Pathophysiology of fetal distress
[Pathophysiology of fetal distress] - PubMed
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
Review
. 1994 Mar;26(2):119-24.
[Article in Japanese]
A Sato 1
Affiliations
Affiliation
- 1 Department of Obstetrics and Gynecology, Fukushima Medical College.
- PMID: 8136183
Review
[Article in Japanese]
A Sato. No To Hattatsu. 1994 Mar.
. 1994 Mar;26(2):119-24.
Author
A Sato 1
Affiliation
- 1 Department of Obstetrics and Gynecology, Fukushima Medical College.
- PMID: 8136183
Abstract
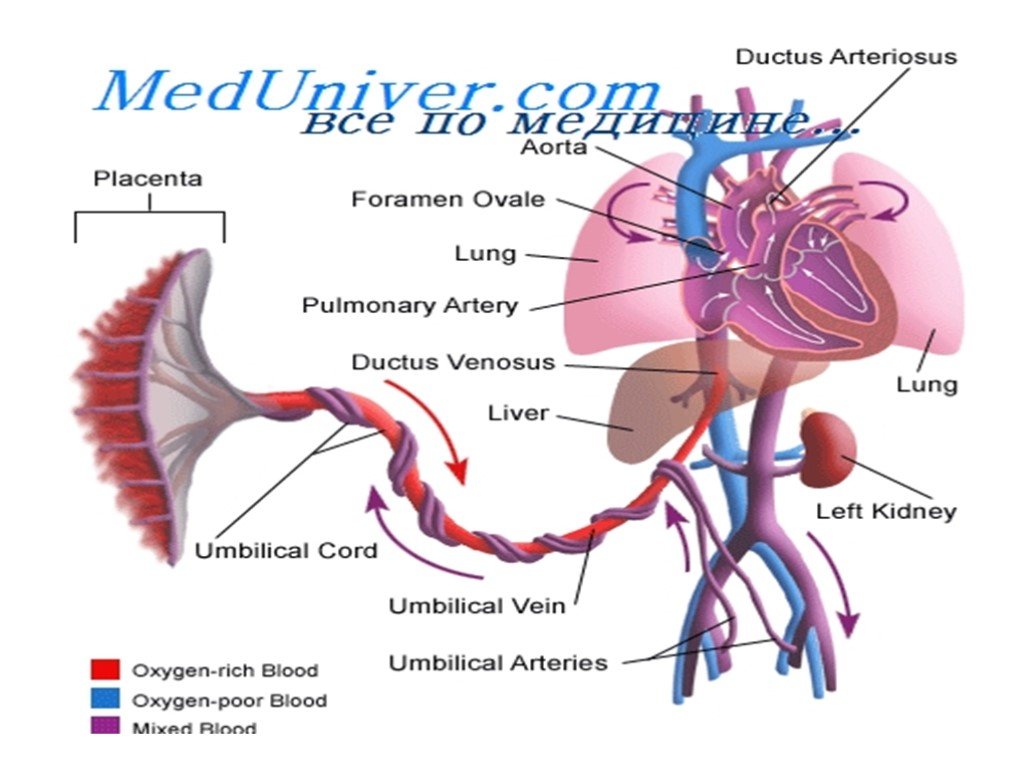
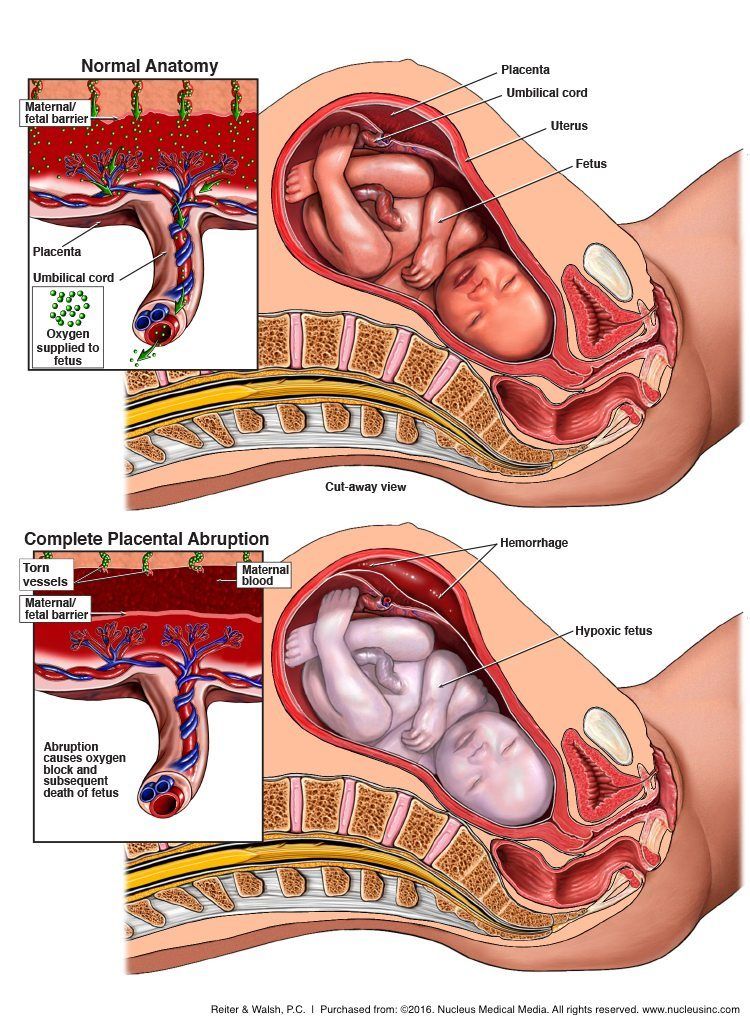
Pathophysiology of fetal distress has not been elucidated completely so far.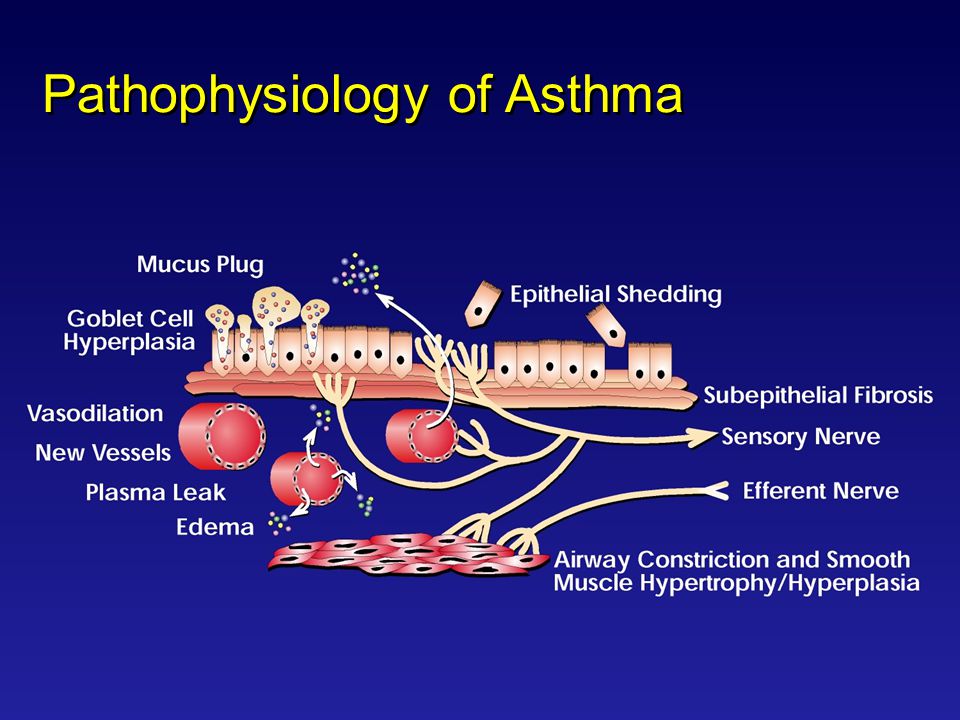 But there has been a rapid progress in the studies both in vitro and in vivo which investigated the causes of neuronal death by hypoxia. At the initiation of hypoxemia, elevation of fetal blood pressure will occur due to constriction of fetal peripheral vessels, and this results in fetal heart rate slowing and respiratory compromise. During moderate hypoxemia, circulating blood is redistributed to the brain, heart and adrenals at the expense of peripheral organs (lung, skin, etc). During prolonged hypoxemia, blood flow to the brain stem is maintained and even greater than that in other brain regions. Neuronal activity of brain stem, an autonomic center, is important for survival of a fetus. As hypoxia progresses, glucose in metabolized anaerobically, lactate concentration elevates, and concentrations of high-energy phosphates decrease in the cerebrum. When cerebral metabolism has collapsed finally, neuronal membranes depolarize, voltage-gated Ca+2 channels open and Ca+2 flux into the cytoplasm increases.
But there has been a rapid progress in the studies both in vitro and in vivo which investigated the causes of neuronal death by hypoxia. At the initiation of hypoxemia, elevation of fetal blood pressure will occur due to constriction of fetal peripheral vessels, and this results in fetal heart rate slowing and respiratory compromise. During moderate hypoxemia, circulating blood is redistributed to the brain, heart and adrenals at the expense of peripheral organs (lung, skin, etc). During prolonged hypoxemia, blood flow to the brain stem is maintained and even greater than that in other brain regions. Neuronal activity of brain stem, an autonomic center, is important for survival of a fetus. As hypoxia progresses, glucose in metabolized anaerobically, lactate concentration elevates, and concentrations of high-energy phosphates decrease in the cerebrum. When cerebral metabolism has collapsed finally, neuronal membranes depolarize, voltage-gated Ca+2 channels open and Ca+2 flux into the cytoplasm increases. These changes result in neuronal death. It is considered that glutamates, oxygen radicals and other substances are involved in the increase of Ca+2 influx. These studies suggest that hypoxic stimulation should be avoided in the chronically deteriorating fetus for prevention of unrecognized fetal brain damage.
