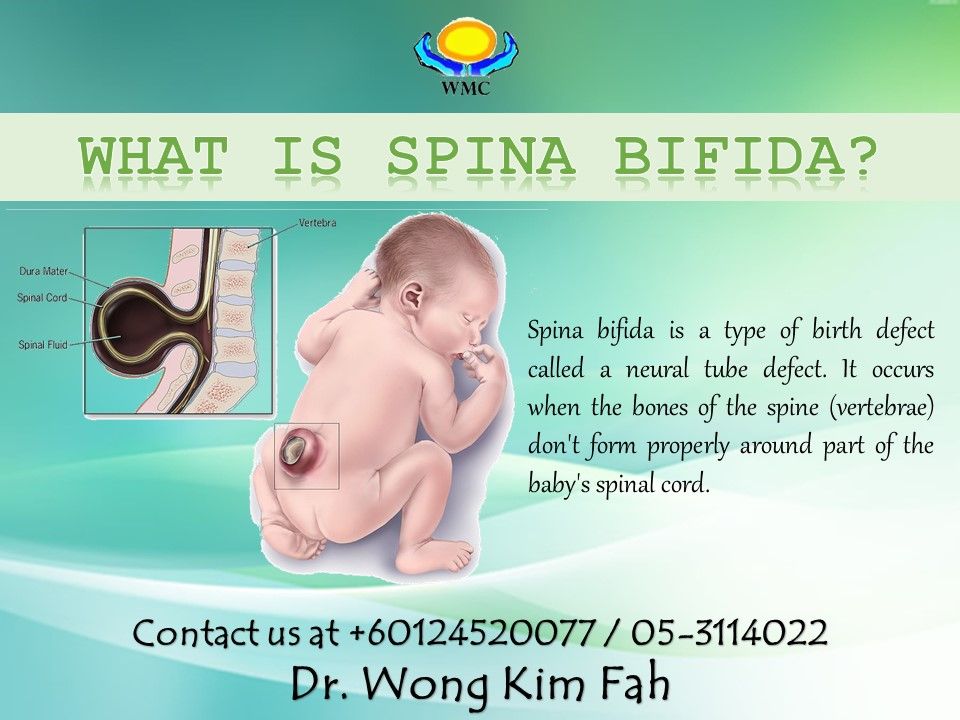 In particular, to create special conditions for the woman in labor and the unborn baby, ”says Moryakina.
In particular, to create special conditions for the woman in labor and the unborn baby, ”says Moryakina.
Vedomosti sent a request to the Ministry of Health.
Berdichevskaya believes that insufficient information and a tendency to refer pregnant women whose fetuses are diagnosed with spina bifida for abortion is a "systemic error."
She stated that, so far, information about treatment options “is distributed mainly among the patient community”. She noted that the lack of information among doctors in the regions is especially significant: “It is necessary to break this stereotype that a genetic defect is a severe pathology.”
Media news2
Do you want to hide ads? Subscribe and read without distractionSpina bifida and how to treat it?
15.07.2021
Spina bifida (spina bifida) is a developmental defect of the spine that occurs as early as the third week of fetal life and consists in incomplete closure of the spinal canal.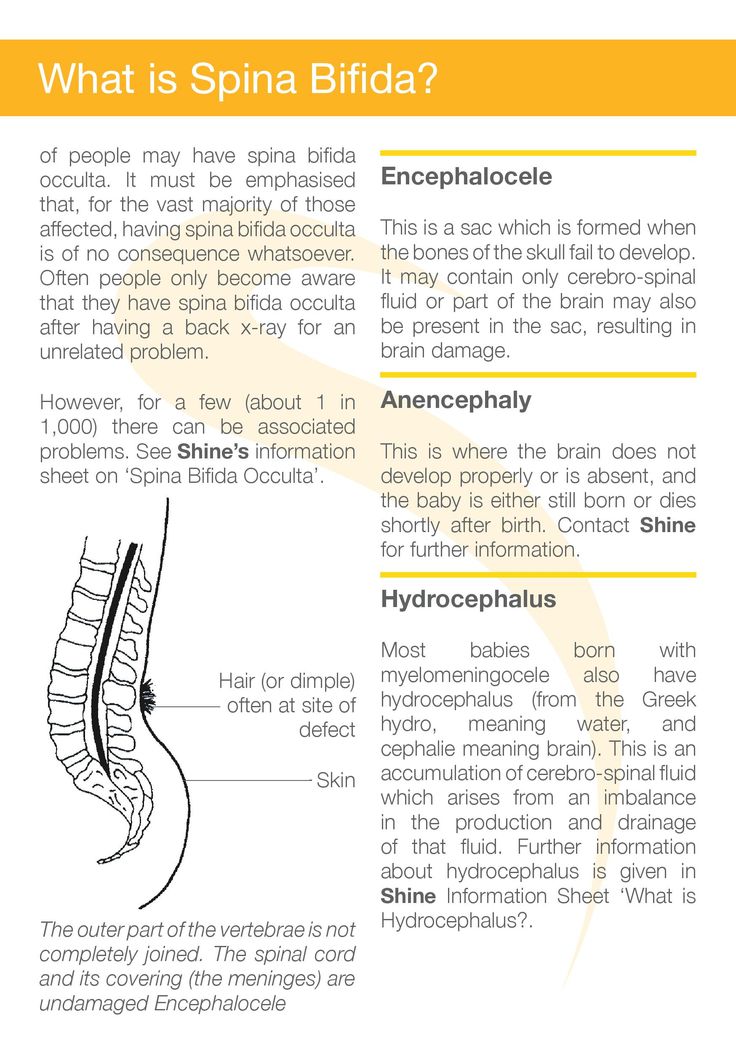 From this free space, the spinal cord with the meninges or the meninges themselves (meningeal hernia ). What are the causes of spina bifida ? How is the treatment and rehabilitation of patients with spawning eggs divided in half?