These changes result in neuronal death. It is considered that glutamates, oxygen radicals and other substances are involved in the increase of Ca+2 influx. These studies suggest that hypoxic stimulation should be avoided in the chronically deteriorating fetus for prevention of unrecognized fetal brain damage.
Similar articles
-
Does acute hypoxia cause fetal arterial blood flow redistribution?
Krampl E, Chalubinski K, Schatten C, Husslein P. Krampl E, et al. Ultrasound Obstet Gynecol. 2001 Aug;18(2):175-7. doi: 10.1046/j.1469-0705.2001.00501.x. Ultrasound Obstet Gynecol. 2001. PMID: 11530003
-
Regional cerebral glucose utilization in immature fetal guinea pigs during maternal isocapnic hypoxemia.
Berger R, Gjedde A, Hargarter L, Hargarter S, Krieglstein J, Jensen A.
 Berger R, et al. Pediatr Res. 1997 Sep;42(3):311-6. doi: 10.1203/00006450-199709000-00011. Pediatr Res. 1997. PMID: 9284271
Berger R, et al. Pediatr Res. 1997 Sep;42(3):311-6. doi: 10.1203/00006450-199709000-00011. Pediatr Res. 1997. PMID: 9284271 -
Adenosine mediates decreased cerebral metabolic rate and increased cerebral blood flow during acute moderate hypoxia in the near-term fetal sheep.
Blood AB, Hunter CJ, Power GG. Blood AB, et al. J Physiol. 2003 Dec 15;553(Pt 3):935-45. doi: 10.1113/jphysiol.2003.047928. Epub 2003 Sep 18. J Physiol. 2003. PMID: 14500776 Free PMC article.
-
Fetal circulatory responses to oxygen lack.
Jensen A, Berger R. Jensen A, et al. J Dev Physiol. 1991 Oct;16(4):181-207. J Dev Physiol. 1991. PMID: 1812154 Review.
-
Modalities of fetal evaluation to detect fetal compromise prior to the development of significant neurological damage.
Maeda K. Maeda K. J Obstet Gynaecol Res. 2014 Oct;40(10):2089-94. doi: 10.1111/jog.12481. Epub 2014 Aug 11. J Obstet Gynaecol Res. 2014. PMID: 25130074 Review.
See all similar articles
Cited by
-
Effect of anaesthetic technique on neonatal morbidity in emergency caesarean section for foetal distress.
Edipoglu IS, Celik F, Marangoz EC, Orcan GH. Edipoglu IS, et al. PLoS One. 2018 Nov 16;13(11):e0207388. doi: 10.1371/journal.pone.0207388. eCollection 2018. PLoS One. 2018. PMID: 30444916 Free PMC article. Clinical Trial.
-
Spinal anaesthesia for caesarean section in pregnant women with fetal distress: time for reappraisal.
Afolayan JM, Olajumoke TO, Esangbedo SE, Edomwonyi NP.
 Afolayan JM, et al. Int J Biomed Sci. 2014 Jun;10(2):103-10. Int J Biomed Sci. 2014. PMID: 25018678 Free PMC article.
Afolayan JM, et al. Int J Biomed Sci. 2014 Jun;10(2):103-10. Int J Biomed Sci. 2014. PMID: 25018678 Free PMC article. -
Effect of decreased fetal perfusion on placental clearance of volatile anesthetics in a dual perfused human placental cotyledon model.
Ueki R, Tatara T, Kariya N, Shimode N, Hirose M, Tashiro C. Ueki R, et al. J Anesth. 2014 Aug;28(4):635-8. doi: 10.1007/s00540-013-1777-3. Epub 2014 Jan 3. J Anesth. 2014. PMID: 24384731
Publication types
MeSH terms
Cite
Format: AMA APA MLA NLM
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Send To
What is fetal distress? - PubMed
Review
. 1990 Jun;162(6):1421-5; discussion 1425-7.
1990 Jun;162(6):1421-5; discussion 1425-7.
doi: 10.1016/0002-9378(90)90901-i.
J T Parer 1 , E G Livingston
Affiliations
Affiliation
- 1 Department of Obstetrics, Gynecology and Reproductive Sciences, University of California, San Francisco 94143.
- PMID: 2193513
- DOI: 10.1016/0002-9378(90)90901-i
Review
J T Parer et al. Am J Obstet Gynecol. 1990 Jun.
. 1990 Jun;162(6):1421-5; discussion 1425-7.
doi: 10.1016/0002-9378(90)90901-i.
Authors
J T Parer 1 , E G Livingston
Affiliation
- 1 Department of Obstetrics, Gynecology and Reproductive Sciences, University of California, San Francisco 94143.
- PMID: 2193513
- DOI: 10.1016/0002-9378(90)90901-i
Abstract
Fetal distress is a widely used but poorly defined term. This confusion of definition compounds the difficulty of making an accurate diagnosis and initiating appropriate treatment. The fetus reacts at the onset of asphyxia with a remarkable series of responses, primarily a complexly regulated redistribution of blood flow that serves to limit the deleterious effects of oxygen limitation in vital organs. This enables the fetus to survive asphyxia intact unless the insult is profound or prolonged. The most common asphyxial stresses imposed on the fetus during labor are insufficiency of uterine blood flow, or insufficiency of umbilical blood flow, and occasionally decrease in uterine arterial oxygenation. Each of these stresses produces characteristic fetal heart rate patterns: late decelerations, variable decelerations, or prolonged bradycardia. There is strong evidence that the presence of normal fetal heart rate variability represents normal central nervous system integrity, including adequate oxygenation. A decrease or loss of variability in the presence of these patterns is a sign that the physiologic compensations are overwhelmed as a result of the severity of asphyxia.
The fetus reacts at the onset of asphyxia with a remarkable series of responses, primarily a complexly regulated redistribution of blood flow that serves to limit the deleterious effects of oxygen limitation in vital organs. This enables the fetus to survive asphyxia intact unless the insult is profound or prolonged. The most common asphyxial stresses imposed on the fetus during labor are insufficiency of uterine blood flow, or insufficiency of umbilical blood flow, and occasionally decrease in uterine arterial oxygenation. Each of these stresses produces characteristic fetal heart rate patterns: late decelerations, variable decelerations, or prolonged bradycardia. There is strong evidence that the presence of normal fetal heart rate variability represents normal central nervous system integrity, including adequate oxygenation. A decrease or loss of variability in the presence of these patterns is a sign that the physiologic compensations are overwhelmed as a result of the severity of asphyxia.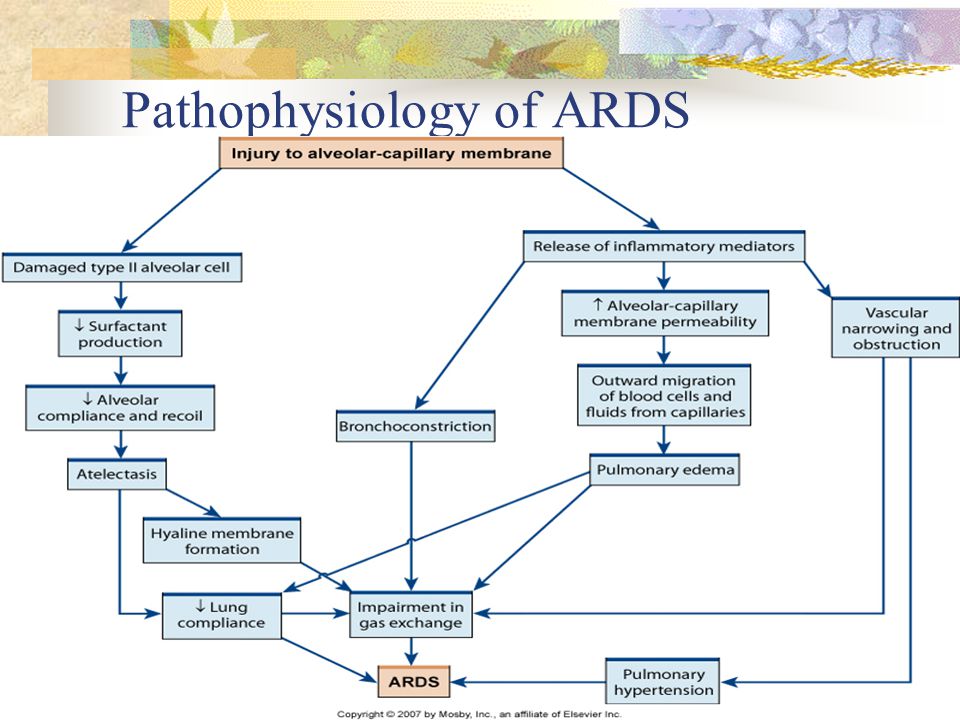 Knowledge of the fetal responses to asphyxia, together with the known evolution of fetal heart rate patterns during asphyxia, should allow a more accurate definition of the onset of unacceptable asphyxia, and more rational management and timing of intervention.
Knowledge of the fetal responses to asphyxia, together with the known evolution of fetal heart rate patterns during asphyxia, should allow a more accurate definition of the onset of unacceptable asphyxia, and more rational management and timing of intervention.
Similar articles
-
The relationship between heart rate and asphyxia in the animal fetus.
Bocking AD. Bocking AD. Clin Invest Med. 1993 Apr;16(2):166-75. Clin Invest Med. 1993. PMID: 8513617 Review.