From this free space, the spinal cord with the meninges or the meninges themselves (meningeal hernia ). What are the causes of spina bifida ? How is the treatment and rehabilitation of patients with spawning eggs divided in half?
Spina bifida - what is it?
Spina bifida, also known as meningeal hernia or bisected scar, is a birth defect that occurs in approximately 2.5% of live newborns. There is a violation of the formation of the structures of the spinal cord and spine . It occurs in utero - approximately in the third week of pregnancy (although most often detected with high accuracy in the second trimester, when seen on ultrasound ) and can appear along the entire length of the spine . The most common localization of hernia is the lumbar or lumbosacral segment (spina bifida L5 - S1).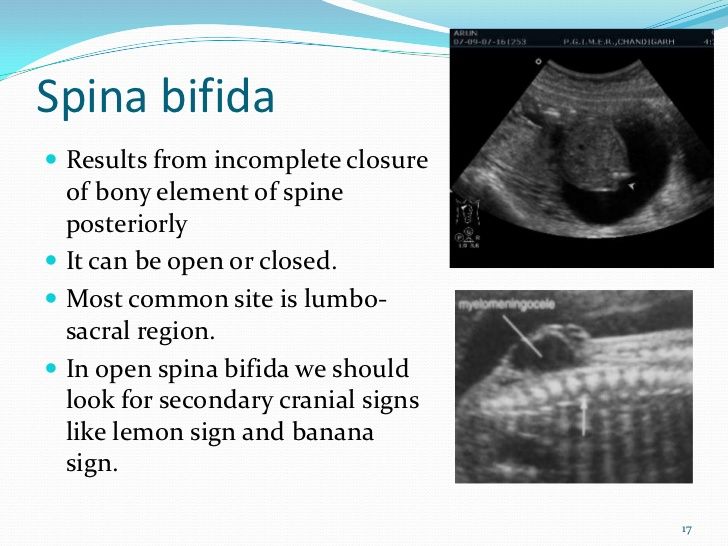 In about 75% of cases, this defect is accompanied by congenital hydrocephalus.
In about 75% of cases, this defect is accompanied by congenital hydrocephalus.
As a result, nerve conduction to various parts of the body is disturbed. We can also deal with the latent cleft, which the patient learns about in adulthood, because it is so limited and asymptomatic that it does not affect the functioning of the body.
The cause of this malformation of the spine has not been fully elucidated. On the one hand, experts talk about genetic determinants and inheritance, on the other hand, about external phenomena, such as infections in the womb, deficiency of folic acid and B vitamins, exposure of pregnant women to X-rays, anticonvulsants.