-
Effects of fetal asphyxia on brain cell structure and function: limits of tolerance.
Parer JT. Parer JT. Comp Biochem Physiol A Mol Integr Physiol. 1998 Mar;119(3):711-6. doi: 10.1016/s1095-6433(98)01009-5. Comp Biochem Physiol A Mol Integr Physiol.
 1998. PMID: 9683410 Review.
1998. PMID: 9683410 Review. -
Does acute hypoxia cause fetal arterial blood flow redistribution?
Krampl E, Chalubinski K, Schatten C, Husslein P. Krampl E, et al. Ultrasound Obstet Gynecol. 2001 Aug;18(2):175-7. doi: 10.1046/j.1469-0705.2001.00501.x. Ultrasound Obstet Gynecol. 2001. PMID: 11530003
-
The intrapartum deceleration in center stage: a physiologic approach to the interpretation of fetal heart rate changes in labor.
Westgate JA, Wibbens B, Bennet L, Wassink G, Parer JT, Gunn AJ. Westgate JA, et al. Am J Obstet Gynecol. 2007 Sep;197(3):236.e1-11. doi: 10.1016/j.ajog.2007.03.063. Am J Obstet Gynecol. 2007. PMID: 17826402
-
The physiology of fetal heart rate patterns and perinatal asphyxia.
King T, Parer J. King T, et al. J Perinat Neonatal Nurs. 2000 Dec;14(3):19-39; quiz 102-3. doi: 10.1097/00005237-200012000-00003. J Perinat Neonatal Nurs. 2000. PMID: 11930377
See all similar articles
Cited by
-
Pregnancy outcomes in patients with polycystic ovary syndrome who conceived after single thawed blastocyst transfer: a propensity score-matched study.
Jie HY, Zhou X, Zhao MP, Hu M, Mai QY, Zhou CQ. Jie HY, et al. BMC Pregnancy Childbirth. 2022 Sep 20;22(1):718. doi: 10.1186/s12884-022-05011-4. BMC Pregnancy Childbirth. 2022. PMID: 36127673 Free PMC article.
-
Mediolateral episiotomy and risk of obstetric anal sphincter injuries and adverse neonatal outcomes during operative vaginal delivery in nulliparous women: a propensity-score analysis.
Desplanches T, Marchand-Martin L, Szczepanski ED, Ruillier M, Cottenet J, Semama D, Simon E, Quantin C, Sagot P. Desplanches T, et al. BMC Pregnancy Childbirth. 2022 Jan 19;22(1):48. doi: 10.1186/s12884-022-04396-6. BMC Pregnancy Childbirth. 2022. PMID: 35045812 Free PMC article.
-
Thromboelastometry in Neonates with Respiratory Distress Syndrome: A Pilot Study.
Katsaras GN, Sokou R, Tsantes AG, Konstantinidi A, Gialamprinou D, Piovani D, Bonovas S, Kriebardis AG, Mitsiakos G, Kokoris S, Tsantes AE. Katsaras GN, et al. Diagnostics (Basel). 2021 Oct 27;11(11):1995. doi: 10.3390/diagnostics11111995. Diagnostics (Basel). 2021. PMID: 34829342 Free PMC article.
-
Reference Values of Thrombolastometry Parameters in Healthy Term Neonates.
Theodoraki M, Sokou R, Valsami S, Iliodromiti Z, Pouliakis A, Parastatidou S, Karavana G, Ioakeimidis G, Georgiadou P, Iacovidou N, Boutsikou T. Theodoraki M, et al. Children (Basel). 2020 Nov 26;7(12):259. doi: 10.3390/children7120259. Children (Basel). 2020. PMID: 33256197 Free PMC article.
-
Skeletal and Cardiac Rhabdomyolysis in a Live-Stranded Neonatal Bryde's Whale With Fetal Distress.
Câmara N, Sierra E, Fernández A, Suárez-Santana CM, Puig-Lozano R, Arbelo M, Herráez P. Câmara N, et al. Front Vet Sci. 2019 Dec 20;6:476. doi: 10.3389/fvets.2019.00476. eCollection 2019. Front Vet Sci. 2019. PMID: 31921928 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Neonatal respiratory distress syndrome (RDSN)
Symptom complex of severe respiratory insufficiency that occurs in the first hours of a child's life due to a decrease surfactant content in the alveoli and the development of pneumopathy.
Adverse outcomes:
-
bronchopulmonary dysplasia.
-
Death of a newborn.
Surfactant begins to be produced at fetal lungs from 20–24 weeks of gestation, by 35–36 weeks, a system that provides its synthesis, fully matures. In the moment childbirth, the synthesis of surfactant increases sharply, which facilitates the initial straightening and stabilization of the alveoli of the newborn. Premature birth (before 36 weeks) pregnancy) immature lungs, number surfactant is not enough for a complete expansion of the alveoli. Formed primary atelectasis. Due to inadequate ventilation develop hypoxia and acidosis, decreased blood pressure. Arise reflex spasm of the pulmonary arterioles, swelling of the walls of the alveoli permeability of the alveolocapillary membranes, which leads to the release of plasma from the pulmonary capillaries followed by deposition on the surface of the respiratory bronchioles, alveolar ducts and alveoli of hyaline-like substances and formation of hyaline membranes. Hyaline membranes further contribute to greater reduction in surfactant synthesis and the development of pulmonary atelectasis. Due to developing pulmonary hypertension and acidosis is broken usual for early neonatal restructuring blood circulation, in connection with which the fetal communications (oval hole in the interatrial septum ductus arteriosus that connects pulmonary trunk with aorta). Wherein hypoxia worsens, DIC syndrome, edema appears, hemorrhages, bleeding; what leads to more disruption. surfactant synthesis, a vicious a circle.
Hyaline membranes further contribute to greater reduction in surfactant synthesis and the development of pulmonary atelectasis. Due to developing pulmonary hypertension and acidosis is broken usual for early neonatal restructuring blood circulation, in connection with which the fetal communications (oval hole in the interatrial septum ductus arteriosus that connects pulmonary trunk with aorta). Wherein hypoxia worsens, DIC syndrome, edema appears, hemorrhages, bleeding; what leads to more disruption. surfactant synthesis, a vicious a circle.
Causes of reduced synthesis surfactant:
- chronic intrauterine hypoxia,
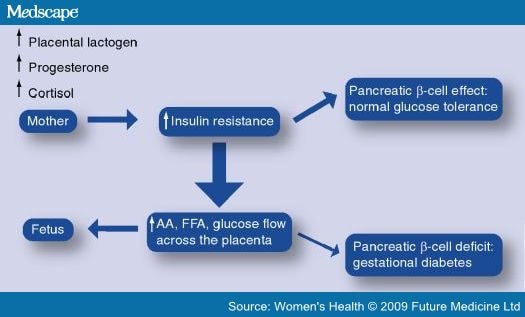
– pregnancy diabetes mellitus,
- acute fetal asphyxia,
- blood loss during childbirth,
infections caused primarily by Gram-negative microorganisms mycoplasma, viruses.
In pathogenesis RDS has a large value anatomical and functional lung immaturity, which is that by the time of birth in the lungs in inadequately produced surfactant.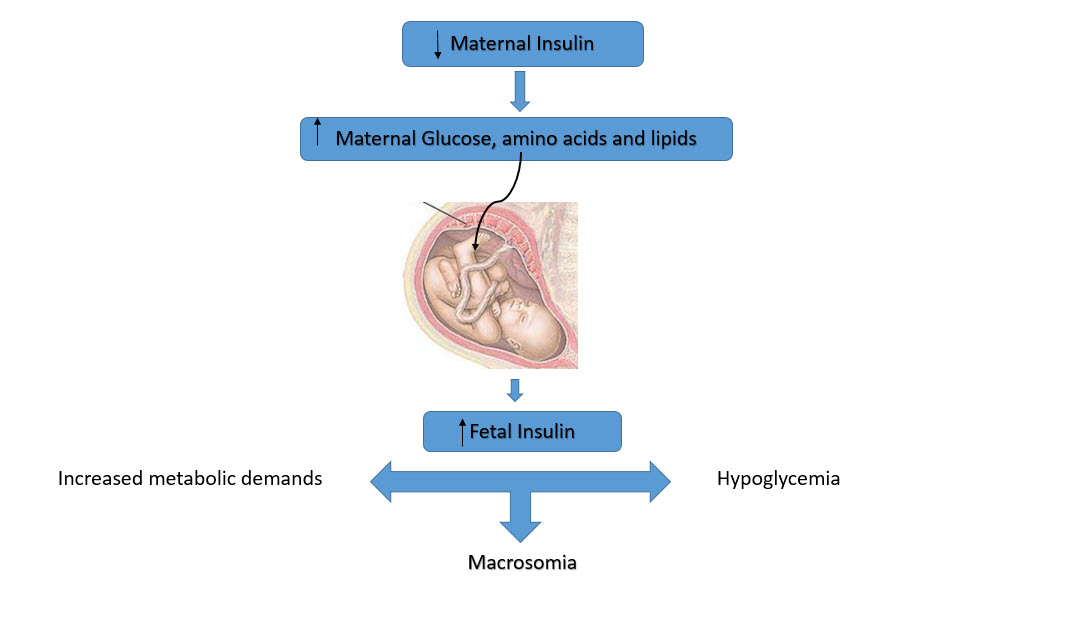 In this regard, at the first inhalation, not all parts of the lungs open, areas of atelectasis. In them increased vascular permeability, which contributes to the development of hemorrhages. Hyaline-like substance on the inside surfaces of the alveoli and alveolar moves contributes to the violation of diffusion gases.
In this regard, at the first inhalation, not all parts of the lungs open, areas of atelectasis. In them increased vascular permeability, which contributes to the development of hemorrhages. Hyaline-like substance on the inside surfaces of the alveoli and alveolar moves contributes to the violation of diffusion gases.
RDSN stages:
I stage - formation of areas of hypoventilation mild and disseminated atelectasis due to primary deficiency "surfactant"
II stage - damage to the pulmonary endothelium capillaries due to progression respiratory hypoxia and acidosis leads to to increase permeability alveolocapillary membranes and perspiration liquid portion of blood into the lumen of the alveoli ("Edematous-hemorrhagic syndrome lungs")
III stage - the formation of the so-called hyaline membranes from blood proteins and necrotic alveolar epithelium. Atelectasis and hyaline membranes lead to the formation alveolar-capillary block (significant reduction or cessation diffusion flow O 2 and CO 2 through the alveolocapillary membranes).
Atelectasis and hyaline membranes lead to the formation alveolar-capillary block (significant reduction or cessation diffusion flow O 2 and CO 2 through the alveolocapillary membranes).
The prognosis is severe, depending on the degree and extent of pathological changes in the lungs.
Respiratory Distress Syndrome - How to Diagnose Pediatric Tips
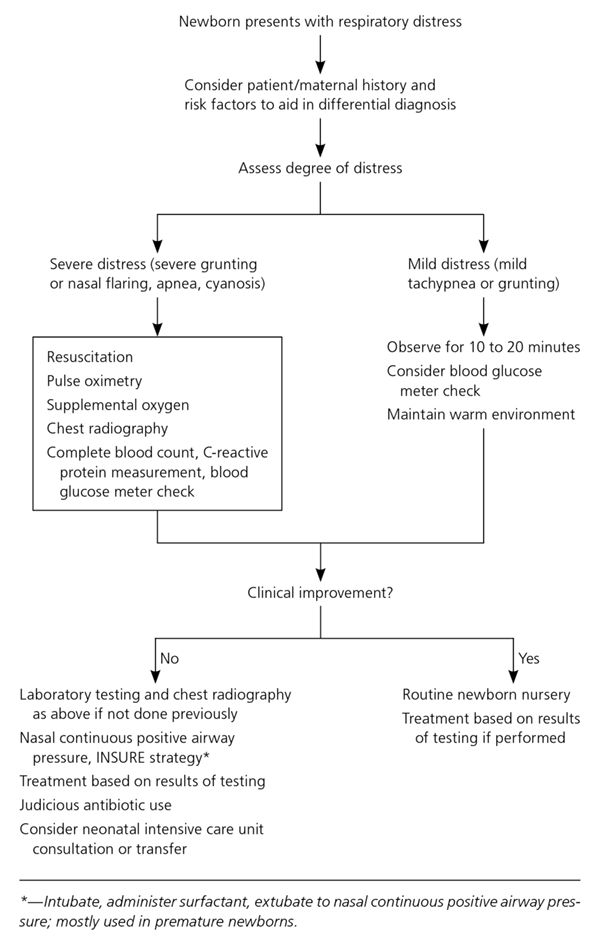
How to Diagnose Neonatal Respiratory Distress Syndrome: Respiratory Distress Syndrome of the Newborn (RDS) occurs when a baby's lungs are not fully developed and cannot provide enough oxygen, causing difficulty breathing. Primary diagnosis of respiratory distress syndrome of the newborn will require consultation with a therapist. As an additional examination based on the results of the examination, the doctor may prescribe:
- x-ray
- CT scan of the chest.