Spina bifida - types of spina bifida
There are three main types of spina bifida: a bunch of hair, often the patient is not aware of the defect because there are no symptoms;
 The first type - meningocele - cyst fluid contains tissue and spinal nerves , as a rule, not severely damaged, there is no significant damage nerves , and operation includes repair of the dura and skin plastic surgery is rare. The second type - meningomyelocele - often formed cyst, in addition to tissues and cerebrospinal fluid, also contains nerves and part of the spinal cord that is damaged or abnormally developed; the degree of disability depends on the location and degree of damage, there is paralysis and loss of sensation below the level of the cyst, as well as problems with the bladder ; surgery is required to close the spinal canal and insert a valve into the ventricles of the brain if the circulation of cerebrospinal fluid is impaired and intracranial pressure is increased ;
The first type - meningocele - cyst fluid contains tissue and spinal nerves , as a rule, not severely damaged, there is no significant damage nerves , and operation includes repair of the dura and skin plastic surgery is rare. The second type - meningomyelocele - often formed cyst, in addition to tissues and cerebrospinal fluid, also contains nerves and part of the spinal cord that is damaged or abnormally developed; the degree of disability depends on the location and degree of damage, there is paralysis and loss of sensation below the level of the cyst, as well as problems with the bladder ; surgery is required to close the spinal canal and insert a valve into the ventricles of the brain if the circulation of cerebrospinal fluid is impaired and intracranial pressure is increased ; 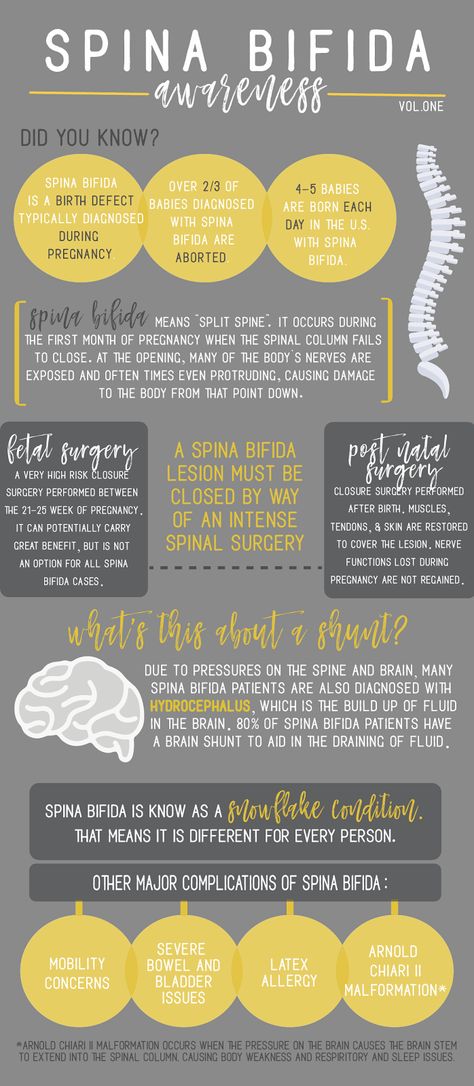
Spina bifida - symptoms
Spina bifida is often a tumor of various sizes on the back covered with thin skin. Sometimes only a depression or dimple, hair spot, bump, or red mole is found.
Depending on the type of cleft and the degree of its occurrence, one can speak of various clinical symptoms. The more the cleft appears in the lower back and the less widespread it is, the better the child will live a normal life. However, one should always remember that a child with spina bifida has several health problems related to different organs.
The most common symptoms of spina bifida include paresis of the limbs, forcing them to move around in a wheelchair. Another problem is uneven circulation of cerebral fluid, which requires the position of the valve, as well as dysfunction of the urinary system. With a cleft located in the lumbosacral region, paresis or paralysis of the muscles of the lower extremities is flaccid, the position of the feet may be clubfoot, sphincter disorders lead to incontinence urine , and sensory disturbances are of the root type. In the case of a cleft, sensory disturbances located in the cervical or thoracic region are of the spinal type, and the lower limbs are of the pyramidal type. It happens that the symptoms of some meningeal hernias may not appear until ectopic development.
In the case of a cleft, sensory disturbances located in the cervical or thoracic region are of the spinal type, and the lower limbs are of the pyramidal type. It happens that the symptoms of some meningeal hernias may not appear until ectopic development.
Spina bifida with age leads to such consequences of the disease as spinal curvature , hip dislocation , muscle contractures and deformities bones and joints .
Spina bifida - treatment
Spina bifida is often diagnosed during pregnancy based on fetal ultrasound. The diagnosis is confirmed by the analysis of amniotic fluid.
After birth or while still in the womb (prenatal surgery ), your baby will have surgery to close hernia and reduce the risk of infection. Most often it is carried out in the first two days of life. Since this defect causes irreversible damage nervous system and various related problems, the child needs specialized care neurologist , orthopedist , urologist , physiotherapist and psychologist .