Quick navigation
This disease usually develops in premature babies. It is also known as childhood respiratory distress syndrome, hyaline membrane disease, or surfactant deficiency lung disease. Despite the similar name, respiratory distress syndrome is not related to acute respiratory distress syndrome.
It is also known as childhood respiratory distress syndrome, hyaline membrane disease, or surfactant deficiency lung disease. Despite the similar name, respiratory distress syndrome is not related to acute respiratory distress syndrome.
Causes of neonatal respiratory distress syndrome
Respiratory distress syndrome of the newborn usually occurs when the baby's lungs do not produce enough surfactant, a protein and fat substance that helps maintain lung inflation and prevents them from collapsing. The fetal lungs usually start producing surfactant somewhere between 24 and 28 weeks of pregnancy. Most babies produce enough surfactant by 34 weeks to breathe on their own at birth at that time. If the baby is born earlier, then there is a high probability of insufficient production of surfactant. More often, respiratory distress syndrome affects premature babies, for example, when:
- mother has diabetes;
- the child is underweight;
- The child's lungs are not developing properly.
Approximately half of all babies born between 28 and 32 weeks of gestation develop this condition. In recent years, the number of premature babies born with respiratory distress syndrome has decreased due to steroid injections that can be given to mothers at risk of preterm birth.
Symptoms of respiratory distress syndrome
Symptoms of neonatal respiratory distress syndrome are often noticeable immediately after birth and worsen over the next few days. These may include:
- blue lips, fingers and toes of a newborn;
- rapid, shallow breathing;
- flaring nostrils;
- grunting sound when breathing.
Diagnosis of respiratory distress syndrome
A number of tests are used to diagnose neonatal respiratory distress syndrome and rule out other possible causes. These include:
These include:
- physical examination;
- blood tests to measure the amount of oxygen in the child's blood and check for infection;
- pulse oximetry test to measure the amount of oxygen in a child's blood using a sensor attached to a finger, toe, or ear;
- X-ray or CT scan of the chest to determine the characteristic cloudy appearance of the lungs in distress syndrome.
Respiratory Distress Treatment
The main goal of treating respiratory distress syndrome is to help the child breathe.
Treatment before birth
If there is a high risk of preterm birth before 34 weeks of gestation, treatment for RDS can be started before delivery. For this, a single injection of steroids is performed, and then the second dose is administered 24 hours after the first. Steroids stimulate the development of the baby's lungs and the production of surfactant. Treatment is estimated to help prevent respiratory distress syndrome in a third of preterm births.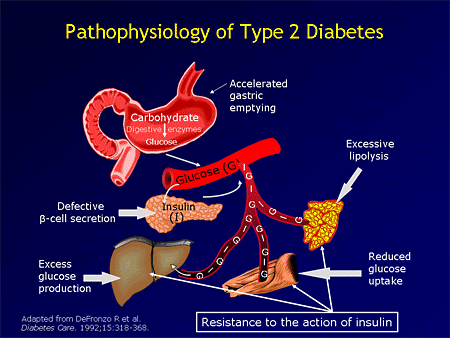 The patient may also be offered magnesium sulfate to reduce the risk of developmental problems associated with early birth. If the course of treatment with magnesium sulfate is more than 5-7 days or is carried out several times during pregnancy, then additional examinations may be offered to the newborn child. This is because long-term use of magnesium sulfate during pregnancy rarely leads to bone problems in newborns.
The patient may also be offered magnesium sulfate to reduce the risk of developmental problems associated with early birth. If the course of treatment with magnesium sulfate is more than 5-7 days or is carried out several times during pregnancy, then additional examinations may be offered to the newborn child. This is because long-term use of magnesium sulfate during pregnancy rarely leads to bone problems in newborns.
Postpartum care
A newborn with respiratory distress syndrome may be transferred to a specialized unit for premature babies (neonatal unit). If the symptoms are mild, he may only need supplemental oxygen. It is usually injected into the nose through an incubator or through a tube. If the symptoms are more severe, the child will be put on a breathing machine (ventilator) to either support or take over his breathing. These procedures are often started immediately in the delivery room before transfer to the neonatal unit. Also, a child with respiratory distress syndrome may be given a dose of artificial surfactant through a breathing tube. Evidence suggests that early treatment within 2 hours of delivery is more effective than if it is delayed. Distressed children will also be given fluids and food through a tube connected to a vein. Some will only need help with breathing for a few days, but some premature babies, usually born earlier, may need support for weeks or even months. The length of a baby's stay in the neonatal unit will depend on how early he was born and what his condition is.
Evidence suggests that early treatment within 2 hours of delivery is more effective than if it is delayed. Distressed children will also be given fluids and food through a tube connected to a vein. Some will only need help with breathing for a few days, but some premature babies, usually born earlier, may need support for weeks or even months. The length of a baby's stay in the neonatal unit will depend on how early he was born and what his condition is.
Complications of neonatal respiratory distress syndrome
Most infants with respiratory distress syndrome can be successfully treated, although they remain at an increased risk of developing other problems later in life.
Sometimes air can escape from the child's lungs and accumulate in the child's chest. This condition is called pneumothorax. The air pocket puts extra pressure on the lungs, causing them to collapse and leading to additional breathing problems. Air leaks can be repaired by inserting a tube into the chest to allow trapped air to escape.
Distressed babies have a significantly increased risk of bleeding inside the lungs (pulmonary hemorrhage) and the brain (cerebral hemorrhage). Pulmonary bleeding is treated with air pressure from a ventilator to stop it and a blood transfusion. Cerebral hemorrhage is quite common in premature babies, but most bleeding is mild and does not cause long-term problems.
Occasionally, ventilation started within 24 hours of birth or a surfactant used to treat respiratory distress syndrome causes scarring of the baby's lungs, which affects their development. This complication is called bronchopulmonary dysplasia. Symptoms of dysplasia include rapid shallow breathing and shortness of breath. Babies with a severe complication like this usually need supplemental oxygen through their nose to help them breathe. Supplemental oxygen support is usually needed for several months while the lungs heal. But some children with bronchopulmonary dysplasia may need regular medications, such as bronchodilators, to widen the airways and make breathing easier.
If a child's brain is damaged as a result of the development of respiratory distress syndrome, either due to bleeding or lack of oxygen, all this can lead to long-term developmental disabilities, such as learning difficulties, movement problems, hearing impairment and vision. But these developmental problems are usually not serious. For example, a study found that 3 out of 4 children with developmental problems have only mild disabilities, which should not prevent them from leading a normal adult life.
Author: Belyakov Nikolai Grigorievich
Specialization: Pediatrician
Where does the appointment: Clinic General Medical Center (GMC), St. Petersburg
4.5+
Zakharova Victoria Valerievna
Specialization: Pediatrician
Medical experience: since 2016
Where does the reception: MC Baltmed Ozerki
Malina Valeria Aleksandrovna
Specialization: Pediatrician
Medical experience: since 2019
Where does the reception: MC Baltmed Ozerki
Egorova Nina Alexandrovna
Specialization: Pediatrician
Medical experience: since 2011
Where does the reception: MC Baltmed Ozerki
Kovzalova Irina Sergeevna
Specialization: Pediatrician
Medical experience: since 2021
Where does the reception: MC Baltmed Ozerki
Pushkareva (Vinogradova) Irina Alekseevna
Specialization: Cardiologist, Pediatrician
Medical experience: since 2009
Place of admission: MC Baltmed Ozerki, Clinical Hospital No. 31, Medswiss Gakkelevskaya
31, Medswiss Gakkelevskaya
Bunyakova Elena Vladimirovna
Specialization: Pediatrician, Rheumatologist
Medical experience: since 2008
Where does the reception: MC Baltmed Ozerki
Strekalova Elena Vladimirovna
Specialization: Therapist, Pediatrician, General Practitioner
Medical experience: since 1999
Where does the reception: MC Baltmed Ozerki
Klimanova Darya Alexandrovna
Specialization: Pediatrician, Neonatologist, Allergist, Immunologist
Medical experience: since 2013
Where does the reception: MC Baltmed Ozerki
Tashtemirov Tokhirjon Makhamatvosilovich
Specialization: Pediatrician
Medical experience: since 2019
Where does the reception: MC Medicenter
Normurodov Alisher Khusan ugli
Specialization: Pediatrician
Medical experience: since 2019
Where does the reception: Medicenter
Markov Anton Ivanovich
Specialization: Pediatrician
Medical experience: since 2011
Where does the reception: MC Medicenter
Babikova Daria Konstantinovna
Specialization: Pediatrician
Medical experience: since 2019
Where does the reception: MC Medicenter
Kim Irina Efremovna
Specialization: Pediatrician
Medical experience: since 1985
Where does the reception: MC Medicenter
Egorova Victoria Alexandrovna
Specialization: Pediatrician
Medical experience: since 2016
Where does the reception: MC Medicenter
Anastasia Anatolyevna Voloshina
Specialization: Pediatrician
Medical experience: since 2020
Where does the reception: MC Medicenter
Budginayte Ksenia Alexandrovna
Specialization: Endocrinologist, Pediatrician
Medical experience: since 2018
Where does the reception: MC Medicenter, Children's Medical Center ONNI
Alla Belyakova
Specialization: Neurologist, Pediatrician, Reflexologist
Medical experience: since 1983
Where does the reception: MC Medicenter, MC Profimedica, MC Family Doctor
Bashmakova Elena Olegovna
Specialization: Pediatrician
Medical experience: since 2018
Where does the reception: Polikarpov Medical Center Medical Center
Anastasia Vasilievna Baramyka
Specialization: Pediatrician
Medical experience: since 2006
Where does the reception: MC Medicenter
Balkova Irina Anatolyevna
Specialization: Pediatrician
Medical experience: since 2013
Where does the reception: MC Medicenter
Radchenko Sergey Ivanovich
Specialization: Gastroenterologist, Pediatrician, General Practitioner
Medical experience: since 1989
Where does the reception: Polikarpov Medical Center Medical Center
Tarasova Rosina Vasilievna
Specialization: Neurologist, Ultrasound Doctor, Pediatrician
Medical experience: since 1990
Where does the reception: MC Medpomoshch 24 Zanevsky, Clinic Miracle Children
Abramova Elena Mikhailovna
Specialization: Pediatrician
Medical experience: from 1976 years old
Where does the reception: MC Energy of Health, MC Poem of Health
Bystritskaya Natalya Vladimirovna
Specialization: Pediatrician
Medical experience: since 1989
Where does the reception: MC Long Vita, Research Institute of Obstetrics and Gynecology. Otta
Otta
Bochkova Olga Yurievna
Specialization: Gastroenterologist, Pediatrician
Medical experience: since 2006
Where does the reception: SM-Clinic on Vyborgsky
Khvatova Elena Anatolyevna
Specialization: Ultrasound doctor, Gastroenterologist, Pediatrician
Medical experience: since 2006
Where does the appointment: SM-Clinic on Danube, SM-Clinic on Malaya Balkanskaya
Svechina Evgenia Alekseevna
Specialization: Gynecologist, Pediatrician
Medical experience: since 2010
Where does the reception: SM-Clinic on Danube
Lidia Alvinovna Nereutsa
Specialization: Pediatrician, Pulmonologist, Allergist, Immunologist
Medical experience: since 2003
Where does the reception: SM-Clinic on Danube
Borisova Daria Sergeevna
Specialization: Pediatrician, Pulmonologist
Medical experience: since 2016
Where does the reception: SM-Clinic on Vyborgsky
Laborer Ksenia Andreevna
Specialization: Pediatrician
Medical experience: since 2013
Where does the reception: SM-Clinic on Marshal Zakharov, Children's Clinic No.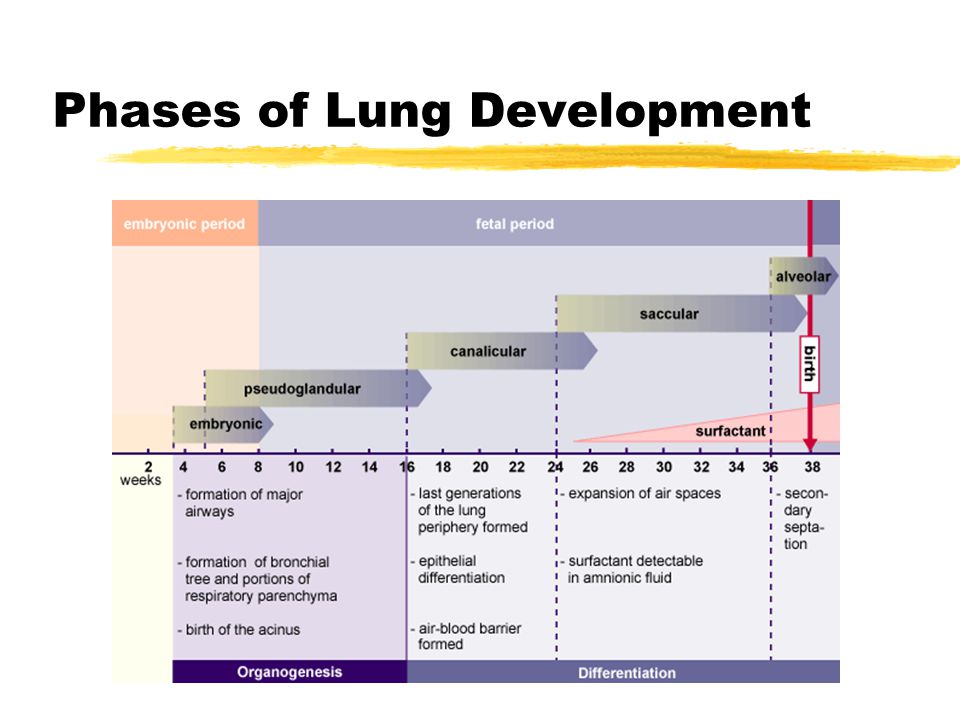 75
75
Olga V. Lashcheva
Specialization: Endocrinologist, Pediatrician
Medical experience: since 2003
Where does the reception: SM-Clinic on Udarnikov
Terekhova Olga Borisovna
Specialization: Gastroenterologist, Pediatrician
Medical experience: since 2010
Where does the reception: SM-Clinic on Udarnikov
Mikhailova Victoria Evgenievna
Specialization: Gastroenterologist, Pediatrician
Medical experience: since 2010
Where does the reception: SM-Clinic on Vyborgsky
Belotitskaya Valeria Eduardovna
Specialization: Gastroenterologist, Pediatrician
Medical experience: since 2015
Where does the reception: SM-Clinic on Danube
Meshcheryakova Irina Fedorovna
Specialization: Cardiologist, Pediatrician
Medical experience: since 1999
Where does the reception: SM-Clinic on Udarnikov
Goltsman Kirill Efimovich
Specialization: Somnologist, Pediatrician, Doctor of functional diagnostics, Epileptologist
Medical experience: since 2013
Where he receives: Clinic Osnova Children, Clinic of the Pediatric Academy
Tarasova Larisa Anatolyevna
Specialization: Gastroenterologist, Pediatrician, Nephrologist, Infectionist
Medical experience: since 1989
Where does the appointment: Dr.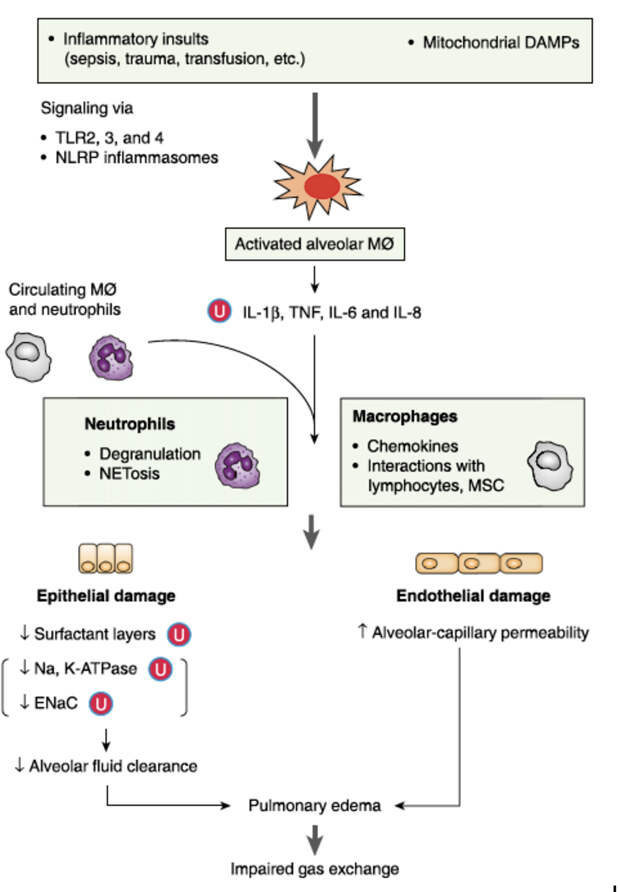 Pel's Clinic
Pel's Clinic
Ulyanova Inna Vladimirovna
Specialization: Hepatologist, Pediatrician, Pulmonologist, Infectionist
Medical experience: since 1990
Where does the appointment: Dr. Pel's Clinic
Kudryashova Maria Yurievna
Specialization: Cardiologist, Pediatrician, Doctor of functional diagnostics
Medical experience: since 1990
Where does the appointment: Dr. Pel's Clinic, MEDA Clinic, Children's Clinic No. 39
References:
- Grebennikov V.A. et al. Respiratory distress syndrome of newborns. Replacement therapy with synthetic surfactant Exosurf Neonatal. M. -1995. -S. 10-16, 54-69
- Bagdatiev V. E. Respiratory distress syndrome / V. E. Bagdatiev, V. A. Gologorsky, B. R. Gelfand // Vestn. intensive care. 1996. - No. 2. - S. 15-25.
- Kuzovlev A.N., Moroz V.V., Golubev A.M., Zarzhetsky Yu.V. Differential diagnosis of pneumonia and acute lung injury // Mat.
 All-Russian conference with international participation "Belomorsky Symposium III". 2009. Arkhangelsk. S. 81.
All-Russian conference with international participation "Belomorsky Symposium III". 2009. Arkhangelsk. S. 81. - Bochun O.N., Savello V.E., Zhidkov K.P. The role of computed tomography in the detection of pulmonary complications in traumatic disease / International Congress "Nevsky Radiological Forum-2005m: Materials of the Congress.-SPb.2005.-C.326.
- Tyurin I.E. Computed tomography of the chest cavity. S-PB., 2006.
Latest diagnostic articles
Lung transplant
A lung transplant is an operation to remove and replace a diseased lung with a healthy lung from a donor. The donor is usually a deceased person, but in rare cases, part of a lung may be taken from a living donor. Lung transplants are performed infrequently, mainly due to a lack of available donors as the demand for transplants far exceeds the available supply of donated lungs. This means that an organ transplant will only be performed if there is a relatively high chance of success.